Abstract
Objective: To investigate the effect of individualized positive end-expiratory pressure (PEEP) titration on intraoperative respiration and circulation in elderly patients undergoing spinal surgery in prone position under general anesthesia. Methods: We prospectively selected 80 elderly patients (39 males and 41 females) aged over 65 years old, at American Society of Anesthesiologists (ASA) grade II or III, who underwent elective prone spinal surgery under general anesthesia, for this study. These patients were randomly divided into titration group and control group, with 40 cases in each group. PEEP of the titration group was increased from 0 to 20 cmH2O by steps of 2 cmH2O. For the control group, PEEP was constantly at 5 cmH2O and ventilation was maintained throughout the surgery. Dynamic pulmonary compliance (Cdyn) measurements were recorded when each PEEP level was kept for 1 min during titration, and individualized PEEP was determined by maximal Cdyn. MAP (mean arterial pressure), heart rate (HR), and CVP (Central venous pressure) were recorded at the set of prone position (T0), PEEP ventilation for 10 min (T1), 30 min (T2), 60 min (T3), end of surgery (T4), and 20 min after extubation (T5). Mean airway pressure (Pmean) and Cdyn were recorded from T0 to T4. Blood gas analysis was performed from T0 to T5 to calculate intrapulmonary shunt fraction (Qs/Qt) and OI (PaO2/FiO2). The rate of phenylephrine use during mechanical ventilation and the incidence of postoperative pulmonary complications were also recorded. Results: The individualized PEEP obtained by titration for 1 min in the titration group was (12.38±2.67) cmH2O, which was significantly higher than the 5 cmH2O in constant PEEP of the control group (P<0.05). There was no significant difference in MAP, HR, and CVP between the two groups at different time points, and no significant difference was noted in Pmean between the two groups from T0 to T4 (all P>0.05). From T2 to T4, Cdyn was significantly higher, and Qs/Qt was lower in the titration group than those in the control group (all P<0.05). From T2 to T5, the OI in the titration group was significantly higher than that in the control group (P<0.05). The rate of phenylephrine use was significantly higher in the titration group than that in the control group (10 patients (25%) vs. 3 patients (8%), P<0.05). The incidence of postoperative pulmonary complications in the titration group was significantly lower than that in the control group (2 cases (5%) vs. 8 cases (20%), P<0.05). Conclusion: Compared with a constant PEEP of 5 cmH2O, intraoperative individualized PEEP titration in elderly patients undergoing spinal surgery in prone position can improve oxygenation, reduce intrapulmonary shunt and postoperative pulmonary complications. (Chinese Clinical Trial Registry, registration number ChiCTR2000040722, https://www.chictr.org.cn).
Keywords: Spinal surgery, prone position, titration, individualization, positive end-expiratory pressure, elderly
Introduction
In general anesthesia, due to inhalation of high concentration of oxygen, myosin drugs and mechanical ventilation can lead to persistent pulmonary atelectasis and postoperative pulmonary complications (PPCs) which may prolong hospital stays and increase mortality. Besides, elderly patients represent a great majority of patients with spinal diseases, and with a decrease in pulmonary function and longer operation time, they can easily develop respiratory and circulatory diseases and atelectasis, resulting from increased thoracoabdominal pressure and anomalous vena caval return caused by prone position during operation [1].
Atelectasis is one of the common complications in patients undergoing surgery in the prone position, which can be effectively prevented by lung-protective ventilation strategy (LPVS) [2-4]. LPVS refers to a respiratory support strategy to reduce alveolar overexpansion, prevent collapse, and bring down the incidence of ventilator-associated lung injury under the premise of maintaining adequate oxygenation, so as to protect and improve pulmonary function, reduce pulmonary complications and decrease the mortality of surgical patients. Such strategy mainly consists of low tidal volume, individualized and moderate positive end-expiratory pressure (PEEP), intermittent lung recruitment and low FiO2, with other auxiliary measures including prone position ventilation, high-frequency oscillatory ventilation and liquid ventilation.
Positive end-expiratory pressure (PEEP), especially individualized PEEP, during which a certain pressure in the end-expiratory airway is maintained under the premise of intermittent positive pressure ventilation, is critical for protecting lung ventilation [5]. However, general and fixed PEEP is not applicable for all patients because of individual differences. As too low PEEP cannot keep the alveoli fully open, effectively improve oxygenation and avoid complications such as atelectasis. In addition, excessive-high PEEP may lead to overexpanded pulmonary alveoli, increase the risk of lung injury and have a greater impact on circulation [6]. Therefore, individualized PEEP has become a major focus in recent studies, including approaches aiming at optimal oxygen, P-V curve, optimal pulmonary compliance, pulmonary stress index, transpulmonary pressure and electrical impedance tomography. Individualized PEEP titration, which often uses dynamic pulmonary compliance (Cdyn) as a clinical indicator, can minimize intrapulmonary shunting and increase oxygen partial pressure [7,8].
For elderly patients, there is no consensus on whether protective ventilation PEEP can bring some benefits. In recent years, the choice of spinal surgery in elderly patients has attracted more and more attention. Most spinal surgery requires reclining, which can significantly reduce lung function and cause respiratory complications associated with surgery. Based on this, this study investigated the effect of Cdyn for individualized PEEP titration on respiration and circulation in elderly patients undergoing spinal surgery in the prone position under general anesthesia. The study was a prospective, single-center, randomized controlled experiment.
