Abstract
Background
Acquired long QT syndrome is an important and preventable cause of cardiac arrest. Certain medications and electrolyte disturbance are common contributors, and often coexist. In this case, we report five contributors to cardiac arrest.
Case presentation
This case is of a 51-year-old Caucasian female patient who presented with vomiting associated with hypokalemia and hypomagnesemia. She subsequently received ondansetron and metoclopramide, on the background of chronic treatment with fluoxetine. She then suffered an in-hospital monitored cardiac arrest, with features of long QT and torsades de pointes retrospectively noted on her prearrest electrocardiogram. She was diagnosed with acquired long QT syndrome, and her QT interval later normalized after removal of offending causes.
Conclusions
This case highlights the importance of proper consideration prior to prescribing QT prolonging medications, especially in patients who have other risk factors for prolonged QT, such as electrolyte disturbances and pretreatment with QT prolonging medications.
Keywords: Acquired long QT syndrome, Torsades de pointes, Ondansetron, Fluoxetine, Metoclopramide, Hypokalemia, Hypomagnesemia, Renewal theory, Case report
Background
Long QT syndrome (LQTS) is complex; a genetically, physiologically, and environmentally multifactorial disorder of cardiac ion channels, which leads to abnormal cardiac repolarization. It is, therefore, a cause of ventricular arrhythmias (VAs), in particular torsades de pointes (TdP) and sudden cardiac death (SCD) [1]. Although much of the interest of cardiologists and researchers is focused on genetic LQTS [2], acquired LQTS has also been recognized as being as “risky” as congenital LQTS [3], and is vastly more common in clinical practice [4]. The prevalence of acquired LQTS is estimated to be 25–30% in hospitalized populations [5], and most commonly occurs in noncardiac units [6]; however, the true incidence of acquired LQTS causing death is likely to be underreported.
Acquired LQTS is commonly caused by medications [7], electrolyte abnormalities [8], structural heart disease, bradyarrhythmias, starvation, hypothermia, toxins, endocrine disease, liver disease, human immunodeficiency virus infection, and inflammation [9]. It is estimated that 5–7% of reports of VAs or SCD are due to drug-induced LQTS and TdP [10]. The “multi-hit theory” suggests that more than one risk factor is required to cause clinical or electrocardiographic manifestations of acquired LQTS [4, 11]. One case series of 11 patients with acquired LQTS revealed all patients had electrolyte abnormalities (including severe hypokalemia), and an average of 2.8 QT prolonging medications administered [12]. In a study of patients admitted to hospital with QT prolongation, 35% of them received QT prolonging medications, commonly leading to further prolongation of the QT interval [5], indicating a genuinely under-appreciated issue. Many cases of TdP can be prevented by careful prescribing [13].
