Abstract
Background
The relationship between COVID‐19 and ischemic stroke is poorly understood due to potential unmeasured confounding and reverse causation. We aimed to leverage genetic data to triangulate reported associations.
Methods and Results
Analyses primarily focused on critical COVID‐19, defined as hospitalization with COVID‐19 requiring respiratory support or resulting in death. Cross‐trait linkage disequilibrium score regression was used to estimate genetic correlations of critical COVID‐19 with ischemic stroke, other related cardiovascular outcomes, and risk factors common to both COVID‐19 and cardiovascular disease (body mass index, smoking and chronic inflammation, estimated using C‐reactive protein). Mendelian randomization analysis was performed to investigate whether liability to critical COVID‐19 was associated with increased risk of any cardiovascular outcome for which genetic correlation was identified. There was evidence of genetic correlation between critical COVID‐19 and ischemic stroke (rg=0.29, false discovery rate [FDR]=0.012), body mass index (rg=0.21, FDR=0.00002), and C‐reactive protein (rg=0.20, FDR=0.00035), but no other trait investigated. In Mendelian randomization, liability to critical COVID‐19 was associated with increased risk of ischemic stroke (odds ratio [OR] per logOR increase in genetically predicted critical COVID‐19 liability 1.03, 95% CI 1.00–1.06, P‐value=0.03). Similar estimates were obtained for ischemic stroke subtypes. Consistent estimates were also obtained when performing statistical sensitivity analyses more robust to the inclusion of pleiotropic variants, including multivariable Mendelian randomization analyses adjusting for potential genetic confounding through body mass index, smoking, and chronic inflammation. There was no evidence to suggest that genetic liability to ischemic stroke increased the risk of critical COVID‐19.
Conclusions
These data support that liability to critical COVID‐19 is associated with an increased risk of ischemic stroke. The host response predisposing to severe COVID‐19 is likely to increase the risk of ischemic stroke, independent of other potentially mitigating risk factors.
Keywords: COVID‐19, cross‐trait linkage disequilibrium score regression, ischemic stroke, Mendelian randomization
Subject Categories: Ischemic Stroke, Genetics, Epidemiology
Nonstandard Abbreviations and Acronyms
- Fdr
false discovery rate
- IVW
inverse‐variance weighted
- LDSC
linkage disequilibrium score regression
- MR
Mendelian randomization
Clinical Perspective
What Is New?
This study identified evidence of genetic correlation between critical COVID‐19 and ischemic stroke, body mass index and C‐reactive protein.
In Mendelian randomization, liability to critical COVID‐19 was associated with increased risk of any ischemic stroke, with similar estimates obtained for ischemic stroke subtypes.
There was no evidence to suggest that genetic liability to ischemic stroke increased the risk of critical COVID‐19.
What Are the Clinical Implications?
These data support that liability to critical COVID‐19 is associated with an increased risk of ischemic stroke.
The host response predisposing to severe COVID‐19 is likely to increase the risk of ischemic stroke, independent of other potentially mitigating risk factors.
SARS‐CoV‐2 infection is the cause of the COVID‐19 pandemic that has resulted in a health crisis of unprecedented magnitude. 1 , 2 While much of the disease burden relates to respiratory failure and sepsis, some studies suggest an increased risk of ischemic stroke. 3 , 4 , 5 , 6 This has been estimated to be seven times greater than in influenza infection, 3 with up to 5% of people with severe COVID‐19 suffering stroke. 5 Strokes that occur in individuals with COVID‐19 are more severe, have poorer outcomes, and higher mortality rates than in those without COVID‐19, despite similar acute management. 6 , 7 Indeed, almost two‐fifths of people with COVID‐19 who develop stroke consequently die. 8 However, some studies do not support an increased risk of stroke in individuals with COVID‐19. 9 , 10 Obtaining unbiased estimates for the risk of stroke in people with COVID‐19 is challenging due to difficulty diagnosing mild COVID‐19 and an overall reduction in the rate of admission to hospital with stroke, and minor stroke in particular, during the pandemic, 9 , 11 Furthermore, observational studies investigating the association between COVID‐19 and stroke are vulnerable to potential confounding and reverse causation. 3 , 4 , 5 , 6 For example, there are common risk factors for severe COVID‐19 and stroke, such as obesity and smoking. 12 Similarly, patients with acute stroke have a dampened immune response and may be more susceptible to severe COVID‐19. 13
Leverage of genetic data can help overcome some of these issues. Cross‐trait linkage disequilibrium score regression (LDSC) can be used to estimate the genetic correlation between traits. Mendelian randomization (MR) can be employed to investigate whether genetic variants predicting an exposure (such as COVID‐19) also associate with risk of an outcome (such as ischemic stroke). 14 There are numerous plausible mechanisms by which COVID‐19 may be increasing ischemic stroke risk. COVID‐19 can trigger a cytokine storm with upregulation of pro‐inflammatory signaling and endothelial dysfunction that predisposes to a hypercoagulable state and can lead to thromboembolic events. 15 Indeed, COVID‐19 also appears to promote the development of other cardiovascular disorders including myocardial injury, myocardial ischemia, arrhythmias, heart failure, and venous thromboembolism. 15 Furthermore, pre‐existing cardiovascular disease (CVD) is associated with high mortality in people with COVID‐19, which has raised the possibility of a bidirectional interaction between COVID‐19 and the cardiovascular system. 15 MR analyses also can allow the exploration of such bidirectional relationships.
