Summary
Background
The updated definition of hypertension by the American College of Cardiology (ACC) and the American Heart Association (AHA) is an important paradigm shift and has lead to extensive discussion. We aimed to examine the association between the updated blood pressure (BP) categories and the risk of cardiovascular diseases (CVDs) with potential modifications from other cardiovascular health metrics (CVHMs).
Methods
This prospective study included 91,204 participants ≥40 years recruited from 20 community sites across mainland China. Participants were followed up during 2010-2016 for CVD events including nonfatal myocardial infarction, stroke, heart failure, and cardiovascular death. BP categories were defined according to the 2017 ACC/AHA guideline and CVHMs included smoking, physical activity, diet, body-mass index, total cholesterol, and fasting glucose.
Findings
Overall, 1,985 major CVD events occurred during a mean follow-up of 3.7 years. Having more ideal CVHMs significantly reduced the risk of CVD events in both stage 1 and stage 2 hypertension. Compared with participants without hypertension, participants having ≥4 ideal CVHMs were no longer associated with an increased CVD risk in stage 1 hypertension (HR=1·04; 95% CI=0·83-1·31), but less so in stage 2 hypertension (HR=1·90, 95% CI=1·70-2·13). Such pattern of association was more evident in participants aged <60 years (P for interaction <0·05).
Interpretation
Stage 1 hypertension defined by the ACC/AHA identifies individuals at increased CVD risk, which can be attenuated by achieving more preferable cardiovascular health, especially in adults aged <60 years.
Keywords: Blood pressure, hypertension, cardiovascular health metrics, cardiovascular disease, cardiovascular prevention
Research in Context.
Evidence before this study
We searched PubMed in any languages for studies published until May 31, 2021, using the key terms (“hypertension” or “high blood pressure”) and “cardiovascular health” and (“cardiovascular disease” or “myocardial infarction” or “stroke”). We also searched the reference lists of retrieved articles to identify further relevant publications. We identified several studies revealing an increased risk of CVD in newly defined hypertension, and one study assessed the association between ideal cardiovascular health metrics (ICVHMs) and the risk of stroke among 5,488 hypertensive patients diagnosed by blood pressure (BP) levels ≥140/90 mmHg. However, no study was found assessing the CVD risks in newly defined hypertension with modifications by ICVHMs.
Added value of this study
We found significantly increased risks of major CVD events in participants with stage 1 and stage 2 hypertension. Having more ICVHMs was related to lower risks of CVD in both stage 1 and stage 2 hypertension, and having ≥4 ICVHMs in stage 1 hypertension attenuated the CVD risk to a level similar to those without hypertension. Although achieving more ICVHMs did not avert a significantly increased CVD risk in stage 2 hypertension, the risk reduced approximately 12% for each 1-increase in the number of ICVHMs. Finally, age-specific analysis revealed that the association between hypertension, ideal CVH status, and CVD development was more evident in adults aged<60 years.
Implication of all the available evidence
Our findings emphasize the need for an early detection and management of the newly defined stage 1 hypertension, and support the importance of promoting cardiovascular health to prevent CVD events in both stages of hypertension.
Alt-text: Unlabelled box
Introduction
Hypertension is the leading global risk factor for cardiovascular disease (CVD) and mortality.1 The definition of hypertension has changed over the years, from a systolic blood pressure (SBP)/diastolic blood pressure (DBP) of ≥160/90 mmHg in 1984 to ≥140/90 mmHg in 1993,2,3 and a further reduction to ≥130/80 mmHg in 2017.4 The recent definition of ≥130/80 mmHg has led to a substantial increase in the prevalence of hypertension and a small increase in recommended antihypertensive medications in the US adults compared with the long used definition of ≥140/90 mmHg.5 Emerging evidence revealed that there is an increased risk for CVD in stage 1 hypertension defined by the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guideline in young and middle-aged adults, while findings were inconsistent among the elderly.6, 7, 8, 9
Seven ideal cardiovascular health metrics (ICVHMs) defined by the AHA were associated with markedly reduced risks for CVD and mortality.10, 11, 12 Better cardiovascular health status was related to lower risks of CVD and mortality in young,13 middle-aged,11 and elderly populations,14 highlighting the importance of maintaining an ideal cardiovascular health status across the life course. However, whether having ICVHMs counteracts the risk of CVD in participants with stage 1 or stage 2 hypertension is unknown.
Therefore, we used data from a large prospective cohort to 1) assess the CVD risk associated with stage 1 and stage 2 hypertension, 2) examine the potential modifications in CVD risks by ICVHMs in stage 1 and stage 2 hypertension, and 3) explore age-specific associations between hypertension status, ICVHMs, and CVD risks.
Methods
Study participants
The China Cardiometabolic Disease and Cancer Cohort (4C) study is a nationwide, multicenter, population-based, prospective cohort study of cardiometabolic diseases and risk factors in Chinese adults.15, 16, 17 In 2010-2012, 193,846 participants 40 years or older from 20 community sites located in 16 provinces, autonomous regions, or municipalities across mainland China were recruited using local resident registration systems to undergo a comprehensive evaluation of cardiometabolic health. In 2014-2016, all participants were invited to participate in a follow-up examination, among whom 170,240 participants responded. We excluded participants with a history of cardiovascular diseases or with antihypertensive medications at baseline (n=29,347), with missing data on cardiovascular health metrics, hypertension, or other covariates at baseline (n=33,804), or without information on CVD development during follow-up (n=15,885). Finally, a total of 91,204 participants were included in the current analysis (Supplementary Figure 1).
