Abstract
Using observational data and variation in hospital admissions across days of the week, we examined the association between ED boarding time and development of delirium within 72 hours of admission among patients aged 65+ years admitted to an inpatient neurology ward. We exploited a natural experiment created by potentially exogenous variation in boarding time across days of the week because of competition for the neurology floor beds. Using proportional hazard models adjusting for socio-demographic and clinical characteristics in a propensity score, we examined the time to delirium onset among 858 patients: 2/3 were admitted for stroke, with the remaining admitted for another acute neurologic event. Among all patients, 81.2% had at least one delirium risk factor in addition to age. All eligible patients received delirium prevention protocols upon admission to the floor and received at least one delirium screening event. While the clinical and social-demographic characteristics of admitted patients were comparable across days of the week, patients with ED arrival on Sunday or Tuesday were more likely to have had delayed floor admission (waiting time greater than 13 hours) and delirium (adjusted HR = 1.54, 95%CI: 1.37–1.75). Delayed initiation of delirium prevention protocol appeared to be associated with greater risk of delirium within the initial 72 hours of a hospital admission.
Keywords: access/demand/utilization of services, aging, clinical practice patterns, geriatrics, health care organizations and systems, hospitals, integrated delivery systems, mental health, quality of care/patient safety
Introduction
Delirium is an acute cognitive disorder characterized by altered awareness, attentional deficits, confusion, and disorientation.1 Current estimates of new-onset delirium underscore the sobering fact that delirium overwhelmingly develops in medical settings (as high as 82% in intensive care settings) compared to the community at large (approximately 1%–2%).2 Critically, research has demonstrated that 30%–40% of all delirium cases are preventable.2–5
Although delirium reverberates through all age populations, older adults (≥65 years of age) are at greater risk of developing delirium during an acute illness, as are individuals with an underlying neurocognitive disorder (mild cognitive impairment and dementia). New-onset delirium in older patients alone translates to a high financial burden on the health care system.6,7 Despite known efficacy of inpatient delirium preventative strategies and predictive models to identify at-risk patients, new-onset delirium occurrence and the associated expenditures remain unchanged.8
Delirium represents a global challenge for healthcare managers, healthcare providers, and payors because it increases hospital costs (i.e., prolonged utilization of services and hospital stay) and also decreases hospital revenue (e.g., reimbursement penalties in value-based payment models).9–12 With the COVID-19 pandemic, administrators have faced several challenges with respect to managing hospital capacity.13,14 As a result, multiple stakeholders began to review their hospital admission processes with the ultimate goal of improving patient outcomes.
However, ongoing endeavors to assess the efficacy of delirium prevention strategies have overlooked the key contributing factors, such as the healthcare experience prior to receiving preventive measures on the inpatient wards (e.g., ED experience and bed transfer processes). Therefore, individuals that experience a delay between initial ED arrival and transfer to an inpatient bed (i.e., “delayed bed-flow,” “boarding”) may have delayed access to preventative care. Unfortunately, traditional estimates of the association between ED boarding and delirium have been confounded by baseline disease severity and other unmeasured variables. For instance, greater disease severity might reduce the ED boarding time while increase delirium risk.
We exploited a natural experiment created by exogenous bed competition to examine the impact of prolonged ED boarding (certain days of the week) on the risk of delirium within 72 hours of admission.
Methods
Study design
We conducted a retrospective study using data abstracted from routine clinical care documented in electronic health records (EHRs) of a large academic medical center between 01/2016 and 12/2018. Our hypothesis was that prolonged ED boarding (i.e., waiting time at the fourth quartile) increases the risk of delirium during an urgent inpatient admission. In our conceptual framework (Figure 1), the association between ED boarding and delirium might be confounded by disease severity and other variables. However, based on the assumption that no one can choose the day of the week they will have a neurological emergency (i.e., strokes are unpredictable), one could putatively exploit the exogenous variation in neurology floor bed competition to indirectly examine the association between ED boarding time and delirium risk.
Figure 1.
