Abstract
Objectives
Healthcare (including dental care) service use is influenced by predisposing, enabling, and need factors. One area with limited research is the association of acculturation (defined as behavioral changes in the adaptation to another culture) as a predisposing factor for dental care preventive service use. Preventive service use is a primary objective of Healthy People, 2030. The purpose of this study was to determine the association of acculturation with one preventive dental service use, dental pit-and-fissure sealant placement, among children in the U.S., ages 6-18 years.
Methods
A cross-sectional, secondary data analysis study was completed using National Health and Nutrition Examination Survey (NHANES), 2013-2016 data. NHANES is a nationally representative survey of non-institutionalized individuals across the U.S. In the dataset, children, ages 6-18 years, had been evaluated for pit-and-fissure dental sealant use. Information that served as proxies for acculturation were: length of stay in the United States (a citizen at the time of the survey; not a citizen and in the country < 5 years; or not a citizen and in the country ≥5 years) and whether English was spoken at home (yes; no). Data were analyzed for descriptive statistics. Multivariable logistic regressions were used to examine strength of the associations. Odds ratios for pit-and-fissure sealants among groups were determined.
Results
There were 2,220 children participants whose data were used for this study. Less than half (45.5%) had received dental pit-and-fissure sealants. A majority (53.3%) were white and were ages 12-18 years (51.6%). The mean number of dental pit-and-fissure sealants among all children was 5.5. There was a lower percentage of children living in the U.S. <5 years who had received pit-and-fissure sealants than children who were citizens of the U.S. (22.2% vs 48.9%, respectively). The adjusted odds ratio was lower for dental pit-and-fissure sealants among children who were in the U.S. <5 years than children who were citizens of the U.S (adjusted odds ratio, 0.38; 95% Confidence Interval: 0.24, 0.58).
Conclusions
In this study, children who had lived in the U.S. < 5 years were less likely to have pit-and-fissure sealants than children who were citizens of the U.S. There is a need to reach all children with preventive services to improve dental quality of life, reduce the need for dental restorations, and decrease overall financial burden regardless of time in the U.S.
Introduction
The global burden of untreated cavitated dental caries in primary dentition is approximately 9% and rises to approximately 35% in permanent dentition. 1 In the United States (U.S.), the caries burden for children, ages 6-11 years, is 15.3%.2 Prevention of dental caries depends on a complex combination of time, individual practices, dental preventive care practices at the individual level, the family’s social position and economic circumstances, various local, state, and national policies, dental marketing practices/consumer behavior, and dental care service utilization.2-4
Dental professionals typically focus on proximal risk-factors such as reducing the number of acidogenic microorganisms in a biofilm through brushing and flossing, encouraging the limitation of fermentable carbohydrates in the diet, and, where possible, reducing the vulnerability of teeth to prevent caries and periodontal disease. Among the preventive treatments that dental professionals can provide to reduce the vulnerability of newly erupted molars (and occasionally premolars) is the application of pit-and-fissure sealants. Many newly erupted molars and premolars have deep pits and fissures that are particularly vulnerable to dental caries because they trap debris.5 Pit-and-fissure sealants protect teeth by safely occluding the pits and fissures.
Placement of dental pit-and-fissure sealants on sound enamel, as well as the therapeutical sealing of non-cavitated carious lesions as a first-line therapy,6 have been advocated as effective preventive measures against caries, 7,8 as well as a cost-saving measure. The American Dental Association (ADA) has had pit-and-fissure sealant placement as an evidence-based, clinical recommendation for years.9 It has been reported that children enrolled in Medicaid who received topical fluoride and dental sealants had lower Medicaid expenditures, with the per-member per-year difference ranged from $88 for Alabama to $156 for Mississippi.10
Recognizing the importance of pit-and-fissure sealants, the U.S. national program, Healthy People 2030, has set a target goal for 42.5% of children, ages 3-19 years, to have at least one dental pit-and-fissure sealant by 2030.11 Public health efforts of school-based pit-and-fissure sealant programs 12 that can benefit nearly 6.5 million low-income children are also in place to increase utilization.13 However, the use of pit-and-fissure sealants to prevent dental caries is determined by many individual, provider, and social-level factors. At the provider level, fewer than 40% of practicing dentists followed the recommendations for pit-and-fissure sealant placement in a 2011 study.14 Similar findings were observed in a 2013 qualitative study of private-practice dentists, in which the dentists generally had not adopted the clinical recommendations regarding pit-and-fissure sealants.15
At the individual parent/guardian level there is lack of awareness about preventing caries with pit-and-fissure sealants. In a study of 3,500 participants, only half (55.1%) of parents/guardians had knowledge of pit-and-fissure sealants.16 In addition, there were disparities in the level of knowledge concerning dental pit-and-fissure sealants. That is, knowledge about pit-and-fissure sealants was lower among low-income, racial/ethnic minorities, and males.16 Similarly, researchers in another study reported that dental health literacy among parents was associated with their children’s dental health.17
