Abstract
Background
Pulmonary diseases have considerable prognostic relevance for all-cause mortality. Most patients with lung diseases such as chronic obstructive pulmonary disease are treated by general practitioners. Understanding the clinical consequences such as pulmonary hyperinflation or reduced diffusion capacity is important for the management and prognosis of patients with chronic respiratory disorders. Therefore, the interpretation of pulmonary function testing (PFT) results needs to see more emphasis in the medical education curriculum.
Objective
To develop PFT training for final-year medical students and to compare the efficacy of instructional training to self-reliant textbook study.
Methods
A two-armed randomized control trial compares learning outcomes in PFT interpretation. A total of 25 final-year medical students were selected at random into the 1) instructional training group or 2) self-reliant textbook study group on PFT interpretation. The learning time for both groups was 2 hours. The duration of the written pre- and post-training examinations was 60 minutes each. Both exams had a knowledge section (30 questions, maximum 120 points) and a skills section (11 case studies, maximum 75 points).
Results
The instructional training group acquired significantly more knowledge and, in particular, higher skill levels when compared with the self-reliant reading group. In the reading group, knowledge scores increased from 48 to 60% (12%) and skills scores increased from 14 to 22% (8%), whereas in the instructional group, knowledge increased from 47 to 71% (24%) and skills from 18 to 58% (40%). A multivariate analysis (Pillai’s Trace: 0.633; P < 0.001) as well as follow-up univariate analyses reveal that these differences are statistically significant (knowledge: F = 8.811, df = 1, P = 0.007; skills F = 33.965, df = 1, P < 0.001). Interestingly, there was no significant group effect in the pure knowledge gain about respiratory disorders per se.
Conclusion
The self-reliant study group was less able to translate their newly acquired knowledge into interpretation of comprehensive PFT reports. A mandatory 2-hour instructional training greatly enhances the students’ knowledge and skills about PFT interpretation. Obligatory PFT instructional training should therefore be included in the students’ curriculum.
Keywords: medical education, instructional training, pulmonary function testing, body plethysmography
Pulmonary function has relevance for well-being and longevity (1, 2), and, according to World Health Organization data, chronic obstructive pulmonary disease (COPD) was number three in the top 10 global causes of death in 2019 (3). To achieve the goal of early diagnosis and reliable management of obstructive and fibrotic pulmonary diseases, there needs to be an increased emphasis on pulmonary function testing (PFT) in the medical education system. Early diagnosis becomes all the more important with the availability of antifibrotic drugs for fibrotic pulmonary diseases. In a survey on COPD among Spanish final-year medical students, only 25% of students had an accurate clinical understanding of the disease (4). Despite this, up to 80% of patients with respiratory diseases such as asthma or COPD are managed by their general physicians (5, 6). Studies demonstrate a widespread underuse of spirometry by general practitioners to establish a diagnosis of COPD (7). Surprisingly, in a primary care quality study, more than three-quarters of PFTs were invalid, according to the quality criteria of the American Thoracic Society and European Respiratory Society (8). A better understanding of pulmonary function parameters in final-year medical students and future physicians presents an opportunity to expedite diagnosis of respiratory diseases and therefore improve patient outcomes (9).
Spirometry (10) is the most widespread used PFT and reports the forced expiratory volume in one second (FEV1), the vital capacity (VC), the ratio of these two volumes (FEV1/VC) and the expiratory flow over the middle 50% of the VC (25–75%). According to the aforementioned guidelines, a PFT is required to make a diagnosis of COPD considering the postbronchodilator flow–volume loop with FEV1/VC. But, neither the residual volume (RV) nor the diffusion capacity (DlCO) can be measured with spirometry. Evaluation of RV, functional residual capacity, and total lung capacity (TLC) requires special techniques. Body plethysmography uses Boyle’s Law to determine lung volumes, whereas inert gas dilution techniques (nitrogen, helium) use dilution properties of gases (11, 12). In our investigation, we focus on body plethysmography, as it is the most widespread clinical method for assessment of RV, functional residual capacity, and TLC in German-speaking countries. For a comprehensive study about PFT interpretation, pulmonary diffusion measurement (DlCO and transfer coefficient Krogh Index) and determination of the maximal inspiratory muscle strength (MIP) were also part of our educational investigation.
Knowledge about these more elaborate lung function parameters is essential for the correct clinical interpretation of respiratory disorders. Diagnosing a restrictive lung disorder requires the TLC and VC according to the American Thoracic Society and European Respiratory Society recommendations on interpretation of PFTs (13). MIP is a useful tool to decide whether a reduced TLC is caused by respiratory muscle weakness or by interstitial lung disease. In contrast, patients with COPD often develop emphysema with pulmonary hyperinflation and increased TLC and RV/TLC. Pulmonary hyperinflation is an independent predictor of all-cause mortality in patients with COPD (14). Knowledge about lung volume measurements is helpful to identify patients who may benefit from endobronchial lung volume reduction (15). Decreased DlCO is associated with increased morbidity in COPD (16) and in interstitial lung disease. Understanding the clinical consequences of pulmonary restriction, absolute and relative hyperinflation, reduced MIP, and reduced DlCO is important for the reliable management and the prognosis of the worldwide millions of patients with chronic respiratory disorders.
