While most guidelines and clinical trials for heart failure (HF) management involve patients hospitalized primarily for HF, limited guidance is available regarding hospitalizations where HF is a secondary diagnosis. Such secondary HF hospitalizations historically outnumber primary HF hospitalizations, but contemporary data are lacking.1 Recent studies suggest that secondary hospitalizations may be a safe and effective setting for HF care optimization.2 Understanding the contemporary burden of HF hospitalizations (primary and secondary) could inform care improvement efforts. We investigated the frequency, healthcare utilization, and mortality of primary and secondary HF hospitalizations from 2012 to 2018 in the US.
All hospitalizations with patients ≥ 18 years in the National Inpatient Sample (NIS) database from January 1, 2012 through December 31, 2018 with discharge diagnosis of HF in the primary diagnosis field (primary HF) or any other diagnosis field (secondary HF) were identified using International Classification of Diseases codes. Yearly hospitalizations per 1,000 U.S. adults were estimated; population estimates were derived from the U.S. Census Bureau.3 Hospitalization rates were age—adjusted based on the U.S. standard population from 2000. Hospital total charges were converted to cost estimates using hospital-specific cost-to-charge ratios from the Healthcare Cost and Utilization Project and inflated to 2019 U.S. dollars.
Trends in hospitalization rates were examined using linear regression, inpatient mortality using logistic regression, and length of stay (LOS) and inflation-adjusted cost using weighted linear regression, with year as the predictor. Models were adjusted for: age, sex, Charlson Comorbidity Index, hospital location/teaching status, region, and size. Survey design complexity was accounted for by incorporating sampling weights, primary sampling units, and strata. p-values< 0.05 were considered statistically significant; analyses were conducted using Stata 16.0 (Stata-Corp, College Station, TX).
A total of 32.8 million HF hospitalizations were identified, of which 25.3 million (77.1%) were for secondary HF and 7.5 million (22.9%) were for primary HF. Patients were older (mean age 72 [standard error 0.03] years) and mostly White (70.6%). About half of HF hospitalizations were for women (50.3%), and were similar between primary (48.5%) and secondary (50.8%) HF. Secondary HF hospitalizations had a higher proportion of patients with hypertension (70.5% vs 49.7%, p < 0.001) and slightly lower proportions with diabetes (44.1% vs 47.5%, p < 0.001) and chronic lung disease (35.1% vs 39.4%, p < 0.001).
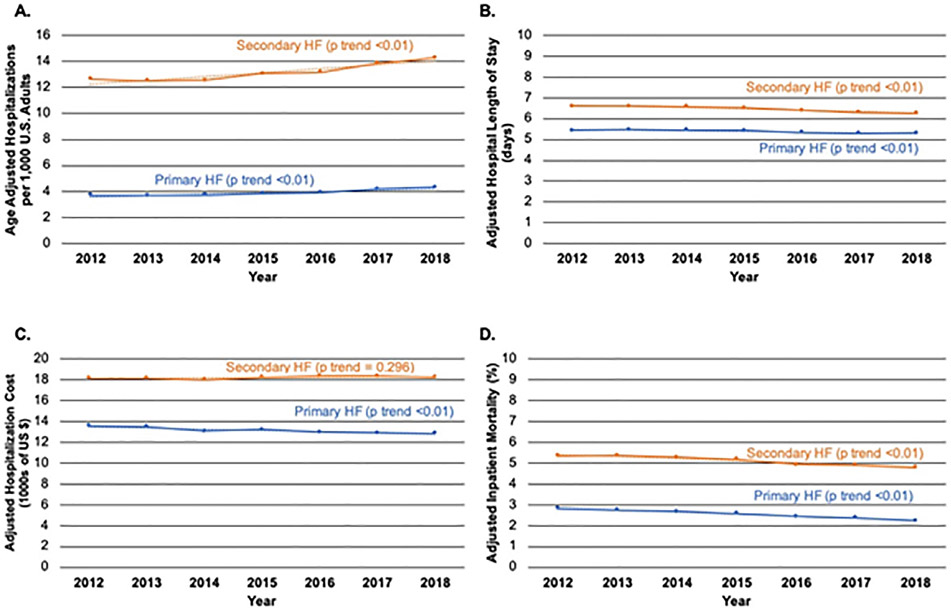
Age-adjusted hospitalization rate increased each year for both hospitalization types, and the ratio between secondary and primary HF hospitalizations was similar during the study period (Figure 1 A). In 2018, the age-adjusted hospitalization incidence per 1,000 U.S. adults was 4.3 for primary HF and 14.3 for secondary HF. Men had a higher incidence of primary HF (5.1 vs 3.7; p < 0.001) and secondary HF (16.2 vs 12.7; p < 0.001) compared with women in 2018. Hospital LOS was longer (6.5 vs 5.3 days; adjusted parameter