Abstract
Introduction
Flexible flat foot is one of the most common foot conditions found amongst any age group across the world. One very important reason for this condition is the incongruency or partial dislocation of one or more joints within the talo-tarsal mechanism. This flexible talo-tarsal malalignment is termed as recurrent talo-tarsal joint dislocation (RTTJD).
Materials and Methods
Between 2016 and 2018, 32 patients were advised Extra osseous talo-tarsal stabilization (EOTTS) as a standalone procedure for RTTJD following detailed clinical examination including foot posture index (FPI) scoring and weight-bearing radiographic evaluation. Subjective assessment was done through Maryland Foot Score (MFS) questionnaire. Radiological parameters like talar declination angle, talar second metatarsal angle and tibio-calcaneal valgus angle were assessed for preoperative and postoperative comparison. 15 patients (20 feet) underwent surgery and rest 17 patients (25 feet) became our control group. A retrospective record analysis of longitudinal data was done over a period of 4 years. The purpose of this study is to depict the short-term results of EOTTS procedure in terms of functional and radiological improvement and compare it with the non-surgical group.
Result
Significant improvement was seen in MFS from 67.31 ± 16.04 to 95.47 ± 4.36 over a mean follow-up period of 30.66 ± 7.09 months. Total FPI improved by 96.83 ± 4.80% at final follow-up of EOTTS group. Radiologically, maximum correction achieved was in coronal plane (93.07 ± 30.05%).
Conclusion
EOTTS, as a standalone procedure improved the foot radiological angles and restored the normal foot biomechanics significantly in presence of competent spring ligament and posterior tibial tendon. This procedure resulted in excellent patient satisfaction score as assessed by MFS questionnaire.
Level of Evidence
III.
Keywords: Extra osseous talo-tarsal joint stabilization (EOTTS), Flat foot, Recurrent talotarsal joint dislocation (RTTJD), Arthroereisis, Minimally invasive surgery
Introduction
Flat foot is one of the most common foot conditions found amongst any age group across the world. In India, the medical fraternity, especially the orthopedic surgeons have travelled a long way in understanding the ever-evolving foot and ankle concepts. The indications for which the treatment is sought for a flat foot are also different as compared to the west. It could be for a cosmetic reason, especially for a girl’s marriage, pain in foot or for recruitment in armed forces. Sports is still on the last priority for which treatment is sought. People don’t seek treatment for a deformed foot if it does not give any trouble. Also, any pain in proximal musculoskeletal chain is least thought to be because of a hyper-pronated foot.
Majority of rural Indians wear slippers (Chappal) and their compliance with orthotics is very poor. Surgery for flat foot is despised by majority of patients. Cost of surgery has to be borne by the patients in majority of cases. Postoperative surgical rehabilitation puts them out of their work place. Many physicians advise against surgical intervention as they feel that flat foot cannot be stitched back.
While introducing Extra Osseous Talo-tarsal Stabilization (EOTTS) in India, the author faced loads of resistance which drove him to do this study. Unacceptability by patients to a new technique, strong belief of physicians in conservative means without any strong evidence and inadequate knowledge about flat foot prevailing in society were some of them.
One important reason for flexible flat foot is the incongruency or partial dislocation of one or more joints within the talo-tarsal mechanism. The talo-tarsal mechanism is composed of talonavicular and middle, anterior, and posterior talocalcaneal joint (Fig. 1). This dislocation or subluxation may exist as recurrent/dynamic/reducible or rigid/static/nonreducible condition. The flexible talo-tarsal malalignment is termed as Recurrent talo-tarsal joint dislocation (RTTJD) [1].
Fig. 1.
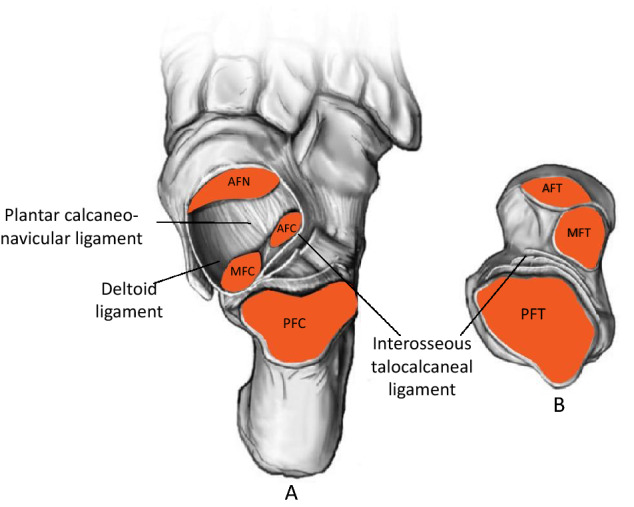
Talo-tarsal mechanism of foot. (A) Dorsal view of hindfoot (after removing talus) with plantar calcaneonavicular ligament, deltoid ligament & Interosseous talocalcaneal ligament and (B) Inferior view of Talus. AFN Articular facet of navicular, MFC Medial facet of calcaneum, AFC Anterior facet of calcaneum, PFC Posterior facet of calcaneum, AFT Anterior facet of talus, MFT Medial facet of talus, PFT Posterior facet of talus
RTTJD leads to anteromedial displacement of talus on calcaneus with extensive force acting anteromedially rather than postero-laterally (Fig. 2A). The gold standard for the diagnosis of RTTJD is weight bearing radiographic evaluation.
