Abstract
Simple Summary
B-cell acute lymphoblastic leukemia (B-ALL) is characterized by an uncontrolled proliferation of blood cells in the bone marrow. A small fraction of B-ALL patients shows abnormally low chromosome numbers, defined as hypodiploidy, in leukemic cells. Hypodiploidy with less than 40 chromosomes is a rare genetic abnormality in B-ALL and is associated to an extremely poor outcome, with low survival rates both in pediatric and adult cases. In this review, we describe the main clinical and genetic features of hypodiploid B-ALL subtypes with less than 40 chromosomes, the current treatment protocols and their clinical outcomes. Additionally, we discuss the potential cellular mechanisms involved on the origin of hypodiploidy, as well as its leukemogenic impact. Studies aiming to decipher the biological mechanisms involved in hypodiploid subtypes of B-ALL with less than 40 chromosomes are crucial to improve the poor survival rates in these patients.
Abstract
Hypodiploidy with less than 40 chromosomes is a rare genetic abnormality in B-cell acute lymphoblastic leukemia (B-ALL). This condition can be classified based on modal chromosome number as low-hypodiploidy (30–39 chromosomes) and near-haploidy (24–29 chromosomes), with unique cytogenetic and mutational landscapes. Hypodiploid B-ALL with <40 chromosomes has an extremely poor outcome, with 5-year overall survival rates below 50% and 20% in childhood and adult B-ALL, respectively. Accordingly, this genetic feature represents an adverse prognostic factor in B-ALL and is associated with early relapse and therapy refractoriness. Notably, half of all patients with hypodiploid B-ALL with <40 chromosomes cases ultimately exhibit chromosome doubling of the hypodiploid clone, resulting in clones with 50–78 chromosomes. Doubled clones are often the major clones at diagnosis, leading to “masked hypodiploidy”, which is clinically challenging as patients can be erroneously classified as hyperdiploid B-ALL. Here, we summarize the main cytogenetic and molecular features of hypodiploid B-ALL subtypes, and provide a brief overview of the diagnostic methods, standard-of-care treatments and overall clinical outcome. Finally, we discuss molecular mechanisms that may underlie the origin and leukemogenic impact of hypodiploidy and may open new therapeutic avenues to improve survival rates in these patients.
Keywords: hypodiploidy, near-haploidy, B-cell acute lymphoblastic leukemia, clinical biomarkers, patient stratification
1. Introduction
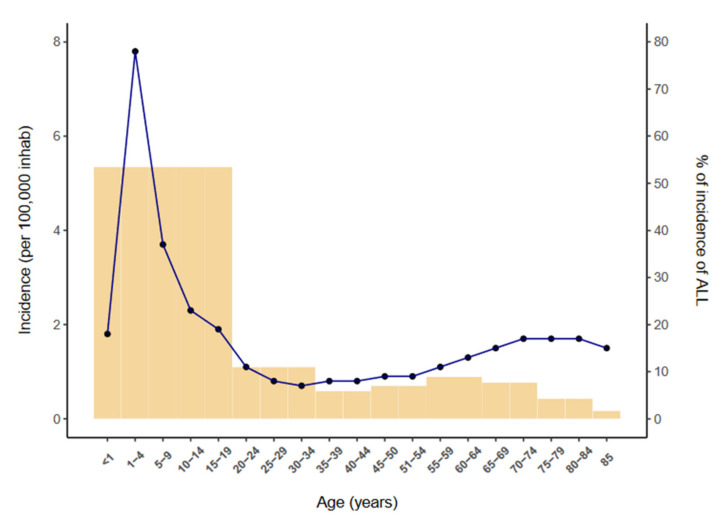
Acute lymphoblastic leukemia (ALL) is a neoplasm arising from lymphoid precursor cells and can be classified as B-ALL or T-ALL based on the immunophenotype of the neoplastic cells [1]. The global incidence of ALL is ~3 cases per 100,000 people and shows a bimodal distribution, with a predominant peak early in life (1 to 15 years) and a second, much lower, peak in older groups (>55 years) [2] (Figure 1). ALL has a slightly higher incidence in males, with a male-to-female ratio of 1.2:1 [3]. The disease is characterized by the uncontrolled proliferation of leukemic cells, which invade the bone marrow (BM), peripheral blood (PB), and other hematopoietic tissues including spleen, liver, and lymph nodes, resulting in a hematopoietic displacement which is responsible for the cytopenias frequently observed at diagnosis. ALL cells also infiltrate commonly the central nervous system (CNS).
Figure 1.
Incidence of ALL per 100,000 inhabitants by age (2014–2018) according to the SEER database [2].
B-cell precursor ALL (B-ALL) accounts for 80–85% of ALL cases and is characterized by small-medium sized leukemic blast cells staining almost always positive for the B-cell antigens CD19, cytoplasmic CD79a and CD22. Although BM and PB are involved in most cases, B-ALL occasionally presents with primary nodal or extranodal sites (B-lymphoblastic lymphoma), which predominantly affect skin, soft tissue, bone and lymph nodes [4]. Currently, B-ALL is classified by the World Health Organization as B-lymphoblastic leukemia/lymphoma with recurrent genetic abnormalities (Table 1) and B-lymphoblastic leukemia/lymphoma not otherwise specified. Among the B-ALL subtypes with recurrent genetic abnormalities, B-ALL with hypoploidy is classified as a well distinguished entity whose blasts contain <46 chromosomes (see below) [1].
Table 1.
WHO classification of precursor lymphoid neoplasms.
| Precursor Lymphoid Neoplasms |
|---|
| B-lymphoblastic leukemia/lymphoma not otherwise specified (NOS) |
B-lymphoblastic leukemia/lymphoma with recurrent genetic abnormalities
|
T-lymphoblastic leukemia/lymphoma
|
| NK-lymphoblastic leukemia/lymphoma |
There has been an extraordinary improvement in outcomes for B-ALL during the last four decades, which have been more pronounced in children than in adults (5-year overall survival [OS] of ~90% compared with ~25% for patients >50 years) [5,6]. There are several known risk factors that can help to stratify patients with B-ALL, including adverse demographic factors such as age <1 or ≥10 years [7,8]; and also adverse clinical features at diagnosis, including CNS infiltration or high white blood cell (WBC) count (>50 × 109/L) [9]. Genetics and cytogenetics also have a direct impact on prognosis [10,11]. Among other genetic features, aneuploidy—defined as the gain or loss of one or more whole chromosomes—is an important prognostic factor [12], and will be examined in this review; specifically, the favorable risk of hyperdiploidy and the adverse risk of hypoploidy. Other genetic findings with prognostic impact used to stratify patients in treatment protocols have been recently discussed elsewhere [13,14]. Finally, one important risk factor with prognostic value is the response to treatment, evaluated as the detection of minimal residual disease (MRD) at specific timepoints of treatment [15].
2. Definition of Hypodiploid B-ALL Subgroups
Hypodiploidy -the loss of one or more whole chromosomes- is a rare cytogenetic finding (≤7%) in children and adults with B-ALL and is generally an adverse prognostic marker [12,16,17,18,19,20,21,22,23,24,25,26]. Most cases (~80%) of hypodiploid B-ALL present with 45 chromosomes and are classified as near-diploid B-ALL, a clinically distinct entity characterized by rearrangements that form dicentric chromosomes but that does not have outcomes as poor as those associated with hypodiploid B-ALL [21]. Hypodiploid B-ALL is strictly defined by most studies as ≤44 chromosomes and can be further subdivided based on chromosome number as: (i) high-hypodiploid B-ALL (40–44 chromosomes), (ii) low-hypodiploid (30–39 chromosomes), and (iii) near-haploid B-ALL (24–29 chromosomes) [17,20,24,26]. Additionally, a DNA index (determined by flow-cytometry) below 0.65 and between 0.65 to 0.82 may also be used to identify near-haploidy and low-hypodiploidy, respectively, in B-ALL samples [24]. The karyotypes and clinical outcomes of high-hypodiploid B-ALL cases differ from those of near-haploid and low-hypodiploid B-ALL, which display significantly poorer clinical outcomes across all age groups [21]. In the present review, we will focus on B-ALL with hypodiploidy of <40 chromosomes—near-haploidy and low-hypodiploidy subgroups—considered as separate cytogenetic entities associated with a very poor prognosis [27].
2.1. Demographic Features of B-ALL with Hypodiploidy <40 Chromosomes
Hypodiploidy is very rare in both childhood and adult B-ALL [27]. Near-haploidy is restricted to childhood B-ALL and represents ~0.5% of all B-ALL cases [21,28], while patients with low-hypodiploidy include both children and adults with frequencies of ~0.5% and ~4%, respectively [21,24,29]. Within the pediatric population, patients with near-haploidy present at a younger age (median age at diagnosis of 6.2 years), whereas low-hypodiploidy is more common in older children, with a median age at diagnosis of 12.9 years [17,21,23,24] (Table 2). Several studies have reported a higher proportion of males in the near-haploid and low-hypodiploid groups [22,24,26]. For example, in a retrospective analysis by the Ponte di Legno Childhood ALL Working Group (PDLWG), the male-to-female ratio was 1.46 in 101 cases with near-haploidy and 1.14 in 118 cases with low-hypodiploid B-ALL [24]. However, male predominance is not consistently reported in different studies [17,21] (Table 2).
Table 2.
Clinical and biological features of patients with hypodiploid ALL.
| Study | Near-Haploid | Low-Hypodiploid | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M/F 1 | Age | WBC (×109/L) * | PreB/T Lineage | M/F 1 | Age | WBC (×109/L) * | PreB/T Lineage | |||||||||
| M 2 | <10 yo at dx * | M 2 | ≤20 | 20–50 | >50 | M 2 | <10 yo at dx * | M 2 | ≤20 | 20–50 | >50 | |||||
| SJCRH [16] | nr | 4.5 | 3 | nr | nr | nr | 11 | 1 | nr | nr | ||||||
| SJCRH-POG [17] | 0.66 | 4.7 | 70 | 13 | 70 | 10 | 20 | 8/13 | 2 | 10.5 | 22.2 | 8.4 | 66.6 | 11.1 | 22.2 | 5/1 3 |
| CCG [19] | 63 | 50 | 13 | 38 | nr | nr | nr | nr | ||||||||
| SJCRH [20] | 7.3 | 100 | 2.5 | 100 | 0 | 0 | 4/0 | nr | 0 | 8.2 | 83.3 | 0 | 16.6 | 5/1 | ||
| MRC [21] | 0.75 | 7.4 | 64.3 | 67.3 | 38.5 | 30.8 | 30.8 | 13/0 3 | 1.1 | 21.6 | 7.1 | 11 | 85.7 | 7.1 | 7.1 | 12/0 3,4 |
| Inc study [22] | 1 | 69.6 | 39.1 | 41.3 | 19.6 | nr | 2.25 | 19.2 | 73 | 19.2 | 7.7 | nr | ||||
| SJTTS 15&16 [23] | 3.6 | 8.1 | 13.9 | 5.6 | ||||||||||||
| PDLWG [24] | 1.46 | 6.2 | 73 | 21.8 | 49 | 20 | 31 | 99/1 | 1.14 | 12.9 | 26 | 7 | 85 | 10 | 4 | 99/1 |
| Japanese study [25] | nr | nr | nr | nr | nr | nr | nr | 3/0 | nr | nr | nr | nr | nr | nr | nr | 3/0 |
* Percentage of patients. 1 Male-to-female-ratio. 2 Median. 3 data not available from 4 patients in the SJCRH-PG study and in 1 patient in the MRC study. 4 one patient reported as “null” immunophenotype. Abbreviations: CCG, Children Cancer Group; CIBMTR, Centre for International Blood and Marrow Transplant Research; CNS, central nervous system; LH; low-hypodiploid; MRC, Medical Research Council; na, not applicable; NH, near-haploid; nr, not reported; PDLWG, Ponte di Legno childhood ALL Working group; POG, Pediatric Oncology Group; preB, B-cell precursor; SJCRH, Saint Jude Children’s Research Hospital; SJTTS, Saint Jude Total Therapy Study; WBC, white blood cell count at presentation.