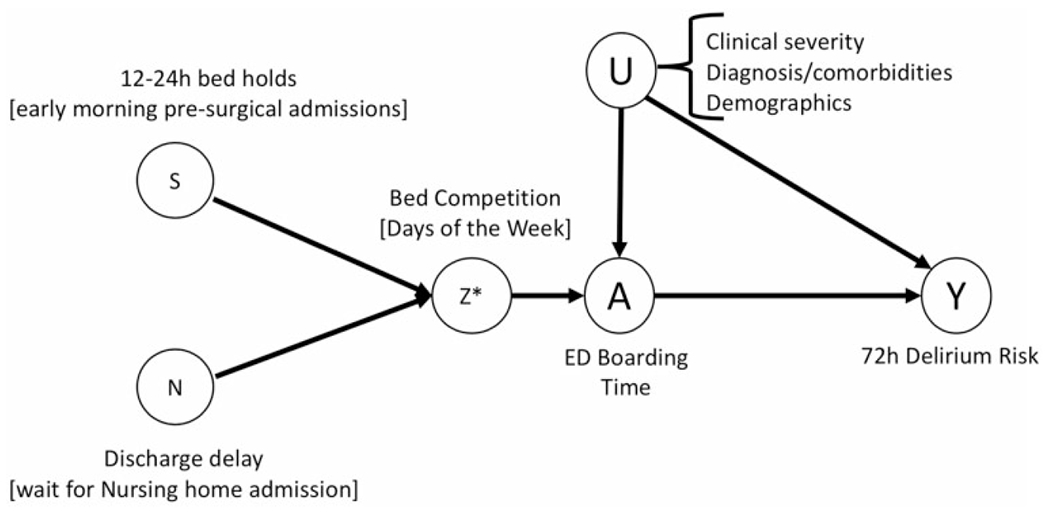
Conceptual framework and hypotheses. Directed acyclic graph (DAG) depicts why ED boarding time should not be simply regressed towards 72h delirium risk (confounded by several knowns and potentially unknown and unmeasurable factors). Instead, we used an exogenous proxy variable for bed competition, which directly alters ED boarding.
Source of participants and data
Between 01/2016 and 12/2018, 79,467 older patients (≥65+ years) were evaluated in our emergency department (ED). From this population, we identified all patients who were subsequently transferred to a specific study neurology hospital floor (n = 1,725), which had implemented a systematic program for delirium prevention and screening. We excluded those who did not have at least one delirium assessment completed during the inpatient stay (n = 867 out of 1,725), resulting in a final analytical sample of 858 patients (Figure 2).
Figure 2.
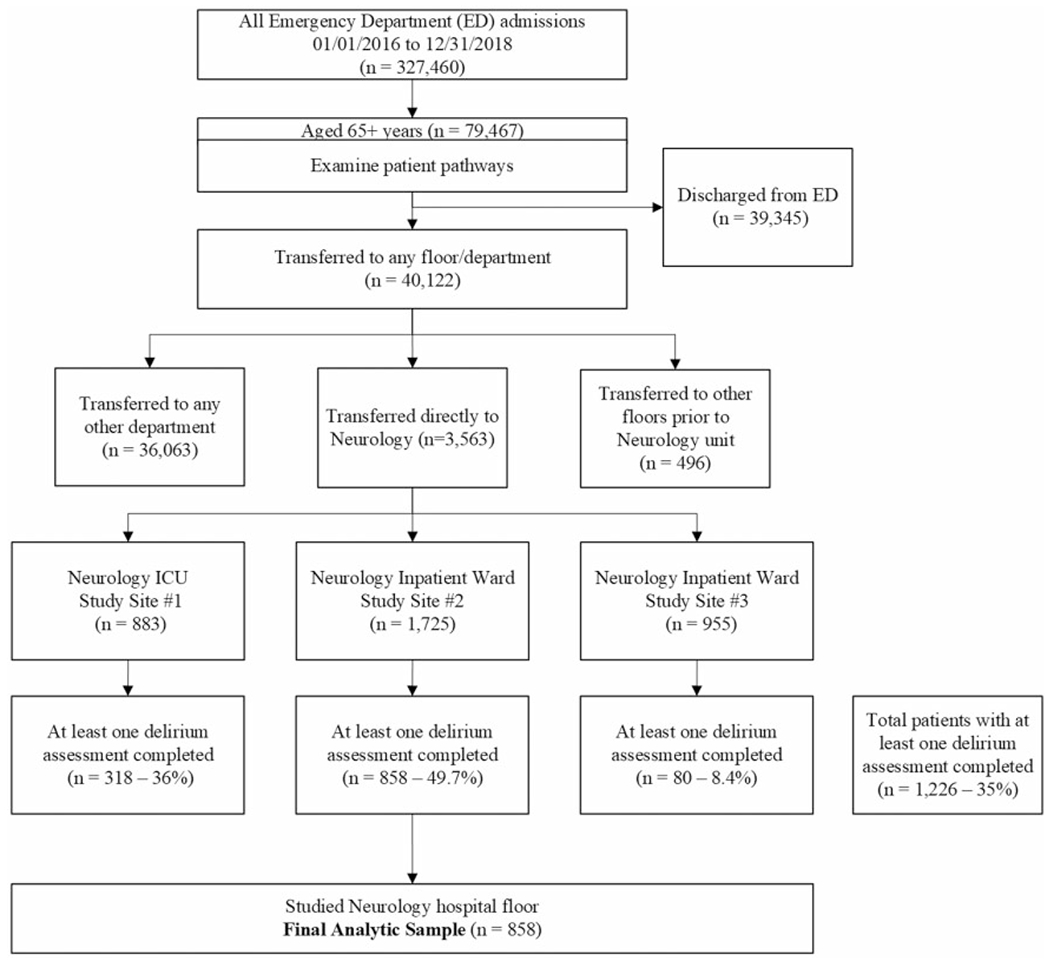
Patient sampling strategy. ED: Emergency Deparment. ICU: Intensive Care Unit.
