Abstract
People living with severe mental illness (SMI) are one of the most marginalized groups in society. Interventions which aim to improve their social and economic participation are of crucial importance to clinicians, policy‐makers and people with SMI themselves. We conducted a systematic review of the literature on social interventions for people with SMI published since 2016 and collated our findings through narrative synthesis. We found an encouragingly large amount of research in this field, and 72 papers met our inclusion criteria. Over half reported on the effectiveness of interventions delivered at the service level (supported accommodation, education or employment), while the remainder targeted individuals directly (community participation, family interventions, peer‐led/supported interventions, social skills training). We identified good evidence for the Housing First model of supported accommodation, for the Individual Placement and Support model of supported employment, and for family psychoeducation, with the caveat that a range of models are nonetheless required to meet the varied housing, employment and family‐related needs of individuals. Our findings also highlighted the importance of contextual factors and the need to make local adaptations when “importing” interventions from elsewhere. We found that augmentation strategies to enhance the effectiveness of social interventions (particularly supported employment and social skills training) by addressing cognitive impairments did not lead to transferable “real life” skills despite improvements in cognitive function. We also identified an emerging evidence base for peer‐led/supported interventions, recovery colleges and other interventions to support community participation. We concluded that social interventions have considerable benefits but are arguably the most complex in the mental health field, and require multi‐level stakeholder commitment and investment for successful implementation.
Keywords: Social interventions, severe mental illness, community‐based interventions, supported accommodation, supported education, supported employment, community participation, family interventions, peer‐supported interventions, social skills training
The high social and economic costs of severe mental illness (SMI) are well recognized, with clear negative impacts on patients, their families and the wider society1, 2. The World Economic Forum has estimated that mental ill‐health will account for more than half the global economic burden attributable to non‐communicable diseases by 2030 3 . People with SMI are at greater risk of poverty, unemployment and poor housing, factors which impact negatively on their social inclusion and exacerbate mental ill‐health. Consequently, clinicians, policy‐makers and many other stakeholders are interested in improving social outcomes for this group. Yet, this has proved to be a very challenging task.
The World Health Organization (WHO) Mental Health Action Plan (2013‐2030) 4 specifically emphasizes the need to implement comprehensive, integrated and responsive mental health and social care services in community‐based settings so that “persons affected by these disorders are able to exercise the full range of human rights and to access high‐quality, culturally‐appropriate health and social care in a timely way to promote recovery, in order to attain the highest possible level of health and participate fully in society and at work, free from stigmatization and discrimination”. Similarly, the Australian Government's Productivity Commission (2020) 5 states that “housing, employment services and services that help a person engage with and integrate back into the community, can be as, or more, important than healthcare in supporting a person's recovery”.
However, despite these and many other calls and concerted efforts over recent decades to develop services that can enable people with severe mental health problems to integrate into their local communities, these people remain one of the most excluded groups in society 6 . In the second national survey of psychosis in Australia, only one third of people experiencing a psychotic disorder was employed, and these people were more than twice as likely to report loneliness compared with the general population 7 .
Whilst this situation is in part due to stigma and discrimination, as well as inadequacies in service provision and mental health systems that continue to institutionalize individuals with more complex problems8, 9, symptoms of the illness itself also contribute. Around a third of people diagnosed with schizophrenia have positive symptoms (delusions and hallucinations) that do not respond to medication10, 11, and negative symptoms and cognitive impairments associated with more severe psychosis impair people's motivation and social skills. These problems create barriers for social inclusion by impacting on the person's ability to build and sustain relationships and to engage in work, education and other community activities12, 13, 14.
Nevertheless, there is a growing body of consumer‐oriented literature which validates the importance of personal recovery from mental illness, which is not defined by the presence or absence of symptoms but by valued social roles and relationships15, 16. There is, therefore, an obvious need to address the social impact of SMI and thus interrupt its bidirectional, negatively reinforcing relationship with social exclusion. Yet, the evidence base to support investment in social interventions has tended to lag behind that concerning pharmacological and psychological therapies, possibly due to their complex nature and the associated challenges they pose in terms of robust study design. Furthermore, due to their complexity, even when supported by good evidence, social interventions are typically more difficult to implement in practice compared with pharmacological (and even psychological) therapies and require commitment and support from multiple stakeholders across the policy and provider spectrum 17 .
Perhaps a more fundamental issue is the lack of clarity about exactly what is meant by a “social intervention”. For example, the UK National Institute for Health and Care Excellence (NICE) guideline on the prevention and management of psychosis and schizophrenia in adults 18 categorizes family interventions under psychological therapies (along with cognitive behavioral therapy and art therapies) in one section and under “psychosocial interventions” in another, but does not use the terms “psychosocial” or “social” in relation to its section on interventions that enable employment, education and occupational activities.
These difficulties with nomenclature are understandable but problematic. If we consider the example of family interventions, these need to be delivered by well‐trained professionals (often, but not exclusively, clinical psychologists) and draw on underpinning psychological theories, and it seems reasonable, therefore, to consider them as psychological interventions. However, they target the individual's immediate social network and aim to impact positively on social outcomes for both service users and carers (for example, through better family relationships and reducing the emotional strain experienced by family members). The term “psychosocial” addresses this issue, but has tended to be used as a catch‐all for any intervention that is not a medicinal or biomedical one.
This term also often conflates models of care with interventions that more specifically target the individual. For example, intensive case management is a well‐described, manualized and internationally recognized model of community‐based multidisciplinary support provided to people with severe mental health problems who are high users of inpatient care. Its effectiveness in reducing inpatient service use is well established (particularly when implemented in settings that have high levels of provision of inpatient services and less developed community services) 19 . However, it is not a psychological or social intervention in itself, but rather a vehicle for the delivery of pharmacological, psychological and social interventions. Despite this, it is often referred to as a psychosocial intervention. Other models of care (such as supported accommodation and supported employment) appear more obviously “social” both in content and in what they aim to achieve and thus, arguably, have a better fit with the term “social intervention”.
Adding to the complexity, there is an increasing interest in peer‐led or co‐led interventions for people with mental health problems, which, by definition, have a “social” component (the “peer” element) but are not commonly described as “social” interventions, despite an emphasis on promoting choice, control and agency.
An additional problem for researchers is that social outcomes are not always well defined, which impacts on how reliably they can be measured. More objective outcomes, such as employment or stable housing, can be operationalized relatively easily, but concepts such as quality of life tend to be more subjective and thus more difficult to assess, not least because they can be confounded by symptoms of the mental illness itself 20 .
A further issue is context. Whilst the belief that schizophrenia and other SMI has a better social prognosis in non‐industrialized societies is no longer universally accepted 21 , there are major challenges associated with the delivery of effective social interventions to enhance social outcomes in less economically developed settings, including sociocultural factors such as the availability of family support, the impact of industrialization, stigma, discrimination, inadequate protection of human rights, and limited access to services 22 . Furthermore, there are even greater barriers to providing and researching social interventions in low‐ and middle‐income (LAMI) than higher‐income countries, due to the limited availability of human and financial resources.
Given these multiple considerations, we focused this review on interventions that were clearly social in content and aimed to improve social outcomes; specifically, those that aimed to improve social and economic participation for people with SMI. We included studies conducted in LAMI countries as well as those from high‐income countries.
METHODS
We conducted a systematic review of the recent literature on models of care and interventions for individuals with SMI for the Australian Royal Commission into Victoria's Mental Health System 23 . The present review includes a subset of identified studies that reported on the effectiveness and/or cost‐effectiveness of community‐based models of care and interventions that had the overarching aim of supporting social inclusion.
Search strategy, inclusion and exclusion criteria
Our search was conducted in July 2020 using Medline, EMBASE, PsycInfo, CINAHL and Cochrane databases, and included peer‐reviewed papers published between January 2016 and July 2020. Our search terms (key words and MeSH terms) reflected three central concepts: “severe mental illness”, “models of care and/or interventions”, and “outcome and experience measurement” (full search string available on request). We limited our search to publications in English and available in full text. Authors were contacted for relevant papers if the full text could not be accessed.
Inclusion criteria for the original search were: a) models of care for adults aged 18 to 65 years with severe and persistent mental illness; b) group or individual interventions that could be delivered alone or through an identified model of care. For example, Individual Placement and Support is a model of care (a form of supported employment), whereas family psychoeducation is an intervention. Additional inclusion criteria for the present review were: c) community‐based models and interventions that aimed to improve social inclusion (i.e., supported accommodation, supported education, supported employment, community participation interventions, family interventions, peer‐supported/developed/led interventions; social skills training interventions); d) studies that evaluated models of care or interventions for people with SMI, defined as a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, or other severe and enduring psychotic disorder. Studies reporting on models of care or interventions that also comprised a peer component were included within the relevant category. The separate peer‐led/supported interventions category included studies where the peer component was not delivered as part of one of the other included models of care or interventions.
Exclusion criteria were: a) studies conducted in environments other than the community, for example inpatient units or prisons; b) studies that focused on individuals with a primary diagnosis of personality, depressive or anxiety disorder, substance use disorder, acquired brain injury, intellectual disability, or trauma due to natural disasters or military service; c) studies where fewer than 50% of the sample met our SMI diagnostic inclusion criteria (see above); d) studies that did not report on any relevant social outcomes; e) publications that did not report primary empirical data, such as reviews, editorials and commentaries.
Social outcomes were broadly defined to include any indicator of improved social or economic participation. For example, for studies evaluating supported accommodation, we included those reporting on housing stability or progression to more independent accommodation; for studies of supported employment or supported education, we included those reporting outcomes related to gaining or sustaining employment in a competitive, paid or unpaid post, or engagement in mainstream or supported study or volunteering. Outcomes of interest for studies of family interventions included measures of family functioning such as expressed emotion and carer burden. Whilst not measured at the individual service user level, these are appropriate to the aims of this review since supportive, healthy family relationships are crucial to most people's recovery and social and community participation 24 . In addition, it is well established that high expressed emotion within the family is a risk factor for relapse and is highly correlated with carer burden 25 . Thus, family interventions often aim to reduce one or both of these. For other interventions, outcomes included measures of social skills, social functioning, engagement in community‐based activities, social connection, self‐efficacy, hope and empowerment.
Study selection
Results of the original search undertaken for the Victorian Royal Commission were screened using the Covidence online software (https://www.covidence.org). After duplicates were removed, reviewers screened by title, abstract and full text. All disagreements were resolved through consulting with the project lead.
The Royal Commission review identified 313 papers. For the present review, an additional 15 papers reporting on studies conducted in LAMI countries (that were excluded from the Royal Commission review) plus eight hand‐searched papers were included in the pool, giving a total of 336 papers.
Publications were selected from these 336 using Covidence on the basis of the inclusion and exclusion criteria described above. A team of six reviewers screened by title, abstract and full text, with each study requiring two “yes” votes at each stage to be included. All conflicting votes were resolved by an independent third reviewer.
Quality of evidence
Primary papers were evaluated by the Kmet standard criteria to assess methodological quality of both quantitative and qualitative research 26 . Quantitative papers were rated on 14 items and qualitative papers on 10 items, related to the study design, participant selection, data analysis methods, and the clarity and interpretation of results. Each paper was rated by one reviewer and validated through discussion between reviewers at weekly meetings to ensure consistency in rating. Total scores were reported out of 100 (i.e., as percentage equivalents) to take account of non‐applicable items.
We developed a data extraction table and guidance notes to assist consistency in the synthesis of findings from studies in each of the seven models of care/community interventions. One co‐author produced a textual summary for each social intervention category, and each summary was then reviewed by both first authors. The textual summaries were then refined and finalized through consensus discussion within the author group.
Narrative synthesis
Given the range of models of care and interventions included, we chose a narrative synthesis approach to summarize our findings. Narrative synthesis includes: a preliminary synthesis to identify patterns of findings across included studies; exploration of whether effects of an intervention vary according to study population; identification of factors that may influence the results within individual studies and explain difference in findings between studies; development of a theoretical framework underpinning specific intervention effects; assessment of the robustness of the synthesis based on the strength of evidence; discussion of the generalizability of conclusions to wider populations and contexts 27 .
Since our review included multiple social interventions, we did not aim to address the development of a theoretical framework underpinning the effects of each intervention. However, factors that might be relevant to the effectiveness and implementation across our included social interventions were summarized.
RESULTS
We identified 72 studies meeting our eligibility criteria (see Figure 1).
Figure 1.
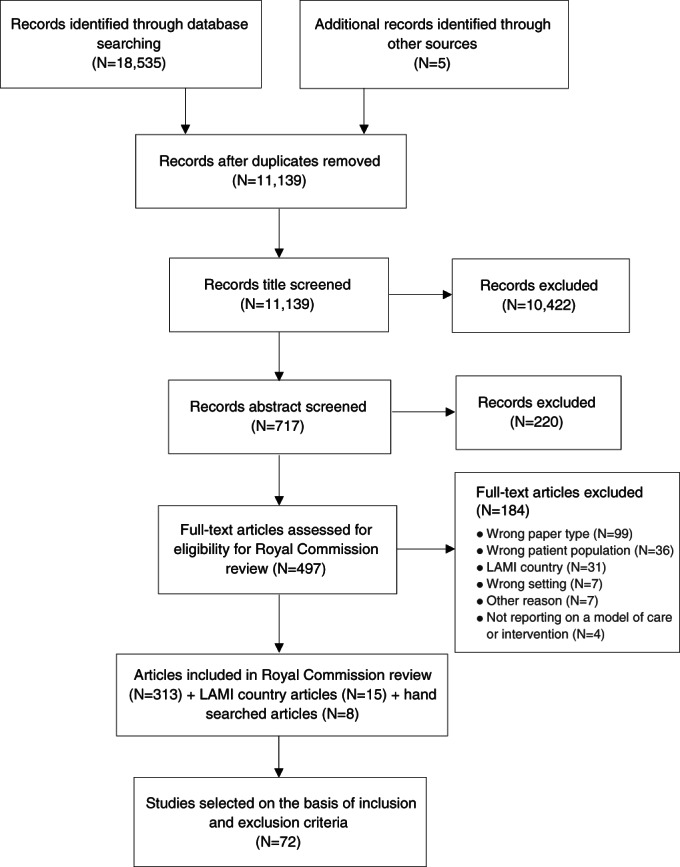
PRISMA flow chart. LAMI – low‐ and middle‐income
Over half (41/72) of the included studies reported on the effectiveness of social interventions delivered at the service level (supported accommodation, supported education, supported employment), and the remainder evaluated interventions targeting people with SMI directly (community participation, family interventions, peer‐developed/led/supported interventions, social skills training). A summary of the characteristics and quality ratings of included studies is provided in Tables 1, 2, 3.
Table 1.