Although traditional teacher-centered learning focuses on content presented by the instructor and self-study focuses on information presented in the textbook, both instructional strategies strive to create learning experiences that result in applicable knowledge and skills.
An analysis of the learning targets, design of the learning materials, finding practical applications of what the students have learned, and an evaluation of the learning progress are integral components of the instructional training strategy. Enhancing the respiratory disease curriculum with an obligatory instructional training about spirometry, body plethysmography, DlCO/Krogh Index, and MIP may well benefit students’ learning progress about respiratory diseases and respiratory disorders (17).
Research Question
This study investigates the effects of two different learning strategies on knowledge and skill acquisition about respiratory disorders and PFT interpretation among final-year medical students. Acquired knowledge and skills are compared in two different learning scenarios: 1) self-reliant studying with medical textbooks and supplied texts about the interpretation of PFTs versus 2) attending an instructional training program about the interpretation of PFTs.
A portion of the work contained in this manuscript has been previously published in abstract form (18).
Study Design and Methods
This is an interventional, randomized, pseudonymized, two-armed, prospective, monocentric learning study. The investigation was conducted at the East-German Lung Center at the Department of Pulmonology at the University Hospital Carl Gustav Carus in Dresden, Germany.
Development of the Instructional Training
The design of the instructional training was inspired by the Four Component Instructional Design (4C/ID) approach (19). The 4C/ID approach aims to facilitate the acquisition of complex knowledge and skills in a coherent, integrated way. It includes the following core components: analysis of complex professional tasks and breakdown into part-tasks; rearrangement of the part-tasks from simple to complex, real-life professional tasks; analysis of the corresponding knowledge to accomplish the part-tasks; selection of instructional materials for teaching and practicing the part-tasks (information can be provided in form of a lecture, tutorial, and/or study materials); step‐by‐step and “just-in-time” procedural instructions and/or tutorial feedback to develop cognitive strategies to complete the part-tasks and, finally, the complex task; and part-task practice to train skills until they can be performed with ease and little cognitive load.
A pulmonologist and an instructional psychology expert collaborated closely to implement the 4C/ID principles (20) when designing the instructional training. To maximize the learning experience, the instructional design included an analysis of the needs, the design process, the development of educational materials, development of a pre- and postinterventional questionnaire, and an assessment of the effectiveness of the training.
The instructional training was designed as follows: 40 Powerpoint slides based on the official recommendations on spirometry and pulmonary function testing from the German Society for Pneumology and Respiratory Medicine and from the Deutsche Atemwgesliga (21–23), with a step-by-step-approach, including bronchodilation studies, metacholine provocation, DlCO, and Krogh Index as well as respiratory muscular strength; tutorial videos about spirometry (1 min, 26 s, slide 7) and body plethysmography (2 min, 38 s, slide 20) of the “Deutsche Atemwegsliga” embedded in the slides; supportive information, including 1) a handout with a written explanation for all abbreviations, 2) a handout with the typical respiratory graphs, and 3) a flow chart with a procedural algorithm; and three authentic training PFT cases (obstructive, restrictive, and bronchodilation testing).
Control Condition
The PFT lecture, demonstration of the body plethysmograph, and the participation in a hands-on training about the interpretation of PFT is voluntary at our medical school. Usually, only a small fraction of medical students take advantage of the opportunity to improve their PFT interpretation skills. Therefore, self-study by reading medical textbooks on the topic is the de facto learning method for our students. The students in the control group were given appropriate literature. A textbook chapter on respiratory disorders and PFT (23 pages, including body plethysmography, lung diffusion measurement, and measurement of MIP) (24) was given to the students of the control group. The textbook chapter provides a detailed explanation of lung function parameters and an extensive discussion and detailed illustrations of spirometry and pulmonary function testing. In addition, the students of the control group had free access to the German recommendations on spirometry and pulmonary function testing, and to a wide range of medical textbooks about pulmonary function testing in the hospital’s library, where they spend their learning time for the interventional study. In contrast to the instructional training group, there was no instructor/tutor for feedback or questions.
Participants, Randomization, and Intervention
The final-year medical education in Germany is split into internship rotations of 16 weeks each in internal medicine, surgery, and an elective subject. All final-year students complete a problem-based learning (PBL) course about heart, vascular, and lung diseases during the 7th semester.
In this PBL course, typical morning lectures for all students are supplemented with weekly alternating ward rounds and small-group discussions about selected topics. Auscultation, electrocardiogram, and PFT courses are offered on a voluntary basis in the afternoon. During the internal medicine rotation, the students at our university hospital have two lessons per week in the afternoons. We asked the final-year students to participate in the investigation in the context of such a lesson. Usually, we supervise about 30 final-year students per rotation in the medical department. The investigation was voluntary, as less motivated students may dilute the effect of the intervention. Twenty-five voluntary students gave their informed consent. Randomization was done by alternately counting the numbers one and two through the whole group. The students’ questionnaires were pseudonymized for the pre- and postinterventional examinations. Thirteen students were in the self-reliant study group (eight female) and 12 students (seven female) in the instructional training group. The duration of the study’s intervention was 2 hours. While the control group studied in the hospital’s medical library, the instructional training was performed in a classroom next door to the library. All participants were pseudonymized for the questionnaires, and the posttest was administered directly after the intervention phase to avoid dropouts.