Delirium prophylactic protocol and screening: In accordance with national guidelines, the study neurology hospital floor has a delirium screening and prevention program.5 The prevention program is based on multimodal, nonpharmacologic delirium prevention programs such as the “The Hospital Elder Life Program” (HELP) and incorporates several preventive measures, including redirection, review of medications, avoidance of restraints.3,15 Delirium screening assessments are performed by registered nurses using the modified Confusion Assessment Method (CAM) and documented in the electronic medical record. Previous controlled studies found that these interventions are effective in preventing delirium, cognitive, and functional decline.16,17 We further detail the program in Supplementary Text 1.
Variables
This study combines demographic (A), clinical (B), process (C), and outcome (D) information:
A: Demographic Information:
We acquired basic demographic information (e.g., age, gender, race) and enriched it with measures of socio-economic status (e.g., insurance type) and other pertinent data (e.g., community dwelling vs not) (Table 1, Supplementary Table 1).
Table 1.
Demographic information (day of the week).
| Overall | Sunday | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| 858 | 132 | 116 | 119 | 125 | 123 | 130 | 113 | ||
| Age at admission (mean (SD)) | 77.99 (8.58) | 77.54 (7.99) | 77.97 (8.58) | 77.02 (8.54) | 78.46 (8.77) | 78.33 (9.45) | 78.35 (8.13) | 78.29 (8.75) | 0.832 |
| Gender = male (%) | 439 (51.2) | 65 (49.2) | 60 (51.7) | 70 (58.8) | 63 (50.4) | 64 (52.0) | 63 (48.5) | 54 (47.8) | 0.681 |
| Admission source = institutionalizeda (%) | 324 (37.8) | 59 (44.7) | 40 (34.5) | 46 (38.7) | 34 (27.2) | 46 (37.4) | 50 (38.8) | 49 (43.4) | 0.096 |
| Race (%) | 0.394 | ||||||||
| Black | 49 (5.9) | 3 (2.3) | 9 (7.8) | 8 (6.8) | 13 (10.8) | 6 (5.2) | 5 (3.9) | 5 (4.5) | |
| Otherb | 60 (7.2) | 11 (8.5) | 6 (5.2) | 10 (8.5) | 7 (5.8) | 7 (6.0) | 9 (7.1) | 10 (9.0) | |
| White | 727 (87.0) | 115 (89.1) | 100 (87.0) | 100 (84.7) | 100 (83.3) | 103 (88.8) | 113 (89.0) | 96 (86.5) | |
| Primary insurance (%) | 0.545 | ||||||||
| Commercialc | 221 (25.9) | 32 (24.2) | 28 (24.1) | 27 (23.1) | 31 (25.2) | 29 (23.6) | 45 (34.6) | 29 (25.7) | |
| Medicare | 610 (71.4) | 98 (74.2) | 86 (74.1) | 86 (73.5) | 90 (73.2) | 91 (74.0) | 80 (61.5) | 79 (69.9) | |
| Otherd | 23 (2.7) | 2 (1.5) | 2 (1.7) | 4 (3.4) | 2 (1.6) | 3 (2.4) | 5 (3.8) | 5 (4.4) |
Skilled Nursing Facility; Psych, Substance Abuse, or Rehab Hospital; Outside Health Care Facility; Outside Hospital or Ambulatory Surgery Center.
Asian; Hispanic or Latino; American Indian or Alaska Native.
Blue Cross Blue Shield; Tufts Health Plan; Harvard Pilgrim; Neighborhood Health Plan and Allways Health Partners.
Medicaid, Free Care; Workers Comp / Motor Vehicle; Other Government; Self-pay and International.
B. Clinical Information:
We obtained data on presence of known delirium risk factors, such as stroke, visual impairment, and fall, from a validated Clinical Classifications Software (ACUP-AHRQ-CCS) for inpatient stays, which utilizes an ICD-10 diagnosis and procedure categorization scheme (Supplementary Table 2, Supplementary Table 3).
C: Process Information:
We abstracted the date and time in which patients arrived at the emergency department. From these variables, we categorized ED arrival date according to days of the week (Monday-Sunday). Second, we created an indicator variable for “Delay”, time from ED arrival-to-neurology bed transfer and categorized in quartiles (Delay, yes ≥13.4 hours vs. no ≤5.97 hours).
D: Outcome Information:
Delirium was assessed using the modified Confusion Assessment Method (CAM), which have been validated in post-stroke populations (94–100% sensitivity, 89–95% specificity, and high inter-rater reliability). At least 49.7% of the study neurology ward patients were assessed (Figure 2). Some patients could be reevaluated the same day as needed. We captured all CAM assessments for each patient and created our primary outcome variable: time from ED arrival to first CAM positive within a 72 h observation period (CAM positive indicated delirium). For sensitivity analysis, we also derived a binary indicator variable for delirium (yes vs no within 72 h of admission, Supplementary Table 4).