Acculturation and Dental Pit-and-fissure Sealants
Acculturation is defined as the process of changing lifestyle practices and behaviors that are associated with movement and adaptation to another culture.18 It has many dimensions, and as such is measured with proxies such as language preference, length of stay in the new culture, country of origin, age of immigration, generational factors and social behavior.18 Acculturation may play an important role in the use of preventive healthcare services, including dental care services18 such as the use of pit-and-fissure sealants. Nearly 25% of children in the U.S. have foreign-born parents with differing cultural beliefs related to healthcare that extend to their children’s health/dental healthcare service use.18-21 These include access to dental care, dietary preferences (particularly exposure to sugars), hygiene practices, attitudes toward primary teeth, and beliefs in the value of preventive dental visits vs. fatalism about caries.18- 21 For example, researchers of a systematic review of 17 studies on oral health beliefs and attitudes of South Asian migrants in high income countries reported that lack of trusts in dentists, cost of dental treatments, home remedies, culture interacting with religion, and low oral health literacy were associated with poor oral health among migrants.22
While cost can be a barrier to preventive dental care23, in the U. S. dental care of children is routinely covered health insurance programs such as Medicaid, the Children Health Insurance Program and private insurance.24 Qualified non-citizens are eligible for Medicaid and Children’s Health Insurance Program if they meet state income and residency rules (generally a 5-year waiting period in 21 states).25 Even when the families/individuals qualify for public insurance, there are still fears and confusion about availing the family to preventive or other healthcare services in the U.S.26, 27 Furthermore, many qualified non-citizens are hesitant to accept these benefits in the misbelief that doing so will negatively impact their chance for citizenship.
There is a need to understand the factor of acculturation in dental care service use for children’s preventive services. The authors of this study wished to estimate acculturation as a factor in a specific dental care service, pit-and-fissure sealant use. The rationale for this study is that although researchers have evaluated acculturation/immigrant status on oral healthcare service use such as caries and periodontal diseases, 28, 29 the association of acculturation with preventive dental services use in children, such as dental pit-and-fissure sealant placement, has not been evaluated. Increasing preventive dental services use, and pit-and-fissure sealants, in particular, are Health and Human Services Healthy People 2030 objectives.11 It is important to determine their use among vulnerable populations.
The Anderson Behavioral Model of Health Services Use30 was the theoretical model used in this study to select variables to estimate the association. In the framework, healthcare service utilization is impacted by contextual and individual characteristics of predisposing factors (sex, age, education, race, beliefs, etc.); enabling factors (financial/family income, health insurance, availability of care, etc.); need factors (perceived or evaluated); and, health behaviors (personal practices, process of medical care, and use of personal health services).30,31 The research hypothesis for this study was that acculturation, as measured with the proxies of length of stay in the U.S. and language other than English spoken at home (which have been previously used by researchers to define acculturation18) would be associated with lower odds of the specific oral healthcare preventive service use of pit-and-fissure use. Therefore, the objectives of this study were to examine the association of the variables associated with acculturation measured by length of stay in the U.S. (a citizen at the time of the survey; not a citizen and in the country < 5 years; or not a citizen and in the country ≥5 years) and whether English was spoken at home (yes; or no) as predisposing factors versus the outcome of preventive service use of dental pit-and-fissure sealants (yes; or no).
Methods
Ethical statement
This study received non-human subject acknowledgement by the West Virginia University Institutional Review Board (Protocol number 2008089719).
Study design
The study design used in this research was a cross-sectional design.
Data source
The data source for this study was the combined National Health and Nutrition Examination Survey (NHANES) surveys, 2013-2014 and 2015-2016. NHANES is a representative sample of the health status of non-institutionalized residents across the U.S. The survey is conducted by the National Center for Health Statistics (a division of the Centers for Disease Control and Prevention, CDC). It was begun in the early 1960s to have an epidemiological view of the health and conditions of U.S redidents.32 Each year approximately 5,000 people participate in the survey.
Sample
Eligible children for this study had complete data on dental pit-and-fissure sealant use. citizenship status of the child, language spoken at home, sex, race/ethnicity, and age. There were 4,518 children whose data were used in the study by having met eligibility criteria.