Elucidating the relationship between COVID‐19 and risk of ischemic stroke could prove important for optimizing prevention and treatment strategies. With this in mind, we performed cross‐trait LDSC to investigate whether there is a genetic correlation between COVID‐19 and ischemic stroke, and followed this up with MR analyses to investigate whether any such statistically significant correlation might be explained by liability to COVID‐19 being associated with increased risk of ischemic stroke.
Methods
All genetic association data used in this work are publicly accessible. Appropriate patient consent and ethical approval had been obtained in the original studies from which they were obtained (Table S1). Statistical code related to the analyses performed in the current study is freely available from Github (https://github.com/verena‐zuber/covid19_and_stroke).
Study Overview
First, we performed cross‐trait LDSC to estimate genetic correlations for COVID‐19 with ischemic stroke, other related CVDs, and risk factors common to both COVID‐19 and CVD. Second, for CVD outcomes that showed evidence of genetic correlation with COVID‐19, MR analysis was performed to investigate whether liability to COVID‐19 was also associated with these outcomes. Finally, bidirectional MR was carried out to investigate potential reverse associations, ie whether genetic liability to the CVD outcome was also associated with increased risk of COVID‐19. A graphical overview of the analysis plan is presented in Figure S1.
Exposure Definitions and Genetic Association Estimates for COVID‐19
Genetic association estimates for COVID‐19 were obtained from release 5 of the COVID‐19 host genetics consortium. 16 , 17 In our main analysis we focused on the most severe definition of COVID‐19 available (referred to critical COVID‐19 from here), where a critical case is defined as an individual who was hospitalized with laboratory confirmed SARS‐CoV‐2 infection and required respiratory support or died. Genetic associations were derived from 5101 cases and 1 383 241 controls from the general population. Hospital admission and requiring respiratory support or death is a proxy for disease severity and is preferred here over other case definitions which are solely based on a positive COVID‐19 test result. Previous studies have shown that bias may impact analyses identifying cases based on likelihood of testing for SARS‐CoV‐2 infection, because participants being tested for SARS‐CoV‐2 infection are selected for a wide range of genetic, behavioral, and demographic traits. 9
Results based on other COVID‐19 definitions from the COVID‐19 host genetics consortium were performed as further sensitivity analysis. As the first sensitivity analysis definition, we compared individuals with laboratory confirmed SARS‐CoV‐2 infection who had been hospitalized (cases) versus individuals with laboratory confirmed SARS‐CoV‐2 infection who did not require hospitalization (4829 cases and 11 816 controls). As a second analysis sensitivity definition, we compared individuals with laboratory confirmed SARS‐CoV‐2 infection who had been hospitalized (cases) versus the general population (9986 cases and 1 877 672 controls). The third sensitivity analysis definition was based on individuals with reported COVID‐19 (laboratory confirmed, physician‐reported or self‐reported; cases) versus controls from the general population (38 984 cases and 1 644 784 controls). An overview of the COVID‐19 definitions is given in Table S1.
Outcomes
Ischemic Stroke
The primary outcome was any ischemic stroke (34 217 cases). In secondary hypothesis‐generating analyses, stroke subtypes were further explored as large artery stroke (LAS, 4373 cases), cardioembolic stroke (CES, 7193 cases), and small vessel stroke (SVS, 5386 cases). 18 The common control pool included 406 111 individuals. Genetic association data were derived from the MEGASTROKE consortium. 18
Related CVD Outcomes
We considered other CVD outcomes related to ischemic stroke in their pathophysiology. These were coronary artery disease (including myocardial infarction, acute coronary syndrome, chronic stable angina, or >50% coronary artery stenosis), heart failure, and atrial fibrillation. Genetic associations with risk for coronary artery disease were measured on 60 801 cases and 123 504 controls and taken from the Coronary ARtery DIsease Genome wide Replication and Meta‐analysis (CARDIOGRAM) plus The Coronary Artery Disease (C4D) consortium (CARDIoGRAMplusC4D), 19 for heart failure were measured on 47 309 cases and 930 014 controls and taken from the HEart failuRe Molecular Epidemiology for therapeutic targetS (HERMES) consortium 20 and for atrial fibrillation were measured on 65 446 cases and 522 744 controls and taken from a transethnic meta‐analysis. 21
Risk Factors Related to Both COVID‐19 and CVD
To investigate whether any genetic correlation between critical COVID‐19 and the CVD outcomes was related to confounding factors, we further considered common risk factors to both, including obesity, smoking, and chronic inflammation. 22 , 23 , 24 , 25 Genetic association estimates to proxy these traits were taken from a genome‐wide association study (GWAS) on body mass index (BMI) measured on 694 649 subjects, 26 lifetime smoking index measured on 462 690 subjects, 27 and CRP (C‐reactive protein) measured on 361 194 individuals in UK Biobank. 28
Statistical Analysis
Cross‐Trait Linkage Disequilibrium Score Regression
We performed LDSC to estimate the genetic correlation (rg) of critical COVID‐19 with the primary outcome ischemic stroke, and secondary outcomes coronary artery disease, heart failure, and atrial fibrillation, using GWAS summary statistics data. 29 We also estimated correlation with possible genetic confounders, including BMI, lifetime smoking index, and CRP. We restricted our analyses to HapMap 3 single‐nucleotide polymorphisms (SNPs), which are known to be well‐imputed across most studies and utilized the pre‐computed European LD‐scores estimated using the 1000G reference panel, provided by the LDSC creators. For each set of summary statistics, the SNP‐specific sample size information was used. If not available, we assumed that all SNPs had the same sample size for that trait, defined as the total sample size for continuous phenotypes or as the sum of cases and controls for case/control phenotypes. By default, LDSC also removed variants that were duplicate, strand‐ambiguous, not SNPs (eg indels), with P‐values not between 0 and 1, with alleles that did not match with the 1000G reference panel, and with low effective sample size or not included in all studies of a GWAS meta‐analysis (if such information was available) for traits with no effective sample size information. After estimation of the genetic correlation across all phenotypes, we corrected for multiple hypothesis testing using the Benjamini and Yekutieli false discovery rate (FDR). 30 FDR‐corrected P‐values <0.05 were considered statistically significant.
