Abstract
Considering that insufficient sleep has long been regarded as a significant public health challenge, the COVID-19 pandemic and its co-evolving infodemic have further aggravated many people's sleep health. People's engagement with pandemic-related news, particularly given that many people are now permanently online via smartphones, has been identified as a critical factor for sleep health, such that public health authorities have recommended limited news exposure. This two-wave panel survey, conducted with a representative sample in Austria during its first COVID-19 lockdown, examines (a) how fear of missing out on pandemic-related news (i.e., COVID-19 information FOMO) is reciprocally related to smartphone-based bedtime news engagement, as well as (b) how both bedtime news engagement and COVID-19 information FOMO predict daytime tiredness. Partial metric measurement invariant structural equation modeling revealed that COVID-19 information FOMO and bedtime news engagement are reciprocally associated over time, indicating a potentially harmful reinforcing loop. However, results further suggested that COVID-19 information FOMO may be the primary driver of daytime tiredness, not smartphone-based bedtime news engagement. These findings suggest that a perceived loss of (informational) control over the pandemic outbreak more strongly than poor sleep habits accounts for depleted energy resources during lockdown. However, given the initial evidence for a reinforcing loop, this effect pattern may change in the long term.
Keywords: COVID-19, Infodemic, FOMO, Bedtime smartphone use, Sleep quality, Daytime tiredness
Sound sleep is a fundamental part of a healthy lifestyle. Because of conceptual complexities surrounding the question of what exactly can be recognized as high-quality sleep and due to interindividual variation in how much good sleep is needed to optimize physical and cognitive functioning, it is considered untenable to determine an optimal amount of sleep (Chaput et al., 2018). Instead, sleep health authorities recommend that adults sleep at least 7 h per night regularly (Watson et al., 2015). Prior research has identified associations between poor sleep and numerous health hazards, including physical conditions such as hypertension (Pepin et al., 2014) or obesity (Rahe et al., 2015) and mental conditions such as depression (Hayashino et al., 2010) or cognitive decline (Spira et al., 2015). Beyond these medical conditions, poor sleep has also been linked to daytime tiredness, which brings with it impaired concentration (Alapin et al., 2000) and reduced productivity (Rosekind et al., 2010). Understandably, given that a considerable percentage of the general population worldwide suffers from insufficient sleep (Grandner, 2019; Simonelli et al., 2018), improving sleep health has been a major goal for public health authorities (CDC, 2020; Colten & Altevogt, 2006).
The pandemic outbreak of COVID-19 at the beginning of 2020 and the co-evolving infodemic (i.e., an overabundance of [mis]information about the pandemic) surrounding it have further complicated this issue. Compared to pre-pandemic levels, several studies have revealed that people on average devoted more time to sleep during the pandemic, primarily because they tend to overcompensate for delayed bedtimes by waking up later (Alfonsi et al., 2021; Gao & Scullin, 2020; Robillard et al., 2021). However, since these longer overall durations were often accompanied by, among other things, longer sleep onset latencies (i.e., the time needed to fall asleep; Alfonsi et al., 2021), more sleep difficulties (e.g., insomnia; Li et al., 2020), and more nightmares (Scarpelli et al., 2021), people's sleep quality nevertheless worsened during the pandemic (Jahrami et al., 2021). This decline in sleep quality coincides with findings on people's intensified news engagement during the COVID-19 pandemic that has been attributed to more extensive reporting and increasing demand for it due to persistent feelings of uncertainty (Mihelj et al., 2021). However, instead of providing reassuring experiences, heavy news engagement has been found related to harmful outcomes (e.g., amplified emotional distress, anxiety, depressive symptoms; Fullana et al., 2020; Olagoke et al., 2020; Stainback et al., 2020) that mirror psychological consequences previously documented for news overconsumption from other traumatic events (e.g., terrorist attacks or natural disasters; Pfefferbaum et al., 2021), so much so that public health authorities have endorsed limited exposure (Crew et al., 2020). In other words, COVID-19 and the extensive spread of information about it made an already great public health challenge even more significant.
Conducted during the first COVID-19 lockdown in Austria, this longitudinal study contributes to our understanding of what promotes inefficient sleep in these challenging times by investigating (a) how people's fear of missing out (FOMO) on pandemic-related news is associated with their smartphone-based bedtime news engagement and (b) how both this bedtime news engagement and COVID-19-related FOMO predict daytime tiredness over time. More specifically, this study contributes to extant findings in several ways: First, it is the first to examine how behavioral and motivational aspects of people's COVID-19 news engagement dynamically influence each other, which may allow for a first glimpse into whether a reinforcing loop (cf. Slater, 2015) may be at work. Second, this study seeks to determine whether bedtime news engagement contributes to the depletion of people's energy resources once an underlying motivational tendency (i.e., COVID-19 information FOMO) is recognized that may be better suited to predict daytime tiredness during lockdown given that a considerable number of people were (at minimum) advised to work from home where they were partially disburdened from transit efforts and occupational schedules. Third, our study is methodologically innovative. It involves a two-wave survey design and measurement invariant over-time structural equation models that, in contrast to predominantly existing cross-sectional research, may allow for insights into the predictive causality of our constructs of interest.
1. Reciprocity of bedtime pandemic-related news engagement and COVID-19 information FOMO
Parallel to the COVID-19 pandemic outbreak, an infodemic has co-evolved with an inordinate amount of (accurate or inaccurate) information being presented during 24-h news cycles and on social media (Gallotti et al., 2020). Bearing in mind the individual and societal uncertainties involved with the pandemic (Koffman et al., 2020), many people have been tempted to closely follow developments at any given time out of concern about missing out on relevant (or reassuring) information—a phenomenon referred to as COVID-19 information FOMO (Yu et al., 2020). While social FOMO was originally understood as “a pervasive apprehension that others might be having rewarding experiences from which one is absent” (Przybylski et al., 2013, p. 1841), Yu and colleagues (2020) have argued that people may feel similarly anxious about losing control over COVID-19-related information. More specifically, COVID-19 information FOMO is driven by people's desire to become and stay fully aware of the latest pandemic information to gain feelings of informational control. Like how social FOMO is associated with stronger social media engagement (Beyens et al., 2016), COVID-19 information FOMO has therefore been linked to people's engagement with pandemic-related news (Shabahang et al., 2021; Yu et al., 2020). However, just as social FOMO often turns out harmful because of people's limited resources to follow up on given social possibilities (Przybylski et al., 2013), COVID-19 information FOMO may become problematic when there is an overabundance of information. Accordingly, another analogy between both forms of FOMO may exist regarding sleep health where social FOMO has been documented predictive of people's sleep duration via enhanced pre-sleep arousal and bedtime social media use (Scott & Woods, 2018). Prior research has suggested that people engage in news avoidance or satisficing (i.e., consuming just enough information to be satisfied but not overwhelmed by it) as efficient strategies to cope with news overload (Ahmed, 2020; Groot Kormelink & Klein Gunnewiek, 2021). People who score high on COVID-19 information FOMO may be less able to pursue such protective strategies and more likely to continue their engagement with pandemic news although they intended to go off(line) to sleep. Thus, we hypothesized:
H1a
: COVID-19 information FOMO positively predicts bedtime pandemic-related news engagement via smartphone over time.