Data analytic approach
To address potential confounders for the primary analysis, we estimated the probability (propensity score) of arriving on each day of the week (Monday-Sunday). We used a categorical logistic-regression to predict the odds of arriving on each day of the week. We examined the distribution of propensity scores across different days of the week, examined for normality assumptions, and compared propensity score means across each day of the week and examined how well the propensity score balanced for potential confounders.
The potential confounders were obtained from linked encounter-level electronic medical record data, and included age, gender, race, site of origin (community dwelling vs not), insurance type, and known comorbidity (e.g., presence of known delirium risk factors such as stroke, visual impairment)). The percentage of patients with missing data for these variables was low (<1%). For missing data, we assumed missingness at random and conducted a complete case analysis.
We compared time from ED door arrival to first documentation of delirium (CAM positive) within a 72h period among those who arrived on different days of the week using a cox proportional hazards model, with propensity score adjustment (as a continuous linear term). To reduce the potential bias from differential follow-up times and the impact the inpatient care and drugs might have on delirium risk overtime that is unrelated to arrival conditions, we limited the maximal follow-up time to 72h. Censored observations included death, transfer, or discharge before 72h. We examined Schoenfeld residuals to examine for potential violation of the proportional-hazards assumption. We reported hazard ratios and 95% confidence intervals for unadjusted and stepwise adjusted analysis. We estimated at least 90% power to detect a 50% higher hazard of delirium, using an estimated sample of at least 100 patients per day of the week (exponential test, hazard difference, alpha 0.5).
Sensitivity analysis:
We conducted additional prespecified sensitivity analysis and examined the robustness and validity of our findings in several ways:
Statistical assumptions:
First, we avoided the use of the propensity score and compared time from ED door arrival to first delirium (CAM+) documented within a 72h period among those who arrived on early days of the week (Sunday-Wed = high demand) versus late days of the week (Thursday-Saturday = low demand) using cox proportional hazards models, with and without adjustment for the potential confounders used in the main analysis; Second, we avoided the use of survival analysis (cox proportional hazards assumption might be unrealistic) and estimated the 72 h odds of delirium using logistic regression models, assuming no loss to follow-up (given very short follow-up time), with and without adjustment for the potential confounders listed in the main analysis. Third, we observed that the care experience of those who arrive to the ED during day might be different than the care experience of those who arrive at night. We hypothesized that “shift” could explain the effect of ED boarding on delirium risk (e.g., more severe cases arriving at night). Delirium screening was implemented at every shift (day and night). We compared time from ED door arrival to first delirium (CAM+) documented within a 72h period among those who arrived on different days of the week using cox proportional hazards models, with propensity score adjustment plus additional adjustment for time of the day (i.e., using “shift” as a binary predictor, meaning arrival to the ED during day vs night hospital shift).
Screening effect:
Systematic delirium screening is hypothesized to naturally increase its detection rate. If ED boarding time increases the 72h delirium risk independent of the destination floor, we expect replication of the results in other samples and settings where delirium prevention protocol was either not done or done differently. For instance, more severe cases (as opposed to systematic screening as in the study floor) are more likely to be screened in a neurological intensive care unit. To examine this assumption, we repeated the analysis expanding the sample to all neurology inpatients (the study floor, one neurological intensive care unit, and one additional neurology floor).
Face validity:
We exploited two potential reasons for competing demands for the neurology floor beds: a) On certain days of the week (e.g., week days), neurosurgeons place holds on floor beds to accommodate the post-operative needs of their scheduled patients, whereas there are fewer bed holds on weekends (Supplementary Table 5); and b) On certain days of the week (e.g., Sundays), discharges from hospital to another institution (e.g., skilled nursing facilities) are systematically delayed until Monday morning (Supplementary Table 6). With high demand for beds, patients admitted from the ED frequently “board” in the ED on Sunday night or Tuesday night until a floor bed opens. The nursing responsibility transfers from ED nurses to neurology ward nurses when the patient arrives on the inpatient ward.
Results
Of the 858 patients who presented to the ED with a neurological emergency, 697 (81.2%) had at least one delirium risk factor in addition to age (e.g., stroke, visual impairment, fall, dementia), with mean age 78 ± 9 years, 51.2% men, and 84.7% white. Patients arriving on different days of the week with neurological emergencies were comparable with respect to age, gender, race, site of origin, insurance type, and comorbidities. Delirium was documented in 234 (30%) patients within the first 72h from ED arrival. Table 1 summarizes the demographic characteristics of the patients upon ED arrival.
