Abstract
Background
The COVID-19 pandemic has led to increased stress, anxiety, and depression in children. A six-session, parent-led, transdiagnostic, cognitive-behavioral teletherapy program was adapted from an established protocol to help youth aged between 5 and 13 years manage emotional problems during the pandemic.
Methods
One-hundred twenty-nine parents of youth struggling with emotional problems during the COVID-19 pandemic participated in the program. Parents reported on their children's psychosocial functioning before and after treatment using validated assessments. They also reported on treatment satisfaction. Clinician-rated global improvement was assessed at each session to determine clinically significant treatment response.
Results
Significant improvements in parent proxy-reported anxiety (d = 0.56), depression (d = 0.69), stress (d = 0.61), anger (d = 0.69), family relationships (d = 0.32), and COVID-19-related distress (d = 1.08) were found, with 62% of participants who completed the program being classified as treatment responders. Parents reported high levels of satisfaction with the program.
Limitations
This study was limited by use of primarily parent-report assessments and a lack of a control group.
Conclusions
Brief, parent-led, transdiagnostic cognitive-behavioral teletherapy appeared to be an effective way to help youth cope with the pandemic and may be a scalable framework in response to large-scale mental health crises.
Keywords: CBT, Unified protocol, Internalizing, Depression, Anxiety, Children
1. Introduction
The COVID-19 pandemic has changed nearly every aspect of daily life for children and families. Mandated social distancing, school closures, transitions to online learning, and general stress related to the pandemic have led to increasing depression (Al Omari et al., 2020; Hawes et al., 2021; Magson et al., 2021; Mayne et al., 2021; Racine et al., 2021), anxiety (Al Omari et al., 2020; Hawes et al., 2021; Magson et al., 2021; Orgilés et al., 2020; Racine et al., 2021), stress (Al Omari et al., 2020), irritability (Orgilés et al., 2020), family conflict (Roos et al., 2021), and COVID-19-related distress (Magson et al., 2021) in youth. Developing and disseminating psychological therapies that are scalable and grounded in evidence-based principles has been an important task for mental health professionals during this time.
Several factors should be considered when developing treatments for youth who have struggled with emotional problems during the pandemic. First, a transdiagnostic approach that addresses overlapping vulnerabilities across internalizing disorders such as anxiety and depression has a growing evidence base (Marchette and Weisz, 2017) and may be particularly well suited to this population, as children have experienced a range of emotional reactions to the COVID-19 pandemic, including loneliness, irritability, anxiety, and depressed mood (Al Omari et al., 2020; Hawes et al., 2021; Magson et al., 2021; Mayne et al., 2021; Orgilés et al., 2020). In particular, the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP) is a form of cognitive-behavioral therapy (CBT) that conceptualizes “emotional disorders” through shared vulnerabilities and targets common underlying mechanisms of internalizing psychopathology (e.g., rumination, emotional avoidance, and underutilization of adaptive cognitive strategies; Barlow et al., 2010; Ehrenreich-May et al., 2017a). This approach uses cognitive-behavioral techniques such as behavioral activation, exposure, cognitive reappraisal, and mindfulness to address these issues, and has been adapted for both children (ages 7–13; UP-C; Kennedy, Bilek; and Ehrenreich-May 2019) and adolescents (UP-A; Ehrenreich-May et al., 2017a).
Although the UP has demonstrated efficacy for youth with internalizing disorders (Ehrenreich-May et al., 2017b; Kennedy et al., 2019), many children and adolescents still experience barriers to accessing efficacious mental health services. Brief models of care may provide an approach to overcome service delivery barriers. Brief therapy matches what is often delivered in primary care, schools, and/or community mental health settings and is often efficacious in its own right (Schleider and Weisz, 2017; Weersing et al., 2017). These approaches are particularly useful and feasible for systems that have the potential to reach large pediatric populations, as they use resources more efficiently compared to longer CBT protocols that are usually tested in clinical trials. Brief, parent-led, therapist-assisted interventions in particular have the potential to be a cost-effective way to promote evidence-based therapy, as parents are often more motivated to seek help for their children's emotional problems than children themselves (Thurston and Phares, 2008). Parent-led CBT can empower parents to more effectively incorporate strategies into daily life in “real time,” target specific parenting behaviors in addition to child behaviors, and may be more durable due to parents’ increased likelihood of implementing strategies after therapy is over (Creswell et al., 2019). This approach also provides support for parents who may experience heightened parenting stress (Creswell et al., 2019). Finally, parent-led approaches can reduce overall therapy time (e.g., for children who are more ambivalent about participating in therapy or require more time to develop rapport and trust with a therapist; Creswell et al., 2019; Kazdin, 2019). Parent-led, therapist-assisted CBT has been found to be equally effective as therapist-led therapy for youth with anxiety disorders and is often delivered remotely via telehealth (McKinnon et al., 2018), a delivery format that has been widely and rapidly adopted during the pandemic in response to public health calls for physical distancing (Perrin et al., 2020).
Although a number of clinical trials testing psychosocial treatments for emotional stress during the pandemic are underway (Boldt et al., 2021), clinical effectiveness data of these programs on psychological symptoms are limited. Preliminary findings from a mindfulness training program in China revealed an increase in resilience and emotional intelligence in adolescents during the pandemic (Yuan, 2021). Additionally, a mobile phone application encouraging social connection helped reduce anxiety and eye-strain (Zheng et al., 2021). Two studies reported on parenting interventions designed to improve parenting stress; in one, military veteran parents reported significant reductions in depression, parenting stress, and family dysfunction after participating in a parenting-oriented teletherapy intervention (James Riegler et al., 2020). In the other, single session cognitive reappraisal and self-compassion interventions were compared with a waitlist control, finding that cognitive appraisal was more effective at reducing stress in parents compared with a waitlist (Preuss et al., 2021). The goal of this study was to evaluate the effectiveness and acceptability of a brief, parent-led, therapist-assisted, transdiagnostic cognitive-behavioral teletherapy program called “Coping with COVID” for youth struggling with emotional problems during the pandemic. To our knowledge, this is the first report on effectiveness of a CBT intervention to ameliorate COVID-19-related distress among youth.
