Abstract
Introduction:
Research examining the influence of neighborhood healthy food environment on diet has been mostly cross-sectional and lacked robust characterization of the food environment. We examined longitudinal associations between features of the local food environment and healthy diet, and whether associations were modified by race/ethnicity.
Methods:
Data on 3,634 adults aged 45–84 at Exam 1 and followed for 10 years were obtained from the Multi-Ethnic Study of Atherosclerosis. Diet quality was assessed using the Alternative Healthy Eating Index at Exam 1 (2000–2002) and Exam 5 (2010–2012). We assessed four measures of local food environment using survey-based measures (e.g. perceptions of healthier food availability) and geographic information system (GIS)-based measures (e.g. distance to and density of healthier food stores) at Exam 1 and Exam 5. Random effects models adjusted for age, sex, education, moving status, per capita adjusted income, and neighborhood socioeconomic status and interactions terms to assess effect modification by race/ethnicity.
Results:
Net of confounders, one standard z-score higher average composite local food environment was associated with higher average AHEI diet score (1.39, 95% CI: 1.05, 1.73) over the follow-up period from Exam 1 to 5. This pattern of association was consistent across both GIS-based and survey-based measures of local food environment and was more pronounced among minoritized racial/ethnic groups. There was no association between changes in neighborhood environment and change in AHEI score, or effect modification by race/ethnicity.
Conclusion:
Our findings suggest that neighborhood-level food environment is associated with better diet quality, especially among racially/ethnically minoritized populations.
Keywords: neighborhood food environment, diet quality
Introduction:
Lack of access to healthy food may negatively impact diet and subsequently lead to worse health outcomes (Caspi et al., 2012b; Cobb et al., 2015; Gamba et al., 2015). Healthier food availability, as an important aspect of the local food environment, has been cross-sectionally associated with the consumption of fruits and vegetables as well as dietary quality (Blitstein et al., 2012; Curl et al., 2013; Franco et al., 2009; Laraia et al., 2004; L.V. Moore et al., 2008; L. V. Moore et al., 2008; Morland et al., 2002; Pearce et al., 2008; Rose and Richards, 2004; Zenk et al., 2009). Furthermore, neighborhoods with higher proportions of minoritized racial/ethnic populations and low income residents may have less access to healthy food due to distance to healthy food stores, prices of healthy food options, and perception of availability (Black et al., 2014; Caspi et al., 2012a; Cobb et al., 2015; Larson et al., 2009).
Although existing studies highlight the potential importance of the neighborhood food environments on diet, several limitations exist. First, studies have been largely cross-sectional, which cannot capture changes in neighborhood healthier food environment over time or allow the estimation of causal effects since temporality cannot be established. Second, among the few longitudinal studies that focused on healthier food environments, findings have been mixed. One longitudinal study of young adults in the US found that greater availability of supermarkets was not associated with fruit and vegetable intake (Boone-Heinonen et al., 2011). Another study of middle-aged residents in a city in Australia found that relocation to a neighborhood with healthier food was associated with greater fruit and vegetable consumption (Bivoltsis et al., 2020). More longitudinal studies are needed to establish temporality and explore how changes in healthier food environment over time affect changes in diet.
Another limitation is the lack of studies that examine the relationship between the local food environment and diet using a robust exposure assessment method that accounts for both perceived and objective food environment. Measures of food environment can include objective assessment, participants’ perception, or a combination of both (Caspi et al., 2012b; Rahmanian et al., 2014). Objective measures can assess the presence of healthier food retailers, the availability and affordability of healthier food items, and marketing influence within the stores through the use of Geographic Information Systems (GIS) and market research data (Charreire et al., 2010; Kern et al., 2017). Subjective measures capture the participants’ impressions of accessibility and affordability of food options, as well as the food shopping experiences, in their neighborhoods (Lytle, 2009; Zenk et al., 2014). Studies comparing objective and perception-based measures are scarce in the literature. A cross-sectional study found that while both types of measures were associated with dietary outcomes, they were not identical and may provide complementary information (L.V. Moore et al., 2008). Thus, measures of the food environment that include both GIS-derived, objective measures, as well as survey-based, perceptive measures, can form a more complete characterization of healthy food availability (Bowen et al., 2015).
A final gap in knowledge is the limited investigation of effect measure modification by race/ethnicity (Galvez et al., 2008; Morland et al., 2002; Powell et al., 2007). While studies have documented racial/ethnic disparities in diet quality, few studies have examined whether the associations between local food environment and dietary outcomes may be more or less pronounced among different racial/ethnic groups (Hiza et al., 2013; Raffensperger et al., 2010). Filling this gap can inform whether improving the availability of healthier foods in the local environment would lead to stronger influence on the dietary quality of racially/ethnically minoritized populations. One study found that living in a census tract with supermarkets and full-service restaurants was associated with having a healthier diet, and this association was more pronounced among African Americans compared to their white counterparts (Morland et al., 2002). Another study found a positive association between the presence of grocery stores and increased fruit and vegetable intake among Hispanic participants, but not among Black participants (Zenk et al., 2009). Authors of these studies suggest that mediating pathways between healthier food availability and diet, such as vehicle access, cultural preferences, and acculturation status, may contribute to the varying influence of healthy food environment for specific minoritized racial/ethnic groups. No study has investigated the local food environment and diet among Asian populations. Given limited literature, more studies are needed in order to examine whether certain minoritized racial/ethnic groups are more susceptible to the impact of the local food environment.
Using data from the Multi-Ethnic Study of Atherosclerosis, a racially/ethnically diverse sample of middle-aged adults, we examined associations between the local food environment and diet over a ten-year follow-up period. We also assessed associations between changes in neighborhood food environment and change in diet quality between Exam 1 (2000–2002) and Exam 5 (2010–2012). We evaluated the robustness of these associations to ascertain whether the environment was best characterized via surveys (perception of environment), GIS, or a combination of the two. Lastly, we evaluated effect measure modification by race/ethnicity. We hypothesized that a better local food environment would be associated with increased diet quality, and this association would be more pronounced for minoritized racial/ethnic groups in the study sample, compared to non-Hispanic white participants.
Methods:
Study Population:
This study used data from the Multi-Ethnic Study of Atherosclerosis (MESA). Details about the study design are described elsewhere (Bild, 2002). Briefly, MESA is a prospective cohort study designed to examine the determinants of subclinical cardiovascular disease in adults aged 45–84 years at baseline. Non-Hispanic Black, Chinese, and Hispanic participants who were free of clinical cardiovascular disease at baseline were recruited from six sites in the United States: New York, New York; Baltimore City and County, Maryland; Forsyth County, North Carolina; St. Paul, Minnesota; Chicago, Illinois; and Los Angeles County, California. Five additional examinations have been completed since baseline. This study also used data from the MESA Neighborhood Ancillary study, which aimed to assess how neighborhood conditions impact cardiovascular disease. The Neighborhood Ancillary study collected survey-based and GIS-derived information on the neighborhood social and physical environment around the participants’ home residences. In addition to MESA participants, individuals residing in the same neighborhoods as MESA participants were recruited as a part of the Community Survey (CS) and asked to rate several aspects of their neighborhoods. The CS reduced same source bias, increased within-neighborhood sample size for constructing contextual variables, and provided a more representative view of the neighborhoods (Echeverria, 2004; Mujahid et al., 2007)
Dietary data were collected as a part of the Dietary Ancillary Study at Exam 1 (2000–2002) and Exam 5 (2010–2012). Of the 6,191 participants who consented to be a part of the Neighborhood Ancillary study, 5,427 participants completed the dietary questionnaire at Exam 1. We excluded those who did not also have diet information at Exam 5 (n=1,718). Participants who did not complete dietary questionnaire at Exam 5 were fairly similar to those who completed dietary questionnaires at both Exams in terms of exposure and covariate distribution, except that those lost to follow-up had lower income and education and were more likely to be Chinese or non-Hispanic Black. We also excluded those who did not have complete exposure information at Exam 1 and at least one available exposure measure at Exam 5 (n=52), and those missing any covariate information at Exam 1 (n=23). The final analytic sample included 3,634 participants. This study was approved by the Institutional Review Boards at each study site and all participants gave written informed consent.