Materials and methods
General data
This prospective, single-center, randomized controlled experiment was approved by the hospital Ethics Committee, and signed informed consent was obtained from all patients. We prospectively included 80 elderly patients (39 males and 41 females) aged over 65 years old, who underwent elective prone spinal surgery under general anesthesia from February 2020 to June 2021, in this study.
Inclusion criteria: Patients at ASA grade II to III, with no obvious heart and lung disease; Patients aged over 65 years old; and Patients with a body mass index of 18.5 to 28.0 kg/m2. Exclusion criteria: Patients with chronic lung diseases including chronic obstructive pulmonary disease and lung cancer; Patients with conditions that may affect the compliance of the respiratory system such as thoracic deformity, pneumothorax, and massive pleural effusion; Patients with severe liver and kidney dysfunction, cardiovascular and cerebrovascular diseases; Patients with a forced expiratory volume in the first second/forced vital capacity (FEV1/FVC) ratio <70%; Patients with a smoking history within 8 weeks before surgery; and Patients who refused to participate in the experiment by themselves or their families. Eliminate criteria: Patients with a peak airway pressure (Ppeak) >40 cmH2O during individualized PEEP titration; Patients with time of operation <2 h or >6 h; Patients with intraoperative hemorrhage, anaphylactic shock or other serious complications; or Patients who presented to ICU.
Anesthesia
Peripheral oxygen saturation (SpO2), electrocardiographic (ECG) and MAP (mean arterial pressure) were monitored after admission. Right radial artery puncture was performed under local anesthesia to monitor invasive arterial pressure. Patients breathed pure oxygen spontaneously through a facial mask for 5 min. Then anesthesia was induced with 0.25 to 0.30 μg/kg of sufentanil (Hubei Yichang Humanwell Pharmaceutical Co., Ltd., China), 0.20 to 0.30 mg/kg of etomidate (Jiangsu Nhwa Pharmaceutical Co., Ltd., China), and 0.60 mg/kg of rocuronium (Jiangsu Dongying Pharmaceutical Co., Ltd., China). After successful endotracheal intubation, volume-controlled mechanical ventilation was performed with a Primus anesthesia machine. Ventilation was set at a tidal volume (VT) of 6 mL/kg (standard weight), 60% FiO2, fresh gas flow of 1 L/min, and an I:E ratio of 1:2. The respiratory rate (RR) was adjusted to maintain the partial pressure end-tidal carbon dioxide (PETCO2) at 30 to 35 mmHg. Anesthesia was maintained by intravenous pump injection of 3 to 4 mg/kg/h propofol (Beijing Fresenius Kabi Pharmaceutical Co., Ltd., Germany) and 4 to 8 μg/kg/h remifentanil (Hubei Yichang Humanwell Pharmaceutical Co., Ltd., China). Bispectral index (BIS) value was maintained at 40 to 60, with intermittent intravenous injection of 0.20 mg/kg rocuronium to keep train of four (TOF) count at 0 to 1. Compound sodium lactate (Guangdong Otsuka Pharmaceutical Co., Ltd., China) at a dose of 10 to 20 mL/kg/h was adopted for fluid replacement. Central venous pressure (CVP), PETCO2, mean airway pressure (Pmean), and Cdyn were monitored during surgery.
Grouping and treatment
The patients were randomly divided into two groups by random number table: the titration group and the control group. In the titration group, patients were adjusted to a prone horizontal position, MAP was recorded before the start of surgery, and individualized PEEP titration was conducted. PEEP of the titration group was increased from 0 to 20 cmH2O by steps of 2 cmH2O every 2 min [9,10]. The results of the preliminary test showed that there was no significant difference in Cdyn and oxygenation index (OI) when each PEEP level was kept for 1 min and 2 min. Therefore, in this study, end-expiratory Cdyn at each PEEP level maintained for 1 min during titration was documented, and individualized PEEP was determined by maximal Cdyn. Individualized PEEP ventilation was maintained in the titration group until the end of surgery. For the control group, PEEP was kept constantly at 5 cmH2O and ventilation was maintained throughout the surgery. The control group was ventilated with PEEP 5 cmH2O until the end of surgery. When the decrease in MAP exceeded 10% of the baseline value during surgery, 0.1 mg intravenous bolus of phenylephrine (Shenyang No. 1 Pharmaceutical Co., Ltd., China) was given.
