Abstract
Purpose
The pandemic related to the novel coronavirus (COVID-19) has led to a decrease in communicable diseases due to social distancing and mask-wearing. How have the prevalence of otitis media (OM) and its associated procedures changed during the pandemic?
Study design
Retrospective Cohort Study.
Methods
This is a retrospective cohort study using the Pediatric Health Information System® (PHIS) database, which consists of 48 children's hospitals. Regions were defined according to PHIS rules. We compared proportion of OM to total diagnoses codes, and collected mastoiditis, and MT placements from all encounters through January 1, 2019-June 31, 2021.
Results
In April 2020, there was a decrease in mean proportion of OM cases per 100 hospital visits (7 v. 2, p < 0.0001) and this was sustained through 2020 and until June 2021 (6–7 v. 2–4, p < 0.05; p < 0.05). Compared to 2020, the months of April and June 2021 showed an increase in mean proportion of OM cases (6–7 v. 3–4, p < 0.05) while May did not. This relative increase in OM cases through April–June were primarily driven by the South, the Midwest, and the Northeast in April and the South and the Midwest in June. MT procedures followed similar trends. In 2020, there was no difference in mastoiditis as a proportion of OM cases compared to 2019 however there was a statistically higher rate of mastoiditis in 2020 compared to 2021.
Conclusions
The COVID-19 pandemic led to declines in OM and MT case volumes that have started to increase. A geographic relationship may exist, and this connection could be influenced by mask mandates and social distancing.
Keywords: Otitis media, Covid-19, Myringotomy tube, Public health
1. Introduction
Otitis Media (OM) is a common reason for medical visits in children. OM is characterized by inflammation of the middle ear with presence of an effusion (MEE) [1]. Acute otitis media (AOM) is the presence of acute middle ear inflammation, sudden onset effusion, and systemic symptoms which can be recurrent [1]. AOM is a common infection, affecting an average of 8 million children per year [2]. By age three, 60% of children experienced at least one episode of AOM, and 24% experienced >3 episodes [3]. Otitis media with effusion (OME) is the presence of MEE without constitutional symptoms like fevers and otalgia [1]. Chronic OME, defined as effusion lasting longer than three months, is associated with conductive hearing loss, speech delay, and poor school performance [1], [4]. Persistent effusion often leads to ear tubes, especially in children with risk factors [1].
Risk factors for OM include male sex, eustachian tube dysfunction, adenoid hypertrophy, day care attendance, exposure to secondhand smoke, and siblings with OM [2], [3], [4], [5], [6], [7]. Incidence of OM increases during winter whereas breastfeeding during the first 6 months of life has a protective effect [3], [7]. Complications of untreated OM include tympanic membrane perforation, acute mastoiditis, subperiosteal abscess, meningitis, and facial paresis—among others [8]. Though these complications are rare, they can cause morbidity.
The high prevalence of OM in children has been linked to increased health care utilization. Children with recurrent OM have higher outpatient pediatrician visits, emergency department (ED) visits, and antibiotic prescriptions [1], [9]. The outpatient health care costs of managing these children with OM ranged from $300 to $500 per child annually with total medical expenditure estimated to be $4 billion annually [2], [9].
In terms of healthcare burden, the COVID-19 pandemic appears to have reduced rates of OM and subsequent medical and surgical interventions. In Italy, a mandatory lockdown has led to decreased rates of OM, otorrhea, antibiotic utilization, and OME in the first half of 2020 [10], [11]. Similarly, McBride et al. found decreased rates of pharyngitis and AOM during the initial lockdown in Dade County, Wisconsin [12]. The largest study to date on the impact of the COVID-19 pandemic examined Vizient claims data and found that April 2020 Otolaryngology outpatient surgical volumes were 18% compared to pre-pandemic levels with rates of recovery varying by geographic regions [13]. To date, no studies have investigated the effect of the COVID-19 pandemic on the incidence rates of pediatric OM and cases volumes of Myringotomy Tube placement (MT) in the United States.