Measures
The outcome variable for the study was dental service use, measured as to whether a child had received at least one dental pit-and-fissure sealant (any; recorded as yes; or none recorded as no). The use of least one pit-and-fissure sealant for the outcome variable was based upon the criterion of “at least one pit-and-fissure sealant” used in Health People 2030 outcome objectives for pit-and-fissure sealant use.11 The main independent variables were acculturation as measured by length of stay in the United States (a citizen at the time of the survey; not a citizen and in the country < 5 years; or not a citizen and in the country ≥5 years) and whether English was spoken at home (yes; no).
Other variables that influence healthcare service use, and pit-and-fissure sealant use in particular were derived from the Andersen model as well as epidemiological variables identified in published literature.13,16,33 These were the predisposing factors of sex (female, male); race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other); and age (6-11 years, 12-18 years, reflecting current practices of a dichotomy between pre-adolescence and adolescence13). The enabling factors included were family income (poor/near poor based on federal family income to poverty ratio of <2.0, and middle/high based on federal family income to poverty ratio of ≥ 2.0); health insurance (yes, no); and, education (<6 years, 7-8 years, 9-12 years, 12+ years). We were unable to control for “previous dental visit” as a co-variate as the data source did not distinguish between visits for sealants and visits for other reasons. (Our directed cyclic graph for the variables is presented in Figure 1.)
Figure 1.
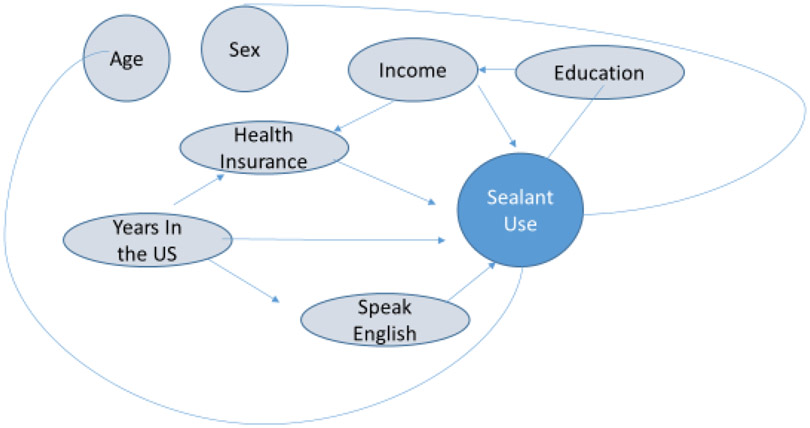
Directed Cyclic Graph for Sealant Use
Statistical Analyses
The data were analyzed with SAS version 9.4 with procedures to accommodate the complex survey design.34 Survey weights were used and adjusted for the combined survey years. Adjustments for primary sampling units and strata were also included in the analyses. Weighted frequencies, Rao Scott Chi-Square, and logistic regression analyses were conducted.
Results
Sample descriptions by time in the U.S. are presented in Table 1. There were 4,518 participants, of whom 48.9% were female. A majority (53.3%) were white and were ages 12-18 years (51.6%). There were 89.2% who spoke English in the home. Nearly two percent (1.8%) were in the U.S. < 5 years. The mean number of dental pit-and-fissure sealants among the children receiving pit-and-fissure sealants was 5.5.
Table 1.
Description of Characteristics among Youth (6- 18 years) National Health and Nutrition Examination Survey, 2013-2014 and 2015-2016
| Less than 5 years in the US | 5 or more years in the US | U.S. Citizen | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Wt % | 95% CI | N | Wt % | 95% CI | N | Wt % | 95% CI | Sig | |
| Sex | ||||||||||
| Female | 62 | 45.1 | [36.2 , 54.0] | 45 | 43.3 | [34.3 , 52.3] | 2119 | 49.1 | [47.0 , 51.1] | |
| Male | 67 | 54.9 | [46.0 , 63.8] | 52 | 56.7 | [47.7 , 65.7] | 2173 | 50.9 | [48.9 , 53.0] | |
| Age Group | ** | |||||||||
| 6-11 years | 57 | 41.4 | [31.6 , 51.2] | 33 | 29.2 | [15.8 , 42.6] | 2417 | 48.8 | [46.9 , 50.8] | |
| 12-18 years | 72 | 58.6 | [48.8 , 68.4] | 64 | 70.8 | [57.4 , 84.2] | 1875 | 51.2 | [49.2 , 53.1] | |
| Education | *** | |||||||||
| 1-6 years | 69 | 52.3 | [41.7 , 62.9] | 37 | 33.7 | [19.3 , 48.1] | 2813 | 59.5 | [57.5 , 61.4] | |
