Shared decision making (SDM) is a collaborative process in which patients and providers work together to create mutually agreed‐on care plans. 1 SDM centers patients' values and preferences and can improve patient‐provider communication and patient experience. SDM is both grounded in and a natural extension of patient‐centered care and has the potential to advance health equity. 1 , 2 We further propose that SDM should take into account the unique social context that contributes to health outcomes. In doing so, SDM can become a lever for improving the quality of cardiovascular care and reducing disparities in cardiovascular disease (CVD). 1 , 3
Disparities in Cardiovascular Care
Despite advances in prevention and treatment that have led to overall reductions in CVD prevalence, morbidity, and mortality, 4 , 5 significant disparities among historically marginalized racial and ethnic groups remain. Although factors beyond the health care setting may contribute to these differences, the Institute of Medicine's Unequal Treatment 6 report revealed that disparities may be attributable to differences in quality of health care. For example, compared with White people, Black people are 3 times more likely to have CVD‐related mortality, 7 and the risk‐adjusted mortality after acute myocardial infarction is significantly higher in hospitals that disproportionately serve Black patients. 8 In addition, a “race‐based invasive procedure gap” exists, where Black patients are less likely than White patients to receive potentially life‐saving procedures, such as percutaneous coronary intervention, coronary bypass grafting, or implantable defibrillator placement. 9 Furthermore, race is often used as a correction factor for calculating cardiovascular‐related risk scores, which often guide conversations related to risk assessment and treatment planning between clinicians and patients. Racial adjustments (eg, changing a patient's race from White to Black) alter risk scores, and may result in inequitable distribution of resources and therapeutic options. 10
Racism, Not Race
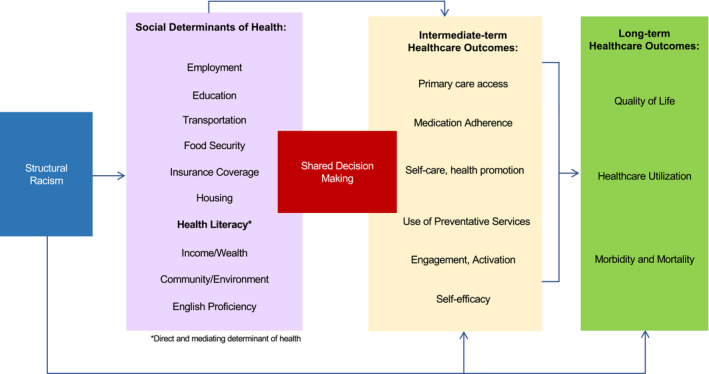
Rather than reliance on race as a biological indicator, risk scores and treatment discussions might be more accurately and effectively guided by understanding lived experiences of racism. Race is a socially constructed label and a poor proxy for physiological and biologic processes. Racism is a system that assigns values and structures opportunities “based on the social interpretation of how one looks.” 11 Racism operates at individual and institutional or structural levels and has downstream social consequences that contribute to the differentials in observed health outcomes. 11 Structural racism “refers to the totality of ways in which societies foster racial discrimination, through mutually reinforcing inequitable systems, that in turn reinforce discriminatory beliefs, values, and distribution of resources, which together affect the risk of adverse health outcomes.” 12 A recent statement from the American Heart Association on structural racism describes how racialized historical and contemporary policies and practices have created fundamental differences in access to health‐supporting resources, including neighborhood environments, employment, educational opportunities, and health care access itself, also known as social determinants of heath (SDoH). 2 , 13 We adapted concepts based on the scientific statements by the American Heart Association on structural racism and health literacy to articulate the symbiotic relationships among structural racism, SDoH, SDM (with the patient‐provider encounter as a conduit), and intermediate‐ and long‐term health care outcomes in (Figure 1). As clinicians and researchers seek interventions to mitigate consequences of structural racism, we propose SDM as a viable health care tool to identify and address structural inequities and resultant social risk factors to optimize care planning and promote health equity in CVD. 4 , 5
Figure 1. Interdependence between structural racism, shared decision making, and social determinants of health on health care outcomes.
