Abstract
The FOURIER (Further Cardiovascular Outcomes Research with PCSK9 inhibition in Subjects with Elevated Risk) trial was conducted to study cardiovascular outcomes of treatment with evolocumab. The trial was terminated after a median follow-up of 2.2 years instead of the planned 3.6 years. We question this decision. According to the investigators, the event rate was 50% higher than expected. However, the accrued number of key secondary events (1829) was only 12% higher than the targeted number (1630). Also, around one-third of the events consisted of non-atherosclerotic myocardial infarctions, hemorrhagic strokes, and cardiovascular deaths unrelated to myocardial infarction or stroke. Moreover, halfway through the trial, the sample size changed from 22,500 to 27,500, even though the accrual of the targeted number of events was on track. Finally, the rate of all-cause mortality had started to diverge in favor of placebo after 2 years of follow-up. It was 4.8% for evolocumab and 4.3% for placebo in participants with > 2.5 years of follow-up. A long-term follow-up would have yielded more events and thus more power to evaluate the effect of evolocumab on all-cause mortality. We conclude that adaptive designs carry a recognized risk of false-positive efficacy results, but the risk of false-negative safety results is underappreciated.
Key Points
| The FOURIER (Further Cardiovascular Outcomes Research with PCSK9 inhibition in Subjects with Elevated Risk) trial included many cardiovascular events that might be unrelated to atherosclerosis. |
| The adaptive design allowed an intermediate increase in the targeted sample size, which resulted in a faster accrual of events and therefore the possibility of shortening the follow-up. |
| The rate of all-cause mortality was growing for evolocumab versus placebo after 2 years of follow-up. |
| The originally planned follow-up of FOURIER would have yielded the necessary evidence about this potential safety issue with evolocumab. |
Introduction
Over recent years, monoclonal antibodies that inhibit proprotein convertase subtilisin-kexin type 9 (PCSK9) have been introduced as a new class of drugs that lower low-density lipoprotein cholesterol (LDL-C). One of these PCSK9 inhibitors is evolocumab, which reduces LDL-C by 60% when used with a statin [1]. In addition, some relatively small phase II and III trials demonstrated a statistically significant reduction in cardiovascular outcomes [1]. To further investigate the effects of evolocumab on cardiovascular outcomes, the large clinical outcomes trial FOURIER (Further Cardiovascular Outcomes Research with PCSK9 inhibition in Subjects with Elevated Risk) was conducted [2].
FOURIER was a randomized, double-blind, placebo-controlled, multicenter, event-driven trial. It included 27,564 patients with atherosclerotic cardiovascular disease and LDL-C levels ≥ 70 mg/dl who were already receiving statin therapy. Patients were randomly assigned to evolocumab (140 mg every 2 weeks or 420 mg monthly) or a matching placebo. The sample size calculation indicated that 1630 key secondary endpoints would provide 90% power to detect a 15% reduction in key secondary events for evolocumab versus placebo. The key secondary endpoint was a composite of cardiovascular death, myocardial infarction (MI), and stroke [2]. These events were expected to accrue during a median follow-up of 3.6 years [3]. The trial’s adaptive design allowed modifications to the trial protocol and statistical plan during the conduct of the trial based on interim review of accrued data.
The study was terminated after a median follow-up of 2.2 years (26 months) when “an event rate that was approximately 50% higher than postulated” had occurred [2]. At that time, the number of key secondary events was 1829, which is only 12% more than required [2]. We question the decision to stop the trial earlier than planned. First, non-atherosclerotic MIs and hemorrhagic strokes were included in the key secondary endpoint. Also, an unusually large number of cardiovascular deaths unrelated to MI or stroke was found. Second, halfway through the trial, the sample size was enlarged, even though the accrual of the targeted number of events was on track. Finally, the increasing rate of all-cause mortality for evolocumab versus placebo after 2 years of follow-up required longer follow-up. We provide evidence that supports our arguments.
Large Number of Non-Atherosclerotic Myocardial Infarctions and Strokes
In FOURIER, MI, which was included in the composite key secondary endpoint, was a composite outcome by itself [2]. The composite outcome MI comprised both spontaneous atherosclerotic MI (type 1) and types of MI that are not always directly related to atherosclerosis, including MI due to a supply–demand imbalance (type 2), cardiac death suggestive of MI without increased biomarkers (type 3), and MI related to revascularization (type 4) and surgical procedures (type 5) [2, 4]. The non-atherosclerotic types might not be relevant in the context of LDL-C-lowering therapy but contributed substantially to the total number of MIs in FOURIER. An analysis of MI subtypes in FOURIER reported a total of 1288 MIs, and 412 (32%) were not type 1 MI [5].