Outcome measures
Primary outcome measures
Cdyn and MAP were recorded at 1 min of titration at each PEEP level in the titration group, and the intrapulmonary shunt fraction (Qs/Qt) and OI were calculated. Hemodynamic index including MAP (mean arterial pressure), heart rate (HR), and CVP (Central venous pressure) was recorded when the prone position (T0) was set up, and PEEP-based ventilation was continued for 10 min (T1), 30 min (T2), 60 min (T3), end of surgery (T4), and 20 min after extubation (T5). Respiratory mechanics including mean airway pressure (Pmean) and Cdyn were recorded from T0 to T4. Radial artery blood and central venous blood of 1 mL each were collected from T0 to T5 for arterial blood gas (ABG) and mixed central venous blood gas (cVBG) analysis using a blood gas analyzer (Osmetech OPTI CCA, USA). Then the blood PH value, partial pressure of carbon dioxide (PaCO2), hemoglobin (Hb), partial pressure of oxygen (PaO2), arterial oxygen saturation (SaO2), mixed venous oxygen saturation (SvO2) and venous partial pressure of oxygen (PvO2) were recorded to calculate Qs/Qt and OI values. The calculation formula is as follows: Alveolar-arterial oxygen partial pressure difference (A - aDO2) = ((PB - PH2O) * FiO2 - PaCO2/R) - PaO2
Arterial oxygen content (CaO2) = (Hb + 1.34) * SaO2 + PaO2 * 0.0031
Mixed venous oxygen content (CvO2) = (Hb + 1.34) * SvO2 + PvO2 * 0.0031
Qs/Qt = P (A - a) DO2 * 0.0031/P (A - a) DO2 * 0.0031 + (CaO2 - CvO2) * 100%
OI = PaO2/FiO2
Secondary outcome measures
The patients’ blood flow mechanics indicators (including MAP, HR, and CVP) at pitch position T0, T1, T2, T3, T4, and T5 were recorded. The rate of phenylephrine use during mechanical ventilation and the occurrence of postoperative pulmonary complications were also documented, including respiratory tract infection, pneumothorax, pleural effusion, respiratory failure, and bronchospasm.
Statistics
Statistical analysis was performed using SPSS 20.0 software. According to the results of the preliminary test with α = 0.05 and statistical power (1 - β) = 0.8, the minimum sample size was calculated to be 32 for each group. Considering a 20% loss rate of follow-up, 40 patients were included in each group. For normally distributed measurement data expressing as mean ± standard deviation (x̅±sd), independent samples t-test was performed for comparison between groups, and repeated measures ANOVA followed with Bonferroni test was conducted for within-group comparison. For enumeration data expressing as case (%), χ2 test or Fisher’s exact probability test was employed for between-group comparisons. Statistical differences were accepted at P<0.05.
Results
Comparison of general data between the two groups
A total of 80 patients were included, with 40 patients in each group, and no patients lost to the study. There was no significant difference in gender, age, BMI, ASA grade, duration of mechanical ventilation, operation time, FEV1/FVC, doses of propofol, remifentanil and compound sodium lactate between the two groups (all P>0.05). See Table 1. In the titration group, the individualized PEEP obtained by titration for 1 min was (12.38±2.67) cmH2O.
Table 1.
Comparison of general data between the two groups
| Characteristics | Titration group (n = 40) | Control group (n = 40) | t/χ2 | P |
|---|---|---|---|---|
| Male/Female (n) | 18/22 | 21/19 | 0.450 | 0.502 |
| Age (years) | 68.2±6.4 | 67.7±6.8 | 0.339 | 0.736 |
| BMI (kg/m2) | 26.81±4.32 | 25.73±3.50 | 1.255 | 0.213 |
| ASA II/III grade (n) | 16/24 | 18/22 | 0.205 | 0.651 |
| Mechanical ventilation (h) | 3.11±0.80 | 3.23±0.71 | -0.595 | 0.554 |
| Operation time (h) | 2.43±0.52 | 2.54±0.63 | -0.810 | 0.421 |
| FEV1/FVC (%) | 87.12±4.93 | 86.74±5.23 | 0.354 | 0.724 |
| Propofol (mg) | 258.62±37.51 | 267.32±41.84 | -0.980 | 0.330 |
| Remifentanil (μg) | 185.32±77.95 | 173.62±82.43 | 0.653 | 0.516 |
| Compound sodium lactate (mL) | 363.71±87.33 | 382.34±90.52 | -0.936 | 0.352 |
Note: BMI: body mass index; ASA: American Society of Anesthesiologists; FEV1/FVC: forced expiratory volume in the first second/forced vital capacity. χ2: Chi-square test value; t: t-test value.
Comparison of Cdyn, MAP and OI at 1 min of titration for each PEEP level in the titration group
Compared with PEEP = 0, Cdyn and OI were significantly higher at PEEP levels of 12, 14, 16 and 18 cmH2O (all P<0.05) and MAP was significantly lower at PEEP levels of 16, 18 and 20 cmH2O (all P<0.05) in the titration group. Among them, OI was highest at PEEP levels of 12, 14 cmH2O. See Table 2.
Table 2.
Comparison of Cdyn, MAP and OI at 1 min of titration for each PEEP level in the titration group (x̅±sd, n = 40)
| PEEP (cmH2O) | Cdyn (mL/cmH2O) | MAP (mmHg) | OI (mmHg) |
|---|---|---|---|
| 0 | 24.89±4.78 | 83.76±8.34 | 362.41±64.78 |
| 2 | 24.98±5.00 | 83.11±7.80 | 367.98±65.00 |
| 4 | 25.44±4.85 | 82.97±8.23 | 370.44±64.85 |
| 6 | 25.83±5.80 | 82.22±7.80 | 374.33±75.80 |
| 8 | 26.77±5.78 | 82.01±7.87 | 377.64±71.78 |
| 10 | 27.03±5.53 | 81.62±7.85 | 389.93±61.53 |
| 12 | 29.49±6.07* | 81.27±9.23 | 422.49±46.07* |
| 14 | 29.81±5.39* | 80.83±7.39 | 427.81±55.39* |
| 16 | 28.86±5.36* | 79.96±8.63* | 399.86±75.36* |
| 18 | 27.89±5.40* | 78.44±7.68* | 391.49±57.40* |
| 20 | 27.11±5.69 | 77.63±9.37* | 380.13±65.69 |
Note: 1 mmHg = 0.133 KPa; 1 cmH2O = 0.098 KPa.