Neighborhood Food Environment:
Participants’ home addresses were geocoded using TeleAtlas EZ-Locate. Based on the participants’ residential addresses, we characterized their neighborhood food environment using four measures: 1. GIS-derived distance to nearest favorable food store, 2. GIS-derived one-mile kernel density of favorable food stores, 3. survey-based measure of perception of healthy food availability, and 4. summary measure combining GIS-derived one-mile kernel density of favorable food stores and survey-based measure of participants’ perception of healthy food availability (composite of measure 2 and 3). All four measures were modeled as continuous and categorical variables. We standardized the continuous measures into standard z-scores by subtracting the mean and dividing by standard deviation. For categorical measures, we used the standardized continuous score to create tertiles and used the lowest tertile as the referent.
For GIS-derived objective measures, we assessed distance to closest favorable food store in meters and density of favorable food stores within a one-mile radius. One-mile area was chosen as the boundary because it aligned with some U.S. government definitions of access to services and was consistent with the one-mile area that survey respondents were asked to consider in surveys (described below) (Ver Ploeg et al., 2009). Data came from the National Establishment Time Series yearly data from Walls and Associates. Favorable food stores included chain and non-chain supermarkets and fruit and vegetable markets (details described elsewhere) (Auchincloss et al., 2012). Supermarkets were defined as businesses that had a “grocery or supermarket” Standard Industrial Classification (SIC) code, with 25 or more employees, or generated sales of $2 million or greater. Fruit and vegetable markets were defined as businesses with SIC code #5431.We used Kernel estimation to calculate the densities, such that food retailers closer to participants’ addresses were given more weight than stores farther away (Silverman, 1986). These measures were calculated using ArcGIS 9.3 (ESRI, 2009). Higher scores indicate longer distance to the closest favorable food store or higher density of favorable food stores.
For survey-based measures, MESA and CS participants were asked to consider the area approximately one-mile around their homes and respond to a three-question survey which measured the perceived availability of healthy food in their neighborhoods. Participants were asked to indicate the extent to which they agreed with the following statements: 1. a large selection of fruits and vegetables is available; 2. the fresh fruits and vegetables in my neighborhood are of high quality, and 3. a large selection of low-fat products is available. Responses were aggregated using conditional empirical Bayes estimates for census tracts, which were derived from three-level hierarchical linear models (i.e. scale items nested within individuals nested within neighborhoods), conditioning on the respondents’ sex, age, whether in MESA or CS sample, and study site (Mujahid et al., 2008). A higher value indicated better availability of healthy food. The composite score of the neighborhood food environment was created using exploratory principal components analysis and Cronbach’s alpha statistics were used to validate this scale, which was also standardized across both Exam 1 and 5. The composite score included GIS-assessed one-mile kernel density of favorable food retailers and survey-based conditional empirical Bayes estimate scale about the perceived availability of healthy food in participants’ neighborhoods. Participants who did not have the perception-based measure at Exam 5 also did not have the composite measure (n=157). Higher score indicated better food environment.
Dietary Outcome:
The Alternative Healthy Eating Index (AHEI) was used to measure the overall quality of the participants’ diets. The AHEI is a summary measure of diet quality that has been associated with lower risk of chronic disease (McCullough et al., 2002; McCullough and Willett, 2006; Nettleton et al., 2006; Sundström et al., 2006). This diet measure was computed from responses to the 120-item food frequency questionnaire at Exam 1 (2000–2002) and Exam 5 (2010–2012). The AHEI was derived from MESA dietary data based on previously developed methods (L. V. Moore et al., 2008; Nettleton et al., 2006). A higher AHEI score (range: 0–110) indicates higher intake of fruits and vegetables, nuts and soy protein, white meat (vs. red meat), cereal fibers, and polyunsaturated fat, as well as moderate alcohol consumption, multivitamin use, and lower intake of trans fat (L. V. Moore et al., 2008). We modeled the AHEI score continuously and as changes in AHEI score between Exam 5 and Exam 1.
For descriptive analyses, we also categorized the AHEI score into healthy and unhealthy diet. A participant’s diet was classified as “healthy” if it was in the top quintile of the sample distribution, based on prior work (McCullough et al., 2002; McCullough and Willett, 2006; L. V. Moore et al., 2008). We also examined the fruit and vegetable-specific AHEI score, calculated from summing the AHEI vegetable component (1–10 points) and the AHEI whole fruit component (1–10 points), in our sensitivity analyses, since fruit and vegetable intake has been used as a proxy for healthy diet quality (Chor et al., 2016).
Covariates:
Participant-level covariates include baseline sex, race/ethnicity (non-Hispanic white, non-Hispanic Black, Chinese American, and Hispanic), level of education, age (year), per capita adjusted income per $10,000, as well as an indicator for residential relocation during the entire follow-up period. At the census-tract level, we adjusted for neighborhood SES as a confounder due to its relationship with both neighborhood environment features, including healthier food availability, and diet. Using data from the 2000 U.S. Census, we calculated a previously developed composite index such that higher scores indicate more socioeconomic advantage (Diez-Roux et al., 2001).
Statistical Analyses:
We described the sample distribution, at Exam 1, overall and by healthy/unhealthy diet quality and present the mean AHEI score by participants’ covariates, including age, sex, race/ethnicity, education, individual-level income, neighborhood-level disadvantage, and whether the participant has moved over the course of follow-up.
To examine the association between neighborhood food environment and AHEI scores over the study follow-up, we first used three-level random effects models to estimate the associations between average neighborhood food environment standardized scores at Exam 1 and at Exam 5 and average AHEI score at Exam 1 and at Exam 5, using random intercepts to account for repeated measures at two time points and neighborhood clustering. To control for residential self-selection into neighborhoods, we adjusted for an indicator of whether the participant moved during follow-up. Time-varying covariates age, income, and neighborhood disadvantage were included in models. Next, we used two-level random effects models (i.e. random intercept to account for neighborhood clustering) to assess the longitudinal association between changes in neighborhood environment (differences in food environment between Exam 5 and Exam1) in relation to change in diet (difference in AHEI between Exam 5 and Exam 1), adjusting for the same set of confounders. For both models, we assessed effect measure modification by race/ethnicity by including a cross-product term between exposure and race/ethnicity and performing race/ethnicity-stratified models. We used a threshold of p value<0.05 to assess the significance of the interaction terms.
We performed four sets of sensitivity analyses. First, given recent efforts in evaluating supermarket-related interventions as a strategy to improve healthier food environment and diet, we assessed distance to and density of chain and non-chain supermarkets as the exposure measures, in place of distance to and density of favorable food stores, to examine if associations were robust across these objective GIS measures (Chrisinger, 2016; Dubowitz et al., 2015; Elbel et al., 2015). Second, we tested for interaction by relocation during follow-up to see if associations differed between those who moved and those who did not. Third, we examined if the results differed using the fruit and vegetable specific AHEI score as the outcome. Lastly, due to loss to follow up, 157 participants did not have a perception measure or composite measure of food environment at Exam 5. Thus, we also conducted a sensitivity analysis by restricting analyses to all participants who had complete exposure variables at both Exam 1 and Exam 5 to evaluate selection bias due to loss to follow-up (n=3,477).