2.2. Clinical and Biological Features of B-ALL with Hypodiploidy <40 Chromosomes
Generally, patients with hypodiploid B-ALL present with a lower diagnostic WBC than patients with non-hypodiploid B-ALL [16]; however, some studies have reported a higher WBC in the near-haploid group [11,21,24]. The aforementioned PDLWG study [24] found a median WBC at presentation of 21.8 × 109/L in the near-haploid group against 7 × 109/L in the low-hypodiploid group. In addition, up to 49% of patients with a near-haploid karyotype presented with ≤20 × 109/L compared with 85% in the low-hypodiploid group, whereas 31% in the near-haploid group presented with >50 × 109/L WBC compared with only 4% in the low-hypodiploid group. These findings are in line with previous reports [21,22,24] (Table 2).
Regarding cell morphology, French-American-British (FAB) L2/L1 or L2 subtypes were reported to be more frequent at presentation in patients with hypodiploid B-ALL. Indeed, up to 50% of near-haploid cases were non-L1 FAB subtype and 25% were L2 subtype in a series reported by the Children Cancer Group (CCG) [16,19]. Patients with B-ALL with hypodiploidy show a B-cell precursor immunophenotype, with positivity for CD19, CD34, CD22, cCD79a and TdT [22,27]. Near-haploid ALL is generally also positive for CD10, whereas low-hypodiploid ALL may exhibit a more immature B-cell precursor immunophenotype, lacking CD10 in a substantial proportion of cases, consistent with a pro-B ALL phenotype [30]. Additionally, a very small proportion of children with hypodiploid ALL present with a T-ALL immunophenotype, usually with positivity for TdT and expressing the T-cell specific markets CD1a, CD2, CD3, CD5, and CD7 [27,31,32]. In a larger series presented by the PDLWG, Nachman et al. and the UK Medical Research Council, only 1% of the total cases with hypodiploidy <40 chromosomes showed a T-cell immunophenotype (Table 2), whereas 11–15% of high-hypodiploid cases exhibited a T-ALL immunophenotype [21,22,24].
2.3. Extramedullary Involvement at Presentation
CNS involvement, which is defined as the presence of blasts in a sample of cerebrospinal fluid with ≥5 leukocytes/µL and <10 erythrocytes/µL or the presence of cranial nerve palsies (CNS3) [33], is rare at diagnosis and was recorded in only one out of 115 and 97 cases (1%) of near-haploid and low-hypodiploid ALL, respectively, in the PDLWG study [24,26]. Other frequent leukemic extramedullary involvements at diagnosis of near-haploid and low-hypodiploid B-ALL is at the spleen and liver, presenting as splenomegaly in 44% and 28% of cases, and hepatomegaly in 43% and 35%, respectively [24,26]. By contrast, mediastinal mass and lymphadenopathy is less frequent, with 7% and 13% and 30% and 14% of cases with near-haploid ALL and low-hypodiploid ALL, respectively [24]. Testicular disease at diagnosis is also rare in both types, with no reported cases in the AALL03B1 study and only 2 of 46 cases (4%) of near-haploid B-ALL in the PDLWG study [24]. Taking these findings together, it seems clear that most of the clinical and biological features in patients with near-haploid and low-hypodiploid B-ALL do not seem to be predictive of poor outcome.
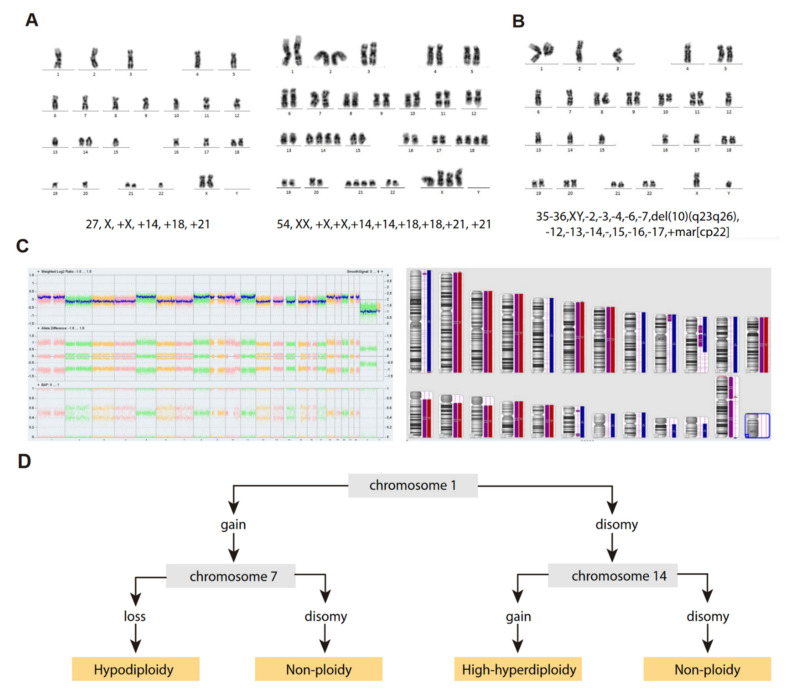
3. Cytogenetic Characterization of B-ALL with Hypodiploidy <40 Chromosomes
Although traditionally defined as the loss of one or more chromosomes in a cell [34], hypodiploidy has been classified according to diverse criteria in different studies to define different hypodiploid B-ALL subtypes (Table 3), and a clear distinction between those cases with <40 chromosomes and those with 40–45 chromosomes has become generally accepted based on the evident differences in treatment response [21,35]. Hypodiploid cases with <40 chromosomes can be further subdivided into two groups based on the bimodal distribution of chromosome numbers: (i) near-haploidy, with 24–29 chromosomes (Figure 2A), and (ii) low-hypodiploidy, with 30–39 chromosomes (Figure 2B,C) [27] (Table 3). Although the modal number of chromosomes is variable, the most recurrent modal numbers are 25–28 for near-haploid and 33–39 for low-hypodiploid B-ALL [36]. Based on conventional chromosome banding analyses, hypodiploidy with <40 chromosomes shows a non-random loss of chromosomes: in near-haploid B-ALL, retained disomies generally comprise chromosomes 8, 10, 14, 18, 21, X and Y [21,22,30,37] whereas in low-hypodiploid cases, retained disomies are more variable and typically comprise chromosomes 1, 5, 6, 8, 10, 11, 14, 18, 19, 21, 22, X and Y, with retained disomies for chromosomes 1, 6, 11 and 18 being the most frequently observed. The most typically lost chromosomes are chromosome 3, 7, 9, 15, 16 and 17 [21,22,30,38,39] (Table 3). The non-random retention of chromosomes suggests that these chromosomes may harbor specific genes that enhance the oncogenic potential of leukemic cells.
Table 3.
Cytogenetic characteristics of B-ALL patients with <40 chromosomes.
| Age (Years) | Near-Haploid | Low-Hypodiploid | Reference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MN | Retained chr | Lost chr | Doubled Clone | Frequency | MN | Retained chr | Lost chr | Doubled Clone | Frequency | ||
| 1–18 | 25–28 | 8, 10, 14, 18, 21 and sex chr. | yes | 0.0046 | 30–40 | 1, 19, 21, 22 and sex chr. | 3, 7, 13, 16, 17 | yes | 0.41 | [17] | |
| 1–10 | 24–28 | 8, 10, 14, 18, 21 and sex chr. | 7, 13, 14, 20, X | yes | 0.0042 | 33–44 | 7, 13, 14, 20, X | nr | 0.79 | [19] | |
| 2–15 | 23–29 | 14, 18, 21 and sex chr. | yes | 0.0039 | 33–39 | 1, 2, 5, 6, 8, 10, 11,12, 14, 18, 19, 21, 22 and the sex chr. | 7, 17 | yes | 0.39 | [21] | |
| 15–84 | - | - | - | - | - | 30–39 | 1, 5, 6, 8, 10, 11, 15, 18, 19, 21, 22, X, Y | 3, 7, 15, 16, 17 | 66 to 78 chr | 0.05 | [31] |
| 15–55 | - | - | - | - | - | 33–39 | nr | nr | nr | 0.0008 | [21] |
| 15–55/>55 | <30 | 0.0016 | 32–39 | 1 | 2, 3, 7, 9, 13, 15, 16, 17, 20, 4 | 64–74 | 3.85% | [40] | |||
| 1–9/>10 | 24–29 | 14, 18, 21 and sex chr. | nr | nr | nr | 33–39 | nrec | 3, 7, 16, 17 | nr | nr | [10] |
| <31 | 24–31 | 14, 18, 21 and sex chr. | nr | yes | 0.008 | 32–39 | 1, 8, 10, 11, 18, 19, 21 and 22 | nr | nr | 0.0064 | [41] |
Abbreviations: chr, chromosomes; MN, modal numbers; nr, non-reported; nrec, non-recurrent.
Figure 2.
Cytogenetic characterization of B-ALL with <40 chromosomes. (A) G-banded karyotype of near-haploid B-ALL leukemic cells. Left panel, near-haploid clone. Right panel, chromosomally-doubled clone of the same patient. (B) G-banded karyotype of low-hypodiploid B-ALL leukemic cells. Karyotype formulas are indicated below. (C) SNP-array karyogram obtained for the low-hypodiploid B-ALL patient in B. Right panel, blue bars indicate chromosomal disomies of the duplicated/near-triploid clone, red bars indicate chromosomal losses, and purple bars indicate absence of heterozygosity. Left panel, Log2 ratio plot detailing whole chromosomal view for each chromosome, the figure demonstrates pattern of low-hypodiploidy where chromosomes with the lowest Log2 ratio represent the monosomies and a partial deletion of chromosome 10. Allele difference plot and B-allele frequency plot (BAF; BB, AB and AA alleles) indicates copy-neutral loss of heterozygosity. (D) Algorithm proposed by Creasey et al. [39] to distinguish hypodiploid with <40 chromosomes and high-hyperdiploid B-ALL cases based on specific chromosomal gains.
Structural chromosome aberrations (i.e., chromosomal translocations) in hypodiploidy of <40 chromosomes are extremely rare, especially in near-haploid B-ALL [21,22,38,42], suggesting that massive chromosomal loss alone may be sufficient for leukemogenesis. Patients with low-hypodiploid B-ALL show some additional alterations, albeit few, in the karyotype beyond monosomies (Figure 2B,C). It has been reported that pediatric patients with B-ALL with <36 chromosomes may show additional structural chromosome aberrations more frequently when compared with those with ≥36 [22]. It would be interesting to learn whether pediatric patients with additional structural alterations are also older than those without them, which would be consistent with different reports on adult B-ALL showing structural chromosome aberrations, especially unbalanced translocations and losses of chromosome arms, in 50% of low-hypodiploid cases [35,38].