| 9-8 years | 29 | 24.2 | [15.7 , 32.6] | 29 | 32.0 | [21.1 , 42.8] | 689 | 18.5 | [17.1 , 19.8] | |
| 9-12 years | 31 | 23.5 | [15.7 , 31.4] | 31 | 34.3 | [25.3 , 43.4] | 788 | 22.1 | [20.3 , 23.8] | |
| Health Insurance | *** | |||||||||
| Yes | 84 | 61.6 | [50.9 , 72.4] | 63 | 61.1 | [49.5 , 72.8] | 4051 | 95.1 | [94.2 , 95.9] | |
| No | 45 | 38.4 | [27.7 , 49.1] | 34 | 38.9 | [27.2 , 50.5] | 241 | 4.9 | [ 4.1 , 5.8] | |
| Poverty Status | *** | |||||||||
| Low Income | 80 | 61.5 | [47.6 , 75.4] | 69 | 71.4 | [59.6 , 83.3] | 2347 | 42.2 | [36.8 , 47.5] | |
| Middle/ High | 31 | 24.5 | [11.7 , 37.2] | 17 | 16.2 | [ 6.8, 25.5] | 1637 | 52.2 | [46.4 , 58.0] | |
| Unknown | 18 | 14.0 | [ 5.7 , 22.4] | 11 | 12.4 | [ 5.8 , 19.0] | 308 | 5.6 | [ 4.4 , 6.9] | |
| Speak English | *** | |||||||||
| Speaks English | 39 | 26.8 | [17.0 , 36.7] | 32 | 31.5 | [20.1 , 42.9] | 3684 | 91.2 | [88.6 , 93.7] | |
| No | 90 | 73.2 | [63.4 , 83.0] | 65 | 68.5 | [57.1 , 79.9] | 608 | 8.8 | [ 6.3 , 11.4] | |
| Sealant | *** | |||||||||
| Yes | 32 | 22.2 | [14.1 , 30.4] | 41 | 41.3 | [28.7, 53.8] | 1920 | 48.9 | [45.3 , 52.5] | |
| No | 97 | 77.8 | [69.6 , 85.9] | 56 | 58.7 | [46.2 , 71.2] | 2372 | 51.1 | [47.5 , 54.7] | |
Note: Based on 4,518 youth participants, ages 6-18 years, who had no missing data on sealant use, speaks English, number of years in the United States and health insurance. Due to missing data in education and poverty status, total do not add to 4,518. (There were 24 who had >12 years of education, but did not provide years in the United States.) Abbreviations: US: United States; Wt: Weighted; HepB: hepatitis B vaccination; Speak English: the family speaks English in the home
p < .05
p < .001
p < .0001.
Table 2 includes the bivariate description of the sample by presence of at least one pit-and-fissure sealant (yes, no). There was a lower percentage of children living in the U.S. < 5 years who had received pit-and-fissure sealants than children who were citizens of the U.S. (22.2% vs 48.9%, respectively). A higher percentage of females than males (50.8% vs 46.0%, respectively) and a higher percentage of children, ages 12-18 years, than children, ages 6-11 years (53.8% vs 42.5%, respectively) had pit-and-fissure sealants.
Table 2.
Number and Weighted Percentages of Sealant Use among Youth (6- 18 years) National Health and Nutrition Examination Survey, 2013-2014 and 2015-2016
| Sealants | No Sealants | Chi-Square | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| N | Wt % | 95%CI | N | Wt % | 95% CI | |||
| ALL | 1,993 | 48.3 | 2,525 | 51.7 | ||||
| Speak English | 2.743 | 0.098 | ||||||
| Speaks English | 1,655 | 48.8 | [45.1, 52.5] | 2,100 | 51.2 | [47.5, 54.9] | ||
| No | 338 | 44.2 | [38.7, 49.7] | 425 | 55.8 | [50.3, 61.3] | ||
| Years in the U.S. | 28.938 | <0.001 | ||||||
| < 5 years | 32 | 22.2 | [14.1, 30.4] | 97 | 77.8 | [69.6, 85.9] | ||
| 5 or more | 41 | 41.3 | [28.8, 53.8] | 56 | 58.7 | [46.2, 71.2] | ||
| Citizen | 1,920 | 48.9 | [45.3, 52.5] | 2,372 | 51.1 | [47.5, 54.7] | ||
| Sex | 8.354 | 0.004 | ||||||
| Female | 1,010 | 50.8 | [46.9, 54.6] | 1,216 | 49.2 | [45.4, 53.1] | ||
| Male | 983 | 46.0 | [42.0, 50.0] | 1,309 | 54.0 | [50.0, 58.0] | ||
| Age Group | 41.356 | <0.001 | ||||||
| 6-11 years | 1,003 | 42.5 | [38.5, 46.5] | 1,504 | 57.5 | [53.5, 61.5] | ||
| 12-18 years | 990 | 53.8 | [49.9, 57.7] | 1,021 | 46.2 | [42.3, 50.1] | ||
| Race/Ethnicity | 29.624 | <0.001 | ||||||