Fig. 2.

(A) Anteromedial displacement of talus on calcaneus, (B) EOTTS shifts force from anteromedial to posterolateral by 24%
The factor that differentiates normal from abnormal talo-tarsal alignment is overlap of the articular facets. This flexible entity of malalignment has a greater potential to contribute to secondary abnormalities than a rigid deformity [2].
The incongruent talo-tarsal deformity leads to a pathologic chain reaction in the entire foot structure distally, and also proximally, up the musculoskeletal chain and therefore a patient with RTTJD can present with a spectrum of picture ranging from low back ache, knee pain, shin splint, arch pain, bunion, plantar fasciitis, tarsal tunnel syndrome, gait abnormalities and can eventually complicate to medial column overloading stress injuries and hindfoot and midfoot arthritis [3].
Interestingly, not all patients with RTTJD will have a fallen arch. Some may have excessive heel valgus while others may have gross forefoot abduction. The root of the problem is a hypermobile talus and not a fallen arch.
Whatever be the pathology for a misaligned foot, the least invasive intervention must be chosen to decrease pain and improve function. The procedure should have least effect on other joints of foot [4].
The technique of subtalar intervention has taken more than half a century to reach the present stage in treating flat foot. Grice did an extra articular subtalar arthrodesis using cortical strut graft for pediatric pes planus [5]. Haraldsson inserted allograft cortical bone wedges in the sinus tarsi to restrict subtalar eversion without arthrodesis [6]. First subtalar arthroereisis with a free floating implant was described by Subotnick [7]. Sinus tarsi implants are now made of silicone, polyethylene, titanium, stainless steel, or bioresorbable polymers.
In the present times, there are many sinus tarsi devices in the market. Understanding their types gives us a broader outlook of their functioning mechanism, their advantages and drawbacks. Sinus tarsi devices can be classified into 2 major types, type I and type II (Fig. 3) [8].
Fig. 3.
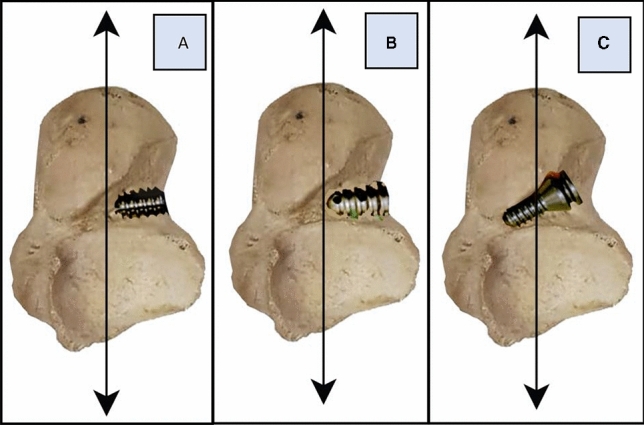
(A) Type IA device, (B) Type IB device, (C) Type II device
Type I devices are further subclassified into type IA (cylindrical) and type IB (conical) (Fig. 3).
Type I device functions by impingement of lateral process of talus to block the talar motion (Talar door stop) having a reported removal rate as high as 40%. The mechanism by which type I device functions is called arthroereisis [9, 10].
Type II device is known as HyProCure (Macomb, MI, USA) and is made of titanium. It is designed to have a lateral-conical and medial- cylindrical geometry, is inserted into the tarsal sinus in a posterior-medial-superior direction. The device is stabilized medially by anchorage from soft tissues within the canalis portion of the tarsal sinus, and laterally by tapered portion of the device that abuts against the entrance to prevent over insertion.
The anterior leading edge of this device goes medially beyond the longitudinal talar bisection line, stabilizes the talus and restore the normal axis point of subatalar joint. It functions by allowing the normal helicoidal motion of the talus within the tarsal mechanism. Reported removal rate is 4–6% [8]. The mechanism by which type II device works is called extra osseous talo-tarsal stabilization (EOTTS).