This study was approved by the Medical Ethics Committee of Ruijin Hospital, Shanghai Jiaotong University School of Medicine. All study participants provided written informed consent.
Data collection
At each study site, trained staff collected data according to a standard protocol at local primary healthcare centers. Information on sociodemographic characteristics, lifestyle and dietary factors, and medical history was collected face-to-face by trained interviewers using a standard questionnaire. Smoking habits at present as well as in the past were recorded. Physical activity was assessed using the International Physical Activity Questionnaire.18 and physical activity duration per week was evaluated based on the intensity (vigorous/intermediate/mild), frequency (days per week), and average duration (minutes per day). Habitual dietary intake was examined by asking the frequency and portion size of typical food items consumed over the past 12 months.
Body weight and height measurements were performed according to a standard protocol and body-mass index (BMI) was calculated as the weight in kilograms divided by height in meters squared. Three BP measurements were obtained by trained observers from each participant using a calibrated automatic electronic device (OMRON Model HEM-752 FUZZY) in a separate examination room after at least 5-minute sitting rest with 1-minute intervals between measurements. Participants were advised to avoid alcohol, coffee, tea, smoking, and exercise at least 30 minutes before BP measurement. The appropriate cuff was used depending on the subject's arm circumference. The average of three readings was used for analysis.
Blood samples were collected from each participant in the morning after an overnight fast for at least 10 hours. Fasting plasma glucose (FPG) levels were measured locally using a glucose oxidase or hexokinase method after blood samples being centrifuged on site within 2 hours of collection. All local laboratories passed a national standardization program and a study-specific quality assurance program.15 Serum samples were aliquoted into 0·5-mL Eppendorf tubes within 2 hours after collection and were then frozen at -80 degrees at local hospitals. All samples were shipped in dry ice to the central laboratory accredited by the College of American Pathologists at Shanghai National Clinical Research Center for Metabolic Diseases, where serum total cholesterol (TC) was measured on an auto-analyzer (c16000 system, ARCHITECT ci16200 analyzer, Abbott Laboratories, Illinois, USA).
Hypertension Classification
According to the 2017 ACC/AHA hypertension guideline recommendations,4 we categorized adults without hypertension when their BP level was <130/80 mmHg, stage 1 hypertension when their BP level was 130-139/80-89 mmHg, and stage 2 hypertension when their BP level was ≥140/90 mmHg.
ICVHMs Definition
ICVHMs were defined according to the 2010 AHA recommendations.10 Ideal smoking status was defined as never smoking or smoking cessation for more than 12 months. Ideal physical activity was defined as ≥150 minutes/week moderate-intensity, ≥75 minutes/week vigorous-intensity, or ≥150 minutes/week moderate- or vigorous-intensity physical activities. Ideal diet was defined as fruit and vegetable intake ≥4·5 cups/day. Ideal BMI was defined as a BMI level <23 kg/m2, a cutoff point specific for Asian populations.19 Ideal TC was defined as a TC level <200 mg/dL without treatment. Ideal FPG was defined as an FPG level <100 mg/dL without treatment (Supplementary Table 1). Ideal BP was not defined and hypertension classification was used instead. The overall cardiovascular health status was grouped according to the number of ICVHMs ≤1, 2, 3, and ≥4 to allow for a reasonable number of participants in each group (Supplementary Table 2).
CVD Outcomes
The occurrence of major CVD events was obtained at the follow-up visit. Incident CVD was defined as the first occurrence of myocardial infarction, stroke, hospitalization or treatment for heart failure, and cardiovascular death during follow-up. As described previously,17 myocardial infarction was defined by characteristic changes in levels of troponin T and creatine-kinase-MB isoform, symptoms of myocardial ischemia, changes in electrocardiogram results, or a combination of them. Stroke was defined as a fixed neurologic deficit for at least 24 hours because of a presumed vascular cause. Heart failure was identified by hospitalization or an emergency department visit requiring a treatment with infusion therapy for a clinical syndrome presenting with multiple signs and symptoms in consistence with cardiac decompensation or inadequate cardiac pump function. Information on vital status and clinical outcomes was also obtained from the local death and disease registries of the National Disease Surveillance Point System and the National Health Insurance System. Throughout the study period, medical records of subjects who visited an emergency department or were hospitalized were collected and adjudicated centrally. Two members of the outcome adjudication committee independently verified each clinical event and discrepancies were resolved by discussion involving other members of the committee. All members of the committee were unaware of the baseline risk factors of study participants.