This study demonstrated an association between days of the week and delirium. ED arrival on Sundays and Tuesdays were associated with shorter time to delirium onset (Sunday: propensity score adjusted HR = 1.54 for delirium onset, 95%CI:1.36–1.75; Tuesday: propensity score adjusted HR = 1.39 for delirium onset, 95% CI:1.22–1.58) in a 72-study follow-up time-frame, using Friday as reference day. These results were similar using different days of the week as reference, and also after adjusting for time of the day (i.e., day vs night shift) (Supplementary Table 7 and 8). For illustrative purposes, we provided unadjusted delirium survival curves (Figure 3(a) to (c) and Supplementary Figure 1). Findings were similar using the sample of all neurology inpatients (each with different protocols for use/screening for delirium).
Figure 3.

(a) Delirium free survival probability - all study sample. Legend: Delirium free survival probability with time zero defined as ED arrival time, failure event defined as first occurrence of delirium (CAM positive), censoring events defined as end of follow up at 72h or loss to follow-up (e.g., death, transference to other units, discharge).(b) Delirium free survival probability (days of the week). Legend: Delirium free survival probability within observational period of 72 h, with time =0 as ED arrival and end of follow up as 72h, occurrence of delirium or loss to follow-up (e.g., death, transference to other units, discharge). Log-rank test null hypothesis – all survival curves are the same. We can reject the null hypothesis and suggest that there was a difference in delirium survival curves for at least one curve (p = 0.03). (c) Delirium free survival probability (Wednesday vs. not). Legend: Delirium free survival probability within observational period of 72 h, with time =0 as ED arrival and end of follow up as 72h, occurrence of delirium or loss to follow-up (e.g., death, transference to other units, discharge). Groups were categorized based on ED arrival day (Wednesday vs all else). Log-Rank test Null hypothesis – both survival curves are the same. There was a substantial difference in delirium survival for those arriving on Wednesday (red line) vs not (p = 0.005).
Sensitivity analysis:
ED arrival on early days of the week (binary, early meaning Sunday to Wednesday vs late meaning Thursday to Saturday) was still associated with a shorter time from ED arrival to delirium onset using covariate adjustment (covariate adjusted HR: 1.242, 95% CI 1.04–1.48), Supplementary Table 9. The adjusted 72h odds of delirium was 1.95-fold greater (95% CI 1.05–3.64) for those arriving to ED on Sunday compared to Saturday, for instance (Supplementary Table 10).
ED arrival on Sundays was associated with delayed floor admission (waiting time greater than 13.4 hours = time from ED arrival to transfer to inpatient bed, p < 0.001, Supplementary Table 11) and with lowest proportion of hospital to skilled nursing facility discharges (p < 0.001, Supplementary Table 6). Similarly, ED arrival on Tuesdays was associated with delayed floor admission (p < 0.001, Supplementary Table 11) and with greater proportion of elective pre-surgical admissions on Wednesday morning, p < 0.001, Supplementary Table 5).
Figure 4 illustrates the measures of bed competition (i.e., elective pre-surgical admissions and discharges to nursing homes or alike), the overtime proportion of patients who had prolonged ED boarding time (i.e., >13h), and the various 72h-delirium hazard ratios in relation to days of the week. In summary: a) the ED boarding time followed the trends in the measures of bed competition, and b) ED boarding time was associated with the 72h-delirium hazard ratio.
Figure 4.
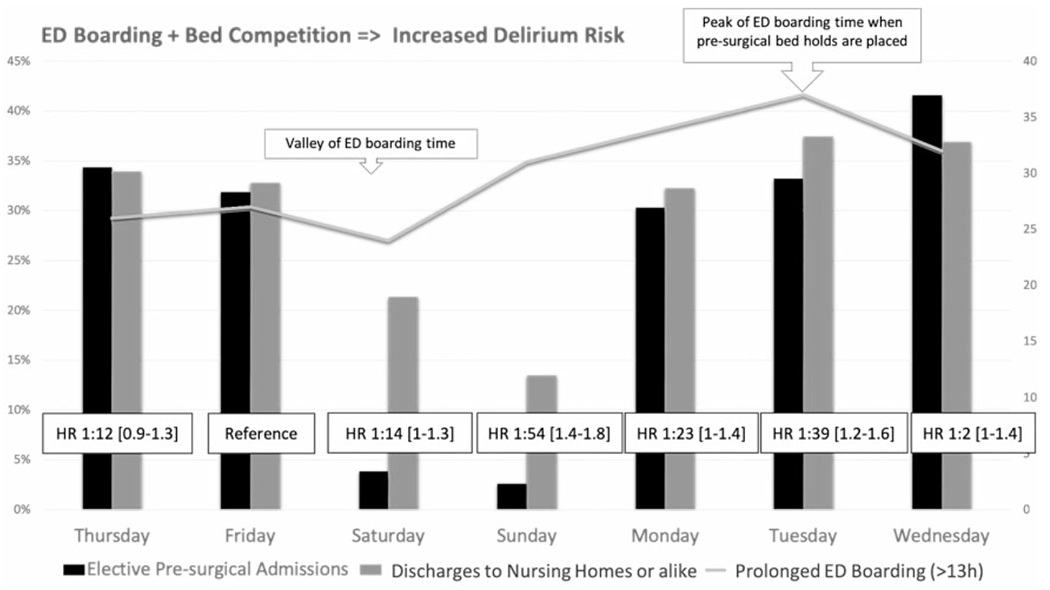
72h delirium risk and bed competition. Grey line: Proportion of Prolonged ED boarding time(defined as greater than 13.4 h of waiting from ED arrival to bed transfer). Gray bars: Proportion of discharges to Nursing homes or alive, in relation to all discharges of the study cohort. Black bars: Proportion of elective pre-surgical admissions, in relation to all admissions to the study neurology floor.
