Abstract
Purpose
Piezoelectric bone surgery was already extensively used in a number of surgical procedures ranging from dental to maxillofacial surgery. The authors aimed to determine whether piezosurgery was suitable and advantageous for performing osteotomies in Hand and Plastic reconstructive surgery.
Methods
The authors overviewed a variety of applications for Piezosurgery® Device, from Mectron, in bone reconstructive surgery with over the last 8 years. An overall number of 156 bone cutting procedures in adults and children was described at the phalanges, metacarpal bones and distal radius level, as well as in bone graft harvesting and bone remodeling following carpal scaphoid nonunion, scapho-lunate bone-ligament-bone reconstruction and fibula free flap in maxillofacial defects.
Results
The consolidation rate was 87.5% in scaphoid nonunion grafting and fixation. Bone healing was achieved in all other cases. No intra-operative complications were recorded.
Conclusion
Piezosurgery® allowed high precision in bone cutting as well as custom-made graft and surface roughness were obtained, while preserving nerves, vessels and tendons integrity. The instrument may be handling moved into the surgical space in absence of vibrations, with a clear view onto the bone. The mechanical and biological characteristics of the piezoelectrical effect perfected this technique as an effective and useful instrument in Hand and Plastic surgery. The selective bone cutting properties avoided injuries to the surrounding soft tissues and thermal damage of the bony cells. Best advantages were described in feasibility and flexibility for intra-articular osteotomies, custom-made grafts and reconstructive microsurgical techniques.
Keywords: Piezoelectric, Bone surgery, Osteotomy, Bone graft, Hand surgery, Plastic surgery
Introduction
The traditional procedure such as sawing, drilling, grinding and milling were associated with several drawbacks facing with bone cutting or remodeling [1–4]. In Hand and Plastic surgery, major challenges arose by the small bones and the proximity of fine anatomical structures.
Bone healing in osteotomy was minimized reducing the thermal damages. A wide variety of parameters were involved in heat generation such as instrument thickness, the force and the speed applied by the rotatory tools, or the utilization of coolant to minimize the temperature rising [2, 5, 6]. Greater force and higher speed resulted in less thermal damage to the bone, as well as multiple drill-hole osteotomy, instead of sawing [7, 8]. Chisels and scalpels may avoid thermal injuries but significantly increased the risks of breakage and inaccurate cutting. When milling was requested in accurate machining of bone surfaces, the thermal damage was greater than cutting, reaching since to 2 mm in depth. According to the bone thickness and properties, the applied cutting forces increased according to the bone density, and temperature increased 10% with a 12% increase in bone density [9].
On the other hand, nerve and tendon lesions were feared complications recurring to oscillating saws and rotational instruments or chisels.
Osteotomies required accurate execution, high precision, strict control, limiting also the damage to surrounding either neurovascular or tendon structures. Piezosurgery® was an advanced device which used the ultrasonic microvibrations to fulfill accurate and selective cut on the bone, in harmony with the surrounding soft tissues and with the thermal bone biology [2, 6]. The piezoelectric effect applied electric tension across the devise producing ultrasonic vibrations and waves. The mechanical contact and the cutting-hammering movement of the tip of the instrument onto the bone induced linear disorganization and fragmentation. Only mineralized tissue was selectively cut at the frequency range of 25–30 kHz, because of soft tissue would only be cut by above 50 kHz [3, 6]. The bone temperature was maintained by the cavitation effect which also washed away debris and cleared the surgical field, enhancing the visibility and ease of operation [4].
The escalating role of piezoelectric bone surgery was improved in surgical techniques requiring fine and high defined cut and remodeling, ranging from implantology and reconstructive maxillo-facial surgery to hand and plastic surgery.
Materials and Methods
Piezosurgery® Device from Mectron (Carasco GE, Italy) was used in 156 bone osteotomies and bone grafts, instead of the usual oscillating saw or chisels/scalpels in adults (102 patients), or multiple drill-hole technique in children (54 patients). Over the last 8 years, the authors used the piezoelectric effect in 83 osteotomies at the phalanges, metacarpal bone and distal radius, as well as in 73 bone grafts following carpal scaphoid nonunion and scapho-lunate bone-ligament-bone reconstructions, of free fibula flaps. Bone union rate was the outcome of interest in all cases.