SDM: A Link Between Patient‐Centered Care and CVD Health Equity
In its 2001 report, Crossing the Quality Chasm: A New Health System for the 21st Century, the Institute of Medicine identified patient‐centered care and equity as 2 of the 6 fundamental elements of high‐quality health care. 14 Patient‐centered care refers to responsive care focused on patients' values, preferences, and needs. With patient‐centered care, the patient‐provider relationship is a partnership based on respecting the patient, promoting patient education, patients' active participation in self‐management of existing conditions, and providing patients support and information to encourage informed decision making. 14 Equity in health care refers to the provision of high‐quality care regardless of personal attributes and the ability of each patient to have equal opportunity to attain his/her highest level of health.
SDM is one approach that may address the intersection of patient's preferences and values, SDoH, and scientific evidence within the context of the clinical encounter to promote health equity (Figure 2). 14 , 15 With SDM, patients are well informed about the details of their diagnosis, and their values and preferences are centered throughout care planning. The clinician and patient each bring unique expertise to the clinical encounter and work as equal partners in making care‐delivery decisions, such as selecting diagnostic tests, treatments, and other evidence‐based ancillary services (eg, home health) that consider the balance of anticipated outcomes, risks, and benefits, as well as the patient's values and preferences. 1 Elwyn and colleagues describe an approach to SDM in clinical practice “based on choice, option and decision talk,” 16 with a 3‐step model: (1) introducing choice, (2) describing options, often with decision aids, and (3) helping patients explore preferences and make decisions in the context of their values. We additionally believe that patients' lived experiences of SDoH should be considered, as they reflect “the conditions in which people are born, grow, live, work and age, shaped by the distribution of money, power and resources at global, national and local levels … and are mostly responsible for health inequities.” 17 Through SDoH‐responsive SDM processes, patients take part in defining and planning toward their attainment of their “highest level of health.” In addition, by addressing SDoH, SDM could have a greater impact on the root cause of disparities, structural racism, from which SDoH have their origin.
Figure 2. Expanded model of shared decision making, accounting for patient‐centered care, social determinants of health, and health equity.
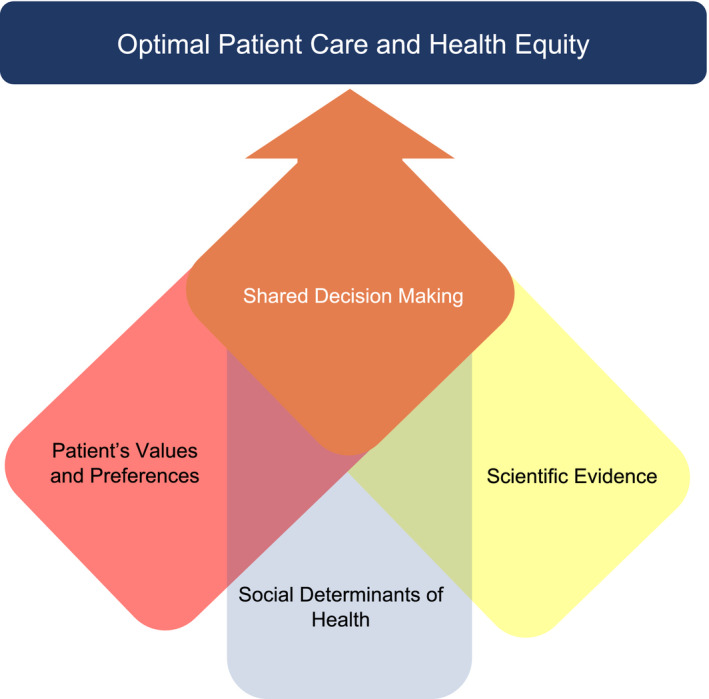
Reproduced with permission from JAMA. 2014;312:1295–1296. 15 ©2014 American Medical Association. All rights reserved.
