Abstract
This paper investigates the mental health effects of the local and global level Covid-19 pandemic among the UK population. To identify the effect, we use a high-quality dataset and an original strategy where we match the previous day’s confirmed pandemic cases to a four-month panel of individual mental health information observed during the interview next day. The approach suggested in this paper aims to identify the average mental health effect on the overall population for the first and second waves of the pandemic. Using a linear fixed-effects model specification, we report robust findings that the average mental health in the UK is substantially reduced by the local and global pandemic. The total reduction in the average mental health of the UK population during our sampling period (April - June, 2020) is about 1.5% for the local and 2.4% for the global cases, which sum up to a 3.9% reduction. Extrapolating the total reduction in average mental health during the first wave of the pandemic (February - September, 2020) sums up to 2.8% while the effect is as large as 9.6% for the first and second waves together, which covers roughly a year since the start. An extensive robustness check suggests that the findings are stable with respect to alternative pandemic datasets, measures, estimators, functional forms, and time functions. The characteristics of the most vulnerable individuals (e.g., elderly, chronic illness, and job security concerns) and their household conditions (e.g., living alone and no private space) are explored. The paper discusses on the implications of the results.
Keywords: Mental Health, Covid-19, Pandemic, Vulnerable Individuals
1. Introduction
The previous experience with global traumatic events (e.g., previous widespread pandemics such as SARS-COV-1 and the Ebola outbreak or globally impactful terror events such as 9/11) suggests that one of the domains expected to be quickly affected by the current coronavirus (Covid-19 hereafter) pandemic is mental health (e.g., Mak et al., 2009; Pandya, 2013; Shultz et al., 2015; Bao et al., 2020; Banks and Xu, 2020; Proto and Quintana-Domeque, 2021). The terrifying daily spread of the Covid-19 pandemic generates fear, anxiety, economic problems, and disturbances in daily life (e.g., social isolation, physical ("social") distancing, changes in day-to-day functioning, job security issues, financial concerns for the future) which might translate into adverse mental health outcomes, including post-traumatic stress, depression, sleep disorders, and reduced overall well-being among many others (e.g., Brodeur et al., 2021b; Proto and Quintana-Domeque, 2021; Goularte et al., 2020; Rajkumar, 2020; Shigemura et al., 2020). Indeed, a recent survey conducted by World Health Organization reports that the current coronavirus pandemic has halted or reduced critical mental health services in 93% of the countries (WHO, 2020; Fusar-Poli et al., 2020).
Using samples from various countries, studies investigating the effect of Covid-19 pandemic on several outcomes including mental health effects of the Covid-19 pandemic have been growing since the beginning of the pandemic (e.g., Banks and Xu, 2020; Brodeur et al., 2021a, Brodeur et al., 2021b; Proto and Quintana-Domeque, 2021; Etheridge and Lisa, 2020; Goularte et al., 2020; Gao et al., 2020; Bao et al., 2020; Rajkumar, 2020; Trudeau et al., 2020; Perez-Arce et al., 2021). A consistent finding is that the pandemic has substantially decreased the mental health of people compared to their average mental health levels during previous years, which also differ by age, gender, and ethnicity, among other factors (e.g., Banks and Xu, 2020; Proto and Quintana-Domeque, 2021; Brodeur et al., 2021b). The prevalence of depression, stress, post-traumatic stress, and sleep disorders has also been substantially increased (see Rajkumar (2020) for a review). Another strand of studies investigating the mental health effects of the pandemic has generally focused on specific risk groups, including health care workers (Bassi et al., 2020; Rossi et al., 2020; Shigemura et al., 2020), the elderly (Yang et al., 2020), the homeless (Tsai and Wilson, 2020), migrants, refugees and ethnic groups (Proto and Quintana-Domeque, 2021; Liem et al., 2020). One immediate insight of the current literature is that there is an urgent need to obtain further evidence on how a marginal increase in the spread of the pandemic affects the average mental health and which groups of people are the most vulnerable to mental health effects of the pandemic.
Existing studies are mostly based on identifying the difference in the average mental health during the pandemic compared to that of previous years (e.g., Brodeur et al., 2021b; Banks and Xu, 2020; Proto and Quintana-Domeque, 2021; Goularte et al., 2020; Davillas and Jones, 2021). To our knowledge, this paper is the first to offer a methodology to identify the average marginal effects of the daily confirmed Covid-19 cases on the mental health outcomes, which can be extrapolated to calculate the total mental effect of whole first and second waves of the pandemic. The strategy also allows us to undertake an extensive range of alternative analyses. First, we make a distinction by considering that mental health is not only affected by the immediate threats and disturbances due to the local pandemic but also by the overall global prevalence of the pandemic. Second, we conduct an extensive investigation on how individual constraints (e.g., old age, underlying chronic diseases, job security, unemployment, poverty, and future financial concerns) and household circumstances (e.g., living alone, household composition, dependent kids, household size, and presence of a garden or a private space) correlate with the average mental health effect of the local and global pandemic.
To reach these aims, the paper uses a high-quality dataset and a highly original strategy to identify the average marginal mental health effect of the local and global pandemic cases in the UK.1 Our micro-dataset includes four waves of a monthly panel from April 2020 to July 2020, which is a part of a long yearly and highly representative panel dataset (the UK Household Longitudinal Survey - UKHLS). The dataset includes the General Health Questionnaire (GHQ), which is a well-known inventory allowing us to develop a solid mental health measure widely used in the literature (e.g., Clark and Oswald, 1994; Akay et al., 2012; Banks and Xu, 2020; Proto and Quintana-Domeque, 2021). The paper offers an identification strategy which differs from the existing studies (cf., Proto and Quintana-Domeque, 2021). Instead of measuring the change in mental health compared to previous years, we match the daily local and global cases with the individual panel using the next day interview dates (Akay et al., 2020). Because the panel in the dataset is observed four times, this strategy of using the data can be interpreted as a series of random experiments on the same individuals conducted by nature four times for the different pandemic circumstances. The effect of the pandemic cases come from the daily fluctuations of the local and global pandemic cases, which are assumed to be random with respect to the date of interview. Thus, our strategy identifies the temporal average marginal effect of the pandemic cases on the mental health of the overall population.
Exploiting the panel aspect of our data and four months of several time-variant individual and household characteristics, we use panel data fixed-effects specifications to estimate the effect of the previous day’s local and global cases on mental health. The results are highly consistent with the earlier studies using alternative identification strategies (cf., Banks and Xu, 2020; Proto and Quintana-Domeque, 2021). Our results suggest a significant and negative mental health effect of the previous day’s cases on the overall population in the UK. To put the effects of the local and global pandemic cases into context and summarise, we calculate the total effect of local and global cases - the average effect of the mean number of cases for a particular pandemic period - relative to average mental health in the UK. The results suggest that the total reduction in the average mental health during the sampling period (May - June, 2020) is about 1.5% for the local cases and 2.4% for the global cases, which sum up to a 3.9% reduction in the average mental health in the UK. The identification strategy also allows for extrapolating the effect for the first wave (February - September, 2020) and for a period covering the first and second waves of the pandemic (February, 2020 - February, 2021). The total reduction in the average mental health during the first wave sums up to 2.8% while the total effect is as large as 9.6% during the first and second waves of the pandemic. The results are also highly robust with respect to functional forms of Covid-19 measures, time functions, alternative estimators, and sources of alternative local and global Covid-19 datasets. The paper presents a discussion using a heterogeneity analysis with respect to individual and household constraints to determine the vulnerable and non-vulnerable individuals. We find that older people with health constraints (e.g., chronic health conditions), people who are living alone, those who are experiencing job insecurity and economic concerns, and households with constraints in their immediate living environment (e.g., no private space or garden) are the most vulnerable.
The rest of the paper is organised as follows: Section 2 presents the micro dataset, the daily Covid-19 dataset, and the empirical design. Section 3 gives the econometric methods, stochastic specifications, and our identification strategy. Section 4 presents the results split by main results and a robustness analysis. Section 5 presents an extensive discussion using a comprehensive heterogeneity analysis with respect to individual and household circumstances. Finally, Section 6 concludes the paper.
2. Data
2.1. The sample and key variables
2.1.1. Micro data
Our individual data is a part of the UK Household Longitudinal Survey (UKHLS, or Understanding Society Data, “US" hereafter).2 The dataset is an innovative extension of the former British household panel (BHPS) including thousands of households and individuals. The US dataset is originally a long yearly panel with a wealth of information on the individual and household socio-demographic and economic characteristics, and subjective measures about the individuals’ well-being, mental health, attitudes, and behaviour.
2.1.2. A new Covid-19 module
The US dataset has a new innovative module collected to obtain information on several dimensions of life in the UK during the Covid-19 pandemic. The module is based on a short twenty-minute questionnaire implemented either with a web portal or with the standard computer assisted telephone interviews. The information obtained in the module covers household composition, coronavirus illness, long-term health conditions management, mental health, loneliness, and employment. There are four waves of the Covid-19 module administered to the same sample of representative individuals during April, May, June, and July. However, because the dataset was originally a long yearly panel, it is also possible to trace individuals back to previous years and obtain information for a decade. There have been about 61,167 interviews conducted during the four-waves of the Covid-19 module and these interviews are conducted over a total of 29 interview days. There are some randomly missing values in the control variables and the final sample size used in our estimations is 57,789 individual-wave observations.