For all analyses, we report estimates and 95% confidence intervals. Analyses were conducted in STATA (StataCorp., 2013).
Results:
The final analytic sample included 3,634 participants with a baseline mean age of 60.3 (SD=9.5) and 51.3% identified as female. The race/ethnic distribution was 44.2% non-Hispanic white, 10.9% Chinese, 24.1% non-Hispanic Black, and 20.8% Hispanic. Table 1 shows mean AHEI score and healthy/unhealthy diet by study population characteristics at Exam 1. The mean AHEI score was higher for those who are of older age, female (compared to males), have a Bachelor’s education or above, and have higher income. Chinese participants had the highest average AHEI scores, followed by white, Black, and Hispanic participants, respectively. Similarly, those who had a healthy diet were more likely to be female, between the age of 45–64, completed a Bachelor’s degree or graduate school, and have higher individual income. There were also bivariate associations between our neighborhood measures and diet measures. The mean AHEI score increased with decreases in distance to the nearest favorable food stores, and with increases in neighborhood SES, density of favorable food stores, perception of healthy food access, and the composite measure of healthy food environment. In terms of absolute change over time for exposure and outcomes, between Exam 1 and 5, the average change in distance to closest favorable food store was 144 meters, the density of favorable food stores decreased by −0.19 stores on average, and perception of the food environment and overall composite score increased by 0.27 and 0.56 on average, respectively (Supplemental Table 1). The mean change in AHEI score from Exam 1 to 5 was 3.05.
Table 1:
Baseline Participant Characteristics and Exposure Categories by Alternative Healthy Eating Index (AHEI) Score, Multi-Ethnic Study of Atherosclerosis, 2000–2002.
| N (%) | Alternative Healthy Eating Index | |||
|---|---|---|---|---|
| Mean AHEI | Unhealthy Diet (%)* | Healthy diet (%)* | ||
| (n=3634) | (n = 2915) | (n = 719) | ||
| Sex | ||||
| Female | 1866 (51.3) | 53.8 ± 12.1 | 1270 (48.8) | 423 (65.4) |
| Male | 1768 (48.7) | 49.9 ± 11.2 | 1334 (51.2) | 224 (34.6) |
| Age (mean=60.3, SD=9.5) | ||||
| 45 – 54 | 1220 (33.6) | 49.9 ± 12.0 | 1030 (35.3) | 190 (26.4) |
| 55 – 64 | 1122 (30.9) | 52.0 ± 11.7 | 895 (30.7) | 227 (31.6) |
| 65 – 74 | 990 (27.2) | 53.6 ± 11.5 | 754 (25.9) | 236 (32.8) |
| 75 – 84 | 302 (8.3) | 54.5 ± 11.1 | 236 (8.1) | 66 (9.2) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 1607 (44.2) | 52.6 ± 12.2 | 1244 (42.7) | 363 (50.5) |
| Non-Hispanic Black | 875 (24.1) | 50.3 ± 12.1 | 732 (25.1) | 143 (19.9) |
| Hispanic | 756 (20.8) | 49.9 ± 10.8 | 656 (22.5) | 100 (13.9) |
| Chinese American | 396 (10.9) | 56.3 ± 10.1 | 283 (9.7) | 113 (15.7) |
| Education | ||||
| Less than High School | 458 (12.6) | 50.3 ± 10.6 | 402 (13.8) | 56 (7.8) |
| High school | 614 (16.9) | 49.4 ± 11.7 | 528 (18.1) | 86 (12.0) |
| Technical school or associate | 1038 (28.6) | 50.7 ± 12.0 | 850 (29.2) | 188 (26.1) |
| Bachelor’s or Graduate Degree | 1524 (41.9) | 54.2 ± 11.7 | 1135 (38.9) | 389 (54.1) |
| Moved during follow up | ||||
| Yes | 1080 (29.7) | 52.2 ± 11.8 | 857 (29.4) | 223 (31.0) |
| No | 2554 (70.3) | 51.8 ± 11.8 | 2058 (70.6) | 496 (69.0) |
| Per capita Adjusted income per $10,000 | ||||
| <1.25 | 826 (22.7) | 50.9 ± 10.9 | 701 (24.0) | 125 (17.4) |
| 1.25–2.25 | 805 (22.2) | 50.0 ± 11.5 | 682 (23.4) | 123 (17.1) |
| 2.25–3.75 | 930 (25.6) | 52.1 ± 12.2 | 745 (25.6) | 185 (25.7) |
| >=3.75 | 1073 (29.5) | 54.1 ± 12.0 | 787 (27.0) | 286 (39.8) |
| Neighborhood SES | ||||
| Low | 1196 (32.9) | 50.4 ± 11.3 | 1025 (35.2) | 171 (23.8) |
| Medium | 1176 (32.4) | 50.7 ± 11.5 | 978 (33.6) | 198 (27.5) |
| High | 1262 (34.7) | 54.5 ± 12.2 | 912 (31.3) | 350 (48.7) |
| Distance to favorable food stores (meter)1 | ||||
| Tertile 1 | 1164 (32.0) | 52.8 ± 11.9 | 914 (31.4) | 250 (34.8) |
| Tertile 2 | 1281 (35.3) | 52.0 ± 11.6 | 1022 (35.1) | 259 (36.0) |
| Tertile 3 | 1174 (32.3) | 51.0 ± 11.9 | 979 (33.6) | 210 (29.2) |
| Density of favorable food stores (1 mile)2 | ||||
| Tertile 1 | 1224 (33.7) | 50.9 ± 12.0 | 1005 (34.5) | 219 (30.5) |
| Tertile 2 | 1236 (34.0) | 51.7 ± 11.4 | 1016 (34.9) | 220 (30.6) |
| Tertile 3 | 1262 (34.7) | 53.3 ± 12.0 | 894 (30.7) | 280 (38.9) |
| Healthy Food Environment (Survey)3 | ||||
| Tertile 1 | 1619 (44.6) | 50.2 ± 11.8 | 1358 (46.6) | 261 (36.3) |
| Tertile 2 | 1208 (33.2) | 51.9 ± 11.2 | 989 (33.9) | 219 (30.5) |
| Tertile 3 | 807 (22.2) | 55.5 ± 11.9 | 568 (19.5) | 239 (33.2) |
| Healthy Food Environment (Survey + GIS)4 | ||||
| Tertile 1 | 1592 (43.8) | 50.2 ± 11.8 | 1333 (45.7) | 259 (36.0) |
| Tertile 2 | 1042 (28.7) | 52.7 ± 11.1 | 830 (28.5) | 212 (29.5) |
| Tertile 3 | 1000 (27.5) | 53.8 ± 12.2 | 752 (25.8) | 248 (34.5) |
We categorized those whose AHEI scores were in the top-fifth of percentiles as having a healthy diet
Tertile categories represent tertiles of continuous standardized score for each neighborhood environment measures
Three-level random-effect hierarchical modeling results showed that average neighborhood food environment standardized scores were associated with average AHEI scores over time and between individuals in a given neighborhood (Table 2, Model 1; Figure 1). A one-unit higher average composite standard score was significantly associated with 1.39-unit higher average AHEI score at Exam 5 and Exam 1 (95% CI: 1.05, 1.73), controlling for confounders. In addition to the composite food environment results, Figure 1 further displays the associations between distance to closest favorable food store, density of favorable food stores, and survey-based healthy food environment scores in relation to AHEI scores. Those in the medium and high tertiles of composite perceived and objective availability of healthy food environment experienced 1.09 (95% CI: 0.41, 1.76) and 3.21 (95% CI: 2.42, 3.99) increase in average AHEI scores compared to the lowest tertile, respectively (Figure 1). Across all four measures of food environment, there were graded associations between categorical exposure variables and AHEI scores: those in the medium tertile experienced a weaker association compared to the referent category than those in the high tertile (Figure 1).