The type II device is designed to provide the closest anatomical fit with the sinus and canalis portions of the tarsal sinus, thus provides greater distribution of forces and gives better results [11]. Type II device is superior in design and function as compared to type I device. It remarkably stabilizes the complicated tri-planar talo-tarsal motion at the “cruciate pivot point”. Cruciate pivot point is located at the entrance of the canalis portion of the tarsal sinus along the longitudinal talar bisection line. It is the origin of a rectangular coordinate system along the axes of which (Fig. 4) the helicoidal motion of the talus during pronation and supination occurs and is the ideal location where the excessive anterior-medial-plantar displacement of the talus within the tarsal mechanism should be eliminated or minimized. The threaded cylindrical portion offers no resistance to talar motion. It doesn’t bear any weight because it obtains an interference grip in the anteroposterior direction and not in the supero-inferior line of axial body weight [12]. The oblique alignment of type II device further contributes to its long-term survivability. Unlike the type I laterally anchored devices that function as a talar door stop, the type II device functions like a stent placed within an artery to keep it open.
Fig. 4.
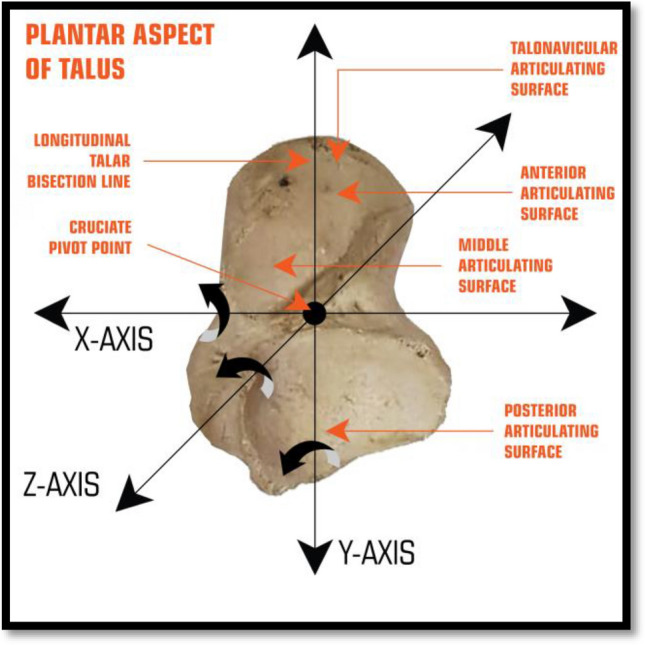
Cruciate pivot point
EOTTS prevents shifting of posterior facet force to anterior and medial facet by approximately 24% (Fig. 2B) and thus patients with medial column pain benefit significantly [1]. Literature has enough evidence that EOTTS has positive effect on plantar faciopathy [13], tarsal tunnel syndrome [14], abnormal plantar pressures [15], stretched spring ligament [16], forefoot deformities [17] and on knee [18, 19] and lower back pain [20, 21] arising from hyper-pronated foot.
In the present study, EOTTS was done as a standalone procedure using type II device on 15 patients (20 feet) suffering with RTTJD. The purpose of this study is to depict the short- term result of EOTTS procedure in terms of functional and radiological improvement and compare it with the functional outcome of those who did not undergo any surgical intervention. Also, to formulate a road map so that the surgery is done on a patient only when appropriately indicated and not otherwise.
Patients and Methods
Between 2016 and 2018, 181 flat foot patients were seen in the Outpatient department of our tertiary care center for foot and ankle. All these patients presented with one or more of the following symptoms: foot pain, easy fatigability while walking and running, early eccentric wearing of shoes, obvious looking deformed foot and shin pain.
All the patients underwent a detailed clinical and radiological evaluation by a single foot and ankle orthopedic surgeon. 58 patients were diagnosed with RTTJD. 26 patients were advised EOTTS along with other bony or soft tissue procedures and 32 patients were advised EOTTS as a standalone procedure. Out of these 32 patients, 15 patients (20 feet) underwent surgery and rest 17 patients (25 feet) didn’t opt for any surgical intervention. These 17 patients became our control group. Demographic comparison of both the groups is given in Table1.
Table 1.
Comparison of Sociodemographic parameters between Non operative (control) and EOTTS group
| Parameters | Categories | Non operative | EOTTS | P value |
|---|---|---|---|---|
| Age (years) | Mean (SD) | 25.52 (10.26) | 24.26 (5.96) | 0.63 |
| Gender | Male (%) | 56 | 63.16 | 0.63 |
| Female (%) | 44 | 36.84 | ||
| Occupation | Athlete (%) | 0 | 10.53 | 0.23 |
| Businessman (%) | 12 | 0 | ||
| Clerk (%) | 8 | 0 | ||
| House wife (%) | 12 | 21.05 | ||
| IT professional (%) | 20 | 15.79 | ||
| Job (%) | 4 | 0 | ||
| Lawyer (%) | 0 | 5.26 | ||
| Shop owner (%) | 0 | 5.26 | ||
| Student (%) | 44 | 42.11 | ||
| Side | Left (%) | 48 | 42.11 | 0.70 |
| Right (%) | 52 | 57.89 | ||
| Follow up (months) | Mean (SD) | 35.23(7.32) | 31.10 (6.85) | 0.09 |
SD Standard deviation, IT Information Technology
Clinical assessment included detailed foot and ankle examination and Foot posture index (FPI) scoring [22]. Standardized anteroposterior (AP), lateral and long axial [23] radiographs of foot and AP radiograph of ankle were taken preoperatively and postoperatively in bilateral resting stance position (Fig. 6). Parameters like talar declination angle (sagittal plane), talar second metatarsal angle (axial plane) and tibio-calcaneal valgus angle (coronal plane) were considered for preoperative and postoperative comparison. Normal values of the above angle measurements is given in Table 2 [24–26]
Fig. 6.