Compared with PEEP = 0 in the titration group;
P<0.05.
PEEP: positive end-expiratory pressure; Cdyn: dynamic pulmonary compliance; MAP: mean arterial pressure; OI: oxygenation index.
Comparison of MAP, HR and CVP at different time points between the two groups
There was no significant difference in MAP, HR, and CVP between the two groups at different time points (all P>0.05). See Table 3 and Figure 1.
Table 3.
Comparison of MAP, HR and CVP at different time points between the two groups (x̅±sd)
| Indicators | n | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|---|
| MAP (mmHg) | |||||||
| Titration group | 40 | 74.82±8.53 | 84.94±13.92 | 76.15±8.80 | 80.52±8.76 | 84.51±13.44 | 85.56±12.08 |
| Control group | 40 | 77.61±10.02 | 86.63±16.27 | 80.16±12.54 | 84.83±10.61 | 86.90±9.93 | 86.91±9.98 |
| HR (beats/min) | |||||||
| Titration group | 40 | 60.03±7.42 | 71.81±14.66 | 72.13±9.92 | 71.56±11.03 | 75.62±12.61 | 84.93±12.11 |
| Control group | 40 | 63.92±9.33 | 73.82±12.69 | 75.84±11.78 | 74.22±11.27 | 75.68±13.56 | 83.85±14.16 |
| CVP (cmH2O) | |||||||
| Titration group | 40 | 6.86±2.04 | 8.62±2.53 | 9.82±2.51 | 9.46 ±2.13 | 7.58±1.96 | 5.67±2.42 |
| Control group | 40 | 6.36±2.39 | 8.51±2.27 | 8.76±1.89 | 8.55±1.76 | 7.62±2.35 | 5.73±1.86 |
Note: 1 mmHg = 0.133 KPa; 1 cmH2O = 0.098 KPa. MAP: mean arterial pressure; HR: heart rate; CVP: central venous pressure; T0: prone position; T1: PEEP ventilation for 10 min; T2: PEEP ventilation for 30 min; T3: PEEP ventilation for 60 min; T4: at the end of surgery; T5: 20 min after extubation.
Figure 1.
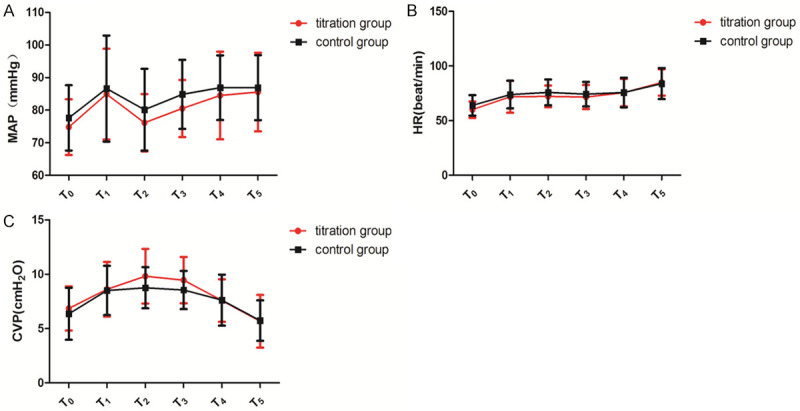
Comparison of MAP, HR and CVP at different time points between the two groups. A: Comparison of MAP at different time points between the two groups; B: Comparison of HR at different time points between the two groups; C: Comparison of CVP at different time points between the two groups. MAP: mean arterial pressure; HR: heart rate; CVP: central venous pressure.
Comparison of Pmean and Cdyn at different time points between the two groups
There was no significant difference in Pmean between the two groups from T0 to T4 (all P>0.05). At T0 and T1, no significant difference was observed in Cdyn between the two groups (all P>0.05). The titration group has significantly higher Cdyn than the control group from T2 to T4 (all P<0.05). See Table 4 and Figure 2.
Table 4.
Comparison of Pmean and Cdyn at different time points between the two groups (x̅±sd)
| Indicators | n | T0 | T1 | T2 | T3 | T4 |
|---|---|---|---|---|---|---|
| Pmean (cmH2O) | ||||||
| Titration group | 40 | 17.44±2.12 | 18.61±3.11 | 19.83±2.86 | 19.75±2.65 | 18.56±3.21 |
| Control group | 40 | 16.26±2.41 | 19.23±3.24 | 20.47±4. 55 | 21.37±4.16 | 17.74±3.18 |
| Cdyn (mL/cmH2O) | ||||||
| Titration group | 40 | 24.88±7.84 | 26.59±9.47 | 30.56±4.99* | 30.78±4.46* | 31.26±5.86* |
| Control group | 40 | 25.09±9.32 | 25.87±9.62 | 26.03±5.52 | 25.81±5.39 | 27.62±5.23 |
Note: 1 mmHg = 0.133 KPa; 1 cmH2O = 0.098 KPa.