Statistical Analysis
Baseline characteristics according to the hypertension status were presented as means (standard deviations [SDs]) for continuous variables with a normal distribution and numbers (proportions) for categorical variables. The one-way analysis of variance (ANOVA) was used to compare continuous variables and the chi-square test was used to compare categorical variables across hypertension status. Incidence rates of major CVD events were described as number of events per 1,000 person-years. Follow-up time was censored at the date of incident CVD event for those who had an event or at the date of follow-up examination for those who remained free from incident CVD cases. Cox proportional hazards models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for major CVD events. Risks were compared between participants without hypertension and participants with stage 1 or stage 2 hypertension who had different CVH status in terms of individual ICVHMs as well as numbers of ICVHMs. Among participants with stage 1 or stage 2 hypertension, risks in participants with vs. without individual ICVHMs and risks in participants with 2, 3, and ≥4 ICVHMs vs. ≤1 ICVHM were calculated. These analyses were repeated in participants with age <60 and ≥60 years separately. The Cox models were adjusted for covariates including age (continuous), sex (men or women), educational attainment (< or ≥ high school), and current drinking (yes or no) in the analysis of ICVHMs numbers and were further adjusted for all the other ICVHMs in the analysis of individual ICVHMs. Interactions between age groups and ICVHMs numbers in the association with risks of major CVD events were estimated by including the product term in the models. In addition, sensitivity analysis was conducted among participants taking antihypertensive medications, using a BMI level <25 kg/m2 to define ideal BMI, or comparing with those with a “normal BP” (systolic BP <120 mmHg and diastolic BP <80 mmHg).
All the tests were two-tailed, with a P value <0·05 considered to indicate statistical significance. Statistical analyses were performed using R version 3.6.3 (R Project for Statistical Computing, http://www.r-project.org).
Role of the funding source
The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Baseline characteristics of study participants according to categories of hypertension status are presented in Table 1 and Supplemental Figure 2. Among the overall 91,204 participants, 41,127 (45·1%) did not have hypertension, 22,190 (24·3%) had stage 1 hypertension, and 27,887 (30·6%) had stage 2 hypertension. Mean systolic BP/diastolic BP in participants without hypertension, stage 1 hypertension, and stage 2 hypertension were 114·2/69·7 mmHg, 130·2/80·0 mmHg, and 150·9/87·0 mmHg, respectively. Mean age and the proportion of men increased across BP groups, as well as levels of BMI, total cholesterol, and FPG (all p values for trend <0·001). The proportions of individual ICVHMs and number of ICVHMs ≥3 decreased significantly across BP groups (all p values for trend <0·001).
Table 1.
Baseline characteristics of 91,204 participants by hypertension status.
| Characteristics | Without hypertension (SBP <130 mmHg and DBP <80 mmHg) | Stage 1 hypertension (SBP 130-139 mmHg or DBP 80-89 mmHg) | Stage 2 hypertension (SBP ≥140 mmHg or DBP ≥90 mmHg) | P Value |
|---|---|---|---|---|
| Participants (n) | 41,127 | 22,190 | 27887 | |
| Age (years) | 53·8 ± 8·3 | 55·4 ± 8·5 | 58·8 ± 8·9 | < 0·001 |
| Men, n (%) | 11337 (27·6) | 8221 (37·0) | 11149 (40·0) | < 0·001 |
| High school education or above, n (%) | 17978 (43·7) | 8380 (37·8) | 8166 (29·3) | < 0·001 |
| Current drinkers, n (%) | 3137 (7·6) | 2660 (12·0) | 3957 (14·2) | < 0·001 |
| BMI (kg/m2) | 23·5 ± 3·3 | 24·8 ± 3·5 | 25·3 ± 3·5 | < 0·001 |
| SBP (mmHg) | 114·2 ± 9·3 | 130·2 ± 7·0 | 152·9 ± 14·6 | < 0·001 |
| DBP (mmHg) | 69·7 ± 6·2 | 80·0 ± 6·2 | 87·0 ± 10·4 | < 0·001 |
| TC (mg/dL) | 183·9 ± 43·8 | 191·3 ± 43·7 | 198·3 ± 43·9 | < 0·001 |
| FPG (mg/dL) | 101·9 ± 24·6 | 107·0 ± 28·5 | 111·4 ± 32·8 | < 0·001 |
| Ideal cardiovascular health metrics, n (%) | ||||
| Ideal smoking status | 33646 (81·8) | 17420 (78·5) | 22067 (79·1) | < 0·001 |
| Physical activity at goal | 6542 (15·9) | 3093 (13·9) | 3657 (13·1) | < 0·001 |
| Healthy diet | 20264 (49·3) | 10211 (46·0) | 10922 (39·2) | < 0·001 |
| BMI at goal | 19019 (46·2) | 6723 (30·3) | 7062 (25·3) | < 0·001 |
| Untreated TC at goal | 26946 (65·5) | 13007 (58·6) | 14612 (52·4) | < 0·001 |
| Untreated FPG at goal | 24923 (60·6) | 10780 (48·6) | 11586 (41·5) | < 0·001 |
| No. of ICVHMs, n (%) | < 0·001 | |||
| ≤1 | 3016 (7·3) | 2988 (13·5) | 5119 (18·4) | |
| 2 | 8350 (20·3) | 6252 (28·2) | 9194 (33·0) | |
| 3 | 13193 (32·1) | 7203 (32·5) | 8345 (29·9) | |
| ≥4 | 16568 (40·3) | 5747 (25·9) | 5229 (18·8) |
Data are presented as means ± standard deviations for continuous variables with a normal distribution or numbers (proportions) for categorical variables.
Abbreviations: BMI, body-mass index; DBP, diastolic blood pressure; FPG, fasting plasma glucose; ICVHMs, ideal cardiovascular health metrics; SBP, systolic blood pressure; TC, total cholesterol.