Heavy pandemic-related news engagement has generally been recommended against by scholars and public health authorities to avoid psychological distress (Crew et al., 2020; Garfin et al., 2020). This recommendation has been validated by findings showing that following COVID-19 news relates to aggravated threat perceptions (Stainback et al., 2020), depressive symptoms (Olagoke et al., 2020), as well as increased symptoms of anxiety (Fullana et al., 2020). Although lacking data to examine it, Stainback et al. (2020) discussed a reinforcing loop between news engagement and perceived threats that may promote these effects: That is, perceived threats may motivate pandemic-related news engagement, which then may amplify perceived threats, which, then again, may trigger intensified COVID-related news engagement, and so forth. A similar reciprocal process can be assumed between bedtime news engagement and COVID-19 information FOMO. In addition to H1a, heavy news engagement (during both day and night) may produce COVID-19 information FOMO through enhanced threat experiences and anxiety (similar to how salient events motivated news consumption during the early stages of the pandemic in Ohme et al., 2020). Concerning bedtime news engagement, one could further argue that it might make more salient the plethora of pandemic-related news from all over the world, from which at least some may otherwise have been stayed unconsidered. This increased salience may further contribute to feelings of missing out on potentially relevant pandemic news, which is why we hypothesized:
H1b
Bedtime pandemic-related news engagement via smartphone positively predicts COVID-19 information FOMO over time.
2. Bedtime news engagement and COVID-19 information FOMO as predictors of daytime tiredness
In times of permanent access(ibility) to social contacts and online content (Vorderer et al., 2017), people's engagement with screen-based media before and during bedtime has often been assigned a leading role in discussions about sleep health (Barnes & Drake, 2015). Extant literature has discussed several mechanisms by which screen-based bedtime media engagement may deteriorate people's sleep quality. Most notably, screen time is said to displace more beneficial activities, suppress melatonin production, and provide unsettling and arousing information (Cain & Gradisar, 2010) that delay both bedtime (i.e., time at which people decide to go to bed) and shuteye time (i.e., time at which people decide to go to sleep; Exelmans & van den Bulck, 2017). Besides these, smartphone notifications can disrupt the sequential progress of sleep cycles (Murdock & Adams, 2019). Albeit relatively modest in overall effect size, empirical research has provided support for the detrimental impact of bedtime smartphone use among adults, most of all after falling asleep, that is, when their sleep is interrupted (Dissing et al., 2021). Apart from being harmful in itself, repeated incidences of insufficient sleep inhibit one of the primal functions of sleeping: energy restoration.
Broadly speaking, the energy hypothesis of sleep states that people's limited brain resources get continuously depleted during active metabolic periods and restored by sleep (cf. Scharf et al., 2008). Insufficient sleep typically fails to allow for full energy recovery, resulting in a shortage of consumable energy resources that is reflected in increased tiredness during daytime activities. As described above, people's engagement in screen-based media, above all smartphones, has been documented as inhibiting good sleep due to its impact on delayed and disrupted sleep via different behavioral, psychological, and psycho-physiological routes (Cain & Gradisar, 2010). Previous research has also established that bedtime smartphone use is predictive of diminished brain resources on the consecutive day (Lanaj et al., 2014) and associated with daytime tiredness (Luqman et al., 2020; Randjelović et al., 2019). Luqman and colleagues (2020) further classified the impact across different types of bedtime smartphone use, showing that heavy information-seeking contributed to poor sleep and, as a consequence of it, daytime energy depletion. Given that the COVID-19 outbreak has brought people to increase their news engagement (Mihelj et al., 2021), we hypothesized that these findings would be replicated for bedtime news engagement and daytime tiredness:
H2a
Bedtime pandemic-related news engagement via smartphone positively predicts daytime tiredness over time.
While presumably reciprocally related (see H1a and H1b), COVID-19 information FOMO may entail an individual influence on daytime tiredness that is not accounted for by bedtime smartphone use (or insufficient sleep). For one thing, people with COVID-19 information FOMO tend to invest more of their limited resources into following and thinking about the latest news (Shabahang et al., 2021; Yu et al., 2020). Such greater involvement with pandemic-related news has been linked to enhanced psychological distress (Stainback et al., 2020), which previous research has established as an essential correlate of excessive tiredness (Bültmann et al., 2002; Pawlikowska et al., 1994). More intense COVID-19 news engagement may also burden people's limited time resources (cf. Kraut et al., 1998), so much so that it might “displace” more beneficial activities during lockdown (e.g., physical activity; Sañudo et al., 2020; or need-satisfying media use; Eden et al., 2020) that likely could serve physical and psychological recovery. Apart from this link to news engagement, COVID-19 information FOMO itself can be functionally conceptualized as a persistent internal stressor fueled by not feeling in control of the all-day available abundance of pandemic-related news. Akin to COVID-19 anxiety (Arslan et al., 2020), COVID-19 information FOMO may by itself wear out people's finite energy resources over time by reinforcing psychological distress due to a perceived lack of informational control and persistent rumination about it, both by day and night. Contrary to how bedtime news engagement was assumed to reduce the likelihood of good (i.e., fully recreative) sleep, we hypothesized that COVID-19 information FOMO is primarily associated with greater energy consumption, either by itself or via correlates, which over time may lead to daytime resource depletion and tiredness:
H2b
COVID-19 information FOMO positively predicts daytime tiredness over time.
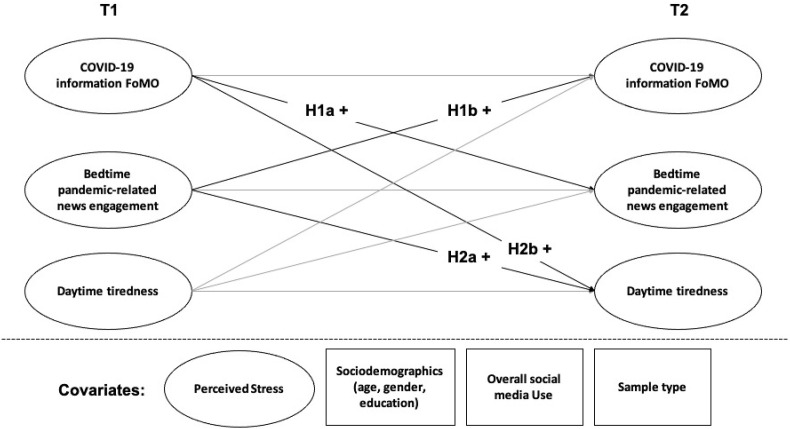
The complete structural model, including all hypotheses as well as covariates, is displayed in Fig. 1 . Although no predictions were hypothesized, we also included reciprocal paths from daytime tiredness to COVID-19 information FOMO and bedtime pandemic-related news engagement in our model for the purpose of controlling for their potential impact.
Fig. 1.
Overview of the structural model. Notes: T1 = First wave (i.e., late March/early April 2020), T2 = second wave (i.e., May 2020).
3. Method
The present study was part of a more comprehensive longitudinal investigation that focused on different nuances of smartphone use and their impact on psychological health during the first lockdown in Austria. Accordingly, this study does not report all available variables of the comprehensive panel survey but those relevant to its research interest.