Compared with control group;
P<0.05.
Pmean: mean airway pressure; Cdyn: dynamic pulmonary compliance; T0: prone position; T1: PEEP ventilation for 10 min; T2: PEEP ventilation for 30 min; T3: PEEP ventilation for 60 min; T4: at the end of surgery.
Figure 2.
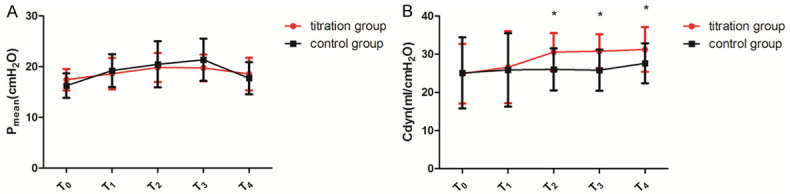
Comparison of Pmean and Cdyn at different time points between the two groups. A: Comparison of Pmean at different time points between the two groups; B: Comparison of Cdyn at different time points between the two groups. Compared with control group, *P<0.05. Pmean: mean airway pressure; Cdyn: dynamic pulmonary compliance.
Comparison of Qs/Qt and OI at different time points between the two groups
There was no significant difference in Qs/Qt between the two groups at T0, T1, and T5 (all P>0.05). Qs/Qt was significantly lower in the titration group than in the control group from T2 to T4 (all P<0.05). No significant difference was found in OI between the two groups at T0 and T1 (all P>0.05). The OI in the titration group was significantly higher than that in the control group from T2 to T5 (all P<0.05).
Compared with T1, Qs/Qt was significantly lower and OI was significantly higher in the titration group from T2 to T4 (P<0.05). See Table 5 and Figure 3.
Table 5.
Comparison of Qs/Qt and OI at different time points between the two groups (x̅±sd)
| Indicators | n | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|---|
| Qs/Qt | |||||||
| Titration group | 40 | 9.78±4.54 | 9.56±3.39 | 8.01±3.43*,# | 7.81±3.72*,# | 7.21±4.64*,# | 8.19±4.42 |
| Control group | 40 | 10.16±3.96 | 9.74±3.32 | 9.67±3.57 | 9.48±3.64 | 9.36±4.92 | 9.65±4.31 |
| OI (mmHg) | |||||||
| Titration group | 40 | 354.50±67.48 | 389.43±78.94 | 422.16±59.95*,# | 431.53±60.40*,# | 442.91±61.67*,# | 415.91±53.51* |
| Control group | 40 | 355.97±69.34 | 380.81±79.62 | 389.82±51.78 | 394.43±67.32 | 402.22±66.48 | 383.64±54.19 |
Note: 1 mmHg = 0.133 KPa; 1 cmH2O = 0.098 KPa.
Compared with the control group;
P<0.05.
Compared with T1 of the titrition group;
P<0.05.
Qs/Qt: intrapulmonary shunt fraction; OI: oxygenation index; T0: prone position; T1: PEEP ventilation for 10 min; T2: PEEP ventilation for 30 min; T3: PEEP ventilation for 60 min; T4: at the end of surgery; T5: 20 min after extubation.
Figure 3.
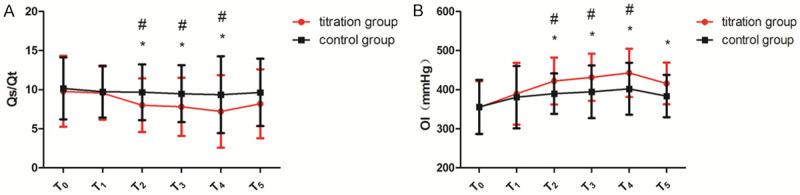
Comparison of Qs/Qt and OI at different time points between the two groups. A: Comparison of Qs/Qt at different time points between the two groups; B: Comparison of OI at different time points between the two groups. Compared with the control group, *P<0.05; compared with T1 of the titration group, #P<0.05. Qs/Qt: intrapulmonary shunt fraction; OI: oxygenation index.
Comparison of phenylephrine usage and postoperative pulmonary complications between the two groups
Significantly higher rate of phenylephrine use was observed in the titration group than in the control group (10 patients (25%) vs. 3 patients (7.5%), P<0.05). The incidence of pulmonary complications after surgery in the titration group was significantly lower than that in the control group (2 cases (5%) vs. 8 cases (20%), P<0.05). See Table 6.
Table 6.
Comparison of phenylephrine usage and postoperative pulmonary complications between the two groups (n = 40, n, %)
| Group | Phenylephrine usage | Pulmonary complications |
|---|---|---|
| Titration group | 10 (25) | 2 (5) |
| Control group | 3 (7.5) | 8 (20) |
| χ2 | 4.501 | 4.114 |
| P | 0.034 | 0.043 |
Note: χ2: Chi-square test value.