Development of the Assessment Tool/Pre- and Postinterventional Questionnaires
The pulmonologist developed the pre- and postinterventional tests (questionnaires) on respiratory physiology respiratory disorders, PFT, PFT parameters, and clinical implications. The written pre- and postinterventional tests were similarly structured and divided into a knowledge section and a skills section. The test duration was 60 minutes each. We used anonymized PFTs and data from real patients from the Department of Pneumology in the skills section.
The knowledge section included 30 short-answer items (maximum 120 points); the skills section required students to work with 11 case reports (maximum 75 points). For each question/item in the skills section, the students had to 1) provide the pathophysiological findings, 2) provide the parameters on which findings are based, 3) provide clinical differential diagnoses, and 4) provide the diagnostic and/or therapeutic consequences of the findings. The questionnaires were structured to avoid random hits and to adapt the questions more closely to clinical practice. The preinterventional assessment was performed the week before the intervention.
Scoring
For the scoring, the pulmonologist created an evaluation template for each item in advance. The template contained synonyms as well as plausible alternative solutions for the test items. An impartial member of the Department of Psychology scored the pseudonymized test questionnaires using the prepared template. One point was awarded for every correct answer. There were a few queries, which were discussed with the pulmonologist.
Data Analysis
To make sure that the knowledge and skill items cover sufficiently the training and textbook content, the set of items for the knowledge test part was designed following the 4C/ID principles as well as Klauer’s approach of developing content-valid item sets for educational contexts (25). The test versions had a range of difficulties that are in accordance with the requirements of the study regulations of the local medical faculty. In the knowledge part of our investigation, three items were classified as easy, 15 items as medium, and 12 items as difficult; at least 70% of the students had to answer the question correctly for simple items, 30–69% of the students for medium items, and <29% of the students for difficult items.
To analyze the differences among the control and the instructional training groups, we calculated the differences among post- and pretest scores of the knowledge test and the skill test, which we consider to accurately reflect knowledge and skills gains. A multivariate analysis of variance (ANOVA) was conducted with two dependent variables: knowledge and skills gain and the between-factor intervention (instructional training vs. self-reliant textbook studying). Because this multivariate ANOVA revealed a significant multivariate main effect of the between factor (Pillai’s trace 0.633; P < 0.001), follow-up univariate ANOVAs were computed for the two dependent variables separately. An inferential statistical analysis of each single test item of the knowledge test and the ability test was not performed because an α error adjustment would have to be made. Given the large number of items, however, the test results could no longer be meaningfully interpreted. The Statistical Product and Service Solutions was used for statistical analysis.
Results
Table 1 presents the basic demographic data and the results of the preinterventional examination.
Table 1.
Comparison of demographic variables and the pretest variables for the instructional training versus the self-reliant textbook studying group
| Demographics | Instructional Training (n = 12) | Textbook Studying (n = 13) | T Value/P Value |
|---|---|---|---|
| Sex | 7 female, 5 male | 8 female, 5 male | |
| Age | Mean, 25.5 (SD, 1.2) | Mean, 26.9 (SD, 2.25) | 1.96/0.07 |
| Range, 24–27 | Range, 24–31 | ||
| Semester | Mean, 12.25 (SD, 1.2) | Mean, 11.7 (SD, 0.9) | −1.34/0.18 |
| Range, 11–14 | Range, 11–14 | ||
| Initial levels of knowledge and skills achieved in the pretest | |||
| Knowledge | Mean score, 57 (SD, 12) | Mean score, 58 (SD, 13) | 0.26/0.74 |
| Range, 40–78 | Range, 41–82 | ||
| Skills | Mean score, 14 (SD, 11) | Mean score, 10 (SD, 8.1) | −0.84/0.41 |
| Range, 0–39 | Range, 0–28 | ||
Definition of abbreviation: SD = standard deviation.
Group differences were tested with Student's t test for independent samples.
Table 2 provides an overview on the achieved scores of the two study groups in the preinterventional and postinterventional questionnaires. To facilitate the comparison among groups, the raw data of the pre- and posttests were transformed into percentage scores because the knowledge and skills test parts differed in their maximum achievable raw scores (120 vs. 75 points).
Table 2.