Congenital Deformities
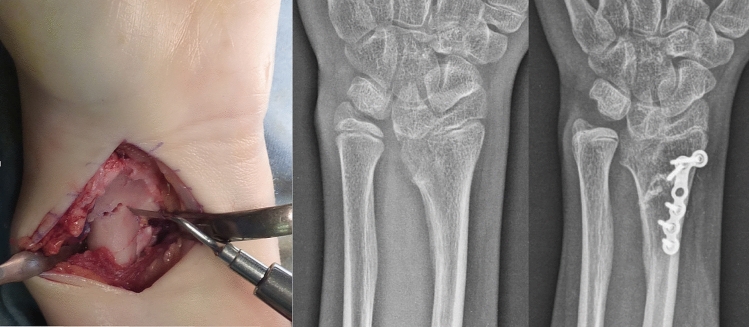
Piezosurgery® was employed in 49 corrective osteotomies in children. Sixteen children with Madelung deformity underwent to Vickers ligament release and volar palate fixation of the dome osteotomy (Fig. 1) with or without reversing bone wedge grafting [10]. In two children with acquired Pseudo-Madelung, following post-traumatic radius malunion, the Piezosurgery® was employed for both radius osteotomy and trapezoidal bone graft from the iliac crest with plate fixation in one child. In the other, the severe deformity was fixed by external fixator allowing gradual lengthening and correction of the radius (2 cm per month until useful correction and consolidation at 6 months). In all children the stable fixation of the osteotomy allowed early rehabilitation program and no plaster cast immobilization. In thirty-one children with clino-camptodactyly, the opening wedge osteotomy performed to correct angular deformity was fixed with K-wires from 5 to 6 weeks, once healing was radiographically confirmed. The digit was immobilized in a gutter orthosis until consolidation.
Fig. 1.
Intra-operative features of the Piezoelectric dome osteotomy in Madelung deformity correction. Radiographic follow-up of volar plate fixation
Distal Radius Malunion
Seventeen corrective osteotomies were performed in adult following dorsally displaced extra-articular distal radius malunion or intra-articular ones. Piezosurgery® allowed osteotomy following volar plate fixation at the epiphyseal fragment without removal of the hardware due to the small-size and handling of the device. On the same base, the technique was performed in the intra-articular corrective osteotomies of the fragments by dorsal surgical approach, because of the high level of roughness of adjacent surfaces and favorable angle and direction of the procedure.
Osteotomies and Arthrodesis at the Hand
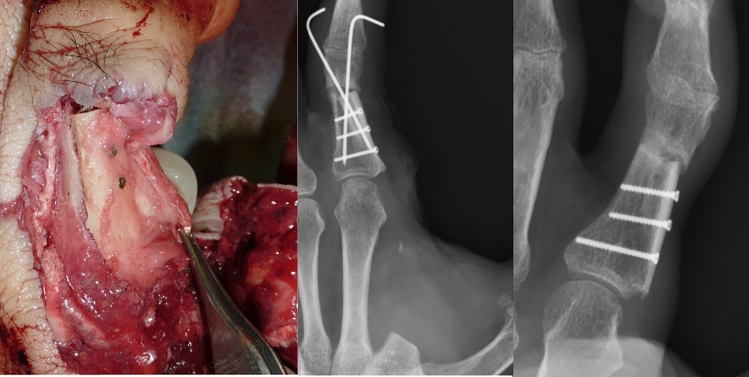
Piezosurgery® was used in eight metacarpal bones, allowing the bone fixation with dedicated plate for rotational correction before the osteotomy. At the phalangeal level, the technique was used in three multiplanar condylar osteotomies according to Teoh technique [11], and in five inter-phalangeal joints arthrodesis with endomedullary screw fixation. In the last one patient, the phalangeal osteotomy was performed in a scarred and amputated donor digit to harvest a remodeled bone graft for another survival digit reconstruction (Figs. 2 and 3).