Stroke was also a composite outcome in FOURIER. It encompassed ischemic stroke, hemorrhagic stroke, and stroke of unknown origin [2]. Ischemic stroke is considered to be due to atherosclerotic disease, whereas hemorrhagic stroke seems to be associated with lower rather than higher levels of LDL-C, especially in patients with a history of stroke [6–8]. Hemorrhagic stroke accounted for 54 of 469 strokes (11.5%).
Many Other Cardiovascular Deaths
Additionally, a relatively large number of cardiovascular deaths not caused by MI or stroke were included, i.e., 372 of 491 (76%) cardiovascular deaths [2]. In contrast, in the general population of the USA, cardiovascular deaths not due to MI and stroke account for 40% of annual cardiovascular deaths [9]. In the ODYSSEY OUTCOMES (Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment With Alirocumab) trial investigating the clinical outcomes of alirocumab, 16% of cardiovascular deaths were attributed to causes other than MI or stroke [10], and 13% in clinical outcomes trials of statins [11]. Thus, the 76% in FOURIER seems fairly high and was not explained by the authors. If it had been 13–40%, there would have been 174–235 fewer cardiovascular deaths unrelated to MI and stroke.
Without the non-atherosclerotic MIs, hemorrhagic strokes, and cardiovascular deaths unrelated to MI and stroke, terminating FOURIER earlier than planned would have been unjustified. The non-atherosclerotic MIs (412), hemorrhagic strokes (54), and cardiovascular deaths unrelated to MI and stroke (175–235) formed 35–38% of the reported 1829 key secondary events. Without these 641–701 events, there were just 1128–1188 events when the trial was stopped, which is around 69–73% of the targeted events (1630). Obviously, this number was insufficient, and the trial should have been continued.
Change in Sample Size
The number of accrued key secondary endpoints also indicates that there was no need for protocol changes that would increase the rate of accruing events. The adaptive design had left room for such changes [12, 13], as reported in the original protocol (see the appendix of the main results by Sabatine et al. [2]). It read that Amgen could decide to increase the sample size so that the trial could be completed with at least 1630 key secondary events observed in approximately 58 months. Alternatively, the study duration could be lengthened to ensure the required number of events.
After 1.5 years of follow-up, the planned sample size was increased from 22,500 to 27,500 patients (22% extra) [2, 14]. This protocol change would enable a faster accrual of the targeted number of events, even though that accrual seemed to be on track. Hence, the change made it possible to shorten the follow-up. Remarkably, the change was not mentioned in the main results paper [2] and was not substantiated with new assumptions underlying the sample size calculation in the amended protocol.
Increased Rate of All-Cause Mortality
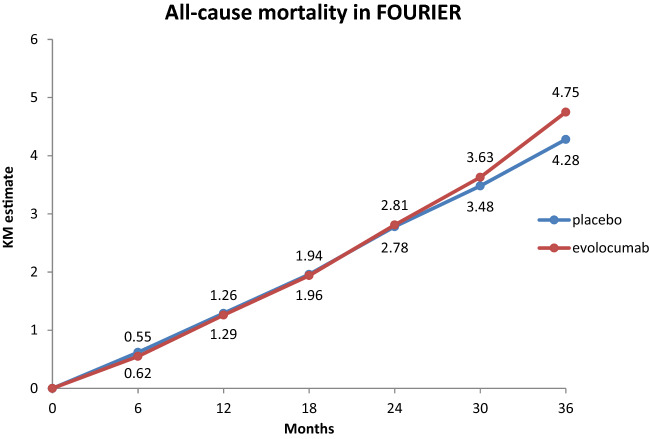
We also question the decision to stop FOURIER earlier than planned because the risk of all-cause mortality in the evolocumab group was growing. Although the main results paper reported a rate of deaths from any cause of 3.2% in the evolocumab group versus 3.1% in the placebo group (hazard ratio [HR] 1.04; 95% confidence interval [CI] 0.91–1.19) [2], cumulative all-cause mortality rates on ClinicalTrials.gov demonstrated that the rate in the evolocumab group was starting to diverge from that in the placebo group after 2 years of follow-up (Fig. 1). It was 4.8% for evolocumab and 4.3% for placebo in participants with >2.5 years of follow-up. A possible problem with all-cause mortality had already been shown in the preceding lipid-lowering trials: the pooled odds ratio was 1.18 (95% CI 0.46–3.02) [15].
Fig. 1.
Cumulative incidence of all-cause mortality in FOURIER. Data are derived from ClinicalTrials.gov. KM Kaplan–Meier
The originally planned follow-up of FOURIER would have yielded the necessary evidence about this potential safety issue with evolocumab. The median and complete follow-up duration would have been longer and the number of deaths higher. Subsequently, the power to detect a difference in the risk of mortality between the treatment groups would have become sufficient. The risk of false-negative findings also applies to other secondary endpoints of FOURIER, such as cardiovascular death not due to MI or stroke (HR 1.10; 95% CI 0.90–1.35), hemorrhagic stroke (HR 1.16; 95% CI 0.68–1.98), new-onset diabetes mellitus (OR 1.05; 95% CI 0.94–1.17), and death in patients with diabetes mellitus at baseline (HR 1.10; 95% CI 0.91–1.32) [2, 16]. If future research confirms the increased risk of mortality, an explanation may be found in a number of these serious adverse events.