“Masked Hypodiploidy”: A Clinical Challenge
A feature common to patients with near-haploid and low-hypodiploid B-ALL is the presence of a clone with an exact or near-exact chromosome doubling of the hypodiploid clone, resulting in a clone with a modal chromosome number of 50–78, in the high-hyperdiploid or triploid range [17,21,22,41] (Table 3) (Figure 2A). Notably, some chromosomes are preferentially lost after chromosome doubling; typically, chromosomes 2, 5, 6, 10, 14 and 22 [38]. The presence of hypodiploid doubled clones has been observed in ~60–65% of patients with near-haploid and low-hypodiploid B-ALL in different studies, and is commonly observed as a mosaic with both hypodiploid and hyperdiploid (doubled) clones visible by standard cytogenetics, fluorescence in situ hybridization (FISH) or flow cytometry analysis of DNA content [21,41,43]. Furthermore, the doubled clone may be the only one detected at diagnosis, leading to the manifestation known as “masked hypodiploidy”, which is clinically challenging since patients can be erroneously classified and treated for high-hyperdiploid B-ALL while being at higher risk of treatment failure. It has been reported that there is no difference in clinical outcome for patients with “masked hypodiploidy”, those who are mosaic for a doubled clone and a hypodiploid clone, and those who have only a hypodiploid clone [22,35,41]. In addition, the hypodiploid clone tends to be quantitatively more frequent at relapse, suggesting that the actual hypodiploid clones may be more chemoresistant than their hyperdiploid (doubled) counterparts [20,44].
There is evidence to suggest that chromosomal doubling arises by endoreduplication [17]: for instance, (i) the hyperdiploid clone is an exact duplication of the near-haploid or low-hypodiploid clone; (ii) in rare cases, the structural chromosomal abnormalities are also shared in paired chromosomes; and (iii) hyperdiploid cell lines have been established in culture from near-haploid B-ALL patient samples [45,46]. However, studies aiming to elucidate the molecular mechanism(s) leading to the chromosomal doubling have not been performed to date.
Whole-genome doubling (WGD) is a common phenomenon in nature that generates cells referred to as “polyploid”, containing multiple copies of the complete set of chromosomes [47]. Indeed, polyploidy has been reported to be indispensable for normal development and organ formation across various organisms, from fungi to humans [47,48], and has more recently been associated with wound healing and tissue homeostasis [48]. Additionally, polyploidization has been implicated in early carcinogenesis and neoplastic progression, as polyploid cells have been reported to be more permissive to aneuploidy through their ability to buffer deleterious mutations that affect cellular fitness [49,50]. In this line, it is tempting to speculate that WGD is even more relevant in near-haploid and low-hypodiploid cellular backgrounds, as it generates chromosomally-doubled clones with presumably lower cell-fitness costs and higher adaptation capacity than their hypodiploid counterparts. WGD arises as a consequence of alternative cell cycle programs referred to as endoreduplication or endocycles, through which cells successively duplicate genomic DNA without segregating their chromosomes during mitosis [47]. Only the most extreme abbreviations of the mitotic phase are correctly referred to as endoreduplication. The cell cycles that include some mitotic processes, such as chromosome condensation, nuclear envelope breakdown and spindle formation, are referred to as “endomitosis”, which abort mitosis mostly during metaphase or anaphase and lack cytokinesis [47]. These cases are associated with mitotic defects leading to mitotic slippage. In both scenarios, the result is either a cell that maintains separate nuclei, generating multinucleate cells, or a cell with an enlarged single nucleus. Endoreduplication cycles use much of the same machinery that regulates the transition from G1 to S phase in normal “mitotic cell cycles”. To convert the mitotic cell cycle into an endoreduplication cycle, the cell cycle must be altered in two essential ways. On the one hand, by bypassing the central processes of mitosis, chromosome segregation and cytokinesis, without blocking DNA replication. This is accomplished in plants and animal cells by downregulating the cyclin-dependent kinases (CDKs) that drive G2-to-M phase progression, while allowing continuous activity of the CDKs that drive G1-to-S progression. On the other hand, periodic inactivation of CDKs involved in G1-to-S phase transition to enable a G1-like gap with low S-phase-specific CDK activity during which pre-replication complexes can be reassembled [47,48]. The precise mechanism underlying WGD in near-haploid and low-hypodiploid B-ALL is currently not known, but as this phenomenon is very common and exclusive of these subtypes of B-ALL, it could be hypothesized that it has an important role on the development of these subtypes of ALL.
4. Molecular Characterization of Hypodiploid B-ALL with <40 Chromosomes
In addition to the massive genetic losses, both near-haploid and low-hypodiploid B-ALL show characteristic and differentiated gene expression profiles, in addition to specific mutational and focal copy-number alteration (CNA) landscapes, those excluding whole chromosome losses [30]. Notably, near-haploid and low-hypodiploid B-ALL presenting with or without doubled clones show similar transcriptional and mutational profiles [30], most likely explaining the similar clinical outcomes between patients with and without chromosomal doubling [17,22,41].
4.1. Near-Haploid B-ALL
The mutational landscape of near-haploid B-ALL is characterized mainly by the presence of alterations involving receptor tyrosine kinases and activating RAS signaling alterations, with >70% of patients showing mutations or focal CNA involving genes in these pathways (Table 4) [30,38,51]. The different RAS signaling alterations have been shown to be mutually exclusive, suggesting that, in contrast to the convergent evolution for RAS mutations observed in infants with MLL-rearranged B-ALL [52], a single alteration in the pathway is sufficient to maintain constitutive RAS-pathway activation. Focal deletions or point mutations in NF1 gene are the most recurrent genetic alterations of near-haploid B-ALL (≥44% of patients) [23,30,53]. NF1 encodes a RAS–GTPase-activating protein that negatively regulates Ras signaling. Deletions affecting this gene are intragenic and involve exons 15–35 in the majority of cases, most likely due to illegitimate recombinase activating gene (RAG) activity [30]. Other recurrently mutated RAS pathway genes in near-haploid B-ALL are NRAS (15% of patients), FLT3 (9% of patients), KRAS (3% of patients) and PTPN11 (1.5% of patients) [30,38,51]. Some of these mutations have been described in patients diagnosed with Noonan syndrome, such as the PTPN11 Gly503Arg substitution, and have been also described in remission samples or in T-cell lymphocytes, such as NRAS Gly12Ser [30], suggesting that the single-nucleotide variants (SNVs) are germline SNVs and that near-haploidy may be a manifestation of this cancer-predisposing syndrome in some instances. Additionally, alterations in PAG1 (mostly deletions) have been reported in 10% of patients with near-haploid B-ALL [23,30]. Most of the deletions were homozygous and affected the upstream region and first exon of the gene, leading to a complete loss of gene expression [30]. PAG1 encodes for a transmembrane adaptor protein that binds to the tyrosine kinase CSK protein, which negatively regulates SRC-family kinases involved in both Ras and B-cell receptor signaling pathways. Importantly, PAG1 deletions together with positive MRD status have been associated with poorer outcomes and increased incidence of relapse in hypodiploid ALL [30]. Other recurrent focal CNAs in near-haploid B-ALL include CDKN2A/B at 9p21.3 (22% of patients), a histone cluster at 6p22 (19% of patients), IKZF3/Aiolos at 17q12 (13% of patients), RB1 at 13q14.2 (9% of patients) and PAX5 at 9p13.2 (7% of patients) [30]. As with other B-ALL subtypes, patients with near-haploid B-ALL have recurrent disruption, by deletion, insertion-deletions or point mutations, of the lysine acetyltransferase gene CREBBP (32% of patients) [30]. CREBBP mediates the expression of glucocorticoid-responsive genes and may play an active role in response to glucocorticoids, suggesting that patients harboring CREBBP alterations may be more prone to therapy failure and relapse [54]. Point mutations in other histone-modifier genes, such as EP300 and EZH2, are also observed in near-haploid B-ALL albeit at lower frequencies (<5% of patients). Of note, alterations involving epigenetic modifiers are more frequently observed in relapsed B-ALL than at diagnosis, highlighting their role in leukemia progression and clonal evolution.
Table 4.
Molecular characteristics of hypodiploid <40 chromosomes B-ALL (Adapted from Holmfelt et al., 2013 [30]).
| Genes | Cellular Pathway | Near-Haploid B-ALL | Low-Hypodiploid B-ALL | ||||
|---|---|---|---|---|---|---|---|
| Mutation | Focal Deletion | Focal DEL + Mut | Mutation | Focal Deletion | Focal DEL + Mut | ||
| NF1 | RTK/RAS pathway | 11/68 (16%) | 16/68 (24%) | 3/68 (4%) | 0 | 2/34 (6%) | 0 |
| KRAS | 2/68 (3%) | 0 | 0 | 0 | 0 | 0 | |
| NRAS | 10/68 (15%) | 0 | 0 | 0 | 0 | 0 | |
| PTPN11 | 1/68 (1%) | 0 | 0 | 0 | 0 | 0 | |
| FLT3 | 6/68 (9%) | 0 | 0 | 0 | 0 | 0 | |
| CRLF2 | 0 | 2/68 (3%) * | 0 | 0 | 0 | 0 | |
| MAPK1 | 1/68 (1%) | 0 | 0 | 0 | 0 | 0 | |
| GAB2 | 0 | 2/68 (3%) | 0 | 0 | 1/34 (3%) | 0 | |
| EPHA7 | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 | |
| RASA2 | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 | |
| IKZF1 | B-cell development | 0 | 3/68 (4%) | 0 | 0 | 1/34 (3%) | 0 |
| IKZF2 | 1/68 (1%) | 0 | 0 | 0 | 18/34 (53%) | 0 | |
| IKZF3 | 1/68 (1%) | 8/68 (12%) | 0 | 0 | 1/34 (3%) | 0 | |
| PAX5 | 1/68 (1%) | 4/68 (6%) | 0 | 0 | 2/34 (6%) | 0 | |
| EBF1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| VPREB1 | 0 | 3/68 (4%) | 0 | 0 | 2/34 (6%) | 0 | |
| CDKN2A/B | Cell cycle and apoptosis | 0 | 15/68 (22%) | 0 | 0 | 8/34 (24%) | 0 |
| TP53 | 2/68 (3%) | 0 | 0 | 31/34 (91%) | 0 | 0 | |
| RB1 | 2/68 (3%) | 3/68 (4%) | 1/68 (1%) | 5/34 (15%) | 8/34 (24%) | 0 | |
| ETV6 | Hematopoiesis | 1/68 (1%) | 3/68 (4%) | 1/68 (1%) | 0 | 0 | 0 |
| Histone cluster (6p22) | Histone-related | 0 | 13/68 (19%) | 0 | 0 | 1/34 (3%) | 0 |
| ARID1B | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 | |
| PAG1 | BCR signalling | 1/68 (1%) | 6/68 (9%) | 0 | 0 | 1/34 (3%) | 0 |
| ARPP21 | Calmodulin signalling | 0 | 1/68 (1%) | 0 | 0 | 0 | 0 |
| SLX4IP (C20orf194) | Telomere length maintenance | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 |
| CUL5 | Ubiquitin pathway | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 |
| FAM53B | Wnt signalling | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 |
| PDS5B (APRIN) | Cohesin complex | 0 | 2/68 (3%) | 0 | 0 | 0 | 0 |
| ANKRD11 | Cell adhesion | 0 | 0 | 0 | 0 | 2/34 (6%) | 0 |
| DMD | 0 | 0 | 0 | 0 | 1/34 (3%) | 0 | |
* one patient encoding P2RY8-CRLF2.