Fig. 2.
Particular of the piezoelectric bone graft harvesting from donor amputated digit, remodeled according to the bone loss of the survival digit
Fig. 3.
Operative features of the implantation and reconstruction of the phalangeal and articular bone loss. Radiographs showed the bone union and osteointegration at the follow-up
Bone Graft
Forty-five bone grafts from iliac crest or distal radius were harvested and accurately remodeled without milling or grinding. Because of the relevant bias in retrospective analysis of scaphoid nonunion, the inclusion criteria enrolled only 35 waist fracture nonunion in presence of proximal and distal poles large enough to support the screw fixation. Cortico-cancellous or wedge bone graft from iliac or radius occurred within 12 months of acute fracture. Vascular or non-vascular bone graft were both recorded because did not appear to influence the union rate in the selected typology of patients [12].
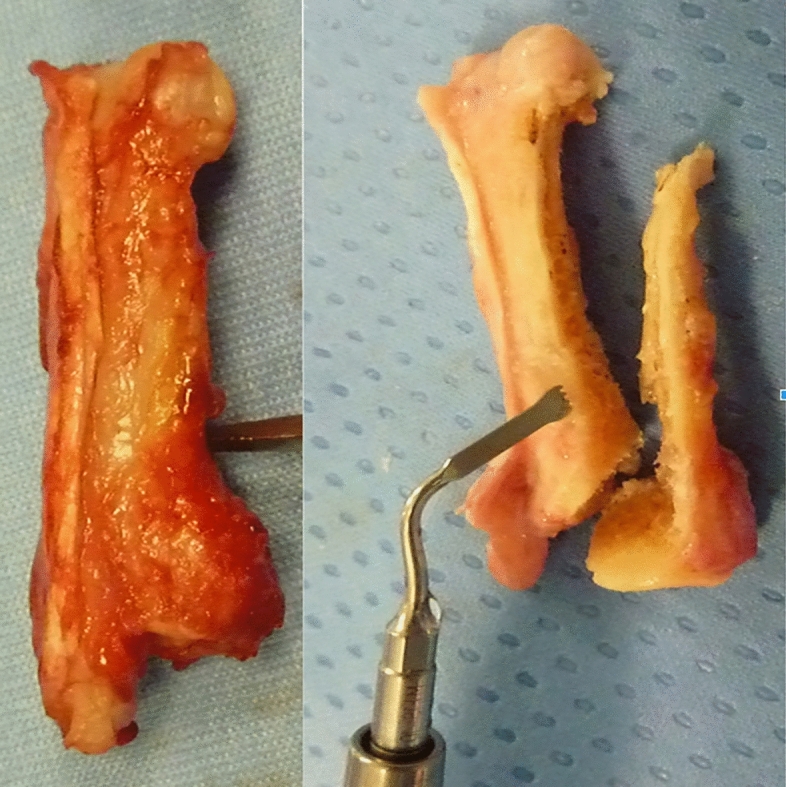
In other five patients, the scaphoid nonunion followed failure of primary screw fixation of fracture. All cases were fixed by scaphoid plate and augmented with double bone graft [13]. The bone grafts were harvested from iliac crest by Piezosurgery®. The axial bone graft was accurately and anatomically remodeled to perfect fill the cavitation of the screw removal, and the transverse one was remodeled to correct the humpback deformity and scalloped to envelope the axial graft (Fig. 4).
Fig. 4.
Intra-operative features of the double bone grafts harvested by piezosurgery. Axial bone graft to fill the cavitation following screw removal. Transverse wedge cortical bone graft to correct and fill the bone loss of the nonunion, and particular of the bone scalloping to envelope the other graft
Five chronic scapho-lunate (S-L) injuries underwent to reconstruction with bone-ligament-bone, the Piezosurgery® was used to harvest and remodel the complex from the donor site, allowing ligament sparing and a precise and well-structured bone stock, as well as a roughness inset of the complex into the scaphoid and lunate.
