Abstract
Fungal infection of the thyroid is rare. Most reported cases have involved Aspergillus, Coccidioides, and Candida species in the setting of disseminated disease. Infection of the thyroid with Histoplasma capsulatum is rarely reported as part of disseminated disease, even in geographic areas where histoplasmosis is endemic. We report a 52-year-old woman with a previous Hashimoto's disease and non-Hodgkin's lymphoma in which a diffuse enlarged thyroid gland with a large nodule was the only apparent locus of histoplasmosis. Fine-needle aspiration of the thyroid was an important diagnostic tool in establishing the diagnosis of histoplasmosis of the thyroid. The patient was initially treated with itraconazole (400 mg/day) for the fungal infection and six cycles of chemotherapy for the lymphoma. At a 6-month follow-up examination, the patient was doing well on suppressive therapy of itraconazole (200 mg/day), with no symptoms and with regression of the thyroid nodule and cervical adenopathy.
CASE REPORT
Infection of the thyroid gland with Histoplasma capsulatum is rarely reported, even in geographic areas in which histoplasmosis is endemic (1). In fact, there has been only one case report of disseminated histoplasmosis in which involvement of the thyroid gland was recognized at autopsy (3).
The present report describes a patient with Hashimoto's disease and non-Hodgkin's lymphoma in which H. capsulatum infection of the thyroid was the first recognized manifestation of fungal disease.
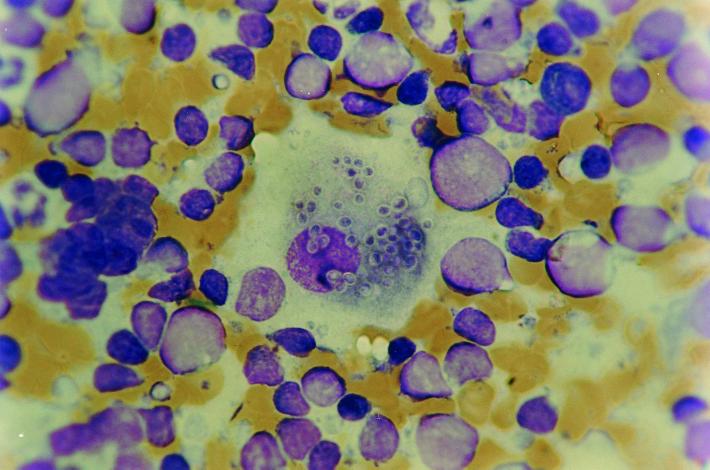
A 52-year-old, previously healthy woman was seen for evaluation of a thyroid nodule with an elevated thyroid-stimulating hormone (TSH) level of 8.5 mU/ml (normal, 0.4 to 4.5 mU/liter), thyroxine (T4), 9.3 μg/dl (normal, 4.5 to 11.0 μg/dl); and antimicrosomal antibody titer of 1:102,400. A fine-needle aspirate of the thyroid revealed innumerable lymphocytes compatible with Hashimoto's disease, and the patient was started on suppressive levothyroxine therapy (25 μg/day). Approximately 12 months later, the patient started experiencing enlargement of the thyroid gland, a 5-kg weight loss, and generalized weakness. Physical examination revealed she was well developed. Her temperature was 37.5°C. There were multiple increased cervical lymph nodes with firm consistency. The thyroid gland was soft, nontender, and diffusely enlarged (100 g), with a large nodule at the right lobe, measuring approximately 8 cm by sonography. The remaining findings of the physical examination were unremarkable. A complete blood count showed the following values: hemoglobin, 10.9 g/liter; leukocyte count, 12.4 × 109/liter; platelet count, 384 × 109/liter. Other routine laboratory tests were within normal limits. The thyroxine (T4) level was 12.4 μg/dl, and the TSH level was 7.09 mU/ml. Three sets of blood cultures were negative by the BACTEC 9240 system (Becton Dickinson, Sparks, Md.) after 6 weeks of incubation, and serology for antibodies to human immunodeficiency virus was negative. A chest X ray and computed tomography were normal. A fine-needle nodule aspirate of the thyroid nodule revealed innumerable lymphocytes and macrophages containing numerous yeast cells consistent with H. capsulatum (Fig. 1). Immunoperoxidase staining was performed as described previously (7) and identified H. capsulatum in cytological smears. Serologic testing of the patient's serum sample demonstrated immunoglobulin G-type immunodiffusion of H. capsulatum antibody to the M antigen and an H. capsulatum complement fixation antibody titer of 1:64. An open biopsy with histopathological examination and immunoperoxidase staining of the cervical lymph node established the diagnosis of intermediate-grade B-cell non-Hodgkin's lymphoma. Cytology of bone marrow aspirate was negative for malignant cells. Cultures of bone marrow aspirate for bacterial and fungal organisms were unrevealing. Staging of the lymphoma did not show any involvement outside the cervical lymph node chain. Oral itraconazole (400 mg/day) and six cycles of chemotherapy (predisone, cyclophosphamide, vincristine, and doxorubicin) were begun. At a 6-month follow-up examination, the patient was doing well on suppressive itraconazole therapy (200 mg/day), with no symptoms and with regression of the thyroid nodule and cervical adenopathy.
FIG. 1.
Thyroid aspirate with macrophage containing numerous blastoconidia of H. capsulatum. Giemsa stain was used. Original magnification, ×1,000.
Discussion.