Weight bearing preoperative & postoperative views. (A,B) Pre & postoperative Talocalcaneal valgus angle 26 deg and 1.2 deg. (C,D) Pre & postoperative Talo-second metatarsal angle 35 deg and 12 deg. (E,F) Pre & postoperative Talar declination angle 34.5 and 23 deg. Significant correction is noted in radiological angles in all the plane
Table 2.
Comparison of Clinico-radiological parameters in EOTTS group
| Paired t test | Normal range | Before (mean) | SD | After (mean) | SD | P value |
|---|---|---|---|---|---|---|
| MFS | # | 67.32 | 16.05 | 95.47 | 4.36 | < 0.001 |
| FPI Rearfoot | * | 4.53 | 0.70 | 0.16 | 0.37 | < 0.001 |
| FPI forefoot | * | 4.58 | 0.77 | 0.16 | 0.37 | < 0.001 |
| FPI total | 0–5 | 9.12 | 1.1 | 0.32 | 0.48 | < 0.001 |
| TDA | 21 | 28.21 | 4.00 | 18.11 | 2.10 | < 0.001 |
| T2MA | 16.2 ± 7.3 | 28.89 | 4.91 | 13.32 | 4.81 | < 0.001 |
| TCVA | 0–5 | 10.95 | 3.92 | 1.42 | 2.32 | < 0.001 |
#A normal range for MFS score cannot be ascertained. However, increased score indicate decreased abnormality
*A normal range for forefoot and rearfoot FPI cannot be ascertained individually in pronation. However. increased score indicate increased abnormality
MFS Maryland foot score, FPI Foot Posture Index, TDA Talar declination Angle, T2MA Angle between axis of talus and axis of 2nd metatarsal on Axial plane, TCVA Tibio calcaneal valgus angle
Postoperative assessment was done at 3 months and at final follow-up. The patients were also asked to complete the MFS Questionnaire. Initial (before the start of treatment) and final MFS scores were assessed and compared for both groups (Tables 3 and 4). The final MFS scoring for non- operative group was done through telephone and text messages.
Table 3.
Comparison of MFS Parameters in EOTTS group
| MFS parameters | Before (mean) | SD | After (mean) | SD | P value |
|---|---|---|---|---|---|
| Pain | 30.79 | 10.31 | 43.42 | 2.39 | < 0.001 |
| Distance walked | 6.37 | 2.56 | 9.47 | 0.90 | < 0.001 |
| Stability | 3.26 | 0.93 | 3.79 | 0.42 | 0.004 |
| Support | 3.63 | 0.50 | 4.00 | 0.50 | 0.005 |
| Limp | 3.11 | 0.81 | 4.00 | 0.81 | < 0.001 |
| Shoes | 4.84 | 1.46 | 8.95 | 1.13 | < 0.001 |
| Stairs | 2.58 | 1.17 | 3.58 | 0.84 | < 0.001 |
| Terrain | 2.84 | 1.01 | 4.00 | 1.01 | < 0.001 |
| Looks | 5.53 | 2.70 | 9.37 | 0.96 | < 0.001 |
| Motion | 4.37 | 0.96 | 4.89 | 0.32 | 0.014 |
| Total | 67.32 | 16.05 | 95.47 | 4.36 | < 0.001 |
MFS Maryland foot score, SD Standard deviation
Table 4.
