Abstract
The detrimental influence of parent psychopathology—and depression, in particular—on adolescent mental health has been well documented. Routes of transmission include both direct and indirect factors, such as poor parent–adolescent communication, ineffective parenting practices, modeling ineffective coping skills, increased family discord and stress, inadvertent reinforcement of adolescent depressed mood and suicidal ideation and behavior, and decreased treatment adherence. This paper introduces a novel treatment to concurrently treat both a depressed adolescent as well as a depressed parent. This approach improves upon traditional cognitive-behavioral therapy by targeting relational factors of each adolescent–parent dyad while simultaneously addressing each individual’s depression. Principles of case conceptualization and treatment planning using this novel approach are illustrated using a case example.
Keywords: depression, cognitive-behavioral therapy, CBT, adolescent, parent
The risk of developing depression among children of depressed parents is between two and four times greater than for children whose parents are not depressed (see Goodman, 2007; Hammen, 2009). Offspring of parents who attempt suicide, the majority of whom are depressed, are six times more likely to attempt suicide than the offspring of nonattempters (Brent et al., 2008). Furthermore, parental depression has been found to be one of the best predictors of youth outcome in depression treatment (Brent et al., 1998).
The Sequenced Treatment Alternatives to Relieve Depression (STAR-D; Weissman et al., 2006) study found that when mothers are successfully treated with medication for depression, their children are also less likely to be diagnosed with or show symptoms of depression. Remission of maternal depression after 3 months of medication treatment was significantly associated with reductions in the children’s diagnoses and symptoms. While greater level of maternal response was associated with fewer current diagnoses and symptoms in the children, a maternal response of at least 50% was required to detect an improvement in the child. Garber, Ciesla, McCauley, Diamond, and Schloredt (2011) found a bidirectional relationship between parent and child depression over the course of 2 years. Changes in parents’ depressive symptoms predicted changes in children’s depressive symptoms, over and above the effect of time, and children’s symptoms significantly predicted parents’ symptoms.
The purpose of this paper is to describe a treatment protocol designed to improve response to treatment for adolescent depression by concurrently treating a depressed parent in the same treatment protocol. That is, both a depressed parent and depressed adolescent are treated in the same setting with a comparable protocol by different individual therapists who work together as a team to improve outcomes of the individuals as well as the dyad. We present a case with clinically elevated levels of both depression and suicidality.
Individual Treatments for Adolescent Depression
The two individual psychotherapies with the most support for the treatment of adolescent depression are interpersonal psychotherapy (IPT-A) and cognitive-behavioral therapy (CBT). IPT focuses on the interrelationship between depressive symptoms and interpersonal functioning. IPT-A is an adaptation specifically for depressed adolescents that modifies treatment goals to be developmentally appropriate (e.g., increasing independence; Mufson & Sills, 2006). IPT-A incorporates parents into the adolescent’s treatment to address relational issues, but does not specifically target the parent’s psychopathology. To date, the handful of randomized controlled trials (RCTs) that have examined the efficacy of IPT-A in both clinic samples and school-based clinics have demonstrated a greater reduction in depressive symptoms and greater improvements in interpersonal functioning for youth receiving IPT-A than youth receiving clinical monitoring or treatment as usual (Mufson et al., 2004; Mufson, Weissman, Moreau, & Garfinkel, 1999). Additionally, youth who received IPT-A displayed comparable reductions in depression symptoms as youth who received CBT, with both treatments showing moderate effects compared with a wait-list control condition (Rosselló & Bernal, 1999).
Numerous studies of CBT for youth with depression suggest that it is efficacious. The degree of efficacy, however, has been variable. For example, meta-analyses have identified effect sizes ranging from 1.27 (Lewinsohn & Clarke, 1999) to .53 (Klein, Jacobs, & Reinecke, 2007). Typical CBT protocols involve parents only minimally and if a parent is depressed, referral for treatment is typically the extent to which this problem is addressed. The largest multisite treatment study for depression in adolescents to date is the Treatment for Adolescents With Depression Study (TADS; March et al., 2004). The study had flexible family involvement that included parent psychoeducation about depression and joint goal setting as well as additional family sessions to address identified parent–adolescent concerns. This study compared CBT, fluoxetine, a combination of CBT and fluoxetine, and a medication placebo. At 12 weeks, CBT alone showed a 48% response rate and CBT in combination with fluoxetine showed a 73% response rate; response rates in all three active conditions were comparable at 36 weeks (ranging from 81 to 86%). Another multisite treatment study, the Treatment of SSRI-Resistant Depression in Adolescents (TORDIA; Brent et al., 2008) similarly found that the combination of CBT with a change in SSRI had a higher response rate (54.8%) than the medication-change alone condition (40.5%). In other words, just under half of the participants in the most efficacious condition did not respond to treatment adequately. These studies illustrate that a significant percentage of adolescents, especially those with treatment-resistant depression, do not respond adequately to treatment for depression, and many who do respond continue to have significant symptoms (e.g., Kennard et al., 2008). Innovative approaches to improve response and remission rates are needed.
A few treatment studies have specifically examined the effects of parental depression on depressed youth. Garber et al. (2009) conducted a cognitive-behavioral prevention program for teens with a depressed parent. Teens in the study had a history of depression or sub-syndromal symptoms of depression. Parents met criteria for depression within the past 3 years or had a history of three or more depressive episodes. The intervention provided group cognitive-behavioral sessions for the teens and two general information meetings for the parents. Results indicated that the program had a significant prevention effect based on both clinical diagnoses and self-reported depressive symptoms, but this effect was not evident for adolescents with a currently depressed parent. Notably, this study included minimal parent involvement.
Taken as a whole, these findings indicate a clear need to improve the efficacy of treatment for the significant portion of adolescents whose depression does not remit with current best treatments. Alternative interventions may be particularly needed when the parent has greater symptomatology. Given the strong influence of parental depression on adolescent symptoms, one promising approach may be to treat parental depression in conjunction with the adolescent’s depression treatment.
Developing a Concurrent Treatment for Depressed Teens and Depressed Parents
A number of contextual variables have been found to be related to the transmission of depression from parents to children. Therefore, in developing a concurrent treatment protocol, it is not only important to address the parent’s depression with effective treatment approaches but also how parental psychopathology in general and depression in particular, and specific family characteristics, affect the parent–teen relationship. Parental psychopathology may increase the likelihood of youth depression, as well as suicidal ideation and behavior, through both direct and indirect processes. One direct process is impaired parent–adolescent communication, which may be exacerbated by parental depression (Beardslee, Gladstone, & O’Connor, 2011). Parental depression is also associated with higher levels of expressed emotion, particularly criticism, which may be associated with increased depressive symptoms among children and adolescents (Tompson et al., 2010). A parent’s own emotion regulation can directly affect parent–child interactions. For example, a parent with maladaptive coping skills who is under stress may be more likely to display negative emotionality in parent–child interactions. This, in turn, may provoke more negative reactions from the teen or increase the teen’s stress, creating a cycle of transactional negativity, stress, and emotion dysregulation. Thus, affect regulation for parents is an important skill to address to improve parental mood and reduce adolescent depression.