Reconstructive Microsurgery
Fibula flap has become fundamental in maxillary and mandibular defects. 28 fibula free flaps were harvested with Piezosurgery® and modeled either in the donor site (thanks to previous Computer-aided Design and Manufacturing) or in the new location, with safely vascular sparing in both cases [14].
All osteotomies with stable fixation had a post-operatively early rehabilitation program started at the hand and wrist with no immobilization, except for the children with K-wire fixation in phalanges or metacarpal bones.
All patients were assessed to value union-rate with radiographic post-operative examinations. Scaphoid CT was assessed in case of uncertain union by X-ray at the follow-up.
All surgical procedures were conducted with the Piezosurgery® Plus Unit and the osteotomy-standard medical handpieces (connected to the medical insert in channel 1 of the Unit). The MT1S-10 standard medical handpiece was used in grafts, phalanges and metacarpal bone osteotomies (length: 10 mm; saw width: 3 mm; saw thickness: 0.35 mm). The dome osteotomy in children was performed recurring to the quite larger MT1-10 standard medical handpiece (length: 10 mm; saw width: 4 mm; saw thickness: 0.55 mm). Only for the distal radius osteotomy in adult or the fibula, the authors used the MT1-10 or the MT4-10/20 plus handpiece (length: 10/20 mm; saw width: 4 mm; saw thickness: 0.55 mm), connected to the plus insert in channel 2 allowing more power, in presence of highly mineralized bone.
The ultrasonic tips of various handpieces vibrate at a controlled speed of 60–200 mm/s, with a linear vibration from 60 to 200 µm horizontally and from 20 to 60 μm vertically. The Piezosurgery® Unit allows seven levels of power, since to 50 W for the plus habdpieces (channel 2 connected) in higher mineralized and larger bones. The irrigation presents five levels of quantity, in linear growing relationship with the degree of power, allowing since to 60 ml/min jet in the standard insert and to 81 ml/min in the more powerful plus insert.
The osteotomy at the hand and wrist were all performed from 4 to 6 range of power (from 25 to 40 W) and at four level of irrigation. However, the Unit has an automatic feedback in power and irrigation regulation adjusting the selected level to the bone resistance.
Results
Corrective osteotomies at the metacarpal bone and phalangeal level healed in all cases, both in stable fixations in adults or K-wire fixations in children. The mean consolidation time was 31 days in children and 42 days in adults.
All radius dome osteotomies or corrective osteotomies healed with a mean consolidation time of 58 days in children and 85 days in adults (no bone grafting was used in plate fixation).
In the scaphoid nonunion, following acute fracture or prior synthesis failure, the mean consolidation time was 83 days and 87.5% of union rate was recorded (5 failure and 35 unions). In bone-ligament-bone of S-L reconstructions, the mean consolidation time was 39 days.
All fibula flaps consolidated in a mean time of 51 days.
At no point in all cohorts there were any neurovascular or tendon disturbances or adverse surgical events.
Despite the thin instruments no breakage of the handpieces were recorded respecting the correct technique.
Discussion
Piezoelectric bone surgery was introduced almost 20 years ago in dental surgery to improve outcomes and bone-implant integration [1]. According to the operative environment, the instruments were designed handy, thin and small. These characteristics, added to the relevant soft tissue sparing property, outweighed piezoelectric surgery over traditional tools and explained its escalating role in wider and wider number of surgical procedures [2–6]. Hand surgery and microsurgery have great potential and are high suitable to piezoelectric surgery [6, 8].
The authors presented an overview of the applications in corrective osteotomies in Hand and Plastic reconstructive surgery. The casuistry highlighted and analyzed the results, the certain or possible advantages and pitfalls.
During the osteotomy, precautionary measures should be taken into account to minimize the extent of temperature rise during sawing. Some author introduced the multiple drill-hole technique to reduce thermal damage, but did not avoid the bone heat [7, 8, 15]. Moreover, the final cutting with scalpel did not fulfill precise cutting or undesired breakage. The piezoelectric effect avoided any alteration in temperature and injury to bony cells, and leaded to safe incision without damaging underlying vital structures like nerve, tendons and vessels [16–21]. A simultaneous decrease of some pro inflammatory cytokines in the bone was described, allowing neo-osteogenesis [2]. Limitation in retraction and stretching of soft tissues was significantly, such as in stripping of the periosteum and in bony exposure [22].