We evaluated the preliminary effectiveness of Coping with COVID by examining changes in parent-reported assessments of anxiety, depression, stress, anger, family relationships, and COVID-19-related distress. Rates of clinical improvement were also evaluated and benchmarked against a prior trial of the UP-C using the same assessment of clinically significant improvement (Kennedy et al., 2019). Treatment satisfaction and attrition were described.
2. Methods
2.1. Procedures
From July 2020 to May 2021, the Coping with COVID program was advertised through online social media platforms, school and community presentations, local news coverage, and word-of-mouth to parents of youth in Houston, Texas and surrounding areas. Social media platforms included Facebook and Reddit groups that were dedicated to caregivers, educators, and allied health professionals based in Texas and focused on the topics of mental health and/or COVID-19. Interested participants would call or email program coordinators to be introduced to the program and were screened for fit (see “Participants” section) over the phone. After a family was determined to be eligible through this phone screening process, parents were asked to complete consent forms for participating in Coping with COVID and receiving telehealth treatment prior to the first session. Families were provided referrals if they were determined not a good fit for the program. The (BLINDED) Institutional Review Board approved the retrospective collection and analysis of patients’ de-identified data for the purposes of evaluating the effectiveness of the program. A waiver of consent was obtained for this study to review the questionnaire data from patient charts. This study was a retrospective analysis of questionnaire data evaluating the effectiveness of the program and was approved by the (BLINDED) Institutional Review Board.
2.2. Participants
Participants were caregivers of youth aged between 5 and 13 years. The primary inclusion criterion was that the child struggled with a primary problem of mild to moderate emotional and/or behavioral concerns such as stress, anxiety, sadness, or loneliness, related to or exacerbated by the COVID-19 pandemic, as assessed by the intake clinician. Formal clinical diagnoses were not a requirement for inclusion. Other inclusion criteria included: families resided in the state of Texas; caregivers had to be the parent or legal guardian of the identified child and be able to read and understand English; and children also had to be able to communicate verbally. Exclusion criteria for the program, assessed first by program coordinators via a 45 min phone screen and then intake clinicians, included severe developmental or intellectual disability or severe psychological distress in need of more intensive services (e.g., youth with active suicidality). Parents were asked about a history of an autism spectrum disorder, bipolar disorder, psychotic disorder, conduct disorder, or oppositional defiant disorder diagnosis. If they endorsed a history of one of these diagnoses, they were considered for inclusion on a case-by-case basis by the intake clinician depending on assessed level of acuity.
2.3. Treatment
The parent-led CBT protocol included six weekly sessions that occurred via videoconferencing and was based on the UP-C and UP-A (Ehrenreich-May et al., 2017a). The program taught parents to implement CBT skills with their children and also provided guidance in designing specific CBT exercises (e.g., brainstorming behavioral activation activities that would be helpful for a given child). The first session focused on goal-setting and psychoeducation related to emotions from a cognitive-behavioral perspective (e.g., functional role of avoidance, breaking down emotional experiences into thoughts, physical sensations, and behaviors). The second session focused on psychoeducation and planning of transdiagnostic, parent-led emotion exposures (i.e., including traditional anxiety-focused exposure or exposures addressing irritability or low mood). The third was focused on continued exposure planning, as well as psychoeducation regarding “emotional parenting behaviors,” or parenting behaviors associated with childhood internalizing symptoms, including overcontrol/overprotection/accommodation, criticism, inconsistency, and modeling of inappropriate reactions to strong emotions (often avoidance). This session also included “opposite parenting behaviors” to counter emotional parenting behaviors. The fourth included continued exposure, behavioral activation activity planning, and opposite parenting behaviors. The fifth session continued exposure and included mindfulness/present-moment awareness exercises parents could teach their children and use in their own parenting. The final session focused on guiding parents in helping their children identify “thinking traps” or cognitive distortions and think more flexibly via cognitive reappraisal (i.e., generating alternative interpretations of situations perceived as threatening, stressful, or otherwise upsetting). Clinicians adapted exercises to ensure adherence to public health guidance related to the COVID-19 virus (for example, planning more outdoor activities for behavioral activation; considering social anxiety exposure for the virtual classroom such as wearing an “embarrassing” article of clothing during virtual school).
Sessions were provided over a HIPAA-compliant videoconferencing platform (Zoom) by advanced doctoral students in counseling/school psychology who focused on children and adolescents. Questionnaires data were entered via Qualtrics. Therapists were trained by developers of the UP-C and UP-A via readings, interactive didactics, and weekly case consultations to ensure strong adherence to the protocol. They also had weekly licensed supervision.
2.4. Measures
2.4.1. Spence children's anxiety scale
The parent-report Spence Children's Anxiety Scale (SCAS) was used to assess anxiety (Spence, 1998). The measure, which has been normed for youth aged seven to 17 years, shows strong convergent and divergent validity, accurate diagnostic predictive validity, and strong internal consistency (Ramme, 2018). It includes 38 items scored on a 0–3 (never-always) Likert scale. The total score was used for this study (α = 0.89).
2.4.2. Patient-reported outcomes measurement information system (PROMIS) parent-proxy questionnaires
The PROMIS measures are brief questionnaires developed to track clinical progress (Irwin et al., 2012). Candidate items for each questionnaire were generated based on comprehensive literature searches and focus groups. Final measures, defined through psychometric testing following an item response theory framework, constitute a clear latent factor, capture a full range of severity, and are normed with clinical and nonclinical youth. The PROMIS Parent Proxy Short Form- V2.0 – Depressive Symptoms 6a (Varni et al., 2012); Anger 5a (Varni et al., 2012); Psychological Stress Experiences 8a (Bevans et al., 2018); and Family Relationships 8a (Bevans et al., 2017) were administered before and after treatment. They each showed good internal consistency (Depressive Symptoms: α = 0.92; Anger: α = 0.86; Stress: α = 0.91; Family Relationships: α = 0.86).