Pre- and posttest levels of knowledge and skills about respiratory disorders and interpretation of pulmonary function tests by experimental conditions (sixth-year medical students, n = 25)
| Experimental Conditions |
||
|---|---|---|
| Instructional Training [Mean (SD)] | Textbook Studying [Mean (SD)] | |
| Measures | ||
| Knowledge, pretest | ||
| Score achieved | 57 (12) | 58 (13) |
| Score achieved, % | 47 (9) | 48 (11) |
| Knowledge, posttest | ||
| Score achieved | 85 (13) | 72 (11) |
| Score achieved, % | 71 (11) | 60 (9) |
| Knowledge gain, % | 24 (10)* | 12 (9)* |
| Skills, pretest | ||
| Score achieved | 14 (11) | 10 (8) |
| Score achieved, % | 18 (14) | 14 (11) |
| Skills, posttest | ||
| Score achieved | 43 (13) | 17 (10) |
| Score achieved, % | 58 (10) | 22 (14) |
| Skills gain, % | 40 (15)† | 8 (12)† |
Definition of abbreviation: SD = standard deviation.
Difference in knowledge gain between the self-reliant textbook study and the instructional training group (F = 8.811, df = 1, P = 0.007)
Difference in skills gain between the self-reliant study and the training group (F = 33.965, df = 1, P < 0.001)
The self-reliant study group had, on average, a small knowledge gain of 12% and a skills gain of 8%, whereas the mean gains of the instructional training group were 24% for knowledge and 40% for skills. A multivariate ANOVA revealed a statistically significant effect of the experimental condition (Pillai’s trace: 0.633; P < 0.001). Univariate analyses of variance show that the differences are significant for both measures (knowledge: F = 8.811, df = 1, P = 0.007; skills: F = 33.965, df = 1, P < 0.001). Table 3 presents the group effects for the following item groups: pulmonary function parameters, respiratory disorders, procedure of body plethysmography, interpretation of body plethysmography graphs and data, differential diagnosis, and clinical consequences.
Table 3.
Analysis of variance of a group effect between self-reliant learning group and training group on the topic of respiratory disorders and interpretation of pulmonary function tests
| Dependent Variable | df | F | P | Partial Eta-Quadrat | Corrected R2 |
|---|---|---|---|---|---|
| Knowledge gain pulmonary function parameters | 1 | 4.963 | 0.036 | 0.177 | 0.142 |
| Knowledge gain pulmonary respiratory disorders | 1 | 1.773 | 0.196 | 0.072 | 0.031 |
| Knowledge gain procedure pulmonary function testing | 1 | 9.021 | 0.006 | 0.282 | 0.251 |
| Skills gain interpretation of pulmonary function testing | 1 | 38.378 | 0.000 | 0.625 | 0.609 |
| Skills gain differential diagnosis and clinical consequences | 1 | 11.689 | 0.002 | 0.337 | 0.308 |
The instructional training group showed a significantly higher gain in knowledge and skills about the diagnostic PFT procedures and interpretation of PFT parameters. Also, the ability for differential diagnosis and understanding of the clinical implications of the findings improved significantly more in the instructional training group. Interestingly there was no significant group effect regarding the knowledge gain about respiratory disorders per se. Figure 1 illustrates the results of the questionnaire scoring in percentage of correct answers for the different item subgroups.
Figure 1.
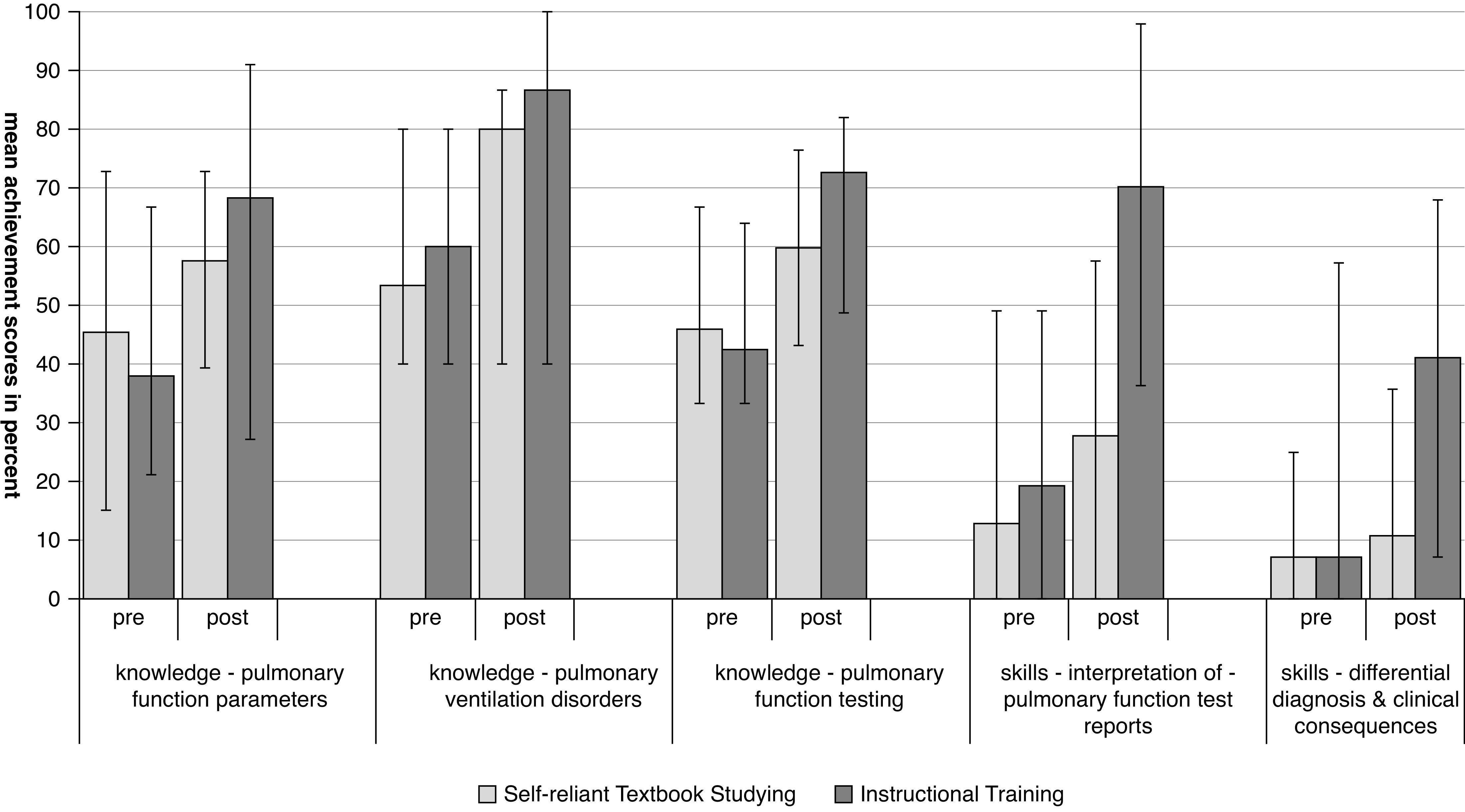
Mean pre- and posttest achievement scores (in percent) for the knowledge and skill test parts by experimental condition. Instructional training group n = 12 (7 female); self-reliant textbook study group n = 13 (8 female).
Discussion