4.2. Low-Hypodiploid B-ALL
The genetic hallmark of low-hypodiploid B-ALL is TP53 mutations, which are observed in >90% of patients in both childhood and adult low-hypodiploid B-ALL (Table 4) [30,38,51,55]. Most are missense mutations in exons 5–8, affecting the DNA-binding domain and the nuclear localization sequence [30,38]. Other characteristic and recurrent genetic alterations in the low-hypodiploid B-ALL subtype are RB1 mutations or deletions (41% of cases), deletions of IKZF2/Helios (53% of cases) and deletions of CDKN2A/B genes (22% of cases) [30,38]. Mutations of TP53 are found in homozygosity in virtually all low-hypodiploid B-ALL cases due to the very recurrent loss of chromosome 17. TP53 mutations are frequently found in non-tumor hematopoietic cells in 50% of the cases of childhood low-hypodiploid B-ALL [38,51], suggesting that these cases may be a manifestation of Li-Fraumeni syndrome or other germline TP53 cancer-predisposing mutations [30,55,56]. Accordingly, genetic counseling is recommended for children with low-hypodiploid B-ALL carrying TP53 mutations, and their relatives [57,58]. In contrast to childhood cases, TP53 mutations in low-hypodiploid adult B-ALL are somatic, are not found in healthy hematopoietic cells, and not detectable in remission samples [30,38].
Focal deletions involving lymphocyte development genes, such as IKZF1, EBF1 or LEF1, are not particularly frequent in low-hypodiploid B-ALL samples. Instead, IKZF2/Helios loss at 2q34 is the most recurrent alteration involving genes associated with B-cell differentiation (53% in children and 36% in adults), being much more frequently observed in low-hypodiploid B-ALL than in any other B-ALL subtype, including near-haploid ALL (Table 4). IKZF2/Helios is highly expressed in common lymphoid progenitors and in pre-pro-B progenitor cells, which is consistent with the immunophenotype observed in low-hypodiploid B-ALL of lower frequencies of antigen-receptor rearrangements, CD19 and CD10 [30,59]. These findings reinforce the hypothesis that low-hypodiploidy targets a more immature lymphoid progenitor (pro-B stage or earlier) than other B-ALL subtypes with a pre-B immunophenotype. Indeed, in one study patients with IKZF2/Helios deletions had a poorer outcome than patients with wild-type IKZF2/Helios in an univariate analysis [30]. Beyond lymphocyte development, alterations of cell cycle regulators are also frequently observed in both childhood and adult low-hypodiploid B-ALL. As discussed earlier, alterations in RB1 are observed in 41% and 19% of childhood and adult patients, respectively. Additionally, CDKN2A/B mutations are observed in 22% of both childhood and adult low-hypodiploid B-ALL samples, and are often mutually exclusive with RB1 mutations [58]. The finding that TP53 is ubiquitously perturbed in low-hypodiploid B-ALL suggests that mutations in an additional member of the TP53/RB1 pathway (either RB1 or CDKN2A/B) would be sufficient to deregulate cell proliferation in these cases. Furthermore, mutations in histone-modifier genes, such as CREBBP, are detected in 60% of patients with low-hypodiploid B-ALL [30]. Strikingly, while patients with low-hypodiploid B-ALL do not show recurrent mutations in genes associated with RAS pathway activation, as do patients with near-haploid B-ALL, transcriptomic analyses of pathway activation in low-hypodiploid B-ALL revealed constitutive signaling of RAS and PI3K pathways [30].
A recent study by the Japan Association Childhood Leukemia Study Group (JACLS) reported a high frequency of mutations in CIC in both low-hypodiploid and near-haploid B-ALL, present in 5 of 9 patients [53]. CIC is a member of the high mobility group (HMG)-box superfamily of transcriptional repressors and is recurrently mutated in oligodendrogliomas and in round cell sarcomas. However, the germline status of CIC in B-ALL with hypodiploidy of <40 chromosomes is unknown and raises the question of whether it could be more prevalent in Asian ancestors than in non-Asian populations [53].
4.3. Proper Identification of Hypodiploid B-ALL with <40 Chromosomes
As previously mentioned, “masked hypodiploidy” represents an important diagnostic challenge, as it may be mis-diagnosed with high-hyperdiploidy of 51–65 chromosomes (Figure 2A). Conventional cytogenetic G-banding analysis provides the modal number of chromosomes, which is essential for the differentiation between these cytogenetic groups with <40 chromosomes, high-hyperdiploid B-ALL and, especially, for those B-ALL cases presenting with >65 chromosomes (near-triploidy), which should always be considered as doubled clones from a low-hypodiploid B-ALL. Cases between 51 and 65 chromosomes, in the range of the high-hyperdiploidy and masked near-haploidy, are especially difficult to define and a detailed analysis of the gained chromosomes is crucial to distinguish between the two B-ALL entities. The major cytogenetic characteristic of masked near-haploid B-ALL is the presence of mainly tetrasomies, which is in contrast to high-hyperdiploidy, which mainly shows trisomies (with the exception of chromosome 21). Accordingly, the presence of tetrasomies other than tetrasomy of chromosome 21 might suggest a masked hypodiploid clone. Moreover, the subsequent loss of some chromosomes is very frequently observed after chromosome doubling in cases of B-ALL with hypodiploidy of <40 chromosomes, suggesting certain levels of chromosome instability and, therefore, not all gained chromosomes are tetrasomic in the karyotypes of masked near-haploid samples [38].
Complementary techniques may be used when there is a suspicion of masked hypodiploidy, including interphase FISH or flow-cytometry analyses of DNA index. These techniques allow scoring a higher number of cells in the samples and may facilitate the detection of hypodiploid clones that were not detectable by conventional cytogenetics. Likewise, single nucleotide polymorphism (SNP)-arrays have emerged as a very reliable tool to identify masked hypodiploid clones, especially their capacity to detect loss of heterozygosity (LOH). Indeed, the presence of LOH in most chromosomes, especially those typically lost in the original hypodiploid clones (Table 3), is defining the near-haploid and low-hypodiploid entities. Some authors have recently provided simple and helpful algorithms for proper discrimination between masked hypodiploidy from high-hyperdiploid B-ALL using SNP-arrays and focusing on specific chromosome gains, such as chromosomes 1, 7 and 14 (Figure 2D) [39].
5. Etiology of Hypodiploidy in B-ALL
No preclinical models of near-haploid or low-hypodiploid B-ALL subtypes are currently available, preventing the direct study of the biological causes and the pathogenic consequences of hypodiploidy in B-ALL. Indeed, most studies describing hypodiploid subtypes in B-ALL are clinical reports, patient sample analyses and retrospective analyses of clinical outcomes. Accordingly, there is only circumstantial evidence for the cellular mechanisms leading to hypodiploidy and its pathogenic consequences. Genomic analyses of these subtypes have been difficult given the limited number of cases; however, a study on a small cohort of 8 near-haploid and 4 low-hypodiploid B-ALL samples suggested that the massive loss of chromosomes is the primary oncogenic event, with other oncogenic insults occurring after hypodiploidy [37]. This is consistent with similar analyses in high-hyperdiploid B-ALL cases, the most frequent aneuploid entity in B-ALL, indicating that chromosome gains were the primary oncogenic event [60,61]. Thus, similar pathogenic mechanisms involving gross aneuploidies may be shared in these B-ALL subtypes. Furthermore, the genomic landscape of near-haploid and low-hypodiploid B-ALL subtypes, as well as that of high-hyperdiploid subtypes, is characterized by aneuploidy and subtype-specific mutations (see above), with significant fewer microdeletions and structural chromosomal rearrangements in comparison with other cytogenetic subtypes containing structural chromosomal reorganizations [30,60]. Collectively, these data strongly suggest that hypodiploidy has a direct impact on cell transformation and leukemogenesis rather than being solely a passenger event. The fact that severe hypodiploidy is observed in a wide spectrum of neoplasms further indicates that it is indeed a major contributor of tumorigenesis [62].
Although the functional impact of extreme hypodiploidy on leukemia initiation is poorly understood, a common assumption is that the widespread LOH resulting from hypodiploidy leads to the unmasking of recessive alleles or to gene-dosage imbalances affecting oncogenes, tumor-suppressor genes, and also protein imbalances affecting different aspects of cell physiology, proliferation and/or survival [30,37,51]. Indeed, loss-of-function mutations of TP53 are a hallmark of both childhood and adult low-hypodiploid B-ALL [30], suggesting that alterations in this gene are an important event in the pathogenesis of this B-ALL subtype. Alternative mechanisms for tumor suppressor pathway inactivation may be involved in the pathogenesis of near-haploid B-ALL; for instance, microdeletions of CDKN2A/B loci on chromosome 9, typically monosomic in near-haploid B-ALL, are common in this hypodiploid subtype [30]. These proteins are involved in the control of the tumor-suppressor RB1 and their inactivation leads to a dysregulation of the G1-to-S checkpoint leading to uncontrolled proliferation [30,51].
Remarkably, the pattern of chromosomal retention in near-haploid B-ALL is similar to the pattern of commonly gained chromosomes in the high-hyperdiploid group [17,30]. Thus, retention of both homologs of specific chromosomes, especially 14, 18, 21 and X, may play an important role in leukemogenesis in these cases. Elucidating the role and cooperativity of the genes on these chromosomes, and their contribution to different cellular pathways, should shed new light on the pathogenic mechanisms resulting from hypodiploidy in B-ALL. In particular, the contribution of alterations in the RAS signaling pathway, Ikaros-family alterations and/or TP53 alterations in leukemogenesis are a subject of active current investigation [58].
6. Origin of Near-Haploidy and Low-Hypodiploidy
While the near-haploid and low-hypodiploid chromosomal patterns have been recognized for many years [16], the factors driving the generation of these aneuploidies and their associated genomic alterations remain poorly understood. They may originate through successive loss of chromosomes or by a single erroneous mitosis event in an early hematopoietic stem/progenitor cell. The latter hypothesis is currently the most accepted owing to the bimodal distribution of chromosome numbers reported in the literature for these hypodiploid B-ALL subtypes [37]. Multipolar mitosis or an abnormal partial mitotic pairing of homologous chromosomes appear to be the most feasible mechanisms underlying hypodiploidy [17,62], but no experimental evidence has been provided to support this hypothesis. Remarkably, high-resolution microscopic analyses of dividing primary hypodiploid B-ALL cells stained with antibodies that recognize different cytoskeleton structures revealed an increase in the frequency of multipolar spindles when compared with non-hypodiploid B-ALL cells (data not previously published) [63], suggesting that multipolar spindles could indeed be a crucial cellular mechanism leading to hypodiploidy. However, whether these multipolar spindles are the cause or a consequence of the chromosome losses remains an open question.
Given that the immunophenotype of both near-haploid and low hypodiploid B-ALL is consistent with that of a common pre-B or pro-B leukemia, respectively [17,30], it is likely that hypodiploidy arises in a similar hematopoietic progenitor as most B-ALLs. Notably, pre-leukemic clones with different chromosome rearrangements and high-hyperdiploidy have been observed in cord blood samples and in neonatal heel prick tests from patients that later develop childhood B-ALL [64]. This finding suggests that the primary genetic abnormalities arise in utero during fetal hematopoiesis and act as pre-leukemic initiating events that remain clinically silent upon the acquisition of secondary cooperating genetic alterations, which are necessary to promote leukemia development [65]. Of note, although no direct evidence has been provided for near-haploid and low-hypodiploid B-ALL subtypes, it is tempting to speculate that hypodiploidy in childhood B-ALL also arises in utero as a consequence of an aberrant mitosis event in early hematopoietic progenitors. The pathogenic mechanisms of extreme hypodiploidy and their contribution to leukemogenesis are the subject of investigation, as the identification of novel therapeutic targets are crucial for developing new treatments to improve the dismal outcome of these rare subtypes of B-ALL.