estimate [aPE] 1.08, 95% confidence interval [CI] 1.06 to 1.09 days; p < 0.001) (Figure 1 B) and hospital costs were greater ($18,224 vs $12,936; aPE $5092, 95% CI $5019 to $5164; p < 0.001) (Figure 1 C) for secondary HF hospitalizations compared with primary HF hospitalizations. While hospital costs decreased over the study period for primary HF (p < 0.001), they did not change for secondary HF hospitalizations (p = 0.296). Inpatient mortality rate was higher for secondary HF vs primary HF (5.5% vs 2.9%; adjusted odds ratio [aOR] 1.94, 95% CI 1.95 to 1.99; p < 0.001). Among secondary HF hospitalizations, inpatient mortality rates were modestly, but significantly, lower in women vs. men (5.3% vs 5.7%, aOR 0.89 95% CI 0.89 to 0.90; p < 0.001). Adjusted inpatient mortality rate trended lower during the study period for both hospitalization types (Figure 1 D).
Figure 1.
A. Age adjusted hospitalizations per 1,000 U.S. adults for primary and secondary heart failure. B. Adjusted length of stay for primary and secondary heart failure hospitalizations. C. Adjusted hospitalization cost for primary and secondary heart failure hospitalizations. D. Adjusted in-hospital mortality rate for primary and secondary heart failure hospitalizations. Abbreviations: HF = heart failure.
Among US HF hospitalizations from 2012 to 2018, for every primary HF hospitalization there were approximately 3.5 secondary HF hospitalizations, and the incidence of both hospitalization types increased over the study period. After adjustment, secondary HF hospitalizations had about one day longer LOS, more than $5,000 additional hospital costs, and almost twice the odds of in-hospital mortality compared with primary HF hospitalizations. Taken together, these results indicate that secondary HF hospitalizations represent a large and growing opportunity for dedicated quality improvement efforts and investigations.
A similarly higher burden of secondary HF relative to primary HF hospitalizations from 2006 to 2014 has been previously demonstrated.1 The present study extends previous analyses by including contemporary patients through 2018, and highlights the growing incidence and higher mortality rate associated with secondary HF compared with primary HF. Additionally, comparably high adverse event rates have been observed after secondary HF and primary HF hospitalizations in HFrEF patients,4 and HF patients have markedly higher risk of adverse outcomes after non-cardiac illness, such as pneumonia.5 Thus, the climbing incidence of secondary HF hospitalizations has important implications for the both inpatient and post-hospitalization care.
Several avenues of investigation could improve short- and longer-term secondary HF hospitalization outcomes. Better understanding the principal reasons for secondary HF hospitalizations may help tailor management for specific diseases in HF patients (e.g., pneumonia). Furthermore, whether in-hospital GDMT intensification during secondary HF hospitalizations mitigates risk of post-discharge adverse events should be investigated. Lastly, understanding secondary HF hospitalization care patterns and whether pre-discharge cardiology evaluation is beneficial should be evaluated.