The instrument was handled and moved into the surgical space comparable to a pen and the cut was highly precise. The absence of vibrations, the fine tip and the clear view onto the bone enabled variable courses and angles, and accurately curved cutting (in Madelung dome osteotomy) as well as custom-made graft or surface remodeling and roughness (in scaphoid and S-L reconstruction). The high precision and thin cutting was very useful in closer and meticulous osteotomies (in Teoh technique, intra-articular malunion, fibula flap, pediatric patients). The handling and downsizing of the Piezosurgery® devices allowed bone cutting without removal of the previously fixed dedicated plates (in dorsally displaced distal radius malunion, de-rotative osteotomy at the hand). Fixation of the bone before cutting reduced surgical duration, and facilitated the intra-operative maneuvers.
The issues of roughness of the bony surface and of accurate and modeled cut were relevant not only in effective and more physiological healing, but also in bone graft harvesting [15]. This was useful in scaphoid nonunion and S-L reconstruction techniques, needing small, wedge or custom-made grafts, such as axial cavity filling or saddle shaping. The accuracy of bone surfaces contact affected the stability and the course of treatment. In absence of sufficient mechanical forces between containing components of the osteotomy the healing occurred under unfavorable angle and direction [23, 24]. Stable fixation and optimal interface of the bone and graft were effective in union rate and time of healing [25, 26].
The sparing soft tissue effect such as the lack of thermal increase and vibration played a relevant role in harvesting microvascular free or pedicled bone grafts for scaphoid reconstruction or fibula free flaps. Piezosurgery® has proved to be more suitable compared to either traditional or more recent J-plasma devise [14] cutting methods, because of the safety of the procedures, giving also minimal periosteal elevation. In the vascularized bone grafts, the vessels were easily respected, with a clear view of the operative field and no local bleeding, positively affecting the microsurgical dissection and environment both in the donor and receiving sites.
Depending on the density, thickness and size of the bone, the time needed for the osteotomy was overall slightly longer than the time needed while using the usual saw, but quite similar to the multiple drill-hall technique. Contraindications have been reported in patient or operator with electrical pacemakers [2] and substantial amount of initial investment was required with the application of piezosurgery. In contrast to conventional micro saws or drilling osteotomy, the piezoelectric surgery required minimal pressure. Contact load of 150 g’s allowed the better depth cut and avoided the breakage of the thin devices. The learning curve is not demanding but it is very important a correct technique in cutting to avoid breakage of the blades and thermal damage of the bone. The handpieces should be moved continuously backward and forward with minimun pressure. Despite these limitations and disadvantages, surgical time [27, 28] and efforts were largely enhanced by the technical advantages in feasibility and flexibility of the technique as well as the pre-fixed plate opportunity.
Despite many histomorphological studies showed no signs of lesions to the mineralized tissues or suffering of the osteocytes, with increasing in neo-osteogenesis, there was a lack of evidence in better rate and earlier bone union. No studies described homogeneous cohorts, without relevant bias, comparing instruments in osteotomies. Even this study did not prove significance in bone healing outcomes, but showed a consolidated proof of feasibility for piezosurgery, ideally sized for hand and reconstructive surgery and microsurgery.
Conclusion
Piezoelectric surgery was a safe and efficient technique, providing selective micrometric bone cuts for minimally invasive procedures requiring high precision. The technical and biological characteristics of the piezoelectric effect perfected this technique as an effective and useful instrument in Hand surgery. The handy and fine device provided an opportunity for a variety of dedicated and clever osteotomies related to the biological and biomechanical aspects of the different pathologies. Soft tissue sparing was high effective in microsurgical reconstructive procedures.
Author Contributions
All authors directly contributed in the surgical and follow-up efforts.
Funding
No funding or royalties were received to assist with the preparation of this manuscript.
Availability of Data and Material
All retrospective reviewed data and material are available into the software and archives of the Institute.
Code Availability
Not applicable.