7. Outcome and Treatment Strategies for B-ALL with Hypodiploidies <40 Chromosomes
7.1. Event-Free Survival and Overall Survival Rates
Patients with hypodiploid B-ALL have an overall very poor clinical outcome, particularly in those cases with <40 chromosomes [17]. While the survival rates are increasingly dismal with decreasing modal chromosome numbers, the outcome of patients with either near-haploidy and low-hypodiploidy do not significantly differ, being similarly poor in both groups with modal numbers below 40 chromosomes [20,21,24]. The poor prognostic impact conferred by hypodiploidy with <40 chromosomes is maintained in multivariate analyses after adjustment for important risk factors including age, WBC count, and Philadelphia/t(9;22) status [19]. Indeed, the MRC UK-ALL trials of childhood B-ALL cases reported 3-year event-free survival (EFS) rates of 29% versus 65% in hypodiploidy below and above 40 chromosomes, respectively [21]. Its prognosis in adults remains extremely poor, with 5-year EFS rates ~20%, despite stratification by high-risk treatment protocols [27]. Importantly, the poor outcome and low EFS rates of B-ALL with hypodiploidy with <40 chromosomes has been consistently reported by different studies (Table 5).
Table 5.
Event-free survival reported for patients with hypodiploid B-ALL by several relevant studies. Colored cells indicate statistical comparisons (blue, between chromosome numbers; orange, between other variables).
| Study group | Years | Outcome variable | MN | Other variables | n | Mean (%) | p-value | Reference |
|---|---|---|---|---|---|---|---|---|
| Total Therapy Studies IX–XI Pediatric Oncology Group (POG) |
1979–1988 1986-1988 |
3-year-DFS | <30 chr 30–40 chr 41–44 chr |
109 8 |
40 33 37 |
[17] | ||
| Children’s Cancer Group (CCG) | 1988–1995 | 6-year-EFS | 33–34 chr 29–32 chr 24–28 chr |
15 | 40 | [19] | ||
| 30–40 chr | 0 | NA | ||||||
| 41–44 chr | 8 | 25 | ||||||
| Total Therapy protocols T11–T14 | 1984–1999 | 5-years EFS | 36–44 chr | 17 | [20] | |||
| 25–29 chr | 26 | |||||||
| ≥45 chr | 75 | <0.001 | ||||||
| <45 chr | 20 | |||||||
| Medical Research Council, UK ALL trial protocols | 1990–2002 | 3-year-EFS | 42–45 chr | 121 | 65 | 0.0002 | [21] | |
| 25–39 chr | 20 | 29 | ||||||
| AIEOP-3; BFM-5; CCG-33; COALL-3; DANA FARBER-4; POG-44; SJCRH-6; UK-20; NOPHO-6; and EORTC-15 | 1986–1996 | 8-year EFS | 44 chr | 50 | 52 | <0.01 | [22] | |
| 40–43 chr | 8 | 19 | ||||||
| 33–39 chr | 26 | 37 | ||||||
| 30–32 chr | 0 | NA | ||||||
| 24–29 chr | 46 | 28 | ||||||
| COG AALL0031 | 2002–2006 | 4-year EFS | <30–44 chr | Chemotherapy alone | 26 | 50 | 0.65 | [66] |
| Chemotherapy + BMT | 13 | 62 | ||||||
| St. Jude Total Therapy Study XV&XVI | 2000–2014 | 5-year EFS | 24–31 chr | 8 | 73 | 0.8 | [23] | |
| 32–39 chr | 12 | 75 | ||||||
| MRD EOI neg | 14 | 85 | 0.03 | |||||
| MRD EOI pos | 6 | 44 | ||||||
| CIBMTR-All BMT in CR1 or CR2 | 1990–2010 | 5-year-DFS | 44–45 chr | 39 | 64 | 0.01 | [67] | |
| ≤43 chr | 39 | 37 | ||||||
| Children’s Healthcare of Atlanta | 2004–2016 | 2-year DFS | 32–39 chr | 5 | 60 | 0.853 | [57] | |
| 24–31 chr | 7 | 71 | ||||||
| MRD EOI neg | 10 | 69 | ||||||
| MRD EOI pos | 2 | 50 | ||||||
| Age ≥ 10 years | 6 | 33 | 0.021 | |||||
| Age < 10 years | 6 | 100 | ||||||
| COG AALL03B1-COG AALL0331 and AALL0232 * | 2003–2011 | 5-year EFS | >46 chr | NR | 85 | <0.01 | [26] | |
| <44 chr | 131 | 52 | ||||||
| BMT en CR1 | 61 | 56 | 0.62 | |||||
| No BMT | 52 | 49 | ||||||
| MRD pos | 30 | 26 | ||||||
| MRD neg | 74 | 64 | ||||||
| Standard NCI risk group | 48 | 60 | 0.026 | |||||
| High NCI risk group | 83 | 47 | ||||||
| Chemotherapy 1 | 4 | 0.13 | ||||||
| HSCT 1 | 7 | |||||||
| Ponte di Legno Childhood ALL Working Group- ≤44 chromosomas | 1997–2013 | 5-year EFS | 44 chr | 40 | 74 | 0.053 | [24] | |
| 40–43 chr | 13 | 58 | ||||||
| 30–39 chr | 118 | 50 | ||||||
| 24–29 chr | 101 | 56 | ||||||
| HCT in LH | 21 | 64 | 0.89 | |||||
| No HCT in LH | 93 | 62 | ||||||
| HCT in NH | 19 | 51 | 0.6 | |||||
| No HCT in NH | 82 | 44 | ||||||
| TCCSG, JACLS, Japanese Children’s Cancer and Leukemia Study Group, Kyushu-Yamaguchi Children’s Cancer Study Group | 1997–2012 | 5-year EFS | 45 chr | 101 | 73 | <0.036 | [25] | |
| 44 chr | 8 | 88 | ||||||
| <44 chr | 8 | 38 | ||||||
| Relapse rate in patients < 44 chr | 5 | 63 |
* B-ALL patients 1–30-years-old. 1 The 5-year cumulative incidence of SMN. Abbreviations: chr, chromosomes; DFS, disease-free survival; EFS, event-free survival; HCT, hematopoietic stem cell transplant; LH, low-hypodiploidy; NH, near-haploidy.
The low EFS rates observed in near-haploid and low-hypodiploid groups are related to a high relapse rate mostly from isolated BM relapses, and succumbing to the disease after first remission [24,25] (Table 5). According to the review by Groeneveld-Krentz et al. on patients with relapsed BCP-ALL [68], those with pediatric B-ALL with hypodiploidy <40 chromosomes show specific characteristics compared with other B-ALL groups, including: (i) association with older age at initial diagnosis, (ii) shorter time to first relapse, (iii) more frequent allocation to the high-risk treatment arm of the relapse trial, and (iv) inferior second remission rates [68]. Remarkably, patients with hypodiploidy with <40 chromosomes presenting with a predominant doubled clone or masked hypodiploidy had late relapses and more often achieved a second remission, as compared with patients with a predominant or exclusive hypodiploid clone. Despite these differences, however, the outcome of these patients is similarly poor, highlighting that all hypodiploidies with <40 chromosomes should be classified as high-risk irrespective of time to relapse [68].
7.2. Relationship of Genetic and Clinical Features with Patient Outcome
The EFS is not significantly different between patients with near-haploid or low-hypodiploid B-ALL, including those cases with “masked hypodiploidy” [23,24,57]. In some cases, hypodiploidy may accompany other primary genetic abnormalities, such as BCR-ABL1, TCF3-PBX1, ETV6-RUNX1 and KMT2A rearrangements, which modulate the prognosis of the disease. Accordingly, some authors have suggested that these patients should be treated based on the primary structural abnormalities rather than the hypodiploidy, and on their MRD values after induction [24]. The high presence of germline TP53 mutations among patients with low-hypodiploidy confer an increased risk of relapse in this group and is associated with the development of secondary neoplasms [24]. Therefore, it is highly recommended that all patients with low-hypodiploidy B-ALL are tested for germline TP53 mutations [24,69]. Strikingly, the germline TP53 mutations in these cases have been associated with increased mortality due to second neoplastic malignancies following hematopoietic stem cell transplantation (HSCT), highlighting the importance of the germline study in low-hypodiploid B-ALL to assess HSCT versus less toxic alternative therapies [26,67,70]. The presence of other recurrent mutations in near-haploid and low-hypodiploid B-ALL cases, such as alterations in the RAS-pathway, IKZF or RB1, has not shown a clear association with patient prognosis [23]. However, the small sample sizes, owing to the rarity of these B-ALL subtypes, may mask a significant association of these mutations with patient outcomes. Interestingly, a study by The Children’s Healthcare of Atlanta found that patients with hypodiploid B-ALL with <40 chromosomes and age ≥10 years display significant worse 2-year EFS rates (33.3% vs. 100%) [57]. Noteworthy, the impact of age on prognosis has also been reflected in other studies of adult B-ALL [35], where low-hypodiploid B-ALL patients < 35 years had survival rates of 71% against 21% in those patients >35 years.
The most important prognostic factor for near-haploid and low-hypodiploid B-ALL groups is the MRD status at the end of induction (EOI) [23]. Univariateanalyses including different clinical factors, such as National Cancer Institute (NCI) risk groups, MRD EOI status or HSCT, showed that only MRD EOI <0.01% was a significant prognostic factor for EFS in these cases [26]. Despite the poor prognosis of hypodiploid B-ALL with <40 chromosomes, the outcome improves significantly if the MRD EOI is negative, with 5-year EFS of 68–85% vs. 44–50% for MRD negative and positive patients, respectively [22,23,26,57,67] (Table 5). In view of these data, several groups have intensified treatments based on MRD-based stratification protocols, which has proven to be the most appropriate strategy associated with more favorable outcomes [24].
7.3. Current Treatment Protocols
Different study groups, such as the UKALL, NOPHO, AALL0031 and COG studies, consistently stratify near-haploid and low-hypodiploid B-ALL subtypes as high-risk based on the poor prognosis of the patients, which does not depend on treatment era or on the NCI risk group in which they are classified [24,26,71]. In view of the poor prognosis of patients with hypodiploid B-ALL, they have been classically treated with high-dose chemotherapy followed by allogeneic transplantation. However, different studies assessing the impact of HSCT on B-ALL with near-haploidy and low-hypodiploidy failed to demonstrate a clear benefit of HSCT in MRD positive or negative patients [23,24,57,66] (Table 5). Notwithstanding these findings, the outcome of hypodiploid B-ALL with <40 chromosomes has been substantially improved by MRD-guided therapy, which intensifies treatments based on the MRD EOI status [23]. MRD-stratified treatment protocols are associated with a favorable outcome after adjusting for sex, age, and leukocyte count, with a 5-year EFS of 62% [24,72]. Interestingly, Jeha et al. described a 5-year EFS of 100% in a series of 6 patients with hypodiploidy of <44 chromosomes using MRD-guided therapy, and even in 1 patient with positive MRD EOI [72]. The favorable impact of treating patients according to protocols stratified by MRD EOI is likely related to the identification of chemosensitive patients, those that are MRD EOI negative, for whom HSCT does not represent any benefit, and to not undertreat MRD-positive patients. To evaluate the real impact of HSCT in this setting, trials comparing HSCT with chemotherapy alone in patients with positive MRD EOI would be necessary, but this would be difficult due to the low incidence and poor prognosis of these patients with only chemotherapy treatment [73]. Given the low survival in this group despite HSCT, it seems imperative to investigate novel treatments and therapeutic approaches. Interestingly, fit adult patients with hypodiploid B-ALL would likely benefit from pediatric-adapted more intensive chemotherapy schemes [74]; however, this is difficult to assess clinically due to the very low incidence and dismal prognosis of hypodiploid B-ALL adult patients.