Characteristics of included supported accommodation and supported education studies
| Country | Study design | Study population | Kmet score/100 (quant.) | Kmet score/100 (qual.) | Social outcomes investigated | Key findings | |
|---|---|---|---|---|---|---|---|
|
Supported accommodation studies | |||||||
|
Aubry et al 28 |
Canada | Non‐blinded RCT comparing HF+ACT with TAU |
Homeless adults with SMI |
92 | Outcomes at 24 months. Primary: housing stability. Secondary: community integration. | HF+ACT group had greater housing stability. No difference between groups in community functioning. | |
|
Bitter at al29 |
The Netherlands | Non‐blinded cluster RCT comparing supported housing staff training in recovery‐based practice with TAU |
Adults with SMI |
92 | Outcomes at 20 months. Primary: social functioning and personal recovery. Secondary: empowerment, hope, self‐efficacy. | No difference between groups in outcomes. | |
|
Brown et al 30 |
US | Pre‐post case‐control study comparing HF+ ACT with TAU | Homeless adults with SMI | 91 | Housing stability over the 12 months before and after intervention or TAU period. | HF+ACT group had greater housing stability. | |
| Gutman et al 31 | UK | Case‐control study comparing supported housing transition program with TAU | Homeless men with SMI | 45 | Primary outcome at 6 months: successful move to supported housing. | Intervention group more likely to have successful move to supported housing. | |
| Holmes et al 32 | Australia | Retrospective non‐controlled pre‐post evaluation of supported housing | Homeless adults with mental health problems | 45 | Housing stability and evictions 2 years before and after moving to the project. | Those with SMI less likely to be evicted than other clients. | |
| Killaspy et al 33 | UK | National survey of supported accommodation services in England | Adults with SMI | 100 |
Cross‐sectional survey. Primary: autonomy and social inclusion. Secondary: costs of care. |
Residential care (RC) and supported housing (SH) had clients with more severe mental illness than floating outreach (FO). Autonomy greatest for SH. SH and FO more socially included than RC. RC most expensive. | |
| Killaspy et al 34 | UK |
Cohort study of participants surveyed in Killaspy et al 33 |
Adults with SMI | 100 | Outcomes at 30 months. Primary: successful move to more independent accommodation. Secondary: costs of care. | 41% moved‐on successfully with associated lower inpatient and community mental health service costs. Move‐on was most likely for FO clients. | |
| Somers et al 35 | Canada | Non‐blinded RCT comparing HF+ACT (scattered housing) vs. HF+ACT (congregate housing) vs. TAU |
Homeless adults with SMI |
92 | Outcomes at 24 months. Primary: housing stability. Secondary: community integration. |
HF+ACT in both scattered and congregate site groups had greater housing stability than TAU. Community integration better than TAU for congregate HF+ACT group. |
|
| Stergiopoulos et al 36 | Canada | Non‐blinded RCT comparing HF+ACT with TAU |
Homeless adults with SMI |
92 | Outcomes at 24 months. Primary: housing stability. Secondary: community integration. |
HF+ACT group had greater housing stability and community integration. |
|
| Macnaughton et al 37 | Canada | Qualitative process evaluation of HF implementation in six regions | HF staff and stakeholders, training and process documents | 92 | Implementation of HF in different contexts. |
Training and support critical for HF staff. Training flexible enough to accommodate different contexts and policy imperatives. |
|
| Padamaker et al 38 | India | Qualitative study of move from long‐term institution to supported housing | Women with SMI and focus group with staff | 40 | Service user and staff experiences of the move. | Gradual improvement in women's functioning and confidence and acceptance by neighbours. | |
| Rhenter et al 39 | France | Qualitative study of participants of RCT comparing HF with TAU | Homeless adults with SMI who received HF | 100 |
Housing and recovery experiences before and after move to HF service. |
Importance of stable housing as “a refuge” that prompts reflection and instils hope. | |
| Roos et al 40 | Norway | Qualitative study of sheltered housing services | Adults with SMI | 90 | Clients’ experiences of the services. | Clients liked having self‐contained apartment plus shared space to socialize and do activities with others. Main issue was time‐limited nature of service. | |
| Stanhope et al 41 | US | Qualitative study of supportive housing projects | Staff of services for homeless adults with SMI | 85 | Case managers’ views on purpose and delivery of the service. |
Staff were overly focused on medication management. |
|
| Stergiopoulos et al 42 | Canada | Qualitative process evaluation of implementation of HF | HF managers, housing providers and case managers | 90 | Facilitators and barriers to implementation of HF. | Facilitators: shared commitment to HF philosophy; shared caseload; monitoring fidelity. Barriers: lack of housing availability; inadequate frequency of client contacts; lack of service user involvement. | |
| Worton et al 43 | Canada | Qualitative process evaluation of implementation of HF in six regions |
HF staff and stakeholders, training and process documents |
92 | Facilitators and barriers to implementation of HF in different contexts. |
Facilitators: stakeholders engaged; resources; local champions; staff trained and supervised, able to adapt model to local context; outcome monitoring. Barriers: lack of structures to align key agencies; staff resistance. |
|
|
Supported education studies | |||||||
| Ebrahim et al 46 | UK |
Non‐controlled, mixed methods pre‐post evaluation of a recovery college |
Recovery college students |
55 | 40 | Outcomes assessed through feedback forms at end of each course: empowerment, well‐being, confidence and free‐text comments. | Students felt more empowered and experienced improved well‐being and confidence. College was enabling, promoted hope and social connection. |
| Hall et al 47 | Australia | Co‐produced, non‐controlled, mixed methods evaluation of a recovery college | Recovery college students, staff, other key stakeholders | 41 | 85 | Experiences of the recovery college | College facilitated learning and growth; was inspiring, encouraging and compassionate; a “stepping‐stone” to mainstream education. |
| Sommer et al 48 | Australia | Non‐controlled pre‐post evaluation of a recovery college | Recovery college students | 91 | Primary outcome: achievement of goals identified in initial learning plan. | 70% of goals achieved at least partially. Most common goals related to education, physical health, social and personal relationships, mental health, and employment. | |
| Sutton et al 49 | UK | Non‐controlled pre‐post evaluation of a recovery college | Recovery college students | 86 | Primary outcome: economic benefits of attending the recovery college. | Attendance associated with higher chance of subsequent employment and increase in personal income. | |
| Wilson et al 50 | UK |
Non‐controlled, mixed methods, pre‐post evaluation of a recovery college |
Recovery college students | 77 | 80 | Primary outcomes at 6 months: well‐being, social inclusion. | Improvement in students’ well‐being and social inclusion, supported by qualitative findings. |
RCT – randomized controlled trial, HF – Housing First, ACT – assertive community treatment, TAU – treatment‐as‐usual, SMI – severe mental illness, quant. – quantitative, qual. – qualitative
Table 2.
Characteristics of included supported employment studies
| Country | Study design | Study population | Kmet score/100 (quant.) | Kmet score/100 (qual.) | Social outcomes investigated | Key findings | |
|---|---|---|---|---|---|---|---|
|
Christensen et al 51 |
Denmark |
Assessor‐blinded RCT comparing IPS with enhanced IPS (E‐IPS) or TAU |
Adults with SMI seeking employment or education |
100 |
Outcomes at 18 months. Primary outcome: competitive employment or education. |
More of those receiving IPS (59.1%) or E‐IPS (59.9%) achieved competitive employment or education than TAU group (46.5%), but advantage for E‐IPS over IPS. |
|
| Cook et al 52 | US | Multisite controlled trial comparing SE with TAU | Adults with SMI from four US regions | 85 | Social security data on employment over 13 years. | 32.9% of participants were employed at some point. This was almost three times more likely for SE recipients. | |
| De Winter et al 53 | The Netherlands | Non‐controlled longitudinal study of IPS | Clients of 27 IPS programs (23 targeted adults with SMI) | 77 | IPS fidelity and employment assessed quarterly over five years. | Greatest improvement in employment outcomes seen after 18 months of IPS. Positive association between IPS fidelity and employment. | |
| Glynn et al 54 | US | Non‐blinded RCT comparing IPS with IPS + work skills training | Adults with SMI | 100 | Primary outcomes at 2 years: employment and job tenure. | 63% of all participants gained employment. No differences between groups. | |
| Kern et al 55 | US | Pooled results from two RCTs comparing IPS with IPS + errorless learning |
Adults with SMI |
77 | Primary outcomes at 12 months: achievement of employment and job tenure. | 32% of all participants obtained jobs (mostly minimum wage and part‐time). The IPS + errorless learning group had greater job tenure. | |
| Lystad et al 56 | Norway | Multi‐site non‐blinded RCT comparing VR+CR with VR+CBT |
Adults with SMI |
62 | Primary outcome at 2 years: employment, hours worked. |
Employment and hours worked increased in both groups. No difference between groups in outcomes. |
|
| McGurk et al 57 | US | Non‐blinded RCT comparing enhanced VR (E‐VR) with E‐VR+CR | Adults with SMI for whom previous VR was ineffective | 85 | Outcomes at 3 years. Primary: employment rate. Secondary: engagement in work related activity. | No differences in employment rate between groups, but E‐VR+CR group more likely to engage in work‐related activity. | |
| McGurk et al 58 | US | Pre‐post feasibility study of VR+CR |
Adults with SMI |
64 | Feasibility (uptake and completion). | Intervention feasible (79% of participants completed at least 6/24 sessions). | |
| Puig et al 59 | US | Sub‐analysis of one arm of RCT comparing IPS with and without cognitive training | Adults with SMI receiving the cognitive training intervention | 82 | Outcomes at 2 years: cognitive skills and competitive employment. | Improved attention and age (younger and older participants) were associated with achieving competitive employment. | |
| Reme et al 60 | Norway | Multicentre non‐blinded RCT comparing IPS with TAU | Adults with severe and moderate mental illness | 85 | Outcomes at 12 and 18 months. Primary: competitive employment. | IPS group more likely to be in competitive employment. Similar employment rates for people with severe and moderate mental illness. | |
| Rodriguez Pulido et al 61 | Spain | Non‐blinded RCT comparing IPS with IPS+CR | Adults with SMI | 100 | Outcomes at 2 years. Primary: employment and hours worked/week. |
IPS +CR group more likely to gain employment and worked more hours. |
|
| Scanlan et al 62 | Australia | Non‐controlled prospective study of recovery‐based IPS service | Adults with SMI | 83 | Outcomes at 2 years: competitive or voluntary employment, job tenure, education engagement. | 49.5% gained competitive employment, mean duration 151 days. 63.9% gained employment or engaged in education or voluntary work. | |
| Schneider et al 63 | UK | Feasibility RCT comparing IPS + work‐focused CBT with IPS alone |
Adults with SMI |
81 | Outcomes at 6 months. Primary: hours in competitive employment. Secondary: participation in education, training or volunteering. | 34% participants gained employment. No differences between groups in outcomes. | |
| Twamley et al 64 | US | Non‐blinded RCT comparing IPS + cognitive training with E‐IPS |
Adults with SMI |
96 | Outcomes at 2 years. Primary: number of weeks worked. Secondary: job attainment, hours worked, wages earned. | No difference between groups in outcomes. | |
| Zhang et al 65 | China | Non‐blinded RCT comparing IPS with VR or IPS + work‐related social skills training (E‐IPS) |
Adults with SMI |
88 |
Outcomes at 2 years. Primary: job attainment Secondary: job tenure, hours per week worked. |
Higher job attainment and longer job tenure in the E‐IPS group than IPS alone. IPS and E‐IPS both had better employment outcomes than VR. | |
| Hutchinson et al 66 | UK |
Mixed methods evaluation of IPS implementation in six regions |
Community mental health services for adults with SMI | 50 | 35 |
Outcomes at 18 months. Primary: competitive employment. Qualitative: factors influencing implementation. |
5 of the 6 sites achieved target of supporting 60 clients into competitive employment. Service resource pressures, stakeholder support and achievement of targets influenced programme sustainability. |
| Gammelgaard et al 67 | Denmark | Phenomenological study of IPS | Adults with SMI participating in RCT evaluating IPS | 80 | How IPS and employment might influence recovery, through a “reflective lifeworld approach”. | Employment specialists adopted recovery‐based practice. Employment boosted self‐esteem, skills, routines and financial security. | |
| Perrez‐Corrales et al 68 | Spain | Phenomenological study of volunteering programs | Adults with SMI working in volunteer roles | 100 | Experiences of volunteering and its impact on the recovery process. | Volunteering enabled people to build a valued identity; having responsibility through volunteering helped people feel they had a “normal” life. | |
| Talbot et al 69 | UK | Descriptive qualitative study of IPS in forensic mental health setting | Adults with SMI under community forensic services | 60 | Implementation of IPS in community forensic mental health service. | Implementation required robust collaboration with internal and external agencies. Barriers: negative staff attitudes and difficulty engaging employers. Facilitators: support of service managers and outside groups. | |
| Yu et al 70 | China | Qualitative process evaluation of E‐IPS recipients in RCT reported above 65 | Adults with SMI who received E‐IPS and gained employment plus their family members | 55 | Participant and family views of the E‐IPS intervention. | Participants reported benefits from work‐related social skills training and valued social connections made at work. Participants valued having choice about jobs whereas carers valued financial benefits more than job fit. |
RCT – randomized controlled trial, IPS – Individual Placement and Support, SE – supported employment, CBT – cognitive behavioral therapy, TAU – treatment‐as‐usual, SMI – severe mental illness, VR – vocational rehabilitation, CR – cognitive remediation, quant. – quantitative, qual. – qualitative
Table 3.