| Non-Hispanic white | 588 | 52.6 | [48.5, 56.2] | 622 | 47.4 | [43.3, 51.5] | ||
| Non-Hispanic black | 394 | 37.1 | [30.7, 43.5] | 707 | 62.9 | [56.5, 69.3] | ||
| Mexican American | 717 | 47.8 | [42.3, 53.3] | 794 | 52.2 | [46.7, 57.7] | ||
| Other Race | 294 | 42.2 | [36.6, 47.9] | 402 | 57.8 | [52.1, 63.4] | ||
| Education | 33.615 | <0.001 | ||||||
| 1-6 years | 1,204 | 44.3 | [40.4, 48.3] | 1,715 | 55.7 | [51.7, 59.6] | ||
| 7-8 years | 387 | 57.4 | [52.2, 62.5] | 360 | 42.6 | [37.5, 47.8] | ||
| 9-12 years | 391 | 51.4 | [46.4, 56.4] | 435 | 48.6 | [43.6, 53.6] | ||
| >12 years | 11 | 46.8 | [24.2, 69.4] | 13 | 53.2 | [30.6, 75.8] | ||
| Health Insurance | 20.667 | <0.001 | ||||||
| Yes | 1,895 | 49.4 | [45.7, 53.0] | 2,303 | 50.6 | [47.0, 54.3] | ||
| No | 98 | 31.9 | [24/8, 39.0] | 222 | 68.1 | [61.0, 75.2] | ||
| Poverty Status | 15.237 | <0.001 | ||||||
| Low | 1,050 | 44.5 | [40.5, 48.5] | 1,446 | 55.5 | [51.5, 59.5] | ||
| Middle/High | 812 | 52.4 | [47.7, 57.2] | 873 | 47.6 | [42.8, 52.3] | ||
Note: Based on 4,518 youth participants, ages 6-18 years, who had no missing data on sealant use, speaks English, number of years in the United States and health insurance. Missing data in education and poverty status are not displayed. Group differences in sealant use were tested with Rao-Scott chi-square.
Abbreviations: U.S.: United States; Wt: Weighted
p < .05
p < .001
p < .0001.
The findings of logistic regression analyses are presented in Table 3. The results are that children in the U.S. < 5 years were less likely to have pit-and-fissure sealant placement than children who were U.S. citizens in the unadjusted model (odds ratio, 0.30; 95% Confidence Interval [CI], 0.19, 0.48) as well as in the fully adjusted model (AOR, 0.38; 95%CI: 0.24, 0.58). Speaking English was significant in the model controlling for sex, age, and race/ethnicity, but failed to reach significance in the fully adjusted model with the addition of education, poverty, health insurance, asthma.
Table 3.
Unadjusted (UOR) and Adjusted Odds Ratios AOR) and 95% Confidence Intervals (CI) Of Years Living in the US and Speaking English on Sealant Use From Logistic Regressions on Sealant Use, Youth Ages 6-18 National Health and Nutrition Examination Survey, 2013-2014 and 2015-2016
| Model 1. Unadjusted Model | |||||||
|---|---|---|---|---|---|---|---|
| UOR | 95%CI | Sig | UOR | 95% CI | Sig | ||
| In U.S. < 5 years | 0.30 | [0.19, 0,48] | *** | Speak English | 1.21 | [0.96, 1.52] | |
| In U.S. ≥5 years | 0.73 | [0.43, 1.24] | No | reference | |||
| Citizen | reference | ||||||
| Model 2. Model adjusting for sex, age, and race/ethnicity | |||||||
| AOR | 95% CI | Sig | AOR | 95% CI | Sig | ||
| In U.S. < 5 years | 0.30 | [0.19, 0.48] | *** | Speak English | 1.24 | [1.03, 1. 50] | * |
| In U.S. ≥5 years | 0.67 | [0.37, 1.22] | No | reference | |||
| Citizen | reference | ||||||
| Model 3. Model adjusting for sex, age, race/ethnicity, education, family income, and health insurance | |||||||
| AOR | 95% CI | Sig | AOR | 95% CI | Sig | ||
| In U.S. < 5 years | 0.38 | [0.24, 0.58] | *** | Speak English | 1.08 | [0.88, 1.32] | |
| In U.S. ≥5 years | 0.87 | [0.48, 1.60] | No | reference | |||
| Citizen | reference | ||||||
Note: Based on 4518 children, ages 6-18 years, from the NHANES, 2013-2014 and 2015-2016 data. Abbreviations: UOR: unadjusted odds ratio; Sig: significance; AOR: adjusted odds ratio
p < .05
p < .001
p < .0001.