2.4.3. COVID-Thoughts and behavioral symptoms
The parent proxy-rated COVID-Thoughts and behavioral symptoms scale (COV-TaBS) was used to assess children's COVID-19-related distress before and after treatment (Schneider et al., 2020). The measure was developed by a team of child psychologists based on preliminary observations during the pandemic. Items assess reactions such as loneliness, fears, and safety behaviors. Distribution of responses to each item are presented in Supplemental Table 1. Items showed adequate internal consistency at pre- (α = 0.78) and post-treatment (α = 0.83).
2.4.4. COVID-19 exposure and impacts questionnaire
Items from the COVID-19 Exposure and Impacts Questionnaire (CEIQ; Schneider et al., 2021) recorded pandemic-related events and emotional responses that a child may have experienced, including social distancing/school closures/other social impacts, fears and worries, feeling generally bad or upset, financial issues, separation from a caregiver, having a loved one seriously ill from COVID-19, having a loved one die from COVID-19, and contracting COVID-19. Parents were also asked to indicate whether each of these was perceived to have a significant impact on emotional functioning.
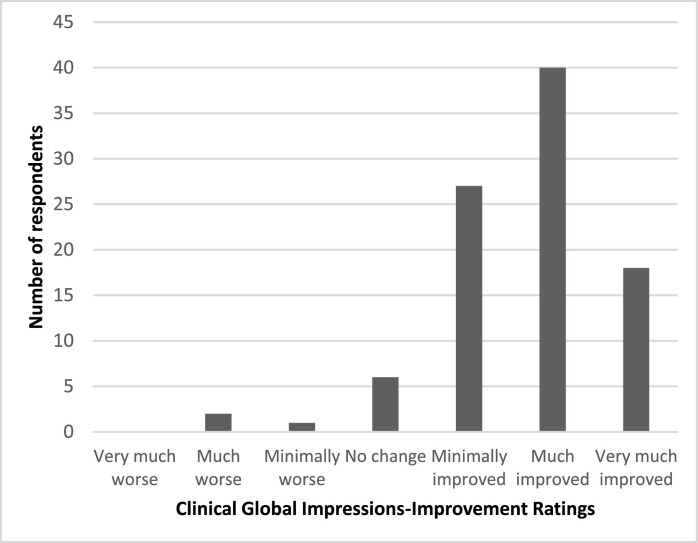
2.4.5. Clinical improvement
Clinical improvement was assessed each session by clinicians using the Clinical Global Impressions-Improvement Scale (CGI-I) (Guy, 1976), which assesses improvement on a 1 (very much improved) to 7 (very much worse) scale. Clinician-rated CGI-I ratings have been shown to have strong convergent validity with blinded assessor-rated CGI-I ratings (Lewin et al., 2012).
2.4.6. Satisfaction
Six items were developed specifically for this study to evaluate satisfaction with the program. At the conclusion of the program, parents were asked to rate six statements regarding their experience of the program on a four-point (0 to 3) Likert scale with the following anchors: “Not at all true,” “Somewhat true,” “Mostly true,” and “True to a great extent.” Responses to each of the items are summarized in Table 5.
2.5. Analysis plan
There were no missing data for the primary outcome questionnaires at pre-treatment (SCAS, PROMIS scales, COV-TaBS), with the exception of the SCAS for four families (3%). CEIQ items were missing for seven families (5%). Little's test suggested pre-treatment data were missing completely at random (χ2 = 28.72, p = .071). CGI-I ratings were available for 114 families (12%). For families who completed the program, two SCAS questionnaires (2%) as well as one each for the PROMIS-Stress and PROMIS-Family Relationships questionnaires (1%) were missing at post-treatment. Post-treatment data were also missing completely at random (χ2 = 12.19, p = .20).
Demographics, clinical characteristics, COVID-19-related impact, and presenting concerns of families attending the Coping with COVID program were first presented. Changes in the SCAS, PROMIS measures, and COV-TaBS were evaluated using within-subjects t-tests. Clinical improvement was determined with a last-recorded CGI-I score of 1 or 2, indicating “much improved” or “very much improved.” Parental satisfaction and impressions of improvement were also presented. Finally, we evaluated whether COVID-19-related stressors impacted psychosocial outcomes using linear regression predicting post-treatment scores when controlling for pre-treatment scores. For all analyses, two-tailed significance tests were conducted with a significance threshold of p < .01 to account for the multiple primary outcomes in this study.
3. Results
3.1. Sample characteristics
A total of 167 parent-child dyads expressed interest in the program, called the intake coordinators, and completed at least some initial questionnaires. Of those families, 129 initiated treatment. One hundred and two completed the program, with 27 dropping out (21%). There were no significant differences between completers and dropouts in pre-treatment SCAS, PROMIS-Depression, PROMIS-Anger, PROMIS-Stress, PROMIS-Family Relationships, or in the COV-TaBS measure (ps > 0.69).
The program began in July 2020, and the first four months was the most common time for families to initiate treatment. As a point of reference, July-August was considered to be the first major “wave” of COVID-19 in Texas, with 7-day new case average of 10,461 peaking on July 19 (Tracking Coronavirus in Texas: Latest Map and Case Count [WWW Document], 2021). The second wave peaked on January 16, 2021, with a 7-day new case average of 22,983 (Tracking Coronavirus in Texas: Latest Map and Case Count [WWW Document], 2021). The mean age of children was 8.5 years (SD = 2.5). Most caregivers were mothers (92%). The majority of parents stated that their child identified as White (78%). There was an approximately equal split between male and female youth. Most families reported an annual household income of at least $80,000/year (71%). The most common presenting concern among children reported by parents was anxiety. Other common concerns included anger, stress, and sadness. See Table 1 for a summary of demographic characteristics of the full sample who participated in the Coping with COVID program.