Comparison of MFS Parameters in Non operative (control) group
| MFS parameters | Before (mean) | SD | After (mean) | SD | P value |
|---|---|---|---|---|---|
| Pain | 34.6 | 4.31 | 32.6 | 3.85 | 0.005 |
| Distance walked | 6.8 | 2.12 | 4.84 | 3.17 | < 0.001 |
| Stability | 3.08 | 0.70 | 2.48 | 1.33 | 0.005 |
| Support | 3.96 | 0.2 | 3.4 | 1.12 | 0.013 |
| Limp | 3.84 | 0.37 | 3.6 | 0.65 | 0.011 |
| Shoes | 7.64 | 2.89 | 6.12 | 3.38 | 0.015 |
| Stairs | 3.44 | 0.51 | 3.2 | 0.58 | 0.011 |
| Terrain | 2.32 | 0.75 | 2.16 | 0.55 | 0.327 |
| Looks | 6.8 | 1 | 6.48 | 0.87 | 0.043 |
| Motion | 3.68 | 1.46 | 3.48 | 1.39 | 0.364 |
| Total | 76.16 | 9.66 | 68.36 | 9.65 | < 0.001 |
MFS Maryland Foot Score, SD Standard deviation
A written informed consent was taken from the patients willing for surgery and from both the groups using their clinico-radiological data for the study. Ethical committee approval was taken for the study.
In the surgical group, only those patients were involved in whom EOTTS was done as an isolated procedure. In case of patients with bilateral foot involvement, second foot was operated at least 21 days after the 1st surgery.
Clinical inclusion criteria for surgery were:
Age > 10 years.
At least one visible deformity: arch collapse, heel valgus and forefoot abduction.
Flexible flat feet (Patient was able to recreate the arch)
Absence of equinus deformity. (At least 10 degrees of ankle dorsiflexion could be achieved)
Absence of posterior tibial tendon insufficiency.
No instability along the 1st ray
Radiological inclusion criteria were:
Talar-2nd metatarsal angle on DP view: 16–35 degrees
Talar declination angle < 36 degrees.
Clinical exclusion criteria were:
Active infection overlying sinus tarsi of the involved foot.
Body mass index > 35
Any neuromuscular imbalance in lower limb.
Previous surgery done on foot for pes planus
Incompetent spring ligament as per neutral lateral heel push test [27].
Radiological exclusion criteria were:
Tarsal coalition
Degenerative changes of ankle and foot joints.
Talar-2nd metatarsal angle on DP view > 35 degrees
Metatarsus adductus
Talar declination angle > 35 degrees
Distal tibial epiphyseal abnormality in pediatric patients.
Intervention
The patient was placed supine on the operating table. For pediatric patients, general anesthesia was used and for adult patients ankle block worked fine. An approximately 1.5 cm linear skin incision was made perpendicular to the axis of foot over the soft spot of sinus tarsi. Using curved tenotomy scissors, the soft tissues (Talocalcaneal interosseous ligament) within the sinus and canalis portions of the sinus tarsi were transected to create pathway for guide wire and trial sizers insertion. This step was the most vital for proper placement of the actual implant. The guide wire was directed lateral to medial, anterior to posterior (towards medial malleolus) and inferior to superior into the sinus tarsi. Trial sizing was performed to determine the appropriate stent (implant for EOTTS) size to achieve the best correction. First trial sizer to be inserted was no. 5 which could be subsequently increased to no. 6 and so on to maximum no. 10 size till satisfactory correction was achieved. The goal was to restore the talo-tarsal motion to 3–5 degree of pronation. Once the proper size was determined, the corresponding stent was inserted. Guide wire was removed and incision was closed with absorbable subcuticular suture followed by application of a sterile and dry compression dressing.
Postoperative Course
The patients were instructed non-weight bearing for 2–3 days post-surgery. Cryotherapy was given for 3–4 times a day till inflammation persisted. At 3rd–4th postoperative day, partial to full weight bearing was allowed as per tolerance. By the end of first week, peronei strengthening, range of motion at ankle and subtalar joint and calf stretching exercises were started. The patients were allowed to gradually increase activity as tolerated after first postoperative week. Patients were encouraged to use new sports shoes as soon as tolerated, making sure that the outer collar did not rub against the incision site [28].
Statistical Analysis
This study is a retrospective record analysis of longitudinal data of two groups. Statistical significance was evaluated between preoperative and final postoperative MFS scores, between initial and final follow-up MFS score of control (non-surgical) group and between the final MFS scores of both operative and control group. Statistical significance was also calculated between relevant clinical and radiological parameters before surgery and at final postoperative follow-up. A paired student’s t test was applied when comparing data within the same group while single t test was applied when two groups were being compared.
Results
There was a significant improvement in MFS at final follow-up of EOTTS group patients (Table 3) in comparison to non-operative group (Table 4). MFS improved from 67.31 ± 16.04 to 95.47 ± 4.36 over a mean follow-up period of 30.66 ± 7.09 months. Pain, shoe wear and looks improved maximally. Rear foot and forefoot FPI improved by 97.01 ± 7.10% and total FPI improved by 96.83 ± 4.80% at final follow-up of EOTTS group (Fig. 5, Table 2). Radiological parameters like talar declination angle, talocalcaneal valgus angle and talar-second metatarsal angle improved significantly (Fig. 6, Table 2). Maximum correction achieved was in coronal plane (93.07 ± 30.05%) followed by axial plane (54.84 ± 16.08%) followed by sagittal plane (34.99 ± 9.1%). This suggests that EOTTS has a definite positive impact in functional and clinico-radiological outcome of patients suffering from RTTJD. The patient satisfaction scores showed excellent short-term results with overall good tolerance to the implant and improved quality of life.