Discussion
This study was a secondary data analysis of 2013-14 and 2015-16 NHANES data. It was conducted to evaluate the use of pit-and-fissure sealants among children, ages 6-18 years, in the U.S. The main finding was that children in the U.S. < 5 years were less likely to have pit-and-fissure sealant placement than children who were U.S. citizens. Children were as likely to have pit-and-fissure sealants if English were spoken in the home or if it were not.
This study is limited by the very nature of all secondary data analysis cross-sectional study designs. That is, the cross-sectional study design also does not allow for causative findings. Furthermore, variables must be constructed from the available data in the data sets. As such, the authors were limited in defining the measure of acculturation to length of stay in the U.S. and if English were spoken in the home. Not having additional variables (such as having parental citizenship status) associated with cultural practices and other proxies for acculturation limited the study. Although not specifically quantified, the data were not examined for differences among primary dentition, mixed dentition, and permanent dentition. Using age 6 years as the initial age for study participants in the study increased the possibility of having at least one first molar (“six-year molar”) present for having a sealant placed. However, the nature of the dentition may be a study limitation.
Our findings included an overall use of dental pit-and-fissure sealants in 48.3% of U.S. children, ages 6-18 years. This is consistent with a published study that used NHANES 2011-2014 data, in which 43% of children, aged 6-11 years, had received at least one pit-and-fissure sealant.13. In this first study of pit-and-fissure sealant use among children in the U.S. < 5 years, children in the U.S. < 5 years were less likely to have received dental pit-and-fissure sealants than children who were citizens of the U.S. This findings is in line with systematic reviews that have documented the positive association of acculturation with oral health. 28, 29 We also observed significant differences in sex, education, and health insurance among immigrant and U.S. citizens, in line with published studies.35
From a public health perspective, having fewer than half of the children in the U.S. with dental pit and fissure sealants is concerning. Existing pit-and-fissure school-based programs need to be aggressively promoted. While we did not explore the possible reasons of low pit-and-fissure sealant use, we can speculate that they include barriers to access to dental care, such as accessing health insurance. In our study, 38.4% of children in the U.S. <5 years had no health insurance whereas only 4.9% of the children who were U.S. citizens had no health insurance. In our study, children with health insurance were 2.3 times as likely as those without health insurance to have received a dental pit-and-fissure sealant. In the U.S., most children with health insurance have coverage for dental care services, if the coverage is sought.36 Increasing the rates of health insurance among immigrant children, may be one pathway to promote pit-and-fissure sealant use in this population.
Although many cultural barriers may explain low pit-and-fissure use, language should not be such a barrier as there are federal guidelines and legal obligations for healthcare providers to have interpreter and translator services available under federal civil rights laws.37 It is discrimination on the basis of national origin to fail to provide an interpreter or translator to individuals with limited English proficiency. This may potentially explain our finding of similar pit-and-fissure use in children from families that spoke or did not speak English at home. Future studies need to explore other barriers for dental preventive care including lack of awareness and knowledge about services such as pit-and-fissure sealants, fear about components of pit-and-fissure sealants negatively affecting health, and cultural orientation about oral health care.38
Conclusion
In this study of dental pit-and-fissure sealant use among children living in the U.S. <5 years were less likely to have dental pit-and-fissure sealants than children who were U.S. citizens. We observed that health insurance was strongly associated with pit-and-fissure sealant use, suggesting that expanding health insurance coverage for dental care is important to promote pit-and-fissure sealant use and reduce the risk of poor oral health among immigrant children and youth.
Acknowledgement
The project described was supported by the National Institute Of General Medical Sciences, 5U54GM104942-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest Statement
The authors report no conflicts of interest.
Contributor Information
R. Constance Wiener, West Virginia University, Department of Dental Practice and Rural Health, School of Dentistry, 104a Health Sciences Addition, PO Box 9415, Morgantown, WV 26506.
Patricia A. Findley, Special Assistant to the Dean for Interprofessional Health Initiatives, Rutgers School of Social Work, 120 Albany Street, New Brunswick, NJ 08901.
Chan Shen, Penn State College of Medicine, 500 University Drive, P.O. Box 850, Mail Code H151 Hershey, PA 17033-0850.