The purpose of this study is to examine the effect of COVID-19 on pediatric OM diagnoses, OM complications, and MT cases in the US in 2020 and into the beginning of 2021 compared to 2019. Secondarily, certain ethnic populations have been incongruently affected by COVID-19 with 3.5 times higher rates of hospitalization among Hispanics compared to non-Hispanic Whites, according to the CDC [14]. Hence, the second objective of this study is to investigate the impact of socioeconomic and racial/ethnic factors on OM and MT trends. COVID-19 remains ongoing so identification of any implications in equity of care will be crucial to mitigate the impact of the pandemic and strategize ways to provide optimal care.
2. Methods
2.1. Data collection
This study is a retrospective database review of associated OM ICD-10 diagnoses codes, CPT/PCS codes for MT, and mastoiditis ICD-10 diagnoses codes from January 1st, 2019-June 31st, 2021, which includes the most recent data available at the time of this analysis. Total pediatric hospital encounters for all diagnoses during the same time were collected as a denominator for OM diagnoses. Socioeconomic and demographic factors, such as age, median household income based on zip code, race, and ethnicity as well as payer type, were included. All data was collected through the Pediatric Health Information System® (PHIS) database. The PHIS hospitals are comprised of over 48 of the largest and most advanced children's hospitals in USA. Clinical data for the following encounter types were included: clinic, inpatient, ambulatory surgery, emergency department, and observation unit. Regions were defined according to PHIS rules with at least five children's hospitals defined per region. We submitted to both Memorial Hermann Institutional Review Board and The University of Texas Health Science Center at Houston's Institutional Review Board and were granted exemption status.
2.2. Data analysis
The primary outcome was monthly count of individual patient visits with an OM diagnosis code which we defined as an OM case. Monthly counts of OM cases were standardized by monthly count of total hospital visits and reported as distinct cases per 100 hospital visits. The secondary outcome was monthly count of MT placement in individual patients which was reported as total combined inpatient and outpatient monthly procedures as well as inpatient and outpatient procedures separately. Monthly summary statistics across all hospitals were compared for all outcomes between 2019, 2020, and the first half of 2021 by Wilcoxon Rank-Sum test. All analyses were completed in R with two-sided Type I error threshold of 0.05.
When a hospital was missing data, missing values were generated as the median value of the region to which the hospital belonged to. OM and mastoiditis data were further analyzed using fitted linear regression and multilevel negative binomial regression models, respectively.
3. Results
3.1. Trends of otitis media between 2019 and 2020 as a proportion of the Total ICD codes
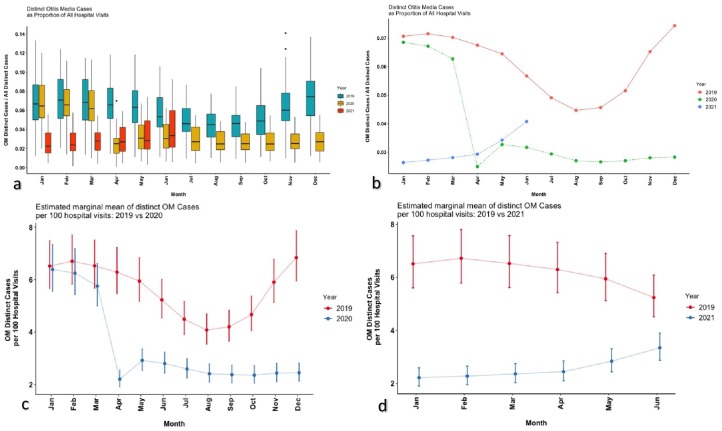
We compared the trends of OM cases as a proportion of total diagnoses codes from all encounters at each hospital (Fig. 1a–c and Supplemental Materials 1–2). Throughout the months of January through March 2019 and 2020, mean OM cases as a proportion of total hospital ICD codes were unchanged from the year prior (6–7 cases per 100 hospital visits). Starting in April 2020, however, there was a sharp decrease in proportional OM cases compared to 2019 (7 v. 2, p < 0.0001) and this decrease was sustained throughout the rest of 2020, with April having the largest relative decrease (Fig. 1a–c and Supplemental Materials 1–2). Geographically, there were no significant differences between the four major regions when comparing 2020 and 2019.