7.4. Novel Therapeutic Targets and Approaches to Treat B-ALL with <40 Chromosomes
New treatments aiming to target recently identified biological drivers of hypodiploidies as well as immunotherapy strategies are currently being explored to achieve better responses before HSCT or to be used as alternative approaches. The recent discovery of near-universal TP53 alterations in low-hypodiploid B-ALL has highlighted a key role for this gene in leukemogenesis. Investigation of this germinal mutation in this population is recommended when evaluating treatment with chemotherapy and HSCT. It remains to be demonstrated, however, whether therapies directed at this genetic lesion have an effect on low-hypodiploidy [58]. The anti-apoptotic protein BCL-2, has been identified as an effective therapeutic target for hypodiploid B-ALL with <40 chromosomes [75], and the efficacy of BCL-2 inhibitors (mainly venetoclax) has been demonstrated in ex vivo models of B-ALL with near-haploidy and low-hypodiploidy, especially in cases with elevated levels of the apoptosis-related factors BIM or BAD. Other authors have investigated the sensitivity of hypodiploid B-ALL cell lines and xenografts to MEK, PI3K, and the dual PI3K/mTOR inhibitors [30]. The PI3K and dual PI3K/mTOR inhibitors substantially inhibited proliferation of all tumors examined, suggesting that inhibition of the PI3K pathway may serve as a novel alternative therapy to treat hypodiploid B-ALL with <40 chromosomes [30].
Immunotherapy has shown encouraging results in relapsed/refractory B-ALL with high-risk cytogenetics, such as near-haploidy and low-hypodiploidy. Chimeric antigen receptor (CAR) T-cell and monoclonal antibodies or bi-specific T-cell engagers (BiTE), such as inotuzumab and blinatumomab, are the main immunotherapy approaches currently in use. It has been described that the patient response to CAR T-cell therapy does not depend on the cytogenetic risk group, with hypodiploid B-ALL representing up to 3.5% of cases according to the series [73]. Some of these cases have shown a promising response to CAR T-cell therapy, including an adult patient with low-hypodiploidy B-ALL in first relapse who received CD19-specific CAR T-cell therapy consolidated with HSCT [76]. Trials with CAR T-cell therapies as frontline approaches remain scarce and in some of them patients with hypodiploidy <40 chromosomes were excluded, such as the AALL1721/Cassiopeia trial (NCT03876769), a phase II single-arm trial of tisagenlecleucel (CD19-specific CAR T) in children and young adults with high risk B-ALL and persistent MRD at end of consolidation [77]. Blinatumomab, a BiTE antibody that directs T-cells to CD19-positive cells, has proven to be effective in adult patients with low-hypodiploid B-ALL, with 2 of the 4 patients reaching a complete response in one study [78]. It has also been used as an additional therapeutic approach in high-risk group protocols, which may induce a more in-depth response in these groups of B-ALL [79]. On the other hand, studies treating patients with inotuzumab ozogamicin, a humanized anti-CD22 antibody-drug conjugate, have not shown any specific high efficacy in patients with hypodiploid B-ALL [80]. Among the 3 patients with <40 chromosomes included in the study, 1 patient did not reach complete remission and the remaining patients did not reach a negative MRD EOI. In conclusion, new targeted treatments and immunotherapy approaches are very promising strategies, with ongoing protocols and active trials being conducted in patients with a very poor prognosis such as hypodiploidy ALL.
8. Concluding Remarks
Both near-haploid and low-hypodiploid B-ALL represent very rare entities, associated with a dismal clinical outcome. Such a low disease incidence represents a challenge to develop pre-clinical models aimed to study the etiology and pathogenesis of the disease and also represents a barrier to design statistically robust clinical trials.
Cutting-edge cytogenetic and genetic assays must be implemented in routine diagnostic laboratories to distinguish between high-hyperdiploid and masked hypodiploid B-ALL patients since this has a major impact on patient treatment stratification and clinical outcome.
The pathogenic effect(s) of chromosome losses and its contribution to leukemogenesis is currently not known. Furthermore, the biological contribution of chromosome doublings occurring in most of hypodiploid B-ALL cases with <40 chromosomes is poorly understood. Future studies aiming to decipher the biological mechanisms involved in the progression of hypodiploid B-ALL will help in the identification of innovative targeted treatments and/or diagnostic biomarkers to improve survival in these patients.
Acknowledgments
We thank Centres de Recerca de Catalunya (CERCA)/Generalitat de Catalunya, the Fundació Josep Carreras, and the Obra Social ‘la Caixa’ for their institutional support. Work in the laboratory of P.M. is supported by the Spanish Ministry of Economy and Competitiveness (PID2019-108160RB-I00/AEI/10.13039/501100011033), the European Research Council (CoG-2014-646903 and PoC-2018-811220), the Spanish Association of Cancer Research (AECC), the Fundación Uno entre Cienmil and la Caixa Foundation Health Research. O.M. is supported by an investigator fellowship from the AECC (INVES211226MOLI). A.B. is supported by Fundación Española de Hematología y Hemoterapia (FEHH).
Author Contributions
Conceptualization, O.M.; Conducted literature review: O.M., A.B., N.T., J.R., I.G., P.V. and J.L.F.; writing-original draft preparation, O.M. and P.M.; writing-review, all authors; supervision, O.M.; All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Spanish Ministry of Economy and Competitiveness (PID2019-108160RB-I00/AEI/10.13039/501100011033), the European Research Council (CoG-2014-646903 and PoC-2018-811220), the Spanish Association of Cancer Research (AECC, INVES211226MOLI).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Swerdlow S.H., Campo E., Pileri S.A., Harris N.L., Stein H., Siebert R., Advani R., Ghielmini M., Salles G.A., Zelenetz A.D., et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–2390. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howlader N., Noone A., Krapcho M., Miller D., Brest A., Yu M., Ruhl J., Tatalovich Z., Mariotto A., Lewis D., et al. SEER Cancer Statistics Review (CSR), 1975–2018. [(accessed on 5 November 2021)]; Available online: https://seer.cancer.gov/csr/1975_2018/
- 3.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2020. CA Cancer J. Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 4.Maitra A., McKenna R.W., Weinberg A.G., Schneider N.R., Kroft S.H. Precursor B-cell lymphoblastic lymphoma. A study of nine cases lacking blood and bone marrow involvement and review of the literature. Am. J. Clin. Pathol. 2001;115:868–875. doi: 10.1309/Q5GV-3K00-WAC6-BBUB. [DOI] [PubMed] [Google Scholar]
- 5.Pulte D., Gondos A., Brenner H. Improvement in survival in younger patients with acute lymphoblastic leukemia from the 1980s to the early 21st century. Blood. 2009;113:1408–1411. doi: 10.1182/blood-2008-06-164863. [DOI] [PubMed] [Google Scholar]
- 6.Pulte D., Jansen L., Gondos A., Katalinic A., Barnes B., Ressing M., Holleczek B., Eberle A., Brenner H., Group G.C.S.W. Survival of adults with acute lymphoblastic leukemia in Germany and the United States. PLoS ONE. 2014;9:e85554. doi: 10.1371/journal.pone.0085554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kadan-Lottick N.S., Ness K.K., Bhatia S., Gurney J.G. Survival variability by race and ethnicity in childhood acute lymphoblastic leukemia. JAMA. 2003;290:2008–2014. doi: 10.1001/jama.290.15.2008. [DOI] [PubMed] [Google Scholar]
- 8.Shuster J.J., Wacker P., Pullen J., Humbert J., Land V.J., Mahoney D.H., Jr., Lauer S., Look A.T., Borowitz M.J., Carroll A.J., et al. Prognostic significance of sex in childhood B-precursor acute lymphoblastic leukemia: A Pediatric Oncology Group Study. J. Clin. Oncol. 1998;16:2854–2863. doi: 10.1200/JCO.1998.16.8.2854. [DOI] [PubMed] [Google Scholar]
- 9.Smith M., Arthur D., Camitta B., Carroll A.J., Crist W., Gaynon P., Gelber R., Heerema N., Korn E.L., Link M., et al. Uniform approach to risk classification and treatment assignment for children with acute lymphoblastic leukemia. J. Clin. Oncol. 1996;14:18–24. doi: 10.1200/JCO.1996.14.1.18. [DOI] [PubMed] [Google Scholar]
- 10.Pui C.H., Relling M.V., Downing J.R. Acute lymphoblastic leukemia. N. Engl. J. Med. 2004;350:1535–1548. doi: 10.1056/NEJMra023001. [DOI] [PubMed] [Google Scholar]
- 11.Moorman A.V., Ensor H.M., Richards S.M., Chilton L., Schwab C., Kinsey S.E., Vora A., Mitchell C.D., Harrison C.J. Prognostic effect of chromosomal abnormalities in childhood B-cell precursor acute lymphoblastic leukaemia: Results from the UK Medical Research Council ALL97/99 randomised trial. Lancet Oncol. 2010;11:429–438. doi: 10.1016/S1470-2045(10)70066-8. [DOI] [PubMed] [Google Scholar]
- 12.Molina O., Abad M.A., Sole F., Menendez P. Aneuploidy in Cancer: Lessons from Acute Lymphoblastic Leukemia. Trends Cancer. 2021;7:37–47. doi: 10.1016/j.trecan.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 13.Inaba H., Mullighan C.G. Pediatric acute lymphoblastic leukemia. Haematologica. 2020;105:2524–2539. doi: 10.3324/haematol.2020.247031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malard F., Mohty M. Acute lymphoblastic leukaemia. Lancet. 2020;395:1146–1162. doi: 10.1016/S0140-6736(19)33018-1. [DOI] [PubMed] [Google Scholar]
- 15.Bassan R., Spinelli O., Oldani E., Intermesoli T., Tosi M., Peruta B., Rossi G., Borlenghi E., Pogliani E.M., Terruzzi E., et al. Improved risk classification for risk-specific therapy based on the molecular study of minimal residual disease (MRD) in adult acute lymphoblastic leukemia (ALL) Blood. 2009;113:4153–4162. doi: 10.1182/blood-2008-11-185132. [DOI] [PubMed] [Google Scholar]
- 16.Pui C.H., Williams D.L., Raimondi S.C., Rivera G.K., Look A.T., Dodge R.K., George S.L., Behm F.G., Crist W.M., Murphy S.B. Hypodiploidy is associated with a poor prognosis in childhood acute lymphoblastic leukemia. Blood. 1987;70:247–253. doi: 10.1182/blood.V70.1.247.247. [DOI] [PubMed] [Google Scholar]