Mendelian Randomization Analyses
Genetic Variants Used as Instrumental Variables
Genetic variants were selected based on associations with critical COVID‐19. In our main analysis, we selected uncorrelated genetic variants (clumped at correlation threshold r2<0.01) at P‐value <5×10−6. In sensitivity analyses, we applied a more stringent threshold and considered only genome‐wide significant genetic variants (P‐value <5×10−8).
Main Analysis
For CVD outcomes that showed evidence of genetic correlation with critical COVID‐19 in LDSC, MR analysis was performed to estimate the association of genetically predicted liability to critical COVID‐19 with that outcome using the random effects 2‐sample inverse‐variance weighted (IVW) method. 31 The IVW estimate can be biased by pleiotropy when a genetic variant associates the outcome (eg, ischemic stroke) via a pathway other than through the exposure (ie, liability to critical COVID‐19). Pleiotropy can cause heterogeneity in the MR estimates obtained by different variants employed as instruments, which was assessed using the Q‐statistic and the respective heterogeneity P‐value. 32 A Mendelian randomization estimate with P‐value <0.05 for the main IVW analysis was deemed to represent supportive evidence, given that MR was only performed to follow up positive LDSC findings.
Sensitivity Analyses—Robust Methods
We performed sensitivity analyses with pleiotropy‐robust two‐sample summary‐level MR approaches, including the weighted median MR 33 and MR‐Egger 34 to compare the MR estimates between different MR models. Each of these methods provides a statistically consistent estimator of the true causal estimate under different assumptions. The intercept of the MR‐Egger model represents a test for directional pleiotropy and we included this in sensitivity analyses. 35
Pleiotropic Pathways—Inflammation and Cardiometabolic Risk Factors
We further performed multivariable MR to adjust for potential pleiotropic pathways via cardiometabolic risk factors that are known to affect risk of both COVID‐19 and CVD12, including obesity (BMI), 26 lifetime smoking index, 27 and chronic inflammation (estimated using CRP). Multivariable MR includes all the respective genetic associations in a joint model to account for genetic confounding. 36 While univariable MR measures the total estimate of an exposure, multivariable MR measures the direct estimate of the exposure independent of other risk factors (ie, pleiotropy or genetic confounders) in the model. 37 In the multivariable MR model, we selected instruments based on the primary exposure of critical COVID‐19. We compared the multivariable MR model with the univariable MR model using likelihood ratio test to evaluate if accounting for the pleiotropic pathway provides a better model fit than the univariable MR model.
Bidirectional MR
For CVD outcomes that showed evidence of genetic correlation with critical COVID‐19 in LDSC, bidirectional MR was also performed to investigate for any association of genetic liability to that CVD outcome with risk of critical COVID‐19. Uncorrelated genetic variants (r2<0.01) associated with the CVD outcome at a P‐value <5×10−6 were selected as instruments.
Power Calculation
Power to detect an association of genetically proxied liability to critical COVID‐19 with all‐cause ischemic stroke and its subtypes was assessed using power calculations for MR. 38 Sample sizes were set according to the number of cases and controls in the MEGASTROKE consortium as given in Table S1. Heritability of the exposure was calculated from the F‐statistic of the genetic variants selected as instrumental variables, which was approximated using the squared regression coefficient divided by its squared standard error. The F‐statistic was then transformed to the proportion of variance in the phenotype explained by the genetic variants R2 using the Cragg–Donald transformation. 39
MR estimates are expressed as odds ratios (OR) per unit increase in the logOR of the exposure for binary traits. All analyses were performed using the ieugwasr (version 0.1.5) and MendelianRandomization (version 0.5.0) R packages. 40
Results
LD Score Regression
Performing LDSC, we found evidence of genetic correlation between critical COVID‐19 and ischemic stroke (rg=0.29, FDR‐P‐value=0.012) (Figure 1). Critical COVID‐19 was also genetically correlated with BMI (rg=0.21, FDR‐P‐value=0.00002) and CRP (rg=0.20, FDR‐P‐value=0.00035). We did not observe evidence for genetic correlation between critical COVID‐19 and the CVD outcomes (Table S2), and therefore focused the consequent MR analysis only on ischemic stroke and its subtypes.
Figure 1. Genetic correlation coefficient (x‐axis) with 95% CI for critical COVID‐19 and ischemic stroke, related cardiovascular disease outcomes, and risk factors for both COVID‐19 and cardiovascular disease (y‐axis), estimated by cross‐trait linkage disequilibrium score regression.