Fig. 1.
a–d. a. Multi-layered box plot with standard error bars that represent the monthly trends of distinct OM cases as a proportion of all hospital visits through the years of 2019, 2020, and 2021. b. Line graph that represents the monthly trends of distinct OM cases as a proportion of all hospital visits through the years of 2019, 2020, and 2021. c. Line graph that shows the estimated marginal mean of distinct OM cases per 100 hospital visits in 2019 compared to 2020. d. Line graph that shows the estimated marginal mean of distinct OM cases per 100 hospital visits in 2019 compared to 2021.
3.2. Trends of otitis media between 2021 vs. 2020 and 2021 vs. 2019 as a proportion of the Total ICD codes
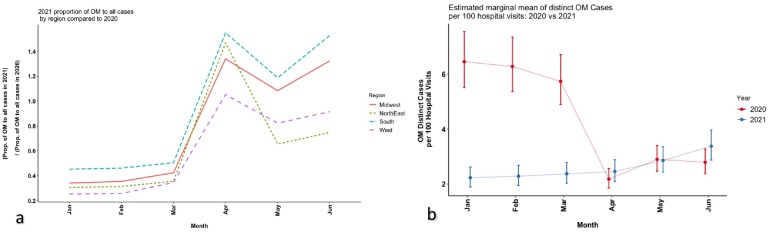
Compared to 2019, every recordable month of 2021 had less OM cases as a proportion of overall hospital cases in comparison to 2019 (3–4 v. 6–7, p < 0.05; Fig. 1a–c and Supplemental Materials 1–2). However, OM cases as a proportion of overall hospital diagnoses started to increase from April–June 2021. Compared to 2020, the months of Jan-March 2021 had a statistically lower proportional OM cases compared to 2020 (Fig. 1a–c and Supplemental Material 1). Yet, April and June had a statistically higher proportional rate of OM cases while May had no difference (Figs. 1d, 2a–b and Supplemental Material 1). The Midwest, the Northeast, and the South all had elevated relative rates of OM in April compared to 2020 while the South and the Midwest had elevated relative rates of OM in May and June (Figs. 1d, 2a–b and Supplemental Material 1).
Fig. 2.
a–b. a. Line graph that shows the regional trends of distinct OM cases per 100 hospital visits in 2021 compared to 2020. b. Line graph that shows the estimated marginal mean of distinct OM cases per 100 hospital visits in 2021 compared to 2020. April 2021 and June 2021 had a statistically significant increase in distinct OM cases per 100 hospital visits while May had no difference between the years.
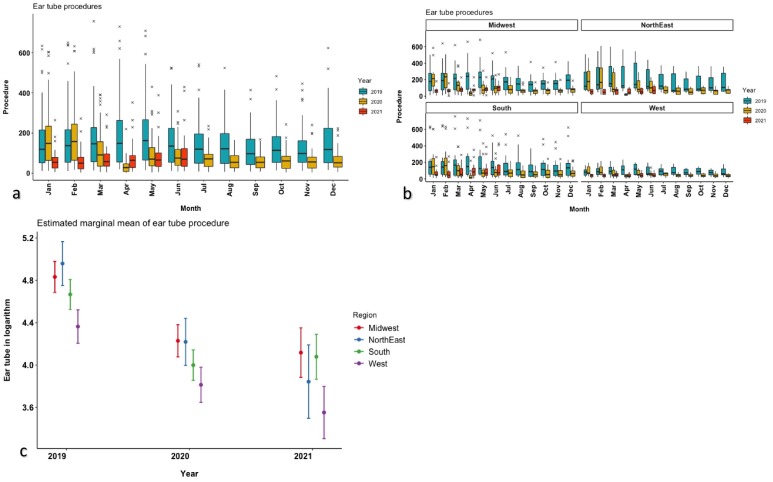
3.3. Trends of MT procedures between 2019, 2020, and the first half of 2021
We compared the trends of MT procedures at each hospital and further analyzed regionally (Fig. 3a–b and Supplemental Material 2). Throughout the months of January through February 2019 and 2020, mean OM cases as a proportion of total hospital ICD codes were unchanged from the year prior (163–177 v. 180–187). Starting in March 2020, however, there was a sharp decrease in MT procedures compared to 2019 (186.54 v. 119.73, p < 0.0001) and this decrease was sustained throughout the rest of 2020, with April having the largest decrease (196.85 v. 28.80, p < 0.0001; Fig. 3a–b and Supplemental Material 2). Compared to 2019, every recordable month of 2021 had less MT procedures in comparison to 2019 (163–199 v. 94, p < 0.05). However, MT procedures started to increase from May–June 2021. The months of Jan–March 2021 had lower proportional OM cases compared to 2020 however April had a higher rate of OM cases while May and June showed no difference. Interestingly, in 2019 and 2020, the West had a lower rate of MT procedures compared to the other three regions however in 2021, the West and the Northeast had a lower MT procedure volume in comparison to the other two regions.