Table 1.
Demographics.
| Full sample participating in treatment (n = 129) | Dropped out (n = 27) | Completed therapy (n = 102) | |
|---|---|---|---|
| Started therapy, N (%) a | |||
| July-October 2020 | 67 (52%) | 12 (44%) | 55 (54%) |
| November 2020-February 2021 | 44 (34%) | 10 (37%) | 34 (33%) |
| March-May 2021 | 18 (14%) | 5 (19%) | 13 (13%) |
| Primary concern at baseline, N (%) b | |||
| Anxiety | 96 (74%) | 20 (74%) | 76 (75%) |
| Stress | 55 (43%) | 9 (33%) | 46 (45%) |
| Sleep problems | 44 (34%) | 8 (30%) | 36 (35%) |
| Sadness | 52 (40%) | 10 (37%) | 42 (41%) |
| Anger | 60 (47%) | 12 (44%) | 48 (47%) |
| Disruptiveness | 35 (27%) | 10 (37%) | 25 (24%) |
| Treatment history, N (%) | |||
| Psychotherapy | 39 (30%) | 9 (33%) | 30 (29%) |
| Medication | 16 (12%) | 5 (19%) | 11 (11%) |
| Age, M (SD) | 8.7 (2.5) | 8.8 (2.7) | 8.7 (2.5) |
| Child Gender, N (%) | |||
| Male | 64 (50%) | 16 (59%) | 48 (47%) |
| Female | 65 (50%) | 11 (41%) | 54 (53%) |
| Child Hispanic/Latinx Ethnicity, N (%) | 40 (31%) | 9 (33%) | 31 (30%) |
| Race, N (%) | |||
| Asian | 20 (16%) | 4 (15%) | 16 (16%) |
| Black or African American | 13 (10%) | 1 (4%) | 12 (12%) |
| White | 101 (78%) | 23 (85%) | 78 (77%) |
| Other | 15 (12%) | 2 (7%) | 13 (13%) |
| Household income | |||
| $10,000–39,999 | 6 (5%) | 4 (15%) | 2 (2%) |
| $40,000–79,999 | 31 (24%) | 6 (22%) | 25 (25%) |
| $80,000 and over | 91 (71%) | 17 (63%) | 74 (73%) |
| Guardian relationship | |||
| Mother | 119 (92%) | 26 (96%) | 93 (91%) |
| Father | 7 (5%) | 1 (4%) | 6 (6%) |
| Grandmother | 1 (1%) | 0 (0%) | 1 (1%) |
| Proportion elevated (T score ≥ 65) | |||
| Spence Child Anxiety Scale | 37 (29%) | 9 (33%) | 28 (28%) |
| PROMIS-Depression | 33 (26%) | 10 (37%) | 23 (23%) |
| PROMIS-Anger | 48 (37%) | 12 (44%) | 36 (35%) |
| PROMIS-Stress | 56 (43%) | 15 (55%) | 41 (40%) |
| At least one measure elevated | 84 (65%) | 19 (70%) | 65 (64%) |
Recruitment periods are divided into three roughly even periods for interpretability.
parents could select multiple options for primary concerns
Note: PROMIS= Patient-Reported Outcomes Measurement Information System.
The vast majority of the sample described multiple COVID-19 impacts, with the most common being social distancing, school closures, and related social impacts (97%), generally feeling bad or upset due to the pandemic (89%), and experiencing fears and worries related to COVID-19 (85%). Impacts are listed in Table 2 .
Table 2.
COVID-19-related impacts.
| Full sample participating in treatment (n = 122)* |
Treatment completers (n = 97)* |
|||
|---|---|---|---|---|
| Impact occurred | Impact occurred and was described as significant | Impact occurred | Impact occurred and was described as significant | |
| Social distancing, school closures, and other impacts | 118 (97%) | 109 (89%) | 93 (96%) | 85 (88%) |
| Experiencing fears and worries | 104 (85%) | 84 (69%) | 82 (85%) | 67 (69 |
| Feeling bad or upset | 109 (89%) | 88 (72%) | 87 (90%) | 70 (72%) |
| Financial issues | 33 (26%) | 14 (11%) | 25 (26%) | 9 (9%) |
| Separated from caregiver | 71 (55%) | 59 (48%) | 56 (58%) | 45 (46%) |
| Loved one seriously ill from COVID-19 | 34 (28%) | 22 (18%) | 26 (27%) | 18 (19%) |
| Loved one died from COVID-19 | 8 (7%) | 5 (4%) | 6 (6%) | 4 (4%) |
| Child contracted COVID-19 | 4 (3%) | 3 (2%) | 4 (4%) | 3 (3%) |
Seven total families did not complete the COVID-19 Experiences and Impacts Questionnaire, including five who completed the program.
The most frequently cited COVID-19-related thoughts and behavioral symptoms were: feeling alone or missing people, being very careful to stay clean, and hiding from COVID-19. At baseline, the mean item response was 1.80 (SD=0.67), indicating the thought or behavior was experienced between “A little” and “Sometimes.” Please see Supplemental Table 1 for a summary.
3.2. Change across treatment
Significant improvements in all outcomes were observed across treatment, including on the, SCAS, and PROMIS-Depression, Stress, Anger, and Family Relationships scales and COV-TaBS. The magnitude of these effects was generally in the medium range following Cohen's recommended effect size interpretation (Cohen, 1992), with the exception of the COV-TaBS, which showed a large effect, and the PROMIS-Family Relationships, which showed small improvements. Table 3 summarizes the changes in psychosocial outcomes across the Coping with COVID clinical program.
Table 3.