Table 2:
Associations between healthy food environment and Alternative Healthy Eating Index (AHEI) score, Multi-Ethnic Study of Atherosclerosis, Exam 1 and 5, 2000–2012.
| Model 1a | Model 2b | |||
|---|---|---|---|---|
| Estimate | 95% Confidence Interval | Estimate | 95% Confidence Interval | |
| Average Healthy Food Environment | 1.39 | 1.05, 1.73 | -- | -- |
| Change in Healthy Food Environment | -- | -- | 0.22 | −0.21, 0.65 |
The Healthy Food Environment score is a composite measure that includes GIS-derived density of favorable food stores and survey-based measures of perceptions of healthy food availability
Model 1: Associations between average food environment composite measure standard score, modeled continuously, and average AHEI score over time and between individuals
Model 2: Associations between change in local food environment composite measure standard score, modeled continuously, and change in AHEI score over follow-up
All models adjust for age, sex, education, moving status, per capita adjusted income, neighborhood SES
Figure 1:
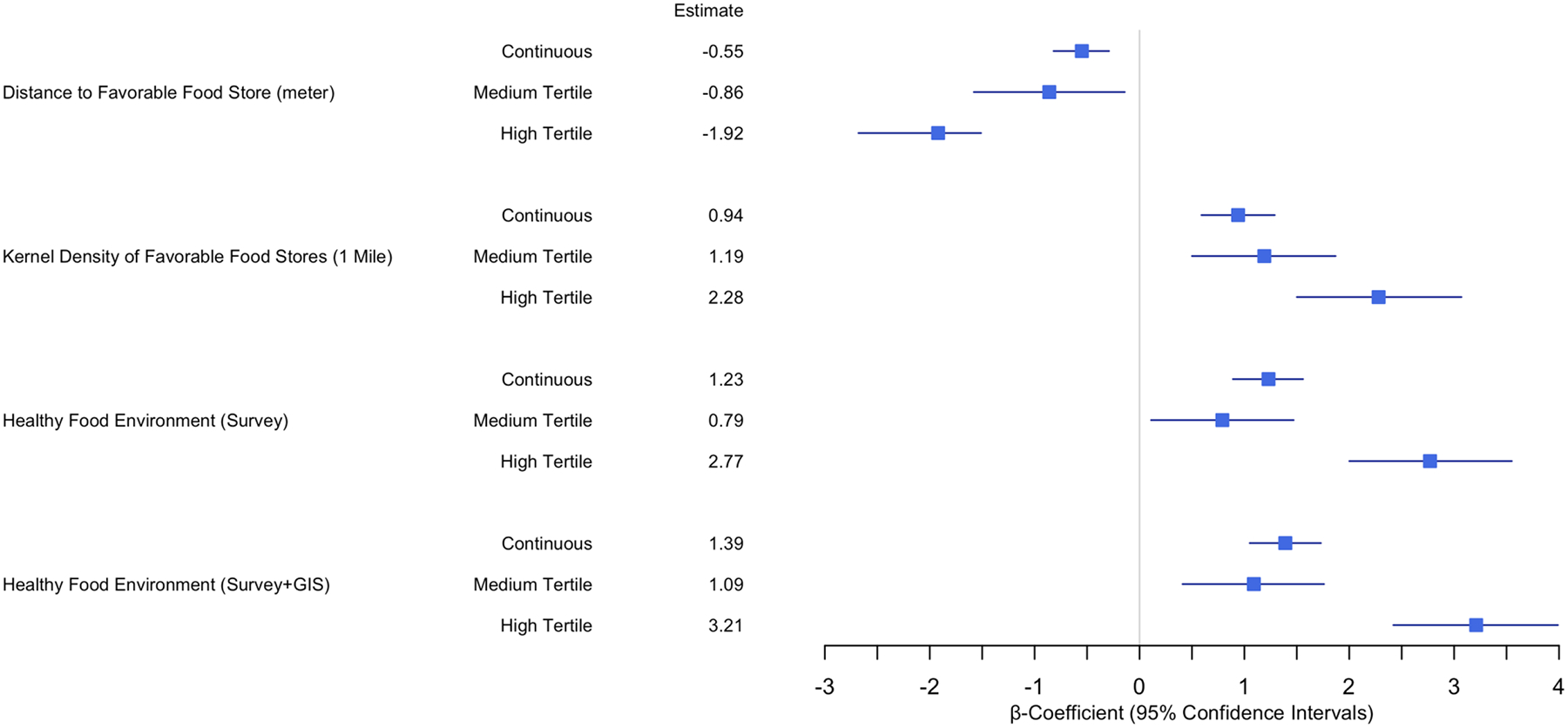
Associations between average local food environment measures and average Alternative Healthy Eating Index (AHEI) scores at Exam 1 and 5, Multi-Ethnic Study of Atherosclerosis, 2000–2012.
1. All neighborhood measures were standardized into z-scores
2. For categorical exposure measures, the reference group is the lowest tertile
3. N=3634 for all models using distance and kernel density GIS-based measures; N=3477 for healthy food environment survey measure and composite measure
4. All models adjust for age, sex, education, moving status, per capita adjusted income, neighborhood SES
Results from models examining changes in local food environment and change in AHEI scores are displayed in Table 2 (Model 2) and Figure 2. Changes in composite food environment score was not associated with change in AHEI score, but the directions of associations were as expected and similar to those in Model 1.