Case presentation
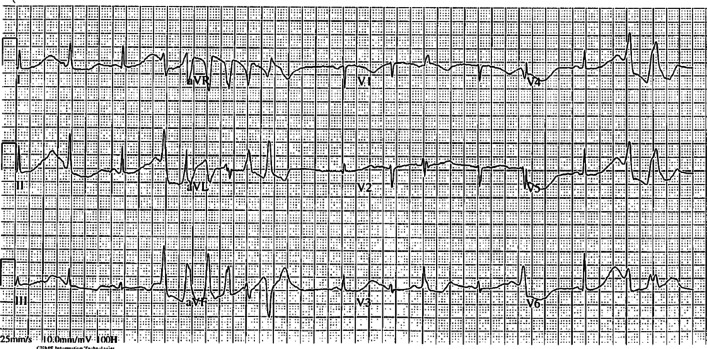
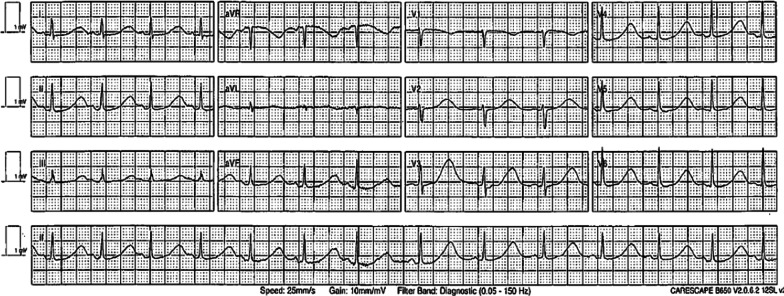
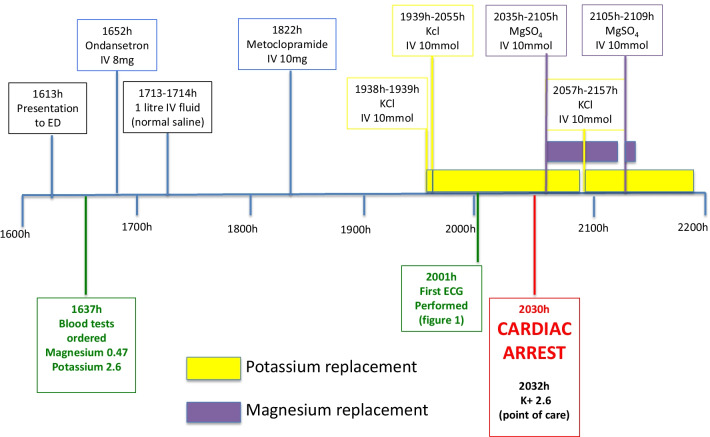
A 51-year-old Caucasian woman presented to the emergency department with several hours of recurrent vomiting, associated with abdominal cramping but no diarrhea. There was no history of unwell contacts or culprit dietary intake, nor was there a history of fevers or any symptoms to suggest another focus of infection. There was no hematemesis or melena. She had no history of illicit drug use. Her past medical history included depression, treated with fluoxetine 20 mg, orally, daily. She had no cardiac history, and no significant family history of sudden cardiac death. She was managed with antiemetics, including ondansetron and metoclopramide, and intravenous fluid rehydration with normal saline. Clinical examination demonstrated dehydration, without any apparent cause of the vomiting detectable on clinical examination. Investigations revealed hypokalemia (2.5 mmol/L) and hypomagnesemia (0.47 mmol/L), and replacement was commenced. Her initial electrocardiogram (ECG), showed sinus rhythm, with corrected QT interval (QTc) of 680 msecond and had nonsustained runs of TdP and T wave alternans (Fig. 1). She then had a witnessed cardiac arrest, with the presenting rhythm of polymorphic ventricular tachycardia. She received 30 seconds of chest compressions and was successfully resuscitated without requirement for defibrillation, and recovered to a normal neurologic baseline. Her postresuscitation ECG (Fig. 2) showed a prolonged QT interval. Her postresuscitation venous blood gas showed a pH of 7.304, bicarbonate of 20.3 mmol/L, sodium of 142 mmol/L, potassium of 2.6 mmol/L, and glucose of 7.5 mmol/L. The sequence of events is represented in Fig. 3. She underwent further cardiac structural assessment, which was normal. Investigations into alternative causes of the vomiting, including septic screening, liver and kidney function testing, and exclusion of pancreatitis did not reveal a specific cause, and her vomiting resolved spontaneously. She was presumed to have had a viral illness. Her QT normalized after several days of observation, following withdrawal of offending medications and replacement of electrolytes, and she was discharged home with a diagnosis of acquired long QT syndrome. At follow up clinic review at 2 months and at 12 months, she remained asymptomatic with a normal QT interval, and will have ongoing follow-up.
Fig. 1.
Electrocardiogram just prior to cardiac arrest, demonstrating very long QT interval, T wave alternans, and short runs of torsades de pointes
Fig. 2.
Electrocardiogram following resuscitation, demonstrating significantly prolonged QT interval
Fig. 3.