Discussion
Currently, perioperative lung protective ventilation strategies mainly include small tidal volume, moderately positive end expiratory pressure, intermittent lung recruitment, low driving pressure, permissive hypercapnia, and low inspired oxygen concentration [9]. Among them, the use of small tidal volume has been proven to improve the prognosis of patients, but if a certain level of PEEP is not applied at the same time, the protective benefits of small tidal volume ventilation may be reduced or even disappear [10]. Simple low tidal volume ventilation can increase alveolar instability, cause atelectasis, and cause ventilation-perfusion ratio imbalance. PEEP can re-open the collapsed lung tissue during mechanical ventilation and keep the alveoli open throughout ventilation [11]. How to get the optimal PEEP is still controversial. Lung compliance refers to the change in lung volume caused by a change in unit pressure, which represents the effect of changes in thoracic pressure on lung volume [12]. There are literatures suggesting that in mechanical ventilation, the individualized PEEP level can be determined based on dynamic lung compliance [13], that is, the PEEP pressure produced on maximum dynamic compliance. In this study, individualized PEEP was titrated based on Cdyn under a small tidal volume (6 mL/kg) to study the effect of general anesthesia on the respiratory function of elderly patients undergoing prone spine surgery.
When the patient lies in prone position, the dynamic compliance of the lung decreases, indicating alveolar collapse, and appropriate PEEP can restore the collapsed alveoli [14]. The results of our study showed that compared with fixed PEEP, individualized PEEP (12.38±2.67) cmH2O titrated according to Cdyn contributes to higher OI, lower Qs/Qt, more open alveoli without increasing pulmonary vascular resistance, thereby improving the proportion of ventilatory blood flow. When Cdyn gradually increases, it indicates that alveoli are increasingly re-expanded; while when Cdyn peaks and begins to decrease, it implies that the alveolar recruitment reaches its maximum level, and higher barometric pressure may aggravate airway and alveolar injury [15,16]. Some studies have adopted PEEP at 12 cmH2O as a means of lung recruitment and achieved significant results [17,18]. In this study, Cdyn was higher in patients with individualized PEEP than those with fixed PEEP at 30 and 60 min of ventilation as well as at the end of surgery. Such result is consistent with the research of Sérgio et al. and also in line with relative theory [19]. In conclusion, compared with 5 cmH2O fixed PEEP, the application of individualized PEEP to elderly patients undergoing prone spine surgery can significantly increase the partial pressure of arterial oxygen and improve oxygenation.
When higher PEEP ventilation is applied, decreased blood pressure may occur due to an increase in intrathoracic pressure and a decline in returned blood volume, which necessitates close monitoring of circulation during PEEP for pulmonary recruitment maneuver [20]. Intraoperative hypotension is an important factor affecting the prognosis of surgery. Referring to recent guidelines for blood pressure control, phenylephrine was used in this study to increase blood pressure when MAP was reduced by 10%, in order to attenuate the effect of titration process on circulation [21]. In this study, the rate of phenylephrine use was significantly higher in patients with individualized PEEP titration than in patients with fixed PEEP. Studies [22,23] have shown that PEEP<10 cmH2O has little effect on hemodynamics, PEEP at 20 cmH2O can cause a certain degree of decrease in blood pressure [15], but when PEEP reaches 30 cmH2O, it will cause a significant decrease in cardiac index [24,25], so 20 cmH2O is often used as the highest level of titrated PEEP in clinical practice. In the study, decreased MAP in patients with titrated PEEP was mainly noticed when the PEEP value reached between 16 to 20 cmH2O. During PEEP titration, MAP decreases as PEEP increases. Although the change in MAP is less correlated with the change in PEEP, this study shows that significant change in PEEP has a certain impact on hemodynamics. Compared with 5 cmH2O PEEP, the application of individualized PEEP did not have a differential impact on hemodynamics, while the PEEP titration process has a certain effect on hemodynamic stability.
Postoperative pulmonary complications are an important factor affecting the prognosis of patients. In this study, postoperative pulmonary complications were mainly pleural effusion, followed by pulmonary infection, which was consistent with the main classification of postoperative pulmonary complications [26]. The patients titrated with individualized PEEP had significantly fewer postoperative pulmonary complications than patients with fixed PEEP. Thus, individualized PEEP is superior to fixed PEEP in terms of improving patient’s outcomes.
Currently, in studies of individualized PEEP titration, there is no uniformity concerning the duration of each PEEP level, which varies from 30 s to 10 min [27,28]. The compliance curve needs to be completed during titration. However, during PEEP titration, due to the fact that the Cdyn of patients has been dynamically changing because of surgical procedures, very short expiratory time increases the difficulty of determining true Cdyn, and prolonged time interval not only increases the duration of titration, but also raises the risk of lung injury and hypotension [29,30]. The results of this study revealed that satisfactory individualized PEEP could be obtained with each level lasting for 1 min during titration, which had little effect on respiration and circulation. Although individualized PEEP titration was performed at the beginning of surgery, the ventilatory function of the lung will be changed during mechanical ventilation. Therefore, the required PEEP level may vary after prolonged surgery. Since inflammatory indicators were not measured in this study, their effect on PEEP setting needs to be further validated. This study is a single-center randomized controlled clinical trial with a small sample size. In addition, further investigation should be focused on individualized PEEP in obese, young, and middle-aged patients during spinal surgery in prone position.