Characteristics of included studies on social interventions delivered at the group or individual client level
| Country | Study design | Study population | Kmet score/100 (quant.) | Kmet score/100 (qual.) | Social outcomes investigated | Key findings | |
|---|---|---|---|---|---|---|---|
|
Community participation studies | |||||||
|
Chen et al 75 |
China | Non‐blinded RCT comparing Clubhouse model with standard care | Adults with SMI | 75 |
Outcomes at 6 months. Primary: social functioning and self‐determination. |
Clubhouse group had greater improvement in social functioning and self‐determination. | |
| Heatherington et al 76 | US | Non‐controlled pre‐post study evaluating a residential farm program | Adults with SMI | 86 | Outcomes at 6 and 36 months: clinical and personal recovery; community participation. | Improved community participation at 36 months. | |
| Varga et al 77 | Hungary | Non‐blinded RCT comparing community social club with case management or TAU | Adults with SMI | 92 | Outcomes at 6 months: social functioning and social cognition. |
Community social club and case management groups had better social function than TAU. Community social club group also had better social cognition. |
|
| Moxham et al 78 | Australia | Qualitative evaluation of Recovery Camp | Adults with SMI | 85 | Participants’ personal goals and whether met during the camp. | Goals: connectedness; developing healthy habits; challenging myself; personal recovery. Most goals reported as met. | |
| Prince et al 79 | US | Qualitative exploration of Clubhouse model | Clubhouse members (adults with SMI) | 85 | Exploration of benefits of Clubhouse membership and most helpful features. |
Benefits: improved social skills, gaining confidence, social connection. Features: flexible, non‐judgmental culture; equality of members and staff; evening and weekend activities; skills acquisition; sharing experiences; outreach support. |
|
|
Rouse et al 80 |
Canada | Participatory qualitative evaluation of Clubhouse model | Clubhouse members (adults with SMI) and staff | 95 | Explored how Clubhouse structures and ethos facilitated members’ recovery. | Structures/ethos: mutual respect, promoting self‐efficacy and autonomy, opportunities for social connection, providing purpose. Recovery: building identity and self‐respect, acquiring skills, being part of an empowered community. | |
| Saavedra et al 81 | UK | Qualitative evaluation of creative workshops in local art gallery | Adults with SMI, mental health staff, and workshop facilitator | 95 | Exploration of impact of workshop participation. | Main benefits: learning about artistic process; social connection; greater psychological well‐being; challenging institutional attitudes; breaking down barriers between service users and staff. | |
| Whitley et al 82 | Canada | Qualitative evaluation of a participatory video project | Adults with SMI | 80 | Exploration of participants’ experiences of the project. | Project well received. Main benefits: skill acquisition; connectedness; meaningful focus; empowerment; personal growth. | |
| Smidl et al 83 | US | Non‐controlled, mixed methods pre‐post evaluation of a therapeutic gardening project |
Adults with SMI and staff |
45 | 60 |
Outcomes at 3 months: motivation, social skills. Qualitative data from participants’ journals. |
Motivation ratings improved. Most participants and staff felt the project helped with social connection and skills. Qualitative: the project gave people a sense of purpose and pride. |
|
Family intervention studies | |||||||
| Kumar et al 84 | India | Assessor‐blinded RCT comparing a brief psychoeducation programme with nonspecific control intervention | Key relatives of adults with SMI | 69 | Outcomes at completion of sessions. Primary: carer burden. | Intervention group experienced greater reduction in carer burden. | |
| Martin‐Carrasco et al 85 | Spain and Portugal | Multicentre, assessor‐blinded RCT comparing psychoeducation intervention programme with TAU |
Primary family caregivers of adults with SMI |
96 | Outcomes at end of intervention (4 months) and 4 months later. Primary: subjective and objective carer burden. | Intervention group experienced reduced subjective carer burden at both follow‐ups. No difference between groups in objective carer burden. | |
| Mirsepassi et al 86 | Iran | Implementation study of a psychoeducation service | Adults with SMI and their family members | 60 | Programme development, implementation and sustainability. | Implementation affected by: low referral rate; limited resources; poor literacy; excessive distance to travel to access service. | |
| Perlick et al 87 | US | Assessor‐blinded RCT comparing carer‐only adaptation of family focused therapy with standard health education | Relatives of adults with SMI | 88 | Outcomes at end of intervention and 6 months later. Primary: carer burden. | Intervention group experienced greater improvement in carer burden at both follow‐ups. | |
| Al‐HadiHasan et al 88 | Jordan | Qualitative process evaluation, nested within an RCT | Adults with SMI and their primary caregivers who received the family intervention | 85 | Impact of family psychoeducation intervention on recipients. | Carers reported improved health, well‐being and coping. Service users reported better motivation. Both groups experienced improved self‐confidence and social interaction. | |
| Edge et al 89 | UK | Mixed methods, feasibility cohort study | African‐Caribbean adults with SMI, their relatives or “proxy” family | 65 | 65 | Feasibility of delivering a culturally appropriate family intervention to “proxy families” (peer supporters or volunteers if no family). |
Intervention highly acceptable. Most service users reported improved family relationships. Relatives’ communication with service users and health professionals improved. |
| Higgins et al 90 | Ireland | Sequential mixed methods, single group, pre‐post pilot evaluation of EOLAS programmes |
Adults with SMI and their family members |
45 | 55 | All outcomes at programme completion. Service users and families: hope for the future and self‐advocacy. Family members: perceptions of available social support. | No significant changes in quantitative outcomes. Qualitative: most participants found hearing other members’ stories was helpful. Co‐facilitation by peer support workers viewed positively, but some clinician facilitators appeared to lack skills to enable peer support worker co‐facilitators to participate equally. |
| Higgins et al 91 | Ireland | Sequential mixed methods, single group, pre‐post evaluation of EOLAS programmes |
Relatives of adults with SMI |
59 | 50 | All outcomes at programme completion: confidence in ability to cope and to access help for relative; self‐advocacy; hope for the future. | Participants experienced increased confidence and hope and were satisfied/very satisfied with the program. Qualitative: increased awareness of communication within the family; value of peer support. |
| Lobban et al 92 and Lobban et al 93 | UK | Assessor‐blinded RCT comparing online psychoeducation + resource directory (RD) with RD alone; mixed methods evaluation and economic analysis |
Relatives and close friends of adults with SMI. Qualitative sample: intervention group only |
100 100 |
65 50 |
Outcomes at 12 and 24 weeks. Primary: carer well‐being and experience of support. Secondary: costs of intervention and health and social care; experiences of the intervention. | No differences between groups in carer well‐being and support. Intervention cost more than RD alone and delivered no better health outcomes. Qualitative: intervention positively received. Proactive support from the peer supporters particularly appreciated. |
| Nguyen et al 94 | Vietnam | Non‐controlled, mixed methods, pre‐post evaluation of family intervention and cost analysis | Adults with SMI and their caregivers | 68 | 45 |
Outcomes at 1 year. Quantitative: service user functioning. Qualitative: intervention acceptability and feasibility. Cost analysis: service user and family income. |
High participation (98%) and acceptability. Service user functioning improved, and one quarter secured a paid job. Financial burden on family decreased. |
|
Peer‐led/supported intervention studies | |||||||
| Agrest et al 95 | Chile | Qualitative evaluation of peer supported intervention promoting recovery | Adults with SMI | 80 | Feasibility and acceptability of the intervention. | Peer support workers well received and helped engagement with community resources. | |
| Beavan et al 96 | Australia | Self‐report survey of Hearing Voices Network |
Adults with SMI who attended network meetings |
85 | 75 |
Cross‐sectional data only. Descriptive and free‐text responses. |
Positive benefits included reduced isolation, gaining social skills and improved self‐esteem. |
|
Easter et al 97 |
US | Non‐blinded RCT comparing facilitation of advance directive by a peer‐support worker or a clinician | Adults with SMI under the care of an ACT team | 69 |
Outcomes at 6 weeks. Primary: empowerment. Secondary: self‐esteem. |
Modest advantage of using peer support workers in terms of empowerment and attitudes toward treatment. | |
| Mahlke et al 98 | Germany | Assessor‐blinded RCT comparing peer support + TAU with TAU alone |
Adults with SMI |
96 |
Outcomes at 6 months. Primary: self‐efficacy. |
Self‐efficacy greater for intervention group. | |
| O'Connell et al 99 | US | Assessor‐blinded RCT comparing peer mentor + TAU with TAU alone | Adult inpatients with SMI, substance misuse and recurrent admissions | 85 |
Outcomes at 9 months. Secondary: social function and sense of community. |
Greater improvement in social function for intervention group. | |
|
Salzer et al 100 |
US | Non‐blinded RCT and qualitative evaluation of addition of peer support workers to community mental health services |
Adults with SMI |
69 | 60 |
Outcomes at 12 months: community participation, empowerment, therapeutic alliance. Qualitative: content of peer support. |
Peer support group had greater community participation days. |
| Thomas et al 101 | US |
Sub‐analysis of intervention arm of RCT comparing peer support with TAU |
Adults with SMI receiving the peer support intervention | 89 | Outcomes at 6 and 12 months: therapeutic alliance, empowerment and satisfaction. | Therapeutic alliance between participants and peer workers was high and positively associated with empowerment and satisfaction. | |
|
Social skills intervention studies | |||||||
| Favrod et al 102 | France | Non‐controlled pre‐post evaluation of Positive Emotions Program for Schizophrenia | Adults with schizophrenia and severe negative symptoms | 86 | Follow‐up assessment point not specified. Primary: social function. |
Social function improved. |
|
| Hasson‐Ohayon et al 103 | Israel | Non‐blinded RCT comparing social cognition and interaction training (SCIT) vs. therapeutic alliance focused therapy (TAFT) vs. TAU | Adults with SMI under a psychiatric rehabilitation service | 75 | Outcomes at end of 6 month intervention and 3 months later. Primary: social function. | No difference between groups in social functioning. | |
| Horan et al 104 | US |
Non‐blinded RCT comparing social cognitive skills training (SCST) delivered in vivo with SCST delivered in clinic or active control intervention |
Adults with SMI | 93 | Outcomes at 3 months. Primary: social cognition. Secondary: social functioning. |
SSCT groups both improved in social cognition. No between‐group differences in social functioning. |
|
| Kayo et al 105 | Brazil | Assessor‐blinded RCT comparing social skills training with an active control intervention | Adults with treatment resistant schizophrenia receiving clozapine | 93 | Outcomes at 20 weeks and 6 months. Primary: negative symptoms. Secondary: social skills. | No between‐group differences in social skills or negative symptoms. | |
RCT – randomized controlled trial, TAU – treatment‐as‐usual, SMI – severe mental illness, quant. – quantitative, qual. – qualitative
Social interventions delivered at the service level
Supported accommodation (see Table 1)
There were 16 eligible studies in this domain, nine of which were quantitative28, 29, 30, 31, 32, 33, 34, 35, 36 and seven qualitative37, 38, 39, 40, 41, 42, 43. The studies were conducted in eight different countries: six in Canada28, 35, 36, 37, 42, 43, three in the UK31, 33, 34, two in the US30, 41, and one each in Australia 32 , France 39 , India 38 , the Netherlands 29 and Norway 40 .
The quantitative studies comprised four randomized controlled trials (RCTs)28, 29, 35, 36, two case‐control studies30, 31, one pre‐post uncontrolled study 32 , one national survey 33 , and one national naturalistic prospective cohort study 34 .
The mean Kmet quality assessment score for quantitative papers was 83 (out of 100) and ranged from 10033,34 to 4531, 32. The mean quality assessment score for the qualitative papers was 85 and ranged from 10039 to 40 38 .
Housing First
Five of the quantitative studies and four of the qualitative studies (53% of all the supported accommodation studies) evaluated the Housing First (HF) model. This approach evolved in the US and Canada to address the high rate of homelessness amongst people with SMI, many of whom also have comorbid substance misuse problems. It involves the provision of rent supplements and support from a clinical team assisting persons to find, move into and sustain a tenancy, and helping them address their mental health issues using a recovery‐oriented framework 44 .
A robust, five centre RCT in Canada (“Chez Soi”) found HF to be associated with greater housing stability compared with treatment‐as‐usual (TAU) at 2‐year follow‐up (74% of HF clients were in stable housing compared to only 41% of those receiving standard care) 45 , but no differences were found between the groups in community functioning or secondary clinical and social outcomes. Our review included five high‐quality studies, two quantitative28, 36 and three qualitative37, 42, 43, associated with the Chez‐Soi trial.
A high‐quality (Kmet 91) case‐control study 30 in Seattle, US reported better housing outcomes for those receiving HF, with a lower percentage homeless and fewer days of homelessness at 12‐month follow‐up compared to standard care. A non‐blinded RCT versus TAU (Kmet 92) 28 reported findings from Moncton, Canada, where the clinical input to HF tenants was provided through assertive community treatment (ACT). Housing outcomes were better for HF recipients than those in the standard care group, with large effect sizes, but there was no difference between groups in community functioning or clinical outcomes.
A sub‐analysis of data from the Chez‐Soi trial's Toronto site 36 (Kmet 92), which provided HF plus intensive case management, adapted to the city's ethnically diverse population, reported that housing stability and community functioning were greater for those who received HF compared to controls. Similar positive results were obtained in a three‐arm RCT conducted in Vancouver 35 (Kmet 92) that compared HF provided to people with SMI (mainly psychosis and co‐occurring substance misuse problems) in scattered tenancies without on‐site staff, versus support provided in 24‐hour staffed congregate housing, and versus standard care. Both forms of supported accommodation (HF and on‐site staffing) were associated with greater housing stability than standard care, but clients in the congregate staffed housing rated their sense of community integration and personal recovery higher than the other two groups.
Using data from preparatory meetings, training events, supervision and focus groups with key stakeholders at HF implementation sites in the Chez‐Soi trial, two qualitative studies37, 43 (both with Kmet scores of 92) investigated the barriers and facilitators to successful implementation of the HF model.
Facilitators included: a) site readiness (i.e., ensuring that local stakeholder organizational policies were aligned to support implementation; that ring‐fenced and adequate resources were available; and that local champions were in place); b) organizing stakeholder sessions to frame the problem (homelessness) in a way that was congruent with different organizations’ values and allowed them to collaborate to address it; c) ensuring that all key players were included and engaged in the process; d) ensuring that housing providers and clinicians were trained and supervised to deliver the key elements of the HF model; e) identifying and addressing obstacles to local implementation (e.g., providing rent subsidies to use private tenancies to address shortages in housing supplies); f) providing forums for staff to share and solve implementation problems, build knowledge and avoid burnout; g) allowing flexibility in the model to fit with local context; h) using data to highlight successful outcomes and expand the programme.
Barriers to implementation included: a) lack of consensus about target client group; b) seeing homelessness as a housing problem rather than a wider health and societal problem; c) lack of consensus on how to organize the various structures of the HF approach; d) staff resistance to change and the (false) belief that they were already delivering HF; e) lack of existing structures to bring agencies together; f) financial disincentives (e.g., organizations competing for the same funds); g) housing stability being seen as an end in itself rather than a vehicle to support clients' ongoing recovery; h) lack of training and supervision to ensure that staff adopted a recovery‐oriented approach.
A qualitative evaluation of the implementation of HF at the Chez‐Soi Toronto site 42 was also conducted through interviews with HF senior managers, housing providers and case managers (Kmet 90). Model fidelity assessments were used to identify services with lower fidelity for further exploration of the barriers to implementation. Three main obstacles were identified: lack of housing availability; inadequate frequency of client contacts (the target was weekly contact, but this proved challenging due to staff time constraints and clients declining visits); and a lack of service user involvement in the HF programme. Facilitators to implementation included: a shared commitment to the HF philosophy across providers, senior managers and case managers; and using a shared team caseload approach to provide staff with peer support. The authors concluded that monitoring model fidelity was helpful to identify and then address implementation challenges.
A further robust (Kmet 100) qualitative study of clients of HF services conducted in France 39 reported benefits that went beyond the concrete outcome of housing stability reported in the quantitative studies. These included the deep sense of security that came from having a permanent home and how this provided a base to access adequate resources, build a routine, reclaim a previous identity or build a new one. However, the findings also highlighted the scale of the challenge for individuals in doing so. The authors noted that, whilst the effects of HF are considerable, they are often insufficient to break negative cycles and may only be able to “cushion” downward trajectories. They also observed that housing stability should not be considered a success in and of itself, but rather a basis for ongoing recovery.
Other models of supported accommodation
A national survey of mental health supported accommodation services in England 33 and a subsequent naturalistic cohort study 34 (both with a Kmet score of 100) identified three main types of service: a) residential care homes that provided congregate facilities, staffed 24 hours, where day‐to‐day needs were addressed (e.g. meals, supervision of medication and cleaning) and places were not time limited; b) supported housing that comprised shared or individual self‐contained, time‐limited tenancies with staff based on‐site up to 24 hours a day to assist individuals to gain skills to move on to less supported accommodation; and c) floating outreach services that provided visiting support for a few hours a week to people living in time‐unlimited, self‐contained, individual tenancies, with the aim of reducing support over time.
Quality of care was best in supported housing, and floating outreach was the cheapest of the three service types, but client characteristics differed significantly. Although two‐thirds of participants had some form of psychosis, those in residential care and supported housing had more severe mental health problems than those receiving floating outreach. However, across all services, 57% had a history of severe self‐neglect and 37% were considered vulnerable to exploitation.
After adjusting for differences in clinical characteristics, supported housing clients had greater autonomy than those of the other two service types. Clients of supported housing and floating outreach services were more socially included than those in residential care, but experienced more crime.
At 30‐month follow‐up, 41% of participants had successfully moved on to more independent accommodation (or, for those receiving floating outreach, were managing with fewer hours of support). After adjustment for clinical characteristics, this was most likely for floating outreach clients compared to clients of the other two service types, and more likely for those in supported housing than those in residential care.
Adjusted multilevel models revealed that clients who progressed to more independence had significantly lower community and inpatient mental health service costs than those who did not. Two aspects of service quality were associated with successful progression to more independence: promotion of human rights and recovery‐based practice. Those with more unmet needs, those with higher ratings of vulnerability to self‐neglect or exploitation, and those who had been living at the supported accommodation service longer were less likely to move on. The authors concluded that there were pros and cons of the various models and that different service types tailored to individual need were required, rather than investing only in the cheapest type (i.e., floating outreach).
Group and individual qualitative interviews were carried out with residents of a sheltered housing project in Trondheim, Norway 40 (Kmet 90), that provided self‐contained bedsits, with some communal areas for socializing, and staff on site 24 hours a day. Residents felt that this model provided them with a good balance of independence and support. They liked not having to share facilities with others, felt safe having staff on site, and reported being supported to gain confidence with daily living skills and social activities. The only drawback was the time‐limited nature of the project (residents were expected to move on after a few years).