Fishbone diagram of presentation, investigations, medications, and infusions administered. ED emergency department, KCl potassium chloride, IV intravenous, MgSO4 magnesium sulfate
Discussion
This case report highlights the “perfect storm” of electrolyte disturbance (potassium, magnesium) and medication effects (fluoxetine, ondansetron, and metoclopramide), leading to acquired long QT syndrome and cardiac arrest.
Ondansetron is known to prolong the QT interval in a dose-dependent manner [14], it is recommended to be used with caution in patients who may develop prolongation of QTc, such as patients with electrolyte abnormalities [15]. Of note, it is very likely for this scenario to occur, as vomiting is not only the indication for administering ondansetron, but is also a risk factor for electrolyte abnormalities and, therefore, QT prolongation.
Fluoxetine is also known to cause prolonged QT interval. The product information suggests it should be used with caution with other clinical conditions that predispose to arrhythmias, such as hypokalemia or hypomagnesemia [16]. Based on a recent comparative review, fluoxetine was reported to have one of the lower risk profiles of its class for causing QT prolongation, along with sertraline and fluvoxamine [17]. Prescription of selective serotonin reuptake inhibitors (SSRIs) is so common in the community that even a rare side effect will be observed. In 2018–2019, 17.1% of the Australian population received a mental health-related prescription, 70.9% of these were antidepressants, and SSRIs are first line antidepressants [18]. These rates are increasing with time, indicating a growing percentage of our population with a baseline risk factor for QT prolongation, even prior to acute illness.
Although metoclopramide on its own is not listed as a QT prolonging medication, and no warnings about QT prolongation exist on its product information, there is evidence that it can contribute to QT prolongation. There are reports of important pharmacokinetic and pharmacodynamic drug–drug interactions that can contribute to QTc prolongation, especially with ondansetron [19]. In addition, metoclopramide has been mechanistically shown to change QT dynamics [20], as well as showing a signal in epidemiological research [21]. It has been added to crediblemeds.org as a “TdP conditional drug” [22], meaning that in combination with other medications, it may prolong the QT interval and increase the risk of TdP.
Despite the good clinical outcome in this case, mortality of cardiac arrest survivors remains high, even when the underlying cause was transient or correctable [23]. Some authors have suggested implantable defibrillators may beneficial, even in this situation of an acquired proarrhythmic state [24]. The patient presented in this case was assessed to have acquired long QT syndrome, rather than congenital long QT syndrome based on the normalization of the QT interval following removal of the five precipitating factors. Following removal of the precipitants, the patient’s Schwartz score for diagnosis of congenital LQTS was 0, indicating low risk of the congenital condition. Given the tendency demonstrated towards prolonged QT with precipitating conditions, however, she will have ongoing clinical electrophysiology review to monitor her symptoms and QT interval.
The patient in this case feels she did not understand what was happening to her, or why it was happening. She does fear another cardiac arrest, which is impacting on her life.
In this case, we make the observation that TdP is self-limited after a number of seconds in the first ECG, with no patient symptoms, and subsequently only a few minutes later, TdP is prolonged, leading to the devastating consequence of cardiac arrest. We do not currently understand what causes TdP to self-terminate, or to continue [1]. Perhaps this could be understood by studying TdP from a wavefront dynamic perspective, given the observations that QRS morphology often abruptly switches from positive to negative during the warm-up phenomenon [11]. A characteristic feature of TdP is that the vast majority of polymorphic ventricular arrhythmia episodes are self-terminating, as observed in this case. The mechanisms underlying this repetitive pattern of self-termination, and what distinguishes TdP from more sustained forms of ventricular fibrillation, are currently unclear. Our group has recently extensively been studying arrhythmia self-termination in atrial fibrillation and ventricular fibrillation. In self-terminating epochs, it appears that the rate of reentrant rotor formation and destruction is much slower compared with more sustained arrhythmia epochs. We have developed a novel statistical framework based on renewal theory to characterize these differences [25–27]. It would be of significant interest to extend these approaches to the clinical scenario of TdP, which would allow us to gain insight into the optimal prophylactic and treatment strategies for this form of arrhythmia.