Changes in psychosocial outcomes across the Coping with COVID program.
| M (SD)pre | M (SD)post | t | d | |
|---|---|---|---|---|
| SCAS | 59.4 (7.9) | 55.5 (8.2) | 5.60*** | 0.56 |
| PROMIS-Depression | 59.2 (9.1) | 53.0 (9.0) | 7.01*** | 0.69 |
| PROMIS-Anger | 58.4 (11.3) | 50.7 (11.5) | 6.97*** | 0.69 |
| PROMIS-Stress | 62.6 (9.2) | 57.0 (9.4) | 6.17*** | 0.61 |
| PROMIS-Family Relationships | 45.1 (8.0) | 47.3 (8.3) | −3.21** | −0.32 |
| COV-TaBS | 1.72 (0.65) | 0.96 (0.64) | 10.99*** | 1.06 |
**p < .01; ***p < .001.
Note: All measures are expressed in norm-referenced standard T scores (M = 50; SD = 10) except for the COV-TaBS, which is expressed as an item-level mean, as well as the PROMIS-Family Relationships measure, for which norms were not available for the full range of scores reported in this sample.
Sixty-two percent of youth who completed the program were classified as responders based on CGI-I ratings of “much improved” or “very much improved.” For intent-to-treat analyses, 55% were classified as responders. These response rates were compared with 71% for completers and 63% for intent-to-treat in a randomized controlled trial of the UP-C involving 15 90-minute sessions with youth with clinical diagnoses (Kennedy et al., 2019). Please see Fig. 1 for a summary of CGI-I responses from completers.
Fig. 1.
Clinician Global Impressions-Improvement (CGI-I) ratings from last appointment (n = 94).
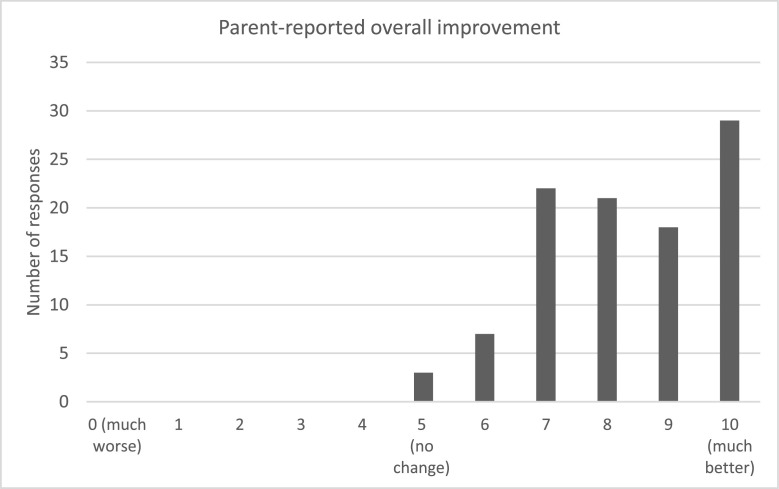
Parents were prompted to rate their child's improvement on a scale of 0 to 10 following the program, with 0 indicating “much worse,” 5 indicating “no change,” and 10 as “much better,” The mean parental response was 8.3 (SD = 1.4). The most frequently endorsed response was 10. Range of scores is displayed in Fig. 2 .
Fig. 2.
Responses to item that asked parents “Please select a number between 0 and 10 indicating the degree of change since receiving treatment through Coping with COVID” (n = 101).
3.3. Feasibility and acceptability
The majority of parents believed that it was “true to a great extent” that the program helped them learn new parenting skills (76%), were satisfied overall with services (87%), and would recommend the program to families with similar problems (94%), with all families in the program endorsing these statements as at least “somewhat true.” All items indicated high overall satisfaction. The dropout rate was 21%, compared with a mean dropout rate of 26% in CBT across format, and compared with a mean dropout rate of 34% in CBT teletherapy as identified by a meta-analysis (Fernandez et al., 2015). Table 4 includes a summary of responses to all satisfaction post-treatment survey items in Table 4.
Table 4.
Satisfaction with Coping with COVID program (n = 101).
| Not at all true | Somewhat true | Mostly true | True to a great extent | |
|---|---|---|---|---|
| I feel as though my child's top problems have meaningfully improved since the screening. | 2 (2%) | 18 (18%) | 36 (35%) | 45 (44%) |
| I have learned new parenting strategies to help my child express and manage their emotions. | 0 (0%) | 4 (4%) | 19 (19%) | 78 (77%) |
| My child has improved their ability to express and manage their emotions. | 1 (1%) | 36 (35%) | 36 (35%) | 28 (28%) |
| I feel that the number of sessions was adequate. | 3 (3%) | 20 (20%) | 40 (39%) | 38 (37%) |
| My child and I are satisfied with the overall services provided by Coping with COVID. | 0 (0%) | 4 (4%) | 8 (8%) | 89 (87%) |
| I would recommend this program to others with similar problems. | 0 (0%) | 2 (2%) | 3 (3%) | 96 (94%) |
3.4. Predicting post-treatment scores from COVID impact
COVID-19 impacts, including being infected or knowing someone seriously ill from COVID, experiencing financial stress, and being separated from a caregiver, were not associated with post-treatment outcomes (SCAS, PROMIS-Depression, PROMIS-Anger, PROMIS-Stress, PROMIS-Family Relationships, COV-TaBS) when controlling for pre-treatment scores. A loved one dying or the child being infected with COVID-19 were not included as predictors because there were small subsets of youth who experienced these impacts (6% and 4%, respectively), and thus the analysis was not powered to detect these effects. Please see Supplemental Table 2 for a summary of model parameters for linear regressions summarizing these analyses.