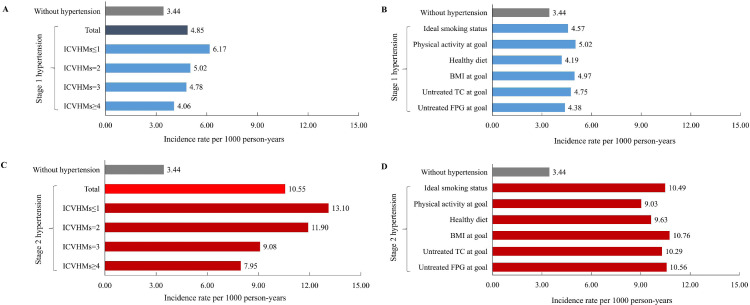
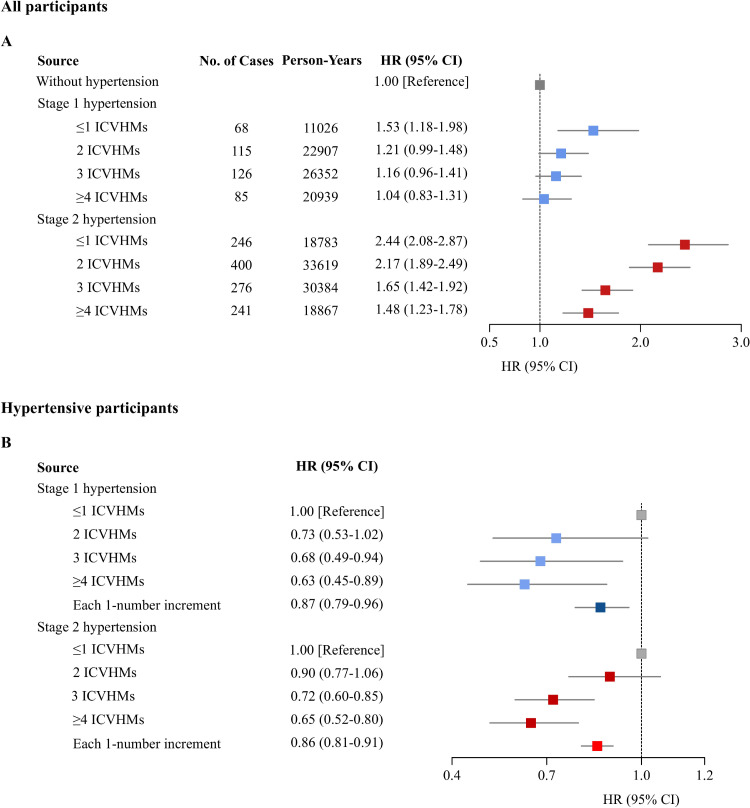
Overall, 1,985 major CVD events occurred during a mean follow-up of 3·7 years (333,756 person-years). The crude CVD incidence rates were 3·44 (3·16-3·75), 4·85 (4·39-5·35), and 10·55 (9·93-11·20) per 1000 person-years in participants without hypertension, with stage 1 hypertension, and stage 2 hypertension, respectively (Figure 1). Compared with participants without hypertension, participants with stage 1 hypertension had a significantly 20% increased risk of developing CVD events (HR, 1·20; 95% CI, 1·05-1·37) (Table 2). However, when participants with stage 1 hypertension had ≥4 ICVHMs, a similar CVD risk was found compared with participants without hypertension (HR, 1·04; 95% CI, 0·83-1·31; Figure 2A). Compared with participants without hypertension, participants with stage 2 hypertension had a significantly 90% increased risk of developing CVD events (HR, 1·90; 95% CI, 1·70-2·13) (Table 2). Although participants having ideal levels of individual CVH metrics (Table 2) or having an increased number of ICVHMs had lower CVD risk (Figure 2A), the development of major CVD events was still significantly enhanced in stage 2 hypertension compared with those without hypertension. Results were similar in participants taking antihypertensive medications (Supplemental Table 3), using BMI <25 kg/m2 to define ideal BMI (Supplemental Table 4), or comparing with those with a “normal BP” (Supplemental Table 5, Supplementary Figure 3). In addition, the relative risk ratio of the HR of stage 1 hypertension with ≥4 ICVHMs vs. without hypertension and the HR of stage 2 hypertension with ≥4 ICVHMs vs. without hypertension was 0·70 (0·52-0·94), indicating a significantly lower risk of stage 1 hypertension with ≥4 ICVHMs than stage 2 hypertension with ≥4 ICVHMs using those without hypertension as the reference.
Figure 1.
Incidence rates of major cardiovascular events. Incidence rate per 1000 person-years for major cardiovascular events according to blood pressure categories and ICVHMs: stage 1 hypertension with ≤1, 2, 3, ≥4 ICVHMs (A), stage 1 hypertension with individual ICVHM (B), stage 2 hypertension with ≤1, 2, 3, ≥4 ICVHMs (C), stage 2 hypertension with individual ICVHM (D).
Abbreviations: BMI, body-mass index; FPG, fasting plasma glucose; ICVHMs, ideal cardiovascular health metrics; TC, total cholesterol.
Table 2.