Limitations of this analysis are inherent to the NIS database, which precludes longitudinal patient tracking or ascertainment of some patient-level information (e.g., ejection fraction). All analyses relied on International Classification of Diseases coding, and changes in coding practices over time may have influenced the results. As NIS only encompasses in-hospital care, HF care delivered at other sites including urgent care facilities would not be captured. Nevertheless, this analysis provides generalizable insights into the contemporary clinical and economic burden of primary and secondary HF hospitalizations in the U.S. These findings indicate that efforts to improve outcomes of secondary HF hospitalizations are of high importance. Future research should investigate the burden and prognostic implications of primary vs. secondary HF hospitalizations based on left ventricular ejection fraction.
Disclosures
Dr. Varshney serves on Advisory Board for Broadview Ventures, reports consulting fees from Buoy Health, Inc, and is supported by the National Heart, Lung, and Blood Institute T32 postdoctoral training grant T32HL007604.
Dr. Minhas has no disclosures. Dr. Bhatt reports speaking fees from Sanofi Pasteur and is supported by the National Heart, Lung, and Blood Institute T32 postdoctoral training grant T32HL007604. Dr. Ambrosy is supported by a Mentored Patient-Oriented Research Career Development Award (K23HL150159) through the National Heart, Lung, and Blood Institute, has received relevant research support through grants to his institution from Amarin Pharma, Inc., Abbott, and Novartis, and modest reimbursement for travel from Novartis. Dr. Fudim was supported by NHLBI K23HL151744 from the National Heart, Lung, and Blood Institute (NHLBI), the American Heart Association grant No 20IPA35310955, Mario Family Award, Duke Chair’s Award, Translating Duke Health Award, Bayer and BTG Specialty Pharmaceuticals. He receives consulting fees from Axon-Therapies, Bodyport, CVRx, Daxor, Edwards LifeSciences, Fire1, NXT Biomedical, Zoll, Viscardia. Dr. Vaduganathan receives research grants from and/or serves on advisory boards for American Regent, Amgen, AstraZeneca, Baxter Healthcare, Bayer AG, Boehringer Ingelheim, Cytokinetics, Lexicon Pharmaceuticals, and Relypsa, has participated in speaking engagements for Novartis and Roche Diagnostics, and participates on clinical endpoint committees for studies sponsored by Galmed and Novartis.
References
- 1.Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail 2018;11:e004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatt AS, Varshney AS, Nekoui M, Moscone A, Cunningham JW, Jering KS, Patel PN, Sinnenberg LE, Bernier TD, Buckley LF, Cook B, Dempsey J, Kelly J, Knowles DM, Lupi K, Malloy R, Matta LS, Rhoten MN, Sharma K, Snyder CA, Ting C, McElrath EE, Amato MG, Alobaidly M, Ulbricht CE, Choudhry NK, Adler DS, Vaduganathan M. Virtual optimization of guideline-directed medical therapy in hospitalized patients with heart failure with reduced ejection fraction: the IMPLEMENT-HF pilot study. Eur J Heart Fail 2021. 10.1002/ejhf.2163. [DOI] [PubMed] [Google Scholar]
- 3.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes 2001:1–10. [PubMed] [Google Scholar]
- 4.Desai AS, Claggett B, Pfeffer MA, Bello N, Finn PV, Granger CB, McMurray JJV, Pocock S, Swedberg K, Yusuf S, Solomon SD. Influence of hospitalization for cardiovascular versus noncardiovascular reasons on subsequent mortality in patients with chronic heart failure across the spectrum of ejection fraction. Circ Heart Fail 2014;7:895–902. [DOI] [PubMed] [Google Scholar]
- 5.Shen L, Jhund PS, Anand IS, Bhatt AS, Desai AS, Maggioni AP, Martinez FA, Pfeffer MA, Rizkala AR, Rouleau JL, Swedberg K, Vaduganathan M, Vardeny O, van Veldhuisen DJ, Zannad F, Zile MR, Packer M, Solomon SD, McMurray JJV. Incidence and outcomes of pneumonia in patients with heart failure. J Am Coll Cardiol 2021;77:1961–1973. [DOI] [PubMed] [Google Scholar]