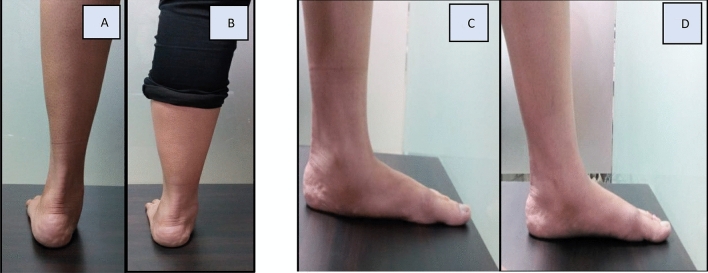
Fig. 5.
Preoperative and postoperative clinical picture. (A,B) Pre & postoperative improvement in heel valgus, (C,D) Pre & postoperative improvement in medial longitudinal arch
Complication rate was 4% with one deep infection leading to permanent implant removal.
One patient had device displacement within 2 months of surgery. Following a revision surgery which essentially involved more thorough cut of talocalcaneal interosseous ligament and replacement of same device, patient did well at final follow-up. It was interesting to observe that while the device was partially displaced, the corrected radiological angles were still maintained.
Short term self-resolving complications like abnormal gait, sprain like feeling over lateral aspect of ankle and appearance of overcorrection disappeared once swelling, pain and inflammation were resolved.
In the non-surgical group, MFS had fallen from 76.16 to 68.36 over a mean follow-up of 35.23 ± 7.32 months. All parameters deteriorated significantly except looks, terrain and motion. This study clearly demonstrated that non-surgical treatment is not effective and leads to deterioration of function with poor outcomes.
Discussion
In recent times, many studies have been published on subtalar minimally invasive intervention for correction of mis-aligned foot.
Vedantam et al. gave satisfactory results in 96% of feet in a study of 78 children who had flexible flatfoot caused by neuromuscular disorders, in whom 140 arthroereisis procedures were performed [29]. Giannini and colleagues reported the 4-year results of subtalar arthroereisis for 21 children who had bilateral flexible flatfoot deformity using a bioresorbable implant. In selected cases, Achilles tendon lengthening and Kidner procedure were added [30]. Needleman did subtalar arthroereisis along with other surgical corrections of flexible flat foot deformity with average follow-up of 44 months. Significant improvements were found in radiographic parameters with high patient satisfaction despite the removal of 11 of 28 implants for sinus tarsi pain [31].
A retrospective study by Graham et al. [28] showed positive outcomes of EOTTS in 83 patients with less than 6% incidence of implant removal and few postoperative complications. Bresnahan [32], in his study concluded that EOTTS using type II subtalar device effectively stabilized the talo-tarsal mechanism and reduced the symptoms associated with talo-tarsal instability.
The intent of the implant is to stay in situ as long as possible. The implant has been used in USA since 2004, and since that time there has been no published reports of ill-effects to the talus or calcaneus. The implant is absolutely extra-articular and is not known to cause arthritis to subtalar joint. So far, the published reports only discuss removal due to persistent pain and upon removal of the implant the pain has resolved.
The present study is the first to report subjective as well as objective short- term outcome on the use of type II subtalar device from Asia for treatment of talo-tarsal joint instability and its associated pathologies. We conclude that appropriate patient selection is the key to success of EOTTS as a stand-alone procedure in mild to moderate cases. For severe cases, adjunctive bony and soft tissue procedures can be added. The inclusion criteria were deliberately kept narrow to asses improvement with isolated EOTTS and offer early rehabilitation to the patients.
There have been other modalities for treating flat foot. Soft tissue and bony procedures result in extensive surgical dissection, big & cosmetically challenging scars, long recovery periods with plasters and non- weight bearing instruction and sometimes inadvertent damage to adjacent joints. The compliance with custom made orthotic supports, braces and shoe inserts is very poor in this part of the world. Also, there is no proven clinical evidence that externally applied foot orthotics realigns the osseous structure and restore the normal biomechanics of foot. With EOTTS, all the above problems are bypassed & the most important advantage is its reversibility. In case of any complication, it can be easily removed without any further loss.
However, EOTTS has its own limitations and cost of implant is the most important one. Most insurance company did not cover the treatment for congenital flat foot. The training and understanding required to do EOTTS was not available in India for many years.
The limitation of the present study is that it has a short-term follow-up with limited number of patients. Our inclusion criteria are narrow. MFS scoring of conservative group and few surgical patients at the end of study were done on phone or using text messages.