Hazard ratio (95% CI) of major cardiovascular events by baseline hypertension status and each individual cardiovascular health metrics.
| Baseline categories | No. of cases | Person-Years | HR (95% CI)* |
|---|---|---|---|
| Without hypertension | 519 | 150,880 | 1 [Reference] |
| Stage 1 hypertension | 394 | 81,224 | 1·17 (1·02-1·34) |
| Ideal smoking status | 290 | 63,470 | 1·15 (0·98-1·34) |
| Physical activity at goal | 57 | 11,349 | 1·16 (0·88-1·53) |
| Healthy diet | 154 | 36,743 | 1·05 (0·87-1·26) |
| BMI at goal | 121 | 24,360 | 1·14 (0·93-1·39) |
| Untreated TC at goal | 226 | 47,545 | 1·20 (1·02-1·40) |
| Untreated FPG at goal | 176 | 40203 | 1·15 (0·97-1·36) |
| Stage 2 hypertension | 1072 | 101,653 | 1·90 (1·70-2·13) |
| Ideal smoking status | 800 | 80,348 | 1·69 (1·49-1·90) |
| Physical activity at goal | 126 | 13,469 | 1·66 (1·35-2·03) |
| Healthy diet | 311 | 38,573 | 1·59 (1·37-1·84) |
| BMI at goal | 266 | 25,262 | 1·69 (1·44-1·98) |
| Untreated TC at goal | 521 | 53,131 | 1·84 (1·61-2·10) |
| Untreated FPG at goal | 439 | 43,451 | 1·81 (1·58-2·08) |
Abbreviations: BMI, body-mass index; CI, confidence interval; FPG, fasting plasma glucose; HR, hazard ratio; TC, total cholesterol.
Adjusted for age, sex, education, drinking status, and other cardiovascular health metrics.
Figure 2.
Hazard ratio (95% CI) of major cardiovascular events. HR (95% CI) of major cardiovascular events according to the number of ICVHMs among participants with stage 1 hypertension (blue) and stage 2 hypertension (red), as compared with those without hypertension, adjusted for age, sex, education, and drinking status (A). HR (95% CI) of major cardiovascular events per 1-number increment in ICVHMs among participants with stage 1 hypertension (blue) or stage 2 hypertension (red), adjusted for age, sex, education, drinking status, systolic and diastolic blood pressure (B).
Abbreviations: CI, confidence interval; HR, hazard ratio; ICVHMs, ideal cardiovascular health metrics.
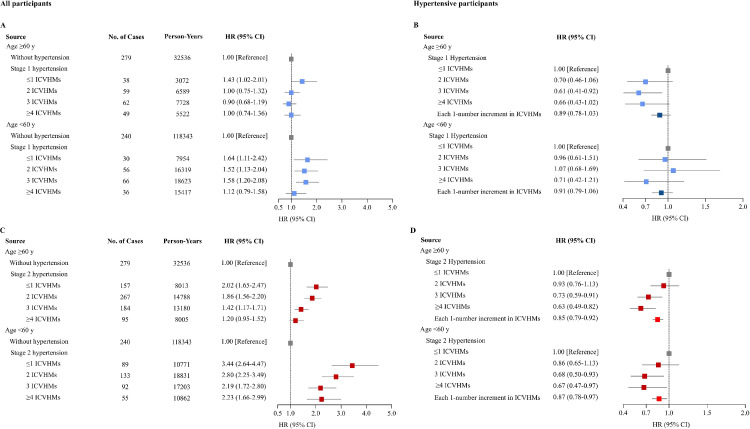
When participants were stratified according to age, stage 1 hypertension was not associated with an increased risk of CVD compared with those without hypertension in participants ≥60 years (HR, 1·02; 95% CI, 0·86-1·23) (Figure 3A). Although stage 1 hypertension overall was associated with an increased risk of CVD in participants <60 years (HR, 1·45; 95% CI, 1·19-1·76), the risk decreased with an increasing number of ICVHMs and having ≥4 ICVHMs attenuated the risk compared with those without hypertension (HR, 1·12; 95% CI, 0·79-1·58; P value for interaction between ICVHMs ≥4 and age groups <0·001). Stage 2 hypertension was associated with an increased risk of CVD compared with those without hypertension in participants ≥60 years (HR, 1·63; 95% CI, 1·42-1·88) and in participants <60 years (HR, 2·65; 95% CI, 2·24-3·13) (Figure 3C). Although the CVD risk decreased with an increasing number of ICVHMs in both age groups, it can hardly be averted compared with participants without hypertension. Interactions between age groups and numbers of ICVHMs in the association with CVD risks were significant in both stage 1 and stage 2 hypertension compared with those without hypertension (both P values for interaction <0·05).
Figure 3.
Hazard ratio (95% CI) of major cardiovascular events according to age categories. HR (95% CI) of major cardiovascular events according to the number of ICVHMs among participants aged ≥60 or <60 years with stage 1 hypertension (A) or stage 2 hypertension (C), as compared with those without hypertension, adjusted for age, sex, education, and drinking status. HR (95% CI) of major cardiovascular events per 1-number increment in ICVHMs among participants aged ≥60 or <60 years with stage 1 hypertension (B) or stage 2 hypertension (D), adjusted for age, sex, education, drinking status, systolic and diastolic blood pressure. Interactions between age groups and ICVHM numbers in the association with risks of major cardiovascular events: P for interaction = 0·002 (A); P for interaction < 0·001 (C). Interactions between age groups and per 1-number increment in ICVHMs in the association with cardiovascular events: P for interaction = 0·74 (B); P for interaction = 0·97 (D).