2.1.3. The mental health measure
The main outcome variable investigated in this study is based on the twelve questions of the General Health Questionnaire (GHQ) inventory. The full set of questions appearing in the inventory is given in Appendix C, Table C.1. The inventory involves twelve domains of an individual’s mental well-being, including sleep problems, depression, enjoyment of day-to-day activities, self-worth, and happiness. Each question is answered on an ordinal scale from (1) to (4). An easy composite measure is formed by summing up the scores obtained from each question (e.g., Akay et al., 2012; Clark and Oswald, 1994). The final measure is normalised to range between 0 and 36. We reverse the scale so that the higher scores indicate higher mental health and use it as the main output variable (GHQ36 with 36-points scale). We also use each item in the inventory as an output variable representing a particular domain of mental health.
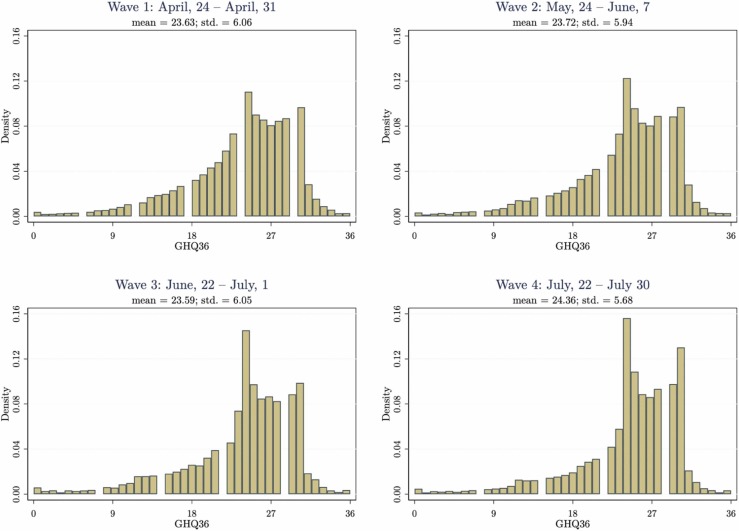
The measure is highly correlated with other psychiatric mental health measures, life satisfaction or happiness measures (Goldberg et al., 1997). The measure is also considered to be a proxy for the overall welfare of an individual or the unobserved ‘experienced’ utility level - as in the case of happiness or life satisfaction measures (see, Kahneman and Sugden (2005) for a comprehensive discussion and Clark and Oswald (1994)). The mean GHQ36 score is 23.8 with a standard deviation of 5.91. The histogram of GHQ36 is given in Appendix B, Fig. B.1, for Waves 1–4. The distributions are not only similar across waves but also in line with the distributional shapes usually observed in other studies using the same types of measurement (e.g., Akay et al., 2012). The averages of the first three waves are highly similar, while there is a statistically significant recovery in GHQ36 scores during the last wave, i.e., June, 2020 (23.59 vs. 24.36, p-value = 0.000). This result is expected because this period corresponds to the end of the first wave of the pandemic, when the pandemic cases are relatively lower.
Fig. B.1.
Distributions of GHQ36 across Waves. Note: Authors’ own calculations from Understanding Society (2020).
2.1.4. The daily Covid-19 data and definition of measures
There are several sources of daily Covid-19 datasets available: i) World Health Organisation (WHO), ii) John Hopkins University (JHU), and iii) European Centre for Disease Prevention and Control (ECDC).3 A straightforward choice for the main analysis is the official Covid-19 dataset of WHO (last accessed January 15, 2021). Most media institutions fetch their data from WHO’s Covid-19 online dashboard, which is also followed by many people via internet worldwide.4 Simple statistics suggest that the datasets supplied by WHO, JHU and ECDC are highly similar to each other, as they mostly use the same official sources. Yet, because these datasets are collected by different institutions, methodologies and countries, they might lead to different estimates, especially for the global sums. We present a series of results in our robustness analyses using alternative Covid-19 datasets to check the robustness of our results.
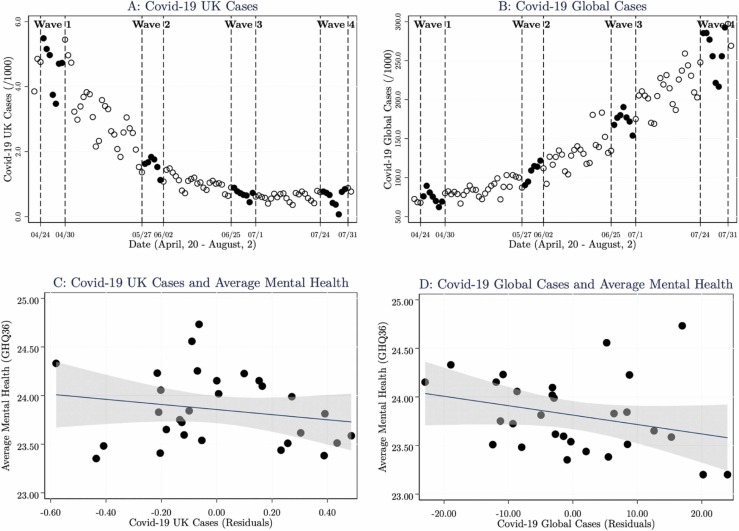
The Covid-19 data are in daily time series format including pandemic related confirmed number of daily cases and deaths by several countries all around the world. First, we define global Covid-19 cases by summing up all cases worldwide (except the UK) for each day. Second, we define the daily pandemic related confirmed cases in the UK. One important remark is that local and global cases and deaths are highly correlated over time. The correlation between global cases and deaths is 0.89 while the correlation in the UK is 0.92. It is also not possible to judge a priori which measure people follow from media or internet sources and which measure generates more fear or anxiety. As there are very high correlations and there might be large measurement error in the measures of the pandemic deaths, we prefer focusing on the local and global pandemic cases. Yet, to check the consistency, we are going to present results from the local and global pandemic deaths. In Fig. 1, Panels A and B, we present the time series patterns of the UK and global Covid-19 cases for the dates surrounding the sampling period from April, 20 to August 2. The overall pattern of the UK cases are decreasing while global cases are increasing during the sampling period. Yet, there is a substantial time variation in both pandemic measures, which is the key to this study.
Fig. 1.
Local and Global Covid-19 Cases Over Time and Sampling. Note: For Panels A and B, data points represent the raw (WHO, 2020) Covid-19 confirmed cases for the UK and whole world. The local and global number of cases are rescaled by 1000. The pandemic cases are represented by hollow circles and the cases corresponding to the interview days in Wave 1 - Wave 4 in Understanding Society (2020) dataset are presented with filled circles. The exact dates and the corresponding number of interviews conducted are given in Appendix A, Table A.1. For Panels C and D, data points are obtained by averaging GHQ36 scores by the residuals of the UK and Global cases. We obtain the residuals from regressions which are conditioned on the linear trend, the day of the week, and wave dummies. The lines represent the linear regressions which use the underlying 29 data points. The grey area represents the 95% confidence intervals.
2.1.5. Empirical Design and Raw Relationships
The strategy of estimating the relationship is based on the exogenous variation in the daily pandemic related local and global cases the day before the interview in which the mental health of individuals is observed. We first identify the date on which the interviews are conducted. The exact dates are given in Fig. 1, Panels A and B, with filled points. We then match the pandemic cases the day before with the interview dates the next day in the US dataset. There are four different data collection episodes (Waves 1–4 as represented in Panels A and B of Fig. 1) during which the mental health information is obtained. We interpret this strategy as a “natural experiment" conducted with the same group of individuals in four different time periods with different pandemic circumstances. There are 29 days on which people are assigned to be interviewed, i.e., “treated" with the previous day’s pandemic cases. The exact number of interviews, the day of the week on which the interview is conducted, and some further descriptive statistics of the individuals’ characteristics are given in Appendix A, Table A.1.
At this point, we present two intuitive figures which show the initial raw relationship between the local and global pandemic cases and the average mental health obtained during the next day’s interview. The results are presented in Panels C and D of Fig. 1. Each point in the figures represents the mean GHQ36 score corresponding to the local (Panel A) and global (Panel B) pandemic cases day before. To draw these figures, we obtain the residuals conditional on linear time trend, the day of the week dummies, and wave dummies. To describe the raw relationship, we also draw the linear regression line on the underlying data together with the 95% confidence intervals of the raw predictions. Our first observation is that there is a visible negative correlation between previous day local and global pandemic cases and the mental health outcomes next day. The slope of the linear regression is highly statistically significant for both cases. In the following sections, we are going to present results from econometric specifications where we allow for alternative sets of individual controls and time functions using our individual panel dataset.