The physician’s understanding of the basics of respiratory/ventilatory disorders is important for the management and outcomes of patients with chronic respiratory disorders. Dyspnea is one of the leading symptoms, causing about 4% of all consultations (26). Knowledge about PFT parameters is important for many disciplines, such as general practitioners, emergency physicians, anesthesiologists, pediatricians, thoracic surgeons, rheumatologists, cardiologists, and radiologists (27–34). Even in nonsmokers, spirometry parameters predict mortality more strongly than systolic blood pressure or body mass index (35), and for this reason, the education of medical students about the interpretation of pulmonary function parameters is mandatory. Although respiratory physiology/pathophysiology is a challenging subject for medical students (36, 37), PFT education in medical schools seems to be a missed opportunity (38). Although most curricular content incorporates lectures presenting normal and abnormal spirometry curves, there is not sufficient time to practice interpretation of PFT test results, and additional instruction tends to occur by chance during hospital-based rotations.
Beyond spirometry, we also recommend more comprehensive instructional training to include plethysmography, DlCO, and assessment of muscle strength. This recommendation is made because 1) most of the patients with respiratory diseases are managed by their general practitioner, 2) these parameters are helpful to improve the patient’s management, and 3) medical students have difficulty translating their knowledge of respiratory disorders into skills for interpretation of pulmonary function parameters.
The results from our preinterventional examination indicate a need to improve competency in the interpretation of PFTs. Although all final-year medical students attended the PBL courses about lung diseases during their medical education, their preinterventional knowledge and skills about PFT parameters were poor. In the preinterventional examination, only about 50% of the knowledge items and only about 20% of the skill items were answered correctly. These results fit with the results of the abovementioned studies about “COPD knowledge” in medical students (4) and fulfillment of quality criteria in primary care spirometry (8).
The lack of financial support for medical education and the strained financial situation of the healthcare system promotes the need for more efficient methods in medical education (39, 40). Advocates of instructional psychology propagate a teaching method with structured training units targeting everyday clinical situations to achieve reliable medical diagnoses and therapies (41). Practical application of learning targets and evaluation of the learning progress are core components of instructional trainings.
PFT is a complex diagnostic tool. Understanding PFT parameters requires basic knowledge about physics, physiology, and pathophysiology of respiratory and gas exchange, and it requires skills in graph pattern recognition and data interpretation. This is why we developed a 2-hour instructional training about respiratory disorders and PFT interpretation for final-year medical students. Because of the ongoing debate regarding the best way to educate medical students, we performed a randomized controlled trial to compare the learning effectiveness of the training with the effectiveness of self-reliant textbook studying. Both groups had the same learning time. Under the given conditions in the context of the weekly lessons, we decided to choose the self-reliant textbook studying format for the control group. The students of the control group were given a comprehensive medical textbook chapter about respiration and the interpretation of pulmonary function testing, and they had free access to the official German recommendations about spirometry and pulmonary function testing, as well as to a multitude of medical textbooks about pulmonary function testing and pulmonology.