Discussion
Older patients admitted from the ED with neurological emergencies have a substantial risk of developing delirium early in their hospitalization. Our study also reveals that increased “boarding time” (or delayed transfer to the hospital floor) is associated with greater short-term risk of delirium in this natural experiment. While risk factors for delirium are multi-dimensional and time-varying, our study identified areas for process improvement that could have a real link with outcomes leading to improved patient care and decreased health care spending.
Our study has several strengths including our very large sample size and its reasonably high rate of delirium, making our comparisons robust. By demonstrating an association between prolonged ED lengths of stay and elevated risk of delirium onset during admission, our results are consistent with the evolving literature suggesting that delirium prophylaxis is critical to prevention and that delays in this process increase the risk of the development of delirium.
Specifically, our study demonstrates that risk of developing delirium during hospitalization is greatest for older patients with acute neurologic conditions who present to the ED on days with higher risk of prolonged ED lengths of stay. One prior study that evaluated the association between ED length of stay and incident delirium, also showed a prolonged ED length of stay (10 hours or greater) prior to admission doubled the risk for delirium onset;18 this study, however, excluded patients with acute stroke which is one of the major risk factors for delirium among older adults. Delirium is a frequent complication of stroke (10–42%).17,19
We theorized that the increased risk of delirium is related to a combination of the care experienced at the ED department and the delayed implementation of delirium prevention measures. For instance, it is also possible that the physical environment of, care limitations of, and/or therapeutics administered in the ED contribute to this short-term increased risk. The physical environment of the ED, with bright lights and high ambient noise level 24 hours a day, is potentially deliriogenic and contrary to the sleep hygiene measures recommended by national delirium prevention guidelines.20–22
This study’s results are intuitively and quantitatively valid. Presenting to the hospital earlier in the week, e.g., Sunday and Tuesday, conveyed higher risk of delirium than presenting later in the week, e.g., Saturday. Some delays in admission have been attributable to exogenous factors. For example, we know that during weekends neurological floors have fewer discharges to skilled nursing facilities (SNF), which, in turn, influences the number of beds available for new admissions on those floors. With respect to mid-week days, we recognized that elective admission to neurological floors, medical or surgical, may impact the number of available beds and cause further delays in admission.23 In this study, we exploited the fact that acute emergencies (e.g., stroke) are largely unpredictable, and will continue to occur independent of human’s ancient Greek calendar scheme (days of week), surgeon’s schedule, or SNF’s opening policies.
In this study, we tested different categorization assumptions for the predictor variable (individual days of the week vs binary), different modeling assumptions (cox proportional hazard vs steady state assumptions), as well as different samples (more homogeneous study floor with high screening rate vs all study floors with low screening rate and a heterogeneous population). The association was stronger with increasing effective sample size (e.g., all samples) and increasing number of assumptions (e.g., propensity score, binary predictor categorization). Overall, our study conclusions about differential short-term delirium risk according to days of the week remained robust across all methods.
Our face validity exploratory analysis, while hypothesis-generating in our work, creates avenues for further study in optimizing communication paths between ED and Neurology department providers. Prioritizing ED arrivals over elective surgery admissions could improve patient care delivery regardless of baseline medical condition. This further adds to the discussion for multidisciplinary neurological care to use large and real-care data analysis to cross departmental boundaries and rethink in-hospital processes. More importantly, it provides an opportunity to make targeted interventions for high risk patients in a high-volume and critical care environment.
This study has several limitations. First, it was conducted at a single tertiary academic center with which may limit its generalizability. This center is known for providing excellent quality care in the emergency room, which suggests that our results could represent a conservative estimation of the impact of ED boarding on delirium risk. Because our center is a tertiary academic center, we may have received a greater share of severe cases when compared to community hospitals. In addition, we also limited our main analysis to patients with neurological emergencies. In fact, roughly two thirds of the patients that were included had stroke as a primary diagnosis and this study did not include details of their stroke type, severity at initial presentation in the ED, which would include hemodynamics, cardiac and pulmonary status, and whether or not they had significant altered mentation or level of consciousness. Because number, type, and severity of medical conditions are known risk factors for delirium, our study may have overestimated the general 72h in-hospital delirium prevalence.