Abbreviations: CI, confidence interval; HR, hazard ratio; ICVHMs, ideal cardiovascular health metrics.
Among participants with stage 1 hypertension, no significant reduction in CVD risk was found in those with most individual ICVHMs compared with participants without that individual ICVHMs (Supplemental Table 6). A significant CVD risk reduction was found in participants having ≥4 ICVHMs compared with those having ≤1 ICVHM (HR, 0·63; 95% CI, 0·45-0·89) (Figure 2B). Among participants with stage 2 hypertension, significant reductions in CVD risk were observed in those with individual ICVHMs such as ideal smoking status, or healthy diet compared with participants without that individual ICVHMs (Supplemental Table 6). Participants having 2, 3, and ≥4 ICVHMs were at 10%, 28%, and 35% decreased CVD risks compared with those having ≤1 ICVHM (Figure 2B).
When participants with stage 1 hypertension or stage 2 hypertension were stratified according to age, a non-significant trend of reduction in CVD risks was observed with more ICVHMs in both age groups for stage 1 hypertension (Figure 3B). Risks of major CVD events were reduced significantly by 15% and 13% with each 1-increment in ICVHM numbers in age groups of ≥60 and <60 years for stage 2 hypertension (Figure 3D).
Discussion
In this large, nationwide, multicenter, prospective cohort study of 91,204 Chinese adults, we found significantly increased risks of major CVD events in participants with stage 1 and stage 2 hypertension. Having more ICVHMs was related to lower risks of CVD in both stage 1 and stage 2 hypertension, and having ≥4 ICVHMs in stage 1 hypertension attenuated the CVD risk to a level similar to participants without hypertension. Although achieving more ICVHMs did not avert a significantly increased CVD risk in stage 2 hypertension, the risk reduced approximately 12% for each 1-increase in the number of ICVHMs. Finally, age-specific analysis revealed that the association between hypertension, ideal CVH status, and CVD development was more evident in adults aged <60 years. Our findings emphasize the need for an early detection and management of the newly defined stage 1 hypertension, and support the importance of promoting cardiovascular health to prevent CVD events in both stages of hypertension.
The prevalence of hypertension is rising globally and in China,20 owing to ageing of the population and increases in exposure to lifestyle risk factors such as unhealthy diets and lack of physical activity.21 Despite the widespread use of antihypertensive medications, hypertension control remains unacceptably low, particularly in low- and middle-income countries.22 The 2017 ACC/AHA hypertension guideline redefined hypertension as SBP ≥130 mmHg or DBP ≥80 mmHg, reclassifying 267 million Chinese adults and 70.1 million US adults in the 45-75 year age group as having hypertension.23 Consistent with previous studies,6,8,24 we found that the newly defined stage 1 hypertension, which accounted for 24% of the study population, contributed to an increased CVD risk by approximately 20%. The increase was more evident in adults aged 40-59 years compared with adults ≥60 years. Similar results were found in younger adults (<40 years) with stage 1 hypertension in the U.S., Korean, and Chinese populations.25, 26, 27 A prospective cohort study with approximately 0.5 million Chinese adults demonstrated a steeper increase in risks of vascular disease with higher systolic BP in young vs. elderly adults.28 However, there has been less consistency regarding the need for antihypertensive drug treatment in patients with stage 1 hypertension, especially younger adults who would most likely have low predicted 10-year ASCVD risk regardless of risk factor burden.29 By using cardiovascular health rather than predicted ASCVD risk to further stratify younger participants with stage 1 hypertension, we demonstrated that adults <60 years of age with stage 1 hypertension who had ≥4 ICVHMs could be considered at a low CVD risk and preventive efforts might be implemented in young stage 1 hypertensive patients with a less number of ICVHMs.
Prior studies have suggested that the presence of more ICVHMs is inversely associated with the risk of CVD and mortality.13,14,30 Moreover, a prospective cohort study of 5,488 hypertensive patients with SBP ≥140 mmHg or DBP ≥90 mmHg found that an increased number of ICVHMs was inversely associated with the incidence of ischemic stroke.31 In the current study, participants with stage 1 hypertension and ≥4 ICVHMs had a CVD risk similar to participants without hypertension. Having more ICVHMs reduced the CVD risk in a dose-response manner in participants with stage 2 hypertension, although the risk cannot be fully averted to a level similar to participants without hypertension. Our findings reveal that achieving more preferable cardiovascular health may help prevent the onset of CVD events among individuals with stage 1 or stage 2 hypertension. This is particularly relevant given that the updated definition of hypertension will markedly increase the number of people as hypertensive and at increased CVD risks.23 Because the percentage of ideal cardiovascular health in Chinese adults was extremely low,32 more aggressive efforts are needed to improve cardiovascular health. In addition, a nationwide cohort study has confirmed the associations of young adulthood CVH status, as well as its change over time, with premature CVD events.33 In the current study, the association between hypertension, ideal CVHMs, and CVD risk was more apparent in adults aged <60 years. These findings indicate the critical importance of maintaining ideal CVH status at young adulthood and beyond in people with or without hypertension.