A six‐week group programme comprising twice weekly sessions with an occupational therapist to prepare people to move to a floating outreach service was evaluated through a small (Kmet 45) case‐control study 31 . More of those who attended the group sustained their supported housing at six‐month follow‐up, suggesting that structured preparatory work for housing transition may be beneficial, but the methodological problems with this study limit the strength of its findings.
Whilst a number of studies identified the importance of supported accommodation services providing a recovery‐oriented approach34, 37, 43, this may prove difficult to implement. A cluster RCT 29 (Kmet 92) in the Netherlands evaluated a recovery‐based practice training intervention for staff of supported accommodation services. The intervention encompassed the use of a collaborative and strengths‐based approach to support service users to identify and work towards individualized goals, but no differences were found between intervention sites and standard services on the primary outcomes of personal recovery, quality of life or social functioning.
Nevertheless, a small qualitative study in Chennai, India 38 (Kmet 40), exploring the experiences of women who moved from a longer‐term mental health institution to a staffed group home, highlights the importance of supported accommodation to people's recovery. The move allowed the women to begin to develop an individual identity and to gain a sense of belonging in the local community for the first time.
Supported education (see Table 1)
Five papers evaluating supported education were identified46, 47, 48, 49, 50, all of which focused on recovery colleges: a recovery‐based mental health education program that uses peer learning advisors to facilitate individual student learning plans 48 and where students are people with lived experience of mental health problems. Two of the studies were quantitative48, 49 and three employed mixed methods46, 47, 50. Three were conducted in the UK46, 49, 50 and two in Australia47, 48.
Although a number of studies reported that attendance at a recovery college inspired students to consider looking for work, only one – a self‐report survey of a college in the UK49 (Kmet 86) – reported data to show a significant positive association between attendance and being in paid or self‐employment at nine‐month follow‐up.
A recovery college in Australia, where students were supported to develop learning plans and identify up to three specific goals, which were reviewed at least annually, was evaluated using routinely collected data on 64 students 48 (Kmet 91). The most commonly cited goals were education, physical health, social and personal relationships, mental health, and employment.
Student engagement in the college courses (including the number of courses enrolled in and the number of classes attended) was found to be associated with goal attainment, but active involvement in the college for over 685 days was negatively associated with goal attainment. The authors concluded that this could be due to a higher severity of mental health needs amongst longer‐term students and a possible need for additional support. The main factors that were reported to impede goal attainment included physical health problems, external stressors/life events, and dependency on others to access the college.
Simpler goals with a relatively short‐time frame appeared easier to achieve than more complex or longer‐term ones. Employment goals were less likely to be achieved than other types of goals, whereas education related goals were the most likely, followed by mental health, social, and physical health goals.
Mixed methods evaluations of recovery colleges of varying quality conducted in the UK46, 50 and Australia 47 have shown consistently positive findings in terms of student satisfaction, improvements in mental well‐being, confidence and reduced social isolation. Many students reported that they were planning to attend mainstream courses, volunteer or gain paid employment in the future46, 50, and some described the college as a “stepping‐stone” to mainstream education 47 . Some colleges provided employment opportunities themselves by involving students in the formulation and facilitation of courses on a paid or voluntary basis, and some signposted students to peer‐support positions elsewhere 47 .
Supported employment (see Table 2)
We identified 20 studies that addressed interventions targeting employment or voluntary work, of which 15 were quantitative51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, one used mixed methods 66 and four were qualitative67, 68, 69, 70.
The mean Kmet quality assessment score for quantitative papers was 82 and ranged from 10051,54,61 to 50 (quantitative component of a mixed methods study) 66 . The mean quality assessment score for the qualitative papers was 66 and ranged from 10068 to 3566 (qualitative component of a mixed methods study).
Seven studies were conducted in the US52, 54, 55, 57, 58, 59, 64, three in the UK63, 66, 69, two each in China65, 70, Denmark51, 67, Norway56, 60 and Spain61, 68, and one each in Australia 62 and the Netherlands 53 .
The interventions studied could be grouped into three main types: Individual Placement and Support (IPS), characterized by rapid individualized job searching for competitive employment, integrated with mental health support, welfare benefits counselling, and on‐the‐job support 71 ; other forms of competitive or sheltered employment with employment specialists providing on‐the‐job support; and vocational rehabilitation, that typically focused on pre‐vocational training, interview and preparation of a curriculum vitae.
Two high‐quality studies (Kmet 10051 and Kmet 85 60 ) compared IPS with usual care, both reporting more favourable employment outcomes achieved through IPS, supporting the international evidence that IPS delivers improved employment outcomes compared to traditional vocational rehabilitation 72 .
A further study 53 (Kmet 77) investigated the longitudinal association between IPS fidelity and employment outcomes among 27 IPS programmes that reported outcomes quarterly to a central registry in the Netherlands. A positive association was found between improvement in IPS fidelity and employment rates over time, with employment outcomes showing the greatest improvement after 18 months of implementation.
Based on emerging evidence that enhanced cognitive functioning could further improve the outcomes achieved from supported employment 73 , eight studies investigated the effectiveness of enhancements to supported employment interventions. Six of these supplemented IPS51, 54, 61, 63, 64, 65, and two supplemented another form of supported employment56, 57. Enhancements included: cognitive remediation computer‐assisted training via CogPack 61 ; manualized compensatory cognitive training 64 ; cognitive remediation (CIRCUITS computer software) in combination with social skills (Thinking Skills for Work) 51 ; computer‐assisted cognitive remediation (CogPack) plus Thinking Skills for Work56, 57, generic work skills training (Workplace Fundamentals) 54 ; work‐related social skills training (10 sessions of behavioral rehearsal plus in vivo problem solving) 65 ; and work‐focused cognitive behavioral therapy (3‐6 sessions matched to need) 63 .
The supplemental interventions were offered at varying levels of intensity, ranging from three to 30 sessions. However, not all studies described in detail the degree of participant engagement, and those which did suggest less than optimal engagement. Twamley et al 64 (Kmet 96) reported a mean of 8.23±4.88 weekly sessions of cognitive training attended in the first 12 weeks of IPS. Christensen et al 51 (Kmet 100) described the enhanced IPS intervention as comprising 30 sessions of cognitive remediation, but 24% of participants did not attend any sessions and the mean attendance was fewer than 10 sessions. In Glynn et al's RCT 54 (Kmet 100), comparing IPS versus IPS plus work skills training, 22% of participants attended none of the work skills classes (an “as‐treated” analysis that removed those participants did not reveal any additional benefits from the supplemental intervention).
While some neurocognitive improvement was described in most of the studies that augmented IPS with a cognitive intervention, only two61, 65 demonstrated significant between‐group findings on employment outcomes. In a Spanish study 61 (Kmet 100), participants in the IPS plus cognitive remediation group achieved significantly greater employment rates and hours worked than those receiving IPS alone. Although well conducted, this was quite a small study, and findings should be interpreted with some caution. In a study carried out in China, Zhang et al 65 (Kmet 88) found that the group receiving IPS plus work‐related social skills training had significantly higher employment rates (63%) than a standard IPS group (50%) and a vocational rehabilitation group who engaged in sheltered work (33%). They suggested that the success of the enhanced IPS intervention might be associated with cultural factors (such as the importance that Chinese employers place on social competence) and concluded that the augmented IPS intervention was a good cultural fit for the Chinese context.
Two studies supplemented supported employment (not IPS) with enhancements that included cognitive remediation56, 57. McGurk et al 57 (Kmet 85) focused their intervention on people who had not previously benefited from vocational services. They randomized participants to either enhanced vocational rehabilitation alone (where participants were supported to identify and address specific cognitive difficulties relevant to the workplace) or enhanced vocational rehabilitation plus computer‐based cognitive remediation (24 sessions) and work‐related coaching (Thinking Skills for Work). There were no between‐group differences on employment outcomes, although the authors noted between‐group differences in education levels at baseline that may have influenced the results.
In Norway, Lystad et al 56 (Kmet 62) investigated the JUMP vocational rehabilitation programme, where participants were offered 10 months of intensive vocational support in sheltered or competitive work environments in addition to either cognitive remediation (40 hours of computer‐based training and coaching, similar to the Thinking Skills for Work intervention), or 40 hours of work‐related cognitive behavioral therapy. Both groups improved in cognitive skills, but no between‐group differences were found in employment outcomes.
Kern et al 55 (Kmet 77) examined how job tenure and work behaviors were impacted by errorless learning (structured training where work behaviors that were causing challenges were broken into elements and addressed hierarchically using cues, prompts, modelling and self‐instruction until high levels of performance were achieved). Data from two studies were combined in the reported paper: a study of 74 veterans with schizophrenia or schizoaffective disorder and a study of 106 participants living in the community with a diagnosis of SMI and memory impairment. Participants all received IPS and were randomized at the point of obtaining a job to either continue IPS alone or to receive IPS plus errorless learning. In total, 58 (32%) participants obtained jobs that were mostly minimum wage and part‐time, and the errorless learning group had significantly better job tenure (41% were still working at the end of 12‐month follow‐up compared to 14% of the IPS alone group). There were no differences in hours worked or wages earned.
Overall, of the eight studies that evaluated supplementing IPS or another form of supported employment, only two found that the augmented approach improved employment outcomes61, 65, despite most of the interventions being associated with improved neurocognitive performance. In addition, Kern et al 55 ’s errorless learning enhancement, predominantly targeting social skills in the workplace, demonstrated enhanced job tenure. Furthermore, a subsequent analysis of participants in the trial conducted by Twamley et al 64 who received IPS and compensatory cognitive training, found that those who were younger or older benefited more in comparison with middle‐aged participants, and that improving attention significantly predicted work attainment 59 (Kmet 82).
Employment outcomes in the included studies were assessed over different periods, up to two years, with the most effective intervention reporting 63% employed and most studies reporting around 50%. These data demonstrate that targeted interventions can be effective in helping a large proportion of people with SMI achieve employment. However, the definition of employment varied and could involve as little as one hour per week in a low wage job over a short period of time.
One study took a longer view, using social security data to understand the impact of engagement in a supported employment programme in the US over many years 52 (Kmet 85). The supported employment programme was not IPS, but comprised employment specialists embedded within multidisciplinary teams coordinating clinical and employment supports and aiming to place people in competitive jobs matched to their preferences. Data on 449 individuals over 13 years showed that a third earned some income and 13% achieved economic self‐sufficiency at least some of the time. Compared to the control group receiving usual care, participants in this study were almost three times more likely to gain employment.
Several studies provided insights into implementation issues. The difficulties of addressing negative staff and employer attitudes, and ensuring that supplemental interventions are delivered by adequately skilled trainers, the contextual challenges of the local labour market and welfare systems, and organizational factors – including the separation of employment and mental health services – have been previously identified 72 and were again highlighted in the included studies.
A mixed methods study of a UK demonstration project to embed IPS into six health service sites 66 (quantitative Kmet 50, qualitative Kmet 35) used various strategies to address barriers to implementation (operational and strategic management, data monitoring, alignment of reporting, use of champions, and learning communities), and many participants gained employment. However, funding was not sustained at several sites, in the context of cost pressures in the health system, highlighting how external factors can undermine implementation efforts. A qualitative evaluation of the implementation of IPS in a forensic context (Kmet 60) 69 identified additional barriers for this client group, such as stigma and restrictions on employment relating to participants’ criminal history.
McGurk et al 58 demonstrated that it was feasible for front‐line staff to engage clients with more complex SMI in their Thinking Skills for Work intervention, prior to referring them to mainstream employment support (Kmet 64). The intervention was tailored to each site, with staff trained via two workshops focused on understanding the cognitive challenges of people with SMI and supporting clients to use a computerized cognitive training software programme. Sites with easier access to mainstream employment support had better employment outcomes, and the authors highlighted the relevance of local contextual factors to the successful implementation of supported employment interventions.
An Australian study 62 (Kmet 83) provided detail on how job coaches used the theory and practice guidance of the Collaborative Recovery Model 74 to underpin their implementation of IPS, including how they engaged with people, instilled hope and built on individuals’ strengths and values. The authors concluded that a recovery‐based approach appeared to enhance the structured activities of high‐fidelity IPS, but the findings warrant further investigation under controlled conditions.
Qualitative studies also provided additional insights into the need to consider cultural factors, personal experiences and family perspectives in implementation. A phenomenological investigation of 12 participants receiving IPS explored how the intervention influenced recovery for people with SMI 67 (Kmet 80). Some participants described the importance of the relationships that they established with employment specialists leading to increased self‐esteem and changes to life patterns, while others identified employment itself as most influential in their recovery. They highlighted how the individualized approach of IPS made them more hopeful about employment, especially in comparison with previous experiences with mainstream employment centres.
The experiences of 15 people with schizophrenia who received the IPS enhanced with social skills training intervention in the study conducted in China described earlier 65 were explored qualitatively 70 (Kmet 55). The findings highlighted the importance of sociocultural factors, such as the legal and moral responsibility of families in mainland China for caring for those with mental illness. The authors identified differences in perspectives between caregivers, who wanted their family member to attain the “best” job, and their relatives with schizophrenia, who wanted to find a job they liked. They concluded that, in collectivist cultures, provision of vocational interventions may benefit from taking a family‐oriented rather than individualistic approach.
Countering the focus on competitive employment as the only important outcome for people with SMI, a high‐quality Spanish study explored volunteering as a vocational intervention 68 (Kmet 100). People with SMI reported that volunteering provided them with a role and responsibilities and supported them in rebuilding a valued identity and sense of a “normal life”, affirming that vocational activities deliver benefits beyond earning an income.
Social interventions delivered at the group or individual client level (see Table 3)
Community participation
Nine studies evaluating interventions aimed to improve the community participation of people with SMI were identified, three of which were quantitative75, 76, 77, five qualitative78, 79, 80, 81, 82, and one employed mixed methods 83 . Three of the studies were conducted in the US76, 79, 83, two in Canada80, 82, and one each in Australia 78 , China 75 , Hungary 77 and the UK81.
A high‐quality RCT 77 (Kmet 92) conducted in Hungary investigated the impact of two types of community‐based psychosocial intervention (a community social club and case management) on social cognition and functional outcomes compared to a matched TAU control group. The authors reported a significant improvement in functional outcomes for participants in both intervention groups at six‐month follow‐up, with the most significant gains in social cognition found amongst those allocated to the community‐based club. They concluded that the club's “supportive social milieu” enabled consumers to engage in more social interactions and practice new social roles, which they posited would, in turn, enable greater societal engagement.
A well‐established, internationally recognized approach to bringing people with SMI together in a “supportive social milieu” to promote community participation is the Clubhouse. This has a strong peer‐led ethos, whereby members are responsible for the everyday running of the programme and mutually supported within the peer structure to achieve a wide range of psychosocial goals, including social and work‐based skills.
An RCT conducted in China 75 (Kmet 75) reported greater improvements in social functioning and self‐determination in participants randomly allocated to join a Clubhouse compared to a standard care control group at six‐month follow‐up.
The Clubhouse approach has also been evaluated through robust qualitative studies. Prince et al 79 (Kmet 85) first identified the key features of the approach through focus groups involving 20 Clubhouse members. These features were then assessed for importance through interviews with a further 150 members. Respondents particularly valued the flexibility of the Clubhouse structure, which they attributed to the lack of organizational hierarchy, the variety of activities provided to support the development of social skills, and the availability of activities outside, as well as within, office hours.
In addition, a large qualitative study of a Clubhouse in Canada80 (Kmet 95) found that the co‐leadership by peers and staff was fundamental to its culture. Other critical aspects included unconditional acceptance, promotion of self‐efficacy and mutual respect. Members reported that being part of the Clubhouse reduced social isolation and stigma and provided them with a sense of purpose, accomplishment and belonging.