Figure 2:
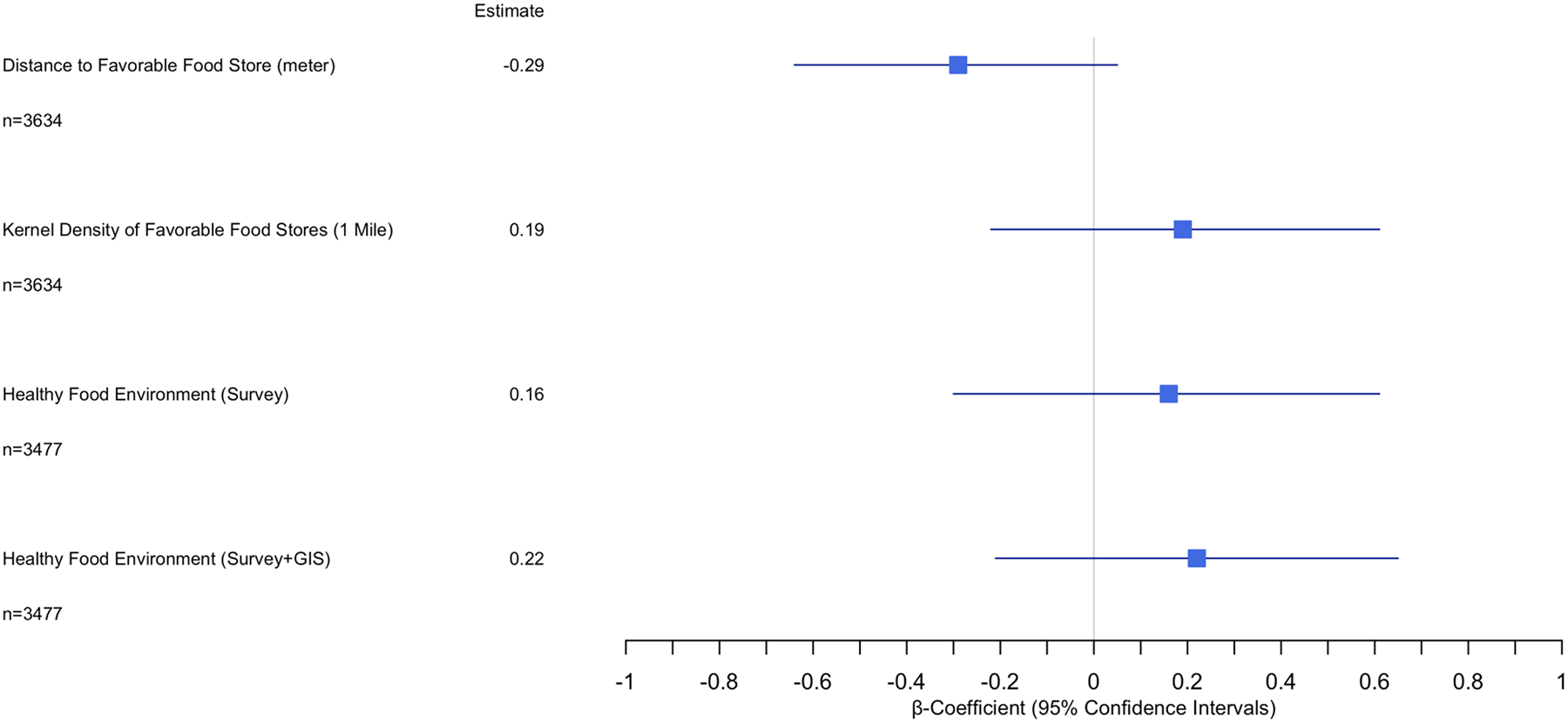
Associations between change in neighborhood environment measures and change in Alternative Healthy Eating Index (AHEI) scores, Multi-Ethnic Study of Atherosclerosis, 2000–2012.
1. Change in neighborhood environment was measured by difference in neighborhood standard scores at Exam 1 and Exam 5
2. Change in diet quality was measured by difference in AHEI scores at Exam 1 and Exam 5
3. All models adjust for age, sex, education, moving status, per capita adjusted income, neighborhood SES
Assessment of effect measure modification showed that race/ethnicity significantly modified the association between neighborhood food environment (density of food stores (p-value for interaction<0.01) and perception of food environment (p-value for interaction=0.03)) and average AHEI scores (Table 3). Race/ethnicity-stratified analyses showed that only among Black participants, all four measures of local food environment were significantly associated with AHEI scores, and the measures of association were larger in magnitude for Black participants compared to their white counterparts. For example, one standard score in composite healthy food environment was associated with 0.85-unit higher average AHEI score among white participants (95% CI: 0.34, 1.37) but 1.73-unit higher average AHEI score among Black participants (95% CI: 1.11, 2.35). On the other hand, only the survey measure and composite measure of the food environment were statistically significantly associated with average AHEI score in Hispanic and Chinese groups. These associations were also more pronounced in Chinese and Hispanic groups compared to their white counterparts. Race/ethnicity did not modify the association between changes in neighborhood food environment and change in AHEI scores.
Table 3:
Associations between Neighborhood Average Food Environment and Alternative Healthy Eating Index (AHEI) Score: Effect Measure Modification by Race/Ethnicity, Multi-Ethnic Study of Atherosclerosis, 2000–2012.
| Non-Hispanic White | Chinese | Non-Hispanic Black | Hispanic | |
|---|---|---|---|---|
| (N=1607) | (N=396) | (N=875) | (N=756) | |
| Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | |
| Distance to favorable food stores (p=0.27) | −0.28 (−0.58, 0.02) | −0.11 (−1.49, 1.26) | −1.05 (−1.82, −0.29) | −0.95 (−2.00, 0.10) |
| Density of favorable food stores* (p=0.01) | 0.91 (0.34, 1.48) | −0.47 (−3.27, 2.33) | 1.71 (1.01, 2.41) | −0.22 (−0.82, 0.38) |
| Healthy food perception (survey)* (p=0.03) | 0.52 (0.04, 1.00) | 1.90 (0.44, 3.35) | 1.21 (0.63, 1.79) | 2.66 (1.74, 3.58) |
| Composite food environment (survey and GIS) (p=0.25) | 0.85 (0.34, 1.37) | 2.07 (0.14, 4.01) | 1.73 (1.11, 2.35) | 0.89 (0.14, 1.65) |
p value displayed is for the interaction term between food environment measure and race/ethnicity; statistically significant using p<0.05 as the threshold.
Racial/ethnic groups are non-Hispanic unless otherwise noted
Three-level hierarchical random effect models assessed race/ethnicity-stratified average food environment score and average AHEI score over time and between individuals
Models adjust for age, sex, education, moving status, per capita adjusted income, neighborhood SES
In sensitivity analyses, we found that a one-unit increase in the standardized distance to the closest supermarket was associated with −0.39 unit change in AHEI score (95% CI: −0.76, −0.02) in Model 2. We did not find significant interaction by relocation status during follow-up. Both GIS measures were associated with the fruit and vegetable-specific AHEI score (Distance: continuous: −0.12, 95% CI: −0.22, −0.01; categorical 2nd vs. 1st tertile: −0.30, 95% CI: −0.59, −0.02; categorical 3rd vs. 1st tertile: −0.50, 95% CI: −0.81, −0.20) (Density: categorical 3rd vs. 1st tertile: 0.44, 95% CI: 0.13, 0.75). There was also an association with the survey-based standardized score (continuous: 0.16, 95% CI: 0.09, 0.23; categorical 3rd vs. 1st tertile: 0.46, 95% CI: 0.29, 0.63), as well as the summary composite score (continuous: 0.15, 95% CI: 0.08–0.22; categorical 3rd vs. 1st tertile: 0.51, 95% CI: 0.34, 0.68). Changes in local food environment were not associated with change in AHEI score of fruits and vegetables. Lastly, restricting analysis to those who had complete exposure information across all four measures at both Exams, by excluding the 157 participants who had objective measures but not perception-based measures at Exam 5, did not change the results.
Discussion:
Using data from a sample of racially and ethnically diverse group of older adults in the United States, we found that residents who lived in a better food environment—in terms of proximity to and density of favorable food stores, as well as perception of a healthier food environment—had higher diet quality over a 10-year period and associations were more pronounced for minoritized racial/ethnic groups. Changes in local food environment in terms of favorable food stores and availability of healthy food over the 10-year follow-up were not associated with change in overall dietary quality. Our study contributes to existing evidence on the impact of the local food environment on diet in middle-aged and older adults.