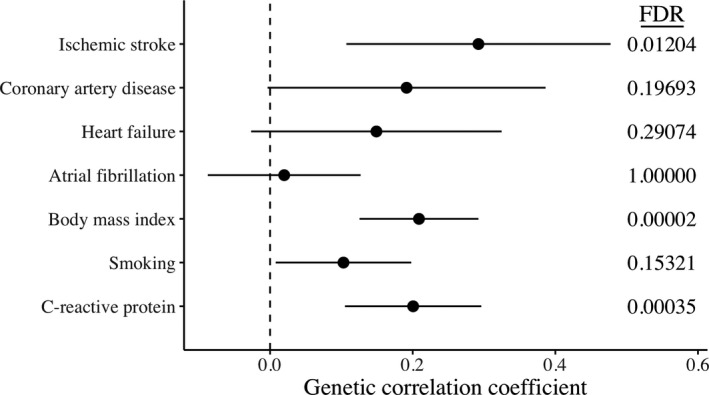
Multiple testing adjustment using the Benjamini and Yekutieli false discovery rate (FDR) are given on the right.
Mendelian Randomization
We selected 31 uncorrelated genetic variants as instrumental variables for liability to critical COVID‐19. These are detailed in Table S3, along with their associations with ischemic stroke and its subtypes. MR estimates are presented in Figure 2. In a univariable MR analysis, genetically proxied liability to critical COVID‐19 was associated with all‐cause ischemic stroke (OR 1.03, 95% CI 1.00 to 1.06, P‐value=0.03). Restricting to ischemic stroke subtypes, there were similar MR estimates for cardioembolic stroke (OR 1.06, 95% CI 1.01 to 1.12, P‐value=0.03), large artery stroke (OR 1.07, 95% CI 1.00 to 1.14, P‐value=0.06) and small‐vessel stroke (OR 1.05, 95% CI 1.00 to 1.11, P‐value=0.06). Power calculations shown in Figure S2 supported lower power for ischemic stroke subtypes compared to all‐cause ischemic stroke. For the MR estimates generated by different variants, we observed heterogeneity greater than would be expected by chance only for cardioembolic stroke (heterogeneity P‐value=0.049), but none of the other considered ischemic stroke categories.
Figure 2. Forest plot illustrating the Mendelian randomization estimates of liability to critical COVID‐19 with stroke outcomes based on inverse‐variance weighted Mendelian randomization using genetic variants that were associated with critical COVID‐19 at a P‐value level of 5×10‐6 or smaller.
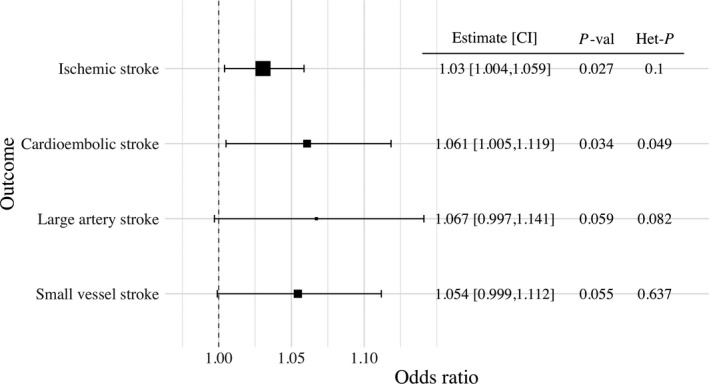
Mendelian randomization estimates represent the odds ratio of ischemic stroke outcomes per unit increase in the log‐odds ratio of liability to critical COVID‐19. Additional columns include the Mendelian randomization estimate, its 95% CI, the P‐value of the inverse‐variance weighted Mendelian randomization estimate to be different from 1 (P‐val), and heterogeneity measured by the Q‐statistic and the respective heterogeneity P‐value (Het‐P). Outcomes included any ischemic stroke, cardioembolic stroke, large artery stroke, and small vessel stroke.
Mendelian Randomization Sensitivity Analyses
Diagnostic scatterplots for ischemic stroke outcomes are presented in Figure S3. We observed consistent MR estimates for ischemic stroke risk in sensitivity analyses based on pleiotropy‐robust approaches as in the main analysis and none of the intercept estimates of MR‐Egger suggested directional pleiotropy (Table S4). In multivariable MR to investigate potential pleiotropy through risk factors common to both COVID‐19 and CVD, there was little evidence for attenuation of the size of the estimate in any of these analyses (Figure S4), which was confirmed by likelihood ratio test (Table S5).
Sensitivity Analysis Based on Genome‐Wide Significant Genetic Variants
As an additional sensitivity analysis, we used a more stringent P‐value threshold based on genome‐wide significance to select genetic variants as instrumental variables. We identified 9 uncorrelated genetic variants that associated with critical COVID‐19 at genome‐wide significance (P‐value <5×10−8 ). This MR analysis based on fewer variants generated consistent estimates to the main analysis, but with wider CIs that crossed the null, reflective of lower statistical power. Results are displayed in Figure S5.
Comparison With Other COVID‐19 Definitions
We further considered other COVID‐19 definitions (Figure S6 and Table S6). Genetically predicted COVID‐19 requiring hospitalization as compared to not requiring hospitalization was associated with increased risk of any ischemic stroke (OR 1.05, 95% CI 1.01 to 1.10, P‐value=0.01) and small‐vessel stroke (OR 1.22, 95% CI 1.11 to 1.34, P‐value=0.000055). Considering reported COVID‐19 (laboratory confirmed, physician‐reported or self‐reported) versus controls from the general population, this was associated with increased risk of any ischemic stroke (OR 1.13, 95% CI 1.01 to 1.26, P‐value=0.04) and large artery stroke (OR 1.46, 95% CI 1.18 to 1.81, P‐value=0.00042).
Bidirectional MR
There was no strong evidence to support that genetic liability to any of the considered ischemic stroke outcomes was associated with increased risk of critical COVID‐19, as illustrated in Figure 3.