3. Empirical approach
3.1. The econometric model
The empirical approach exploits daily fluctuations in the local and global pandemic measures and the daily information on individuals’ mental health. As the same individuals are measured four times at different points in time, the data is a monthly panel in which we allow for time-variant characteristics which can also influence mental health. The baseline model specification is given in Eqs. (1) and (2).
| (1) |
| (2) |
The dependent variable, mental health GHQ i,d,w, is measured for each individual i on the day of interview d for four waves w. The Covid-19 related cases C that occurred in the UK and globally GL the day before the interview d − 1, are given in and . The key parameters to be estimated are β UK and β GL. The main reason that we prefer the previous day d − 1 is to ensure that people in the UK learned about the number of daily pandemic cases within the past 24 h. To guarantee this for the global cases, we use 48 h by considering the time zone differences. In the econometric analysis below, we are going to present results where we also estimate alternative combinations of these measures in the same regression. In our baseline model specification, we prefer using the levels of the pandemic measures rescaled by 1000 cases as in Fig. 1, Panels A and B. A robustness analysis with respect to functional forms of Covid-19 measures, estimators, and time functions is also presented.
3.1.1. Control variables
The model specification (Eqs. (1) and (2)) includes a large set of control variables which might confound the effect of the pandemic on mental health. These variables are all wave specific and included in . γ is the vector of parameters to be estimated. As the model specification is a fixed-effect model, the time-invariant variables are all swept away. That is, we use only those variables that change during the four waves of our data. They include whether living in a couple (couples=1), whether tested for coronavirus (tested=1), employment status (paid or self-employed=1), log of personal income, weekly hours of work, working from home (home-office=1), taking alternative social security benefits (five dummies for universal credit, working tax credit, jobseekers’ allowance, employment and support allowance), financial satisfaction (satisfied=1), risk of coronavirus infection (five dummies), owning a house (owning=1), household size, age composition of household members (#people aged 0–4, 5–15, 16–18, 19–69, and 70 or more), time spent caring for a dependent person, time spent for daily housework, and using the internet (internet=1). The full set of control variables used in the baseline regressions can be found in Appendix B, Table B.1.
3.1.2. Stochastic specifications
The error specification in (2) include several components. First, we include wave specific effects W w. These are four wave dummies corresponding to the month of interview. Then, we introduce a series of further time functions to capture the time series properties of the daily pandemic cases. First, we control for the day of the week on which the interview is conducted dow s. Second, we add time trend specified in alternative functional forms f(t, W w), including linear, quadratic, and wave-specific quadratic trends. To allow regional heterogeneity within the UK, e.g., to capture regional unobserved attitudes towards the pandemic or alternative lockdown rules, we control for the Government Official Regions (12 GOR dummies ρ r). Finally, by exploiting the panel structure of the dataset, we allow for the time-invariant unobserved individual effects α i (e.g., personality or genetic predisposition). Because pandemic cases are time-variant, we can identify the parameters within a fixed-effects framework where we allow for correlation between observed and unobserved variables.
3.2. Identification
As we merge daily pandemic data with individuals’ mental health observations and other characteristics, the model specification involves a ‘between’ variation, which is distributed across 29 interview days, and a ‘within’ individual variation, which is distributed across four months. The requirement for identifying the “causal” effect of the previous day’s pandemic cases on mental health is that the characteristics of individuals should be similar across the interview days and that there is no sorting of individuals on a particular interview day by the previous day’s local or global pandemic cases. Are these assumptions reasonable? We can imagine some possible threats relating to how the interviews are conducted, attrition, and sorting. First of all, during the pandemic, e.g., due to fear or lockdown restrictions, most people stay at home and interviews are held via digital sources, i.e., internet or phone. Second, there is a very little attrition in the data as the time between waves is very short and the participation rate in the survey is very high. As shown in Appendix A, Table A.1, the interviews are targeted to be conducted during one week of each month and most interviews are held during the first days of the interview week.
Third, we conduct a series of balance tests to check whether the number of interviews conducted in a particular interview day is a function of the previous day’s pandemic cases. Fig. A.1 presents the first balance test, where we calculate the daily number of interviews and relate them to the previous day’s pandemic cases. The figures suggest that there is basically no relationship. To investigate the relationship further, we estimate two model specifications using poisson regressions in which we allow for the linear or quadratic time trend, day of the week dummies, wave dummies, and the UK and global pandemic cases. We find that the parameter estimates of the previous day’s local (0.015, s.e., 0.024) and global (0.002, s.e., 0.003) Covid-19 cases are not statistically significant on the number of interviews. Finally, we focus on confounders generated by sorting of individuals into particular interview days by their observed characteristics (e.g., age, gender, being a couple, owning the house, working from home, income, and employment) as a function of the previous day’s pandemic cases. The results in Table A.2 suggest that there is no statistically significant correlation between the average values of individual characteristics on an interview day and the local and global pandemic cases of the previous day.
Fig. A.1.
Balance Tests 1: Number of Interviews and Previous Day Covid-19 Cases. Note: Authors’ own calculations from Understanding Society (Understanding Society, 2020) and World Health Organisation (WHO, 2020). We obtain the residuals of the #interviews, the local, and global pandemic cases conditional on the time trend, the day of the week, and wave dummies. The solid line is the linear regression based on the underlying 29 observations.
3.2.1. Which estimator should we use?
To be able to exploit the within variation, the convenient model specification is a fixed-effects model. The output variable of interest is an ordinal variable measured on a 36 point-scale, which calls for an ordered probit model. The literature suggests that there are no significant differences between a linear model and an ordered probit (Ferrer-i-Carbonell and Frijters, 2004). We prefer linear fixed-effects model specification as it is easy to estimate and also allows for interpreting the coefficients directly. This model specification also helps us to deal with further confounders leading individuals to be sorted into interview days due to their time-invariant unobserved characteristics. Yet, we note that, as the identification mainly comes from the time variation in pandemic measures, the fixed-effects model and a random-effects model specification are expected to give a similar result in the case when there is no particular sorting by unobservable characteristics. In a rich robustness analysis below, we also investigate the role of estimators.
4. Results
Our strategy of presenting our results is as follows. First, we obtain the baseline results and immediately present a stability analysis and results from the pandemic deaths. Second, interpretation and magnitudes of the results are provided. Third, we present detailed results by using each GHQ item in the inventory as a distinct output variable. Fourth, we conduct an extensive robustness analysis. Finally, an heterogeneity analysis in which we explore the vulnerable and non-vulnerable individuals are given in the next section.
4.1. Local and global mental health effects
4.1.1. Main results
Table 1 provides the baseline estimates and initial checks. Our baseline specification (Eqs. (1) and (2)) uses a linear fixed-effects model, which includes the full set of individuals’ personal and household characteristics as well as the pandemic measures. Column I of Table 1 presents the baseline estimates (see Table B.1 for the full estimation results). The model specification includes the UK and global cases in the same specification. To simplify the presentation of the estimation results, we rescale the pandemic measures by dividing 1000. The parameter estimate of the local number of cases is − 0.161 (s.e. 0.062), while the estimate is − 0.0043 (s.e. 0.001) for the number of global cases. These estimates suggest highly significant mental health effects of the previous day’s (d − 1) local and global cases. At this point, we present an initial check where we estimate the local and global cases in two separate regressions (Columns II and III of Table 1). The estimated coefficients are similar to those of the baseline given in Column I.
Table 1.
Baseline results and initial checks.
| Dep var: “GHQ36" Covid Data: WHO (#cases and #deaths /1000) | I | II | III | IV | V | VI |
|---|---|---|---|---|---|---|
| Local: Covid-19 cases, d-1 | -0.161*** | -0.174* | ||||
| (0.061) | (0.093) | |||||
| Global: Covid-19 cases, d-1 | -0.004*** | -0.004*** | ||||
| (0.001) | (0.001) | |||||
| Local: Covid-19 deaths, d-1 | -0.148 | -0.137 | ||||
| (0.093) | (0.109) | |||||
| Global: Covid-19 deaths, d-1 | -0.035*** | -0.035*** | ||||
| (0.011) | (0.010) | |||||
| #obs. | 57789 | 57789 | 57789 | 57789 | 57789 | 57789 |
| R-squared | 0.017 | 0.016 | 0.016 | 0.016 | 0.016 | 0.016 |
Note: Authors’ own calculations from the Understanding Society (2020) Covid-19 module and WHO Covid-19 data (WHO, 2020). The local and global number of cases and deaths are rescaled by 1000. The model specifications include the full set of individual, regional and time specific characteristics (see Appendix B, Table B.1). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
As mentioned previously, pandemic cases and deaths are highly correlated, and they are expected to give similar information about the prevalence of the pandemic. Nevertheless, to check the consistency, in Columns IV, V, and VI, we present results from the local and global pandemic related deaths. The parameter estimates of the local and global deaths (rescaled by 1000) are also negative and highly comparable with the local pandemic cases. Yet, the coefficient of the local deaths on mental health is imprecisely estimated and only marginally significant with p-value= 0.115. Compared to the estimated parameter of global cases, the relative magnitude of global deaths is more prominent on mental health, and the coefficient is highly statistically significant. One possible interpretation of this result is that people might fear more from the covid related deaths than cases. Yet, this result might also be related to measurement error or the lower level of pandemic related deaths in the UK during the sampling period. In the rest of the paper, we focus only on the local and global cases as the main pandemic measure.