SDM and CVD Outcomes
Scientific statements have been published on SDM and cardiac surgery, 18 and recent studies have evaluated the role of SDM in communicating absolute CVD risk, when considering a left ventricular assist device as destination therapy, 19 and for treatment planning with symptomatic aortic stenosis. 20 In addition, editorials exist discussing the role of SDM in specific patient care populations, including among patients with hypertension, 3 patients with heart failure, 21 older adults, 22 and athletes with CVD. 23 In some studies in hypertension and heart failure care, SDM is associated with better patient‐reported satisfaction, quality of life, 24 adherence to medical therapy, 25 symptom improvement, and decreases in both systolic and diastolic blood pressures. Conversely, some studies examining SDM in cardiovascular care have found no appreciable impact in decisions, care, or outcomes, 26 and poor SDM is associated with poor patient‐reported health outcomes and lower satisfaction. 27 However, little information is available on the quality and frequency of SDM. Future research should seek to understand consequences of poor SDM on the quality of cardiovascular care and related health outcomes as well as potential benefits for sustaining SDM models of care.
Consideration of SDoH in Clinical Practice
Understanding SDoH is critical to reaching decisions that align with patients' values, preferences, and life circumstances. To incorporate SDoH considerations into daily clinical practice, clinicians should make SDoH assessment and their potential impact, individually and interactively, on the patient's care and decision making, a routine part of clinical encounters. Through SDM, decisions may be made that take into consideration the interaction of different SDoH elements that may not only contextualize patient behavior, but reveal important details relevant for treatment/care planning to promote successful adherence. For example, reliable transportation or stable housing can impact patients' engagement in care, affecting their ability to attend appointments regularly or store medications/therapies safely. Assessment of cultural preferences and SDoH start with preferred language(s) of communication and health literacy and include education level, income, insurance, housing, transportation, and food security.
Clinicians can assess SDoH using screening tools, such as the Protocol for Responding to and Assessing Patients' Assets, Risks, and Experiences, the Health‐Related Social Needs Screening Tool, or the EveryONE Project. These assessments can be incorporated into the clinical workflow or electronic medical record and documented in patients' records. Health care support staff can be instrumental in this process, especially in the outpatient or nonemergent settings, where these assessments can be performed and documented before the clinician encounter. The urgency and complexity of the clinical decision may affect when to address the SDoH that influence SDM. Some SDoH, such as preferred language and education level, need to be addressed before engaging in SDM. Patients' physical and social environments must also be considered before making treatment decisions.
Similarly, to implement lifestyle modifications to reduce the risk of CVD risk factors (eg, obesity and hypertension), patients should have access to healthy food and safe outdoor spaces to exercise. To facilitate this process, clinicians can engage in social prescribing, which is an interdisciplinary approach involving referrals to community nonclinical services, to integrate food and exercise prescription programs into their practice. Food prescription programs (eg, FoodRx and Fruit and Vegetable Prescription, among others) allow clinicians to prescribe fruits and vegetables to people who are food insecure and provide information about community resources, often incorporating food coupons. 28 Physical activity programs (such as the Prescribing Parks, ParkRx, and Exercise Is Medicine programs) can connect patients to parks and community‐based resources to provide safe places for physical activity. 29
Beyond identifying SDoH elements that impact SDM, clinicians should work together with other members of the health care team to resolve identified SDoH gaps. Collaboration with care coordinators, case managers, and/or community health workers may provide much‐needed aid. These evidence‐based health care support staff have access to and knowledge of institutional and community resources to improve patients' quality of life and reduce health disparities. These support staff can go a long way in helping to improve patients' access to beneficial resources when relevant SDoH deficits are encountered. 30 For example, these support staff often help in arranging alternate transportation or home health visits for those with barriers to transportation, and they may provide information on food assistance or safe community resources for physical activity. Referrals to relevant support staff can be incorporated to workflows in the electronic medical record when relevant SDoH deficits are encountered. SDoH deficits may be revealed with inquiries about food insecurity before prescribing medications that require food consumption, internet access, and stability before scheduling telemedicine visits, and housing stability or refrigeration for medication storage. Involving support staff in these roles may help address challenges to implementation, such as lack of time.
Finally, in discussing SDoH deficits, it is important to consider financial insecurity as they play a significant part in decision making. Although often outside the purview of the support staff, the support staff can refer patients to medical financial advisors; and interactions that address patients' financial situations and medical costs can help socioeconomically disadvantaged patients choose treatment courses that align with their resources.