Nilanjana Dwibedi, Department of Pharmaceutical Systems and Policy, West Virginia University School of Pharmacy, Robert C. Byrd Health Sciences Center [North], P.O. Box 9510 Morgantown, WV 26506-9510.
Usha Sambamoorthi, UNT System College of Pharmacy.
Data Availability Statement
The data that support the finding of this study are openly available from the National Health and Nutrition Examination Survey website at https://wwwn.cdc.gov/nchs/nhanes/Default.aspx, reference number 39.
References
- 1.Frencken JE, Sharma P, Stenhouse L, Green D, Laverty D, Dietrich T. Global epidemiology of dental caries and severe periodontitis–a comprehensive review. J Clin Periodontol. 2017. Mar; 44:94–105. [DOI] [PubMed] [Google Scholar]
- 2.Fleming E, Afful J. Prevalence of Total and Untreated Dental Caries Among Youth: United States, 2015-2016. NCHS Data Brief. 2018;(307):1–8. [PubMed] [Google Scholar]
- 3.Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–260. [DOI] [PubMed] [Google Scholar]
- 4.Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, Newacheck PW. Influences on children's oral health: a conceptual model. Pediatrics. 2007. Sep 1;120(3):e510–20. [DOI] [PubMed] [Google Scholar]
- 5.Batchelor PA, Sheiham A. Grouping of tooth surfaces by susceptibility to caries: a study in 5-16 year-old children. BMC Oral Health. 2004;4(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leal SC, Moreira KMS, Imparato JCP. Dental Sealants. Pediatric Restorative Dentistry; Springer, 2019: 117–125. [Google Scholar]
- 7.Roydhouse RH. Prevention of occlusal fissure caries by use of a sealant: a pilot study. ASDC J Dent Child. 1968;35(3):253–262. [PubMed] [Google Scholar]
- 8.Takeuchi M, Kizu T, Shimizu T, Eto M, Amano F. Sealing of the pit and fissure with resin adhesive. II. Results of nine months' field work, an investigation of electric conductivity of teeth. Bull Tokyo Dent Coll. 1966;7(1):60–71. [PubMed] [Google Scholar]
- 9.Beauchamp J, Caufield PW, Crall JJ, Kohn W, Siegal M, Simonsen R. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139(3):257–268. [DOI] [PubMed] [Google Scholar]
- 10.Lee I, Monahan S, Serban N, Griffin PM, Tomar SL. Estimating the Cost Savings of Preventive Dental Services Delivered to Medicaid-Enrolled Children in Six Southeastern States. Health Serv Res. 2018;53(5):3592–3616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Healthy People 2030. DPHP Disease Preventions and Health Promotion, Healthy People 2030. Department of Health and Human Services. 2020. https://health.gov/healthypeople/objectives-and-data/browse-objectives/oral-conditions/reduce-proportion-children-and-adolescents-active-and-untreated-tooth-decay-oh-02 [Google Scholar]
- 12.Griffin SO, Naavaal S, Scherrer C, Patel M, Chattopadhyay S, Community Preventive Services Task Force. Evaluation of school-based dental sealant programs: an updated community guide systematic economic review. Am J Prev Med. 2017. Mar 1;52(3):407415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Griffin SO, Wei L, Gooch BF, Weno K, Espinoza L. Vital signs: dental sealant use and untreated tooth decay among US school-aged children. MMWR. 2016;65(41):1141–1145. [DOI] [PubMed] [Google Scholar]
- 14.Tellez M, Gray SL, Gray S, Lim S, Ismail AI. Sealants and dental caries: dentists' perspectives on evidence-based recommendations. J Am Dent Assoc. 2011;142(9):1033–1040. [DOI] [PubMed] [Google Scholar]
- 15.O'Donnell JA, Modesto A, Oakley M, Polk DE, Valappil B, Spallek H. Sealants and dental caries: insight into dentists' behaviors regarding implementation of clinical practice recommendations. J Am Dent Assoc. 2013;144(4):e24–e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Junger ML, Griffin SO, Lesaja S, Espinoza L. Awareness Among US Adults of Dental Sealants for Caries Prevention. Prev Chronic Dis. 2019;16:180398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khodadadi E, Niknahad A, Sistani MM, Motallebnejad M. Parents' Oral Health Literacy and its Impact on their Children's Dental Health Status. Electron Physician. 2016;8(12):3421–3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crespo E The Importance of Oral Health in Immigrant and Refugee Children. Children (Basel). 2019;6(9):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amin M, ElSalhy M. Factors Affecting Dental Attendance of Children of New Immigrant Parents: A Cross-Sectional Study. J Immigr Minor Health. 2017;19(6):1351–1361. [DOI] [PubMed] [Google Scholar]
- 20.Guendelman S, Angulo V, Wier M, Oman D. Overcoming the odds: access to care for immigrant children in working poor families in California. Matern Child Health J. 2005;9(4):351–362. [DOI] [PubMed] [Google Scholar]