Figure 3. Forest plot of the bidirectional Mendelian randomization analysis illustrating the inverse‐variance weighted Mendelian randomization estimate of liability to stroke phenotypes with critical COVID‐19.

Genetic variants which were associated with the stroke phenotypes were selected as instrumental variables at a P‐value level of 5×10‐6 or smaller. Mendelian randomization estimates represent the odds ratio of critical COVID‐19 per unit increase in the log odds ratio of stroke phenotype. Additional columns include the Mendelian randomization estimate, its 95% CI, the P‐value of the inverse‐variance weighted Mendelian randomization estimate to be different from 1 (P‐val), and heterogeneity measured by the Q‐statistic and the respective heterogeneity P‐value (Het‐P). Exposures included any ischemic stroke, cardioembolic stroke, large artery stroke, and small vessel stroke.
Discussion
In this study, we used cross‐trait LDSC to explore the genetic correlation of critical COVID‐19 with ischemic stroke, other CVD outcomes, and risk factors common to both. We identified a genetic correlation between critical COVID‐19 and ischemic stroke, and performed MR analyses that found genetic liability to critical COVID‐19 to be associated with increased risk of ischemic stroke. Notably, there was no evidence to support that these associations were attributable to shared risk factors, such as obesity, smoking, and chronic inflammation. Furthermore, there was no MR evidence that genetic liability to ischemic stroke increases risk of critical COVID‐19.
When we considered critical COVID‐19 and ischemic stroke subtypes, only cardioembolic stroke remained statistically significant. There are 2 main possible explanations for this observation. The first is that there are pathophysiological differences across stroke subtypes. Indeed, it is conceivable that the host response to critical COVID‐19 may be more likely to culminate in cardioembolic stroke through an acute, pro‐inflammatory, hypercoagulable state that results in cardiac thromboembolism; as opposed to occlusion of small penetrating cerebral arteries and small vessel strokes which are generally a result of more longstanding conditions such as hypertension or diabetes. 41 The second possible explanation is that smaller sample sizes for each stroke subtype compared to any ischemic stroke may mean that we were unable to detect a statistically significance difference in stroke subtypes due to reduced power as shown in Figure S2. This explanation would be supported by similar point estimates to any ischemic stroke across stroke subtypes.
To date, studies assessing the incidence of ischemic stroke during the COVID‐19 pandemic have produced contrasting findings. It has also been uncertain whether any association between COVID‐19 and ischemic stroke is due to a direct effect of SARS‐CoV‐2 viral infection, the host response in COVID‐19, or both. On one hand, some studies demonstrate that the likelihood of stroke is 7‐fold higher in people with COVID‐19 than with influenza, 3 that COVID‐19 is associated with 21‐fold increased odds of in‐hospital stroke compared to patients without COVID‐19, 6 and that stroke is the most common neurological/neuropsychiatric complication of COVID‐19. 4 On the contrary, other studies have demonstrated a reduced rate of hospital admissions with stroke during the first wave of the pandemic compared to one year before. 9 Two main hypotheses have been proposed as explanations for these contrasting findings. The first is that the incidence of stroke declined during the first wave of the pandemic and that COVID‐19 is not mechanistically associated with stroke, and the second is that the observed reduction in stroke presentations was due to a higher proportion of people with mild strokes not reaching stroke services. 11 , 42
We have leveraged large‐scale genetic data to address this and find that liability to critical COVID‐19 is associated with increased risk of ischemic stroke. Moreover, our results are consistent with the hypothesis that it is the host response in COVID‐19 which contributes to increased ischemic stroke risk. However, it is also important to note that our study design cannot directly inform on whether the SARS‐CoV‐2 virus itself also be increases ischemic stroke risk, irrespective of the host inflammatory response. Mechanisms that increase risk of ischemic stroke in patients with COVID‐19 are complex, 5 , 15 and include systemic inflammation and endotheliopathy. 15 , 43 , 44 , 45 COVID‐19 can trigger a cytokine storm with upregulation of pro‐inflammatory cytokines and chemokines such as tumor necrosis factor‐α (TNF‐α), interleukin‐1 (IL‐1) and IL‐615. Endothelial inflammation can induce a microvascular and macrovascular endotheliopathy that contributes to a pro‐thrombotic state. 15 , 43
While prophylactic low molecular weight heparin is used to prevent thromboembolism in patients with COVID‐19, more targeted approaches to prevent strokes are yet undefined. 5 , 46 Moreover, the REMAP‐CAP (A Randomised, Embedded, Multi‐factorial, Adaptive Platform Trial for Community‐Acquired Pneumonia), ACTIV‐4 (Anti‐thrombotics for Adults Hospitalized With COVID‐19), and ATTACC (Antithrombotic Therapy to Ameliorate Complications of COVID‐19) trials have recently reported that therapeutic doses of anticoagulation do not improve clinical outcome and may increase bleeding for people with COVID‐19 in the critical care setting. Previous work using an MR approach anticipated a beneficial effect of IL‐6 receptor inhibition on both risk of ischemic stroke and severe COVID‐19. 47 , 48 More recently, clinical trials have demonstrated that IL‐6 receptor inhibition can improve outcomes in patients hospitalized with COVID‐19. 49 Targeting the deleterious host immune response through similar approaches may also help to reduce the risk of ischemic stroke and should be further evaluated.