Addressing the SDoH requires interdisciplinary support and ultimately may require policy‐level solutions to improve health determinants (eg, access to healthy food and safe spaces for physical activity). This may be outside the scope of general medical practice; however, clinicians can advocate for the ways in which social and structural determinants of health can change among the people in communities they serve to cardiovascular health. For example, with community education/outreach, there may be written or oral testimony on health or SDoH‐related policy and collaborations to fundraise or mobilize resources, among others. 31
SDM That Addresses SDoH and Communication
Above all, patients have the need and right to understand clinical options and alternatives, and have enough information to weigh the pros and cons, and make informed decisions. Clinicians should therefore engage patients in dialogue that goes beyond the risk and benefits of their decisions to address the impact of the decision at hand on other aspects of the patients' lives. Conversations that equally values psychosocial or socioemotional exchanges and the lived experiences of patients as much as biomedical or procedural talk and the clinician's clinical expertise are required. 32 Clinicians should also pay attention to patients' health literacy needs and assess patients' knowledge and understanding throughout the SDM process.
An example tying the elements just discussed together could include the following: A 47‐year‐old man with a history of stage 3 chronic kidney disease is diagnosed with viral pericarditis. Treatment options include glucocorticoids, colchicine, or an NSAID, which should not be taken on an empty stomach. During the course of his interactions with his medical team, he has the diagnosis and treatment options explained to him, and an assessment of his health priorities, values, and social situation (SDoH) is made and he is found to have up to a high school education, be food insecure, and be able to afford only about half of his monthly medication needs. He agrees to take the colchicine but is concerned about the cost of the medication; in addition, he expresses hesitation in taking the NSAIDs given his renal impairment. He also considers an alternative treatment option, a glucocorticoid, and the clinician discusses risks and benefits of the NSAID compared with glucocorticoid use. Together, the patient and clinician decide on a combination of glucocorticoids and colchicine, and case management is engaged to work with him to find affordable sources of the medication through a scaled financial assistance plan. A follow‐up appointment is made to assess his status and tolerance for the treatment, with options for pursuing alternative therapies. Case management also provides him with information for food pantries close to his residence.
Patient‐provider relationships that encourage open and transparent communication may help identify relevant SDoH. However, SDM is often what helps patients and clinicians consider those SDoH that are relevant to treatment planning and are potential barriers to practical application of treatment recommendations. To improve patient‐provider interactions, clinicians should engage in communication techniques that reinforce SDM, including using open‐ended questions, using periodic pauses (to assess understanding), summarizing, or using teach‐back at the end the interaction and even using communication aids.
Certain groups of people (including older adults, immigrants, and people with less education and literacy) may perceive high‐quality SDM differently for several reasons, including low health literacy, mistrust (of health care providers), cultural norms on clinician interactions, or preconceived notions about the physician‐provider relationship, among others. For example, a study examining SDM among Black patients with diabetes reported that Black patients perceived high‐quality SDM as being able to “tell their story and be heard” by clinicians. 33 These findings imply that in the context of health disparities, a disconnect may exist between what clinicians believe high‐quality SDM to be and patients' perception of what high‐quality SDM is; and therefore, clinicians must not use a one size fits all approach to achieve high‐quality SDM. High‐quality SDM may also be beneficial in ways that are not as tangible (eg, promoting trust and feelings of respect). For example, when the patient's well‐being is the focus of care (patient‐centered care) and the clinician takes the opportunity to incorporate the patient's values, social situation, and goals, engaging in SDM may build trust, value, and mutual respect. Thus, high‐quality SDM improves the therapeutic alliance between clinicians and patients, short‐term outcomes, intermediate outcomes, and, ultimately, long‐term outcomes.
It is possible that our current models of SDM do not prioritize our patients' values related to defining SDM or that clinicians need to pay more attention to patients' preferences and their self‐described needs. As clinicians, the onus is on us to ensure that patients are engaged in SDM, even if that requires modifying our communication behaviors and providing more resources to specific groups of people, especially people who have been historically marginalized and underserved.