The current study has several limitations. First, a significant proportion of participants were not included in the current analysis and there might be selection and lost to follow-up biases. We compared baseline characteristics between participants included and those excluded for missing data by using standardized differences in Supplementary Tables 7 and 8. A standardized difference <0.1 was considered balanced between groups34 and all of the standardized difference values were <0.1 for compared variables. In addition, the sensitivity analysis using multiple imputations of missing baseline data revealed similar findings to those of the main analysis (Supplementary Figure 4). Second, data on smoking status, physical activity, and dietary habits were self-reported. Although a standard and detailed questionnaire was used and a face-to-face interview was conducted to collect information, recall bias could not be ruled out. Third, healthy diet was evaluated based on consumptions of fruit and vegetable, and a more comprehensive assessment of dietary habits should have been used. Forth, newly-diagnosed hypertension was determined by only one attended examination, although 3 BP measurements were obtained during the study visit using a standard protocol. Fifth, although the CVHMs information was re-evaluated at the follow-up examination, we only had 1 follow-up examination and CVD events occurred during the follow-up. Therefore, the relationship between the changes of CVHMs and CVD risk cannot be analyzed or time-varying analysis cannot be done, and more follow-up examinations are needed. In addition, the relatively short duration of follow-up limited the number of incident CVD events and prevented further analysis based on individual CVD components. Finally, despite adjustment for multiple covariates in the Cox models, residual confounding can hardly be avoided.
Conclusions
In this large, nationwide, community-based, prospective cohort study of Chinese adults, we found that stage 1 hypertension defined by the 2017 ACC/AHA guideline was associated with an increased risk of major CVD events compared with those without hypertension. Having more ICVHMs diminished the risk of CVD in both stage 1 and stage 2 hypertension. When participants with stage 1 hypertension had ≥4 ICVHMs, the CVD risk could be attenuated to a level similar to participants without hypertension. The association between hypertension, ICVHMs, and CVD events was more evident in adults <60 years of age. Our findings highlight the importance of identifying individuals with stage 1 hypertension and emphasize the benefits of improving CVH status in both stage 1 and stage 2 hypertension for the primary prevention of CVD events.
Declaration of interest
None.
Acknowledgments
Contributors
Shujing Wu, Yu Xu, Weiqing Wang, and Guang Ning conceived and designed the study. Shujing Wu analyzed the data. Yu Xu and Ruizhi Zheng verified the data. Shujing Wu, Yu Xu, and Ruizhi Zheng drafted the manuscript. Jieli Lu, Mian Li, Weiqing Wang, and Guang Ning revised the manuscript. Li Chen, Yanan Huo, Min Xu, Tiange Wang, Zhiyun Zhao, Shuangyuan Wang, Hong Lin, Meng Dai, Di Zhang, Jingya Niu, Guijun Qin, Li Yan, Qin Wan, Lulu Chen, Lixin Shi, Ruying Hu, Xulei Tang, Qing Su, Xuefeng Yu, Yingfen Qin, Gang Chen, Zhengnan Gao, Guixia Wang, Feixia Shen, Zuojie Luo, Yuhong Chen, Yinfei Zhang, Chao Liu, Youmin Wang, Shengli Wu, Tao Yang, Qiang Li, Yiming Mu, Jiajun Zhao, and Yufang Bi collected the data and critical revised the manuscript for important intellectual content. All authors agreed to be held accountable for all aspects of this work and approved the final version of the manuscript. Shujing Wu, Yu Xu, Weiqing Wang, and Guang Ning are all guarantors of this work and, take responsibility for the integrity of the data and accuracy of the data analysis. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Data sharing
Data are available from the corresponding authors upon reasonable request. A proposal with detailed description of study objectives and statistical analysis plan will be needed for evaluation of the reasonability of requests. Additional, relevant documents might also be required during the process of evaluation.
Acknowledgments
This work was supported by the grants from the National Key R&D Program of China (2017YFC1310700, 2016YFC1305600, 2018YFC1311800, 2016YFC0901200), the National Natural Science Foundation of China (81870560, 81970691, 81941017, 81770842, 81970706, 82022011, 82070880), Chinese Academy of Medical Sciences (2018PT32017, 2019PT330006), the Shanghai Municipal Government (18411951800), the Shanghai Shenkang Hospital Development Center (SHDC12019101, SHDC2020CR1001A, SHDC2020CR3069B), the Shanghai Jiaotong University School of Medicine (DLY201801), and the Ruijin Hospital (2018CR002).
Footnotes
Funding: National Key R&D Program of China.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2021.100350.