Our findings also support the hypothesis that few patients with minor strokes reached stroke services during the first wave of the COVID‐19 pandemic. 11 This is reinforced by data that demonstrate the reduction in stroke admissions observed in some centers during the first wave of the pandemic was driven mainly by a reduction in presentations with minor stroke syndromes. 11 People with minor stroke are at high risk of early recurrence 50 and public health messaging should encourage people to attend stroke services if they have any symptom of stroke during the COVID‐19 pandemic.
We did not observe genetic correlation between critical COVID‐19 and other CVD outcomes such as coronary heart disease, heart failure or atrial fibrillation. Other studies have reported acute coronary syndrome, heart failure, and arrhythmia in people with COVID‐19. 15 There are a number of possible explanations for these findings, which at first may appear discordant. First, myocardial injury and myocarditis may be a more common cardiac manifestation of COVID‐19 than coronary artery plaque rupture and thrombosis. Second, the pulmonary oedema that is observed in people with critical COVID‐19 is usually accompanied by acute respiratory distress syndrome and is mainly regarded as non‐cardiogenic. 15 Third, while arrhythmias are common manifestations of COVID‐19, these may be triggered by acute myocardial injury and systemic factors (such as fever, sepsis, hypoxia, and electrolyte imbalance), rather than atrial fibrillation due to a chronic atrial cardiopathy, which is more likely to make up cases in the pre‐pandemic atrial fibrillation GWAS. 20
Our current study has strengths. We have made efficient use of existing large‐scale data resources to address an important clinical issue in the context of the rapidly evolving global pandemic. A key strength of MR analysis is the use of randomly allocated genetic variants to help overcome environmental confounding, which is analogous to randomization of treatment allocation in clinical trials. This has helped to overcome some of the limitations of previous observational studies (either retrospective or cross‐sectional) assessing the relationship between COVID‐19 and ischemic stroke. 3 , 4 , 5 , 6
Our work also has limitations. A series of modelling assumptions are made when using MR, in particular, that the genetic variants do not affect the considered outcomes through pathways independent of the exposure. While this can never be completely excluded, we employed methods that are robust to genetic confounding (pleiotropy) in a series of sensitivity analyses (including pleiotropy‐robust MR methods and accounting for measured pleiotropy using multivariable MR) and the estimates were consistent with our main analyses. We cannot be certain that genetic associations with liability to critical COVID‐19 accurately reflect the pathophysiological process that actually occurs during critical COVID‐19. For example, while genetic predisposition may place an individual at increased liability to critical COVID‐19, it is not possible to determine from our analyses whether that factor is involved in the pathophysiological response to COVID‐19.
In conclusion, we have found genetic evidence that liability to critical COVID‐19 is associated with increased risk of ischemic stroke. Our results are consistent with the host response in critical COVID‐19 underlying this relationship, and support the evaluation of strategies to mitigate this.
Sources of Funding
VZ is supported by UK Dementia Research Institute at Imperial College London, which is funded by the Medical Research Council, Alzheimer’s Society and Alzheimer’s Research UK (MC_PC_17114). The research leading to these results has been conducted as part of the COVIRNA project (grant agreement n°101016072) funded by the European Union’s Horizon 2020 Framework Programme for Research and Innovation. EPM is supported by the National Institutes of Health of the United States (R01NS103924, U01NS069763). LB acknowledges the MRC grant MR/S02638X/1, The BHF‐Turing Cardiovascular Data Science Awards 2017 and The Alan Turing Institute under the Engineering and Physical Sciences Research Council grant EP/N510129/1. IF‐C is supported by Inmungen‐Cov2 project, Centro Superior de Investigaciones Científicas (CSIC). SB is supported by a Sir Henry Dale Fellowship jointly funded by the Wellcome Trust and the Royal Society (204623/Z/16/Z). This research was supported by the UKRI Medical Research Council [MC_UU_00002/7] and the NIHR Cambridge Biomedical Research Centre (BRC‐1215‐20014). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. CDA is supported by the National Institutes of Health of the United States (R01NS103924, U01NS069763). DG is supported by the British Heart Foundation Centre of Research Excellence at Imperial College London (RE/18/4/34215) and by a National Institute for Health Research Clinical Lectureship at St. George's, University of London (CL‐2020‐16‐001). This research was funded in part by the Wellcome Trust.
Disclosures
CDA receives sponsored research support from the American Heart Association, Massachusetts General Hospital, and Bayer AG, and has consulted for ApoPharma, Inc. DG is employed part‐time by Novo Nordisk. The remaining authors have no disclosures to report.
Supporting information
Table S1–S6
Figure S1–S6
Acknowledgments
This work is dedicated to the memory of Maria Mion who died from COVID‐19 related complications. Leonardo Bottolo is very grateful to the doctors, nurses, and staff of the Ospedale di Oderzo (TV, Italy) for the high standard of care for his mother.
Preprint posted on MedRxiv March 1, 2021. doi: https://doi.org/10.1101/2021.02.25.21252441.
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.022433
For Sources of Funding and Disclosures, see page 8.