Combined bacterial and fungal infection is an uncommon cause of thyroiditis (1). Most reported cases have involved Aspergillus species, presumably as part of disseminated disease (5). Isolated reports of thyroid involvement have been described in the setting of disseminated candidiasis, coccidioidomycosis, and pseudallescheriasis (8–10). Although H. capsulatum is mentioned as a rare cause of thyroid involvement as part of disseminated histoplasmosis (1, 3), there is no reported case of Histoplasma involvement of the thyroid as the only apparent locus of infection in the English-language literature.
Infection of the thyroid with H. capsulatum in this case was diagnosed in a patient with a previous goitrous autoimmune thyroiditis. The most common predisposing condition for thyroid infection appears to be preexisting thyroid disease (1, 11). Predisposing conditions include simple goiter, nodular goiter, adenoma, autoimmune thyroiditis, and carcinoma. A predisposing condition is noted in over two-thirds of women and one-half of men with infections of the thyroid gland (2).
Fungal infection of the thyroid usually presents with many characteristics of subacute thyroiditis (6). Histoplasmosis of the thyroid in this patient did not manifest with the characteristic of subacute thyroiditis. Gradual weight loss and increased fatigability were constitutional symptoms that could be related to either Histoplasma infection or lymphoma. Diffuse thyromegaly with a large nodule was the only clinical manifestation of histoplasmosis in this patient. The diagnosis of histoplasmosis was made unexpectedly by a routine fine-needle aspiration for evaluation of a thyroid nodule. The Histoplasma was isolated to the thyroid, and there was no symptomatic or clinical evidence of histoplasmosis in other organs. The present case appears to represent a chronic progressive disseminated form of histoplasmosis in which the course of the disease is protracted over months to years with long asymptomatic periods and terminated by reactivation of endogenous focus of latent infection and patent expression of disease in mucosa, skin, adrenals, gastrointestinal tract, meninges, and heart valves (4). People who are immunocompromised and reside or lived in regions of endemicity, such as the southern region of Brazil, are susceptible to this clinical form of histoplasmosis.
Oral itraconazole is effective for mild or moderately severe clinical forms of histoplasmosis (12). The introduction of azole agents such as itraconazole has moved the treatment of histoplasmosis from an inpatient to an outpatient setting. However, in severe histoplasmosis, amphotericin B is the preferred agent. Chronic suppressive therapy with itraconazole should be considered for those patients who might remain on immunosuppressive therapy.
In summary, we report the first case of histoplasmosis in an immunocompromised patient with a previous autoimmune thyroiditis in which the thyroid gland was the only apparent locus of infection. Fine-needle aspiration of the thyroid was an important diagnostic tool in establishing the diagnosis of histoplasmosis of the thyroid.
Acknowledgments
This work was supported in part by FIPE/HCPA, Brazil.
REFERENCES
- 1.Basgoz N, Swartz M N. Infections of the thyroid gland. In: Braverman L E, Utiger R D, editors. Werner and Ingbar's the thyroid. 7th ed. Philadelphia, Pa: Lippincott-Raven; 1996. pp. 1049–1056. [Google Scholar]
- 2.Berger A S, Zonszein J, Vilamena P, Mittman N. Infectious diseases of the thyroid gland. Rev Infect Dis. 1983;5:108–115. doi: 10.1093/clinids/5.1.108. [DOI] [PubMed] [Google Scholar]
- 3.Chan K S, Looi M, Chan S P. Disseminated histoplasmosis mimicking miliary tuberculosis: a case report. Malays J Pathol. 1993;15:155–158. [PubMed] [Google Scholar]
- 4.Goodwin R A, Shapiro J L, Thurman G H, Thurman S S, De Prez R M. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine. 1980;59:1–33. [PubMed] [Google Scholar]
- 5.Halazun J F, Anast C S, Lukens J N. Thyrotoxicosis associated with Aspergillus thyroiditis in chronic granulomatous disease. J Pediatr. 1972;80:106–108. doi: 10.1016/s0022-3476(72)80464-5. [DOI] [PubMed] [Google Scholar]
- 6.Hazard J. Thyroiditis: a review. Am J Clin Pathol. 1995;25:289–298. doi: 10.1093/ajcp/25.3.289. [DOI] [PubMed] [Google Scholar]
- 7.Klatt E C, Cosgrove M, Meyer P R. Rapid diagnosis of disseminated histoplasmosis in tissues. Arch Pathol Lab Med. 1986;11:1173–1175. [PubMed] [Google Scholar]
- 8.Robinson M F, Forgan-Smith W R, Craswell P W. Candida thyroiditis treated with 5′fluorocytosine. Aust NZ J Med. 1975;5:472–474. doi: 10.1111/j.1445-5994.1975.tb03061.x. [DOI] [PubMed] [Google Scholar]
- 9.Rosen F, Deck J H, Rewcastle N B. Allescheria boydii unique systemic dissemination to thyroid and brain. Can Med Assoc J. 1965;93:1125–1127. [PMC free article] [PubMed] [Google Scholar]
- 10.Smilack J D, Argueta R. Coccidioidal infection of the thyroid. Arch Intern Med. 1998;158:89–92. doi: 10.1001/archinte.158.1.89. [DOI] [PubMed] [Google Scholar]
- 11.Tomer Y, Davies T F. Infection, thyroid disease, and autoimmunity. Endocr Rev. 1993;14:107–120. doi: 10.1210/edrv-14-1-107. [DOI] [PubMed] [Google Scholar]
- 12.Wheat J, Sarosi G, McKinsey D, Hamill R, Bradsher R, Johnson P, Loyd J, Kauffman C. Practice guidelines for the management of patients with histoplasmosis. Clin Infect Dis. 2000;30:688–695. doi: 10.1086/313752. [DOI] [PubMed] [Google Scholar]