4. Discussion
This study investigated a brief, parent-led, therapist-assisted cognitive-behavioral teletherapy program adapted from the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders in Children (UP-C) that was designed to address emotional problems in youth during the COVID-19 pandemic. To our knowledge, this was the first report of effectiveness outcomes of CBT for COVID-19-related distress in children. Results provide strong preliminary support for the acceptability and effectiveness of this approach. Parent proxy-rated anxiety, depression, stress, anger, family relationship quality, and COVID-19-related distress all improved significantly following program participation, with 62% of youth estimated to be treatment responders after six sessions. Treatment outcome did not differ for families with different levels of COVID-19-related impacts. Parents also reported a high degree of satisfaction with the program and high rates of perceived improvement in their children's’ overall emotional functioning. The dropout rate (21%) was less than the estimated dropout rate typically observed in CBT (26.2%, 95% CIs [23.1%, 29.7%]), especially when compared with telehealth dropout rates (34.2%, 95% Cis [22.5%, 48.3%]) based on a prior meta-analysis (Fernandez et al., 2015).
The COVID-19 pandemic has placed an enormous mental health burden on children and families, leading to increased depression, anxiety, stress, irritability, and family conflict in addition to COVID-specific fears, worries, and isolation (Al Omari et al., 2020; Hawes et al., 2021; Magson et al., 2021; Mayne et al., 2021; Orgilés et al., 2020; Racine et al., 2021; Roos et al., 2021). A transdiagnostic CBT telehealth protocol with a strong focus on exposure and behavioral activation techniques appeared to be an effective way to reach youth who were struggling with a range of emotional reactions during the pandemic, and it is likely that the flexible approach used in the UP-C was particularly well suited to address these diverse needs. Ealy intervention has been proposed as a way to improve mental health trajectories in response to disasters, and it is likely that this treatment program served a timely, protective role in the wake of the pandemic for at-risk youth (Goldmann and Galea, 2014). An estimated 62% of youth who completed the full program were classified as treatment responders, as well as 55% of youth who completed at least two sessions. These results are encouraging when compared to response rates of 71% for completers and 63% for intent-to-treat samples in a randomized controlled trial of the full UP-C using the same assessment of treatment response (Kennedy et al., 2019). Notably, Kennedy et al. (2019) included a sample with clinical diagnoses and high comorbidity rates, which was not fully assessed in this study.
In community settings where behavioral health services are often provided (e.g., primary care, community mental health centers, schools), brief models of care are often the standard, as these settings may not have the ability to provide more extended psychotherapy. For this reason, the six-session, parent-led UP-C program described in this report may be a scalable model for these settings and thus may have the potential to reach many families. It is also worth noting that effect sizes were consistently medium for psychological symptom scales but were notably larger for COVID-19-specific concerns. This finding may suggest that this approach would be similarly effective in response to other widespread stressors in the future.
The primary techniques used in this program were exposure therapy and behavioral activation, two central approaches in CBT for internalizing disorders (Weersing et al., 2017; Whiteside et al., 2020). Many productive exposure or behavioral activation exercises that are used during normal times have directly contradicted public health guidelines during the pandemic (e.g., scheduling social activities for individuals struggling with loneliness, touching objects perceived to be “contaminated” for those with contamination fears). This has challenged cognitive-behavioral therapists to think creatively about designing exercises that will promote corrective learning during exposure or contact with positive reinforcers during behavioral activation. For example, parents in the Coping with COVID Program may have coached their children in showing their face or speaking during virtual school or walk around their neighborhood wearing something “embarrassing” for social exposures (Khan et al., 2021), or identified contamination-based exposures to challenge behaviors that go far beyond public health recommendations and/or target non-COVID-19-related fears (Palo and D'Souza, 2021). While youth are more isolated than they were before the pandemic, parents were still encouraged to maintain social contact with peers through outdoor, socially distant gatherings with friends, arranging time with extended family, or finding “quarantine pods.” Indeed, loneliness was the most frequently cited COVID-19-related problem for youth in this sample, underscoring the importance of thinking creatively about socially focused behavioral activation during the pandemic. Thus, the promising outcomes reported here suggest that Coping with COVID therapists were likely able to design effective behavioral exercises even within the limitations set by the COVID-19 pandemic.
Limitations to this study should be noted. First, a lack of a control group prohibits conclusions about efficacy of the program. At least one study shows declines in depression and anxiety in children across the pandemic after initial increases in these symptoms (Hawes et al., 2021). Indeed, COVID-19-related restrictions relaxed in the greater Houston area across the duration of the program, and emotional symptoms may have improved with these changes. Further, many families were recruited during the peak of the July-August wave in the area, and thus youth may have experienced improved emotional symptoms as community outbreak of COVID-19 decreased during their course of treatment. Another limitation was the use of primarily parent-reported assessments and a psychometrically unvalidated COVID-19-related distress measure (COV-TaBS), as when we initiated the study, COVID-19 distress measures for youth had not been published. Including both clinician-rated and child-report measures would have provided more reliable results, as parents may have over- or under-estimated symptom severity across timepoints. Finally, 78% of families identified as White, and 69% as non-Hispanic; although this is more diverse than what is typically observed in clinical trials, these results may not translate to more racially and socioeconomically diverse populations, who have been disproportionately affected by the pandemic.
5. Conclusions
Brief, parent-led, therapist-assisted transdiagnostic cognitive-behavioral teletherapy appears to be a promising option for youth who struggle with emotional problems during the COVID-19 pandemic. Future work should continue to consider similar approaches in response to large-scale crises like the COVID-19 pandemic and in systems that aim to serve large numbers of children and families.