Conversely, the adolescent’s depression may increase the parent’s level of dysfunction. For instance, it has been suggested that a depressed adolescent’s own depressive symptoms and difficult temperament, in addition to commonly co-occurring and difficult-to-manage risk behaviors (e.g., substance use, risky sexual behavior), may evoke more negative parental reactions (Beardslee et al., 2011) and subsequently less effective parenting practices, than an adolescent with an easier disposition. These findings suggest that an effective intervention for adolescent depression should address parent–teen relationship quality through techniques that enhance communication and parenting skills. This approach may improve treatment efficacy and reduce symptoms of depression by two means: improving parental communication, which in turn may improve teen affect; and decreasing provocative adolescent behavior, which in turn may improve parental affect. The reciprocal effects of improving each individual’s mood and ability to effectively communicate with the other would appear to have the potential for better overall outcomes than separate treatments.
Parental psychopathology may also influence an adolescent’s development of depression through indirect transmission, as in behavioral modeling. A parent with depression may use (and therefore model) ineffective coping skills, including a depressogenic cognitive style or ineffective problem solving. Given that suicidal behavior among depressed youth may be related to poor problem-solving ability (Adams & Adams, 1996), modeling of this behavior may be particularly deleterious for a teen with already underdeveloped problem-solving skills. All of these behaviors—coping skills, cognitive distortions, and problem solving—are targets of intervention for any depressed individual, adult or adolescent.
Broader family characteristics may also play an important role in an adolescent’s development of depression. For example, high levels of discord and stress in the parent’s life, such as employment, marital, or housing difficulties, may indirectly affect the adolescent’s stress and functioning. It has been found that individuals with depression are not only exposed to more stressful life events beyond their control (i.e., independent stressful life events), such as the death of a loved one, but also experience higher rates of stressful life events in which they play a causal role (i.e., dependent stressful life events), for example, termination from employment due to absenteeism (Hammen, 2006). Increased rates of stressful life events may impact not only the parent’s level of stress but also overall family functioning and a child’s level of stress. Thus, parental stress-management skills (including problem solving and affect regulation) may affect an adolescent’s response to treatment. If depressed parents and depressed teens are treated concurrently, this issue may be more closely monitored and more effectively addressed.
Finally, a parent’s response to a depressed adolescent who is also suicidal may inadvertently reinforce the behavior (Wagner, Silverman, & Martin, 2003). Increased positive attention, such as more frequent displays of affection, and decreased demands (e.g., relief from chores or permitted absenteeism from school) act as rewards for suicidal behavior and may result in increasing the maladaptive behavior rather than reducing it. Similarly, depressed teens often demonstrate challenging risk behavior that parents struggle to manage. Parents of depressed teens would therefore benefit from psychoeducation on principles of behavior management to understand and recognize problem behavior in their depressed teens as well as training in effective parenting skills to address the maladaptive behaviors.
In summary, although the influence of parental depression on youth depression is strongly supported by research, parental depression has not been a primary target of empirically supported interventions for adolescent depression. In fact, most treatment protocols prescribe parents a minimal role, if any, in the adolescent’s treatment. Although it is common clinical practice to refer parents to individual treatment for their own depression, follow-up on whether these services have been attained is typically limited. Despite this, there is evidence (e.g., in STAR-D; Weissman et al., 2006) that the treatment of maternal depression alone can reduce adolescent depression without direct treatment of the adolescent’s symptoms. Although it is unclear to which parental factors this is attributable, it is evidence that treatment of parental depression is a clear target for intervention that can improve adolescent functioning. Another advantage of a concurrent treatment approach is its potential to increase treatment adherence. Treatment that requires parental participation, therefore, may be more likely to improve the adolescent’s outcome by increasing attendance alone.
Despite the inherent clinical logic underlying the notion of treating a depressed parent at the same time as a depressed teen, protocols addressing both adolescent and parent depression have yet to be tested empirically. The current paper presents the development of a CBT protocol to concurrently treat adolescents who are depressed and a depressed parent. In addition to addressing the common barriers to treatment described above (e.g., attendance, parent psychopathology), the current design facilitates treatment by (a) coordinating adolescent and parent treatment goals; (b) integrating treatment to ensure that adolescents and parents have the opportunity to practice skills in communication, problem-solving, and affect regulation; and (c) providing support and skills to parents relevant to parenting a challenging adolescent, and tailoring this support to the parents’ current level of functioning and skill development.
Method
Participants
The case presented here was selected from a small pilot RCT designed to test the feasibility and acceptability of the concurrent treatment protocol (Spirito et al., 2015). This case was selected to illustrate the rationale for this novel treatment approach and exemplify the relationship between parent’s and adolescent’s symptoms of depression and response to specific intervention strategies regarding the parent–adolescent relationship over the course of treatment. In addition, because suicidality is frequently encountered in moderate to severely depressed adolescents, this case also illustrates how suicidality is addressed in the protocol.
For the RCT, participants (13- to 18-year-olds living at home with a parent) were recruited from the adolescent unit of a psychiatric hospital in the Northeastern United States. Interested families were scheduled for diagnostic assessments to determine eligibility. Because the focus of treatment was teens with more severe cases of depression, teens not only had to meet diagnostic criteria for major depressive disorder (MDD) but also report current suicidal ideation or a history of a suicide attempt. One parent had to endorse a current or past MDD episode and had a minimum score of 15 on the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996). Parents and teens were excluded if they met criteria for bipolar disorder, substance use disorder, or psychosis. Details about the RCT can be seen in Spirito et al. (2015).
Measures
Adolescent and parent depression diagnoses were assessed via semistructured interviews administered by trained clinicians. Severity of depression, suicidality, and potential mechanisms of action were assessed using self-report measures completed by both adolescents and parents. The diagnostic interviews and self-report measures were administered at pretreatment, posttreatment, and 6-months posttreatment. In addition, select measures were administered at weekly therapy appointments to track changes in severity of depression and suicidality over the course of treatment.
Adolescent Depression Diagnoses
Adolescent depression was determined using the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL; Kaufman, Birmaher, Brent, & Rao, 1997). The K-SADS-PL is a semistructured diagnostic interview that provides an assessment of DSM-IV psychopathology in children and adolescents. Interrater agreement on screens and diagnoses is high (range: 93–100%). Test–retest reliability and kappa coefficients are in the excellent range for present and lifetime diagnoses of major depressive, any bipolar, generalized anxiety, conduct, and oppositional defiant disorders (.77–1.00; Kaufman et al., 1997). The K-SADS was administered to adolescents to determine eligibility for the current study.