While numerous cross-sectional studies have documented the influence of healthier food environment on diet, our study further leveraged longitudinal data to strengthen evidence of this relationship and added to the mixed findings from existing longitudinal studies (Franco et al., 2009; Laraia et al., 2004; Morland et al., 2002). For example, Boone-Heinonen et al. used fifteen years of data from the Coronary Artery Risk Development Study to document that supermarket availability (within 1–2.9 km of the home) was associated with greater adherence to fruit and vegetable recommendations but not overall dietary quality in men. There were no associations between supermarket availability and dietary outcomes in women (Boone-Heinonen et al., 2011). Another longitudinal analysis of the RESIDential Evironments Study in Perth, Australia, found that moving to a neighborhood with a greater percentage of healthy food outlets (i.e. supermarkets and greengrocers) around the home was associated with an increase in healthy food and fruit/vegetable intake. However, this study did not assess a measure of overall dietary quality (Bivoltsis et al., 2020). We found that the local food environment, measured using both survey-based and GIS measures, was associated with better average dietary quality, and to a similar extend, with fruit and vegetable consumption. over a ten-year period, providing a missing link in the existing literature.
This study also examined how changes in neighborhood food environment relates to changes in dietary quality. The fact that we did not find associations between changes may be because changes in neighborhood environment over the 10-year period were relatively small. More longitudinal studies that capture larger changes in food environment and dietary quality over a longer follow-up period may be beneficial. In sensitivity analyses, we found that change in distance to the closest supermarket was negatively associated with change in AHEI scores such that increasing distance between Exam 1 and 5 is associated with worse diet. This suggests that more studies evaluating supermarkets as a diet-improving feature of the neighborhood may be needed, given current initiatives to subsidize supermarket and other food store development in neighborhoods lacking healthier food retailers to promote healthy diet. Studies evaluating whether improvements in the healthy food retail environment positively influence diet have yielded mixed results. For example, studies have leveraged natural experiment design to assess diet outcomes after the opening of a supermarket and did not find significant change (Cummins, 2005; Cummins et al., 2014; Elbel et al., 2015). However, one quasi-experimental longitudinal design in Pittsburgh found improvement in some outcomes such as overall diet quality and perceived access to healthy food, but not in other health outcomes such as fruit and vegetable intake and body mass index (Dubowitz et al., 2015). The largely null findings in existing quasi-experimental studies may suggest that more investigation is needed to identify other effective strategies to modify the food environment. Longitudinal study design can examine a variety of changes in food environment, include both low- and well-resourced neighborhoods over larger geographic regions, and recruit diverse study populations. These features would enable identification of changes needed to improve population health and address racial/ethnic disparities in dietary quality.
Another significant contribution of our study was the use of both GIS and survey measures in analytic models. In existing literature, GIS-derived objective measures have been more frequently used to characterize the food environment than perceptive measures (Caspi et al., 2012b; Rahmanian et al., 2014). However, the GIS-characterized food environment has produced more mixed associations with diet quality, whereas the perception-based measures have been more consistently related to diet (Charreire et al., 2010). Despite the increasing popularity of GIS measures due to improvements in technology and availability of spatial data, there are some conceptual and methodological challenges in using them to characterize the local food environment. For example, access to healthy food also involves material and social dimensions that are not captured by density and proximity of retailers such as cultural norms and affordability. Furthermore, the definition of a “neighborhood” varies widely between GIS-derived measurements of local food environment (Caspi et al., 2012b; Charreire et al., 2010; Matthews et al., 2009). In this study, we found that shorter distance to favorable food stores and higher one-mile kernel density of favorable food stores were significantly associated with average AHEI scores, lending support that GIS-measures can capture the influence of food environment on diet quality. Similarly, we found that the survey-based measure yielded the same findings as the GIS-derived measures, The composite measure, which included both the participants’ perception and the density of healthy food retailers, was associated with slightly larger increase in diet quality compared to the survey-only measure or GIS-only measures, suggesting that comprehensive characterization of the local food environment may need both types of measures to capture the influence on dietary quality. On the other hand, we only found change in distance to supermarkets to be associated with change in AHEI score. This may have been due to a larger change in distance to supermarkets over time but much smaller changes in our other measures, including distance to and density of favorable food stores. A re-examination of these associations with an additional follow-up may improve our ability to capture changes in food environment.
The overall quality of the diet of racially/ethnically minoritized populations may be more strongly associated with the influence of the food environment. We found support for this for two of our four measures such that associations were most pronounced among Black participants (density of favorable food stores) and Hispanic participants (perception measure) (p<0.05). Associations among Chinese participants were also stronger than among their white counterparts for the perception and composite measures. These findings suggest that while better local food environment may promote healthier diets for all, a healthier food environment can influence diet among minoritized racial/ethnic groups more prominently. Hispanic and Chinese groups may have different culturally diet-related practices compared to Black and white participants, which can explain why the perception of a healthy food environment matters more than the presence of favorable food stores around the homes (Pérez-Escamilla, 2009; Zenk et al., 2009). Studies have documented how ethnic markets in low-income, immigrant neighborhoods may also promote healthier diet (Joassart-Marcelli et al., 2017; Khojasteh and Raja, 2017). At the same time, lack of favorable food stores, including supermarkets, can be indicative of structural disinvestment, since these retailers are less likely to be located in Black and low-income neighborhoods potentially due to structural racism and residential segregation, driving the associations between GIS measures and AHEI scores among Black participants that are absent in other minoritized groups (Bower et al., 2014; Boyd et al., 2020; Kurtz, 2013). Thus, given the stronger association between local food environment and diet among racially/ethnically minoritized participants, addressing structural factors that shape the food environment may be necessary to address racial/ethnic disparities in diet.
Several limitations warrant comment. First, we defined a neighborhood as the area within one mile of the residents’ homes, which may not accurately capture the area where people primarily access food and other boundaries have also been assessed (Charreire et al., 2010; Morland et al., 2002). Second, we only evaluated the areas surrounding the participants’ homes, but other contexts, such as the food environment around workplaces or in schools, may also matter. Additional studies can further evaluate other aspects that influence people’s interactions with their food environment, such as mode of transportation, prices and quality of food items, and community norms around diet. Third, our GIS-derived measures only included supermarkets and fruit and vegetable markets, but our perception-based measures broadly assessed the food environment which may have included other type of retailers such as ethnic markets, smaller grocery stores, seasonal farmers’ markets, etc., a discrepancy that may have accounted for the different magnitude of associations between these two measures. Outcome assessment, which were based on AHEI score, could be another source of limitation. AHEI may not fully characterize ethnic diets, which can result in bias due to misclassification of diet outcomes among racially/ethnically minoritized study participants in our sample. Furthermore, the AHEI score largely characterized a healthy diet, and the food environment may also influence unhealthy dietary patterns, which was not extensively examined in this study. We also had loss-to-follow-up with regards to outcome, which may create bias since participants with lower SES were more likely to be lost to follow-up. There could be confounding by poorly measured individual-level variables or common factors that influenced both the food environment and diet that we did not adjust for. However, we were able to control for neighborhood SES, individual income and education, which allowed us to examine associations between food environment and diet quality independent of SES. While adjusting for relocation status may have helped to address self-selection into neighborhoods, future studies should investigate more rigorous approaches for dealing with neighborhood self-selection (i.e. longitudinal structural equation models with control groups, marginal structural modeling) (Cao et al., 2009; Lei et al., 2019). Social conditions, including SES and structural racism, have been cited as fundamental causes of disease; local food environment may be one “intervening mechanism” through which fundamental causes operate to influence health disparities (Link and Phelan, 1995; Phelan and Link, 2015). Fundamental causes shape neighborhood social and material conditions, as well as people’s differential access to resources that determines their selection into neighborhoods. Future studies should examine fundamental causes that shape neighborhood food environment.