Declarations
Conflict of Interest
All the authors declare they have no financial interests, no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangement, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical Approval
The article does not contain any trial with human participants or animals performed by any of the authors. The retrospective analysis of the human data was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. No studies regarding human and/or animal rights were conducted in the study.
Informed Consent
Informed consent was obtained from all patients before surgery as well as for the collected data at the follow-up.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cicciù M, Stacchi C, Fiorillo L, Cervino G, Troiano G, Vercellotti T, Herford AS, Galindo-Moreno P, Di Lenarda R. Piezoelectric bone surgery for impacted lower third molar extraction compared with conventional rotary instruments: A systematic review, meta-analysis, and trial sequential analysis. International Journal of Oral and Maxillofacial Surgery. 2021;50(1):121–131. doi: 10.1016/j.ijom.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal E, Masamatti S, Kumar A. Escalating role of piezosurgery in dental therapeutics. J Clin Diagn Res. 2014;8(10):ZE08–ZE11. doi: 10.7860/JCDR/2014/9161.4988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlee M, Steigmann M, Bratu E, et al. Piezosurgery: Basics and possibilities. Implant Dentistry. 2006;15(4):334–340. doi: 10.1097/01.id.0000247859.86693.ef. [DOI] [PubMed] [Google Scholar]
- 4.Nalbandian S. Piezosurgery techniques in implant dentistry. Aust Dent Pract. 2011;22:116–126. [Google Scholar]
- 5.Shakouri E, Abbasi M. Investigation of cutting quality and surface roughness in abrasive water jet machining of bone. Proceedings of the Institution of Mechanical Engineers Part H. 2018;232(9):850–861. doi: 10.1177/0954411918790777. [DOI] [PubMed] [Google Scholar]
- 6.Hoigne DJ, Stubinger S, VonKaenel O, et al. Piezoelectric osteotomy in hand surgery: First experience with new technique. BMC Musculoskeletal Disorders. 2006;7:36–39. doi: 10.1186/1471-2474-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Augustin G, Zigman T, Davila S, et al. Cortical bone drilling and thermal steonecrosis. Clinical Biomechanics. 2012;27:313–325. doi: 10.1016/j.clinbiomech.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Haide T, Geisler D, Thalhammer G, et al. Multiple drill-hole osteotomy in hand surgery—description of a novel application and proof of feasibility. BMC Musculoskeletal Disorders. 2017;18:529–535. doi: 10.1186/s12891-017-1895-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marco M, Millán MR, Santiuste C, et al. A review on recent advances in numerical modelling of bone cutting. Journal of Mechanical Behaviour of Biomedical Materials. 2015;44:179–201. doi: 10.1016/j.jmbbm.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Acciaro AL, Garagnani L, Lando M, Lana D, Sartini S, Adani R. Modified dome osteotomy and anterior locking plate fixation for distal radius variant of Madelung deformity. Journal of Plastic Surgery and Hand Surgery. 2021 doi: 10.1080/2000656X.2021.1934845. [DOI] [PubMed] [Google Scholar]
- 11.Teoh LC, Yong FC, Chong KC. Condylar advancement osteotomy for correcting condylar malunion of the finger. Journal of Hand Surgery (Edinburgh, Scotland) 2002;27(1):31–35. doi: 10.1054/JHSB.2001.0694. [DOI] [PubMed] [Google Scholar]
- 12.Ammori MA, Elvey M, Mahmoud SS, et al. The outcome of bone graft surgery for nonunion of fractures of the scaphoid. Journal of Hand Surgery. 2019;44(7):676–684. doi: 10.1177/1753193419841278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leti Acciaro A, Lana D, Fagetti A, et al. Plate fixation in challenging traumatic carpal scaphoid lesions. Musculoskeletal Surgery. 2021 doi: 10.1007/s12306-020-00689-1. [DOI] [PubMed] [Google Scholar]