3.1. Sampling and procedure
A two-wave panel survey with a one-month interval between both waves was carried out during the first COVID-19 lockdown in Austria. The first survey (T1) was conducted in late March/beginning of April 2020 and the second survey (T2) in May 2020. For the recruitment of participants, we cooperated with (1) a professional polling institute and (2) students of the University of Vienna. Using identical surveys, both simultaneously started data collection based on quota for age, gender, and education in Austria. While participants recruited by the polling institute may have received monetary compensation, participants recruited by collaborating students did not. People could take part if they agreed to the informed consent, had a smartphone, and were at least 16 years old. Before data collection, ethical clearance was obtained from the Institutional Review Board of the Department of Communication of the University of Vienna. To safeguard against poor data quality, we excluded participants who completed the surveys unreasonably fast (i.e., in less than 9 min from a polling institute data; T1: n = 62; T2: n = 7 and from collaborating students’ data; T1: n = 170; T2: n = 1).
The first survey consisted of data from N = 731 participants (M age = 40.49, SD age = 13.33; 53.90% women; 20.52% no education and lower-secondary education, 46.51% secondary education, 32.97% complete university education), comprising N = 265 (36.25%) participants who had been recruited by the polling institute (M age = 41.60, SD age = 13.13; 52.08% women; 31.70% no education and lower-secondary education, 50.57% secondary education, 17.74% complete university education) and N = 466 (63.75%) participants recruited by students (M age = 39.87, SD age = 13.41; 54.94% women; 14.16% no education and lower-secondary education, 44.21% secondary education, 41.63% complete university education). A total of N = 416 of these participants (M age = 41.97, SD age = 13.59; 54.33% women; 21.64% no education and lower-secondary education, 44.95% vocational school education and secondary education, 33.41% complete university education) also completed the second survey, indicating a 43.09% attrition rate (polling institute: 38.11%; student recruitment: 45.92%). From this sample, N = 164 (39.42%) participants were recruited by the polling institute (M age = 43.18, SD age = 14.00; 45.12% women; 33.54% no education and lower-secondary education, 48.78% secondary education, 17.68% complete university education), and N = 252 (60.58%) from students (M age = 41.18, SD age = 13.29; 60.32% women; 13.89% no education and lower-secondary education, 42.46% secondary education, 43.65% complete university education).
Participants who dropped out after T1 (n = 315) and those who completed T2 (n = 416) did not differ regarding their education, χ 2(5) = 5.33, p = .377. However, the drop-out sample differed significantly from respondents who participated in both surveys in that they were younger (M = 38.53, SD = 12.80 vs. M = 41.98, SD = 13.55; t(729) = 3.49, p = .001, Cohen's d = . 261), had a stronger bedtime engagement with pandemic news (M = 2.08, SD = 1.34 vs. M = 1.87, SD = 1.23; t(643.798) = −2.21, p = .028, d = −0.164), and experienced more COVID-19 information FOMO (M = 1.76, SD = 0.86 vs. M = 1.63, SD = 0.85; t(729) = −1.98, p = .048, d = −0.152), and more daytime tiredness (M = 3.51; SD = 1.55 vs. M = 3.26, SD = 1.50; t(729) = −2.24, p = .025, d = −0.164). Notably, all of these differences were either small or negligible in size.
4. Measures
4.1. COVID-19 information FOMO
We measured COVID-19 information FOMO with three customized items inspired by Przybylski et al. (2013) and Wegmann et al. (2017): “When I miss the latest news about the novel coronavirus or hear about it later than others, I get annoyed”; “I am afraid that others are more up-to-date or better informed about the novel coronavirus than I am”; “When I don't keep up with the latest things regarding the novel coronavirus on social media, I get annoyed.” Participants were asked to indicate how strongly they agree with these statements on five-point Likert scales ranging from ‘strongly disagree’ to ‘strongly agree’ (T1: Cronbach's α = 0.77; M = 1.68, SD = 0.86; T2: α = 0.83; M = 1.46, SD = 0.75).
4.2. Bedtime pandemic-related news engagement via smartphone
To assess bedtime pandemic-related news engagement via smartphone, we relied on three adapted items from Van den Bulck (2007). We asked participants to indicate how often they had used the smartphone during the past weeks to do the following activities when they were lying in bed with the lights off to sleep: “Receiving any messages regarding the novel coronavirus (e.g., on WhatsApp)”; “Sending any messages regarding the novel coronavirus (e.g., on WhatsApp)”; “Posting content or commenting on social media (e.g., Facebook) about the novel coronavirus.” Participants responded on seven-point Likert scales ranging from ‘never’ to ‘more than 8 times’ (T1: α = 0.73; M = 1.96, SD = 1.28; T2: α = 0.77; M = 1.57, SD = 0.99).
4.3. Daytime tiredness
Daytime tiredness was assessed via three items adapted from Van den Bulck (2007). On seven-point Likert scales ranging from ‘not tired at all’ to ‘very tired’, participants were asked to think back over their last week and indicate “how tired they had been in general”; “how tired they had been when getting up”; and “how tired they had beenduring the day” (T1: α = 0.86; M = 3.37, SD = 1.52; T2: α = 0.86; M = 3.26, SD = 1.48).
4.4. Covariates
We entered several variables into the statistical model that were not included in the hypotheses but needed to be controlled to highlight the prediction results of the constructs of interest. Besides sociodemographics (age, gender, and education), which may act as proxies for different behavioral tendencies and life situations that influence the outcome variables, we controlled for perceived stress (to covary out the impact of varying experiences of stress during the pandemic; Robillard et al., 2020), overall social media use (to parcel out the influence of people's general proclivity for screen-based media usage, both day and night), and sample type as covariates. For perceived stress, we used four items from the Brief Inventory of Perceived Stress Scale by Lehman and colleagues (2012) adapted to the smartphone context by Karsay and colleagues (2019). On a seven-point Likert scale ranging from ‘never’ to ‘very often,’ participants answered the following questions: “In the last week, how often did you have too many things to do?“; “In the last week, how often did you feel like you were in a hurry?“; “In the last week, how often did you feel like you had to do things even though you didn't want to do them?“; “In the last week, how often did you feel as if difficulties were so great that you could not overcome them?” (T1: α = 0.79; M = 2.86, SD = 1.41). To measure overall social media use, participants indicated on seven-point Likert scales ranging from ‘never’ to ‘very often’ how often they use the following eight social media channels on their smartphone: Instagram, YouTube, Twitter, Tik Tok, Snapchat, Skype, Messaging Apps (e.g., WhatsApp, Telegram), and Facebook (T1: α = 0.63; M = 2.96, SD = 0.99). Lastly, given that we made use of two recruitment strategies, we controlled for sampling type using a dummy-coded variable (0 = online quota sample recruited by professional polling institute, N = 164; 1 = online quota sample recruited by students, N = 252).