Conclusion
This case serves as an important reminder that vomiting leads to both electrolyte disturbances and the prescription of antiemetics, which here led to a quadruple hit (hypokalemia, hypomagnesemia, ondansetron, metoclopramide) causing TdP and cardiac arrest. SSRIs are so commonly prescribed, that 1 in 6 patients may have this preexisting risk factor for TdP, as this patient did, contributing to the multiple hits required for clinical manifestations of acquired LQTS. This case occurred in a monitored hospital emergency room, and the patient had a favorable outcome. However, there is a genuine risk of fatal outcomes from a similar situation for a patient in the ambulatory setting, where patients can present with vomiting and are often given antiemetics without performing biochemistry or clinical observation.
Take home message
This case illustrates the clinical teaching point that care must be taken to avoid multiple “hits” that contribute to QT prolongation. The commonly available antiemetics have all been associated with QT prolongation to some extent, so if antiemetic therapy is needed in the future for this patient, care must be taken to check electrolytes and monitor the QT interval during treatment. In such a patient, SSRI treatment in the future should be considered on a risk versus benefit basis. If indicated, fluoxetine, along with sertraline and fluvoxamine are least QT prolonging SSRIs. These may be given, but careful attention must be paid to monitoring the QT interval and avoiding other risk factors for QT prolongation.
Acknowledgements
Not applicable.
Abbreviations
- LQTS
Long QT syndrome
- VA
Ventricular arrhythmias
- TdP
Torsades de pointes
- SCD
Sudden cardiac death
- ECG
Electrocardiogram
- QTc
Corrected QT interval
- SSRI
Selective serotonin reuptake inhibitor
- ED
Emergency department
- KCl
Potassium chloride
- MgSO4
Magnesium sulfate
Authors’ contributions
KT wrote the manuscript; DD, JQ, AL, KWS, and AG had scientific contribution and input into the final manuscript. All authors read and approved the final manuscript.
Funding
Nil funding required.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not required.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schwartz PJ, Crotti L, Insolia R. Long-QT syndrome: from genetics to management. Circ Arrhythm Electrophysiol. 2012;5(4):868–877. doi: 10.1161/CIRCEP.111.962019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waddell-Smith KE, Skinner JR, C.G.C.W.G. members of the Update on the diagnosis and management of familial long QT syndrome. Heart Lung Circ. 2016;25(8):769–776. doi: 10.1016/j.hlc.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 3.Wong LC, Behr ER. Acquired long QT syndrome: as risky as congenital long QT syndrome? Europace. 2012;14(3):310–311. doi: 10.1093/europace/eur372. [DOI] [PubMed] [Google Scholar]
- 4.El-Sherif N, Turitto G, Boutjdir M. Acquired long QT syndrome and electrophysiology of Torsade de Pointes. Arrhythm Electrophysiol Rev. 2019;8(2):122–130. doi: 10.15420/aer.2019.8.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tisdale JE, et al. Prevalence of QT interval prolongation in patients admitted to cardiac care units and frequency of subsequent administration of QT interval-prolonging drugs. Drug Saf. 2012;35(6):459–470. doi: 10.2165/11598160-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.Yu H, et al. Acquired long QT syndrome in hospitalized patients. Heart Rhythm. 2017;14(7):974–978. doi: 10.1016/j.hrthm.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62(4):760–781. doi: 10.1124/pr.110.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Sherif N, Turitto G. Electrolyte disorders and arrhythmogenesis. Cardiol J. 2011;18(3):233–245. [PubMed] [Google Scholar]
- 9.Lazzerini PE, Capecchi PL, Laghi-Pasini F. Long QT syndrome: an emerging role for inflammation and immunity. Front Cardiovasc Med. 2015;2:26. doi: 10.3389/fcvm.2015.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molokhia M, et al. Case ascertainment and estimated incidence of drug-induced long-QT syndrome: study in Southwest France. Br J Clin Pharmacol. 2008;66(3):386–395. doi: 10.1111/j.1365-2125.2008.03229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drew BJ, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047–1060. doi: 10.1161/CIRCULATIONAHA.109.192704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Digby GC, et al. Acquired long QT interval: a case series of multifactorial QT prolongation. Clin Cardiol. 2011;34(9):577–582. doi: 10.1002/clc.20945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas SH, Behr ER. Pharmacological treatment of acquired QT prolongation and torsades de pointes. Br J Clin Pharmacol. 2016;81(3):420–427. doi: 10.1111/bcp.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MIMS online. Ondansetron MIMS Full Product Information. 2020. https://www-mimsonline-com-au.salus.idm.oclc.org/Search/FullPI.aspx?ModuleName=Product%20Info%26searchKeyword=ondansetron%26PreviousPage=~/Search/QuickSearch.aspx%26SearchType=%26ID=90140001_2#Precautions8812
- 15.Administration TG. Ondansetron consumer medicines information. 2021. https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2009-CMI-00741-3&d=202104011016933.