A variety of other activity‐based group programmes aiming to improve people's confidence and community participation have also been studied. The Gould Farm programme, described as providing “recovery‐focused, milieu treatment on a 700‐acre working farm, that integrates counselling and medication with a work program providing opportunities for the development of daily living, social, and work skills as well as mental and physical health” was evaluated through an uncontrolled, pre‐post study 76 (Kmet 86). Participants showed improvements in psychosocial functioning of medium effect size, and maintenance of gains six months after finishing the programme. At 36‐month follow‐up, it was reported that participants had subsequently been able to gain work or volunteering positions, attend mainstream education, or participate in hobbies.
A five‐day “Recovery Camp” for people with SMI in Australia, staffed by mental health professionals, their students and a peer support worker, providing a range of recreational pursuits including physical, creative and relaxing activities, was evaluated qualitatively 78 (Kmet 85). Attendees identified specific goals at the start of the camp that the authors grouped into four main themes: feeling more connected, developing healthy habits, challenging oneself, and personal recovery. The findings suggested that the camp activities were particularly helpful in supporting individuals to make social connections and build on their existing strengths, resulting in them attaining many of the goals they had set.
A series of six‐week creative art workshops for people with SMI and mental health staff in the UK, hosted in a local art gallery, was evaluated through a robust qualitative study 81 (Kmet 95). The workshops included guided gallery exhibitions, group discussion and making art. Participants described very positive experiences of the workshops and reported that their social networks, communication skills and confidence improved as a result. There was also a positive change in how staff and clients viewed each other, with greater mutual respect.
In Canada, a two‐year group intervention for people with SMI provided training in video editing and production, and participants then worked in groups to make a film 82 . Across three cities, 23 participants produced 26 videos and 1,500 people viewed these at 49 community screenings. A qualitative evaluation at the end of the programme (Kmet 80) found that participants valued the opportunity to acquire new skills, and that the programme helped them feel more socially connected and enabled personal growth.
Similar benefits were reported from a therapeutic gardening project for people with SMI in the US83. The authors of this small, non‐controlled, mixed methods, pre‐post study used quantitative feedback (Kmet 45) and qualitative evaluation of participant journals (Kmet 60) to assess experiences of the project. At three‐month follow‐up, there was an improvement in participants’ motivation and social interactions, and many experienced positive gains in respect of personal responsibility and achievement.
Family interventions
In total, 11 papers assessing family interventions were identified, of which four reported on quantitative studies84, 85, 86, 87, three of which were RCTs84, 85, 87, and one described a programme development and implementation 86 . One study was qualitative in design 88 , and the remaining six employed mixed methods89, 90, 91, 92, 93, 94.
Of the mixed methods papers, two reported on the EOLAS (Eolas is the Irish word for knowledge) family information programme study90, 91, and two on the REACT (Relatives’ Education And Coping Toolkit) RCT92, 93. Two studies were conducted in the UK89, 92, 93, and one each in India 84 , Iran 86 , Ireland90, 91, Jordan 88 , Spain and Portugal 85 , the US87 and Vietnam 94 .
The mean Kmet score for quantitative papers was 75 and ranged from 10092,93 (one study) to 45 90 . The mean score for qualitative papers was 59 and ranged from 8588 to 45 94 .
The evaluated family interventions were varied, although all included psychoeducational elements. A number also included cognitive behavioral strategies85, 87, 89, 92, 93. The interventions were typically delivered in secondary or tertiary community care settings, mostly outpatient or community clinics84, 85, 86, 87, 89, 90, 91. One of the UK interventions was virtual92, 93; the Jordanian family intervention was carried out in the family home 88 ; and one paper described an intervention delivered at the local community level to residents of a rural commune in Vietnam 94 . Two studies evaluated family interventions that were co‐facilitated by peers alongside clinicians90, 91, 92, 93.
Carers receiving a family intervention showed significantly reduced caregiver burden compared with carers in the control group in three RCTs of high85, 87 to moderate 84 quality. The two high‐quality trials each evaluated psychoeducational programmes based on a cognitive‐behavioral approach. One of them (Kmet 96), conducted across 23 centres in Spain and Portugal, targeted families of people diagnosed with schizophrenia or schizoaffective disorder 85 . The other (Kmet 88) was carried out across three US centres and comprised a caregiver‐only adaptation of family focused therapy versus standard health education for relatives of people diagnosed with bipolar I or II disorder 87 . Both trials reported sustained decreases in carer burden at four and six months follow‐up respectively.
The third RCT (Kmet 69) evaluated a brief psychosocial family intervention in a LAMI setting (Northern India) 84 . This intervention consisted of two initial psychoeducation sessions for families of people with schizophrenia, followed by six multi‐family group sessions. The burden of care was significantly reduced at the completion of sessions. The authors postulated that the involvement of multiple families in the sessions, along with psychoeducation, might explain their positive outcomes compared with negative studies from elsewhere in India. Poor confidence in psychosocial treatments amongst the general public in the country was cited as a possible reason for the high rate of treatment dropout 84 .
Relatives or close friends of people with psychosis or bipolar disorder participated in a high‐quality (quantitative Kmet 100) mixed methods study, including an RCT, comparing an online family intervention (REACT plus access to a resource directory) with a control intervention comprising access to the resource directory only92, 93. The REACT intervention consisted of 12 online psychoeducation modules, alongside a group forum and a confidential direct messaging service, that were both moderated by REACT supporters (trained relatives with lived experience of supporting someone with SMI). There were no significant between‐group differences in social outcomes, and both groups showed improved well‐being and experience of support92, 93.
A pre‐post uncontrolled proof‐of‐concept mixed methods study of moderate quality 94 (quantitative Kmet 68) trialled a community‐based family intervention for Vietnamese people with SMI and their families. Staff from a local social organization, the Women's Union, facilitated psychoeducation group meetings over 12 months, alongside community awareness activities (e.g., talent shows and a summer programme for school students in the commune). The authors reported a significant positive impact on the personal functioning of service user participants, with approximately one quarter achieving a paid job 94 .
Several qualitative studies of varying quality reported that family interventions were associated with potential improvements in social inclusion for all participants, service users and family members alike88, 89, 91. An Irish study of an information programme for families of people with SMI 89 (qualitative Kmet 50) and a British study of a culturally‐adapted family intervention for African‐Caribbean people diagnosed with schizophrenia and their families 91 (qualitative Kmet 65) both reported that participants learnt more constructive ways of communicating with each other and experienced better family relationships. A high‐quality (Kmet 85) Jordanian study 88 reported that service user and family participants gained skills that made them feel more equipped to cope with daily life and/or caregiving and improved confidence and empowerment, leading to an enhanced social life.
Only two papers92, 94 reported on cost analyses. A health economic analysis found that the virtual family intervention delivered in the UK (REACT) incurred higher costs and resulted in no better health outcomes than the comparison, making it very unlikely that the intervention was cost‐effective at a standard willingness‐to‐pay threshold of £20,000 92 . In contrast, a health economic analysis based on pre‐post data reported in the Vietnamese study 94 showed a significant increase in the annual income of service user participants (from nearly US$80 to around US$120), with an associated reduction in the annual financial burden on the family (from around US$1500 to US$1100).
Two studies were specifically designed to explore the implementation of family interventions for people with SMI: the above‐mentioned Vietnamese study 94 (qualitative Kmet 45) and a study in Iran 86 (Kmet 60). Referral rates were low in the Iranian study of a psychoeducation service (comprising eight service user group sessions and six multiple family group sessions in parallel), despite the provision of information on the programme to hospital clinicians 86 . The authors concluded that poor awareness and negative attitudes towards psychosocial treatments amongst clinicians were major implementation barriers requiring cultural and organizational change. In addition, obstacles to families’ participation included the need to travel long distances to access the sessions, as well as poor literacy amongst a substantial minority 86 .
Several facilitators of implementation were reported in the Vietnamese study 94 , although it should be noted that this component of the study was of low quality. A good fit between the characteristics of the family intervention and the facilitators (Women's Union staff employed in a community‐based “task‐shifting” approach) was highlighted as especially suitable for resource‐constrained settings. The importance of providing facilitators with training and ongoing supervision, to ensure that they had adequate confidence and skills to provide the family intervention, was also emphasized 94 . Finally, the “whole community” nature of the intervention and the fact that meetings took place in participants' houses in each village at a time decided by participants was thought to facilitate the very high participation rate (98%).
Both UK studies provided useful insights into optimal delivery and implementation of family interventions89, 92, 93. In the above‐mentioned uncontrolled feasibility trial of a culturally adapted family intervention for African‐Caribbean people diagnosed with schizophrenia and their families 89 , the most frequently cited barriers to implementation were resource constraints and service pressures (demanding caseloads and the need to prioritize emergencies over routine care) that curtailed therapists’ capacity to deliver therapeutic interventions. Difficulties were also noted in recruiting suitably qualified and experienced therapists. Competing demands also hindered relatives' engagement in the REACT virtual family intervention 92 , and some reported difficulty processing the new information provided during the intervention due to feeling too stressed.
Peer‐led and peer‐supported interventions
Seven publications evaluating peer‐led or peer‐supported interventions that did not fit into any of the other six intervention categories were identified95, 96, 97, 98, 99, 100, 101. Five studies were quantitative97, 98, 99, 100, 101, four of which were randomized trials97, 98, 99, 100, one was qualitative 95 , and two used mixed methods96, 100. Four were conducted in the US97, 99, 100, 101, and one each in Australia 96 , Chile 95 and Germany 98 .
A robust RCT in Germany 98 (Kmet 96) found that one‐to‐one peer support provided over six months within a community mental health service was associated with greater self‐efficacy for participants who received the intervention compared to those who did not. The mean number of meetings between participants and peer support workers (12.2±9.6) and the high retention rate (75% versus 60% in the comparison group) also suggested that the intervention was highly acceptable.
In the US, a randomized trial 99 (Kmet 85), evaluating the addition of peer mentors to standard care for people with SMI who were high users of inpatient care, found that it led to greater improvement in social functioning (as well as reduction in symptoms, substance abuse and inpatient service use) compared to standard care at nine‐month follow‐up. However, one third of those assigned a peer mentor had no contact with him/her during the study period. Participants who engaged with their peer mentor differed from those who did not (they were more likely to be white, had completed more years of formal education, had fewer psychiatric symptoms and physical health problems, and used less alcohol), thus limiting the strength and generalizability of the findings.
A community‐based intervention delivered by peer workers and community mental health workers in Chile 95 (Kmet 80) aimed to promote recovery and community reintegration by strengthening the individual's engagement with community resources, family and friends. Qualitative evaluation showed that the intervention was feasible, but concerns were expressed about its time‐limited nature, and some participants were worried that their neighbours would know they were being treated for a mental illness when they saw staff visiting them at home. Nevertheless, most participants reported that they enjoyed meeting with the peer support worker. The intervention helped people gain a greater understanding of the importance of participating in community activities and reconnecting with their social supports. Peer workers were also reported to facilitate better relationships between clients and mental health staff.
The addition of certified peer specialists to community‐based mental health services was investigated in the US through a trial (Kmet 69) that included a qualitative component 100 (Kmet 60). Those who received the intervention did not differ from controls in their community participation or empowerment at six or 12‐month follow‐up. However, of the 50 participants allocated to receive the intervention, only 29 met with their peer worker more than once. In a post‐hoc analysis at 24‐months follow‐up, participants who did engage with their peer supporter spent more days participating in community activities compared to those who did not. The qualitative findings showed that the peer workers provided the expected support, including help with using public transport, addressing substance misuse issues, and accessing community activities. The authors suggested that the poor engagement with the intervention may have been due to participants finding it too intrusive or assertive, but they also commented that non‐engagement could represent positive self‐determination.
A related sub‐study 101 reported a strong positive association between the quality of the working alliance between the peer support worker and the participant (rather than the number of contacts made) and participants’ empowerment and satisfaction with the service.
A trial assessed the use of peer support workers to facilitate advance directives 97 (Kmet 69). Clients of an ACT team were randomly assigned to draw up an advance directive in collaboration with either a peer support worker or a mental health clinician. The advance directive aimed to prevent involuntary treatment during a future mental health crisis by clarifying preferences and plans prior to the crisis. The authors reported a modest advantage of using peer support workers in terms of ratings of service users' empowerment and attitudes towards treatment, but no differences between peer support or clinician facilitated directives in preventing involuntary admission.
Finally, a small mixed methods evaluation of peer‐led Hearing Voice Network groups in New South Wales, Australia 96 (quantitative Kmet 85, qualitative Kmet 75) found that the groups helped attendees feel less socially isolated and gain a better understanding of their voice‐hearing experiences.
Social skills interventions
Only four papers evaluating social skills training interventions for people with SMI that met our inclusion criteria were identified102, 103, 104, 105, all of which were quantitative. The studies were conducted in the US104, Brazil 105 , France 102 and Israel 103 .
Three of the papers reported on RCTs103, 104, 105, each investigating a different social skills training intervention. A three‐arm trial 104 (Kmet 93) investigated whether the inclusion of some in vivo community‐based sessions within a 24‐session social cognitive skills training programme enhanced the generalization of improvements in social cognition to “real world” social functioning. Although both forms of social skills training (clinic‐based or in vivo enhanced) were associated with greater improvements in emotional intelligence, facial emotional recognition and empathy than an active control intervention, there were no differences between the three trial arms in any measure of functioning. The authors suggested that their results could be due to the low sensitivity of their outcome tools.
However, similar findings were reported from an RCT 103 (Kmet 75) evaluating social cognition and interaction training, a manualized group‐based intervention, versus therapeutic alliance focused therapy or TAU delivered over six months to patients of psychiatric rehabilitation services. Unlike the previous trial, the primary outcome in this study was social functioning rather than social cognition. Although both intervention groups showed greater improvement in various aspects of social cognition compared to TAU controls, there was no difference between groups in social functioning at three‐month follow‐up. Of note, only around one third of participants completed all the intervention sessions.
A small but high‐quality (Kmet 93) trial 105 compared a 20‐week, group‐based social skills training programme, including role play and homework exercises, with an active control intervention for people with treatment‐resistant schizophrenia receiving clozapine therapy. The study was designed to assess improvement in negative symptoms, with social skills as a secondary outcome. No between‐group differences were found in social skills (or negative symptoms) at the end of the intervention or at six‐month follow‐up. The authors noted that their measure of social skills had not been formally standardized with people with SMI and thus potential benefits may have been missed.
In contrast to the findings of these three trials, significant improvements in negative symptoms and social functioning were reported in a small, pre‐post study 102 (Kmet 86) assessing the Positive Emotions Program for Schizophrenia. The intervention comprised eight weekly group sessions to address anhedonia and apathy amongst people with SMI through reinforcing positive emotions and developing positive thinking. Apart from the study design limitations, participants were relatively young compared to the other studies described in this section, which may partially account for the more positive findings.
NARRATIVE SYNTHESIS
Overall pattern of findings
We identified an encouraging level of recent research evaluating social interventions for people with SMI. We included interventions with a more established evidence base (supported accommodation, supported employment, and family interventions) as well as those at an earlier stage of development (supported education, peer led/supported interventions, and interventions aiming to improve social skills or community participation). Although we found higher numbers of studies evaluating supported accommodation and supported employment compared to the other interventions, most of which were of high quality, we also identified a growing evidence base for peer‐led/supported interventions. However, there was a paucity of recent studies assessing the cost‐effectiveness of the interventions.
Our results corroborate previous studies indicating the value of investing in the HF model of supported accommodation45, 106, the IPS model of supported employment 72 , and family psychoeducation interventions 107 , but we also identified research showing that a range of supported accommodation, supported employment and family interventions should be available, to allow tailoring to individuals’ needs and context rather than adopting a “one size fits all” approach108, 109, 110.