Declaration of Competing Interest
Andrew Guzick receives grant support from the Texas Higher Education Coordinating Board and the Milken Institute/REAM Foundation. Eric Storch receives grant support from NIH, the REAM Foundation, Greater Houston Community Foundation, International OCD Foundation, and Texas Higher Education Coordinating Board. He receives book royalties from Elsevier, Springer, American Psychological Association, Jessica Kingsley, Oxford, and Lawrence Erlbaum. He was a consultant for Levo Therapeutics; he currently consults for Biohaven. He owns stock in NView. Schneider received grant funding from the Texas Higher Education Coordinating Board, the American Red Cross, and the Ream Foundation. Alison Salloum's receives grant support from Patient-Centered Outcomes Research Institute, The Norwegian center for Violence and Traumatic Stress Studies, Department of Education, Office of Special Education and Rehabilitative Services, NIMH and royalties from Taylor and Francis. Further, Salloum is a co-author of Stepping Together, a treatment manual used in stepped care TF-CBT, and holds a licensing agreement with Guilford Press for adaptation of some of the handouts and worksheets in the manual. Salloum is also a national trainer for TF-CBT. All other authors declare that they have no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2022.01.034.
Appendix. Supplementary materials
References
- Al Omari O., Al Sabei S., Al Rawajfah O., Abu Sharour L., Aljohani K., Alomari K., Shkman L., Al Dameery K., Saifan A., Al Zubidi B., Anwar S., Alhalaiqa F. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: an online cross-sectional multicountry study. Depress. Res. Treat. 2020 doi: 10.1155/2020/8887727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow D.H., Ellard K.K., Fairholme C.P., Boisseau C.L. Oxford University Press; USA: 2010. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Workbook. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevans K.B., Gardner W., Pajer K.A., Becker B., Carle A., Tucker C.A., Forrest C.B. Psychometric evaluation of the PROMIS® pediatric psychological and physical stress experiences measures. J. Pediatr. Psychol. 2018;43:678–692. doi: 10.1093/jpepsy/jsy010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevans K.B., Riley A.W., Landgraf J.M., Carle A.C., Teneralli R.E., Fiese B.H., Meltzer L.J., Ettinger A.K., Becker B.D., Forrest C.B. Children's family experiences: development of the PROMIS® pediatric family relationships measures. Qual. Life Res. 2017;26:3011–3023. doi: 10.1007/s11136-017-1629-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldt K., Coenen M., Movsisyan A., Voss S., Rehfuess E., Kunzler A.M., Lieb K., Jung-Sievers C. Interventions to ameliorate the psychosocial effects of the COVID-19 pandemic on children—a systematic review. Int. J. Environ. Res. Public Health. 2021;18:2361. doi: 10.3390/ijerph18052361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol. Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Creswell C., Parkinson M., Thirlwall K., Willetts L. Guilford Publications; 2019. Parent-Led CBT for Child Anxiety: Helping Parents Help their Kids. [Google Scholar]
- Ehrenreich-May J., Kennedy S.M., Sherman J.A., Bilek E.L., Buzzella B.A., Bennett S.M., Barlow D.H. Oxford University Press; 2017. Unified Protocols for Transdiagnostic Treatment of Emotional Disorders in Children and Adolescents: Therapist Guide. [Google Scholar]
- Ehrenreich-May J., Rosenfield D., Queen A.H., Kennedy S.M., Remmes C.S., Barlow D.H. An initial waitlist-controlled trial of the unified protocol for the treatment of emotional disorders in adolescents. J. Anxiety Disord. Transdiagn. Approaches. 2017;46:46–55. doi: 10.1016/j.janxdis.2016.10.006. [DOI] [PubMed] [Google Scholar]
- Fernandez E., Salem D., Swift J.K., Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: magnitude, timing, and moderators. J. Consult. Clin. Psychol. 2015;83:1108. doi: 10.1037/ccp0000044. [DOI] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annu. Rev. Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Guy W. Assessment Manual for Psychopharmacology. U.S. Department of Health, Education, and Welfare; 1976. Clinical global impression; pp. 217–222. [Google Scholar]
- Hawes M.T., Szenczy A.K., Olino T.M., Nelson B.D., Klein D.N. Trajectories of depression, anxiety and pandemic experiences; a longitudinal study of youth in New York during the spring-summer of 2020. Psychiatry Res. 2021;298 doi: 10.1016/j.psychres.2021.113778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin D.E., Gross H.E., Stucky B.D., Thissen D., DeWitt E.M., Lai J.S., Amtmann D., Khastou L., Varni J.W., DeWalt D.A. Development of six PROMIS pediatrics proxy-report item banks. Health Qual Life Outcomes. 2012;10:22. doi: 10.1186/1477-7525-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James Riegler L., Raj S.P., Moscato E.L., Narad M.E., Kincaid A., Wade S.L. Pilot trial of a telepsychotherapy parenting skills intervention for veteran families: implications for managing parenting stress during COVID-19. J. Psychother Integr. 2020;30:290. doi: 10.1037/int0000220. [DOI] [Google Scholar]
- Kazdin A.E. Annual research review: expanding mental health services through novel models of intervention delivery. J. Child Psychol. Psychiatry. 2019;60:455–472. doi: 10.1111/jcpp.12937. [DOI] [PubMed] [Google Scholar]
- Kennedy S.M., Bilek E.L., Ehrenreich-May J. A randomized controlled pilot trial of the unified protocol for transdiagnostic treatment of emotional disorders in children. Behav. Modif. 2019;43:330–360. doi: 10.1177/0145445517753940. [DOI] [PubMed] [Google Scholar]