Fig. 3.
a–c. a. Multi-layered box plot with standard error bars that represent the monthly trends of ear tube procedures through the years of 2019, 2020, and 2021. b. Multi-layered box plot with standard error bars that represent the monthly trends of ear tube procedures through the years of 2019, 2020, and 2021 as separated out by region. c. Estimated marginal mean of ear tube procedures grouped by 2019, 2020, and 2021 and separated out by region.
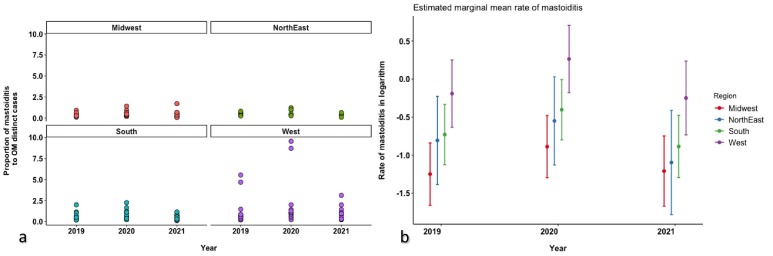
3.4. Trends of mastoiditis between 2019 and 2021
We compared the trends of mastoiditis codes at each hospital as a proportion of overall OM codes and performed further analysis regionally (Fig. 4a–b). Across all regions, 2020 had a higher rate on average compared to 2019, but the difference was not significant. Similarly, there was no difference between 2019 and 2021. However, the proportion of mastoiditis to OM was higher in 2020 compared to 2021 (p < 0.05). Importantly, the West had a higher rate compared to other regions (Fig. 4a–b).
Fig. 4.
a–b. a. Boxplot depicting the proportion of mastoiditis cases to OM distinct cases throughout the years of 2019, 2020, and 2021 and grouped by region. b. Boxplot again depicting the estimated marginal mean rate of mastoiditis in a logarithmic fashion with standard error bars and grouped separately by region and by year. The rate of mastoiditis in 2020 had a significantly higher rate compared to 2021 (p < 0.05).
3.5. Socioeconomic and demographic differences between OM patients in 2019–2021
No clinically significant socioeconomic or demographic differences were found between patients who sought care during 2020 or 2021 compared to 2019 in terms of age, median household income, payer type, race, or ethnicity (Table 1 ).
Table 1.
Demographics of patients with otitis media related diagnoses.