Parental Depression Diagnoses
Parental depression was diagnosed using the Structured Clinical Interview for DSM-IV-TR–Clinical Trials Version (SCID-CT; First, Williams, Spitzer, & Gibbon, 2007). The SCID-CT is a semistructured interview used to diagnose major Axis I disorders according to DSM-IV-TR criteria. The Psychotic, Bipolar, and Substance Abuse modules were also administered to rule out anyone with current psychotic symptoms, bipolar disorder, or alcohol/drug dependence, as specified in the exclusion criteria.
Depression Severity
Severity of depression was evaluated at the major assessment points using the Beck Depression Inventory (BDI-II; Beck et al., 1996). The BDI-II is a 21-item inventory used to assess affective, cognitive, motivational, vegetative, and psychosomatic aspects of depression. Severity of each item is rated on a scale ranging from 0 to 3. Several studies have demonstrated the applicability of the BDI with adolescents (Kashani, Sherman, Parker, & Reid, 1990; Steer, Clark, Beck, & Ranieri, 1995; Strober, Green, & Carlson, 1981) as well as adults. This scale was administered to both parents and adolescents.
Weekly Symptom Ratings
Indicators of depression and suicidality were also tracked at weekly appointments. Symptoms of depression and suicidality were tracked weekly using the Quick Inventory of Depressive Symptoms (QIDS; Rush et al., 2003) and the Beck Scale for Suicidal Ideation (BSS; Beck & Steer, 1991), respectively. The QIDS is a 16-item self-report inventory of depressive symptoms that corresponds to the nine symptom domains of a major depressive episode as defined in the DSM-IV. The BSS is a 21-item self-report instrument designed to measure severity of suicidal ideation experienced over the prior week. Higher scores on both scales indicate higher levels of severity.
Mechanisms Hypothesized to Affect Treatment Response
The Conflict Behavior Questionnaire (CBQ; Robin & Foster, 1989) was used to assess parental and adolescent perception of family conflict and communication. A total summary score was computed from the 20-item short form. The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) was used to assess parents’ self-reported ability to modulate emotional responses. The DERS comprises 36 items, rated on a Likert scale from 1 (almost never) to 5 (almost always).
Concurrent CBT Protocol
The concurrent CBT protocol for adolescent and parent depression is a 24-week intervention, consisting of an acute phase (weekly appointments for the first 12 weeks) and a maintenance phase (appointments every two weeks for the second 12 weeks). The parent and teen are each assigned their own therapist and treatment includes individual sessions for parents and adolescents as well as joint parent–teen sessions. At the start of therapy, adolescent sessions are typically 60 minutes, while parent sessions are 90 minutes. The longer length of parent sessions is designed to allot sufficient time to provide individual treatment targeting parent depression, as well as to address parenting practices and ways in which to support their teen’s treatment. Each session has common structural elements typical of many adolescent CBT protocols, such as those used in TADS and TORDIA, including (a) setting an agenda, (b) reviewing homework from the prior session, (c) skill review or teaching of a new skill, (d) skill practice, and (e) addressing any patient–generated agenda items using CBT skills. Worksheets and handouts for each CBT skill are used to assist in the learning process. All individual sessions conclude with a brief conjoint meeting with the parent, adolescent, and both therapists. This check-in includes an exchange of positive comments to enhance positive communication between the parent and teen and a review of the skills learned. Finally, the parent and adolescent are assigned a personalized “homework” assignment at the end of each session to facilitate practice of a particular CBT skill.
Skills in the CBT protocol encompass behavioral, cognitive, and affective components of functioning (see Table 1). The behavioral component emphasizes various skill deficits in the domains of interpersonal relationships and participation in pleasant activities. The cognitive component focuses on problem solving and identifying and challenging negative automatic thoughts, while the affective component teaches skills to cope with intense emotions and reduce impulsive behavior. The protocol proceeds in a modular fashion, such that each dyad receives a set of core foundational skill sessions at the start of treatment (problem solving, behavioral activation, cognitive restructuring, and affect regulation). Several core parent–teen modules (family problem solving, social support, and family communication) are specifically designed as conjoint 60- to 90-minute sessions to directly target the common relational difficulties of parent–adolescent dyads. The therapist then selects which core skills are reinforced in later sessions in the protocol based on the specific presenting problems of a family.
Table 1.
Description of Session Content
| Name of Session | Type of Session |
Objective |
|---|---|---|
| Introduction to treatment | Conjoint | Orient to treatment program and conduct safety planning; safety planning also involves identifying a plan for parenting support. |
| Behavioral activation | Individual, conjoint | Decrease sedentary behavior and increase the frequency of healthy pleasant activities for the individual; plan conjoint activity to improve parent–teen relationship. |
| Problem solving | Individual, conjoint | Learn how to generate and evaluate options to problems, and identify the most effective solution. When this is conducted as conjoint problem solving, the dyad also works on perspective taking. |
| Cognitive restructuring | Individual | Become aware of the link between thoughts and feelings, and identify thinking mistakes that contribute to negative emotions and behaviors that apply to the individual and parenting practices. |
| Affect regulation | Individual | Become aware of triggers and signs (physiological, cognitive, and behavioral) of affect arousal and develop coping plan that applies to the individual and parenting practices. |
| Relaxation | Individual | Decrease stress through the use of deep breathing, muscle relaxation, and the use of imagination. |
| Chain analysis | Individual, conjoint | Identify and address the sequence of thoughts, feelings, and behaviors that culminate in risky behaviors and poor parenting. |
| Distress tolerance | Individual | Develop safe, effective coping skills to help tolerate situations that trigger significant negative emotions. |
| Increasing social support | Individual, conjoint | Identify supporters, learn how to increase support from current support system, and add new supporters. |
| Crisis management and planning for emergencies | Individual | Identify situations that place teen at risk for making poor decisions and develop a coping plan. |
| Parental monitoring | Parent | Teach how to monitor teen behaviors, activities, and friends to help teen avoid risky situations and dangerous moods and behaviors. |
| Contingency management | Parent, conjoint | Identify appropriate limits and set up rewards and consequences to help change teen behavior. |
| Family communication | Conjoint | Learn and practice positive communication skills. |
| Relapse prevention | Individual, conjoint | Review treatment progress, recommendations, and prevention plan, and conclude treatment. |
Core skill sessions can be supplemented by a number of optional individual and conjoint parent–adolescent sessions that can be selected based on each dyad’s specific concerns. Individual modules that can be selected for either the parent and/or the adolescent include chain analysis of problem behaviors, distress tolerance, and relaxation. As additional parenting support is often indicated, sessions to address parenting skills are included. Therapists are able to choose appropriate skill topics to match the specific needs of individual families. For example, contingency management was included in cases where a teen’s behavior was challenging but it was not necessary if the teen’s behavior was not a primary focus of concern. On any given weekly visit, either an individual or conjoint session is conducted such that the weekly time commitment never exceeds 90 minutes. Finally, all dyads receive a relapse prevention session at the end of treatment to identify early warning signs of relapse and develop a concrete coping plan.