4.2. Magnitudes
4.2.1. Average marginal effects
The results presented in Column I of Table 1 give the effect of pandemic measures on the mental health for 1000 people increase in the local and global cases. In order to calculate the magnitudes for a more realistic local and global pandemic figures, we first calculate the average marginal effect for a standard deviation increase in the pandemic cases. A standard deviation increase in the local (global) cases leads to a − 0.049 (−0.042) standard deviation decrease in the GHQ36 scores. The effect of a standard deviation increase in the local cases is only slightly higher than global cases.5 In order to obtain an easy measure to interpret the results, in Column I of Table 2, we present the percentage change in the mean GHQ36 score (mean GHQ36 is 23.8 while s.d. is 5.91) for a standard deviation increase in the pandemic cases (standard errors are in parentheses). A standard deviation increase in the local (global) cases leads to 1.22% (1.09%) decrease in the mean GHQ36 (about 23.8 × 0.0122 = 0.29 and 23.8 × 0.0109 = 0.26 points on the GHQ36 scale). Another tangible measure is obtained by summing the effects of the local and global pandemic cases. The average total mental health effect of a standard deviation increase in the local and global pandemic cases sums up to 2.31% reduction in the mean GHQ36 scores (0.092 standard deviation of the GHQ36 scores - Column I, Table 2).
Table 2.
Magnitudes, extrapolation of the effect, and sensitivity checks.
| Sampling Period |
First Wave of the Pandemic |
First and Second Waves | ||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III(A) | III(B) | III(C) | IV | |||
| Average Marginal Effect |
29 Interview days (04/24/2020–07/31/2020) |
(01/31/2020–09/01/2020) |
Sensitivity Check 1:Excluding April, 2020 (1th sampling period) |
Sensitivity Check 2: Excluding July, 2020 (4th sampling period) |
(01/31/2020–01/15/2021) |
|||
| Dep var: “GHQ36" Covid Data: WHO |
1 sd. increase (%"change in mean GHQ") |
% “total effect in mean GHQ" |
% “total effect in mean GHQ" |
Parameter Estimates |
% “total effect in mean GHQ" |
Parameter Estimates |
% “total effect in mean GHQ" |
% “total effect in mean GHQ" |
| Local: Covid-19 cases | -1.221 | -1.459 | -1.110 | -0.468** | -3.216 | -0.135** | -0.818 | -5.359 |
| (0.467) | (0.558) | (0.424) | (0.236) | (1.621) | (0.058) | (0.350) | (2.048) | |
| Global: Covid-19 cases | -1.090 | -2.410 | -1.678 | -0.004*** | -1.699 | -0.008*** | -2.795 | -4.237 |
| (0.250) |
(0.505) |
(0.351) |
(0.001) |
(0.560) |
(0.002) |
(0.612) |
(0.887) |
|
| Total in s.d. of GHQ36 |
-0.092 |
-0.155 |
-0.112 |
-0.197 |
-0.145 |
-0.384 |
||
| Total #obs. | 41739 | 44758 | ||||||
| R-squared | 0.009 | 0.007 | ||||||
Note: Authors’ own calculations from the Understanding Society (2020) Covid-19 module and WHO Covid-19 data (WHO, 2020). The model specifications include the full set of individual, regional and time specific characteristics (see Appendix B, Table B.1). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
4.2.2. Total effect of the pandemic
To be able to obtain comparable measures across studies that use alternative identification strategies (e.g., Banks and Xu, 2020; Proto and Quintana-Domeque, 2021; Etheridge and Lisa, 2020) and to develop measures describing the “total effect” of the pandemic, we calculate the ‘non-marginal’ mental health effect for the overall mean pandemic cases relative to the mean GHQ36 score as and . We calculate the total effect of the whole pandemic for i) the sampling period, ii) the first wave of the pandemic, and iii) the first and second waves of the pandemic. First, in Column II of Table 2, we calculate the total effect for the sampling period using the mean pandemic cases for the 29 interview days (April 24, 2020 - July 31, 2020, see Table A.1). The total reduction in the mean mental health of the UK population is about 1.5% for the local cases and 2.4% for the global cases. The total reduction in the mean mental health due to the pandemic cases sums up to 3.9% (1.5 + 2.4). We also express these figures in the standard deviation of GHQ36. The total mental health effect of the pandemic cases is 0.16 standard deviation of GHQ36, which is in line with the existing literature using alternative identification strategies (c.f., Proto and Quintana-Domeque, 2021).
4.2.3. First and second waves of the pandemic
In the remaining columns of Table 2, we conduct a series of extrapolation exercises and sensitivity checks with respect to the sample used in the analysis. First, we extrapolate the total effect for the overall first wave of the pandemic (covering the period about January 31, 2020 - September 1, 2020). Column III(A) suggests that the total effect sums up to 0.11 standard deviation of GHQ36, which is slightly lower, as the mean local and global cases are lower at the beginning and the end of the first wave of the pandemic. At this point, we report two additional sets of checks to investigate the sensitivity of extrapolation with respect to the sample used. We exclude the first sample period of data collected during April, 2020 (the sample size is 41,739) and find that the estimated coefficient for the local cases is about three times larger compared to the baseline specification (Column I, Table 1). The total effect without the first sample period is found to be as large as 0.20 standard deviation of GHQ36 (Column III(B)). Next, we exclude the last wave collected during July, 2020 (the sample size is 44,758). The results are stable and the total effect of the pandemic (Column III(C)) is almost the same sizes as that reported in Column II. Finally, we extrapolate the total effect for a period covering the first and second waves of the pandemic. The period roughly covers a year (January 31, 2020 - January 15, 2021). The results presented in Column IV suggest that the total effect of the pandemic is 0.38 standard deviation of GHQ36 or about 9.6% of the mean GHQ36 (about 2.5 points reduction relative to the mean GHQ36 score).
4.3. Results by each GHQ item
Each item asked in the GHQ inventory can be considered as a proxy for the mental well-being experienced for a particular domain. Thus, we estimate the baseline model specification with twelve different dependent variables. Each item is measured on a 4-point ordinal scale (see Appendix C, Table C.1). A higher value indicates that individuals experience a higher level of mental health issues from a specific domain. The overall results presented in Column I of Table 1 can be considered as an average mental health effect experienced in these domains. The results, presented in the rows and columns of Table 3, are also split by the local and global pandemic cases. First, the pandemic cases (rescaled by 1000 cases) are significantly related to several mental health domains existing in the GHQ36 inventory. Second, the signs of the estimated coefficients are all consistent with the expected directions. For instance, while people experience a lower level of concentration, they experience higher sleep and happiness loss for an increase in the local and global cases. Third, the influence of the pandemic cases on some mental health domains is stronger and the estimates tend to produce a higher degree of statistical significance. Finally, focusing on particular items, people experience higher sleep disturbances (Xiao et al., 2020), higher feelings of depression (e.g., Bueno-Notivol et al., 2021), and importantly, reduced joy and happiness (e.g., Brodeur et al., 2021b) in their life for an increase in the local and global pandemic cases.
Table 3.
Results by each GHQ item.
| Dep var: ordered values (from 1 to 4) of each GHQ item | I | II |
|---|---|---|
| Local: Covid-19 cases | Global: Covid-19 cases | |
| When you are doing something, do you find that.you can concentrate | -0.0454 | -0.0043*** |
| (0.1626) | (0.0016) | |
| Do you often lose sleep over worry? | 0.1872* | 0.0054*** |
| (0.1068) | (0.0018) | |
| Can you play useful part in things? | -0.0819 | -0.0046*** |
| (0.0830) | (0.0014) | |
| Are you capable of making decisions? | -0.3118*** | -0.0016 |
| (0.0789) | (0.0011) | |
| Are you constantly under strain? | -0.1150 | 0.0019 |
| (0.0733) | (0.0017) | |
| Do you feel you couldn’t overcome difficulties? | 0.2582*** | 0.0042** |
| (0.0844) | (0.0016) | |
| Are you able to enjoy day-to-day activities? | 0.0508 | -0.0066*** |
| (0.1039) | (0.0015) | |
| Are you able to face problems? | -0.1670*** | -0.0027*** |
| (0.0614) | (0.0008) | |
| Do you feel depressed? | 0.1975 | 0.0066*** |
| (0.1504) | (0.0021) | |
| Do you always lack confidence? | 0.2369** | 0.0050*** |
| (0.1130) | (0.0016) | |
| Do you often think that you have no value? | 0.1587* | 0.0017 |
| (0.0943) | (0.0016) | |
| Are you happy when you consider each aspect of your life? | -0.1373** | -0.0025* |
| (0.0640) | (0.0014) |
Note: Authors’ own calculations from the Understanding Society (2020) Covid-19 module and WHO Covid-19 data (WHO, 2020). The local and global number of cases are rescaled by 1000. The model specifications include the full set of individual, regional and time specific characteristics (see Appendix B, Table B.1). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
4.4. Robustness
4.4.1. Estimators
Table 4 presents an extensive robustness analysis. To compare the results, we replicated the baseline results in the first row (Column I, Table 1). In Rows II-V, we investigate the robustness of the baseline fixed-effects specification with various alternative specifications. As mentioned above, the ordered probit model is the convenient model in our case as the GHQ36 measure is observed on an ordinal scale. We also note that, as the ordered probit is a non-linear model, the parameter estimates of this model specification cannot be directly compared with the baseline. The results from the cross-sectional ordered probit model are given in Row II. We obtain the same sign and significance levels for both the local and global cases. To account for the ordinal nature of the dependent variable and fixed-effects in a non-linear model, we estimate a “Blow and Cluster" ordered logit fixed-effects model (Row III). The results follow the same signs and the parameter estimates are statistically significant at the conventional levels. Finally, in Rows IV and V, we estimate the model specification with the cross-sectional pooled OLS and panel data linear random-effects model specification. We obtain highly comparable results with those of the baseline.