- 17.Pui C.H., Carroll A.J., Raimondi S.C., Land V.J., Crist W.M., Shuster J.J., Williams D.L., Pullen D.J., Borowitz M.J., Behm F.G., et al. Clinical presentation, karyotypic characterization, and treatment outcome of childhood acute lymphoblastic leukemia with a near-haploid or hypodiploid less than 45 line. Blood. 1990;75:1170–1177. doi: 10.1182/blood.V75.5.1170.1170. [DOI] [PubMed] [Google Scholar]
- 18.Chessels J.M., Swansbury G.J., Reeves B., Bailey C.C., Richards S.M. Cytogenetics and prognosis in childhood lymphoblastic leukaemia: Results of MRC UKALL X. Medical Research Council Working Party in Childhood Leukaemia. Br. J. Haematol. 1997;99:93–100. doi: 10.1046/j.1365-2141.1997.3493163.x. [DOI] [PubMed] [Google Scholar]
- 19.Heerema N.A., Nachman J.B., Sather H.N., Sensel M.G., Lee M.K., Hutchinson R., Lange B.J., Steinherz P.G., Bostrom B., Gaynon P.S., et al. Hypodiploidy with less than 45 chromosomes confers adverse risk in childhood acute lymphoblastic leukemia: A report from the children’s cancer group. Blood. 1999;94:4036–4045. [PubMed] [Google Scholar]
- 20.Raimondi S.C., Zhou Y., Mathew S., Shurtleff S.A., Sandlund J.T., Rivera G.K., Behm F.G., Pui C.H. Reassessment of the prognostic significance of hypodiploidy in pediatric patients with acute lymphoblastic leukemia. Cancer. 2003;98:2715–2722. doi: 10.1002/cncr.11841. [DOI] [PubMed] [Google Scholar]
- 21.Harrison C.J., Moorman A.V., Broadfield Z.J., Cheung K.L., Harris R.L., Reza Jalali G., Robinson H.M., Barber K.E., Richards S.M., Mitchell C.D., et al. Three distinct subgroups of hypodiploidy in acute lymphoblastic leukaemia. Br. J. Haematol. 2004;125:552–559. doi: 10.1111/j.1365-2141.2004.04948.x. [DOI] [PubMed] [Google Scholar]
- 22.Nachman J.B., Heerema N.A., Sather H., Camitta B., Forestier E., Harrison C.J., Dastugue N., Schrappe M., Pui C.H., Basso G., et al. Outcome of treatment in children with hypodiploid acute lymphoblastic leukemia. Blood. 2007;110:1112–1115. doi: 10.1182/blood-2006-07-038299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mullighan C.G., Jeha S., Pei D., Payne-Turner D., Coustan-Smith E., Roberts K.G., Waanders E., Choi J.K., Ma X., Raimondi S.C., et al. Outcome of children with hypodiploid ALL treated with risk-directed therapy based on MRD levels. Blood. 2015;126:2896–2899. doi: 10.1182/blood-2015-09-671131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pui C.H., Rebora P., Schrappe M., Attarbaschi A., Baruchel A., Basso G., Cave H., Elitzur S., Koh K., Liu H.C., et al. Outcome of Children With Hypodiploid Acute Lymphoblastic Leukemia: A Retrospective Multinational Study. J. Clin. Oncol. 2019;37:770–779. doi: 10.1200/JCO.18.00822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ishimaru S., Okamoto Y., Imai C., Sakaguchi H., Taki T., Hasegawa D., Cho Y., Kakuda H., Sano H., Manabe A., et al. Nationwide survey of pediatric hypodiploid acute lymphoblastic leukemia in Japan. Pediatr. Int. 2019;61:1103–1108. doi: 10.1111/ped.14006. [DOI] [PubMed] [Google Scholar]
- 26.McNeer J.L., Devidas M., Dai Y., Carroll A.J., Heerema N.A., Gastier-Foster J.M., Kahwash S.B., Borowitz M.J., Wood B.L., Larsen E., et al. Hematopoietic Stem-Cell Transplantation Does Not Improve the Poor Outcome of Children With Hypodiploid Acute Lymphoblastic Leukemia: A Report From Children’s Oncology Group. J. Clin. Oncol. 2019;37:780–789. doi: 10.1200/JCO.18.00884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Safavi S., Paulsson K. Near-haploid and low-hypodiploid acute lymphoblastic leukemia: Two distinct subtypes with consistently poor prognosis. Blood. 2017;129:420–423. doi: 10.1182/blood-2016-10-743765. [DOI] [PubMed] [Google Scholar]
- 28.Gibbons B., MacCallum P., Watts E., Rohatiner A.Z., Webb D., Katz F.E., Secker-Walker L.M., Temperley I.J., Harrison C.J., Campbell R.H., et al. Near haploid acute lymphoblastic leukemia: Seven new cases and a review of the literature. Leukemia. 1991;5:738–743. [PubMed] [Google Scholar]
- 29.Moorman A.V. The clinical relevance of chromosomal and genomic abnormalities in B-cell precursor acute lymphoblastic leukaemia. Blood Rev. 2012;26:123–135. doi: 10.1016/j.blre.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Holmfeldt L., Wei L., Diaz-Flores E., Walsh M., Zhang J., Ding L., Payne-Turner D., Churchman M., Andersson A., Chen S.C., et al. The genomic landscape of hypodiploid acute lymphoblastic leukemia. Nat. Genet. 2013;45:242–252. doi: 10.1038/ng.2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Groupe Francais de Cytogenetique Hematologique Cytogenetic abnormalities in adult acute lymphoblastic leukemia: Correlations with hematologic findings outcome. A Collaborative Study of the Group Francais de Cytogenetique Hematologique. Blood. 1996;87:3135–3142. [PubMed] [Google Scholar]
- 32.Moorman A.V., Harrison C.J., Buck G.A., Richards S.M., Secker-Walker L.M., Martineau M., Vance G.H., Cherry A.M., Higgins R.R., Fielding A.K., et al. Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): Analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial. Blood. 2007;109:3189–3197. doi: 10.1182/blood-2006-10-051912. [DOI] [PubMed] [Google Scholar]
- 33.Pui C.H., Howard S.C. Current management and challenges of malignant disease in the CNS in paediatric leukaemia. Lancet. Oncol. 2008;9:257–268. doi: 10.1016/S1470-2045(08)70070-6. [DOI] [PubMed] [Google Scholar]
- 34.McGowan-Jordan J., Hastings R.J., Moore S. An International System for Human Cytogenomic Nomenclature (ISCN 2020) Karger; Basel, Switzerland: 2020. [Google Scholar]
- 35.Ribera J., Granada I., Morgades M., Vives S., Genesca E., Gonzalez C., Nomdedeu J., Escoda L., Montesinos P., Mercadal S., et al. The poor prognosis of low hypodiploidy in adults with B-cell precursor acute lymphoblastic leukaemia is restricted to older adults and elderly patients. Br. J. Haematol. 2019;186:263–268. doi: 10.1111/bjh.15887. [DOI] [PubMed] [Google Scholar]
- 36.Mitelman F., Johansson B., Mertens F. Mitelman Database of Chromosome Aberrations and Gene Fusions in Cancer. 2021. [(accessed on 5 November 2021)]. Available online: https://www.clinicalgenetics.lu.se/division-clinical-genetics/database-chromosome-aberrations-and-gene-fusions-cancer.
- 37.Safavi S., Forestier E., Golovleva I., Barbany G., Nord K.H., Moorman A.V., Harrison C.J., Johansson B., Paulsson K. Loss of chromosomes is the primary event in near-haploid and low-hypodiploid acute lymphoblastic leukemia. Leukemia. 2013;27:248–250. doi: 10.1038/leu.2012.227. [DOI] [PubMed] [Google Scholar]
- 38.Muhlbacher V., Zenger M., Schnittger S., Weissmann S., Kunze F., Kohlmann A., Bellos F., Kern W., Haferlach T., Haferlach C. Acute lymphoblastic leukemia with low hypodiploid/near triploid karyotype is a specific clinical entity and exhibits a very high TP53 mutation frequency of 93% Genes Chromosomes Cancer. 2014;53:524–536. doi: 10.1002/gcc.22163. [DOI] [PubMed] [Google Scholar]
- 39.Creasey T., Enshaei A., Nebral K., Schwab C., Watts K., Cuthbert G., Vora A., Moppett J., Harrison C.J., Fielding A.K., et al. Single nucleotide polymorphism array-based signature of low hypodiploidy in acute lymphoblastic leukemia. Genes Chromosomes Cancer. 2021;60:604–615. doi: 10.1002/gcc.22956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Charrin C., Thomas X., Ffrench M., Le Q.H., Andrieux J., Mozziconacci M.J., Lai J.L., Bilhou-Nabera C., Michaux L., Bernheim A., et al. A report from the LALA-94 and LALA-SA groups on hypodiploidy with 30 to 39 chromosomes and near-triploidy: 2 possible expressions of a sole entity conferring poor prognosis in adult acute lymphoblastic leukemia (ALL) Blood. 2004;104:2444–2451. doi: 10.1182/blood-2003-04-1299. [DOI] [PubMed] [Google Scholar]
- 41.Carroll A.J., Shago M., Mikhail F.M., Raimondi S.C., Hirsch B.A., Loh M.L., Raetz E.A., Borowitz M.J., Wood B.L., Maloney K.W., et al. Masked hypodiploidy: Hypodiploid acute lymphoblastic leukemia (ALL) mimicking hyperdiploid ALL in children: A report from the Children’s Oncology Group. Cancer Genet. 2019;238:62–68. doi: 10.1016/j.cancergen.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paietta E., Roberts K.G., Wang V., Gu Z., Buck G.A.N., Pei D., Cheng C., Levine R.L., Abdel-Wahab O., Cheng Z., et al. Molecular classification improves risk assessment in adult BCR-ABL1-negative B-ALL. Blood. 2021;138:948–958. doi: 10.1182/blood.2020010144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harrison C.J., Moorman A.V., Barber K.E., Broadfield Z.J., Cheung K.L., Harris R.L., Jalali G.R., Robinson H.M., Strefford J.C., Stewart A., et al. Interphase molecular cytogenetic screening for chromosomal abnormalities of prognostic significance in childhood acute lymphoblastic leukaemia: A UK Cancer Cytogenetics Group Study. Br. J. Haematol. 2005;129:520–530. doi: 10.1111/j.1365-2141.2005.05497.x. [DOI] [PubMed] [Google Scholar]
- 44.Stark B., Jeison M., Gobuzov R., Krug H., Glaser-Gabay L., Luria D., El-Hasid R., Harush M.B., Avrahami G., Fisher S., et al. Near haploid childhood acute lymphoblastic leukemia masked by hyperdiploid line: Detection by fluorescence in situ hybridization. Cancer Genet. Cytogenet. 2001;128:108–113. doi: 10.1016/S0165-4608(01)00411-3. [DOI] [PubMed] [Google Scholar]
- 45.Kohno S., Minowada J., Sandberg A.A. Chromosome evolution of near-haploid clones in an established human acute lymphoblastic leukemia cell line (NALM-16) J. Natl. Cancer Inst. 1980;64:485–493. [PubMed] [Google Scholar]
- 46.Aburawi H.E., Biloglav A., Johansson B., Paulsson K. Cytogenetic and molecular genetic characterization of the ‘high hyperdiploid’ B-cell precursor acute lymphoblastic leukaemia cell line MHH-CALL-2 reveals a near-haploid origin. Br. J. Haematol. 2011;154:275–277. doi: 10.1111/j.1365-2141.2011.08601.x. [DOI] [PubMed] [Google Scholar]
- 47.Edgar B.A., Zielke N., Gutierrez C. Endocycles: A recurrent evolutionary innovation for post-mitotic cell growth. Nat. Rev. Mol. Cell Biol. 2014;15:197–210. doi: 10.1038/nrm3756. [DOI] [PubMed] [Google Scholar]