- Khan A.N., Bilek E., Tomlinson R.C., Becker-Haimes E.M. Treating social anxiety in an era of social distancing: adapting exposure therapy for youth during COVID-19. Cogn. Behav. Pract. 2021 doi: 10.1016/j.cbpra.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin A.B., Peris T.S., De Nadai A.S., McCracken J.T., Piacentini J. Agreement between therapists, parents, patients, and independent evaluators on clinical improvement in pediatric obsessive-compulsive disorder. J. Consult. Clin. Psychol. 2012;80:1103–1107. doi: 10.1037/a0029991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N.R., Freeman J.Y.A., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchette L.K., Weisz J.R. Practitioner review: empirical evolution of youth psychotherapy toward transdiagnostic approaches. J. Child Psychol. Psychiatry. 2017;58:970–984. doi: 10.1111/jcpp.12747. [DOI] [PubMed] [Google Scholar]
- Mayne S.L., Hannan C., Davis M., Young J.F., Kelly M.K., Powell M., Dalembert G., McPeak K.E., Jenssen B.P., Fiks A.G. COVID-19 and adolescent depression and suicide risk screening outcomes. Pediatrics. 2021 doi: 10.1542/peds.2021-051507. [DOI] [PubMed] [Google Scholar]
- McKinnon A., Keers R., Coleman J.R.I., Lester K.J., Roberts S., Arendt K., Bögels S.M., Cooper P., Creswell C., Hartman C.A., Fjermestad K.W., In-Albon T., Lavallee K., Lyneham H.J., Smith P., Meiser-Stedman R., Nauta M.H., Rapee R.M., Rey Y., Schneider S., Silverman W.K., Thastum M., Thirlwall K., Wergeland G.J., Eley T.C., Hudson J.L. The impact of treatment delivery format on response to cognitive behaviour therapy for preadolescent children with anxiety disorders. J. Child Psychol. Psychiatry. 2018;59:763–772. doi: 10.1111/jcpp.12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front. Psychol. 2020 doi: 10.3389/fpsyg.2020.579038. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palo A., D'Souza J.M. The impact of COVID-19 on the treatment of obsessive-compulsive disorder. Bull. Menninger Clin. 2021:1–13. doi: 10.1521/bumc_2021_85_03. [DOI] [PubMed] [Google Scholar]
- Perrin P.B., Pierce B.S., Elliott T.R. COVID-19 and telemedicine: a revolution in healthcare delivery is at hand. Health Sci. Rep. 2020;3:e166. doi: 10.1002/hsr2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preuss H., Capito K., van Eickels R.L., Zemp M., Kolar D.R. Cognitive reappraisal and self-compassion as emotion regulation strategies for parents during COVID-19: an online randomized controlled trial. Internet Interv. 2021;24 doi: 10.1016/j.invent.2021.100388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N., McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021 doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramme, R., 2018. Spence children's anxiety scale: an overview of psychometric findings. Retrieved from: https://www.scaswebsite.com/wp-content/uploads/2021/07/Ramme-SCAS-Psychomet-evidence.pdf.
- Roos L.E., Salisbury M., Penner-Goeke L., Cameron E.E., Protudjer J.L.P., Giuliano R., Afifi T.O., Reynolds K. Supporting families to protect child health: parenting quality and household needs during the COVID-19 pandemic. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0251720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider J.L., Weisz J.R. Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. J. Am. Acad. Child Adolesc. Psychiatry. 2017;56:107–115. doi: 10.1016/j.jaac.2016.11.007. [DOI] [PubMed] [Google Scholar]
- Schneider, S.C., Weinzimmer, S.A., Nwankwo, G.N., Cepeda, S.L., Storch, E.A., 2020. COVID-related thoughts and behavioral symptoms, parent proxy version (COV-TaBS-P). Retrieved from: https://www.researchgate.net/publication/340872041_COVID-Related_Thoughts_and_Behavioral_Symptoms_Parent_Proxy_Version_COV-TaBS-P.
- Schneider, S.C., Weinzimmer, S.A., Zhang, C., Chen, R., Zhou, X., Storch, E.A., 2021. COVID-19 Exposure and Impacts Questionnaire (CEIQ). Retrieved from: https://www.researchgate.net/publication/350471637_COVID-19_Exposure_and_Impacts_Questionnaire_CEIQ.
- Spence S.H. A measure of anxiety symptoms among children. Behav. Res. Ther. 1998;36:545–566. doi: 10.1016/S0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Thurston I.B., Phares V. Mental health service utilization among African American and Caucasian mothers and fathers. J. Consult. Clin. Psychol. 2008;76:1058–1067. doi: 10.1037/a0014007. [DOI] [PubMed] [Google Scholar]
- Tracking Coronavirus in Texas: Latest Map and Case Count [WWW Document], 2021 . URL https://www.nytimes.com/interactive/2021/us/texas-covid-cases.html, (accessed 8.26.21).
- Varni J.W., Thissen D., Stucky B.D., Liu Y., Gorder H., Irwin D.E., DeWitt E.M., Lai J.-.S., Amtmann D., DeWalt D.A. PROMIS® parent proxy report scales: an item response theory analysis of the parent proxy report item banks. Qual. Life Res. 2012;21:1223–1240. doi: 10.1007/s11136-011-0025-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing V.R., Brent D.A., Rozenman M.S., Gonzalez A., Jeffreys M., Dickerson J.F., Lynch F.L., Porta G., Iyengar S. Brief behavioral therapy for pediatric anxiety and depression in primary care: a randomized clinical trial. JAMA Psychiatry. 2017;74:571–578. doi: 10.1001/jamapsychiatry.2017.0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside S.P.H., Sim L.A., Morrow A.S., Farah W.H., Hilliker D.R., Murad M.H., Wang Z. A meta-analysis to guide the enhancement of CBT for childhood anxiety: exposure over anxiety management. Clin. Child Fam. Psychol. Rev. 2020;23:102–121. doi: 10.1007/s10567-019-00303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan Y. Mindfulness training on the resilience of adolescents under the COVID-19 epidemic: a latent growth curve analysis. Pers. Individ. Dif. 2021;172 doi: 10.1016/j.paid.2020.110560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Wang W., Zhong Y., Wu F., Zhu Z., Tham Y.C., Lamoureux E., Xiao L., Zhu E., Liu H., Jin L., Liang L., Luo L., He M., Morgan I., Congdon N., Liu Y. A peer-to-peer live-streaming intervention for children during COVID-19 homeschooling to promote physical activity and reduce anxiety and eye strain: cluster randomized controlled trial. J. Med. Internet Res. 2021;23:e24316. doi: 10.2196/24316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.