Table 4.
Robustness.
| Dep var: “GHQ-36" (36 points scale); Covid Data: WHO | I | II |
|---|---|---|
| Local: Covid-19 Cases | Global: Covid-19 Cases | |
| Baseline | ||
| I Baseline specification (Column I, Table 1) | -0.1609*** | -0.0043*** |
| (0.0615) | (0.0009) | |
| Estimators | ||
| II Cross sectional ordered probit model | -0.0061** | -0.0005* |
| (0.0024) | (0.0003) | |
| III “Blow and Cluster" ordered logit fixed-effect model | -0.1033 * | -0.0023** |
| (0.0553) | (0.0010) | |
| IV Cross sectional linear model (OLS) | -0.1263* | -0.0041*** |
| (0.0682) | (0.0016) | |
| V Linear random-effects panel data model | -0.1468*** | -0.0036** |
| (0.0086) | (0.0014) | |
| Time functions | ||
| VI Quadratic trend | -0.1960*** | -0.0053*** |
| (0.0745) | (0.0007) | |
| VII Exponential trend function | -0.1558** | -0.0043*** |
| (0.0626) | (0.0009) | |
| VIII First differences of Covid-19 measures | -0.0240*** | -0.0003** |
| (0.0062) | (0.0001) | |
| IX Wave specific quadratic trend | -0.1900*** | -0.0077*** |
| (0.0685) | (0.0013) | |
| Alternative Covid-19 Dataset | ||
| X Alternative Covid-19 Data 1: UK Government and WHO datasets | -0.1501*** | -0.0035*** |
| (0.0572) | (0.0011) | |
| XI Alternative Covid-19 Data 2: JHU dataset | 0.1814*** | -0.0049*** |
| (0.0358) | (0.0002) | |
| XII Alternative Covid-19 Data 3: EDCD dataset | 0.1120** | -0.0046*** |
| (0.0566) | (0.0001) | |
| XIII Alternative Covid-19 Data 4: Daily average of WHO, JHU, and EDCD datasets | 0.1720*** | -0.0038*** |
| (0.0623) | (0.0009) |
Notes: Authors’ own calculations from the Understanding Society (2020) and World Health Organisation (WHO, 2020), and John Hopkins University Database (JHU, 2020), and European Centre for Disease Prevention and Control (ECDC, 2020). The local and global number of cases are rescaled by 1000. The model specifications include the full set of individual, regional and time specific characteristics (see Appendix B, Table B.1). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
4.4.2. Is the relationship spurious?Time functions
There are different time patterns in the local and global pandemic cases during the sample period (see Fig. 1). To account for time related heterogeneity, our baseline specifications have already used a linear trend term, the day of the week dummies, and wave-specific dummies. First, we introduce the quadratic trend into our baseline model specification (Row VI of Table 4). The estimated parameters are somehow larger in magnitude but they are all negative and the significance levels hold. Second, we add the exponential trend term in the specification and obtain results which are highly similar to the baseline (Row VII). Third, to account for the strong persistence in the time series of Covid-19 measures, we estimate a model with the first differences of Covid-19 measures from day d − 2 to d − 1. We find negative and statistically significant effects for both local and global pandemic cases (Row VIII). Finally, we estimate our model specification with the wave-specific quadratic trend. The signs, sizes, and significance levels of the estimated coefficients are highly in line with those of the baseline (Row IX).
4.4.3. Does the Covid-19 dataset matter?
Our baseline analysis uses the Covid-19 data collected by WHO. To investigate potential measurement error and whether the results are consistent when using another pandemic dataset, we employ data from the UK government, John Hopkins University (JHU) and the European Centre for Disease Prevention and Control (ECDC). The baseline model specification in Eqs. (1) and (2) is first estimated by combining the covid data supplied by the UK governments for the local and WHO data for the global cases. The results reported in Row X of Table 4 are highly similar to those of the baseline, as expected. Then, the baseline model is also estimated by using the JHU and ECDC Covid-19 datasets, and the results are reported in Rows XI and XII, respectively. While the results are highly similar to the JHU dataset, the estimated coefficient for the local cases is somehow lower when we use the ECDC dataset. For a final check, we have estimated the model parameters by using the daily averages of the pandemic measures obtained from the WHO, JHU, and ECDC datasets. The results reported in Row XIII of Table 4 are highly in line with those of the baseline.
5. Discussion: who are the most vulnerable?
Previous results suggest that there is a statistically significant and large mental health effects of the local and global Covid-19 pandemic on the overall population in the UK. The preceding analysis documents heterogeneous effects for various dimensions. People who experience personal, social and household related constraints, and living environment and housing related factors might correlate with the better or worse mental health outcomes of the pandemic. We focus on dimensions relating to i) individuals’ personal constraints (e.g., older people or chronic health conditions), ii) responses of individuals (e.g., exercises or prayer), iii) economic constraints (e.g., working from home or job security), iv) household circumstances (e.g., household composition), and v) constraints in living environment (e.g., no private garden or personal space). The methodology is based on an interaction specification where we interact pandemic cases with specific characteristics S k. The extended model specification replaces the coefficients of pandemic cases β UK and β GL in Eq. (1) with and , where S k is a binary variable defined for each variable k for which we investigate the heterogeneous effect. To be brief, we present only two coefficients for S k = 1 and S k = 0 for each binary variable S k used in the heterogeneity analyses. The hypotheses that we aim to test are and . The results are summarised in Tables 5 and 6 below.
Table 5.
Discussion 1: individual constraints.
| Local: Covid-19 Cases |
Global: Covid-19 Cases |
||||||
|---|---|---|---|---|---|---|---|
| S= 1 | S= 0 | p-value | S= 1 | S= 0 | p-value | ||
| I | Age | -0.184*** | -0.154** | 0.729 | -0.006*** | -0.002*** | 0.000 |
| (S=1: older people, Age>55) | (0.062) | (0.065) | (0.001) | (0.001) | |||
| II | Underlying Health Conditions | -0.176*** | -0.095 | 0.081 | -0.005*** | -0.004** | 0.083 |
| (S=1: presence of a health condition) | (0.068) | (0.061) | (0.001) | (0.001) | |||
| III | Vigiourius activities | -0.178*** | -0.079 | 0.000 | -0.004*** | -0.004*** | 0.383 |
| (S=1: less active) | (0.060) | (0.067) | (0.001) | (0.001) | |||
| IV | Religiosity | -0.195*** | -0.146** | 0.015 | -0.006*** | -0.004*** | 0.017 |
| (S=1: less praying person) | (0.063) | (0.062) | (0.001) | (0.001) | |||
| V | Income | -0.171*** | -0.120* | 0.004 | -0.004*** | -0.004*** | 0.961 |
| (S=1: income less than median) | (0.060) | (0.068) | (0.001) | (0.001) | |||
| VI | Employment Status | -0.186*** | -0.128** | 0.004 | -0.005*** | -0.004*** | 0.475 |
| (S=1: unemployed) | (0.064) | (0.063) | (0.001) | (0.001) | |||
| VII | Work Conditions | -0.178*** | -0.119* | 0.000 | -0.006*** | -0.003** | 0.001 |
| (S=1, not working from home) | (0.062) | (0.061) | (0.001) | (0.001) | |||
| VIII | Job Security Concerns | -0.172*** | -0.092 | 0.000 | -0.004*** | -0.004*** | 0.850 |
| (S=1, high concerns about job security) | (0.063) | (0.064) | (0.001) | (0.001) | |||
| IX | Future Financial Concerns | -0.172*** | -0.103* | 0.011 | -0.004*** | -0.003** | 0.170 |
| (S=1, high concerns about future) | (0.063) | (0.057) | (0.001) | (0.001) | |||
Note: Authors’ own calculations from the Understanding Society (2016) and WHO Covid-19 data (WHO, 2020). The local and global number of cases are rescaled by 1000. The model specifications include the full set of individual, regional and time specific characteristics (see Appendix B, B.1). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
Table 6.