We also noted considerable research interest in augmentation strategies to enhance outcomes from social interventions, particularly supported employment and social skills training, where supplements to the standard interventions mainly focused on addressing the cognitive impairments associated with SMI. However, results are rather disappointing so far: despite their success in improving cognitive ability, most of these augmentation strategies do not seem to lead to transferable “real life” skills. Nevertheless, this is an ongoing area of research, and we identified two studies where augmentation of supported employment (training in social skills for the workplace, and a behavioral psychological approach, “errorless learning”)55, 65 appeared to be associated with better outcomes.
The majority of studies that investigated peer‐led/supported interventions reported positive findings, including four randomized trials97, 98, 99, 100. The addition of peer workers in the delivery of some of the other social interventions included in our review was also commonly noted, including as staff of recovery colleges46, 47, 48, 49, 50 and co‐facilitators of family interventions90, 91, 92, 93, providing knowledge and experience distinct from that of health professionals. Peer involvement was noted to be particularly helpful for people in building confidence and social connections47, 50, gaining a better understanding of their mental health issues 96 , and improving engagement with mental health services 95 .
Our review also identified a number of common facilitators of successful implementation of social interventions. These included ensuring that relevant stakeholders were authentically supportive of the plans, and that local policies and resources were in place to support the intervention; and providing training for those delivering the intervention, and ongoing supervision and discussion forums to support staff, share ideas and prevent mission drift. Monitoring fidelity and progress through the collection of routine metrics or outcome data was also considered helpful in sustaining the intervention, and the identification of local champions to keep everyone focused was commonly recommended37, 42, 43, 66.
Several barriers to implementation were also identified. For example, in supported accommodation studies, barriers included poor local housing availability, and stakeholder policies that did not align with the plans or obstructed implementation. In supported employment studies, barriers included high local unemployment rates, and welfare benefits systems that disincentivized or prevented people taking up part‐time paid employment. In studies of family interventions, obstacles included negative referrer attitudes and practical obstacles such as sessions being held too far from where people lived 86 .
Factors that influenced findings
Context
Many of the studies highlighted the importance of considering the influence on the results of the context in which the studies were conducted. This is particularly relevant to the supported accommodation literature, since housing policy varies from one setting to another (for example, in the supply of social housing and the rules pertaining to eligibility) and there are major international differences in the way in which mental health care has evolved in the post‐deinstitutionalization era.
Many of the supported accommodation studies we identified focused on HF, which has been shown to be effective in facilitating stable housing for homeless people with mental health problems, usually SMI, but whose impact on other outcomes is less clear45, 111. The HF model is popular in the US and Canada because of the high levels of homelessness amongst those with SMI, secondary to deficiencies in health, social care and welfare benefits coverage 112 , whereas other countries that have more universal access to these systems (such as the UK) have, historically, seen far lower levels of homelessness amongst people with SMI. The UK's approach has evolved over recent decades into providing a range of types of supported accommodation, organized into graduated pathways, with the expectation that people progress from higher to lower supported settings. This has the disadvantage that people have to make repeated moves as they progress in their recovery.
The impact of HF even varied from one Canadian city to another. Stergiopoulos et al 36 concluded from their trial in Vancouver that, for those with psychosis, HF should be combined with ACT to be effective, whereas Aubry et al 28 did not find this combination to be effective in improving community functioning in a smaller Canadian city.
The study of enhanced IPS conducted in China65, 70 noted that cultural factors specific to the local context influenced the success of the intervention. Likewise, cultural factors were found to be relevant in some of the family intervention studies we included, with both the community‐based intervention developed for the Vietnamese context 94 and the culturally‐adapted intervention for African‐Caribbean people in the UK89 showing promise. For the latter, it was concluded that the greatest adaptation should be in its “ethos of delivery”, and that this would rely on the family therapists’ cultural competency and skills. Similarly, the inclusion of group therapy sessions facilitated by a proactive moderator within a brief psychosocial family intervention in India was considered a useful cultural adaptation 84 .
In contrast, specific challenges may arise in certain contexts, such as those identified in relation to the implementation of a supported employment programme in a forensic setting 69 , including stigma and the difficulty of gaining employment when an individual has a criminal history.
Taken together and consistent with the implementation literature 113 , these findings highlight the need to consider all relevant contextual factors and make appropriate, specific adaptations when “importing” social interventions from other countries or settings.
Inconsistent terminology
Our interpretation of the evidence was challenged by the lack of a consistent terminology used to describe the interventions. This was particularly obvious in the supported accommodation studies. This issue has been previously acknowledged, and a common taxonomy has been proposed114, 115. However, our findings suggest that researchers are not yet following this suggestion.
Whilst the evidence for HF appears strong in regard to improving housing stability outcomes, a number of studies used this term to describe models of supported accommodation that did not appear to reflect the classic HF model, with staff on‐site rather than visiting32, 41, or with accommodation provided in congregate rather than self‐contained settings 35 . Of note, the high‐quality trial conducted by Somers et al 35 found no difference in housing outcomes for those who received the classic version of HF (visiting support) compared to those who had on‐site support. This suggests that further trials comparing different models are warranted, although the logistic difficulties of doing so have been highlighted recently 116 .
Heterogeneity of the target population
We attempted to minimize variation in the target population by selecting those studies where the majority of participants had SMI. However, this was not always clearly described, particularly in studies reporting on supported education and peer‐led/supported interventions, possibly due to ideological considerations about diagnostic “labels” and the methodological distinctions between quantitative and qualitative studies.
In addition, the difficulties in taxonomy mentioned above also extended sometimes to the target population for a specific intervention. For example, the HF model of supported accommodation is very similar to the UK's “floating outreach” services, but the latter tend to target people with less severe mental health problems 33 .
Content of interventions
In general, the studies described the specific intervention being evaluated relatively well. However, there was considerable heterogeneity in the range of interventions evaluated within each of our seven categories. Some were more established and well defined (e.g., HF, IPS, family psychoeducation), whereas others (most notably in the community participation and peer‐led/supported categories) were more varied and not at a stage of development where internationally accepted models or fidelity criteria exist (an exception being the Clubhouse). Nevertheless, most studies included a description of how staff were trained and supported to deliver the intervention and, where relevant, most included an assessment of fidelity.
There was, however, considerable variation in the length of the intervention phase in different studies evaluating the same intervention (or the same type of social intervention). This was particularly noted in the peer‐led/supported group of studies and raises questions about the optimum duration of interventions resulting in positive outcomes.
Strength of the evidence
The aggregation of findings of the studies we identified was confounded by some limitations, including the heterogeneity in what constituted a positive outcome, the range of measures and metrics used to assess similar outcomes, the use of bespoke tools that lacked psychometric testing, the use of varying follow‐up periods, and the variation in what constituted usual care in comparison groups. For example, amongst supported employment studies, success could refer to the achievement of competitive employment, sheltered employment or other vocational activity, and various outcome metrics were reported (employment rates, duration of employment, hours worked, and wages earned).
Bearing these limitations in mind, our findings provided good evidence that HF is effective at improving housing stability for homeless people with SMI; IPS is effective at improving employment outcomes; and family interventions facilitate better social connections and relationships, improved functioning and reduced carer burden. We also found consistent good evidence for peer‐led/supported interventions. We identified a number of well‐conducted trials evaluating cognitive interventions aimed to enhance people's social skills or outcomes from supported employment but, whilst these led to improvement on measures of cognition, they rarely translated to better social functioning.
Studies evaluating interventions to enable people's community participation were diverse in approach and of lower quality, but they reported similar benefits: improved social function, reduced social isolation and increased confidence and empowerment.
All the studies investigating supported education reported on evaluations of a single recovery college and had significant limitations, including small sample sizes, lack of control groups and sampling biases. Nevertheless, consistently positive findings are promising and suggest that these interventions can assist some people to achieve personal and educational goals.
Generalizability
Most of the studies we identified were conducted in high‐income countries, with only 11 (out of 72) coming from outside the US, Canada, Europe or Australia, limiting generalizability to other settings. The contextual considerations and variability in target populations detailed above also limit the generalizability of findings.
The majority of participants in the studies were male, and this may mean that findings are less relevant for women. In addition, when the interventions were delivered alongside existing mental health services, the latter were often not described at all. This applied particularly to peer involvement studies, limiting generalizability.
Further issues, common to all complex intervention research, include the fact that the implementation of many of the interventions we examined was driven by a local enthusiast and supported by the framework of a research study, and therefore wider implementation may be less successful.
DISCUSSION
Our review highlights the value of investment in supported accommodation, supported employment and family psychoeducation for people with SMI, in order to foster their social and economic participation, and provides evidence of positive outcomes associated with peer involvement in the development and delivery of social interventions. It also indicates that greater consistency in the parameters and methods of studies evaluating the same intervention (such as the core elements, the length of the intervention, the outcomes assessed, and the time frames over which data are collected) is required to improve the evidence base. The development of a shared language to describe participants with SMI will also be important in future research, given the reluctance to use clinical “diagnosis” in some of the papers we included.
Despite the various limitations of the studies we identified, there was considerable high‐quality evidence for several of the interventions examined. However, our findings particularly emphasize that social interventions, whether delivered at the service or individual level, need to be tailored to the person and context specific. This is unsurprising, since their aim is to influence positively the individual's social world. In other words, social interventions are, perhaps, the most complex of all mental health interventions.
Furthermore, although studies of the same or similar interventions may report similar “positive” findings, this may obscure a more nuanced interpretation. In regard to supported employment, there is increasing concern as to whether being employed for minimal hours in a low wage job is delivering the secondary gains and “material or ontological security” anticipated from competitive employment 117 . This highlights the need for a more critical review of what is considered a success in this field. In addition, despite the evidence supporting IPS, its success rate in facilitating competitive employment has not improved since 2011 118 .
Similarly, the supported accommodation literature is dominated by studies of HF. Yet, housing stability, the primary outcome used to assess its effectiveness, whilst clearly important, does not appear to provide the platform for consistent improvement in other social benefits. Studies of other forms of supported accommodation report on different important outcomes, such as successful progression to more independent settings, reflecting the different systems that operate in different countries, but the impact on social (and clinical) functioning has been less commonly studied.
Killaspy et al33, 34 concluded, from their national research programme into mental health supported accommodation in the UK, that a range of different types of accommodation should be provided to allow for tailoring of the most appropriate setting and support for people with different needs, rather than investing in only one model such as HF. They also highlighted the importance of considering the safety of individuals when making decisions about the most suitable type of accommodation, given the high prevalence of severe self‐neglect and vulnerability to exploitation amongst this group. In addition, a qualitative meta‐synthesis of the experiences of people living in mental health supported housing 119 highlighted that people supported through the HF approach had quite varied experiences of reconnecting within their community, with some reporting social exclusion.
The supported employment studies also highlighted an important element in terms of international adoption: collectivist versus individualistic cultural context. In particular, the study from China by Zhang et al 65 suggested that the intervention could (and should) not target the individual alone, but rather the whole family. This is also relevant in the supported accommodation field, where the vast majority of research has been conducted in Western settings with a culturally congruent goal of achieving independent living, while this may be far less important in countries or communities with stronger family‐based cultures.
The extent to which other social interventions should take cultural considerations into account remains relatively unexplored, but the potential relevance of cultural adaptations for the implementation of these interventions has been acknowledged 120 and, for people with SMI, it appears to have been considered most often in relation to family interventions 121 .
A number of studies highlighted the benefits of delivering social interventions within a recovery‐oriented framework45, 46, 47, 48, 49, 50, 62, 76, 78. In supported accommodation settings in the UK, recovery‐based practice has been shown to assist individuals to progress to more independent accommodation 34 . However, few staff training approaches have proved effective in improving recovery‐based practice29, 122, 123. As highlighted by Agrest et al 95 in their study from Chile, one element that may assist services with recovery orientation is the use of peer support workers. The first step is to allow adequate time and flexibility for a trusting, therapeutic alliance to be established between the peer worker and the service user 101 .
Our findings concerning the benefits of peer‐led/supported interventions in the delivery of mental health services synergize well with the results of a previous Cochrane review 124 . However, attrition was quite high in some of these studies, suggesting poor acceptability. Of course, poor engagement can be due to a range of personal or practical issues (such as illness severity or service accessibility). Nevertheless, positive “chemistry” in the relationship between peer support worker and client appears critical to successful implementation 101 . Perhaps more work is needed to develop processes for increasing compatibility and “matching” between the two parties to maximize uptake.
Despite their robust evidence base, the implementation of family interventions in mental health services continues to present a challenge, often secondary to resource constraints 89 . In LAMI countries, negative attitudes towards people with SMI and a lack of understanding of the potential benefits of psychosocial approaches may further hinder take‐up, alongside practical issues such as illiteracy and inaccessibility 86 . Our evidence suggested that family psychoeducation is gaining popularity, possibly due to it being perceived as more feasible to deliver. However, surprisingly, we identified only one study evaluating an online family psychoeducation package for people with SMI92, 93, a format which appears to be gaining traction for other groups such as children and adolescents 125 .
We found that interventions aiming to support the community participation of people with SMI demonstrated a high degree of innovation, with promising initial results. This is clearly an area of growing interest, although research into which types of interventions are most effective and how to address implementation challenges is at a fledgling stage of development 126 . However, one of the main strengths of these interventions is their diversity and creativity, so it may well be counterproductive to “over‐operationalize”. Nevertheless, further research can help to identify critical ingredients such as the structural and relational components that provide the opportunity for peer support, social connection and personal growth.
This might be assisted by learning from studies of the Clubhouse approach. We identified considerable benefits for this approach, in keeping with a recent review 127 which concluded that Clubhouse programmes are worthy of support as one component of a spectrum of rehabilitative services for people with SMI, providing a highly acceptable and useful vehicle for increasing social integration and social competence. The authors also noted that further trials are needed to compare the effectiveness of these programmes with IPS in terms of employment outcomes 127 .
We identified surprisingly few studies evaluating social skills training programmes that assessed social outcomes relevant to this review. Most evaluated cognitive interventions103, 104, 105 which were also assessed for their ability to enhance supported employment51, 54, 56, 57, 63, 64. The results were disappointing, with improvements in cognitive function rarely generalizing to social outcomes such as employment or social functioning. Whilst this may have been due to poor uptake51, 54, 103, a recent, robust trial of social cognition and interaction training for people with schizophrenia 128 reported no differences in social cognition or social functioning at three‐month follow‐up compared with an active control group. Sub‐analysis of those who attended at least half the planned sessions did not alter these negative findings.
Although we excluded studies that reported only on quality of life rather than any of our social outcomes of interest, we did not exclude health economic papers on this basis, since most use quality of life for the calculation of Quality Adjusted Life Years. Nevertheless, we identified very few health economic studies. The main exception was in research into family interventions92, 93. We also identified a study showing that, as people move from higher to lower supported accommodation, the total costs of care decrease 34 , presumably since the move signifies gains in the person's ability to manage in a more independent setting.
Our review was wide‐ranging in scope and included seven domains of social intervention that targeted people with SMI. A strength of our approach was the use of narrative synthesis to summarize a diverse range of quantitative, qualitative and mixed methods research reporting on both effectiveness and implementation of interventions. However, the difficulties in defining social interventions, as noted in our introduction, may have led to exclusion of relevant studies.
We restricted our search to studies that focused on people with SMI to ensure the relevance of our findings for this group. However, studies that targeted other diagnostic groups or that did not report the diagnoses of participants, and were thus excluded, may also have findings relevant to those with SMI. Similarly, studies that did not report on social outcomes within our scope were excluded and, again, may provide evidence relevant to people with SMI.