References
- 1. Carter P, Anderson M, Mossialos E. Health system, public health, and economic implications of managing COVID‐19 from a cardiovascular perspective. Eur Heart J. 2020;41:2516–2518. doi: 10.1093/eurheartj/ehaa342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani L, et al. COVID‐19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941 [DOI] [PubMed] [Google Scholar]
- 3. Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, Lantos J, Schenck EJ, Goyal P, Bruce SS, et al. Risk of ischemic stroke in patients with Coronavirus Disease 2019 (COVID‐19) vs patients with influenza. JAMA Neurol. 2020;77:1–7. doi: 10.1001/jamaneurol.2020.2730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M, et al. Neurological and neuropsychiatric complications of COVID‐19 in 153 patients: a UK‐wide surveillance study. Lancet Psychiatry. 2020;7:875–882. doi: 10.1016/S2215-0366(20)30287-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Qureshi AI, Abd‐Allah F, Al‐Senani F, Aytac E, Borhani‐Haghighi A, Ciccone A, Gomez CR, Gurkas E, Hsu CY, Jani V, et al. Management of acute ischemic stroke in patients with COVID‐19 infection: report of an international panel. Int J Stroke. 2020;15:540–554. doi: 10.1177/1747493020923234 [DOI] [PubMed] [Google Scholar]
- 6. Katz JM, Libman RB, Wang JJ, Sanelli P, Filippi CG, Gribko M, Pacia SV, Kuzniecky RI, Najjar S, Azhar S. Cerebrovascular complications of COVID‐19. Stroke. 2020;51:e227–e231. doi: 10.1161/STROKEAHA.120.031265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fuentes B, Alonso de Leciñana M, García‐Madrona S, Díaz‐Otero F, Aguirre C, Calleja P, Egido JA, Carneado‐Ruiz J, Ruiz‐Ares G, Rodríguez‐Pardo J, et al. Stroke acute management and outcomes during the COVID‐19 outbreak. Stroke. 2021;52:552–562. doi: 10.1161/STROKEAHA.120.031769 [DOI] [PubMed] [Google Scholar]
- 8. Li Y, Li M, Wang M, Zhou Y, Chang J, Xian Y, Wang D, Mao L, Jin H, Hu B. Acute cerebrovascular disease following COVID‐19: a single center, retrospective, observational study. Stroke Vasc Neurol. 2020;5:279–284. doi: 10.1136/svn-2020-000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sacco S, Ricci S, Ornello R, Eusebi P, Petraglia L, Toni D, Rota E, Bruzzone G, Testa L, Bongioanni R, et al. Reduced admissions for cerebrovascular events during COVID‐19 outbreak in Italy. Stroke. 2020;51:3746–3750. doi: 10.1161/STROKEAHA.120.031293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Qureshi AI, Baskett WI, Huang W, Shyu D, Myers D, Raju M, Lobanova I, Suri MFK, Naqvi SH, French BR, et al. Acute ischemic stroke and COVID‐19: an analysis of 27 676 patients. Stroke. 2021;52:905–912. doi: 10.1161/STROKEAHA.120.031786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Perry R, Banaras A, Werring DJ, Simister R. What has caused the fall in stroke admissions during the COVID‐19 pandemic? J Neurol. 2020;267:3457–3458. doi: 10.1007/s00415-020-10030-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ponsford MJ, Gkatzionis A, Walker VM, Grant AJ, Wootton RE, Moore LSP, Fatumo S, Mason AM, Zuber V, Willer C, et al. Cardiometabolic traits, sepsis, and severe COVID‐19: a Mendelian randomization investigation. Circulation. 2020;142:1791–1793. doi: 10.1161/CIRCULATIONAHA.120.050753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shi K, Wood K, Shi F‐D, Wang X, Liu Q. Stroke‐induced immunosuppression and poststroke infection. Stroke Vasc Neurol. 2018;3:34–41. doi: 10.1136/svn-2017-000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Didelez V, Sheehan N. Mendelian randomization as an instrumental variable approach to causal inference. Stat Methods Med Res. 2007;16:309–330. doi: 10.1177/0962280206077743 [DOI] [PubMed] [Google Scholar]
- 15. Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID‐19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–558. doi: 10.1038/s41569-020-0413-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. COVID‐19 Host Genetics Initiative . A global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS‐CoV‐2 virus pandemic. Eur J Hum Genet. 2020;28:715–718. doi: 10.1038/s41431-020-0636-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. COVID‐19 Host Genetics Initiative . Mapping the human genetic architecture of COVID‐19. Nature. 2021. doi: 10.1038/s41586-021-03767-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Malik R, Chauhan G, Traylor M, Sargurupremraj M, Okada Y, Mishra A, Rutten‐Jacobs L, Giese A‐K, van der Laan SW, Gretarsdottir S, et al. Multiancestry genome‐wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50:524–537. doi: 10.1038/s41588-018-0058-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, Kanoni S, Saleheen D, Kyriakou T, Nelson CP, Hopewell JC, et al. A comprehensive 1000 Genomes–based genome‐wide association meta‐analysis of coronary artery disease. Nat Genet. 2015;47:1121–1130. doi: 10.1038/ng.3396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shah S, Henry A, Roselli C, Lin H, Sveinbjörnsson G, Fatemifar G, Hedman ÅK, Wilk JB, Morley MP, Chaffin MD, et al. Genome‐wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun. 2020;11:163. doi: 10.1038/s41467-019-13690-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Roselli C, Chaffin MD, Weng L‐C, Aeschbacher S, Ahlberg G, Albert CM, Almgren P, Alonso A, Anderson CD, Aragam KG, et al. Multi‐ethnic genome‐wide association study for atrial fibrillation. Nat Genet. 2018;50:1225–1233. doi: 10.1038/s41588-018-0133-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke. 2003;34:2518–2532. doi: 10.1161/01.STR.0000089015.51603.CC [DOI] [PubMed] [Google Scholar]