Use of Decision Aids
Patient decision aids are often used to support SDM. Decision aids can take the form of brochures, videos, web‐based programs, and the like, and can be used before (in preparation for) or during the clinical encounter. These tools help facilitate patient‐provider discussions, increase patient knowledge and well‐being, decrease anxiety and decisional conflict, and serve as a reference for future use. 34 Within CVD care specifically, evidence suggests that decision aids have a positive impact on decision making across a broad range of therapeutic decisions. 34 In addition, decision aids can help patients access information in a way that allows them to reflect on whether the presented therapeutic option is in line with their values. This is particularly important for historically marginalized patient populations or those with low health literacy. However, the potential role of decision aids in improving health inequities among these populations remains understudied.
To improve health equity, innovative culturally relevant decision aids are needed to engage patients with low literacy levels, patients who are socioeconomically disadvantaged, and those from underrepresented and marginalized backgrounds. There is also a need for more rigorous evaluations to understand how decision aids can best acknowledge the social, historical, and contemporary contexts of marginalized and underrepresented populations.
Potential Barriers to Using SDM in Practice
Despite its potential utility, there is a dearth of literature on the implementation of SDM to improve CVD disparities. Several practice‐based factors, including those specific to cardiovascular care, may render the benefits of SDM unrealized: underuse of SDM in clinical practice, reliance solely on the biomedical model (while excluding psychosocial factors) in the choice of treatment modalities, need for decision planning in urgent situations (eg, cardiac catheterization for acute coronary syndrome), time constraints of clinical practice, and perceptions of social and professional roles in addressing SDoH within the context of clinical practice. Not specific to cardiovascular care, bias, both implicit and explicit, may play a role in providers' perceptions of patients' ability to participate in decision making or adhere to specific therapeutic options. Although SDM does not address the structural bias that may be inherent in the health care system, a clinician's conscious choice to include patients as equal partners in care planning through SDM may help mitigate individual‐level bias and improve patients' experience and quality of care.
Future Directions for SDM in CVD Care and Disparities Elimination
The value of SDM and its potential in improving equity in cardiovascular care should be recognized by clinicians and institutions alike. Federal agencies, such as the Centers for Medicare and Medicaid Services, require SDM, including the use of evidence‐based patient decision aids, as a condition for provider reimbursement for some cardiovascular conditions (for nonprocedural therapies or decisions) and procedures. Currently, the Centers for Medicare and Medicaid Services requires SDM for reimbursement for some CVD procedures, including implantable cardioverter‐defibrillator placement and left atrial appendage closure therapy. In addition to procedures, tools specifically designed to support SDM for nonprocedural therapies and conditions in cardiovascular care exist and include decision aids for acute chest pain, arrhythmias (eg, nonvalvular atrial fibrillation), hypertension, heart failure, peripheral artery disease, hyperlipidemia (statin therapy), and stroke, among others. However, despite the requirements for SDM, more evidence is needed to shed light on the impact that these requisites and established SDM tools have on actual health outcomes and disparities.
Conclusions
SDM requires valuing patients as equally positioned and important partners in their care. It is not only the right thing to do from the standpoint of autonomy, but it is essential for collaborating with patients to achieve their desired outcomes and is particularly important when the goal is sustained behavioral change. Sharing power in the prioritization of care needs as well as options for treatment may lead to a greater sense of self‐determination and agency, which ultimately may augment patient activation, improve outcomes, and advance health equity. This requires a cultural shift in the practice of medicine from top‐down to a position that honors patients as experts in their own lived experiences. Such a level of respect for diverse perspectives may facilitate a sense of mutual respect between clinicians and patients during the health care encounter, which could lead to more effective decision sharing and better, more equitable management of cardiovascular conditions.
Sources of Funding
Dr Turkson‐Ocran is supported by the Strategically Focused Research Network Award from the American Heart Association (17SFRN33590069). Dr Ogunwole is supported by a training grant from the Health Resources and Services Administration (Institutional National Research Service Award T32HP10025BO). Dr Hines is supported by an award from the National Heart, Lung and Blood Institute (1K01HL152011‐01A1). Dr Peterson is supported by an award from the National Heart, Lung, and Blood Institute (5R33HL14332403).
Disclosures
Dr Peterson is supported by grants from National Heart, Lung, and Blood Institute and serves as a Senior Associate Editor for the Journal of the American Heart Association. The remaining authors have no disclosures to report.