To address these issues, we employed an iterative approach to ensure consistency in the decision‐making process for study inclusion, with each paper considered by two assessors and a third assessor where agreement was not reached, alongside frequent meetings of the authorship group to discuss decisions. In addition, each paper was assessed for quality using a robust assessment tool which allowed us to emphasize findings with greater validity.
Finally, as we only included papers published in the English language, we may have excluded significant contributions produced in other languages, and studies from LAMI countries may have been under‐represented.
CONCLUSIONS
Our review identified an encouraging level of interest in research into social interventions for people with SMI. Of note, the service level interventions with the strongest evidence (supported accommodation and supported employment) have often been fostered by specific policy and government investment (e.g., HF in Canada and the US; IPS in the US, UK and Australia), which has facilitated their widespread adoption and ongoing research, whilst other effective interventions, such as family interventions, have struggled with implementation.
This may be due to policy‐makers being more receptive to the potential cost benefits of some interventions (for example, through reduced use of inpatient care and greater employment) than others. However, these kinds of “hard outcomes” do not always reflect the authentic success of an intervention. Many of the studies we included reported positive but “softer” outcomes, such as gaining confidence and building social connections. This invites the question as to whether such outcomes, whilst clearly valued by people with SMI, are valued enough by society to convince governments to invest in the relevant interventions.
In addition, we aimed to identify the social interventions that are most effective in increasing the social and economic participation of people with SMI, yet many of the studies reported on interventions that took place within settings where participants mixed mainly with other service users. Whether this represents social participation depends on the definition of the term. There is growing evidence to suggest that loneliness is a driver of poor health and social outcomes and therefore any opportunities to support social connection should be valued 129 .
The research we identified on supported education is also relevant here. All the studies we identified evaluated recovery colleges. Yet, only a few years ago, research in this field focused on interventions to support individuals in mainstream educational settings 130 . Perhaps this indicates a growing awareness that specialist mental health settings should be considered part of the “mainstream”, or certainly an important component of the whole system of services that facilitates “mainstream” participation.
A further tension in this field is the lack of priority given to the use of social interventions compared to pharmacological and, to some degree, psychological interventions. Whilst relatively small benefits from medication are often tolerated amongst those with longer‐term SMI, there appears to be a higher threshold for the expected effectiveness of social interventions. The low uptake of some of the interventions we identified was concerning, but no worse than other treatments that are widely considered essential aspects of multidisciplinary care. A recent systematic review 131 reported non‐adherence to psychotropic medication amongst people with SMI at 49% 131 , and uptake of psychological interventions amongst this group in the UK is under 20% 132 . Our findings suggest that greater consumer involvement during the development of interventions may assist acceptability and uptake.
Finally, our review identified a number of recommendations for future research in this field. First, a clear definition of what constitutes a social intervention is needed. Similarly, agreement on relevant, high‐level social outcomes to be reported in studies of different types of social intervention should be considered. A standard taxonomy should be adopted by journals publishing studies on specific models of care, such as supported accommodation and supported employment, to enable easier interpretation and comparison of results. Further discussion is also needed on how to address the lack of detailed description of participants’ diagnoses, particularly in the qualitative and peer support literature. Finally, given the limitations of the studies we identified and the influence of contextual issues, further multisite RCTs are needed, even for the interventions for which we found the strongest evidence.
ACKNOWLEDGEMENTS
The authors would like to thank C. Bressanutti (University of Melbourne) and A. Holman (Neami National, Australia) for their administrative assistance in the preparation of this paper. H. Killaspy and C. Harvey are joint first authors of the paper.
REFERENCES
- 1. Thornicroft G. European mental health policy: the key issue is social inclusion. Eur J Public Health 2011;21:548‐9. [DOI] [PubMed] [Google Scholar]
- 2. Knapp M, Wong D. Economics and mental health: the current scenario. World Psychiatry 2020;19:3‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bloom D, Cafiero E, Jané‐Llopis E et al. The global economic burden of non‐communicable diseases. Presented at the World Economic Forum, Geneva, January 2011. [Google Scholar]
- 4. World Health Organization . Comprehensive mental health action plan 2013‐2030. Geneva: World Health Organization, 2021. [Google Scholar]
- 5. Australian Government Productivity Commission . Mental health inquiry report. Canberra: Productivity Commission, 2020. [Google Scholar]
- 6. Boardman J, Currie A, Killaspy H et al. Social inclusion and mental health. London: RCPsych Publications, 2010. [Google Scholar]
- 7. Morgan V, Waterreus A, Carr V et al. Responding to challenges for people with psychotic illness: updated evidence from the Survey of High Impact Psychosis. Aust N Z J Psychiatry 2017;51:124‐40. [DOI] [PubMed] [Google Scholar]
- 8. World Health Organization Regional Office for Europe. Mental health, human rights and standards of care. Assessment of the quality of institutional care for adults with psychosocial and intellectual disabilities in the WHO European Region. Copenhagen: World Health Organization Regional Office for Europe, 2018. [Google Scholar]
- 9. Care Quality Commission . Mental health rehabilitation inpatient services; ward types, bed numbers and use by clinical commissioning groups and NHS trusts. London: Care Quality Commission, 2018. [Google Scholar]
- 10. Meltzer H. Treatment resistant schizophrenia: the role of clozapine. Curr Med Res Opin 1997;14:1‐20. [DOI] [PubMed] [Google Scholar]
- 11. Menezes M, Arenovich T, Zipursky R. A systematic review of longitudinal outcome studies of first‐episode psychosis. Psychol Med 2006;36:1349‐62. [DOI] [PubMed] [Google Scholar]
- 12. Green M. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996;153:321‐30. [DOI] [PubMed] [Google Scholar]
- 13. Allott K, Liu P, Proffitt T et al. Cognition at illness onset as a predictor of later functional outcome in early psychosis: systematic review and methodological critique. Schizophr Res 2011;125:221‐35. [DOI] [PubMed] [Google Scholar]
- 14. Fett A, Viechtbauer W, Dinubgyez M et al. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia. Neurosci Biobehav Rev 2011;35:573‐88. [DOI] [PubMed] [Google Scholar]
- 15. Deegan P. Recovery as a journey of the heart. Psychiatr Rehabil J 1996;19:91‐7. [Google Scholar]
- 16. Le Boutillier C, Leamy M, Bird V et al. What does recovery mean in practice? A qualitative analysis of international recovery‐oriented practice guidance. Psychiatr Serv 2011;62:1470‐6. [DOI] [PubMed] [Google Scholar]
- 17. Falkov A, Goodyear M, Hosman C et al. A systems approach to enhance global efforts to implement family‐focused mental health interventions. Child Youth Serv 2016;37:175‐93. [Google Scholar]
- 18. National Institute for Health and Care Excellence . Psychosis and schizophrenia in adults: prevention and management. London: National Institute for Health and Care Excellence, 2014. [PubMed] [Google Scholar]
- 19. Dieterich M, Irving C, Bergman H et al. Intensive case management for severe mental illness. Cochrane Database Syst Rev 2017;1:CD007906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Priebe S. Social outcomes in schizophrenia. Br J Psychiatry 2007;191:S15‐20. [DOI] [PubMed] [Google Scholar]
- 21. Cohen A, Glynn S, Murray‐Swank A et al. The family forum: directions for the implementation of family psychoeducation for severe mental illness. Psychiatr Serv 2008;59:40‐8. [DOI] [PubMed] [Google Scholar]
- 22. Hill H, Killaspy H, Ramachandran P et al. A structured review of psychiatric rehabilitation for individuals living with severe mental illness within three regions of the Asia‐Pacific: implications for practice and policy. Asia Pac Psychiatry 2019;11:e12349. [DOI] [PubMed] [Google Scholar]
- 23. Royal Commission into Victoria's Mental Health System . A new approach to mental health and wellbeing in Victoria. Melbourne: Royal Commission into Victoria's Mental Health System, 2021. [Google Scholar]
- 24. Price‐Robertson R, Obradovic A, Morgan B. Relational recovery: beyond individualism in the recovery approach. Adv Ment Health 2017;15:108‐20. [Google Scholar]
- 25. Kuipers E, Onwumere J, Bebbington P. Cognitive model of caregiving in psychosis. Br J Psychiatry 2010;196:259‐65. [DOI] [PubMed] [Google Scholar]
- 26. Kmet L, Lee R, Cook L. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta: National Institute for Health Research, 2004. [Google Scholar]
- 27. Popay J, Roberts H, Sowden A et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. Lancaster: Lancaster University, 2006. [Google Scholar]
- 28. Aubry T, Bourque J, Goering P et al. A randomised controlled trial of the effectiveness of Housing First in a small Canadian city. BMC Public Health 2019;19:1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bitter N, Roeg D, van Assen M et al. How effective is the comprehensive approach to rehabilitation (CARe) methodology? A cluster randomized controlled trial. BMC Psychiatry 2017;17:396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brown M, Jason L, Malone D et al. Housing first as an effective model for community stabilization among vulnerable individuals with chronic and nonchronic homelessness histories. J Community Psychol 2016;44:384‐90. [Google Scholar]
- 31. Gutman S, Raphael‐Greenfield E. Effectiveness of a supportive housing program for homeless adults with mental illness and substance use: a two‐group controlled trial. Br J Occup Ther 2017;80:286‐93. [Google Scholar]
- 32. Holmes A, Carlisle T, Vale Z et al. Housing First: permanent supported accommodation for people with psychosis who have experienced chronic homelessness. Australas Psychiatry 2017;25:56‐9. [DOI] [PubMed] [Google Scholar]
- 33. Killaspy H, Priebe S, Bremner S et al. Quality of life, autonomy, satisfaction, and costs associated with mental health supported accommodation services in England: a national survey. Lancet Psychiatry 2016;3:1129‐37. [DOI] [PubMed] [Google Scholar]
- 34. Killaspy H, Priebe S, McPherson P et al. Predictors of moving on from mental health supported accommodation in England: national cohort study. Br J Psychiatry 2020;216:331‐7. [DOI] [PubMed] [Google Scholar]
- 35. Somers J, Moniruzzaman A, Patterson M et al. A randomized trial examining Housing First in congregate and scattered site formats. PLoS One 2017;12:e0168745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stergiopoulos V, Gozdzik A, Misir V et al. The effectiveness of a Housing First adaptation for ethnic minority groups: findings of a pragmatic randomized controlled trial. BMC Public Health 2016;16:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Macnaughton E, Nelson G, Worton SK et al. Navigating complex implementation contexts: overcoming barriers and achieving outcomes in a national initiative to scale out Housing First in Canada. Am J Community Psychol 2018;62:135‐49. [DOI] [PubMed] [Google Scholar]
- 38. Padmakar A, de Wit E, Mary S et al. Supported Housing as a recovery option for long‐stay patients with severe mental illness in a psychiatric hospital in South India: learning from an innovative de‐hospitalization process. PLoS One 2020;15:e0230074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rhenter P, Moreau D, Laval C et al. Bread and shoulders: reversing the downward spiral, a qualitatitve analyses of the effects of a Housing First‐type program in France. Int J Env Res Pub Health 2018;15:520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Roos E, Bjerkeset O, Sondenaa E et al. A qualitative study of how people with severe mental illness experience living in sheltered housing with a private fully equipped apartment. BMC Psychiatry 2016;16:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Stanhope V, Choy‐Brown M, Tiderington E et al. Case manager perspectives on the role of treatment in supportive housing for people with severe mental illness. J Soc Soc Work Res 2016;7:507‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Stergiopoulos V, Zerger S, Jeyaratnam J et al. Dynamic sustainability: practitioners’ perspectives on Housing First implementation challenges and model fidelity over time. Res Soc Work Pract 2016;26:61‐8. [Google Scholar]
- 43. Worton S, Hasford J, Macnaughton E et al. Understanding systems change in early implementation of Housing First in Canadian communities: an examination of facilitators/barriers, training/technical assistance, and points of leverage. Am J Community Psychol 2018;61:118‐30. [DOI] [PubMed] [Google Scholar]
- 44. Nelson G, Goering P, Tsemberis S. Housing for people with lived experience of mental health issues: Housing First as a strategy to improve quality of life. In: Walker C, Johnson K, Cunningham L (eds). Community psychology and the socio‐economics of mental distress: international perspectives. Basingstoke: Palgrave MacMillan, 2012:191‐205. [Google Scholar]
- 45. Aubry T, Goering P, Veldhuizen S et al. A multiple‐city RCT of Housing First with assertive community treatment for homeless Canadians with serious mental illness. Psychiatr Serv 2016;67:275‐81. [DOI] [PubMed] [Google Scholar]
- 46. Ebrahim S, Glascott A, Mayer H et al. Recovery Colleges: how effective are they? J Ment Health Train Educ Pract 2018;13:209‐18. [Google Scholar]
- 47. Hall T, Jordan H, Reifels L et al. A process and intermediate outcomes evaluation of an Australian recovery college. J Rec Mental Health 2018;1:7‐20. [Google Scholar]
- 48. Sommer J, Gill K, Stein‐Parbury J et al. The role of recovery colleges in supporting personal goal achievement. Psychiatr Rehabil J 2019;42:394‐400. [DOI] [PubMed] [Google Scholar]
- 49. Sutton R, Lawrence K, Zabel E et al. Recovery college influences upon service users: a recovery academy exploration of employment and service use. J Mental Health Train Educ Pract 2019;14:141‐8. [Google Scholar]
- 50. Wilson C, King M, Russell J. A mixed‐methods evaluation of a recovery college in South East Essex for people with mental health difficulties. Health Soc Care Community 2019;27:1353‐62. [DOI] [PubMed] [Google Scholar]
- 51. Christensen T, Wallstrøm I, Stenager E et al. Effects of individual placement and support supplemented with cognitive remediation and work‐focused social skills training for people with severe mental illness: a randomized clinical trial. JAMA Psychiatry 2019;76:1232‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cook J, Burke‐Miller J, Roessel E. Long‐term effects of evidence‐based supported employment on earnings and on SSI and SSDI participation among individuals with psychiatric disabilities. Am J Psychiatry 2016;173:1007‐14. [DOI] [PubMed] [Google Scholar]
- 53. de Winter L, Couwenbergh C, van Weeghel J et al. Fidelity and IPS: does quality of implementation predict vocational outcomes over time for organizations treating persons with severe mental illness in the Netherlands? Soc Psychiatry Psychiatr Epidemiol 2020;55:1607‐17. [DOI] [PubMed] [Google Scholar]
- 54. Glynn S, Marder S, Noordsy D et al. An RCT evaluating the effects of skills training and medication type on work outcomes among patients with schizophrenia. Psychiatr Serv 2017;68:271‐7. [DOI] [PubMed] [Google Scholar]
- 55. Kern R, Zarate R, Glynn S et al. Improving work outcome in supported employment for serious mental illness: results from 2 independent studies of errorless learning. Schizophr Bull 2018;44:38‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lystad J, Falkum E, Haaland V et al. Cognitive remediation and occupational outcome in schizophrenia spectrum disorders: a 2 year follow‐up study. Schizophr Res 2017;185:122‐9. [DOI] [PubMed] [Google Scholar]