Taken together, compared with a constant PEEP of 5 cmH2O, individualized PEEP titration with each PEEP level merely kept for 1 min during titration in elderly patients undergoing spinal surgery in prone position can better improve oxygenation, reduce intrapulmonary shunt and postoperative pulmonary complications.
Disclosure of conflict of interest
None.
References
- 1.Lin HF, Cheng F, Huang M, Wang CZ. Influential factors of early pulmonary complications after laparoscopic surgery in elderly patients. J Pract Med. 2018;034:2213–2216. [Google Scholar]
- 2.Spadaro S, Karbing DS, Mauri T, Marangoni E, Mojoli F, Valpiani G, Carrieri C, Ragazzi R, Verri M, Rees SE, Volta CA. Effect of positive end-expiratory pressure on pulmonary shunt and dynamic compliance during abdominal surgery. Br J Anaesth. 2016;116:855–861. doi: 10.1093/bja/aew123. [DOI] [PubMed] [Google Scholar]
- 3.Al-Otaibi K. Complications of 411 laparoscopic urological procedures: a single surgeon experience. Urol Ann. 2018;10:308–312. doi: 10.4103/UA.UA_190_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu SF, Tian SY, Li C, Zhang WJ, Wang X, Zhang HB, Su XS, Yuan X. Application of intermittent apnea combined with low-level PEEP ventilation strategy in flexible ureteroscopy. J Clin Anesthesiol. 2020;36:881–885. [Google Scholar]
- 5.Dong Y, Jia YNE, Yang LX, Quan RX. Study on the effect of perioperative pulmonary protective ventilation strategy on lung function, inflammatory reaction and lung complications in patients with esophageal cancer laparoscopy. J Prac Cardio Cere Vas Dis. 2019;27:43–47. [Google Scholar]
- 6.Zhang AY, Wang ZW. Effect of positive end expiratory pressure on hemodynamics and hemodynamics in patients with severe sepsis after inhalation. J Clin Pulmonary Med. 2019;24:988–991. [Google Scholar]
- 7.Mazzinari G, Diaz-Cambronero O, Alonso-Iñigo JM, Garcia-Gregorio N, Ayas-Montero B, Ibañez JL, Serpa Neto A, Ball L, Gama de Abreu M, Pelosi P, Maupoey J, Argente Navarro MP, Schultz MJ. Intraabdominal pressure targeted positive end-expiratory pressure during laparoscopic surgery: an open-label, nonrandomized, crossover, clinical trial. Anesthesiology. 2020;132:667–677. doi: 10.1097/ALN.0000000000003146. [DOI] [PubMed] [Google Scholar]
- 8.Spadaro S, Mauri T, Böhm SH, Scaramuzzo G, Turrini C, Waldmann AD, Ragazzi R, Pesenti A, Volta CA. Variation of poorly ventilated lung units (Silent Spaces) measured by electrical impedance tomography to dynamically assess recruitment. Crit Care. 2018;22:26. doi: 10.1186/s13054-017-1931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao YJ, Cao JB, Mi WD. Progress in the application of lung protective ventilation strategies in the perioperative period. J Clin Anesthesiol. 2016;32:1229–1232. [Google Scholar]
- 10.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369:2126–36. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 11.Watson X, Chereshneva M, Odor PM, Chis Ster I Pan-London Perioperative Audit and Research Network (PLAN) Cecconi M. Adoption of lung protective ventilation in patients undergoing emergency laparotomy: the ALPINE study. A prospective multicentre observational study. Br J Anaesth. 2018;121:909–917. doi: 10.1016/j.bja.2018.04.048. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Wang H, Wang HJ, Zhao X, Li ST, Chen LH. Exploring the intraoperative lung protective ventilation of different positiveend-expiratory pressure levels during abdominal laparoscopic surgery with trendelenburg position. Ann Transl Med. 2019;7:171. doi: 10.21037/atm.2019.03.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrando C, Mugarra A, Gutierrez A, Carbonell JA, García M, Soro M, Tusman G, Belda FJ. Setting individualized positive end-expiratory pressure level with a positive end-expiratory pressure decrement trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesth Analg. 2014;118:657–665. doi: 10.1213/ANE.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 14.Park M, Ahn HJ, Kim JA, Yang M, Heo BY, Choi JW, Kim YR, Lee SH, Jeong H, Choi SJ, Song IS. Driving pressure during thoracic surgery: a randomized clinical trial. Anesthesiology. 2019;130:385–393. doi: 10.1097/ALN.0000000000002600. [DOI] [PubMed] [Google Scholar]
- 15.Zhu C, Yao JW, An LX, Bai YF, Li WJ. Effects of intraoperative individualized PEEP on postoperative atelectasis in obese patients: study protocol for a prospective randomized controlled trial. Trials. 2020;21:618. doi: 10.1186/s13063-020-04565-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Su XS, Tian SY, Wang X, Nie LX, Yuan X, Zhang R, Li C, Liu SF. Effect of dynamic lung compliance-guided PEEP titration on extravascular lung water in elderly patients undergoing robot-assisted radical prostatectomy. Chin J Anesthesiol. 2019;039:415–417. [Google Scholar]