- 16.Administration TG. Australian product information APO-fluoxetine. 2018. https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-01265-3.
- 17.Funk KA, Bostwick JR. A comparison of the risk of QT prolongation among SSRIs. Ann Pharmacother. 2013;47(10):1330–1341. doi: 10.1177/1060028013501994. [DOI] [PubMed] [Google Scholar]
- 18.Australian Institute for Health and Welfare. Mental health services in Australia. 2021. https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/mental-health-related-prescriptions.
- 19.Fernandes FM, et al. Assessment of the risk of QT-interval prolongation associated with potential drug-drug interactions in patients admitted to intensive care units. Saudi Pharm J. 2019;27(2):229–234. doi: 10.1016/j.jsps.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellidokuz E, Kaya D. The effect of metoclopramide on QT dynamicity: double-blind, placebo-controlled, cross-over study in healthy male volunteers. Aliment Pharmacol Ther. 2003;18(1):151–155. doi: 10.1046/j.1365-2036.2003.01641.x. [DOI] [PubMed] [Google Scholar]
- 21.Sarganas G, et al. Epidemiology of symptomatic drug-induced long QT syndrome and Torsade de Pointes in Germany. Europace. 2014;16(1):101–108. doi: 10.1093/europace/eut214. [DOI] [PubMed] [Google Scholar]
- 22.CredibleMeds.com. CredibleMeds. 2014. https://www.crediblemeds.org/blog/two-medicines-added-tdp-conditional-risk-list/.
- 23.Al-Khatib SM, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018;138(13):e272–e391. doi: 10.1161/CIR.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 24.Monnig G, et al. Role of implantable cardioverter defibrillator therapy in patients with acquired long QT syndrome: a long-term follow-up. Europace. 2012;14(3):396–401. doi: 10.1093/europace/eur316. [DOI] [PubMed] [Google Scholar]
- 25.Dharmaprani D, et al. M/M/infinity birth-death processes—a quantitative representational framework to summarize and explain phase singularity and wavelet dynamics in atrial fibrillation. Front Physiol. 2020;11:616866. doi: 10.3389/fphys.2020.616866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dharmaprani D, et al. Renewal theory as a universal quantitative framework to characterize phase singularity regeneration in mammalian cardiac fibrillation. Circ Arrhythm Electrophysiol. 2019;12(12):e007569. doi: 10.1161/CIRCEP.119.007569. [DOI] [PubMed] [Google Scholar]
- 27.Quah JX, Dharmaprani D, Lahiri A, Tiver K, Ganesan AN. Reconceptualising atrial fibrillation using renewal theory: a novel approach to the assessment of atrial fibrillation dynamics. Arrhythm Electrophysiol Rev. 2021;10:77–84. doi: 10.15420/aer.2020.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.