Discussion
Termination of the FOURIER trial was explained by the investigators as required because of a larger than expected rate of cardiovascular events, but these consisted of many non-atherosclerotic MIs, hemorrhagic strokes, and cardiovascular deaths unrelated to MI or stroke. The trial results on ClinicalTrials.gov show an increasing rate of all-cause mortality after 2 years of follow-up for evolocumab versus placebo. A longer follow-up of FOURIER would have yielded the necessary evidence about this and other potential safety issues with evolocumab.
Adaptive designs legitimize protocol changes in response to unfavorable intermediate results. Consequently, they carry a risk of false-positive efficacy results, which is recognized in the literature [12, 13]. The risk of false-negative safety results seems to be underappreciated, and it makes clinical outcomes trials with an adaptive design less appropriate to address safety issues. Adaptive designs of trials should be mentioned explicitly in the abstracts of publications, and essential changes to the protocol should be explained in the main text.
Declarations
Funding
Not applicable.
Conflicts of interest
FH van Bruggen and HJ Luijendijk have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
FHB designed the paper, extracted the data, analysed the data, and drafted the manuscript. HJL analysed the data and helped draft the manuscript. HJL is guarantor of the paper and affirms that the manuscript is an honest, accurate, and transparent account of the study being reported. Both authors have approved the final manuscript and consented to its publication.
References
- 1.Sabatine MS, Giugliano RP, Wiviott SD, Raal FJ, Blom DJ, Robinson J, et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1500–1509. doi: 10.1056/NEJMoa1500858. [DOI] [PubMed] [Google Scholar]
- 2.Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–1722. doi: 10.1056/NEJMoa1615664. [DOI] [PubMed] [Google Scholar]
- 3.Sabatine MS, Giugliano RP, Keech A, Honarpour N, Wang H, Liu T, et al. Rationale and design of the Further cardiovascular OUtcomes Research with PCSK9 Inhibition in subjects with Elevated Risk trial. Am Heart J. 2016;173:94–101. doi: 10.1016/j.ahj.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018) Eur Heart J. 2019;40:237–269. doi: 10.1093/eurheartj/ehy462. [DOI] [PubMed] [Google Scholar]
- 5.Wiviott SD, Giugliano RP, Morrow DA, De Ferrari GM, Lewis BS, Huber K, et al. Effect of evolocumab on type and size of subsequent myocardial infarction: a prespecified analysis of the FOURIER randomized clinical trial. JAMA Cardiol. 2020;5:787–793. doi: 10.1001/jamacardio.2020.0764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke. 2013. 1833–9. [DOI] [PubMed]
- 7.Vergouwen MDI, De Haan RJ, Vermeulen M, Roos YBWEM. Statin treatment and the occurrence of hemorrhagic stroke in patients with a history of cerebrovascular disease. Stroke. 2008;39:497–502. [DOI] [PubMed]
- 8.Ma C, Gurol ME, Huang Z, Lichtenstein AH, Wang X, Wang Y, et al. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology. 2019;93:e445–e457. doi: 10.1212/WNL.0000000000007853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:E67–492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–2107. doi: 10.1056/NEJMoa1801174. [DOI] [PubMed] [Google Scholar]
- 11.C Baigent, A Keech, P M Kearney, L Blackwell, G Buck CP. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. [DOI] [PubMed]
- 12.Bauer P, Bretz F, Dragalin V, König F, Wassmer G. Twenty-five years of confirmatory adaptive designs: opportunities and pitfalls. Stat Med. 2016;35:325–347. doi: 10.1002/sim.6472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emerson SS, Fleming TR. Adaptive methods: telling “the rest of the story.” J Biopharm Stat 2010. 1150–65. [DOI] [PubMed]
- 14.https://clinicaltrials.gov/ (Internet). Available from: https://clinicaltrials.gov/
- 15.van Bruggen FH, Nijhuis GBJ, Zuidema SU, Luijendijk HJ. Serious adverse events and deaths in PCSK9 inhibitor trials reported on ClinicalTrials.gov: a systematic review. Expert Rev Clin Pharmacol. 2020; 13:1–10. [DOI] [PubMed]
- 16.Sabatine MS, Leiter LA, Wiviott SD, Giugliano RP, Deedwania P, De Ferrari GM, et al. Cardiovascular safety and efficacy of the PCSK9 inhibitor evolocumab in patients with and without diabetes and the effect of evolocumab on glycaemia and risk of new-onset diabetes: a prespecified analysis of the FOURIER randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5:941–950. doi: 10.1016/S2213-8587(17)30313-3. [DOI] [PubMed] [Google Scholar]