Conclusion
EOTTS, as a standalone procedure using type II device resulted in excellent results in presence of competent spring ligament and posterior tibial tendon. The procedure improved the foot radiological angles and was able to restore the normal foot biomechanics significantly. The present study opens a gateway for further research into EOTTS wherein long-term study can be done with broader inclusion criteria and added procedures on a larger group of patients.
Author contributions
AJ: Study design, performed measurements, manuscript preparation. GG: Study design, performed measurements, manuscript preparation. AG: Statistical analysis, manuscript preparation.
Declarations
Conflict of interest
The author declares that they have no competeing interest.
Ethical approval
Ethical committee approval was taken for the study.
Informed consent
A written informed consent was taken from the patients willing for surgery and from both the groups using their clinicoradiological data for the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abhishek Jain, Email: drabhishek@delhifoot.in.
Gaurav Gupta, Email: gauravgupta5038@gmail.com.
Anant Gupta, Email: anant933@gmail.com.
References
- 1.Graham ME, Parikh R, Goel V, Mhatre D, Matyas A. Stabilization of joint forces of the subtalar complex via hyprocure sinus tarsi stent. Journal of the American Podiatric Medical Association. 2011;101(5):390–399. doi: 10.7547/1010390. [DOI] [PubMed] [Google Scholar]
- 2.Graham ME. Congenital talotarsal joint displacement and pes planovalgus evaluation, conservative management, and surgical management. Clinics in Podiatric Medicine and Surgery. 2013;30(4):567–581. doi: 10.1016/j.cpm.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Graham ME. Extra-osseous talotarsal joint stabilization (EOTTS) in the treatment of hyperpronation syndromes. Update in Management of Foot and Ankle. 2018;2:2. [Google Scholar]
- 4.Myerson MS. Instructional course lectures, the American academy of orthopaedic surgeons—adult acquired flatfoot deformity. treatment of dysfunction of the posterior tibial tendon*†. Journal of Bone and Joint Surgery. 1996;78(5):780–792. doi: 10.2106/00004623-199605000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Grice. An extra-articular arthrodesis of the subastragalar joint for correction of paralytic flat feet in children—PubMed. Journal of Bone and Joint Surgery [Internet]. 1952 [cited 2020 Jun 13];927–40. Available from: https://pubmed.ncbi.nlm.nih.gov/12990633/ [PubMed]
- 6.Haraldsson S. Operative treatment of pes planovalgus staticus juvenilis: Preliminary communication. Acta Orthopaedica. 1962;32(1–4):492–498. doi: 10.3109/17453676208989613. [DOI] [PubMed] [Google Scholar]
- 7.Subotnick SI. The subtalar joint lateral extra-articular arthroereisis: A preliminary report. Journal of the American Podiatric Medical Association. 1974;64(9):701–711. doi: 10.7547/87507315-64-9-701. [DOI] [PubMed] [Google Scholar]
- 8.Graham ME, Jawrani NT. Extraosseous talotarsal stabilization devices: A new classification system. Journal of Foot and Ankle Surgery. 2012;51(5):613–619. doi: 10.1053/j.jfas.2012.05.030. [DOI] [PubMed] [Google Scholar]
- 9.Clinical, C., Vogt, B., Toporowski, G., Gosheger, G., Rölfing, J.D., Rosenbaum, D. et al. 2021. Subtalar arthroereisis for flexible flatfoot in. [DOI] [PMC free article] [PubMed]
- 10.Bernasconi A, Lintz F, Sadile F. The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Reviews. 2017;2(11):438–446. doi: 10.1302/2058-5241.2.170009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schon LC. Subtalar arthroereisis: A new exploration of an old concept. Foot and Ankle Clinics. 2007;12(2):329–339. doi: 10.1016/j.fcl.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Bali N, Theivendran K, Prem H. Computed tomography review of tarsal canal anatomy with reference to the fitting of sinus tarsi implants in the tarsal canal. Journal of Foot and Ankle Surgery. 2013;52(6):714–716. doi: 10.1053/j.jfas.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Graham ME, Jawrani NT, Goel VK. Evaluating plantar fascia strain in hyperpronating cadaveric feet following an extra-osseous talotarsal stabilization procedure. Journal of Foot and Ankle Surgery. 2011;50(6):682–686. doi: 10.1053/j.jfas.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Graham ME, Jawrani NT, Goel VK. The effect of HyProCure® sinus tarsi stent on tarsal tunnel compartment pressures in hyperpronating feet. Journal of Foot and Ankle Surgery. 2011;50(1):44–49. doi: 10.1053/j.jfas.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald RH, Vedpathak A. Plantar pressure distribution in a hyperpronated foot before and after intervention with an extraosseous talotarsal stabilization device-a retrospective study. Journal of Foot and Ankle Surgery. 2013;52(4):432–443. doi: 10.1053/j.jfas.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Williams BR, Ellis SJ, Deyer TW, Pavlov H, Deland JT. Reconstruction of the spring ligament using a peroneus longus autograft tendon transfer. Foot and Ankle International. 2010;31(7):567–577. doi: 10.3113/FAI.2010.0567. [DOI] [PubMed] [Google Scholar]