4.5. Data analysis
We used SPSS Amos (Arbuckle, 2014) to conduct Structural Equation Modeling with Full Maximum Likelihood estimation. Our statistical analysis controlled for autoregressive effects (i.e., COVID-19 information FOMO at T1 as a predictor for COVID-19 information FOMO at T2). Further, we constrained factor loadings of all the latent variables at both times (T1 and T2) to be equal to test for longitudinal measurement invariance (Vandenberg & Lance, 2000). After releasing this constraint for item 3 of bedtime news engagement, the fit of the constrained model was good: CFI = 0.95; TLI = 0.93; NFI = 0.91; χ2/df = 2.03, p < .001; RMSEA = 0.04, 90%-CI [0.03; 0.04]. No significant difference was found when comparing the unconstrained and constrained model, χ2 (5) = 6.05, p = .301. Together, these results suggest that the constructs show partial metric invariance over time.
5. Results
Zero-order correlations between averaged indices of all main variables are displayed in Table 1 . Key results from the autoregressive latent variable model are presented in Table 2 .
Table 1.
Zero-order correlations between averaged indices of all main variables.
| Variablesa | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Bedtime news engagement (T1) | 1 | |||||
| 2. Bedtime news engagement (T2) | .47∗∗∗ | 1 | ||||
| 3. COVID-19 information FOMO (T1) | .25∗∗∗ | .24∗∗∗ | 1 | |||
| 4. COVID-19 information FOMO (T2) | .27∗∗∗ | .40∗∗∗ | .50∗∗∗ | 1 | ||
| 5. Daytime tiredness (T1) | .15∗∗∗ | .14∗∗ | .12∗∗ | .14∗∗ | 1 | |
| 6. Daytime tiredness (T2) | .13∗∗ | .20∗∗∗ | .17∗∗∗ | .21∗∗∗ | .64∗∗∗ | 1 |
Notes: T1 = Measurement time 1 (i.e., April 2020), T2 = Measurement time 2 (i.e., May 2020).
∗∗ < 0.01, ∗∗∗ < 0.001.
NT1 = 731, NT2 = 416.
Table 2.
Overview of results of the autoregressive latent variable model.
| Predictorsa | Bedtime news engagement (T2) |
COVID-19 information FOMO (T2) |
Daytime tiredness (T2) |
|||
|---|---|---|---|---|---|---|
| b (SE), β | p | b (SE), β | p | b (SE), β | p | |
| Bedtime news engagement (T1) | .35 (.05), .45 | < .001 | .08 (.03), .13 | .016 | -.02 (.05), −.02 | .712 |
| COVID-19 information FOMO (T1) | .15 (.07), .12 | .046 | .51 (.06), .54 | < .001 | .18 (.09), .10 | .043 |
| Daytime tiredness (T1) | .02 (.04), .02 | .716 | .03 (.03), .05 | .405 | .66 (.06), .66 | < .001 |
| Overall social media use (T1) | .15 (.06), .14 | .009 | .07 (.04), .09 | .097 | .03 (.07), .02 | .705 |
| Perceived Stress (T1) | -.001 (.06), −.002 | .981 | .01 (.05), .02 | .776 | -.04 (.08), −.04 | .556 |
| Age | .002 (.004), .03 | .610 | .001 (.003), .02 | .726 | -.01 (.01), -.09 | .038 |
| Gender | .002 (.10), .001 | .982 | -.11 (.07), −.07 | .121 | .10 (.12), .03 | .389 |
| Education: low vs. moderate | -.13 (.13), −.06 | .331 | .05 (.10), .03 | .600 | .19 (.16), .06 | .223 |
| Education: low vs. high | -.02 (.14), −.01 | .886 | .03 (.11), .02 | .745 | -.07 (.17), −.02 | .679 |
| Sample type | -.53 (.11), -.24 | < .001 | .01 (.08), .004 | .936 | -.24 (.13), −.08 | .072 |
Notes: T1 = Measurement time 1 (i.e., April 2020), T2 = Measurement time 2 (i.e., May 2020). Significant findings are in bold. Sample types were coded: 0 = polling quota sample data, 1 = university quota-sample data. Self-identified gender are coded: 0 = male, 1 = female).
NT1 = 731, NT2 = 416.
5.1. Hypothesis testing
Results indicate that COVID-19 information FOMO at T1 significantly predicted participants’ bedtime pandemic-related news engagement via smartphone at T2, b = 0.15, SE = 0.07, β = 0.12, p = .046. Furthermore, bedtime news engagement at T1 also significantly predicted COVID-19 information FOMO at T2, b = 0.08, SE = 0.03, β = 0.13, p = .016. These findings suggest meaningful reciprocity between motivational (i.e., COVID-19 information FOMO) and behavioral aspects (i.e., bedtime news engagement) of participants’ engagement with COVID-19-related news: The stronger our participants desired to be aware of all the latest pandemic information, the more likely they were to continue consuming related news despite intending to sleep a month later; vice versa, the more participants consumed news during bedtime via smartphone, the higher their score for COVID-19 information FOMO turned out to be in the coming month.
With regard to participants’ daytime tiredness, analysis revealed no significant prediction over time by bedtime consumption of pandemic-related news, b = −0.02, SE = 0.05, β = −0.02, p = .712. However, COVID-19 information FOMO at T1 did significantly predict daytime tiredness at T2, b = 0.18, SE = 0.09, β = 0.10, p = .043. These results indicate that participants consuming pandemic-related news during bedtime did not explain whether or not they felt tired during the day, while the extent to which they desired to keep track of COVID-19 news did so. The data supported only H2b; H2a must be rejected.
5.2. Covariate effects
We included several covariates into the autoregressive latent variable model to control their influence on the respective endogenous variables. Concerning participants’ bedtime news engagement at T2, only overall social media use, b = 0.15, SE = 0.06, β = 0.14, p = .009, and the sampling method, b = −0.53, SE = 0.11, β = −0.24, p < .001 (lower scores for the polling quota), explained individual variance in a statistically meaningful manner. None of the covariates turned out significant for COVID-19 information FOMO. Lastly, only participants’ age emerged as a significant predictor for daytime tiredness, with older participants feeling less tired than younger participants, b = −0.01, SE = 0.01, β = −0.09, p = .038.
6. Discussion
While poor sleep health has been stressed for many years to be alarmingly widespread (CDC, 2020; Colten & Altevogt, 2006), the COVID-19 pandemic and infodemic of 2020 have worked in tandem to further exacerbate this public health issue (Jahrami et al., 2021). With international developments concerning COVID-19 steadily feeding the 24-h news cycle, health authorities advised against heavy news engagement, which has been found associated with fatalistic assessments of the personal and societal consequences of the pandemic (Stainback et al., 2020) and impaired mental health (Fullana et al., 2020). However, the extent to which people's news engagement contributes to poor sleep health when in lockdown yet needs to be determined. Examining how strongly news engagement influences people's sleep health under these circumstances is by no means a trivial exercise, given that lockdown orders may have relieved people from their occupational schedules. Otherwise harmful behaviors (e.g., delayed sleep due to bedtime media engagement) may be less consequential under these conditions.
Using partial metric measurement invariant structural equation modeling, this study documents initial evidence that news engagement during the pandemic/infodemic may involve behavioral (i.e., bedtime news engagement) and motivational aspects (i.e., FOMO on pandemic news) that are reciprocally related to each other. Over time, this reciprocity could create a reinforcing loop that might lead to harmful news habits (e.g., Shabahang et al., 2021). Somewhat unexpectedly, we further found longitudinal evidence that COVID-19 information FOMO might be the primary driver of daytime tiredness, not smartphone-based news engagement during bedtime. Overall, these findings suggest that people's finite energy resources during lockdown may have been most strongly depleted by a persistently elevated anxiety regarding a loss of (informational) control and less so by poor sleep hygiene. However, this effect pattern may change over more extended periods because of the reinforcing loop.