In conclusion, average proximity to and density of favorable food stores, as well as perception of the local food environment, were significantly associated with average diet quality at Exam 1 and Exam 5 over the 10-year follow up. Another important finding was that the influence of the food environment was more pronounced among minoritized racial/ethnic groups. Our study provides additional evidence that the local food environment matters for diet quality, highlighting the importance of incorporating both GIS- and perception-based measures as well as selecting appropriate dietary outcomes. Furthermore, our findings suggest that interventions that improve the food environment may benefit minoritized racial/ethnic groups due to the stronger influence on diet. These findings can inform local, state, and national policies on community development and promotion of access to healthy food. By including longitudinal follow-up data, assessing multiple exposure measures of the food environment, and controlling for neighborhood-level socioeconomic status, this study offered evidence that the local food environment significantly impacts diet quality.
Supplementary Material
Acknowledgments
We thank the investigators, staff, and participants of the MESA study for their contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. This research was supported by contracts 75N92020D00001, HHSN268201500003I, N01-HC-95159, 75N92020D00005, N01-HC-95160, 75N92020D00002, N01-HC-95161, 75N92020D00003, N01-HC-95162, 75N92020D00006, N01-HC-95163, 75N92020D00004, N01-HC-95164, 75N92020D00007, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, by grants UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 from the National Center for Advancing Translational Sciences (NCATS), and by R01 HL131610 from the National Institutes of Health (NIH) grants. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
For submission to: Social Science and Medicine
References:
- Auchincloss AH, Moore KAB, Moore LV, Diez Roux AV, 2012. Improving retrospective characterization of the food environment for a large region in the United States during a historic time period. Health Place 18, 1341–1347. 10.1016/j.healthplace.2012.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bild DE, 2002. Multi-Ethnic Study of Atherosclerosis: Objectives and Design. American Journal of Epidemiology 156, 871–881. 10.1093/aje/kwf113 [DOI] [PubMed] [Google Scholar]
- Bivoltsis A, Trapp G, Knuiman M, Hooper P, Ambrosini GL, 2020. The influence of the local food environment on diet following residential relocation: longitudinal results from RESIDential Environments (RESIDE). Public Health Nutrition 23, 2132–2144. 10.1017/S1368980019005111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black C, Moon G, Baird J, 2014. Dietary inequalities: what is the evidence for the effect of the neighbourhood food environment? Health Place 27, 229–242. 10.1016/j.healthplace.2013.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blitstein JL, Snider J, Evans WD, 2012. Perceptions of the food shopping environment are associated with greater consumption of fruits and vegetables. Public Health Nutrition 15, 1124–1129. 10.1017/S1368980012000523 [DOI] [PubMed] [Google Scholar]
- Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM, 2011. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med 171, 1162–1170. 10.1001/archinternmed.2011.283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen DJ, Barrington WE, Beresford SAA, 2015. Identifying the Effects of Environmental and Policy Change Interventions on Healthy Eating. Annu Rev Public Health 36, 289–306. 10.1146/annurev-publhealth-032013-182516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower KM, Thorpe RJ Jr, Rohde C, Gaskin DJ, 2014. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Preventive medicine 58, 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd RW, Lindo EG, Weeks LD, McLemore MR, 2020. On racism: a new standard for publishing on racial health inequities. Health Affairs Blog 10. [Google Scholar]
- Cao X. (Jason), Mokhtarian PL, Handy SL, 2009. Examining the Impacts of Residential Self-Selection on Travel Behaviour: A Focus on Empirical Findings. Transport Reviews 29, 359–395. 10.1080/01441640802539195 [DOI] [Google Scholar]
- Caspi CE, Kawachi I, Subramanian SV, Adamkiewicz G, Sorensen G, 2012a. The relationship between diet and perceived and objective access to supermarkets among low-income housing residents. Soc Sci Med 75, 1254–1262. 10.1016/j.socscimed.2012.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi CE, Sorensen G, Subramanian SV, Kawachi I, 2012b. The local food environment and diet: A systematic review. Health & Place 18, 1172–1187. 10.1016/j.healthplace.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charreire H, Casey R, Salze P, Simon C, Chaix B, Banos A, Badariotti D, Weber C, Oppert J-M, 2010. Measuring the food environment using geographical information systems: a methodological review. Public Health Nutrition 13, 1773–1785. 10.1017/S1368980010000753 [DOI] [PubMed] [Google Scholar]
- Chor D, Cardoso LO, Nobre AA, Griep RH, Fonseca M. de J.M., Giatti L, Bensenor I, del Carmen Bisi Molina M, Aquino EML, Diez-Roux A, de Pina Castiglione D, Santos SM, 2016. Association between perceived neighbourhood characteristics, physical activity and diet quality: results of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). BMC Public Health 16. 10.1186/s12889-016-3447-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisinger B, 2016. A Mixed-Method Assessment of a New Supermarket in a Food Desert: Contributions to Everyday Life and Health. J Urban Health 93, 425–437. 10.1007/s11524-016-0055-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CAM, 2015. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results: The Local Food Environment and Obesity. Obesity 23, 1331–1344. 10.1002/oby.21118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S, 2005. Large scale food retailing as an intervention for diet and health: quasi-experimental evaluation of a natural experiment. Journal of Epidemiology & Community Health 59, 1035–1040. 10.1136/jech.2004.029843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S, Flint E, Matthews SA, 2014. New Neighborhood Grocery Store Increased Awareness Of Food Access But Did Not Alter Dietary Habits Or Obesity. Health Affairs 33, 283–291. 10.1377/hlthaff.2013.0512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curl CL, Beresford SAA, Hajat A, Kaufman JD, Moore K, Nettleton JA, Diez-Roux AV, 2013. Associations of Organic Produce Consumption with Socioeconomic Status and the Local Food Environment: Multi-Ethnic Study of Atherosclerosis (MESA). PLoS One 8. 10.1371/journal.pone.0069778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL, 2001. Neighborhood of Residence and Incidence of Coronary Heart Disease. New England Journal of Medicine 345, 99–106. 10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- Dubowitz T, Ghosh-Dastidar M, Cohen DA, Beckman R, Steiner ED, Hunter GP, Flórez KR, Huang C, Vaughan CA, Sloan JC, Zenk SN, Cummins S, Collins RL, 2015. Diet And Perceptions Change With Supermarket Introduction In A Food Desert, But Not Because Of Supermarket Use. Health Affairs 34, 1858–1868. 10.1377/hlthaff.2015.0667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echeverria SE, 2004. Reliability of Self-Reported Neighborhood Characteristics. Journal of Urban Health: Bulletin of the New York Academy of Medicine 81, 682–701. 10.1093/jurban/jth151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbel B, Moran A, Dixon LB, Kiszko K, Cantor J, Abrams C, Mijanovich T, 2015. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutrition 18, 2881–2890. 10.1017/S1368980015000282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESRI, 2009. ArcGIS Desktop: Release 9.3 Environmental Systems Research Institute., Redlands, CA. [Google Scholar]