- 57. McGurk S, Mueser K, Xie H et al. Cognitive remediation for vocational rehabilitation nonresponders. Schizophr Res 2016;175:48‐56. [DOI] [PubMed] [Google Scholar]
- 58. McGurk S, Mueser K, Watkins M et al. The feasibility of implementing cognitive remediation for work in community based psychiatric rehabilitation programs. Psychiatr Rehabil J 2017;40:79. [DOI] [PubMed] [Google Scholar]
- 59. Puig O, Thomas K, Twamley E. Age and improved attention predict work attainment in combined compensatory cognitive training and supported employment for people with severe mental illness. J Nerv Ment Dis 2016;204:869‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Reme S, Monstad K, Fyhn T et al. A randomized controlled multicenter trial of individual placement and support for patients with moderate‐to‐severe mental illness. Scand J Work Environ Health 2019;45:33‐41. [DOI] [PubMed] [Google Scholar]
- 61. Rodríguez Pulido F, Caballero Estebaranz N, González Dávila E et al. Cognitive remediation to improve the vocational outcomes of people with severe mental illness. Neuropsychol Rehabil 2021;31:293‐315. [DOI] [PubMed] [Google Scholar]
- 62. Scanlan J, Feder K, Ennals P et al. Outcomes of an individual placement and support programme incorporating principles of the collaborative recovery model. Aust Occup Ther J 2019;66:519‐29. [DOI] [PubMed] [Google Scholar]
- 63. Schneider J, Akhtar A, Boycott N et al. Individual placement and support versus individual placement and support enhanced with work‐focused cognitive behaviour therapy: feasibility study for a randomised controlled trial. Br J Occup Ther 2016;79:257‐69. [Google Scholar]
- 64. Twamley E, Thomas K, Burton C et al. Compensatory cognitive training for people with severe mental illnesses in supported employment: a randomized controlled trial. Schizophr Res 2019;203:41‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zhang G, Tsui C, Lu A et al. Integrated supported employment for people with schizophrenia in mainland China: a randomized controlled trial. Am J Occup Ther 2017;71:7106165020p1‐8. [DOI] [PubMed] [Google Scholar]
- 66. Hutchinson J, Gilbert D, Papworth R et al. Implementing supported employment. Lessons from the making IPS Work Project. Int J Env Res Pub Health 2018;15:1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Gammelgaard I, Christensen T, Eplov L et al. “I have potential”: experiences of recovery in the individual placement and support intervention. Int J Soc Psychiatry 2017;63:400‐6. [DOI] [PubMed] [Google Scholar]
- 68. Pérez‐Corrales J, Pérez‐de‐Heredia‐Torres M, Martínez‐Piedrola R et al. ‘Being normal’ and self‐identity: the experience of volunteering in individuals with severe mental disorders – a qualitative study. BMJ Open 2019;9:e025363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Talbot E, Bird Y, Russell J et al. Implementation of individual placement and support (IPS) into community forensic mental health settings: lessons learned. Br J Occup Ther 2018;81:338‐47. [Google Scholar]
- 70. Yu L, Lu A, Tsui M et al. Impact of integrated supported employment program on people with schizophrenia: perspectives of participants and caregivers. J Rehabil 2016;82:11‐7. [Google Scholar]
- 71. Drake R, Bond G, Becker D. Individual placement and support: an evidence‐based approach to supported employment. London: Oxford University Press, 2012. [Google Scholar]
- 72. Modini M, Tan L, Brinchmann B et al. Supported employment for people with severe mental illness: systematic review and meta‐analysis of the international evidence. Br J Psychiatry 2016;209:14‐22. [DOI] [PubMed] [Google Scholar]
- 73. Wykes T, Huddy V, Cellard C et al. A meta‐analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry 2011;168:472‐85. [DOI] [PubMed] [Google Scholar]
- 74. Oades L, Deane F, Crowe T. Collaborative recovery model: from mental health recovery to wellbeing. In: Slade M, Oades L, Jarden A (eds). Wellbeing, recovery and mental health. London: Cambridge University Press, 2017:99‐110. [Google Scholar]
- 75. Chen Y, Yau E, Lam C et al. A 6‐month randomized controlled pilot study on the effects of the clubhouse model of psychosocial rehabilitation with Chinese individuals with schizophrenia. Adm Policy Ment Health 2020;47:107‐14. [DOI] [PubMed] [Google Scholar]
- 76. Heatherington L, Bonner B, Rosenberg D et al. Sustaining outcomes research in residential treatment: a 15‐year study of the Gould Farm program. Psychol Serv 2019;16:675‐86. [DOI] [PubMed] [Google Scholar]
- 77. Varga E, Endre S, Bugya T et al. Community‐based psychosocial treatment has an impact on social processing and functional outcome in schizophrenia. Front Psychiatry 2018;9:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Moxham L, Taylor E, Patterson C et al. Goal setting among people living with mental illness: a qualitative analysis of recovery camp. Issues Ment Health Nurs 2017;38:420‐4. [DOI] [PubMed] [Google Scholar]
- 79. Prince J, Mora O, Ansbrow J et al. Nine ways that clubhouses foster interpersonal connection for persons with severe mental illness: lessons for other types of programs. Soc Work Ment Health 2018;16:321‐36. [Google Scholar]
- 80. Rouse J, Mutschler C, McShane K et al. Qualitative participatory evaluation of a psychosocial rehabilitation program for individuals with severe mental illness. Int J Ment Health 2017;46:139‐56. [Google Scholar]
- 81. Saavedra J, Arias S, Crawford P et al. Impact of creative workshops for people with severe mental health problems: art as a means of recovery. Arts Health 2018;10:241‐56. [Google Scholar]
- 82. Whitley R, Sitter K, Adamson G et al. A meaningful focus: investigating the impact of involvement in a participatory video program on the recovery of participants with severe mental illness. Psychiatr Rehabil J 2021;44:63‐9. [DOI] [PubMed] [Google Scholar]
- 83. Smidl S, Mitchell D, Creighton C. Outcomes of a therapeutic gardening program in a mental health recovery center. Occup Ther Mental Health 2017;33:374‐85. [Google Scholar]
- 84. Kumar R, Nischal A, Dalal P et al. Impact of brief psychosocial intervention on key relatives of patients with schizophrenia: a randomized controlled trial. Indian J Psychiatry 2020;62:137‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Martin‐Carrasco M, Fernandez‐Catalina P, Dominguez‐Panchon A et al. A randomized trial to assess the efficacy of a psychoeducational intervention on caregiver burden in schizophrenia. Eur Psychiatry 2016;33:9‐17. [DOI] [PubMed] [Google Scholar]
- 86. Mirsepassi Z, Tabatabaee M, Sharifi V et al. Patient and family psychoeducation: service development and implementation in a center in Iran. Int J Soc Psychiatry 2018;64:73‐9. [DOI] [PubMed] [Google Scholar]
- 87. Perlick D, Jackson C, Grier S et al. Randomized trial comparing caregiver‐only family‐focused treatment to standard health education on the 6‐month outcome of bipolar disorder. Bipolar Disord 2018;20:622‐33. [DOI] [PubMed] [Google Scholar]
- 88. Al‐HadiHasan A, Callaghan P, Lymn JS. Qualitative process evaluation of a psycho‐educational intervention targeted at people diagnosed with schizophrenia and their primary caregivers in Jordan. BMC Psychiatry 2017;17:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Edge D, Degnan A, Cotterill S et al. Culturally‐adapted Family Intervention (CaFI) for African Caribbeans with schizophrenia and their families: a feasibility study of implementation and acceptability. Health Serv Deliv Res 2018;6(32). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Higgins A, Hevey D, Boyd F et al. Outcomes of a co‐facilitation skills training programme for mental health service users, family members, and clinicians: the EOLAS project. Int J Ment Health Nurs 2018;27:911‐21. [DOI] [PubMed] [Google Scholar]
- 91. Higgins A, Downes C, Monahan M et al. Family members’ perspectives on the acceptability and impact of a co‐facilitated information programme: the EOLAS mental health programme. Ir J Psychol Med 2019;10.1017. [DOI] [PubMed] [Google Scholar]
- 92. Lobban F, Akers N, Appelbe D et al. Clinical effectiveness of a web‐based peer‐supported self‐management intervention for relatives of people with psychosis or bipolar (REACT): online, observer‐blind, randomised controlled superiority trial. BMC Psychiatry 2020;20:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Lobban F, Akers N, Appelbe D et al. A web‐based, peer‐supported self‐management intervention to reduce distress in relatives of people with psychosis or bipolar disorder: the REACT RCT. Health Technol Assess 2020;24:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Nguyen T, Tran T, Green S et al. Proof of concept of participant informed, psycho‐educational, community‐based intervention for people with severe mental illness in rural Vietnam. Int J Soc Psychiatry 2020;66:232‐9. [DOI] [PubMed] [Google Scholar]
- 95. Agrest M, Le P, Yang LH et al. Implementing a community‐based task‐shifting psychosocial intervention for individuals with psychosis in Chile: perspectives from users. Int J Soc Psychiatry 2019;65:38‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Beavan V, de Jager A, dos Santos B. Do peer‐support groups for voice‐hearers work? A small scale study of Hearing Voices Network support groups in Australia. Psychosis 2017;9:57‐66. [Google Scholar]
- 97. Easter M, Swanson J, Robertson A et al. Impact of psychiatric advance directive facilitation on mental health consumers: empowerment, treatment attitudes and the role of peer support specialists. J Mental Health 2021;30:585‐93. [DOI] [PubMed] [Google Scholar]
- 98. Mahlke C, Priebe S, Heumann K et al. Effectiveness of one‐to‐one peer support for patients with severe mental illness – a randomised controlled trial. Eur Psychiatry 2017;42:103‐10. [DOI] [PubMed] [Google Scholar]
- 99. O'Connell M, Sledge W, Staeheli M et al. Outcomes of a peer mentor intervention for persons with recurrent psychiatric hospitalization. Psychiatr Serv 2018;69:760‐7. [DOI] [PubMed] [Google Scholar]
- 100. Salzer M, Rogers J, Salandra N et al. Effectiveness of peer‐delivered center for independent living supports for individuals with psychiatric disabilities: a randomized, controlled trial. Psychiatr Rehabil J 2016;39:239. [DOI] [PubMed] [Google Scholar]
- 101. Thomas E, Salzer M. Associations between the peer support relationship, service satisfaction and recovery‐oriented outcomes: a correlational study. J Mental Health 2018;27:352‐8. [DOI] [PubMed] [Google Scholar]
- 102. Favrod J, Nguyen A, Tronche A et al. Impact of positive emotion regulation training on negative symptoms and social functioning in schizophrenia: a field test. Front Psychiatry 2019;10:532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Hasson‐Ohayon I, Mashiach‐Eizenberg M, Lavi‐Rotenberg A et al. Randomized controlled trial of adjunctive social cognition and interaction training, adjunctive therapeutic alliance focused therapy, and treatment as usual among persons with serious mental illness. Front Psychiatry 2019;10:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Horan W, Dolinsky M, Lee J et al. Social cognitive skills training for psychosis with community‐based training exercises: a randomized controlled trial. Schizophr Bull 2018;44:1254‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Kayo M, Scemes S, Savoia M et al. A randomized controlled trial of social skills training for patients with treatment‐resistant schizophrenia with predominantly negative symptoms. Psychiatry Res 2020;287:112914. [DOI] [PubMed] [Google Scholar]
- 106. Rog D, Marshall T, Dougherty R et al. Permanent supportive housing: assessing the evidence. Psychiatr Serv 2014;65:287‐94. [DOI] [PubMed] [Google Scholar]
- 107. Harvey C. Family psychoeducation for people living with schizophrenia and their families. Br J Psych Advances 2018;24:9‐19. [Google Scholar]
- 108. Barbato A, D'Avanzo B, Harvey C et al. Editorial: From residential care to supported housing. Front Psychiatry 2020;11:560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Guhne U, Weinmann S, Riedel‐Heller S et al. Psychosocial therapies in severe mental illness: update on evidence and recommendations. Curr Opin Psychiatry 2020;33:414‐21. [DOI] [PubMed] [Google Scholar]
- 110. Harvey C, O'Hanlon B. Family psycho‐education for people with schizophrenia and other psychotic disorders and their families. Aust N Z J Psychiatry 2013:47:516‐20. [DOI] [PubMed] [Google Scholar]
- 111. McPherson P, Krotofil J, Killaspy H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry 2018;18:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Dalmia S. The ugly truth of Canada's welfare state. The Week, March 23, 2017. [Google Scholar]
- 113. Greenhalgh T, Robert G, Macfarlane F et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581‐629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. McPherson P, Krotofil J, Killaspy H. What works? Toward a new classification system for mental health supported accommodation services: the simple taxonomy for supported accommodation (STAX‐SA). Int J Env Res Public Health 2018;15:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Siskind D, Harris M, Pirkis J et al. A domains‐based taxonomy of supported accommodation for people with severe and persistent mental illness. Soc Psychiatry Psychiatr Epidemiol 2013;48:875‐94. [DOI] [PubMed] [Google Scholar]
- 116. Killaspy H, Priebe S. Research into mental health supported accommodation – desperately needed but challenging to deliver. Br J Psychiatry 2021;218:179‐81. [DOI] [PubMed] [Google Scholar]
- 117. Atterbury K. Rethinking why we do what we do: individual placement and support. Psychiatr Serv 2021;72:1088‐90. [DOI] [PubMed] [Google Scholar]
- 118. Becker D, Drake R, Bond G. Benchmark outcomes in supported employment. Am J Psychiatr Rehabil 2011;14:230‐6. [Google Scholar]
- 119. Watson J, Fossey E, Harvey C. A home but how to connect with others? A qualitative meta‐synthesis of experiences of people with mental illness living in supported housing. Health Soc Care Community 2019;27:546‐64. [DOI] [PubMed] [Google Scholar]
- 120. Fendt‐Newlin M, Jagannathan A, Webber M. Cultural adaptation framework of social interventions in mental health: evidence‐based case studies from low‐ and middle‐income countries. Int J Soc Psychiatry 2020;66:41‐8. [DOI] [PubMed] [Google Scholar]
- 121. Maura J, de Mamani A. Culturally adapted psychosocial interventions for schizophrenia: a review. Cogn Behav Pract 2017;24:445‐58. [Google Scholar]
- 122. McPherson P, Lloyd‐Evans B, Dalton‐Locke C et al. A systematic review of the characteristics and efficacy of recovery training for mental health staff: implications for supported accommodation services. Front Psychiatry 2021;12:631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Meadows G, Brophy L, Shawyer F et al. REFOCUS‐PULSAR recovery‐oriented practice training in specialist mental health care: a stepped‐wedge cluster randomised controlled trial. Lancet Psychiatry 2019;6:103‐14. [DOI] [PubMed] [Google Scholar]
- 124. Pitt V, Lowe D, Hill S et al. Consumer‐providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev 2013;3:CD004807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Wetterborg D, Enebrink P, Lönn Rhodin K et al. A pilot randomized controlled trial of Internet‐delivered parent training for parents of teenagers. J Fam Psychol 2019;33:764. [DOI] [PubMed] [Google Scholar]
- 126. Webber M, Ngamaba K, Moran N et al. The implementation of connecting people in community mental health teams in England: a quasi‐experimental study. Br J Soc Work 2021;51:1080‐100. [Google Scholar]
- 127. McKay C, Nugent K, Johnsen M et al. A systematic review of evidence for the clubhouse model of psychosocial rehabilitation. Admin Policy Ment Health 2018;45:28‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Dark F, Scott JG, Baker A et al. Randomized controlled trial of social cognition and interaction training compared to befriending group. Br J Clin Psychol 2020;59:384‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Wang J, Mann F, Lloyd‐Evans B et al. Association between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry 2018;18:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Ennals P, Fossey E, Howie L. Postsecondary study and mental ill‐health: a meta‐synthesis of qualitative research exploring students’ lived experiences. J Ment Health 2015;24:111‐9. [DOI] [PubMed] [Google Scholar]
- 131. Semahegn A, Torpey K, Manu A et al. Psychotropic medication non‐adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta‐analysis. Syst Rev 2020;9:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Royal College of Psychiatrists . Report of the Second Round of the National Audit of Schizophrenia. London: Healthcare Quality Improvement Partnership and Royal College of Psychiatrists, 2014. [Google Scholar]