6.1. A reinforcing spiral of COVID-19 information FOMO and bedtime news engagement
According to the Reinforcing Spirals framework (Slater, 2015), media selection and media effects can be understood as mutually influencing processes that could produce substantial consequences. The present study may suggest that a similar reciprocal process can be found for people's FOMO on pandemic-related information and their news engagement during bedtime. People who are more anxious about losing informational control and, therefore, may have a stronger desire to become or stay utterly aware of all the latest developments tend to consume more pandemic-related news when they already lie in bed. This bedtime news engagement may, then again, further foster people's COVID-19 information FOMO, and the loop starts anew. People who are stuck in this reinforcing spiral may be less likely to engage in efficient coping behaviors, such as selective news engagement (Ahmed, 2020; Groot Kormelink & Klein Gunnewiek, 2021), to avoid more severe consequences and may be more likely to become “news junkies” for whom news engagement is compulsive (Broersma & Swart, 2021).
As COVID-19 information FOMO is a relatively novel concept (albeit similar phenomena may emerge during other global or regional crises as well where information is mounting), it is unclear what other attitudes and behaviors may be associated with it (e.g., overall news engagement, negligence of other activities, pessimism, depressive mood, lack of motivation). While our data did not reveal any correlates, Broersma and Swart (2021) found that people who were more strongly affected by the pandemic were also more likely to show compulsive news engagement—essentially mirroring a general trend that established vulnerable populations are more severely harmed by the pandemic (Kuy et al., 2020). Another question for future research is how this (and other) potentially harmful reinforcing spirals may be broken for those who cannot on their own find their way back to normal after the current wave (or even the pandemic altogether) has faded away. Of course, additional research is needed to validate this potential reinforcing spiral; however, if it will be “proven to be true,” then considerable (research) effort should be directed towards promising approaches for disengagement.
6.2. COVID-19 information FOMO is the primary driver of daytime tiredness
Since people have limited brain energy resources, one of the most basic functions of sleep is to restore those resources that had been consumed throughout the day (cf. Scharf et al., 2008). Accordingly, daytime tiredness can be considered the result of an imbalance where resource consumption exceeds recovery. Viewed through this lens, bedtime news engagement and COVID-19 information FOMO operate on opposite sides of the equation: While bedtime news engagement may make healthy sleep less likely and, thus, inhibit the energetic recharge, COVID-19 information FOMO may involve increased energy consumption during daytime. Our findings suggest that during the first lockdown in Austria, the additional strain associated with COVID-19 information FOMO may be more relevant in predicting daytime tiredness over time than smartphone-based news engagement during bedtime.
These results are notable in two regards: First, it is noteworthy that people's bedtime news engagement at the beginning of the first lockdown in late March/early April was not predictive of their daytime tiredness at the end of it in May 2020. This non-effect, which stands in contrast to most previous research (e.g., Mac Cárthaigh et al., 2020; but also see Orben & Przybylski, 2020), may be explained by many people's obligation (or decision) to work from home during lockdown. Regular work schedules and transit efforts often force people to get up early so that additional news engagement in the evenings haunts them during the days. Working from the home office may have eased up these occupational zeitgebers’ influence considerably (Bryson, 2020), such that bedtime news engagement ends up less consequential than during “normal” times. This interpretation corresponds with prior research demonstrating better daytime functioning and sleep health during lockdown among some people due to less rigid morning commitments (Alfonsi et al., 2021; Gao & Scullin, 2020). The null effect of bedtime news engagement also aligns with Dissing et al.’s (2021) suggestion that it is not delayed but disrupted sleep that is the main reason for inefficient sleep. However, we have to note that the scale's wording (i.e., “when you lie in bed and the lights are switched off to sleep”) might not have been concise enough to differentiate between delayed and disrupted sleep (even though we think the former may be much more likely). Importantly, both interpretations may also be highly relevant in a post-lockdown or even post-COVID-19 world, provided that home office work will become more accepted among both employers and employees. Future research will have to investigate whether our findings can be validated and generalized to post-pandemic times.
Second and in contrast to bedtime news engagement, COVID-19 information FOMO emerged as the primary driver of people's daytime tiredness. While others already emphasized the prominent role that social FOMO plays during the pandemic for problematic media habits (Elhai et al., 2021) and poor sleep (Hayran & Anik, 2021), the present study is, to our knowledge, the first to demonstrate that informational FOMO predicts sleep health over time (similar to pre-pandemic findings for social FOMO; Scott & Woods, 2018). That is, people who experience a lack of control about pandemic-related news are more likely to feel tired during the day. However, since COVID-19 information FOMO (or, more broadly, informational FOMO) is a very novel construct, it is yet unclear what its behavioral and cognitive correlates might be. Excessive news engagement (or online news addiction; Shabahang et al., 2021) or perceived news overload (Song et al., 2017) are perhaps the most evident candidates. We would also encourage researchers to engage qualitative methods to gain more unique insights into this new construct. Notably, this study cannot differentiate between the direct impact of informational FOMO and possible indirect paths via, for instance, increased news engagement or perceived overload. Our data do not determine whether people's persistent anxiety of not being aware of novel pandemic-related information makes them tired or an associated tendency to minimize the likelihood of missing out on relevant news through heavier engagement throughout the day. Then again, perceived overload resulting from this heavy news engagement could also be influential—or all of them together. Additional data are needed to test these (and other) paths. Again, it is essential to note that, albeit the COVID-19 pandemic/infodemic arguably provided ideal conditions for informational FOMO to emerge, the construct is not necessarily confined to this most extraordinary of circumstances. It could also occur during other infodemic-like situations (e.g., presidential elections, natural disasters, sports events) or perhaps even any other event once people are incredibly involved with them. If replicated, our results may thus be generalizable to such other circumstances.
6.3. Limitations
In addition to those already mentioned, the present study is subject to further limitations. The study was conducted during the first lockdown in Austria (i.e., late March/early April 2020 to May 2020). This means that our findings cannot easily be generalized without additional evidence toward other countries (where pandemic activities and governmental measures against it, as well as local news coverage, may have differed), later lockdowns (during which prior experiences and habitualization may be influential), or, generally, the entire COVID-19 pandemic/infodemic (given substantial developments during this period). The one-month survey interval might have been sufficient to examine medium-term processes that unfold over a matter of weeks (such as news engagement, informational FOMO, or daytime tiredness). However, it also prevented us from investigating both more elusive (e.g., event-related news rumination and dream activity) and long-term processes (e.g., news habits and insomnia symptoms). Relatedly, we performed only two measurements during this period, which prohibits us from thoroughly testing the suggested reinforcing loop between bedtime news engagement and COVID-19 information FOMO or any longitudinal mediation effects. Multi-wave designs that include different time intervals (e.g., measurement-burst designs; Sliwinski, 2008) will be vital to gain more comprehensive insights in the future.