Discussion 2: household characteristics and living environment.
| Local: Covid-19 Cases |
Global: Covid-19 Cases |
||||||
|---|---|---|---|---|---|---|---|
| S= 1 | S= 0 | p-value | S= 1 | S= 0 | p-value | ||
| I | Living Alone | -0.188*** | -0.069 | 0.001 | -0.005*** | -0.002* | 0.000 |
| (S=1: individual is living alone) | (0.062) | (0.064) | (0.001) | (0.001) | |||
| II | Household Size | -0.175*** | -0.164*** | 0.585 | -0.004*** | -0.004*** | 0.336 |
| (S=1: larger households, #members>3) | (0.059) | (0.063) | (0.001) | (0.001) | |||
| III | Dependent Kids | -0.211*** | -0.158** | 0.012 | -0.005*** | -0.004*** | 0.240 |
| (S=1: at least one dependent kid) | (0.065) | (0.062) | (0.001) | (0.001) | |||
| IV | Time-Use | -0.167*** | -0.142** | 0.345 | -0.004*** | -0.004*** | 0.396 |
| (S=1: long time for caring > median) | (0.063) | (0.057) | (0.001) | (0.001) | |||
| VI | House Ownership | -0.172*** | -0.078 | 0.001 | -0.006*** | -0.003** | 0.004 |
| (S=1, not owning the accomodation) | (0.061) | (0.069) | (0.001) | (0.001) | |||
| VI | Mortgage | -0.160** | -0.165*** | 0.737 | -0.004*** | -0.004*** | 0.347 |
| (S=1, have to pay mortgage) | (0.063) | (0.062) | (0.001) | (0.001) | |||
| VII | Size of the Accomodation | -0.171*** | -0.137** | 0.061 | -0.005*** | -0.004*** | 0.015 |
| (S=1, #rooms<3) | (0.063) | (0.058) | (0.001) | (0.001) | |||
| VIII | Private Space: Garden | -0.171*** | -0.125* | 0.043 | -0.005*** | -0.003*** | 0.018 |
| (S=1, there is no garden) | (0.061) | (0.067) | (0.001) | (0.001) | |||
| IX | Priavage Space: Desk/Room | -0.182*** | -0.114* | 0.000 | -0.006*** | -0.002** | 0.000 |
| (S=1, there is no private desk/room) | (0.061) | (0.062) | (0.001) | (0.001) | |||
Note: Authors’ own calculations from the Understanding Society (2016) and WHO Covid-19 data (WHO, 2020). The local and global number of cases are rescaled by 1000. The model specifications include the full set of individual, regional and time specific characteristics (see Appendix B, B.1). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
5.1. Individuals’ constraints
5.1.1. Individual characteristics
The statistics (WHO, 2020) suggest that the mortality risk of coronavirus is higher among older people, and thus these individuals might fear the pandemic more, leading to greater mental health problems. Indeed, Row I of Table 5 suggests that the mental health of older people (older than age 55) is affected more. Yet, the difference in the estimated effects is statistically significant only for the global cases. Another important constraint is the health status of individuals. The statistics also suggest that mortality risk due to coronavirus is higher among people with an underlying health condition, including coronary diseases, stroke, diabetes, and hypertension. The conjecture is that the pandemic creates greater fear and anxiety among individuals with an underlying health condition, which can trigger mental health problems. To investigate this, we generate a dummy variable indicating people who have long-term coronary disease, stroke, diabetes, or hypertension (the share is 7.4%). Row II of Table 5 suggests that people with a long-term baseline health condition experience a significantly higher mental health effect for both the local and global pandemic cases.
5.1.2. Releasing stress
People who do vigorous activities (e.g., home exercises, aerobics, walking, running, and cycling, among others) at home, in their private gardens, or the immediate neighbourhood during lockdown restrictions might cope better with the adverse mental health effects of the pandemic. A large literature already suggests that physical activity plays an important role in managing fear, anxiety, and depression (see, for instance, Paluska and Schwenk, 2000), for a comprehensive review). In Row III of Table 5, we present the mental health effects among people who are doing low and high levels of vigorous activities. The indicator variable is defined among people who are active more than zero hours (41% of the population, mean (median) is 0.46 (0) hours). The results in Row III suggest that people who are active experience significantly lower mental health effects only for the local pandemic. Another activity that might relate to lower stress and coping with adverse events is the religious belief and prayer (Aneshensel et al., 2013). To investigate this, we use the frequency of praying.6 The indicator variable is defined among people who never pray and zero if they sometimes pray (the share is 26.7%). People who pray experience significantly smaller mental health effects from the local and global pandemic cases (Row IV of Table 5).
5.1.3. Current economic constraints
Rows V-IX of Table 5 report the heterogeneous effects with respect to several economic and financial constraints, which can generate stress and anxiety during the pandemic. First, we begin with the low income individuals. The low-income dummy is defined among individuals earning less than the 3rd quartile of the income distribution (about 1501 £ per month). Row V suggests that the mental health of relatively poor individuals is affected significantly more, only for an increase in the local cases. Second, we focus on the individuals who are unemployed during the pandemic (the share is 40%). The mental health effect is significantly larger among the unemployed only for the pandemic cases in the UK. Third, we investigate the mental health effects among individuals who have a possibility of working from home versus those who have to commute to work (the share of home working individuals is 24.6%). People who commute to work during the pandemic might have more fear of contracting coronavirus, and thus their mental health might be affected more. The results reported in Row VII of Table 5 suggest strong evidence confirming this conjecture for both the UK and global cases.
5.1.4. Job and future financial security
Fourth, we focus on the mental health effects among people who are concerned with their job security. The job security measure aims to obtain the individuals’ subjective belief about the likelihood of losing their jobs using the scale from unlikely (0%) to very likely (100%). Using workers who report a positive probability of losing their job, we define an indicator variable for the high job security concerns (the share is 26.4%). The results reported in Row VIII of Table 5 suggest that the mental health effects among people who have high job security concerns are significantly higher for an increase in the pandemic cases in the UK. Finally, we investigate the mental health effects among people who have financial worries about the future. The proxy aims to capture whether people believe that their financial situation is going to be (1) better off than now; (2) worse off than now; and (3) about the same as now. The indicator variable is defined among people who believe that their financial situation is going to be worse off than now (the share is 17.9%) during the future. The estimates reported in Row IX suggest that individuals who have financial worries experience significantly higher mental health effects for an increase in the local pandemic cases.
5.2. Households’ constraints
5.2.1. Household structure
During the lockdown, household composition (e.g., whether living with a partner or household size) might play an important role in mental health. For example, individuals who have spent their time with family members in a larger household with a private garden might experience smaller mental health effects from the pandemic. In Table 6, we present a heterogeneity analysis investigating how household physical and social circumstances relate to the mental health effect of the pandemic. First, we focus on the mental health of individuals who are living alone (the share of people living alone is 30.5%). The results in Row I of Table 6 suggest that people who live without a partner experience significantly higher mental health effects for both the local and global cases.
As reported in a recent study by Brodeur et al. (2021b), loneliness appears to be one of the prominent factors relating to the mental health effects of the pandemic. However, living in a large household (number of household members is greater than 3) does not generate significant differences in the mental health effects of the pandemic (Row II, Table 6). Even though people in larger households might enjoy their time more during restrictions, the risk of coronavirus infection among the family members might also generate anxiety. Next, we investigate the mental health effects of individuals in households with a dependent child (the share is 9.5%), which can be another source of anxiety. Indeed, these individuals experience significantly higher mental health effects for the local cases (Row III, Table 6). A partially similar result is also obtained among the people who spend time (higher than median hours 0) caring for a dependent person (the share is 23.4%). Yet, the differences are not statistically significant in any of the pandemic measures (Row IV, Table 6).
5.2.2. Living environment and housing
The characteristics of individuals’ physical living arrangements and constraints on where individuals reside might be correlated with the mental health effect of the pandemic. To investigate this, we first focus on home ownership (the share is 75.9%). The results presented in Row V of Table 6 suggest that people who do not own the residential house experience a significantly larger mental health effect for both the local and global cases. 21.6% of the house owners pay a mortgage and the financial concerns during the pandemic might trigger further anxiety among these individuals. However, the results in Row VI suggest that the mental health effect is not significantly different among these people. In the last three rows of Table 6, we focus on the physical arrangement of the residential house during the pandemic. People who live in a small house (the number of rooms is less than 3) during the pandemic experience significantly larger mental health problems (Rows VII, Table 6). Finally, we focus on individuals who do not have a private garden (the share is 12.3%) or a private space (room or desk) at their residential place (the share is 67.6%). These individuals experience significantly higher mental health effects for an increase in the local and global cases (Rows VIII and IX, Table 6).