Appendix. Supplementary materials
References
- 1.Forouzanfar MH, Liu P, Roth GA, et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 2.The 1984 Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1984;144:1045–1057. [PubMed] [Google Scholar]
- 3.The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V) Arch Intern Med. 1993;153:154–183. [PubMed] [Google Scholar]
- 4.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Muntner P, Carey RM, Gidding S, et al. Potential US Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation. 2018;137:109–118. doi: 10.1161/CIRCULATIONAHA.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han M, Chen Q, Liu L, et al. Stage 1 hypertension by the 2017 American College of Cardiology/American Heart Association hypertension guidelines and risk of cardiovascular disease events: systematic review, meta-analysis, and estimation of population etiologic fraction of prospective cohort studies. J Hypertens. 2020;38:573–578. doi: 10.1097/HJH.0000000000002321. [DOI] [PubMed] [Google Scholar]
- 7.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qi Y, Han X, Zhao D, et al. Long-Term Cardiovascular Risk Associated With Stage 1 Hypertension Defined by the 2017 ACC/AHA Hypertension Guideline. J Am Coll Cardiol. 2018;72:1201–1210. doi: 10.1016/j.jacc.2018.06.056. [DOI] [PubMed] [Google Scholar]
- 9.Lee H, Cho SMJ, Park JH, Park S, Kim HC. 2017 ACC/AHA Blood Pressure Classification and Cardiovascular Disease in 15 Million Adults of Age 20-94 Years. J Clin Med. 2019;8(11):1832. doi: 10.3390/jcm8111832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 11.Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perak AM, Ning H, Khan SS, et al. Associations of Late Adolescent or Young Adult Cardiovascular Health With Premature Cardiovascular Disease and Mortality. J Am Coll Cardiol. 2020;76:2695–2707. doi: 10.1016/j.jacc.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaye B, Canonico M, Perier MC, et al. Ideal Cardiovascular Health, Mortality, and Vascular Events in Elderly Subjects: The Three-City Study. J Am Coll Cardiol. 2017;69:3015–3026. doi: 10.1016/j.jacc.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Lu J, He J, Li M, et al. Predictive Value of Fasting Glucose, Postload Glucose, and Hemoglobin A1c on Risk of Diabetes and Complications in Chinese Adults. Diabetes Care. 2019;42:1539–1548. doi: 10.2337/dc18-1390. [DOI] [PubMed] [Google Scholar]
- 16.Li M, Xu Y, Wan Q, et al. Individual and Combined Associations of Modifiable Lifestyle and Metabolic Health Status With New-Onset Diabetes and Major Cardiovascular Events: The China Cardiometabolic Disease and Cancer Cohort (4C) Study. Diabetes Care. 2020;43:1929–1936. doi: 10.2337/dc20-0256. [DOI] [PubMed] [Google Scholar]
- 17.Wang T, Lu J, Su Q, et al. Ideal Cardiovascular Health Metrics and Major Cardiovascular Events in Patients With Prediabetes and Diabetes. JAMA Cardiol. 2019;4:874–883. doi: 10.1001/jamacardio.2019.2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 19.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 20.Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project) Lancet. 2017;390:2549–2558. doi: 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 21.Mills KT, Bundy JD, Kelly TN, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–237. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khera R, Lu Y, Lu J, et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2018;362:k2357. doi: 10.1136/bmj.k2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu N, Yang JJ, Meng R, et al. Associations of blood pressure categories defined by 2017 ACC/AHA guidelines with mortality in China: Pooled results from three prospective cohorts. Eur J Prev Cardiol. 2020;27:345–354. doi: 10.1177/2047487319862066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yano Y, Reis JP, Colangelo LA, et al. Association of Blood Pressure Classification in Young Adults Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Cardiovascular Events Later in Life. JAMA. 2018;320:1774–1782. doi: 10.1001/jama.2018.13551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Son JS, Choi S, Kim K, et al. Association of Blood Pressure Classification in Korean Young Adults According to the 2017 American College of Cardiology/American Heart Association Guidelines With Subsequent Cardiovascular Disease Events. JAMA. 2018;320:1783–1792. doi: 10.1001/jama.2018.16501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu S, Song Y, Chen S, et al. Blood Pressure Classification of 2017 Associated With Cardiovascular Disease and Mortality in Young Chinese Adults. Hypertension. 2020;76:251–258. doi: 10.1161/HYPERTENSIONAHA.119.14239. [DOI] [PubMed] [Google Scholar]
- 28.Lacey B, Lewington S, Clarke R, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0.5 million adults in China: a prospective cohort study. Lancet Glob Health. 2018;6:e641–e649. doi: 10.1016/S2214-109X(18)30217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones DW, Whelton PK, Allen N, et al. Management of Stage 1 Hypertension in Adults With a Low 10-Year Risk for Cardiovascular Disease: Filling a Guidance Gap: A Scientific Statement From the American Heart Association. Hypertension. 2021;77(6):e58–e67. doi: 10.1161/HYP.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 30.Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: A meta-analysis of prospective studies. Clin Cardiol. 2017;40:1339–1346. doi: 10.1002/clc.22836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ying Y, Lin S, Kong F, et al. Ideal Cardiovascular Health Metrics and Incidence of Ischemic Stroke Among Hypertensive Patients: A Prospective Cohort Study. Front Cardiovasc Med. 2020;7 doi: 10.3389/fcvm.2020.590809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bi Y, Jiang Y, He J, et al. Status of cardiovascular health in Chinese adults. J Am Coll Cardiol. 2015;65:1013–1025. doi: 10.1016/j.jacc.2014.12.044. [DOI] [PubMed] [Google Scholar]
- 33.Lee H, Yano Y, Cho SMJ, et al. Associations of Ideal Cardiovascular Health and Its Change During Young Adulthood With Premature Cardiovascular Events: A Nationwide Cohort Study. Circulation. 2021;144(1):90–92. doi: 10.1161/CIRCULATIONAHA.121.054212. [DOI] [PubMed] [Google Scholar]
- 34.Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27(12):2037–2049. doi: 10.1002/sim.3150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.