- Franco M, Diez-Roux AV, Nettleton JA, Lazo M, Brancati F, Caballero B, Glass T, Moore LV, 2009. Availability of healthy foods and dietary patterns: the Multi-Ethnic Study of Atherosclerosis. The American Journal of Clinical Nutrition 89, 897–904. 10.3945/ajcn.2008.26434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvez MP, Morland K, Raines C, Kobil J, Siskind J, Godbold J, Brenner B, 2008. Race and food store availability in an inner-city neighbourhood. Public Health Nutr. 11, 624–631. 10.1017/S1368980007001097 [DOI] [PubMed] [Google Scholar]
- Gamba RJ, Schuchter J, Rutt C, Seto EYW, 2015. Measuring the Food Environment and its Effects on Obesity in the United States: A Systematic Review of Methods and Results. J Community Health 40, 464–475. 10.1007/s10900-014-9958-z [DOI] [PubMed] [Google Scholar]
- Hiza HAB, Casavale KO, Guenther PM, Davis CA, 2013. Diet Quality of Americans Differs by Age, Sex, Race/Ethnicity, Income, and Education Level. Journal of the Academy of Nutrition and Dietetics 113, 297–306. 10.1016/j.jand.2012.08.011 [DOI] [PubMed] [Google Scholar]
- Joassart-Marcelli P, Rossiter JS, Bosco FJ, 2017. Ethnic markets and community food security in an urban “food desert.” Environment and Planning A 49, 1642–1663. 10.1177/0308518X17700394 [DOI] [Google Scholar]
- Kern DM, Auchnicloss AH, Stehr MF, Diez Roux AV, Moore LV, Kanter GP, Robinson LF, 2017. Neighborhood Prices of Healthier and Unhealthier Foods and Associations with Diet Quality: Evidence from the Multi-Ethnic Study of Atherosclerosis. Int J Environ Res Public Health 14. 10.3390/ijerph14111394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khojasteh M, Raja S, 2017. Agents of Change: How Immigrant-Run Ethnic Food Retailers Improve Food Environments. Journal of Hunger & Environmental Nutrition 12, 299–327. 10.1080/19320248.2015.1112759 [DOI] [Google Scholar]
- Kurtz H, 2013. Linking food deserts and racial segregation: Challenges and limitations. Geographies of race and food: Fields, bodies, markets 247–264. [Google Scholar]
- Laraia BA, Siega-Riz AM, Kaufman JS, Jones SJ, 2004. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Prev Med 39, 869–875. 10.1016/j.ypmed.2004.03.018 [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC, 2009. Neighborhood Environments. American Journal of Preventive Medicine 36, 74–81.e10. 10.1016/j.amepre.2008.09.025 [DOI] [PubMed] [Google Scholar]
- Lei M-K, Simons RL, Beach SRH, Philibert RA, 2019. Neighborhood Disadvantage and Biological Aging: Using Marginal Structural Models to Assess the Link Between Neighborhood Census Variables and Epigenetic Aging. J Gerontol B Psychol Sci Soc Sci 74, e50–e59. 10.1093/geronb/gbx015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J, 1995. Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior 80–94. 10.2307/2626958 [DOI] [PubMed] [Google Scholar]
- Lytle LA, 2009. Measuring the Food Environment. American Journal of Preventive Medicine 36, S134–S144. 10.1016/j.amepre.2009.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews SA, Moudon AV, Daniel M, 2009. Work Group II: Using Geographic Information Systems for Enhancing Research Relevant to Policy on Diet, Physical Activity, and Weight. American Journal of Preventive Medicine 36, S171–S176. 10.1016/j.amepre.2009.01.011 [DOI] [PubMed] [Google Scholar]
- McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, Spiegelman D, Hunter DJ, Colditz GA, Willett WC, 2002. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. The American Journal of Clinical Nutrition 76, 1261–1271. 10.1093/ajcn/76.6.1261 [DOI] [PubMed] [Google Scholar]
- McCullough ML, Willett WC, 2006. Evaluating adherence to recommended diets in adults: the Alternate Healthy Eating Index. Public Health Nutrition 9, 152–157. 10.1079/PHN2005938 [DOI] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV, Brines S, 2008. Comparing Perception-Based and Geographic Information System (GIS)-Based Characterizations of the Local Food Environment. Journal of Urban Health 85, 206–216. 10.1007/s11524-008-9259-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR, 2008. Associations of the Local Food Environment with Diet Quality--A Comparison of Assessments based on Surveys and Geographic Information Systems: The Multi-Ethnic Study of Atherosclerosis. American Journal of Epidemiology 167, 917–924. 10.1093/aje/kwm394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Wing S, Roux AD, 2002. The Contextual Effect of the Local Food Environment on Residents’ Diets: The Atherosclerosis Risk in Communities Study. American Journal of Public Health 92, 1761–1768. 10.2105/AJPH.92.11.1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T, 2007. Assessing the Measurement Properties of Neighborhood Scales: From Psychometrics to Ecometrics. American Journal of Epidemiology 165, 858–867. 10.1093/aje/kwm040 [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, Shea S, 2008. Neighborhood Characteristics and Hypertension. Epidemiology 19, 590–598. 10.1097/EDE.0b013e3181772cb2 [DOI] [PubMed] [Google Scholar]
- Nettleton JA, Steffen LM, Mayer-Davis EJ, Jenny NS, Jiang R, Herrington DM, Jacobs DR, 2006. Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclerosis (MESA). The American Journal of Clinical Nutrition 83, 1369–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce J, Hiscock R, Blakely T, Witten K, 2008. The contextual effects of neighbourhood access to supermarkets and convenience stores on individual fruit and vegetable consumption. Journal of Epidemiology & Community Health 62, 198–201. 10.1136/jech.2006.059196 [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla R, 2009. Dietary Quality among Latinos: Is Acculturation Making Us Sick? Journal of the American Dietetic Association 109, 988–991. 10.1016/j.jada.2009.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, 2015. Is Racism a Fundamental Cause of Inequalities in Health? Annual Review of Sociology 41, 311–330. 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ, 2007. Food store availability and neighborhood characteristics in the United States. Preventive Medicine 44, 189–195. 10.1016/j.ypmed.2006.08.008 [DOI] [PubMed] [Google Scholar]
- Raffensperger S, Fanelli Kuczmarski M, Hotchkiss L, Cotugna N, Evans MK, Zonderman AB, 2010. Effect of Race and Predictors of Socioeconomic Status on Diet Quality in the HANDLS Study Sample. Journal of the National Medical Association 102, 923–930. 10.1016/S0027-9684(15)30711-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahmanian E, Gasevic D, Vukmirovich I, Lear SA, 2014. The Association between the Built Environment and Dietary Intake-A Systematic Review. Asia Pacific Journal of Clinical Nutrition 23, 183–196. 10.6133/apjcn.2014.23.2.08 [DOI] [PubMed] [Google Scholar]
- Rose D, Richards R, 2004. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutrition 7, 1081–1088. 10.1079/PHN2004648 [DOI] [PubMed] [Google Scholar]
- Silverman B, 1986. Density Estimation for Statistics and Data Analysis. CRC Press. [Google Scholar]
- StataCorp., 2013. Stata Statistical Software: Release 13. StataCorp LP., College Station, TX. [Google Scholar]
- Sundström J, Risérus U, Byberg L, Zethelius B, Lithell H, Lind L, 2006. Clinical value of the metabolic syndrome for long term prediction of total and cardiovascular mortality: prospective, population based cohort study. BMJ 332, 878–882. 10.1136/bmj.38766.624097.1F [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ver Ploeg M, Breneman V, Farrigan T, Hamrick K, Hopkins D, Kaufman P, Lin B-H, Nord M, Smith T, Williams R, Kinnison K, Olander C, Singh A, Tuckermanty E, Krantz-Kent R, Polen C, McGowan H, Kim S, 2009. Access to Affordable and Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences 160.
- Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W, 2009. Neighborhood Retail Food Environment and Fruit and Vegetable Intake in a Multiethnic Urban Population. American Journal of Health Promotion 23, 255–264. 10.4278/ajhp.071204127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, Mentz G, Miranda PY, Opperman A, Odoms-Young AM, 2014. Food Shopping Behaviors and Exposure to Discrimination. Public Health Nutr 17, 1167–1176. 10.1017/S136898001300075X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