| Demographics | 2019 (N = 446,325) | 2020 (N = 236,279) | 2021 (N = 99,556) | Total (N = 782,160) | p-value |
|---|---|---|---|---|---|
| Race | <0.001 | ||||
| Other | 61,699 (13.8%) | 32,279 (13.7%) | 11,055 (11.1%) | 105,033 (13.4%) | |
| Asian | 11,246 (2.5%) | 5479 (2.3%) | 2300 (2.3%) | 19,025 (2.4%) | |
| Black | 92,167 (20.7%) | 44,905 (19.0%) | 20,129 (20.2%) | 157,201 (20.1%) | |
| Multi-Racial | 7713 (1.7%) | 4501 (1.9%) | 2128 (2.1%) | 14,342 (1.8%) | |
| Unknown | 23,260 (5.2%) | 8471 (3.6%) | 3085 (3.1%) | 34,816 (4.5%) | |
| White | 250,240 (56.1%) | 140,644 (59.5%) | 60,859 (61.1%) | 451,743 (57.8%) | |
| Ethnicity | <0.001 | ||||
| Hispanic/Latino | 100,995 (22.6%) | 51,064 (21.6%) | 19,483 (19.6%) | 171,542 (21.9%) | |
| Not Hispanic/Latino | 306,851 (68.8%) | 169,339 (71.7%) | 77,487 (77.8%) | 553,677 (70.8%) | |
| Unknown | 38,479 (8.6%) | 15,876 (6.7%) | 2586 (2.6%) | 56,941 (7.3%) | |
| Insurance | <0.001 | ||||
| Miscellaneous | 2047 | 1002 | 100 | 3149 | |
| Private | 162,288 (36.5%) | 87,982 (37.4%) | 37,828 (38.0%) | 288,098 (37.0%) | |
| Government | 262,291 (59.0%) | 138,789 (59.0%) | 57,988 (58.3%) | 459,068 (58.9%) | |
| Other | 19,699 (4.4%) | 8506 (3.6%) | 3640 (3.7%) | 31,845 (4.1%) | |
| Admission age in months | <0.001 | ||||
| Median | 28.000 | 31.000 | 28.000 | 29.000 | |
| Q1, Q3 | 14.000, 60.000 | 15.000, 68.000 | 15.000, 64.000 | 14.000, 63.000 | |
| Range | 0.000–1060.000 | 0.000–1083.000 | 0.000–903.000 | 0.000–1083.000 | |
| N | 446,325 | 236,279 | 99,556 | 782,160 | |
| Median household income | <0.001 | ||||
| Median | 41,696.000 | 41,696.000 | 41,961.000 | 41,725.000 | |
| Q1, Q3 | 33,231.000, 54,031.000 | 33,297.000, 54,016.000 | 33,814.000, 54,295.000 | 33,311.000, 54,057.000 | |
| Range | 6320.000–196,032.000 | 6320.000–196,032.000 | 6320.000–196,032.000 | 6320.000–196,032.000 | |
| N | 437,937 | 231,798 | 97,519 | 767,254 |
4. Discussion
Our study sought to understand national trends in OM diagnoses and changes in MT case volume during the COVID-19 pandemic. We found a decline in OM diagnoses starting in April 2020 compared to April 2019 and this decline continued throughout the rest of 2020 and until April 2021. The Midwest and the South had elevated rates of OM throughout April–June 2021 compared to 2020 but was still lower than 2019. The trend of MT procedures generally followed the same trend however the statistically significant decline in procedures started in March 2020. However, the number of mastoiditis cases as a proportion of OM cases increased in 2020 compared to 2021 however was not statistically significantly to 2019. There were no clinically significant socioeconomic or demographic differences in OM patients between 2019 and 2020.
Response to the COVID-19 pandemic varied across the US. The Northeast, specifically New York City, was an epicenter of the COVID-19 pandemic. This was due to higher population density, international airports, and reliance of public transportation in major Northeastern cities. In response, New York and New Jersey declared a state of emergency in early March 2020 with mandatory quarantines [15]. By mid-March 2020, the Surgeon General of the US and US centers for Medicare and Medicaid Services (CMS) put forth recommendations that all healthcare institutions across the country should cease elective procedures in an effort to conserve critical healthcare resources and limit the spread of SARS-CoV-2 virus [15], [16]. States like New York and New Jersey postposed elective cases beginning mid-late March 2020 [15]. In the south, stay-at-home mandates lagged behind the NE and did not begin until late-March to early April and, interestingly, these states were among the first to lift mandatory stay at home orders or change to an advisory order whereas New York and New Jersey continued its mandatory quarantine orders through May 2020 [14]. The stay-at-home orders led to cessation of in-person school/day care and transition to virtual classes for all ages that continued through most of 2020. School closures and quarantine practices not only led to decreased COVID-19 incidence and mortality [17], but also reduced infectious diseases stemming from close personal contact that contribute to OM.