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
This article was sent to Viola Vaccarino, MD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
Ruth‐Alma N. Turkson‐Ocran is a member of the JAHA Early Career Editorial Board.
For Sources of Funding and Disclosures, see page 6.
References
- 1. National Learning Consortium Shared decision making fact sheet. Washington DC: The Office of the National Coordinator for Health Information Technology; 2017. Available at: https://www.healthit.gov/sites/default/files/nlc_shared_decision_making_fact_sheet.pdf. Accessed September 1, 2021.
- 2. Magnani JW, Mujahid MS, Aronow HD, Cené CW, Dickson VV, Havranek E, Morgenstern LB, Paasche‐Orlow MK, Pollak A, Willey JZ. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. 2018;138:e48–e74. doi: 10.1161/CIR.0000000000000579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Langford AT, Williams SK, Applegate M, Ogedegbe O, Braithwaite RS. Partnerships to improve shared decision making for patients with hypertension—health equity implications. Ethn Dis. 2019;29:97–102. doi: 10.18865/ed.29.S1.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 5. Weisfeldt ML, Zieman SJ. Advances in the prevention and treatment of cardiovascular disease. Health Aff. 2007;26:25–37. doi: 10.1377/hlthaff.26.1.25 [DOI] [PubMed] [Google Scholar]
- 6. Betancourt JR, King RK. Unequal treatment: the Institute of Medicine report and its public health implications. Public Health Rep. 2003;118:287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Willis M, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 8. Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yancy CW, Wang TY, Ventura HO, Piña IL, Vijayaraghavan K, Ferdinand KC, Hall LL. The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (credo): why credo matters to cardiologists. J Am Coll Cardiol. 2011;57:245–252. doi: 10.1016/j.jacc.2010.09.027 [DOI] [PubMed] [Google Scholar]
- 10. Vyas DA, Eisenstein LG, Jones DS. Hidden in plain sight—reconsidering the use of race correction in clinical algorithms. N Engl J Med. 2020;383:874–882. doi: 10.1056/NEJMms2004740 [DOI] [PubMed] [Google Scholar]
- 11. Jones CP. Action and allegories. In: Ford CL, Griffith DM, Bruce MA, Gilbert KL, eds. Racism: Science & Tools for the Public Health Professional. Washington DC: American Public Health Association; 2019:223–241. Available at: https://ajph.aphapublications.org/doi/abs/10.2105/9780875533049ch11 [Google Scholar]
- 12. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 13. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 14. Institute of Medicine Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press (US); 2001. [Google Scholar]
- 15. Hoffmann TC, Montori VM, Del Mar C. The connection between evidence‐based medicine and shared decision making. JAMA. 2014;312:1295–1296. doi: 10.1001/jama.2014.10186 [DOI] [PubMed] [Google Scholar]
- 16. Elwyn G, Frosch D, Thomson R, Joseph‐Williams N, Lloyd A, Kinnersley P, Cording E, Tomson D, Dodd C, Rollnick S, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Healthy People 2030. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Available at: https://health.gov/healthypeople/objectives‐and‐data/browse‐objectives. Accessed September 1, 2021.