Second, the delirium screening (CAM protocol) was not implemented consistently among the older patients admitted through the ED, with only 50% of patients being screened within the 72h study period. In our main analysis, we chose the study floor that had implemented a systematic protocol for screening at least twice per day to attempt to eliminate the variable of staff judgment when screening. However, the well-trained nurses still used their best judgement about who could have deferred screening in a large proportion of cases. Therefore, it is possible that those at higher risk for delirium (e.g., older age) were more likely to have a documented delirium screening. In a worst-case scenario, if we assume that the in-hospital unconscious selection of patients to screen for delirium was driven by a nurses’ judgment (prior probability of potential risk for delirium), we expect that the analytical sample would systematically exclude those healthier patients. However, the nurses’ judgment is expected to be independent of the day of the week surgeon’s schedule, and SNF’s opening policies. In this scenario (extreme case of independent differential misclassification of the outcome), the results could represent an over or underestimate of the true rates of delirium. In this scenario of independent non-differential misclassification of a binary outcome, the estimates are still valid (preserves type I error, alpha set) but is likely conservative (towards the null). Therefore, our results are likely conservative in the main analysis, and potentially biased in an unpredictable direction in the all sample analysis. Further, one could use the reported CAM specificity (95.9%) to obtain the adjusted estimate of the risk.24
Another common potential source of bias is the misclassification of covariates (e.g., diagnoses). As outlined before, we attempted to mitigate misclassification bias with careful and conservative sensitivity analysis and face validity checks. One additional source of potential misclassification is our use of “elective presurgical admissions” as a proxy for “bed-holds” for surgery. We measured the volume of neurology admissions coming from the elective surgical admission department (as opposed to the ED department or else). An ideal measure of bed competition would actually be the volume of “bed holds” placed by surgeons each day (some eventually become an elective surgical admission while others are canceled for several reasons).
Our study could not differentiate the effect of prolonged lengths of stay in the ED environment (e.g., noisy and disruptive day and night) from the effect of delayed initiation of delirium prevention protocol on the neurology floor. Though some EDs do have volunteer-based programs similar to the HELP delirium prevention program,25 there are no studies evaluating the impact of ED-initiated delirium prevention programs on incident delirium.
The specific or long-term impact of preventive strategies for delirium is an area for further study. Physicians in training have reported delirium prevention education is often sparse and disproportionate to their exposure to high risk patients.26 In addition to enhanced awareness, electronic delirium risk alerts and targeted deployment of hospital resources are all avenues by which delirium screening rates could improve, and thereby outcomes for high risk patients, can be immediately improved.
Finally, our study was not designed to demonstrate causation (cause-and-effect). A randomized controlled clinical trial would not be feasible or ethical in this vulnerable population of patients with neurological emergencies. Therefore, we conducted this rigorous observational study that identified an association between ED boarding time and the documentation of delirium in the first 72 hours of admission.
In a healthcare management framework, common factors associated with ED boarding could be grouped into four main categories: a) how primary care and continuity are organized, b) the existence and effectiveness of organizational models and clinical pathways for chronic patients, c) the presence of bottlenecks related to ED’s personnel or equipment endowment, and d) how the ED is organized and its connection with the rest of the hospital.27 Our study may help healthcare managers to identify feasible targets for process improvement in the connection between ED and the rest of the hospital (e.g., a sensible elective surgery’s schedule).
This study design did not seek to determine whether it is prolonged ED boarding time or the delayed Neurology transfer arrival that increased the risk of delirium. Some argue that the ED boarding is “delirium-genic” (i.e., the extra hours in the ED extends the patient’s exposure to noisy, cold, stressful, and unwelcoming environment without direct exposure to external light). In contrast, the delirium prevention protocols include steps to minimize potential environmental insults. Nevertheless, this study provides some feasible suggestions for process improvement that are still within the scope of healthcare managers, such as better alignment between discharge volume needs and SNF’s admitting hours. This represents a new category for process improvement in the healthcare management framework: relationships between hospitals and post-acute care facilities.
Conclusion
Older patients admitted from the ED with neurologic conditions have a substantial risk of developing delirium early in their hospitalization. Prolonged wait for transfer to the hospital floor appear to be associated with increased risk of delirium in this natural experiment. Hospital complications such as delirium might be prevented by early initiation of prophylaxis protocols and transfer from the ED to the hospital bed. Healthcare managers may improve outcomes and reduce spending by removing bottlenecks in the clinical pathways across primary care, emergency rooms, operating rooms, and post-acute services.
Supplementary Material
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental material
Supplemental material for this article is available online.