These quarantine mandates and postponement of elective surgeries coincided with the drop in both inpatient and ambulatory MT cases found in our study between March 2020 and April 2020 across the country. The recovery of case volumes observed in this study beginning in late April 2020 through May and June 2020 can be attributed to an announcement by CMS on April 16, 2020, outlining a pathway to reopening facilities for non-emergent procedures, which was followed by the reversal of many executive orders prohibiting elective surgical procedures [18]. While case volumes did recover from May 2020 to September 2020 compared to the lowest levels that were observed, these volumes remained lower than the numbers observed during these same months in 2019. This is likely due to a lower overall incidence of OM and fewer outpatient visits.
Social distancing mandates and school/daycare closures across the US likely played a role in the decreased OM rates and lower MT case volume observed in this study. Day care attendance is a risk factor for OM as children are exposed to viruses from sick day care attendees [7]. Though OM rates increase during winter, this study shows a decline in OM diagnoses starting in March 2020 that persisted through the summer. Proportion of OM in August and September 2020 is still 40% less than the same time in 2019 suggesting that other factors play a role. As the OM rate declined, children likely no longer met criteria for MT placement [19]—another reason explaining the drop in MT cases.
The expansion of telemedicine and decreased outpatient physician visits likely led to declining trends in OM and MT cases. According to The Commonwealth Fund, outpatient visits to ambulatory practices declined by nearly 60% compared to pre-pandemic levels, and while outpatient visits partially recovered, the total number of visits in May 2020 were more than one third lower compared to before the pandemic [20]. Interestingly, this report also found that visits to both pediatricians and surgical specialists, particularly Otolaryngologists, declined during the early stages of the pandemic. Moreover, outpatient visits to Pediatricians and Otolaryngologists did not recover to the same degree as non-surgical specialists [20]. In the emergency setting, DeLaroche et al. found that emergency department (ED) visits at 27 US children's hospitals declined more than 45% between March 15, 2020 to August 31, 2020 compared to prior years [21]. The sharpest decline was for OM (75.1%) followed by URIs (69.6%) [21]. These findings may explain the lower referrals to Pediatricians and Otolaryngologists for further assessment of OM. While this suggests a reluctance to seek medical care, it is plausible that children just became “healthier” due to the ongoing pandemic restrictions. OM pathology, for example, appears to have high rate of self-resolution during periods of lockdown as noted by Torreta et al. who found over 80% of children with recurrent OM having improvement in their practice [10].
Though the rate of communicable disease like URIs and OM decreased during the pandemic, one cannot ignore the possibility that parents are reluctant to seek healthcare for their children for less urgent conditions. However, a retrospective study by Pines et al. showed that emergency visits for serious conditions like appendicitis or septicemia—which warrants hospitalization and intervention—were lower during the early-mid pandemic in 2020 [22]. While this may suggest lack of health care utilization, there was also decreased rates of children presenting dead on arrival or URIs (which can act as precursors severe medical pathologies) [22].
Interestingly, near the middle of the 2021 year both the OM and the MT rates started to increase, which could be associated with social distancing “fatigue” due to less of a concern of the pandemic. Public polling around this time elicited the highest rate of people “not at all” concerned and the least amount of people “very” concerned in over a year [23]. However, healthcare utilization was still lower than prior years [24]. There also may be a geographic tilt in our data, with the Midwest and the South having the higher relative rates of OM throughout April 2021–June 2021 compared to the Northeast and the West. This could be due to expiring pandemic related mandates and lax restrictions in the Southern and Midwestern states [25]. Another theory that could be influencing OM transmission rates could be voluntary mask utilization, which varies geographically [26]. In the paper referenced by Fischer et al., during that period of time, eight states reported at least a 75% mask adherence rate and one of them was either a southern or midwestern state [26]. This increased mask adherence representative in the West and the Northeast could be a factor associated with less increase in OM and MT cases in the April–June 2021 months. Furthermore, March 2021 was when the Delta variant was detected in the US; this more contagious variant led to a surge in pediatric COVID infections [27]. Other respiratory viruses such as RSV have also risen, especially in the South in summer 2021, which is atypical given that RSV is traditionally a winter virus [28].
Our study showed a non-statistically significant increase in mastoiditis cases as a proportion of OM in 2020 and 2021 compared to 2019 however 2020 did have a higher relative rate of mastoiditis in comparison to 2019. This may suggest a shift in OM pathology with a changing disease severity or case mix index (CMI). Similar findings were shown in the presentation given by Kory Kittle and Dr. Matt Hall from the PHIS team, who found that as low severity patients dropped out during the pandemic, the 2020 CMI increased more than expected [29]. Since mastoiditis is often progression of disease from untreated acute otitis media, factors such as delay in care due to the pandemic may play a role.