The design of an instructional training requires more effort than PBL courses and much more effort when compared with self-reliant textbook studying. It took us about 1 month to develop the 40 Powerpoint slides, the supportive elements, the case-based exercise examples, the tutoring feedback strategies, and the pre- and posttest examination versions. The development of the instructional training was thus somewhat time consuming, but because of its electronic documentation, it is scalable and can also be reproduced in online sessions for many medical students. We used recommendations from modern theories like the 4C/ID approach about instructional and motivational design (19, 20, 42–49) for the development of the instructional training. Complex authentic tasks were included to avoid the fragmentation of knowledge and skills, and attention was given to graph interpretation (50). Tutoring feedback strategies were considered a core component of the instructional training (49, 51).
The results of our investigation show that it is well worth developing a PFT instructional training. The results reveal a moderate benefit of the instructional training regarding the knowledge acquisition but a great beneficial effect regarding the skills acquisition. Within the same learning time, the knowledge gain was twice as high and the skills gain 4.4 times higher in the instructional training group. Interestingly, there was no significant difference in the knowledge gain about respiratory disorders between the self-reliant study group and the instructional training group. Despite their gains in knowledge about respiratory disorders, the students of the self-reliant study group failed to transfer their knowledge into the practical skill for correct graph and data interpretation. The results of the present study indicate that the instructional training contributed substantially to overcome this lack of transfer performance. Understanding the implications of the changes in lung function parameters on patients’ daily life and prognosis seems to be very challenging if there is no expert instructor available.
Strengths and Limitations
To the best of our knowledge, this is the first RCT about medical education on PFT interpretation. On the Medical Education Research Quality Instrument (52) scale, the study achieves a score of 11.5 points. The students’ learning progress about PFT interpretation was focused and measured objectively. Our investigation is characterized by a complete follow up of 100%, objective outcome data, blinded scoring, and a sophisticated data analysis beyond descriptive statistics. The results of the investigation provide a sound basis for further studies in the field of medical education on PFT. The limitations of the investigation are the relatively small number of subjects in each investigational arm, the single-center design, and the lack of external validation of the evaluation questionnaire. Furthermore, the short time interval between intervention and postinterventional examination allows no statements about the long-term knowledge and skill effects, and like with most educational research studies, there is no patient-level outcome impact data. Self-reliant textbook study was used as a control condition because a more complex control condition was not possible.
Perspectives
A multicenter investigation with a consideration of larger cohorts, longer intervals between pre- and postinterventional examination, and a variety of control conditions is needed to validate the results of our investigation.
Conclusions
This investigation demonstrates that it is possible to effectively teach final-year medical students the interpretation of comprehensive PFT within 2 hours. The study discloses the difficulty of medical students to transform knowledge to skill in the field of interpretation of pulmonary function parameters. The investigation also demonstrates that this lack of transfer performance can be overcome with the help of a well-designed instructional training given by an expert in the subject. Because of the global burden of noncommunicable chronic respiratory diseases to human health, instructional PFT training must be integrated into the students’ curriculum. Further RCTs about medical education on the topic of PFT interpretation are needed.
Acknowledgments
Acknowledgments
The authors thank Annika Bochmann for the preparation and data collection as part of her master thesis in psychology and the final-year medical students who participated in the study.
Footnotes
Author Contributions: S.D.B., M.C., D.K., C.P., S.N., and H.K. had all full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis; S.D.B. and H.K. contributed substantially to the study design; S.D.B., C.P., H.K., and S.N. contributed substantially to the data analysis and interpretation; and S.D.B., M.C., D.K., H.K., and SN contributed substantially to the writing of the manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Schünemann HJ, Dorn J, Grant BJB, Winkelstein W, Trevisan M. Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. Chest . 2000;118:656–664. doi: 10.1378/chest.118.3.656. [DOI] [PubMed] [Google Scholar]