- 23. Toyoda K, Ninomiya T. Stroke and cerebrovascular diseases in patients with chronic kidney disease. Lancet Neurol. 2014;13:823–833. doi: 10.1016/S1474-4422(14)70026-2 [DOI] [PubMed] [Google Scholar]
- 24. Kernan WN, Inzucchi SE, Sawan C, Macko RF, Furie KL. Obesity: a stubbornly obvious target for stroke prevention. Stroke. 2013;44:278–286. doi: 10.1161/STROKEAHA.111.639922 [DOI] [PubMed] [Google Scholar]
- 25. Wolf PA, D’Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke. The Framingham Study. JAMA. 1988;259:1025–1029. doi: 10.1001/jama.1988.03720070025028 [DOI] [PubMed] [Google Scholar]
- 26. Pulit SL, Stoneman C, Morris AP, Wood AR, Glastonbury CA, Tyrrell J, Yengo L, Ferreira T, Marouli E, Ji Y, et al. Meta‐analysis of genome‐wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum Mol Genet. 2019;28:166–174. doi: 10.1093/hmg/ddy327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wootton RE, Richmond RC, Stuijfzand BG, Lawn RB, Sallis HM, Taylor GMJ, Hemani G, Jones HJ, Zammit S, Davey Smith G, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study. Psychol Med. 2020;50:2435–2443. doi: 10.1017/S0033291719002678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Neale lab . Rapid GWAS of thousands of phenotypes in the UK Biobank 2020. http://www.nealelab.is/uk‐biobank/
- 29. Bulik‐Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR, Duncan L, Perry JRB, Patterson N, Robinson EB, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47:1236–1241. doi: 10.1038/ng.3406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. 2001;29:1165–1188. doi: 10.1214/aos/1013699998 [DOI] [Google Scholar]
- 31. Pierce BL, Burgess S. Efficient design for mendelian randomization studies: subsample and 2‐sample instrumental variable estimators. Am J Epidemiol. 2013;178:1177–1184. doi: 10.1093/aje/kwt084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Del Greco MF, Minelli C, Sheehan NA, Thompson JR. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med. 2015;34:2926–2940. doi: 10.1002/sim.6522 [DOI] [PubMed] [Google Scholar]
- 33. Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–314. doi: 10.1002/gepi.21965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–525. doi: 10.1093/ije/dyv080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bowden J, Smith GD, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–314. doi: 10.1002/gepi.21965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Burgess S, Thompson SG. Multivariable Mendelian randomization: the use of pleiotropic genetic variants to estimate causal effects. Am J Epidemiol. 2015;181:251–260. doi: 10.1093/aje/kwu283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Burgess S, Thompson DJ, Rees JMB, Day FR, Perry JR, Ong KK. Dissecting causal pathways using Mendelian randomization with summarized genetic data: application to age at menarche and risk of breast cancer. Genetics. 2017;207:481–487. doi: 10.1534/genetics.117.300191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Burgess S. Sample size and power calculations in Mendelian randomization with a single instrumental variable and a binary outcome. Int J Epidemiol. 2014;43:922–929. doi: 10.1093/ije/dyu005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Burgess S, Thompson SG, Collaboration CRPCHDG . Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 2011;40:755–764. doi: 10.1093/ije/dyr036 [DOI] [PubMed] [Google Scholar]
- 40. Yavorska OO, Burgess S. MendelianRandomization: an R package for performing Mendelian randomization analyses using summarized data. Int J Epidemiol. 2017;46:1734–1739. doi: 10.1093/ije/dyx034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.STR.24.1.35 [DOI] [PubMed] [Google Scholar]
- 42. Aguiar de Sousa D, Sandset EC, Elkind MSV. The curious case of the missing strokes during the COVID‐19 pandemic. Stroke. 2020;51:1921–1923. doi: 10.1161/STROKEAHA.120.030792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID‐19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lee SG, Fralick M, Sholzberg M. Coagulopathy associated with COVID‐19. Can Med Ass J. 2020;192:E583. doi: 10.1503/cmaj.200685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fauvel C, Weizman O, Trimaille A, Mika D, Pommier T, Pace N, Douair A, Barbin E, Fraix A, Bouchot O, et al. Pulmonary embolism in COVID‐19 patients: a French multicentre cohort study. Eur Heart J. 2020;41:3058–3068. doi: 10.1093/eurheartj/ehaa500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Robinson RG, Bolduc PL, Price TR. Two‐year longitudinal study of poststroke mood disorders: diagnosis and outcome at one and two years. Stroke. 1987;18:837–843. doi: 10.1161/01.STR.18.5.837 [DOI] [PubMed] [Google Scholar]
- 47. Georgakis MK, Malik R, Gill D, Franceschini N, Sudlow CLM, Dichgans M. Interleukin‐6 signaling effects on ischemic stroke and other cardiovascular outcomes: a Mendelian randomization study. Circ Genom Precis Med. 2020;13:e002872. doi: 10.1161/CIRCGEN.119.002872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Larsson S, Burgess S, Gill D. Genetically proxied inhibition of interleukin‐6 signaling: opposing associations with susceptibility to COVID‐19 and pneumonia. Eur Respir J. 2021;57:2003545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Salama C, Han J, Yau L, Reiss WG, Kramer B, Neidhart JD, Criner GJ, Kaplan‐Lewis E, Baden R, Pandit L, et al. Tocilizumab in patients hospitalized with COVID‐19 pneumonia. New Engl J Med. 2021;384:20–30. doi: 10.1056/NEJMoa2030340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Coull AJ, Lovett JK, Rothwell PM. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ. 2004;328:326. doi: 10.1136/bmj.37991.635266.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1–S6
Figure S1–S6