4.1. Limitations
This study has limitations. First, this data reflects the experience of 48 Children's hospitals in 25 states and one district (Washington, DC), which may limit generalizability to local, state, regional, national, or international scales. Due to pandemic restrictions, caregivers may have sought care closer to home in centers not reflected in the PHIS. Additionally, data entry is subject to errors, although PHIS utilizes data quality checks and updates. Explanations for how the COVID-19 pandemic has affected declines in OM and MT cases are multifactorial and do not offer causality. Additional studies may distinguish new pathologic changes. Finally, the newest change in 2021 has been availability of COVID vaccines for children. However, vaccine uptake has been suboptimal with 46% of children being fully vaccinated [30]. Time will tell how vaccination rates will change as eligibility expands.
5. Conclusions
OM is a common childhood illnesses and MT placement remains the most common childhood surgery. The COVID-19 pandemic has led to a decline in OM and MT cases which may reflect a shift in pediatric population health. Pandemic-related behavioral may play a role in the increasing rates of OM and MT procedures. Additionally, the relative increase in mastoiditis seen in 2020 could represent changing case severity. Further investigation is warranted to delineate the factors responsible.
Meeting information
Panel Presentation at AAO-Head and Neck Surgery Annual Meeting, Los Angeles, CA, October 4, 2021.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
We have no conflicts of interests to disclose.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amjoto.2021.103369.
Appendix A. Supplementary data
Supplementary tables
References
- 1.NS. DP Otitis media: what is new? Curr Opin Otolaryngol Head Neck Surg. 2019;27(6):495–498. doi: 10.1097/MOO.0000000000000591. [DOI] [PubMed] [Google Scholar]
- 2.JA A., SF Acute otitis media, antimicrobial prescriptions, and medical expenses among children in the United States during 2011-2016. Vaccine. 2018;36(49):7479–7486. doi: 10.1016/J.VACCINE.2018.10.060. [DOI] [PubMed] [Google Scholar]
- 3.Kaur R., Morris M., Pichichero M.E. Epidemiology of acute otitis media in the postpneumococcal conjugate vaccine era. Pediatrics. 2017;140(3):20170181. doi: 10.1542/PEDS.2017-0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.BK, FF, ME, ZHD Auditory processing abilities in children with chronic otitis media with effusion. Acta Otolaryngol. 2016;136(5):456–459. doi: 10.3109/00016489.2015.1129552. [DOI] [PubMed] [Google Scholar]
- 5.van I G. Environmental determinants associated with acute otitis media in children: a longitudinal study. Pediatr Res. 2020;87(1):163–168. doi: 10.1038/S41390-019-0540-3. [DOI] [PubMed] [Google Scholar]
- 6.Buzatto G.P., Tamashiro E., Proenca-Modena J.L., et al. The pathogens profile in children with otitis media with effusion and adenoid hypertrophy. PLoS One. 2017;12(2) doi: 10.1371/JOURNAL.PONE.0171049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee J.Y., Kim S.-H., Il Song C., Kim Y.R., Kim Y.-J., Choi J.H. Risk factors for persistent otitis media with effusion in children: a case-control study. Yeungnam UnivJ Med. 2018;35(1):70. doi: 10.12701/YUJM.2018.35.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ren Y., Sethi R.K.V., Stankovic K.M. Acute otitis media and associated complications in United States emergency departments. Otol Neurotol. 2018;39(8):1005. doi: 10.1097/MAO.0000000000001929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.SA, NLS, NB Incremental health care utilization and costs for acute otitis media in children. Laryngoscope. 2014;124(1):301–305. doi: 10.1002/LARY.24190. [DOI] [PubMed] [Google Scholar]
- 10.Torretta S., Capaccio P., Coro I., et al. Incidental lowering of otitis-media complaints in otitis-prone children during COVID-19 pandemic: not all evil comes to hurt. Eur J Pediatr. 2021;180(2):1. doi: 10.1007/S00431-020-03747-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MA, FDB, PM Effects of COVID-19 lockdown on otitis media with effusion in children: future therapeutic implications. Otolaryngol Head Neck Surg. 2021 doi: 10.1177/0194599820987458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.JAM, JE, ERW Impact of COVID-19 quarantine and school cancelation on other common infectious diseases. Pediatr Infect Dis J. 2020;39(12):E449–E452. doi: 10.1097/INF.0000000000002883. [DOI] [PubMed] [Google Scholar]
- 13.Saraswathula A., Gourin C.G., Stewart C.M. National trends in US otolaryngology surgical volume during the early COVID-19 pandemic. AMA Otolaryngol Neck Surg. 2021;147(4):397–399. doi: 10.1001/JAMAOTO.2020.5472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVID-19 Hospitalizations. https://gis.cdc.gov/grasp/covidnet/covid19_3.html. Accessed September 30, 2021.