A total of 337 sessions were conducted in this treatment trial (Spirito et al., 2015). A total of 33% of sessions were conducted primarily with the adolescent (with a parent check-in at the end of session); 33% were conducted primarily with the parent; 15% were conducted as conjoint sessions; and 19% were conducted half individually and half conjointly. The most frequently used modules were individual or family problem solving (25% of all sessions), behavioral activation (12%), affect regulation (11%), family communication (9%), social support (7%), and contingency management or parental monitoring (5%).
Case Example
Baseline Demographic and Clinical Characteristics
Lynn was a 34-year-old Latina mother who was seeking treatment for herself and her daughter, Sophia (age 14, Latina). Lynn and Sophia’s biological father had never been married, and Sophia did not have any contact with him. Lynn and Sophia lived with Lynn’s current husband, whom she described as supportive, and three other children: a 20-year-old stepsister, a 13-year-old half-brother, and a 5-year-old half-sister. Lynn reported a long history of depression, anxiety, and panic attacks. She had never previously received therapy. Lynn reported ongoing suicidal ideation, but denied prior or current suicidal intent or plans. She had no history of psychiatric hospitalizations, substance abuse, or mania. She had medical diagnoses of diabetes and sleep apnea. Lynn completed some college and was a stay-at-home mom. When asked why she was seeking treatment, Lynn stated that she cried a lot and feared it was affecting her children; she reported chronic feelings of guilt, worthlessness, and fatigue, and described herself as a “bad mother.” At baseline, BDI and BSS scores indicated that Lynn’s depression was in the severe range and that she had a mild level of suicidality (see Figures 1 and 2). On the BSS, specific items endorsed included “a weak wish to die” and “reasons for dying outweigh her reasons for living.”
Figure 1.
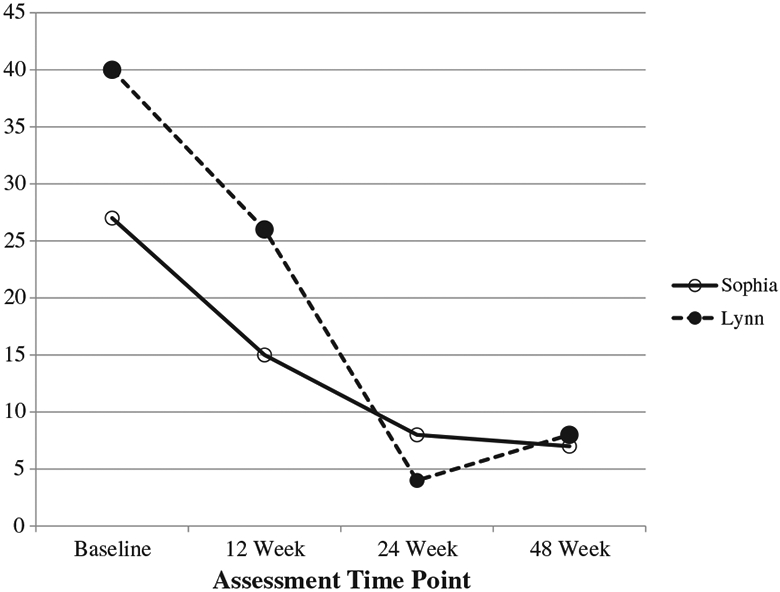
Parent and child Beck Depression Inventory scores at baseline and Weeks 12, 24, and 48.
Figure 2.
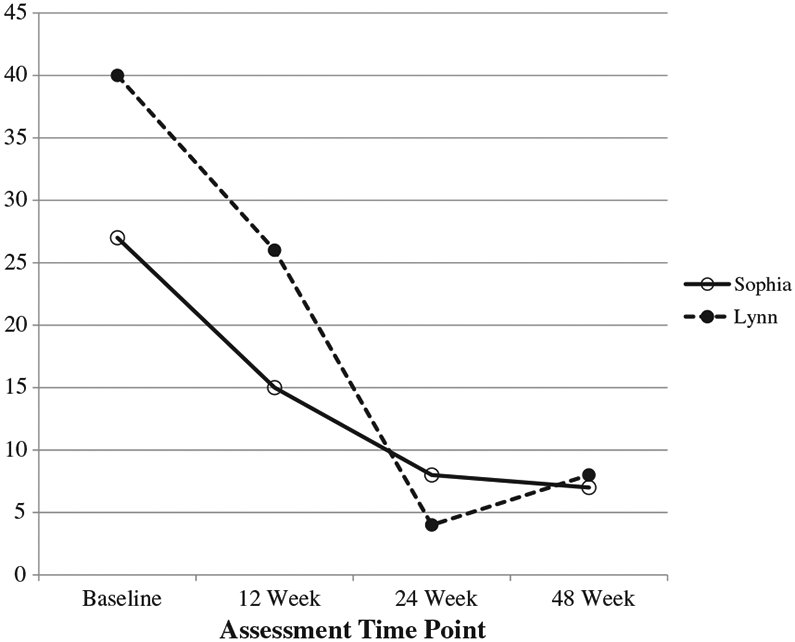
Parent and child Beck Scale for Suicidal Ideation scores at baseline, end of acute treatment, end of maintenance treatment, 6-month follow-up.
Sophia also reported a relatively long history of depression, as well as symptoms of attention-deficit/hyperactivity disorder (ADHD) and social anxiety disorder. Similar to her mother, she had never previously received therapy. She had engaged in nonsuicidal self–injurious behavior on two previous occasions, including one episode after she threatened to run away following an argument with her mother. Following this incident, Lynn took her daughter to the hospital where Sophia reported suicidal ideation and was hospitalized in an inpatient psychiatric facility for 1 day. At intake, Sophia was not taking any prescribed medications. In the months before treatment, her school grades had dropped and she reported difficulty concentrating. It is also important to note that Sophia was reportedly molested at a young age. Lynn indicated that, largely because of this incident, she tended to be overprotective of her daughter. Both mother and daughter reported that their relationship was highly conflictual and that they were reactive to each other’s moods and behaviors. At baseline, Sophia’s depression was in the moderate range on the BDI and she reported a moderate level of suicidality on the BSS (see Figures 1 and 2). Specific items that she endorsed on the suicidality scale included “having a weak wish to live,” “equal reasons for living and dying,” “thinking about writing a suicide note,” and “wanting to commit suicide to escape from (her) problems.”