6. Conclusion
Using an original empirical strategy, we investigate the effect of the local and global Covid-19 pandemic on the mental health of the overall population in the UK. The strategy is based on matching the previous day’s local and global pandemic cases with the mental health measures obtained during the interview the next day in a large household survey. Our extensive investigation of alternative functional forms, model specifications, time functions, and alternative Covid-19 datasets suggests that people in the UK experienced lower mental health not only due to the local pandemic but also due to the global spread of the pandemic. For the first time in the literature, the paper also identifies the mental health effects of the first and second waves of the pandemic. In sum, we find that the total mental health effect of the pandemic during the sampling period (April - July, 2020) is about a 3.9% reduction in the average mental health of the UK population. Our extrapolations suggest that the first wave of the pandemic (February - September, 2020) reduced mental health by 2.8%, while the reduction during the first and second waves of the pandemic (February, 2020 - February, 2021) sums up to 9.6%. The results are robust to allowing fixed-effects that capture potential sorting into interview days and other time-invariant unobserved individual characteristics.
There are several important additional results reported in this paper. The paper investigates who is more vulnerable to the adverse mental health effects of the pandemic. We find that older people with a chronic health condition, those who are unemployed or have job security concerns, and people who have to commute to working place experience greater mental health effects of the pandemic. People who are doing exercises and praying often experience lower mental health disturbances. During the pandemic period, the household composition, living environment, and housing play important roles on mental health. We find that lonely people experience very high mental health problems due to the pandemic. Moreover, people with a dependent kid or those living in smaller houses, with no garden, and private space are also found to be more vulnerable for the adverse mental health effects of the Covid-19 pandemic.
These results have important policy implications for the current and future pandemics. First, our detailed heterogeneity results can allow the policymaker to make specific policies for the efficient management of the pandemic, particularly in designing psychological interventions. Second, as one of the tools to reach individuals, the UK government (also WHO) have published online guidelines to raise awareness and to give support on potential adverse mental health effects.7 The information supplied in this paper can help address psychological factors stemming from individual and household constraints, which can help prevent excessive use of mental health care institutions. Finally, one of the limitations of this study is that it does not include an investigation for the role of the vaccination and policy responses of the governments on the mental health outcomes of the individuals. These issues are left for future research as they require further data and identification strategies.
Acknowledgement
This study has received financial support from the Region "Nouvelle-Aquitaine", France, in the framework of the COV-POP project.
Footnotes
We mainly focus on the confirmed cases as a measure of the pandemic instead of using confirmed pandemic deaths or cases and deaths together. One important issue to point out is that the pandemic cases and deaths might involve different degrees of measurement errors. This might be the situation when the pandemic cases and deaths are registered on different dates due to the choices made by governments. For instance, while the number of pandemic related cases supplied by the UK government reflects the exact confirmed cases for a specific day, the pandemic dataset covers deaths within 28 days after being tested positive.
The dataset can be obtained from “https://www.understandingsociety.ac.uk". Further information about the Covid-19 module can be found at the same address “/topic/covid-19".
Datasets can be obtained from the links for WHO data https://covid19.who.int, JHU data https://data.humdata.org and EDCD data https://www.ecdc.europa.eu. See the links to get further information about the methodology of collecting Covid-19 data.
The UK government also supplies local Covid-19 data, which can be downloaded from the internet page as follows: https://coronavirus.data.gov.uk/. The number of people who tested positive and died due to coronavirus are highly similar to the figures supplied by the WHO dataset that we use. We combine the UK government data with other sources in our robustness analysis.
The effect of a standard deviation increase in the local (global) deaths on the mental health is − 0.009 (−0.007). The relative magnitudes are highly comparable between local and global deaths. Yet their absolute sizes are lower and statistically imprecise compared to those of local and global cases.
The data is obtained on a seven-point scale as (1) every day; (2) more than once a week; (3) once a week; (4) at least once a month; (5) only on special holidays; (6) less often; (7) never.
See https://www.gov.uk/government/publications/ and www.who.int for further information.
Appendix A. Distribution of interview days and balance tests
Tables A.1 and A.2, Fig. A.1.
Table A.1.
Distribution of interview days.
| Mean Characteristics (Std.) |
|||||||
|---|---|---|---|---|---|---|---|
| Wave | Date of Interview | #Interviews | Day of the week | Age | Females | Employed | Couples |
| 1 | 24-Apr-20 | 6983 | Friday | 50.2 (16.6) | 0.59 | 0.62 | 0.71 |
| 1 | 25-Apr-20 | 3906 | Saturday | 53.6 (16.8) | 0.58 | 0.57 | 0.73 |
| 1 | 26-Apr-20 | 2481 | Sunday | 52.2 (16.7) | 0.56 | 0.59 | 0.74 |
| 1 | 27-Apr-20 | 1143 | Monday | 53.6 (17.1) | 0.53 | 0.58 | 0.72 |
| 1 | 28-Apr-20 | 520 | Tuesday | 52.6 (17.1) | 0.53 | 0.59 | 0.74 |
| 1 | 29-Apr-20 | 800 | Wednesday | 50.6 (16.5) | 0.58 | 0.69 | 0.69 |
| 1 | 30-Apr-20 | 207 | Thursday | 52.6 (17.1) | 0.52 | 0.61 | 0.67 |
| 2 | 27-May-20 | 6559 | Wednesday | 51.6 (16.1) | 0.61 | 0.61 | 0.68 |
| 2 | 28-May-20 | 3401 | Thursday | 55.1 (16.2) | 0.58 | 0.55 | 0.72 |
| 2 | 29-May-20 | 1818 | Friday | 54.0 (16.7) | 0.56 | 0.57 | 0.71 |
| 2 | 30-May-20 | 668 | Saturday | 54.1 (16.8) | 0.57 | 0.58 | 0.69 |
| 2 | 31-May-20 | 1338 | Sunday | 50.1 (16.4) | 0.54 | 0.67 | 0.68 |
| 2 | 01-Jun-20 | 533 | Monday | 51.0 (16.5) | 0.53 | 0.66 | 0.71 |
| 2 | 02-Jun-20 | 121 | Tuesday | 52.1 (16.1) | 0.55 | 0.61 | 0.69 |
| 3 | 25-Jun-20 | 5688 | Thursday | 52.1 (16.1) | 0.60 | 0.60 | 0.69 |
| 3 | 26-Jun-20 | 3323 | Friday | 56.1 (16.4) | 0.59 | 0.52 | 0.70 |
| 3 | 27-Jun-20 | 2103 | Saturday | 53.6 (16.8) | 0.56 | 0.59 | 0.71 |
| 3 | 28-Jun-20 | 778 | Sunday | 54.9 (16.1) | 0.56 | 0.58 | 0.73 |
| 3 | 29-Jun-20 | 509 | Monday | 54.1 (16.1) | 0.52 | 0.58 | 0.73 |
| 3 | 30-Jun-20 | 1081 | Tuesday | 51.9 (16.3) | 0.56 | 0.68 | 0.69 |
| 3 | 01-Jul-20 | 246 | Wednesday | 52.1 (15.3) | 0.56 | 0.67 | 0.68 |
| 4 | 24-Jul-20 | 5108 | Friday | 52.2 (16.1) | 0.61 | 0.59 | 0.68 |
| 4 | 25-Jul-20 | 3229 | Saturday | 55.9 (16.2) | 0.57 | 0.53 | 0.71 |
| 4 | 26-Jul-20 | 1955 | Sunday | 54.3 (16.3) | 0.57 | 0.58 | 0.72 |
| 4 | 27-Jul-20 | 1013 | Monday | 56.3 (15.8) | 0.54 | 0.55 | 0.74 |
| 4 | 28-Jul-20 | 363 | Tuesday | 55.6 (16.2) | 0.52 | 0.56 | 0.73 |
| 4 | 29-Jul-20 | 899 | Wednesday | 48.8 (16.5) | 0.57 | 0.67 | 0.71 |
| 4 | 30-Jul-20 | 362 | Thursday | 52.5 (15.6) | 0.51 | 0.61 | 0.73 |
| 4 | 31-Jul-20 | 102 | Friday | 51.4 (16.7) | 0.54 | 0.61 | 0.74 |
| #Interviews | 57789 | 52.7 (16.6) | 0.56 | 0.60 | 0.71 | ||
Table A.2.
Balance Tests 2: Selection by Individual Characteristics and Previous Day Covid-19 Cases.
| Dependent variable: | Age | Gender | Living with a |
|---|---|---|---|
| (Female=1) | partner (=1) | ||
| Local: Covid-19 cases | -0.388 | 0.000 | -0.012 |
| (1.588) | (0.029) | (0.041) | |
| Global: Covid-19 cases | 0.041 | 0.001 | -0.001 |
| (0.041) | (0.001) | (0.002) | |
| #obs |
29 |
29 |
29 |
| Dependent variable: |
Employed (=1) |
Income |
Working from home (=1) |
| Local: Covid-19 cases | 0.017 | 0.133 | 0.028 |
| (0.068) | (0.431) | (0.038) | |
| Global: Covid-19 cases | -0.002 | -0.013 | -0.002 |
| (0.002) | (0.010) | (0.001) | |
| #obs | 29 | 29 | 29 |
Note: Authors’ own calculations from Understanding Society (2020) and World Health Organisation (WHO, 2020). The reduced data is obtained by calculating averages by the wave, the day of the week for each individuals characteristics during 29 interview days. The model specifications include time trend, the day of the week dummies, and wave dummies. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
B. Additional results
Table B.1.