- 2. Neas LM, Schwartz J. Pulmonary function levels as predictors of mortality in a national sample of US adults. Am J Epidemiol . 1998;147:1011–1018. doi: 10.1093/oxfordjournals.aje.a009394. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- 4. Mohigefer J, Calero-Acuña C, Marquez-Martin E, Ortega-Ruiz F, Luis Lopez-Campos J. Understanding of COPD among final-year medical students. Int J Chron Obstruct Pulmon Dis . 2018;13:131–139. doi: 10.2147/COPD.S138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murphy KR, Meltzer EO, Blaiss MS, Nathan RA, Stoloff SWDD. Asthma management and control in the United States: results of the 2009 Asthma Insight and Management survey. Allergy Asthma Proc . 2012;33:54–64. doi: 10.2500/aap.2011.32.3518. [DOI] [PubMed] [Google Scholar]
- 6. Yawn B, Kim V. COPD in primary care: key considerations for optimized management. J Fam Pract . 2018;67:S28–S37. [PubMed] [Google Scholar]
- 7. Caramori G, Bettoncelli G, Tosatto R, Arpinelli F, Visona G, Invernizzi G, et al. Underuse of spirometry by general practitioners for the diagnosis of COPD in Italy. Monaldi Arch Chest Dis . 2005;63:6–12. doi: 10.4081/monaldi.2005.651. [DOI] [PubMed] [Google Scholar]
- 8. Gillette C, Loughlin CE, Sleath BL, Williams DM, Davis SD. Quality of pulmonary function testing in 3 large primary care pediatric clinics in rural North Carolina. N C Med J . 2011;72:105–110. [PubMed] [Google Scholar]
- 9. Brereton CJ, Wallis T, Casey M, Fox L, Pontopiddan K, Laws D, et al. Time taken from primary care referral to a specialist centre diagnosis of idiopathic pulmonary fibrosis: an opportunity to improve patient outcomes? ERJ Open Res . 2020;6:00120–2020. doi: 10.1183/23120541.00120-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update an official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med . 2019;200:E70–E88. doi: 10.1164/rccm.201908-1590ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Robinson PD, Latzin P, Verbanck S, Hall GL, Horsley A, Gappa M, et al. Consensus statement for inert gas washout measurement using multiple- and single-breath tests. Eur Respir J . 2013;41:507–522. doi: 10.1183/09031936.00069712. [DOI] [PubMed] [Google Scholar]
- 12. Flesch JD, Dine CJ. Lung volumes: measurement, clinical use, and coding. Chest . 2012;142:506–510. doi: 10.1378/chest.11-2964. [DOI] [PubMed] [Google Scholar]
- 13. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J . 2005;26:948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 14. Shin TR, Oh Y-M, Park JH, Lee KS, Oh S, Kang DR, et al. The prognostic value of residual volume/total lung capacity in patients with chronic obstructive pulmonary disease. J Korean Med Sci . 2015;30:1459–1465. doi: 10.3346/jkms.2015.30.10.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ramaswamy A, Puchalski J. Bronchoscopic lung volume reduction: recent updates. J Thorac Dis . 2018;10:2519–2527. doi: 10.21037/jtd.2018.02.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Balasubramanian A, Macintyre NR, Henderson RJ, Jensen RL, Kinney G, Stringer WW, et al. Diffusing capacity of carbon monoxide in assessment of COPD. Chest . 2019;156:1111–1119. doi: 10.1016/j.chest.2019.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bintley HL, Bell A, Ashworth R. Remember to breathe: teaching respiratory physiology in a clinical context using simulation. Adv Physiol Educ . 2019;43:76–81. doi: 10.1152/advan.00148.2018. [DOI] [PubMed] [Google Scholar]
- 18. Braun SD, Koschel D, Körndle H, Narciss S. Whole body plethysmography test interpretation: development and efficiency testing of a tailored skills training program for sixth-year medical students. Chest . 2020;157:A207. [Google Scholar]
- 19.van Merriënboer JJG, Kirschner PA. Ten steps to complex learning: a systematic approach to four-component instructional design. 2013. [Google Scholar]
- 20. Vandewaetere M, Manhaeve D, Aertgeerts B, Clarebout G, Van Merriënboer JJG, Roex A. 4C/ID in medical education: how to design an educational program based on whole-task learning: AMEE Guide No. 93. Med Teach . 2015;37:4–20. doi: 10.3109/0142159X.2014.928407. [DOI] [PubMed] [Google Scholar]
- 21. Criée C, Berdel D, Heise D, Kardos P, Köhler D, Leupold W, et al. Empfehlungen der Deutschen Atemwegsliga zur Spirometrie [in German] Pneumologie . 2006;60:576–584. doi: 10.1055/s-2006-944245. [DOI] [PubMed] [Google Scholar]
- 22.Criee C, Berdel D, Heise D, Jörres RA, Kardos P, Köhler D, et al. 2009. [Google Scholar]
- 23. Criée CP, Baur X, Berdel D, Bösch D, Gappa M, Haidl P, et al. Leitlinie zur Spirometrie: Leitlinie der Deutschen Atemwegsliga, der Deutschen Gesellschaft für Pneumologie und Beatmungsmedizin und der Deutschen Gesellschaft für Arbeitsmedizin und Umweltmedizin zur Spirometrie [in German] Pneumologie . 2015;69:147–164. doi: 10.1055/s-0034-1391345. [DOI] [PubMed] [Google Scholar]
- 24.Matthys H, Sorichter S. 2002. pp. 59–89. [Google Scholar]
- 25.Klauer KJ.Kontentvalidität [in German] Diagnostica 1984301–23.. [Google Scholar]
- 26. Frese T, Sobeck C, Herrmann K, Sandholzer H. Dyspnea as the reason for encounter in general practice. J Clin Med Res . 2011;3:239–246. doi: 10.4021/jocmr642w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Coates AL, Tamari IE, Graham BL. Role of spirometry in primary care. Can Fam Physician . 2014;60:1069–1070. [PMC free article] [PubMed] [Google Scholar]