- 18. Mihalj M, Carrel T, Urman RD, Stueber F, Luedi MM. Recommendations for preoperative assessment and shared decision‐making in cardiac surgery. Curr Anesthesiol Rep. 2020;10:185–195. doi: 10.1007/s40140-020-00377-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Allen LA, McIlvennan CK, Thompson JS, Dunlay SM, LaRue SJ, Lewis EF, Patel CB, Blue L, Fairclough DL, Leister EC, et al. Effectiveness of an intervention supporting shared decision making for destination therapy left ventricular assist device: the DECIDE‐LVAD randomized clinical trial. JAMA Intern Med. 2018;178:520–529. doi: 10.1001/jamainternmed.2017.8713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Coylewright M, O’Neill E, Sherman A, Gerling M, Adam K, Xu K, Grande SW, Dauerman HL, Dodge SE, Sobti NK, et al. The learning curve for shared decision‐making in symptomatic aortic stenosis. JAMA Cardiol. 2020;5:442–448. doi: 10.1001/jamacardio.2019.5719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Enard KR, Hauptman PJ. Heart failure, shared decision‐making, and social determinants of health: an upstream perspective. JAMA Cardiol. 2019;4:609–610. doi: 10.1001/jamacardio.2019.1763 [DOI] [PubMed] [Google Scholar]
- 22. Backman WD, Levine SA, Wenger NK, Harold JG. Shared decision‐making for older adults with cardiovascular disease. Clin Cardiol. 2020;43:196–204. doi: 10.1002/clc.23267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Baggish AL, Ackerman MJ, Putukian M, Lampert R. Shared decision making for athletes with cardiovascular disease: practical considerations. Curr Sports Med Rep. 2019;18:76–81. doi: 10.1249/JSR.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 24. Korteland NM, Ahmed Y, Koolbergen DR, Brouwer M, de Heer F, Kluin J, Bruggemans EF, Klautz RJM, Stiggelbout AM, Bucx JJJ, et al. Does the use of a decision aid improve decision making in prosthetic heart valve selection? Circ Cardiovasc Qual Outcomes. 2017;10:e003178. doi: 10.1161/CIRCOUTCOMES.116.003178 [DOI] [PubMed] [Google Scholar]
- 25. Schoenthaler A, Rosenthal DM, Butler M, Jacobowitz L. Medication adherence improvement similar for shared decision‐making preference or longer patient‐provider relationship. J Am Board Fam Med. 2018;31:752–760. doi: 10.3122/jabfm.2018.05.180009 [DOI] [PubMed] [Google Scholar]
- 26. Kunneman M, Branda ME, Hargraves IG, Sivly AL, Lee AT, Gorr H, Burnett B, Suzuki T, Jackson EA, Hess E, et al. Assessment of shared decision‐making for stroke prevention in patients with atrial fibrillation: a randomized clinical trial. JAMA Intern Med. 2020;180:1215–1224. doi: 10.1001/jamainternmed.2020.2908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hughes TM, Merath K, Chen Q, Sun S, Palmer E, Idrees JJ, Okunrintemi V, Squires M, Beal EW, Pawlik TM. Association of shared decision‐making on patient‐reported health outcomes and healthcare utilization. Am J Surg. 2018;216:7–12. doi: 10.1016/j.amjsurg.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 28. Trapl ES, Smith S, Joshi K, Osborne A, Benko M, Thornton Matos A, Bolen S. Dietary Impact of Produce Prescriptions for Patients With Hypertension. Prev Chronic Dis. 2018;15:E138. doi: 10.5888/pcd15.180301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Müller‐Riemenschneider F, Petrunoff N, Yao J, Ng A, Sia A, Ramiah A, Wong M, Han J, Tai BC, Uijtdewilligen L. Effectiveness of prescribing physical activity in parks to improve health and wellbeing ‐ the park prescription randomized controlled trial. Int J Behav Nutr Phys Act. 2020;17:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community health worker support for disadvantaged patients with multiple chronic diseases: a randomized clinical trial. Am J Public Health. 2017;107:1660–1667. doi: 10.2105/AJPH.2017.303985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haq C, Stiles M, Rothenberg D, Lukolyo H. Effective advocacy for patients and communities. Am Fam Physician. 2019;99:44–46. [PubMed] [Google Scholar]
- 32. Hines AL, Roter D, Ghods Dinoso BK, Carson KA, Daumit GL, Cooper LA. Informed and patient‐centered decision‐making in the primary care visits of African Americans with depression. Patient Educ Couns. 2018;101:233–240. doi: 10.1016/j.pec.2017.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Peek ME, Quinn MT, Gorawara‐Bhat R, Odoms‐Young A, Wilson SC, Chin MH. How is shared decision‐making defined among African‐Americans with diabetes? Patient Educ Couns. 2008;72:450–458. doi: 10.1016/j.pec.2008.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sepucha KR. Shared decision‐making and patient decision aids: is it time? Circ Cardiovasc Qual Outcomes. 2012;5:247–248. doi: 10.1161/CIRCOUTCOMES.112.966192 [DOI] [PubMed] [Google Scholar]