References
- 1.Sachdev PS, Blacker D, Blazer DG, et al. Classifying neurocognitive disorders: the DSM-5 approach. Nat Rev Neurol 2014; 10: 634–642. [DOI] [PubMed] [Google Scholar]
- 2.Dharmarajan K, Swami S, Gou RY, et al. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc 2017; 65: 1026–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999; 340: 669–676. [DOI] [PubMed] [Google Scholar]
- 4.Inouye SK, Westendorp RGJ and Saczynski JS. Delirium in elderly people. Lancet 2014; 383: 911–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Neurology. Inpatient and emergency neurology: quality measurement set. https://www.aan.com/siteassets/home-page/policy-and-guidelines/quality/quality-measures/17iemeasureset_pg.pdf (2016).
- 6.Dittrich T, Tschudin-Sutter S, Widmer AF, et al. Risk factors for new-onset delirium in patients with bloodstream infections: independent and quantitative effect of catheters and drainages-a four-year cohort study. Ann Intens Care 2016; 6: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lundstrom M, Edlund A, Karlsson S, et al. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc 2005; 53: 622–628. [DOI] [PubMed] [Google Scholar]
- 8.Davis DH, Kreisel SH, Muniz Terrera G, et al. The epidemiology of delirium: challenges and opportunities for population studies. Am J Geriatr Psychiatry 2013; 21: 1173–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collier R Hospital-induced delirium hits hard. Can Med Assoc J 2012; 184: 23–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haas DA, Kaplan RS, Reid D, et al. Getting bundled payments right in health care. Harvard Business Review, Available at: https://hbr.org/2015/10/getting-bundled-payments-right-in-health-care (2015). [Google Scholar]
- 11.Mate KS and Compton-Phillips AL. The antidote to fragmented health care. Harvard Business Review, Available at: https://hbr.org/2014/12/the-antidote-to-fragmented-health-care (2014). [Google Scholar]
- 12.Porter ME and Kaplan RS. How to pay for health care. Harvard Business Review, July–August 2016, pp.88–100). Available at: https://hbr.org/2016/07/how-to-pay-for-health-care [PubMed] [Google Scholar]
- 13.Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US department of veterans affairs hospitals during the COVID-19 pandemic. JAMA Netw Open 2021; 4: e2034266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eriksson CO, Stoner RC, Eden KB, et al. The association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med 2017; 32: 686–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inouye SK, Baker DI, Fugal P, et al. Dissemination of the Hospital Elder Life Program: implementation, adaptation, and successes. J Am Geriatr Soc 2006; 54: 1492–1499. [DOI] [PubMed] [Google Scholar]
- 16.Inouye SK, Van dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113: 941–948. [DOI] [PubMed] [Google Scholar]
- 17.Mitasova A, Kostalova M, Bednarik J, et al. Poststroke delirium incidence and outcomes: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med 2012; 40: 484–490. [DOI] [PubMed] [Google Scholar]
- 18.Bo M, Bonetto M, Bottignole G, et al. Length of stay in the emergency department and occurrence of delirium in older medical patients. J Am Geriatr Soc 2016; 64: 1114–1119. [DOI] [PubMed] [Google Scholar]
- 19.Dahl MH, Ronning OM and Thommessen B. Delirium in acute stroke–prevalence and risk factors. Acta Neurol Scand Suppl 2010; 190: 39–43. doi: 10.1111/j.1600-0404.2010.01374.x. [DOI] [PubMed] [Google Scholar]
- 20.Grover S and Avasthi A. Clinical practice guidelines for management of delirium in elderly. Indian J Psychiatry 2018; 60: S329–S340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inouye SK, Bogardus ST Jr, Baker DI, et al. The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. J Am Geriatr Soc 2000; 48: 1697–1706. [DOI] [PubMed] [Google Scholar]
- 22.National Institute for Health and Care Excellence. Clinical guidelines, www.ncbi.nlm.nih.gov/books/NBK11822/ (2003, accessed 27 December 2019).
- 23.Mchugh M, Regenstein M and Siegel B. The profitability of Medicare admissions based on source of admission. Acad Emerg Med 2008; 15: 900–907. [DOI] [PubMed] [Google Scholar]
- 24.Gusmao-Flores D, Salluh JI, Chalhub RA, et al. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care 2012; 16: R115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanon M, Baumlin KM, Kaplan SS, et al. Care and respect for elders in emergencies program: a preliminary report of a volunteer approach to enhance care in the emergency department. J Am Geriatr Soc 2014; 62: 365–370. [DOI] [PubMed] [Google Scholar]
- 26.Pickett J, Haas MRC, Fix ML, et al. Training in the management of psychobehavioral conditions: a needs assessment survey of emergency medicine residents. AEM Educ Train 2019; 3: 365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vainieri M, Panero C and Coletta L. Waiting times in emergency departments: a resource allocation or an efficiency issue? BMC Health Serv Res 2020; 20: 549. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