Given that we relied entirely on self-report short scales for measuring our focal constructs, the present study may suffer from common method bias and other measurement errors (e.g., social desirability). Due to the two-wave panel structure of the study, some of the measures also involved aggregated estimations over a prolonged period (e.g., during last week), which are vulnerable to answering and memory biases (Chevance et al., 2020). Future research should consider implementing objective measures to complement self-report measures, particularly to indicate sleep health (e.g., actigraphy in addition to established self-assessments; cf. Mac Cárthaigh et al., 2020) or smartphone use (e.g., integrated trackers; Rod et al., 2018). Another limitation of this study's self-report measures is their lack of content flexibility. Accordingly, we cannot assume whether bedtime engagement with specific content or content-specific informational FOMO might be more or less influential than other news content. Such qualitative data are necessary to prevent overgeneralization of effects and should be included in future studies.
Lastly, while representative sampling is aimed to improve the overall generalizability of any given results, it often comes with a significant downside: Particularly vulnerable individuals or subgroups, for which severe effects may exist, get easily overlooked when only considering overall effects. Including, for example, indicators of sociodemographic or psychosocial vulnerabilities (Valkenburg & Peter, 2013) or determining person-specific effects (Beyens et al., 2020) may help against these shortcomings. They should be stronger pursued in future research.
7. Conclusion
The pandemic outbreak of COVID-19 brought many people an unprecedented feeling of uncertainty, which was further amplified by a co-evolving infodemic. Well-dosed news engagement had been essential to gain sufficient knowledge about the pandemic, especially during its first months. Notwithstanding this necessity, the present study indicates that a firm desire to become and stay fully informed about the latest pandemic-related developments (i.e., COVID-19 information FOMO) might over time contribute to how tired people feel during the day. Although smartphone-based bedtime news engagement did not similarly predict daytime tiredness, its reciprocal relationship with COVID-19 information FOMO suggests that it might be part of a potentially harmful reinforcing loop. Taken together, these findings may send a signal to researchers and policymakers that recent calls for global strategies on post-pandemic public health (Reid et al., 2021) should also include the aftermath of the COVID-19 infodemic.
CRediT author statement
Kevin Koban: Conceptualization, Methodology, Writing – Original Draft, Writing - Review & Editing; Ariadne Neureiter: Methodology, Data Curation, Investigation, Writing – Original Draft; Anja Stevic: Methodology, Data Curation, Investigation, Writing – Original Draft; Jörg Matthes: Formal analysis, Writing – Original Draft, Supervision.
References
- Ahmed S.T. Managing news overload (MNO): The COVID-19 infodemic. Information. 2020;11(8):375. doi: 10.3390/info11080375. [DOI] [Google Scholar]
- Alapin I., Fichten C.S., Libman E., Creti L., Bailes S., Wright J. How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? Journal of Psychosomatic Research. 2000;49(5):381–390. doi: 10.1016/S0022-3999(00)00194-X. [DOI] [PubMed] [Google Scholar]
- Alfonsi V., Gorgoni M., Scarpelli S., Zivi P., Sdoia S., Mari E., Fraschetti A., Ferlazzo F., Giannini A.M., De Gennaro L. COVID‐19 lockdown and poor sleep quality: Not the whole story. Journal of Sleep Research. 2021 doi: 10.1111/jsr.13368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle J.L. IBM SPSS; 2014. Amos. [Computer Program] [Google Scholar]
- Arslan G., Yıldırım M., Aytaç M. Subjective vitality and loneliness explain how coronavirus anxiety increases rumination among college students. Death Studies. 2020:1–10. doi: 10.1080/07481187.2020.1824204. [DOI] [PubMed] [Google Scholar]
- Barnes C.M., Drake C.L. Prioritizing sleep health: Public health policy recommendations. Perspectives on Psychological Science. 2015;10(6):733–737. doi: 10.1177/1745691615598509. [DOI] [PubMed] [Google Scholar]
- Beyens I., Frison E., Eggermont S. “I don't want to miss a thing”: Adolescents' fear of missing out and its relationship to adolescents' social needs, Facebook use, and Facebook related stress. Computers in Human Behavior. 2016;64:1–8. doi: 10.1016/j.chb.2016.05.083. [DOI] [Google Scholar]
- Beyens I., Pouwels J.L., van Driel I.I., Keijsers L., Valkenburg P.M. The effect of social media on well-being differs from adolescent to adolescent. Scientific Reports. 2020;10(1):10763. doi: 10.1038/s41598-020-67727-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broersma M., Swart J. Do novel routines stick after the pandemic? The formation of news habits during COVID-19. Journalism Studies. 2021;1–18 doi: 10.1080/1461670X.2021.1932561. [DOI] [Google Scholar]
- Bryson W.J. Circadian rhythm sleep-wake disorders and the COVID-19 pandemic. Journal of Clinical Sleep Medicine. 2020;16(8) doi: 10.5664/jcsm.8540. 1423–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bültmann U., Kant I.J., Schröer C., Kasl S. The relationship between psychosocial work characteristics and fatigue and psychological distress. International Archives of Occupational and Environmental Health. 2002;75(4):259–266. doi: 10.1007/s00420-001-0294-0. [DOI] [PubMed] [Google Scholar]
- Cain N., Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Medicine. 2010;11(8):735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Sleep and sleep disorders.https://www.cdc.gov/sleep [Google Scholar]
- Chaput J.-P., Dutil C., Sampasa-Kanyinga H. Sleeping hours: What is the ideal number and how does age impact this? Nature and Science of Sleep. 2018;10:421–430. doi: 10.2147/NSS.S163071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevance G., Perski O., Hekler E.B. Innovative methods for observing and changing complex health behaviors: Four propositions. Translational Behavioral Medicine. 2020 doi: 10.1093/tbm/ibaa026. ibaa026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colte H.R., Altevogt B.M. National Academies Press; 2006. Sleep Disorders and sleep Deprivation: An Unmet public health Problem. [PubMed] [Google Scholar]
- Crew E.C., Baron K.G., Grandner M.A., Ievers-Landis C.E., McCrae C.S., Nadorff M.R., Nowakowski S., Ochsner Margolies S., Hansen K. The society of behavioral sleep medicine (SBSM) COVID-19 task force: Objectives and summary recommendations for managing sleep during a pandemic. Behavioral Sleep Medicine. 2020;18(4):570–572. doi: 10.1080/15402002.2020.1776288. [DOI] [PubMed] [Google Scholar]
- Dissing A.S., Andersen T.O., Nørup L.N., Clark A., Nejsum M., Rod N.H. Daytime and nighttime smartphone use: A study of associations between multidimensional smartphone behaviours and sleep among 24,856 Danish adults. Journal of Sleep Research. 2021 doi: 10.1111/jsr.13356. [DOI] [PubMed] [Google Scholar]