- 21.Watson MR, Horowitz AM, Garcia I, Canto MT. Caries conditions among 2-5-year-old immigrant Latino children related to parents' oral health knowledge, opinions and practices. Community Dent Oral Epidemiol. 1999;27(1):8–15. [DOI] [PubMed] [Google Scholar]
- 22.Batra M, Gupta S, Erbas B. Oral Health Beliefs, Attitudes, and Practices of South Asian Migrants: A Systematic Review. Int J Environ Res Public Health. 2019;16(11):1952. Published 2019 Jun 1. doi: 10.3390/ijerph16111952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vujicic M, Buchmueller T, Klein R. Dental Care Presents The Highest Level Of Financial Barriers, Compared To Other Types Of Health Care Services. Health Aff (Millwood). 2016;35(12):2176–2182. [DOI] [PubMed] [Google Scholar]
- 24.Berdahl T, Hudson J, Simpson L, McCormick MC. Annual Report on Children's Health Care: Dental and Orthodontic Utilization and Expenditures for Children, 2010-2012. Acad Pediatr. 2016;16(4):314–326. [DOI] [PubMed] [Google Scholar]
- 25.Healthcare.gov. Health coverage for lawfully present immigrants. Coverage for lawfully present immigrants. 2020. https://www.healthcare.gov/immigrants/lawfully-present-immigrants. Accessed November 4, 2020. [Google Scholar]
- 26.Bernstein H, McTarnaghan S, Gonzalez D. Safety Net Access in the Context of the Public Charge Rule. Urban Institute. 2019. https://www.urban.org/research/publication/safety-net-access-context-public-charge-rule. Accessed November 4, 2020. [Google Scholar]
- 27.Lakshmanan L, Gurunathan D. Parents' knowledge, attitude, and practice regarding the pit and fissure sealant therapy. Journal of Family Medicine and Primary Care. 2020. Jan;9(1):385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gao XL, McGrath C. A review on the oral health impacts of acculturation. J Immigr Minor Health. 2011;13(2):202–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dahlan R, Badri P, Saltaji H, Amin M. Impact of acculturation on oral health among immigrants and ethnic minorities: A systematic review. PLoS One. 2019;14(2):e0212891. Published 2019 Feb 28. doi: 10.1371/journal.pone.0212891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Babitsch B, Gohl D, von Lengerke T. Re-visiting Andersen’s Behavioral Model of Health Services Use: a systematic review of studies from 1998-2011. Psychosoc Med. 2012;9:Doc11. doi: 10.2305/psm000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen RM, Davidson PL, Baumeister SE. Improving access to care in America. Changing the US health care system: key issues in health services policy and management. 3a. Edition. San Francisco: Jossey-Bass. 2007:3–31. [Google Scholar]
- 32.Centers for Disease Control and Prevention. About the National Health and Nutrition Examination Survey. 2017; https://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 33.Alos-Rullan V Households' age, country of birth, and marital status, stronger predictor variables than education in the prevalence of dental sealants, restorations, and caries among US children 5-19 years of age, NHANES 2005-2010. BMC Oral Health. 2019;19(1):195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.SAS [computer program]. Version 9.4. Cary, NC: SAS Institute Inc; 2014. [Google Scholar]
- 35.Carrasquillo O, Carrasquillo AI, Shea S. Health insurance coverage of immigrants living in the United States: differences by citizenship status and country of origin. Am J Public Health. 2000;90(6):917–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Larson K, Cull WL, Racine AD, Olson LM. Trends in access to health care services for US children: 2000–2014. Pediatrics. 2016. Dec 1;138(6):e20162176. [DOI] [PubMed] [Google Scholar]
- 37.Bulletin: Civil Rights, HIPAA, and the Coronavirus Disease 2019 (COVID-19). Health and Human Services Office for Civil Rights Action. March 28, 2020. https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf.
- 38.Bonetti D, Johnston M, Clarkson JE, Grimshaw J, Pitts NB, Eccles M, Steen N, Thomas R, Maclennan G, Glidewell L, Walker A. Applying psychological theories to evidence-based clinical practice: identifying factors predictive of placing preventive fissure sealants. Implementation Science. 2010. Dec 1;5(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.NHANES National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention. December 16, 2020. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the finding of this study are openly available from the National Health and Nutrition Examination Survey website at https://wwwn.cdc.gov/nchs/nhanes/Default.aspx, reference number 39.