- 14.De Santis G, Pinelli M, Starnoni M. Extended and unusual indications in jaw reconstruction with the fibula flap: An overview based on our 30-year experience. Annals of Medicine and Surgery. 2021;62:37–42. doi: 10.1016/j.amsu.2020.12.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson SR, James DF. Drilling in bone: Modeling heat generation and temperature distribution. Journal of Biomechanical Engineering. 2003;125(3):305–314. doi: 10.1115/1.1535190. [DOI] [PubMed] [Google Scholar]
- 16.Starnoni M, Colzani G, De Santis G, et al. Median nerve injury caused by screw malpositioning in percutaneous scaphoid fracture fixation. Plastic and Reconstructive Surgery. Global Open. 2019;7(6):e2292. doi: 10.1097/GOX.0000000000002292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leti Acciaro A, Pilla F, Faldini C, et al. The carpal tunnel syndrome in children. Muskoloskeletal Surgery. 2018;102(3):261–265. doi: 10.1007/s12306-017-0527-3. [DOI] [PubMed] [Google Scholar]
- 18.Leti Acciaro A, Lando M, Russomando A, et al. A mini-invasive tenolysis of the flexor tendons following hand fractures: Case series. Musculoskeletal Surgery. 2018;102(1):41–45. doi: 10.1007/s12306-017-0493-9. [DOI] [PubMed] [Google Scholar]
- 19.Leti Acciaro A, Pilla F, Colzani G, et al. A new sign allowing diagnosis in the pathologies of the extensor tendons of the hand. Injury. 2018;49(6):119–1125. doi: 10.1016/j.injury.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 20.Starnoni M, Colzani G, De Santis G, et al. Management of locked volar radio-ulnar joint dislocation. Plastic and Reconstructive Surgery. Global Open. 2019;7(10):e2480. doi: 10.1097/GOX.0000000000002480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Acciaro AL, Colzani G, Starnoni M, et al. The challenges in restoration of extensor tendns function at the hand. Acta Biomedica. 2021;92(S1):e2021151. doi: 10.23750/abm.v92iS1.9756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoigne D, Hug U, Von Wartburg U. Piezoelectric osteotomy in hand surgery: The autologous osteocartilage transplantation for joint. Handchirurgie, Mikrochirurgie, Plastische Chirurgie. 2011;43(5):319–320. doi: 10.1055/s-0031-1285885. [DOI] [PubMed] [Google Scholar]
- 23.Ichihara S, Vaiss L, Acciaro AL, et al. External bone remodeling after injectable calcium-phosphate cement in benign bone tumor: Two case in the hand. Orthopaedics and Traumatology, Surgery and Research. 2015;101(8):983–986. doi: 10.1016/j.otsr.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 24.Landi A, Cavazza S, Caserta G, et al. The upper limb in cerebral palsy: Surgical management of shoulder and elbow deformities. Hand Clinics. 2003;19(4):631–648. doi: 10.1016/s0749-0712(03)00062-3. [DOI] [PubMed] [Google Scholar]
- 25.Claire S, Lea SC, Walmsley AD. Characterization of bone following ultrasonic cutting. Clinical Oral Investigations. 2013;17(3):905–912. doi: 10.1007/s00784-012-0754-9. [DOI] [PubMed] [Google Scholar]
- 26.Vercellotti T, Nevins ML, Kim DM, Nevins M, Wada K, Schenk RK, Fiorellini JP. Osseous response following resective therapy with piezosurgery. The International Journal of Periodontics and Restorative Dentistry. 2005;25(6):543–549. [PubMed] [Google Scholar]
- 27.Battiston B, Leti Acciaro A, De Leo A. The role of the FESSH Hand Trauma Committee in Europe. Handchirurgie, Mikrochirurgie, Plastische Chirurgie. 2013;45(6):326–331. doi: 10.1055/s-0033-1361100. [DOI] [PubMed] [Google Scholar]
- 28.Leti Acciaro A, Montanari S, Venturelli M, et al. Retrospective study in clinical governance and financing system impacts of the COVID-19 pandemic in the hand surgery and microsurgery HUB center. Musculoskeletal Surgery. 2021 doi: 10.1007/s12306-021-00700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All retrospective reviewed data and material are available into the software and archives of the Institute.
Not applicable.