- Eden A.L., Johnson B.K., Reinecke L., Grady S.M. Media for coping during COVID-19 social distancing: Stress, anxiety, and psychological well-being. Frontiers in Psychology. 2020;11:577639. doi: 10.3389/fpsyg.2020.577639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai J.D., McKay D., Yang H., Minaya C., Montag C., Asmundson G.J.G. Health anxiety related to problematic smartphone use and gaming disorder severity during COVID‐19: Fear of missing out as a mediator. Human Behavior and Emerging Technologies. 2021;3(1):137–146. doi: 10.1002/hbe2.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exelmans L., Van den Bulck J. Bedtime, shuteye time and electronic media: Sleep displacement is a two-step process. Journal of Sleep Research. 2017;26(3):364–370. doi: 10.1111/jsr.12510. [DOI] [PubMed] [Google Scholar]
- Fullana M.A., Hidalgo-Mazzei D., Vieta E., Radua J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. Journal of Affective Disorders. 2020;275:80–81. doi: 10.1016/j.jad.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallotti R., Valle F., Castaldo N., Sacco P., De Domenico M. Assessing the risks of ‘infodemics’ in response to COVID-19 epidemics. Nature Human Behaviour. 2020;4(12):1285–1293. doi: 10.1038/s41562-020-00994-6. [DOI] [PubMed] [Google Scholar]
- Gao C., Scullin M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Medicine. 2020;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner M.A. Sleep and health. Elsevier; 2019. Epidemiology of insufficient sleep and poor sleep quality; pp. 11–20. [DOI] [Google Scholar]
- Groot Kormelink T., Klein Gunnewiek A. From “far away” to “shock” to “fatigue” to “back to normal”: How young people experienced news during the first wave of the COVID-19 pandemic. Journalism Studies. 2021;1–18 doi: 10.1080/1461670X.2021.1932560. [DOI] [Google Scholar]
- Hayashino Y., Yamazaki S., Takegami M., Nakayama T., Sokejima S., Fukuhara S. Association between number of comorbid conditions, depression, and sleep quality using the Pittsburgh Sleep Quality Index: Results from a population-based survey. Sleep Medicine. 2010;11(4):366–371. doi: 10.1016/j.sleep.2009.05.021. [DOI] [PubMed] [Google Scholar]
- Hayran C., Anik L. Well-being and fear of missing out (FOMO) on digital content in the time of COVID-19: A correlational analysis among university students. International Journal of Environmental Research and Public Health. 2021;18(4):1974. doi: 10.3390/ijerph18041974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. Journal of Clinical Sleep Medicine. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karsay K., Schmuck D., Matthes J., Stevic A. Longitudinal effects of excessive smartphone use on stress and loneliness: The moderating role of self-disclosure. Cyberpsychology, Behavior, and Social Networking. 2019;22(11):706–713. doi: 10.1089/cyber.2019.0255. [DOI] [PubMed] [Google Scholar]
- Koffman J., Gross J., Etkind S.N., Selman L. Uncertainty and COVID-19: How are we to respond? Journal of the Royal Society of Medicine. 2020;113(6):211–216. doi: 10.1177/0141076820930665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraut R., Patterson M., Lundmark V., Kiesler S., Mukophadhyay T., Scherlis W. Internet paradox: A social technology that reduces social involvement and psychological well-being? American Psychologist. 1998;53(9):1017–1031. doi: 10.1037/0003-066X.53.9.1017. [DOI] [PubMed] [Google Scholar]
- Kuy S., Tsai R., Bhatt J., Chu Q.D., Gandhi P., Gupta R., Gupta R., Hole M.K., Hsu B.S., Hughes L.S., Jarvis L., Jha S., Annamalai A., Kotwal M., Sakran J.V., Vohra S., Henry T.L., Correa R. Focusing on vulnerable populations during COVID-19. Academic Medicine. 2020;95(11):e2–e3. doi: 10.1097/ACM.0000000000003571. “Sunny,”. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanaj K., Johnson R.E., Barnes C.M. Beginning the workday yet already depleted? Consequences of late-night smartphone use and sleep. Organizational Behavior and Human Decision Processes. 2014;124(1):11–23. doi: 10.1016/j.obhdp.2014.01.001. [DOI] [Google Scholar]
- Lehman K.A., Burns M.N., Gagen E.C., Mohr D.C. Development of the brief inventory of perceived stress. Journal of Clinical Psychology. 2012;68(6):631–644. doi: 10.1002/jclp.21843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Qin Q., Sun Q., Sanford L.D., Vgontzas A.N., Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. Journal of Clinical Sleep Medicine. 2020;16(8):1417–1418. doi: 10.5664/jcsm.8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luqman A., Masood A., Shahzad F., Shahbaz M., Feng Y. Untangling the adverse effects of late-night usage of smartphone-based SNS among University students. Behaviour & Information Technology. 2020:1–17. doi: 10.1080/0144929X.2020.1773538. [DOI] [Google Scholar]
- Mac Cárthaigh S., Griffin C., Perry J. The relationship between sleep and problematic smartphone use among adolescents: A systematic review. Developmental Review. 2020;55:100897. doi: 10.1016/j.dr.2020.100897. [DOI] [Google Scholar]
- Mihelj S., Kondor K., Štětka V. Audience engagement with COVID-19 news: The impact of lockdown and live coverage, and the role of polarization. Journalism Studies. 2021;1–19 doi: 10.1080/1461670X.2021.1931410. [DOI] [Google Scholar]
- Murdock K.K., Adams S.K., Crichlow-Ball C., Horissian M., Roberts M. Nighttime notifications and compulsivity illuminate the link between emerging adults' cellphone use and sleep-related problems. Psychology of Popular Media Culture. 2019;8(1):12–21. doi: 10.1037/ppm0000156. [DOI] [Google Scholar]
- Ohme J., Vanden Abeele M.M.P., Van Gaeveren K., Durnez W., De Marez L. Staying informed and bridging “social distance”: Smartphone news use and mobile messaging behaviors of flemish adults during the first weeks of the COVID-19 pandemic. Socius: Sociological Research for a Dynamic World. 2020;6 doi: 10.1177/2378023120950190. 237802312095019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olagoke A.A., Olagoke O.O., Hughes A.M. Exposure to coronavirus news on mainstream media: The role of risk perceptions and depression. British Journal of Health Psychology. 2020;25(4):865–874. doi: 10.1111/bjhp.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben A., Przybylski A.K. Teenage sleep and technology engagement across the week. PeerJ. 2020;8 doi: 10.7717/peerj.8427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlikowska T., Chalder T., Hirsch S.R., Wallace P., Wright D.J.M., Wessely S.C. Population based study of fatigue and psychological distress. BMJ. 1994;308(6931):763–766. doi: 10.1136/bmj.308.6931.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepin J.-L., Borel A.-L., Tamisier R., Baguet J.-P., Levy P., Dauvilliers Y. Hypertension and sleep: Overview of a tight relationship. Sleep Medicine Reviews. 2014;18(6):509–519. doi: 10.1016/j.smrv.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B., Nitiéma P., Newman E. The association of mass trauma media contact with depression and anxiety: A meta-analytic review. Journal of Affective Disorders Reports. 2021;3:100063. doi: 10.1016/j.jadr.2020.100063. [DOI] [Google Scholar]