- 17.Nieman GF, Satalin J, Andrews P, Aiash H, Habashi NM, Gatto LA. Personalizing mechanical ventilation according to physiologic parameters to stabilize alveoli and minimize ventilator induced lung injury (VILI) Intensive Care Med Exp. 2017;5:8. doi: 10.1186/s40635-017-0121-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong H, Nari W, Yiri DU. Effects of positive end expiratory pressure ventilation on endothelial function during general anesthesia in patients with obstructive sleep apnea syndrome patient. J Clin Anesthesiol. 2018;34:456–458. [Google Scholar]
- 19.Pereira SM, Tucci MR, Morais CCA, Simões CM, Tonelotto BFF, Pompeo MS, Kay FU, Pelosi P, Vieira JE, Amato MBP. Individual positive end-expiratory pressure settings optimize intraoperative mechanical ventilation and reduce postoperative atelectasis. Anesthesiology. 2018;129:1070–1081. doi: 10.1097/ALN.0000000000002435. [DOI] [PubMed] [Google Scholar]
- 20.Zhao Z, Chang MY, Chang MY, Gow CH, Zhang JH, Hsu YL, Frerichs I, Chang HT, Möller K. Positive end-expiratory pressure titration with electrical impedance tomography and pressure-volume curve in severe acute respiratory distress syndrome. Ann Intensive Care. 2019;9:7. doi: 10.1186/s13613-019-0484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D’Antini D, Huhle R, Herrmann J, Sulemanji DS, Oto J, Raimondo P, Mirabella L, Hemmes SNT, Schultz MJ, Pelosi P, Kaczka DW, Vidal Melo MF, Gama de Abreu M, Cinnella G European Society of Anaesthesiology and the PROtective VEntilation Network. Respiratory system mechanics during low versus high positive end-expiratory pressure in open abdominal surgery: a substudy of PROVHILO randomized controlled trial. Anesth Analg. 2018;126:143–149. doi: 10.1213/ANE.0000000000002192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang GL, Li N, Yuan YQ, Chen LM, Fang MP. The effect of positive end expiratory pressure on intra-abdominal pressure in patients with acute respiratory distress syndrome. Mod Diagn Treat. 2017;2:220–221. [Google Scholar]
- 23.Bai YS, Zhai X, Chen ZQ, Wei XZ, Yang MY, Yang C, Zhou XH, Li WS, Li L, Wu JG, Xu JZ, Zhao JH, Wang DY, Qian BP, Zhu ZZ, Hu Y, Sun WQ, Fang M, Zhen ZM, Wang Z, Li CD, Ding WY, Xia L, Shen JX, JI JG, Sun TS, Luo ZJ, Hai Y, Lv GH, Hao DJ, Qiu Y, Li M. Expert consensus on perioperative management strategies for degenerative scoliosis surgery to accelerate rehabilitation surgery. Acad J Second Milit Med Uni. 2020;41:7–16. [Google Scholar]
- 24.Li XD, Li T, Di XW. Study on the effect of optimal positive end expiratory pressure based on pulmonary artery pressure on oxygenation index and hemodynamics in patients with ARDS. Chin J Crit Care Med. 2020;40:5. [Google Scholar]
- 25.Xu TX, Yang JZ, Peng P. The effect of different positive end-expiratory pressure levels on the variability of stroke volume during mechanical ventilation of acute respiratory distress syndrome. Chin J Emerg Med. 2016;25:305–309. [Google Scholar]
- 26.Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology; Bluth T, Serpa Neto A, Schultz MJ, Pelosi P, Gama de Abreu M PROBESE Collaborative Group. Bluth T, Bobek I, Canet JC, Cinnella G, de Baerdemaeker L, Gama de Abreu M, Gregoretti C, Hedenstierna G, Hemmes SNT, Hiesmayr M, Hollmann MW, Jaber S, Laffey J, Licker MJ, Markstaller K, Matot I, Mills GH, Mulier JP, Pelosi P, Putensen C, Rossaint R, Schmitt J, Schultz MJ, Senturk M, Serpa Neto A, Severgnini P, Sprung J, Vidal Melo MF, Wrigge H. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs. low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA. 2019;321:2292–2305. doi: 10.1001/jama.2019.7505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soares J, Pavlisko N, Guerrero NH, Williamson A, Giannella-Neto A, Carvalho A. Cardiovascular and respiratory mechanics effects during an alveolar recruitment maneuver followed by a positive end-expiratory pressure (PEEP) titration in dogs anesthetized with isoflurane. Vet Anaesth Analg. 2017;44:1262–1266. [Google Scholar]
- 28.Cheng JL, Yang J, Kang Y. Method for setting positive end-expiratory pressure in patients with mechanical ventilation of acute respiratory distress syndrome. Chin J Resp Crit Care Med. 2019;18:89–92. [Google Scholar]
- 29.Huang LP, Fu H, Wang QS, Tang SL, Peng LS. The influence of different methods to titrate the positive end expiratory pressure on the circulatory dynamics of patients with acute respiratory distress syndrome. Guangdong Med J. 2017;38:2141–2146. [Google Scholar]
- 30.Li G, Rong L, Zhao MJ, Sun J. The effect of bedside ultrasound-guided optimal positive end expiratory pressure on oxygenation index and hemodynamics in patients with acute respiratory distress syndrome. Chin Gen Prac. 2019;22:616–620. [Google Scholar]