- 17.Eustace S, Byrne JO, Beausang O, Codd M, Stack J, Stephens MM. Hallux valgus, first metatarsal pronation and collapse of the medial longitudinal arch - a radiological correlation. Skeletal Radiology. 1994;23(3):191–194. doi: 10.1007/BF00197458. [DOI] [PubMed] [Google Scholar]
- 18.Levinger P, Menz HB, Fotoohabadi MR, Feller JA, Bartlett JR, Bergman NR. Foot posture in people with medial compartment knee osteoarthritis. Journal of Foot and Ankle Research. 2010;3:1. doi: 10.1186/1757-1146-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kolodziej L, Summers RK, Graham ME. The effect of extra-osseous talotarsal stabilization (EOTTS) to reduce medial knee compartment forces—An in vivo study. PLoS ONE. 2019;14(12):1–10. doi: 10.1371/journal.pone.0224694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen AD, Shultz SJ. Identifying relationships among lower extremity alignment characteristics. Journal of Athletic Training. 2009;44(5):511–518. doi: 10.4085/1062-6050-44.5.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khamis S, Yizhar Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait & Posture. 2007;25(1):127–134. doi: 10.1016/j.gaitpost.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clinical Biomechanics. 2006;21(1):89–98. doi: 10.1016/j.clinbiomech.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Reilingh ML, Beimers L, Tuijthof GJM, Stufkens SAS, Maas M, Van Dijk CN. Measuring hindfoot alignment radiographically: The long axial view is more reliable than the hindfoot alignment view. Skeletal Radiology. 2010;39(11):1103–1108. doi: 10.1007/s00256-009-0857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gentili A, Masih S, Yao L, Seeger LL. Pictorial review: Foot axes and angles. British Journal of Radiology. 1996;69(826):968–974. doi: 10.1259/0007-1285-69-826-968. [DOI] [PubMed] [Google Scholar]
- 25.Buck FM, Hoffmann A, Mamisch-Saupe N, Espinosa N, Resnick D, Hodler J. Hindfoot alignment measurements: Rotation-stability of measurement techniques on hindfoot alignment view and long axial view radiographs. American Journal of Roentgenology. 2011;197(3):578–582. doi: 10.2214/AJR.10.5728. [DOI] [PubMed] [Google Scholar]
- 26.Thomas JL, Kunkel MW, Lopez R, Sparks D. Radiographic values of the adult foot in a standardized population. Journal of Foot and Ankle Surgery. 2006;45(1):3–12. doi: 10.1053/j.jfas.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 27.Pasapula C, Devany A, Magan A, Memarzadeh A, Pasters V, Shariff S. Neutral heel lateral push test: The first clinical examination of spring ligament integrity. The Foot. 2015;25(2):69–74. doi: 10.1016/j.foot.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Graham ME, Jawrani NT, Chikka A. Extraosseous talotarsal stabilization using HyProCure ® in adults: A 5-year retrospective follow-up. Journal of Foot and Ankle Surgery. 2012;51(1):23–29. doi: 10.1053/j.jfas.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Vedantam, R., Capelli, A.M., Schoenekar, P.L. 1998. Subtalar Arthroereisis for the Correction of Planovalgus Foot in Children With Neuromuscular Disorders - PubMed. J Pediatr Orthop [Internet]. 1998 [cited 2020 Jun 14];18(3):294–8. Available from: https://pubmed.ncbi.nlm.nih.gov/9600551/ [PubMed]
- 30.Giannini S, Ceccarelli F, Benedetti MG, Catani F, Faldini C. Surgical treatment of flexible flatfoot in children: A four-year follow-up study. The Journal of Bone and Joint Surgery. 2001;83:73–79. doi: 10.2106/00004623-200100022-00003. [DOI] [PubMed] [Google Scholar]
- 31.Needleman RL. A surgical approach for flexible flatfeet in adults including a subtalar arthroereisis with the MBA sinus tarsi implant. Foot and Ankle International. 2006;27(1):9–18. doi: 10.1177/107110070602700103. [DOI] [PubMed] [Google Scholar]
- 32.Bresnahan PJ, Chariton JT, Vedpathak A. Extraosseous talotarsal stabilization using HyProCure®: Preliminary clinical outcomes of a prospective case series. The Journal of Foot & Ankle Surgery. 2013;52(2):195–202. doi: 10.1053/j.jfas.2012.11.013. [DOI] [PubMed] [Google Scholar]