- 48.Shu Z., Row S., Deng W.M. Endoreplication: The Good, the Bad, and the Ugly. Trends Cell Biol. 2018;28:465–474. doi: 10.1016/j.tcb.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bielski C.M., Zehir A., Penson A.V., Donoghue M.T.A., Chatila W., Armenia J., Chang M.T., Schram A.M., Jonsson P., Bandlamudi C., et al. Genome doubling shapes the evolution and prognosis of advanced cancers. Nat. Genet. 2018;50:1189–1195. doi: 10.1038/s41588-018-0165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Storchova Z., Kuffer C. The consequences of tetraploidy and aneuploidy. J. Cell Sci. 2008;121:3859–3866. doi: 10.1242/jcs.039537. [DOI] [PubMed] [Google Scholar]
- 51.Safavi S., Olsson L., Biloglav A., Veerla S., Blendberg M., Tayebwa J., Behrendtz M., Castor A., Hansson M., Johansson B., et al. Genetic and epigenetic characterization of hypodiploid acute lymphoblastic leukemia. Oncotarget. 2015;6:42793–42802. doi: 10.18632/oncotarget.6000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Agraz-Doblas A., Bueno C., Bashford-Rogers R., Roy A., Schneider P., Bardini M., Ballerini P., Cazzaniga G., Moreno T., Revilla C., et al. Unravelling the cellular origin and clinical prognostic markers of infant B-cell acute lymphoblastic leukemia using genome-wide analysis. Haematologica. 2019;104:1176–1188. doi: 10.3324/haematol.2018.206375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ueno H., Yoshida K., Shiozawa Y., Nannya Y., Iijima-Yamashita Y., Kiyokawa N., Shiraishi Y., Chiba K., Tanaka H., Isobe T., et al. Landscape of driver mutations and their clinical impacts in pediatric B-cell precursor acute lymphoblastic leukemia. Blood Adv. 2020;4:5165–5173. doi: 10.1182/bloodadvances.2019001307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mullighan C.G., Zhang J., Kasper L.H., Lerach S., Payne-Turner D., Phillips L.A., Heatley S.L., Holmfeldt L., Collins-Underwood J.R., Ma J., et al. CREBBP mutations in relapsed acute lymphoblastic leukaemia. Nature. 2011;471:235–239. doi: 10.1038/nature09727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stengel A., Schnittger S., Weissmann S., Kuznia S., Kern W., Kohlmann A., Haferlach T., Haferlach C. TP53 mutations occur in 15.7% of ALL and are associated with MYC-rearrangement, low hypodiploidy, and a poor prognosis. Blood. 2014;124:251–258. doi: 10.1182/blood-2014-02-558833. [DOI] [PubMed] [Google Scholar]
- 56.Moorman A.V. Does TP53 guard ALL genomes? Blood. 2014;124:160–161. doi: 10.1182/blood-2014-05-576934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Miller L., Kobayashi S., Pauly M., Lew G., Saxe D., Keller F., Qayed M., Castellino S. Evaluating approaches to enhance survival in children with hypodiploid acute lymphoblastic leukaemia (ALL) Br. J. Haematol. 2019;185:613–616. doi: 10.1111/bjh.15590. [DOI] [PubMed] [Google Scholar]
- 58.Comeaux E.Q., Mullighan C.G. TP53 Mutations in Hypodiploid Acute Lymphoblastic Leukemia. Cold Spring Harb. Perspect. Med. 2017;7:a026286. doi: 10.1101/cshperspect.a026286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lafage-Pochitaloff M., Baranger L., Hunault M., Cuccuini W., Lefebvre C., Bidet A., Tigaud I., Eclache V., Delabesse E., Bilhou-Nabera C., et al. Impact of cytogenetic abnormalities in adults with Ph-negative B-cell precursor acute lymphoblastic leukemia. Blood. 2017;130:1832–1844. doi: 10.1182/blood-2017-05-783852. [DOI] [PubMed] [Google Scholar]
- 60.Paulsson K., Lilljebjorn H., Biloglav A., Olsson L., Rissler M., Castor A., Barbany G., Fogelstrand L., Nordgren A., Sjogren H., et al. The genomic landscape of high hyperdiploid childhood acute lymphoblastic leukemia. Nat. Genet. 2015;47:672–676. doi: 10.1038/ng.3301. [DOI] [PubMed] [Google Scholar]
- 61.Paulsson K. High hyperdiploid childhood acute lymphoblastic leukemia: Chromosomal gains as the main driver event. Mol. Cell. Oncol. 2016;3:e1064555. doi: 10.1080/23723556.2015.1064555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mandahl N., Johansson B., Mertens F., Mitelman F. Disease-associated patterns of disomic chromosomes in hyperhaploid neoplasms. Genes Chromosomes Cancer. 2012;51:536–544. doi: 10.1002/gcc.21947. [DOI] [PubMed] [Google Scholar]
- 63.Molina, O. (Josep Carreras Leukemia Research Institute, Barcelona, Spain). High-resolution confocal microscopy analyses of mitotic progression using PDX samples derived from near-haploid and low-hypodiploid B-ALL. 2021. material not intended for publication.
- 64.Gruhn B., Taub J.W., Ge Y., Beck J.F., Zell R., Hafer R., Hermann F.H., Debatin K.M., Steinbach D. Prenatal origin of childhood acute lymphoblastic leukemia, association with birth weight and hyperdiploidy. Leukemia. 2008;22:1692–1697. doi: 10.1038/leu.2008.152. [DOI] [PubMed] [Google Scholar]
- 65.Greaves M. A causal mechanism for childhood acute lymphoblastic leukaemia. Nat. Rev. Cancer. 2018;18:471–484. doi: 10.1038/s41568-018-0015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schultz K.R., Devidas M., Bowman W.P., Aledo A., Slayton W.B., Sather H., Zheng H.W., Davies S.M., Gaynon P.S., Trigg M., et al. Philadelphia chromosome-negative very high-risk acute lymphoblastic leukemia in children and adolescents: Results from Children’s Oncology Group Study AALL0031. Leukemia. 2014;28:964–967. doi: 10.1038/leu.2014.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mehta P.A., Zhang M.J., Eapen M., He W., Seber A., Gibson B., Camitta B.M., Kitko C.L., Dvorak C.C., Nemecek E.R., et al. Transplantation Outcomes for Children with Hypodiploid Acute Lymphoblastic Leukemia. Biol. Blood Marrow Transplant. 2015;21:1273–1277. doi: 10.1016/j.bbmt.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Groeneveld-Krentz S., Schroeder M.P., Reiter M., Pogodzinski M.J., Pimentel-Gutierrez H.J., Vagkopoulou R., Hof J., Chen-Santel C., Nebral K., Bradtke J., et al. Aneuploidy in children with relapsed B-cell precursor acute lymphoblastic leukaemia: Clinical importance of detecting a hypodiploid origin of relapse. Br. J. Haematol. 2019;185:266–283. doi: 10.1111/bjh.15770. [DOI] [PubMed] [Google Scholar]
- 69.Shetty D., Amare P.K., Mohanty P., Talker E., Chaubal K., Jain H., Tembhare P., Patkar N., Chaturvedi A., Subramanian P.G., et al. Investigating the clinical, hematological and cytogenetic profile of endoreduplicated hypodiploids in BCP-ALL. Blood Cells Mol. Dis. 2020;85:102465. doi: 10.1016/j.bcmd.2020.102465. [DOI] [PubMed] [Google Scholar]
- 70.Winter G., Kirschner-Schwabe R., Groeneveld-Krentz S., Escherich G., Moricke A., von Stackelberg A., Stanulla M., Bailey S., Richter L., Steinemann D., et al. Clinical and genetic characteristics of children with acute lymphoblastic leukemia and Li-Fraumeni syndrome. Leukemia. 2021;35:1475–1479. doi: 10.1038/s41375-021-01163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee S.H.R., Li Z., Tai S.T., Oh B.L.Z., Yeoh A.E.J. Genetic Alterations in Childhood Acute Lymphoblastic Leukemia: Interactions with Clinical Features and Treatment Response. Cancers. 2021;13:4068. doi: 10.3390/cancers13164068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jeha S., Choi J., Roberts K.G., Pei D., Coustan-Smith E., Inaba H., Rubnitz J.E., Ribeiro R.C., Gruber T.A., Raimondi S.C., et al. Clinical significance of novel subtypes of acute lymphoblastic leukemia in the context of minimal residual disease-directed therapy. Blood Cancer Discov. 2021;2:326–337. doi: 10.1158/2643-3230.BCD-20-0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Talleur A.C., Maude S.L. What is the role for HSCT or immunotherapy in pediatric hypodiploid B-cell acute lymphoblastic leukemia? Hematol. Am. Soc. Hematol. Educ. Program. 2020;2020:508–511. doi: 10.1182/hematology.2020000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ribera J.M., Oriol A., Morgades M., Montesinos P., Sarra J., Gonzalez-Campos J., Brunet S., Tormo M., Fernandez-Abellan P., Guardia R., et al. Treatment of high-risk Philadelphia chromosome-negative acute lymphoblastic leukemia in adolescents and adults according to early cytologic response and minimal residual disease after consolidation assessed by flow cytometry: Final results of the PETHEMA ALL-AR-03 trial. J. Clin. Oncol. 2014;32:1595–1604. doi: 10.1200/JCO.2013.52.2425. [DOI] [PubMed] [Google Scholar]
- 75.Diaz-Flores E., Comeaux E.Q., Kim K.L., Melnik E., Beckman K., Davis K.L., Wu K., Akutagawa J., Bridges O., Marino R., et al. Bcl-2 Is a Therapeutic Target for Hypodiploid B-Lineage Acute Lymphoblastic Leukemia. Cancer Res. 2019;79:2339–2351. doi: 10.1158/0008-5472.CAN-18-0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fang M., Becker P.S., Linenberger M., Eaton K.D., Appelbaum F.R., Dreyer Z., Airewele G., Redell M., Lopez-Terrada D., Patel A., et al. Adult Low-Hypodiploid Acute B-Lymphoblastic Leukemia With IKZF3 Deletion and TP53 Mutation: Comparison With Pediatric Patients. Am. J. Clin. Pathol. 2015;144:263–270. doi: 10.1309/AJCPW83OXPYKPEEN. [DOI] [PubMed] [Google Scholar]
- 77.Diorio C., Maude S.L. CAR T cells vs allogeneic HSCT for poor-risk ALL. Hematol. Am. Soc. Hematol. Educ. Program. 2020;2020:501–507. doi: 10.1182/hematology.2020000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhao Y., Aldoss I., Qu C., Crawford J.C., Gu Z., Allen E.K., Zamora A.E., Alexander T.B., Wang J., Goto H., et al. Tumor-intrinsic and -extrinsic determinants of response to blinatumomab in adults with B-ALL. Blood. 2021;137:471–484. doi: 10.1182/blood.2020006287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang L., Ashraf D.C., Kinde B., Ohgami R.S., Kumar J., Kersten R.C. Hypodiploid B-Lymphoblastic Leukemia Presenting as an Isolated Orbital Mass Prior to Systemic Involvement: A Case Report and Review of the Literature. Diagnostics. 2020;11:25. doi: 10.3390/diagnostics11010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bhojwani D., Sposto R., Shah N.N., Rodriguez V., Yuan C., Stetler-Stevenson M., O’Brien M.M., McNeer J.L., Quereshi A., Cabannes A., et al. Inotuzumab ozogamicin in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. Leukemia. 2019;33:884–892. doi: 10.1038/s41375-018-0265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]