Full Estimation Results at the Baseline.
| Control variables | Estimates | Control variables | Estimates |
|---|---|---|---|
| Living with partner | 0.133 | Owner of house (=1) | 0.02 |
| (0.163) | (0.052) | ||
| Tested for coronavirus | 0.356*** | Internet user (=1) | -0.043 |
| (0.101) | (0.233) | ||
| Employed (=1) | 0.598** | Household composition - Aged 0–4 | 0.048 |
| (0.271) | (0.174) | ||
| Log of personal income | 0.015 | Household composition - Aged 5–15 | 0.215 |
| (0.012) | (0.140) | ||
| Weekly working hours | 0.074*** | Household composition - Aged 16–18 | -0.125 |
| (0.026) | (0.153) | ||
| Working from home (home-office) | -0.122 | Household composition - Aged 19–69 | 0.021 |
| (0.080) | (0.073) | ||
| Benefits: Universal credit | -0.278 | Household composition - Aged 70 or older | 0.146 |
| (0.276) | (0.096) | ||
| Benefits: Working tax credit | -0.232 | Time-use: Caring a dependent person | -0.002 |
| (0.189) | (0.003) | ||
| Benefits: Child tax credit | -0.648*** | Time-use: Housework | -0.001 |
| (0.145) | (0.002) | ||
| Benefits: Jobseekers’ allowance | 0.288 | Local: Covid-19 (log) cases | -0.161*** |
| (0.541) | (0.061) | ||
| Benefits: Employment allowance | 0.341 | Global: Covid-19 (log) cases | -0.004*** |
| (0.319) | (0.001) | ||
| Financially satisfied (=1) | 1.152*** | ||
| (0.112) | |||
| Coronavirus risk: Very unlikely | 0.237 | ||
| (0.306) | |||
| Coronavirus risk: Unlikely | 0.064 | ||
| (0.266) | |||
| Coronavirus risk: Likely | 0.188 | ||
| (0.258) | |||
| Coronavirus risk: Very likely | 0.191 | R2-overall | 0.017 |
| (0.247) | #Observations | 57789 |
Note: Authors’ own calculations from Understanding Society (2020) and World Health Organisation (WHO, 2020). Clustered (at the day of the observation) standard errors are presented in the parentheses. *, **, and *** indicate significance level at 10%, 5%, and 1% levels of significance, respectively.
C. Inventories
Table C.1.
GHQ Inventory.
| 1- When you are doing something, do you find that |
| (1) Can concentrate; (2) Attention occasionally diverted; (3) Attention sometimes diverted; (4) Attention frequently diverted, cannot concentrate |
| 2- Do you often lose sleep over worry? |
| (1) Not at all; (2) Occasionally; (3) Fairly often; (4) Very often |
| 3 Can you play useful part in things? |
| (1) Always can; (2) Can play some positive roles; (3) Can play positive roles poorly; (4) Cannot play a positive role |
| 4- Are you capable of making decisions? |
| (1) Always have own opinions; (2) Sometimes have own opinions; (3) Do not have many own opinions; (4) Do not have any personal opinion at all |
| 5- Are you constantly under strain? |
| (1) Never; (2) Sometimes; (3) Fairly often; (4) Very often |
| 6- Do you feel you couldn’t overcome difficulties? |
| (1) Never; (2) Sometimes; (3) Fairly often; (4) Very often |
| 7- Are you able to enjoy day-to-day activities? |
| (1) Very interesting; (2) Fairly interesting; (3) Not very interesting; (4) Not interesting at all |
| 8- Are you able to face problems? |
| (1) Never; (2) Seldom; (3) Sometimes; (4) Always |
| 9- Do you feel depressed? |
| (1) Not at all; (2) A little bit; (3) Fairly seriously; (4) Very seriously |
| 10- Do you always lack confidence? |
| (1) Not at all; (2) A little bit; (3) Fairly seriously; (4) Very seriously |
| 11- Do you often think that you have no value? |
| (1) Not at all; (2) A little bit; (3) Fairly seriously; (4) Very seriously |
| 12- Are you happy when you consider each aspect of your life? |
| (1) Very happy; (2) Fairly happy; (3) Not very happy; (4) Not happy at all |
References
- Akay A., Bargain O., Zimmermann K.F. Relative concerns of rural-to-urban migrants in China. J. Econ. Behav. Organ. 2012;81:421–441. [Google Scholar]
- Akay A., Bargain B.O., Elsayed A. Global terror and well-being. Eur. Econ. Rev. 2020;123 [Google Scholar]
- Aneshensel C.S., Plelan J.C., Bierman A. Handbook of the Sociology of Mental Health. Springer; Dordrecht Heidelberg New York London: 2013. Religion and mental health. [DOI] [Google Scholar]
- Banks J., Xu X. The mental health effects of the first two months of lockdown and social distancing during the Covid-19 pandemic in the UK. Covid Econ. 2020;28:91–118. [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;22(395):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassi M., Negri L., Fave A.D., Accardi R. The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy, Italy. J. Affect. Disord. 2020;280:1–6. doi: 10.1016/j.jad.2020.11.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur A., Gray D., Islam A., Bhuiyan S. A literature review of the economics of COVID-19. J. Econ. Surv. 2021 doi: 10.1111/joes.12423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur A., Clark A.E., Fleche S., Powdthavee N. Assessing the impact of the coronavirus lockdown on unhappiness, loneliness, and boredom using google trends. J. Public Econ. 2021;193 doi: 10.1016/j.jpubeco.2020.104346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno-Notivol J., García P.G., Olay B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021;21 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A., Oswald A. Unhappiness and unemployment. Econ. J. 1994;104:648–659. [Google Scholar]
- Davillas, A., Jones, A.M., 2021. The first wave of the COVID-19 pandemic and its impact on socioeconomic inequality in psychological distress in the UK, IZA DP No. 14057. [DOI] [PMC free article] [PubMed]
- Etheridge B., Lisa S. The gender gap in mental well-being during the Covid-19 outbreak: evidence from the UK. Covid Econ. 2020;33:46–72. [Google Scholar]
- Ferrer-i-Carbonell A., Frijters P. How important is methodology for the estimates of the determinants of happiness? Economic Journal. 2004;114(497):641–659. [Google Scholar]
- Fusar-Poli P., Brambilla P., Solmia M. Learning from COVID-19 pandemic in Northern Italy: impact on mental health and clinical care. J. Affect. Disord. 2020;275:78–79. doi: 10.1016/j.jad.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D.P., Gater R., Sartorius N., Ustun T.B., Piccinelli M., Gureje O., et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997;27(1):191–197. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- Goularte J.F., Serafim S.B., Colombo R., Hogg B., Caldieraro M.A., Rosa A.R. COVID-19 and mental health in brazil: psychiatric symptoms in the general population. J. Psychiatr. Res. 2020;132:32–37. doi: 10.1016/j.jpsychires.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D., Sugden R. Experienced utility as a standard of policy evaluation. Environ. Resour. Econ. 2005;32(1):161–181. [Google Scholar]
- Liem A., Wang C., Wariyanti Y., Latkin C.A., Hall B.J. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4) doi: 10.1016/S2215-0366(20)30076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paluska S.A., Schwenk T.L. Physical activity and mental health. Sports Med. 2000;29(3):167–180. doi: 10.2165/00007256-200029030-00003. [DOI] [PubMed] [Google Scholar]
- Pandya A. A review and retrospective analysis of mental health services provided after the september 11 attacks. Can. J. Psychiatry. 2013;58(3):128–134. doi: 10.1177/070674371305800302. [DOI] [PubMed] [Google Scholar]
- Perez-Arce F., Angrisani M., Bennett D., Darling J., Kapteyn A., Thomas K. COVID-19 vaccines and mental distress. PLoS One. 2021;16(9) doi: 10.1371/journal.pone.0256406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proto E., Quintana-Domeque C. COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLos ONE. 2021;16(1) doi: 10.1371/journal.pone.0244419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatry. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Pacitti F., DiLorenzo G., DiMarco A., Siracusano A., Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the Novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020;74(4):281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shultz J.M., Baingana F., Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. JAMA. 2015;313(6):567–568. doi: 10.1001/jama.2014.17934. [DOI] [PubMed] [Google Scholar]
- Trudeau J.M., Alicea-Planas J., Vásquez W.F. The value of COVID-19 tests in Latin America. Econ. Human Biol. 2020;39 doi: 10.1016/j.ehb.2020.100931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J., Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;S2468–2667(20):30053–30060. doi: 10.1016/S2468-2667(20)30053-0. ([Epub ahead of print]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Essex, 2020. Institute for Social and Economic Research (2020): Understanding Society: COVID-19 Study [data collection], 4th ed. UK Data Service. SN: 8644, 10.5255/UKDA-SN-8644-4.
- World Health Organization, 2020. WHO coronavirus disease (COVID-19) dashboard [WWW Document]. URL 〈https://covid19.who.int/〉. (Accessed 11.25.20).
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Li W., Zhang Q., Zhang L., Cheung T., Xiang Y.-T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4) doi: 10.1016/S2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]