Case Conceptualization: Lynn’s Depression
Consistent with the CBT model proposed here, Lynn reported that she frequently had negative thoughts related to parenting self-efficacy such as “I am an inadequate mother.” Two primary behavioral triggers were difficulty setting age-appropriate limits for Sophia due to concerns related to Lynn’s own struggles with mood, and difficulty controlling her temper when Sophia verbally challenged Lynn’s parenting. Lynn often asked her mother and sister for advice on how to parent Sophia, but reported feeling criticized by her extended family for her parenting skills. Lynn also identified feelings of anxiety as a trigger for her depressed mood, as well as a barrier to engaging in positive activities leading to social isolation and low positive engagement with her daughter.
Case Conceptualization: Sophia’s Depression
Sophia described her primary mood triggers as related to interpersonal situations and perceived rejection by peers and romantic interests. Specifically, she reported feeling very depressed and suicidal when “people talk about me or ignore me,” “someone doesn’t want to go out with me anymore,” “people put me down,” and “people don’t trust me.” She also reported triggers related to feelings of guilt, worthlessness, and regret when reprimanded by her mother and in response to her poor academic performance.
Case Conceptualization: Cycle of Maternal–Child Depression
The depressive symptoms experienced by both mother and adolescent provided significant challenges in their relationship and exacerbated each other’s depressed moods. Due to their depression, Sophia and Lynn both engaged in isolative behavior resulting in few opportunities for positive interactions. In addition, Sophia often demonstrated increased irritable and disrespectful behavior toward her mother when she was feeling depressed (e.g., about poor school performance). Lynn, on the other hand, often felt responsible and guilty for Sophia’s challenges and bewildered about how to help her daughter. As described above, this triggered negative cognitions about her parenting ability and led to worsening anxiety and depressive symptoms. Furthermore, these feelings of guilt and helplessness often interfered with consistent limit setting; her limits were often reactive to Sophia’s behavioral and emotional outbursts. She only rarely instituted limits for everyday, typical misbehavior, such as curfew violations. In addition, consequences were often overly punitive and/or difficult to enforce and communicated in a harsh and critical tone. Mother and daughter interactions and communications increasingly revolved around negative circumstances and their own conflict. Following these interactions, both mother and daughter would experience increased depressive symptoms and, occasionally, increases in suicidal ideation.
Course of Treatment
The parent and child attended 16 sessions over a period of 6 months (weekly for first 12 weeks and then tapered to every other week; two scheduled appointments were not attended). The therapists for the mother and daughter were both doctoral-level clinical psychologists. Session 1 began with rapport building with the adolescent and parent independently, followed by a conjoint parent–adolescent meeting that included an introduction to the treatment process, session adherence enhancement procedures, and goal setting. Psychoeducation regarding the CBT model on the relationship between thoughts, feelings, and behavior and the relationship between parent and adolescent depression was presented and discussed. Mother and teen each identified a list of reasons for living and established individual treatment goals. Sophia established primary goals of improving her mood, reducing conflict and yelling at home, improving friendships, and paying attention in classes. Lynn indicated she wanted to be a better wife and mother, reduce her guilt related to parenting, and participate in more parent–teen activities. Safety plans were then developed in the event of increased suicidality or severe mood or behavioral dysregulation. Because the protocol is specifically designed for parents who are coping with their own depressed mood, the therapist incorporated alternative supportive adults, besides Sophia’s mother, into the safety plans to ensure that the adolescent would be adequately supported in safety situations. Sophia identified her stepfather as an alternative adult support.
In Session 2, behavioral activation was used to increase engagement in pleasant activities both individually (e.g., listening to music, spending time with friends) and conjointly (i.e., scheduling family time). Lynn initially voiced concerns that her depression and anxiety often prevented her from engaging in these activities and she feared that she would have a panic attack if she engaged in activities outside of the home. However, when the therapists presented the idea of doing activities together and pointed out that these activities were also important for Sophia, Lynn agreed to give them a try. Lynn and Sophia both remarked that the most useful part of this session was scheduling these joint activities to improve their motivation and provide opportunities to improve their relationship.
In Session 3, a problem-solving skill exercise was used to effectively generate and evaluate options in response to triggers for depression and suicidality. During this particular week, Sophia reported an increase in her depression and suicidality in response to breaking up with her boyfriend (see Week 3, Figures 3 and 4). The problem-solving skill was used to help Sophia think through various options in response to the situation. She considered apologizing to him, talking to him, and dating other people. She decided to try talking to her boyfriend and reported that she felt better recognizing that she had some options in the situation. Lynn had identified her own anxiety and her daughter’s depression as barriers to effective parenting and limit setting. Thus, the problem-solving skill was used to help her generate alternative and more effective parenting practices.
Figure 3.
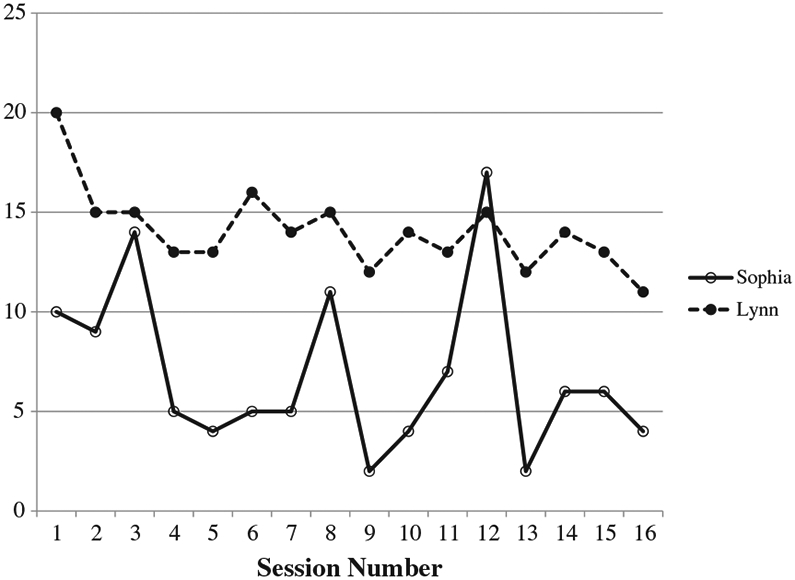
Parent and child depression scores at each session over the course of 6 months.
Figure 4.
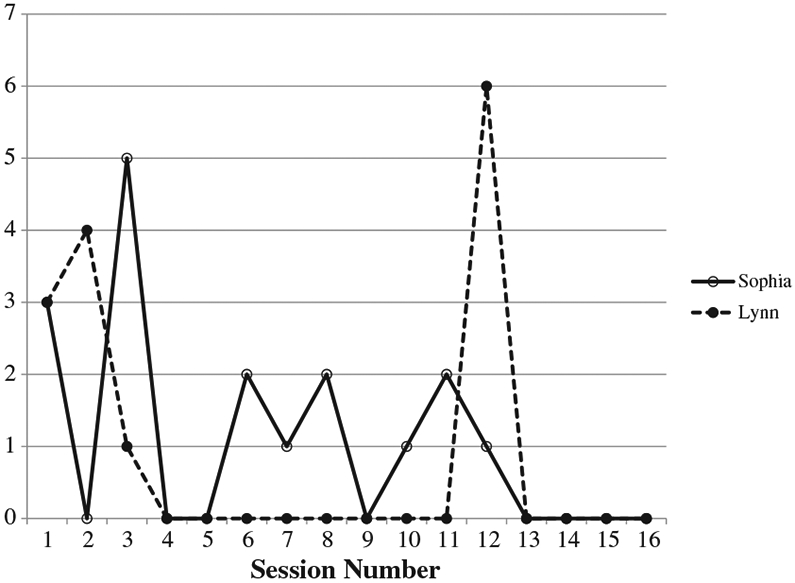
Parent and child weekly suicidality scores at each session over the course of 6 months.
Presented in session 4, the cognitive restructuring skill is designed to help parents and adolescents recognize common thinking mistakes, identify their negative or “hot” cognitions associated with a specific situation, and generate more helpful thoughts. Lynn described her mood triggers as thoughts related to poor parenting self-efficacy (e.g., “I am an inadequate mother”). She also stated that her daughter’s own mental health problems contributed to these thoughts and, in turn, her difficulty implementing appropriate consequences to avoid compounding her daughter’s depression. As part of her coping thoughts, Lynn reflected on the positive changes she was making through treatment including using more effective discipline techniques and spending more time with her daughter. She recalled several recent positive conversations she had with her daughter as evidence that her parenting was improving. Sophia applied the cognitive restructuring skill to core negative beliefs related to discord in her romantic relationships (e.g., “I’m all alone,” “No one cares about me”) and her poor academic performance (e.g., “I’m stupid,” “I’m lazy”).
In Session 5, mother reported that she discovered teen’s intent to text inappropriate photos of herself to a male peer, and became so upset that she hit Sophia on the arm and told her she couldn’t forgive her. Hitting was not a typical parental response in this family, no marks were observed or reported to the clinicians, and Sophia did not report the action hurt her. The therapists cautioned Lynn about their duty to report more serious incidents of physical abuse if they were to occur, but did not report this incident to protective services. Sophia reported a subsequent increase in depressive symptoms (“I feel like a disgrace”; see Figures 3 and 4, Week 8). Using an affect regulation skill, Lynn was able to identify her own emotional reactions as a barrier to effective communication and parenting. Additionally, this skill was applied to the ongoing parent–teen conflicts over Sophia’s use of social media and electronics. Mother and daughter further used this skill to identify times they were becoming angry at each other and times that they should take space from each other or use other coping skills.
Throughout therapy, Lynn and Sophia communicated about fluctuations in their moods. During parent and teen check-ins, both mother and daughter were encouraged to talk about aspects of their relationship that influenced these factors. Family communication skills, taught in Sessions 6 and 7, were central to reestablishing positive communication, particularly following the event when mother hit her daughter (described above). During these conjoint sessions the parent and teen practiced listening and responding to each other’s concerns and making amends with regard to recent conflicts. Mother specifically communicated her concerns about who the teen was dating and the teen communicated her concerns about being judged or rejected by her mother. These sessions served to decrease sarcasm, communicate genuine praise, and improve the parent–teen relationship.
Sessions 8 and 9 were used to review cognitive restructuring and improve affect regulation skills. Lynn and Sophia learned relaxation strategies, including deep breathing, progressive muscle relaxation, and visualization. After practicing these skills, both reported less difficulty falling asleep.
In Session 10, family problem solving and contingency management principles were used to manage parent–teen conflict over using social media and dating. Lynn indicated that her discipline tended to be inconsistent, in part, due to concerns about her daughter’s fluctuations in mood. For example, Lynn worried that dating would ultimately lead to Sophia feeling rejected so Lynn enacted harsh restrictions that limited all social contact. When these restrictions increased conflict and had a deleterious effect on Lynn’s and Sophia’s moods, Lynn would remove these restrictions altogether. In this session, mother and teen worked together to discuss house rules. These skills helped Lynn establish and enforce consistent rules for dating and phone and computer usage. Mother and daughter indicated that this process decreased reoccurring conflicts, increased self-efficacy related to parenting, and decreased parenting stress.
Session 11 focused on increasing social support. The family discussed ways to obtain social support from one another when upset and ways in which mother could support teen in improving her academic performance. Following an incident in which Lynn restricted Sophia’s access to a social media site and set appropriate limits on her daughter’s current romantic relationship with an older man, Sophia reported increased depressive symptoms, while her mother had a sharp rise in suicidal ideation (see Figures 3 and 4, Week 12). Mother and daughter were able to let each other know that they were struggling with their moods and needed support from each other and their extended family. Although Lynn had a rise in suicidal ideation, she did not endorse a plan or intent. Her safety plan was reviewed and the need for support from other adults was reiterated. Although Lynn talked openly about her emotions and expressed, in general terms, that the situation made her “want to escape,” she did not share her suicidal thoughts with her daughter because the protocol emphasizes teens asking for support from adults around safety issues rather than parents seeking support from teens. It should be noted that if Lynn’s ideation had increased (i.e., to a suicidal plan or intent), the need for hospitalization and stabilization would have been discussed with Sophia in terms of her mother taking the necessary steps to ensure her safety. Lynn was also encouraged to seek parenting support from her husband and family members as a way to improve her mood. For Sophia, this skill was used to identify alternative methods of social contact and strategies to proactively obtain social support from prosocial peers. Distress tolerance skills were also emphasized in Sophia’s individual session to promote positive coping.
In the maintenance phase of treatment (Sessions 13–16), mother and daughter continued to apply skills to improve their moods, and Lynn continued to work on applying these skills to parenting. For example, Sophia continued to apply the problem-solving skill to her primary mood triggers of romantic relationships and conflicts with peers. In addition, family problem solving was utilized to address Sophia’s poor academic performance. Specifically, Lynn and Sophia generated options regarding actions Sophia could take to improve her grades and ways in which Lynn could help support these efforts and advocate for her daughter (e.g., communicating with school staff).
Over the course of the parent’s and teen’s treatment, 43% of sessions were conducted individually, 25% were conducted conjointly, and the remainder were half and half. The most frequently used session was problem solving, which was conducted a total of five times comprising 31% of all of their sessions. Half of these problem-solving sessions were conducted individually and half were conducted conjointly. The decision to conduct these sessions individually or conjointly was based on Lynn’s and Sophia’s levels of affective arousal at the time of sessions and willingness to discuss issues together. For example, during times that Lynn was frustrated with Sophia’s behaviors, sessions began individually to help Lynn apply affect management skills so she could more effectively communicate with her daughter and problem solve potential solutions to the problems at hand.
End of Treatment and 6-Month Follow-Up
Depression and Suicidality
Levels of depression and suicidality had decreased for both Lynn and Sophia by the end of treatment (see Figures 1 and 2). Specifically, at the conclusion of treatment, Lynn’s and Sophia’s depressive symptoms were in the mild range on the BDI and remained low at the 6-month follow-up assessment. Both denied suicidal thoughts and behaviors at the end of treatment. At 6-month follow-up, Lynn’s suicidality score was 1, while Sophia’s remained at 0. In the exit interview, the parent and teen indicated that their communication and interactions were greatly improved so they were better able to support each other rather than exacerbating each other’s moods.
Mechanisms of Change
Parental emotion regulation and family conflict were examined as potential mechanisms of change. At baseline, Lynn (mother) reported clinically significant challenges with emotion regulation as assessed by the DERS (sample item: “When I’m upset, I become out of control”; score of 136). Scores at end of treatment (54) and 6-month follow-up (64) indicated clinically significant improvement (with scores no longer in the clinical range: <98). Family conflict demonstrated similar improvement, as assessed via both parent and teen report of the CBQ (sample items: “We almost never seem to agree,” “My mom puts me down”). Lynn and Sophia both reported significant family conflict at baseline (scores of 14 and 8, respectively) with improvements by the end of treatment (scores of 2 and 1, respectively) that were maintained at follow-up (scores of 4 and 2, respectively). These scores demonstrate a decrease from the clinical to the nonclinical range (≥10 for parent report and >8 for adolescent report) over the course of treatment.
Discussion
This paper presents a case example demonstrating a novel treatment for a depressed adolescent and her depressed parent. The case of Lynn and Sophia illustrates the value of coordinated treatment and the process of treating parents and teens concurrently. Parents and teens are explicitly made aware of how their behavior affects each other and how they can use the skills they develop in each session to support each other as well as their own therapeutic goals.
A concurrent treatment protocol for parents and adolescents may also enhance treatment adherence thereby improving overall treatment efficacy. Aspects of treatment adherence that may be facilitated include increased attendance due to fewer appointment and transportation demands; coordination of treatment, which may increase confidence in treatment outcomes; and improved parenting interventions because appropriate modifications can be made based on a thorough understanding of the parent’s level of functioning at the time. In the larger study from which this case was selected, there were several cases that illustrated increased attendance following the encouragement of one member of the dyad to the other to attend (or return if a session was missed).
This case illustrates common deficits in communication and problem solving characteristic of depressed parent–teen dyads. These deficits were particularly pronounced in family conflict about Sophia’s dating as well as phone and computer use. By coordinating acquisition of specific skills in family communication and family problem solving, the dyad was able to build a common language to help reduce discord and stress between them and reduce the latency to a return to positive emotions following an argument. As the pair developed greater mastery of these skills, they were able to generate more effective solutions to their conflicts. In addition, over time, family conflicts appeared to have less of an effect on Lynn’s and Sophia’s experience of individual depressive symptoms (e.g., hopelessness, irritability).
Coordination of treatment also increases the amount of support that the parent and adolescent provide each other to practice their skills more frequently. This process may be present to a lesser degree in traditional CBT for adolescents, as adolescent treatment often includes occasional parent sessions. However, the extent of each party’s understanding of CBT skills, and the relevance of these skills to their own treatment success in the concurrent treatment model, may facilitate greater overall commitment to the treatment and greater opportunities for skill generalization. Lynn and Sophia demonstrated this when they coordinated their practice of behavioral activation by scheduling activities together. This coordination had the added benefit of increasing positive family interactions, which helped to strengthen their relationship.
The current case also illustrates the importance of developing effective parenting practices to benefit the adolescent and parent. It is important to consider the parent’s current level of functioning to individually tailor an effective parent intervention. By attending to both the parent’s individual treatment goals and parenting practices, the current treatment is designed to help the parent set appropriate expectations and select the skills that are most likely to be used and succeed. In this way, the clinician can scaffold the learning process by gradually introducing important skills later in treatment that may be too difficult for the parent to implement initially.
In the current case, Lynn had difficulty enforcing limits with Sophia early in treatment; her parenting efficacy was low and she feared limit setting would compound Sophia’s depression. When Sophia’s high-risk behavior on social media compelled Lynn to respond, the restrictions placed on Sophia’s use were often inconsistent, poorly enforced, and/or overly restrictive. In addition, parent–teen communication surrounding these conflicts was highly negative and critical. As predicted, both Sophia’s and Lynn’s depressive symptoms increased following these limit-setting attempts, and Lynn experienced increased suicidality in response to her daughter’s increased depression and misbehavior. The structure of the concurrent protocol, designed to coordinate treatment according to the needs of the dyad, enabled Lynn to use problem-solving and contingency management skills to implement reasonable house rules. Although this worsened Sophia’s negative mood initially, the improved consistency, structure, and reasonableness decreased the tumult and increased the predictability of her mother’s responses, which ultimately appeared to reduce triggers for depression. Treatment also targeted Lynn’s negative cognitions about her parenting, building her sense of self-efficacy. As a result of this, Lynn no longer responded to her daughter’s reaction to limits by becoming suicidal, which directly influenced Lynn’s functioning and provided appropriate modeling of more effective coping skills for Sophia.
Conclusion
The case presented here illustrates how the concurrent treatment of depression and suicidality for adolescents and their parents can improve upon individual treatment for either party alone. If this protocol is found to be effective in a fully powered clinical trial, then examination of whether the protocol affects the hypothesized mechanisms of action (i.e., family conflict and communication as well as parental distress tolerance) will be important. Determining whether certain skills are associated with better outcomes will also be important. For example, the conjoint sessions (i.e., family problem solving and family communication) were described as particularly useful by most parents in the clinical trial and the parent in this case example.
There are some cautionary factors that need to be considered when recommending this treatment approach. The families that agreed to participate were willing to be treated conjointly. There were some families that were approached and refused enrollment because they did not feel this approach was right for a parent, an adolescent, or both. Some adolescents in the study did not like the conjoint sessions or receiving treatment at the same time as a parent. Although any disclosure of material by the teen’s therapist was discussed and approved prior to any parent–teen sessions, some teens were concerned about confidentiality if a parent was very involved in their treatments. Other teens did not want to hear about their parent’s depressed mood or stressors in their parent’s life. Thus, like any treatment approach, it will be important to determine for whom this approach is best suited versus who will do better in traditional, nonconjoint, individual CBT treatment for depression.
Another important area for future study is to develop a systematic approach to module selection. In this study, individual and group supervision was used to determine the modules best suited to this particular parent–teen dyad. A clinical algorithm for determining module selection would be very useful if the protocol is to be used more broadly in community settings.
Finally, the cost effectiveness of a concurrent treatment approach should be examined to determine whether (and for whom) it is indicated above the current individual treatment recommendations. If concurrent treatment is associated with better overall outcomes (i.e., reduced depression and suicidality) and reduced use of auxiliary mental health services (e.g., emergency department visits, hospitalizations) for one or both members of the dyad, it might be the preferred treatment modality. The protocol was designed such that two therapists would need to work in tandem, which might prove logistically challenging in some treatment settings.
Acknowledgments
This research was supported by NIMH grant R34MH82211 and awarded to Anthony Spirito.
Contributor Information
Jennifer C. Wolff, The Alpert Medical School of Brown University and Rhode Island Hospital
Barbara Jandasek, The Alpert Medical School of Brown University and Rhode Island Hospital.
Bethany D. Michel, The Alpert Medical School of Brown University
Sara J. Becker, The Alpert Medical School of Brown University
Anthony Spirito, The Alpert Medical School of Brown University.
References
- Adams J, & Adams M (1996). The association among negative life events, perceived problem solving alternatives, depression, and suicidal ideation in adolescent psychiatric patients. Child Psychology and Psychiatry and Allied Disciplines, 37(6), 715–720. 10.1111/j.1469-7610.1996.tb01463.x. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Gladstone TRG, & O’Connor EE (2011). Transmission and prevention of mood disorders among children of affectively ill parents: A review. Journal of the American Academy of Child and Adolescent Psychiatry, 50(11), 1098–1109. 10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- Beck AT, & Steer RA (1991). Manual for the Beck Scale for Suicide Ideation. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, … Zelazny J (2008). Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. Journal of the American Medical Association, 299(8), 901–913. 10.1001/jama.299.8.901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, & Holder D (1998). Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry, 37(9), 906–914. 10.1097/00004583-199809000-00010 [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Spitzer RL, & Gibbon M (2007). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Clinical Trials Version (SCID-CT). New York: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Garber J, Ciesla JA, McCauley E, Diamond G, & Schloredt KA (2011). Remission of depression in parents: Links to healthy functioning in their children. Child Development, 82(1), 226–243. 10.1111/j.1467-8624.2010.01552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Clarke GN, Weersing VR, Beardslee WR, Brent DA, Gladstone TR, … Iyengar S (2009). Prevention of depression in at-risk adolescents: A randomized controlled trial. Journal of the American Medical Association, 301(21), 2215–2224. 10.1001/jama.2009.788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH (2007). Depression in mothers. Annual Review of Clinical Psychology, 3, 107–135. 10.1146/annurev.clinpsy.3.022806.091401 [DOI] [PubMed] [Google Scholar]
- Gratz K, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Hammen C (2006). Stress generation in depression: Reflections on origins, research, and future directions. Journal of Clinical Psychology, 62(9), 1065–1082. 10.1002/jclp.20293 [DOI] [PubMed] [Google Scholar]
- Hammen C (2009). Children of depressed parents. In Gotlib IH & Hammen C (Eds.), Handbook of depression (2nd ed., pp. 275–297). New York, NY: Guilford Press. [Google Scholar]
- Kashani JH, Sherman DD, Parker DR, & Reid JC (1990). Utility of the Beck Depression Inventory with clinic-referred adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 29(2), 278–282. 10.1097/00004583-199003000-00018 [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, & Rao U (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Kennard BD, Emslie GJ, Mayes TL, Nightingale-Teresi J, Nakonezny PA, Hughes JL, … Jarrett RB (2008). Cognitive-behavioral therapy to prevent relapse in pediatric responders to pharmacotherapy for major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 47(12), 1395–1404. 10.1097/CHI.0b013e31818914a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein JB, Jacobs RH, & Reinecke MA (2007). Cognitive-behavioral therapy for adolescent depression: A meta-analytic investigation of changes in effect-size estimates. Journal of the American Academy of Child and Adolescent Psychiatry, 46(11), 1403–1413. 10.1097/chi.0b013e3180592aaa [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, & Clarke GN (1999). Psychosocial treatments for adolescent depression. Clinical Psychology Review, 19(3), 329–342. 10.1016/S0272-7358(98)00055-5 [DOI] [PubMed] [Google Scholar]
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, … Severe J (2004). Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association, 292(7), 807–820. 10.1001/jama.292.7.807 [DOI] [PubMed] [Google Scholar]
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, & Weissman MM (2004). A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 61, 577–584. 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- Mufson L, & Sills R (2006). Interpersonal psychotherapy for depressed adolescents (IPT-A): An overview. Nordic Journal of Psychiatry, 60, 431–437. 10.1080/08039480601022397. [DOI] [PubMed] [Google Scholar]
- Mufson L, Weissman MM, Moreau D, & Garfinkel R (1999). Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 56, 573–579. 10.1001/archpsyc.56.6.573 [DOI] [PubMed] [Google Scholar]
- Robin AL, & Foster SL (1989). Negotiating parent–adolescent conflict: A behavioral–family systems approach. New York, NY: Guilford Press. 10.1207/s15374424jccp1901_11. [DOI] [Google Scholar]
- Rosselló J, & Bernal G (1999). The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology, 67, 734–745. 10.1037//0022-006x.67.5.734. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, … Keller MB (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. 10.1016/S0006-3223(02)01866-8 [DOI] [PubMed] [Google Scholar]
- Spirito A, Wolff JC, Seaboyer LM, Hunt J, Esposito-Smythers C, Nugent N, … Miller I (2015). Concurrent treatment for adolescent and parent depressed mood and suicidality: Feasibility, acceptability, and preliminary findings. Journal of Child and Adolescent Psychopharmacology, 25(2), 131–139. 10.1089/cap.2013.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, Clark DA, Beck AT, & Ranieri WF (1995). Common and specific dimensions of self-reported anxiety and depression: A replication. Journal of Abnormal Psychology, 104(3), 542. 10.1037/0021-843X.104.3.542 [DOI] [PubMed] [Google Scholar]
- Strober M, Green J, & Carlson G (1981). Utility of the Beck Depression Inventory with psychiatrically hospitalized adolescents. Journal of Consulting and Clinical Psychology, 49(3), 482. 10.1037/0022-006X.49.3.482. [DOI] [PubMed] [Google Scholar]
- Tompson MC, Pierre CB, Boger KD, McKowen JW, Chan PT, & Freed RD (2010). Maternal depression, maternal expressed emotion, and youth psychopathology. Journal of Abnormal Child Psychology, 38(1), 105–117. 10.1007/s10802-009-9349-6 [DOI] [PubMed] [Google Scholar]
- Wagner BM, Silverman MAC, & Martin CE (2003). Family factors in youth suicidal behaviors. American Behavioral Scientist, 46(9), 1171–1191. 10.1177/0002764202250661 [DOI] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, … Rush AJ (2006). Remissions in maternal depression and child psychopathology: A STAR*D-child report. Journal of the American Medical Association, 295(12), 1389–1398. 10.1001/jama.295.12.1389 [DOI] [PubMed] [Google Scholar]