- 28. Tseng TJ, Henry TS, Veeraraghavan S, Mittal PK, Little BP. Pulmonary function tests for the radiologist. Radiographics . 2017;37:1037–1058. doi: 10.1148/rg.2017160174. [DOI] [PubMed] [Google Scholar]
- 29. Klings ES, Wyszynski DF, Nolan VG, Steinberg MH. Abnormal pulmonary function in adults with sickle cell anemia. Am J Respir Crit Care Med . 2006;173:1264–1269. doi: 10.1164/rccm.200601-125OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoeper MM, Meyer K, Rademacher J, Fuge J, Welte T, Olsson KM. Diffusion capacity and mortality in patients with pulmonary hypertension due to heart failure with preserved ejection fraction. JACC Heart Fail . 2016;4:441–449. doi: 10.1016/j.jchf.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 31. Hyldgaard C, Ellingsen T, Hilberg O, Bendstrup E. Rheumatoid arthritis-associated interstitial lung disease: clinical characteristics and predictors of mortality. Respiration . 2019;98:455–460. doi: 10.1159/000502551. [DOI] [PubMed] [Google Scholar]
- 32. Gu Z, Wang H, Mao T, Ji C, Xiang Y, Zhu Y, et al. Pulmonary function changes after different extent of pulmonary resection under video-assisted thoracic surgery. J Thorac Dis . 2018;10:2331–2337. doi: 10.21037/jtd.2018.03.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Caron M, Hoa S, Hudson M, Schwartzman K, Steele R. Pulmonary function tests as outcomes for systemic sclerosis interstitial lung disease. Eur Respir Rev . 2018;27:170102. doi: 10.1183/16000617.0102-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bigatello L, Pesenti A. Respiratory physiology for the anesthesiologist. Anesthesiology . 2019;130:1064–1077. doi: 10.1097/ALN.0000000000002666. [DOI] [PubMed] [Google Scholar]
- 35. Gupta RP, Strachan DP. Ventilatory function as a predictor of mortality in lifelong non-smokers: evidence from large British cohort studies. BMJ Open . 2017;7:e015381. doi: 10.1136/bmjopen-2016-015381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Badenhorst E, Mamede S, Abrahams A, Bugarith K, Friedling J, Gunston G, et al. First-year medical students’ naïve beliefs about respiratory physiology. Adv Physiol Educ . 2016;40:342–348. doi: 10.1152/advan.00193.2015. [DOI] [PubMed] [Google Scholar]
- 37. West JB. Challenges in teaching the mechanics of breathing to medical and graduate students. Adv Physiol Educ . 2008;32:177–184. doi: 10.1152/advan.90146.2008. [DOI] [PubMed] [Google Scholar]
- 38. Yawn BP, Yawn RA. Spirometry testing education in medical schools: a missed opportunity? Prim Care Respir J . 2005;14:21–24. doi: 10.1016/j.pcrj.2004.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Block JA. Who will teach the medical students? Chest . 1995;107:1. doi: 10.1378/chest.107.1.1. [DOI] [PubMed] [Google Scholar]
- 40. Blatt AE, Nofziger AC, Levy PC. Incorporating medical student documentation into the billable encounter a pragmatic approach to implementation of the 2018 Centers for Medicare & Medicaid Services Rule Revision. Chest . 2020;158:698–704. doi: 10.1016/j.chest.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 41.Lee HS, Anderson JR.Student learning: what has instruction got to do with it? Annu Rev Psychol 201364445–469.. [DOI] [PubMed] [Google Scholar]
- 42. Janssen-Noordman AMB, Merriënboer JJG, van der Vleuten CPM, Scherpbier AJJA. Design of integrated practice for learning professional competences. Med Teach . 2006;28:447–452. doi: 10.1080/01421590600825276. [DOI] [PubMed] [Google Scholar]
- 43. Merrill MD. First principles of instruction. ETR&D . 2002;50:43–59. [Google Scholar]
- 44. Kühl T, Eitel A, Damnik G, Körndle H. The impact of disfluency, pacing, and students’ need for cognition on learning with multimedia. Comput Human Behav . 2014;35:189–198. [Google Scholar]
- 45.Wichmann A, McNamara DS, Bolzer M, Strijbos JW, Fischer F, Leiba M, et al. 20141416–1425..
- 46. Damnik G, Proske A, Körndle H. Designing a constructive learning activity with interactive elements: the effects of perspective-shifting and the quality of source material. Interact Learn Environ . 2017;25:634–649. [Google Scholar]
- 47. Goldin I, Narciss S, Foltz P, Bauer M. New directions in formative feedback in interactive learning environments. Int J Artif Intell Educ . 2017;27:385–392. [Google Scholar]
- 48. Joughin G. Scaling up assessment for learning in higher education. Assess Eval High Educ . 2018;43:341–343. [Google Scholar]
- 49. Narciss S. The impact of informative tutoring feedback and self-efficacy on motivation and achievement in concept learning. Exp Psychol . 2004;51:214–228. doi: 10.1027/1618-3169.51.3.214. [DOI] [PubMed] [Google Scholar]
- 50. Glazer N. Challenges with graph interpretation: a review of the literature. Stud Sci Educ . 2011;47:183–210. [Google Scholar]
- 51.Narciss S. Scaling up assessment for learning in higher education: the enabling power of assessment. Singapore: Springer; 2017. Conditions and effects of feedback viewed through the lens of the interactive tutoring feedback model; pp. 173–189. [Google Scholar]
- 52. Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA . 2007;298:1002–1009. doi: 10.1001/jama.298.9.1002. [DOI] [PubMed] [Google Scholar]