- Przybylski A.K., Murayama K., DeHaan C.R., Gladwell V. Motivational, emotional, and behavioral correlates of fear of missing out. Computers in Human Behavior. 2013;29(4):1841–1848. doi: 10.1016/j.chb.2013.02.014. [DOI] [Google Scholar]
- Rahe C., Czira M.E., Teismann H., Berger K. Associations between poor sleep quality and different measures of obesity. Sleep Medicine. 2015;16(10):1225–1228. doi: 10.1016/j.sleep.2015.05.023. [DOI] [PubMed] [Google Scholar]
- Randjelović P., Stojiljković N., Radulović N., Ilić I., Stojanović N., Ilić S. The association of smartphone usage with subjective sleep quality and daytime sleepiness among medical students. Biological Rhythm Research. 2019;50(6):857–865. doi: 10.1080/09291016.2018.1499374. [DOI] [Google Scholar]
- Reid M., Abdool-Karim Q., Geng E., Goosby E. How will COVID-19 transform global health post-pandemic? Defining research and investment opportunities and priorities. PLoS Medicine. 2021;18(3) doi: 10.1371/journal.pmed.1003564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robillard R., Dion K., Pennestri M., Solomonova E., Lee E., Saad M., Murkar A., Godbout R., Edwards J.D., Quilty L., Daros A.R., Bhatla R., Kendzerska T. Profiles of sleep changes during the COVID‐19 pandemic: Demographic, behavioural and psychological factors. Journal of Sleep Research. 2021;30(1) doi: 10.1111/jsr.13231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robillard R., Saad M., Edwards J.D., Solomonova E., Pennestri M.-H., Daros A., Louis Veissière S.P., Quilty L., Dion K., Nixon A., Phillips J.L., Bhatla R., Spilg E., Godbout R., Yazji B., Rushton C.H., Gifford W., Gautam M., Boafo A., Kendzerska T. Social, Financial and psychological Stress during an emerging pandemic: Observations from a population web-based Survey in the acute phase of the COVID-19 pandemic [preprint] Public and Global Health. 2020 doi: 10.1101/2020.06.29.20142638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rod N.H., Dissing A.S., Clark A., Gerds T.A., Lund R. Overnight smartphone use: A new public health challenge? A novel study design based on high-resolution smartphone data. PLoS One. 2018;13(10) doi: 10.1371/journal.pone.0204811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosekind M.R., Gregory K.B., Mallis M.M., Brandt S.L., Seal B., Lerner D. The cost of poor sleep: Workplace productivity loss and associated costs. Journal of Occupational and Environmental Medicine. 2010;52(1):91–98. doi: 10.1097/JOM.0b013e3181c78c30. [DOI] [PubMed] [Google Scholar]
- Sañudo B., Fennell C., Sánchez-Oliver A.J. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns pre- and during-COVID-19 quarantine in young adults from Spain. Sustainability. 2020;12(15):5890. doi: 10.3390/su12155890. [DOI] [Google Scholar]
- Scarpelli S., Alfonsi V., Mangiaruga A., Musetti A., Quattropani M.C., Lenzo V., Freda M.F., Lemmo D., Vegni E., Borghi L., Saita E., Cattivelli R., Castelnuovo G., Plazzi G., De Gennaro L., Franceschini C. Pandemic nightmares: Effects on dream activity of the COVID‐19 lockdown in Italy. Journal of Sleep Research. 2021 doi: 10.1111/jsr.13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf M.T., Naidoo N., Zimmerman J.E., Pack A.I. The energy hypothesis of sleep revisited. Progress in Neurobiology. 2008;86(3):264–280. doi: 10.1016/j.pneurobio.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott H., Woods H.C. Fear of missing out and sleep: Cognitive behavioural factors in adolescents' nighttime social media use. Journal of Adolescence. 2018;68:61–65. doi: 10.1016/j.adolescence.2018.07.009. [DOI] [PubMed] [Google Scholar]
- Shabahang R., Aruguete M.S., Shim H. Online news addiction: Future anxiety, fear of missing out on news, and interpersonal trust contribute to excessive online news consumption. Online J. Commun. Media Technol. 2021;11(2):e202105. doi: 10.30935/ojcmt/10822. [DOI] [Google Scholar]
- Simonelli G., Marshall N.S., Grillakis A., Miller C.B., Hoyos C.M., Glozier N. Sleep health epidemiology in low and middle-income countries: A systematic review and meta-analysis of the prevalence of poor sleep quality and sleep duration. Sleep Health. 2018;4(3):239–250. doi: 10.1016/j.sleh.2018.03.001. [DOI] [PubMed] [Google Scholar]
- Slater M.D. Reinforcing spirals model: Conceptualizing the relationship between media content exposure and the development and maintenance of attitudes. Media Psychology. 2015;18(3):370–395. doi: 10.1080/15213269.2014.897236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwinski M.J. Measurement-burst designs for social health research: Longitudinal measurement-burst design. Social and Personality Psychology Compass. 2008;2(1):245–261. doi: 10.1111/j.1751-9004.2007.00043.x. [DOI] [Google Scholar]
- Song H., Jung J., Kim Y. Perceived news overload and its cognitive and attitudinal consequences for news usage in South Korea. Journalism & Mass Communication Quarterly. 2017;94(4):1172–1190. doi: 10.1177/1077699016679975. [DOI] [Google Scholar]
- Spira A.P., Chen-Edinboro L.P., Wu M.N., Yaffe K. Impact of sleep on the risk of cognitive decline and dementia. Current Opinion in Psychiatry. 2014;27(6):478–483. doi: 10.1097/YCO.0000000000000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stainback K., Hearne B.N., Trieu M.M. COVID-19 and the 24/7 news cycle: Does COVID-19 news exposure affect mental health? Socius: Sociological Research for a Dynamic World. 2020;6 doi: 10.1177/2378023120969339. 237802312096933. [DOI] [Google Scholar]
- Valkenburg P.M., Peter J. The differential susceptibility to media effects model: Differential susceptibility to media effects model. Journal of Communication. 2013;63(2):221–243. doi: 10.1111/jcom.12024. [DOI] [Google Scholar]
- Van den Bulck J. Adolescent use of mobile phones for calling and for sending text messages after lights out: Results from a prospective cohort study with a one-year follow-up. Sleep. 2007;30(9):1220–1223. doi: 10.1093/sleep/30.9.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenberg R.J., Lance C.E. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods. 2000;3(2000):4–70. doi: 10.1177/109442810031002. [DOI] [Google Scholar]
- Vorderer P., Hefner D., Reinecke L., Klimmt C., editors. Permanently online, permanently connected: Living and communicating in a POPC world. Routledge; 2017. [Google Scholar]
- Watson N.F., Badr M.S., Belenky G., Bliwise D.L., Buxton O.M., Buysse D., Dinges D.F., Gangwisch J., Grandner M.A., Kushida C., Malhotra R.K., Martin J.L., Patel S.R., Quan S.F., Tasali E. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American academy of sleep medicine and sleep research society. Journal of Clinical Sleep Medicine. 2015;11(6):591–592. doi: 10.5664/jcsm.4758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegmann E., Oberst U., Stodt B., Brand M. Online-specific fear of missing out and Internet-use expectancies contribute to symptoms of Internet-communication disorder. Add. Behav. Rep. 2017;5:33–42. doi: 10.1016/j.abrep.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu S.-C., Chen H.-R., Liu A.-C., Lee H.-Y. Toward COVID-19 information: Infodemic or fear of missing out? Healthcare. 2020;8(4):550. doi: 10.3390/healthcare8040550. [DOI] [PMC free article] [PubMed] [Google Scholar]