- 15.COVID-19 Resource Center: Resources for States - Ambulatory Surgery Center Association (ASCA). https://www.ascassociation.org/asca/resourcecenter/latestnewsresourcecenter/covid-19-resources-for-states. Accessed September 30, 2021.
- 16.CMS. CMS Adult Elective Surgery and Procedures Recommendations.
- 17.Auger K.A., Shah S.S., Richardson T., et al. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA. 2020;324(9):859–870. doi: 10.1001/JAMA.2020.14348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.State Resumption of Elective Surgery Orders, Guidance, and Resources. https://www.facs.org/covid-19/archives/legislative-regulatory/state-resumption. Accessed September 30, 2021.
- 19.RMR, SRS, MAP Clinical practice guideline: tympanostomy tubes in children. Otolaryngol Head Neck Surg. 2013;149(1 Suppl) doi: 10.1177/0194599813487302. [DOI] [PubMed] [Google Scholar]
- 20.The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges | Commonwealth Fund. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. Accessed September 30, 2021.
- 21.DeLaroche A.M., Rodean J., Aronson P.L., et al. Pediatric emergency department visits at US Children’s hospitals during the COVID-19 pandemic. Pediatrics. 2021;147(4) doi: 10.1542/PEDS.2020-039628. [DOI] [PubMed] [Google Scholar]
- 22.Jm P., Ms Z., Bs B., et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021;41:201–204. doi: 10.1016/J.AJEM.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.How Americans View Biden’s Response To The Coronavirus Crisis|FiveThirtyEight. https://projects.fivethirtyeight.com/coronavirus-polls/. Accessed September 30, 2021.
- 24.Early 2021 data show no rebound in health care utilization - Peterson-KFF Health System Tracker. https://www.healthsystemtracker.org/brief/early-2021-data-show-no-rebound-in-health-care-utilization/. Accessed September 30, 2021.
- 25.Does Your State Have a Mask Mandate Due to Coronavirus? https://www.aarp.org/health/healthy-living/info-2020/states-mask-mandates-coronavirus.html. Accessed September 30, 2021.
- 26.Fischer C.B., Adrien N., Silguero J.J., Hopper J.J., Chowdhury A.I., Werler M.M. Mask adherence and rate of COVID-19 across the United States. PLoS One. 2021;16(4) doi: 10.1371/JOURNAL.PONE.0249891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Is the delta variant of the coronavirus worse for kids? https://apnews.com/article/delta-variant-coronavirus-kids-4035798709ec77b8acaf96a49d48acfa
- 28.CDC Warning: RSV is spreading in southern U.S., why this is unusural for Respiratory Synctial Virus. https://www.forbes.com/sites/brucelee/2021/06/12/cdc-warning-rsv-is-spreading-in-southern-us-why-this-is-unusual-for-this-respiratory-virus/?sh=c01999944ba8
- 29.Kittle K., Hall M. Children’s Hospital Association; 2020. 2020 Trends: The COVID-19 Pandemic’s Impact on Revenue, Volumes, and Specific Patient Populations [Webinar] [Google Scholar]
- 30.https://covid.cdc.gov/covid-data-tracker/#vaccinations-cases-trends. Accessed October 21, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables