Abstract
Objective
Ankylosing spondylitis (AS) is a rheumatic inflammatory disease marked by chronic inflammation of the axial skeleton. This condition, particularly when severe, can lead to increased risk of vertebral fractures attributed to decreased ability of the stiffened spinal column to sustain normal loads. However, little focus has been placed on understanding the locations of spinal fractures and associated complications and assessing the correlation between these. In this review, we aim to summarize the complications and treatment patterns in the United States in AS patients with spinal fractures, using the latest Nationwide Inpatient Sample (NIS) database (2016–2018).
Methods
We analyzed the NIS data of years 2016–2018 to compare the fracture patterns and complications.
Results
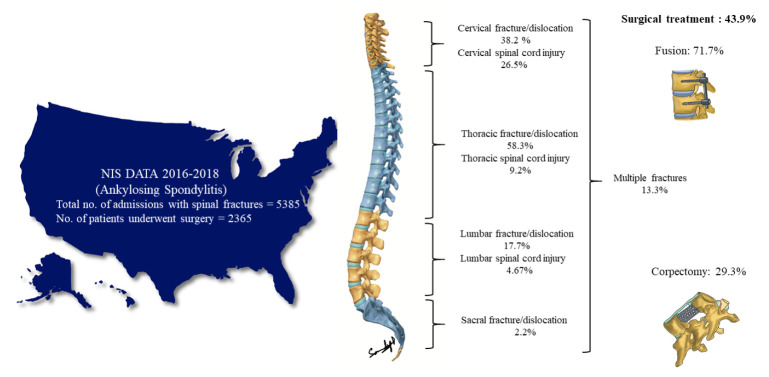
A total of 5,385 patients were included. The mean age was 71.63 years (standard deviation [SD], 13.21), with male predominance (83.8%). The most common population is Whites (77.4%), followed by Hispanics (7.9%). The most common fracture level was thoracic level (58.3%), followed by cervical level (38%). Multiple fracture levels were found in 13.3% of the patients. Spinal cord injury (SCI) was associated with 15.8% of the patients. The cervical level had a higher proportion of SCI (26.5%), followed by thoracic level (9.2%). The mean Elixhauser comorbidity score was 4.82 (SD, 2.17). A total of 2,365 patients (43.9%) underwent surgical treatment for the fractures. The overall complication rate was 40.8%. Respiratory complications, including pneumonia and respiratory insufficiency, were the predominant complications in the overall cohort. Based on the regression analysis, there was no significant difference (p=0.45) in the complication rates based on the levels. The presence of SCI increased the odds of having a complication by 2.164 times (95% confidence interval, 1.722–2.72; p≤0.001), and an increase in Elixhauser comorbidity score predicted the complication and in-hospital mortality rate (p≤0.001).
Conclusion
AS patients with spinal fractures have higher postoperative complications than the general population. The most common fracture location was thoracic in our study, although it differs with few studies, with SCI occurring in 1/6th of the patients.
Keywords: Ankylosing spondylitis, Spinal fractures, Respiratory complications, National Inpatient Sample
INTRODUCTION
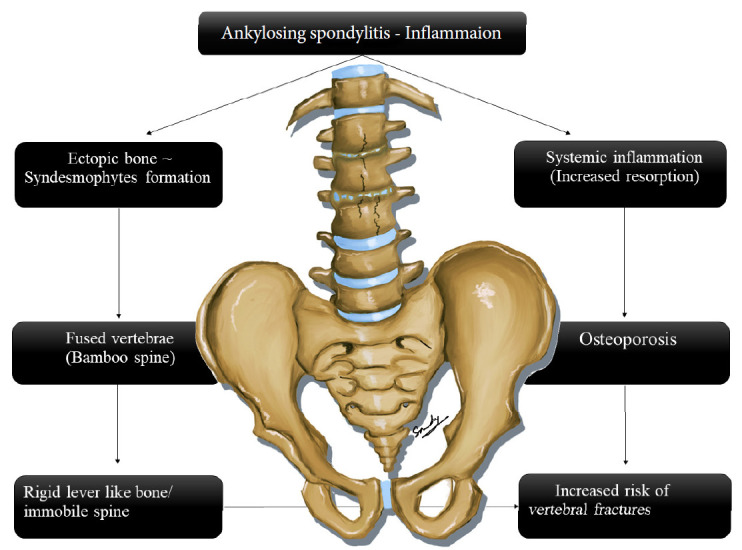
Ankylosing spondylitis (AS) is a rheumatic disorder marked by chronic inflammation of the axial skeleton [1]. It is a relatively rare disease with an incidence of 0.5–14 per 100,000 people per year [2]. This condition, particularly when severe, can lead to increased risk of vertebral fractures attributed to decreased ability of the stiffened spinal column to sustain normal loads (decreased tensile strength of the spine as a unit) [3]. A population-based study reported an odds ratio of 7.7 for sustaining a spinal fracture in patients with AS compared to the average population. With each year of increasing age, a 1.3% risk of having a fracture is added [3]. The reported prevalence of spinal fractures in AS patients is highly variable (1.4%–58%). Spinal trauma literature details a 6%–11% mortality rate in AS patients who underwent hospitalization for traumatic spinal fracture [4]. Spinal cord injury (SCI) is a severe complication after traumatic fracture of the ankylosed spine [2,5]. A Finnish national study reported the incidence of SCI in AS patients 11.4 times more than the average population [6].
The etiology behind vertebral fractures in AS patients stems from inflamed facet joints and ligaments and stiffened intervertebral spaces, resulting in decreased spinal column flexibility [1]. The classic "bamboo spine" develops with even marginal syndesmophyte formation, contributing to compromised bone integrity (Fig. 1) [7]. Literature advocates comprehensive spinal imaging in AS patients who suffer from even mild trauma to ensure fractures are not overlooked. However, little focus has been placed on understanding the locations of spinal fractures and postfracture complications and the correlation between these. The extra-articular manifestations in AS affect the other systems (cardiovascular, respiratory, and renal, etc.), further complicating the postoperative course. In this review, we aim to summarize the complications and treatment patterns in the United States in AS patients with spinal fractures, using the latest Nationwide Inpatient Sample (NIS) database (2016–2018).
Fig. 1.
Pathogenesis involved in ankylosing spondylitis.
MATERIALS AND METHODS
1. Study Population
Data were extracted from the NIS database for the years 2016–2018 (3 years). NIS data is the largest database providing data of more than 7 million hospitalizations in the United States. The data is coded in the form of diagnostic and procedural International Statistical Classification of Diseases, 10th revision (ICD-10) codes.
2. Inclusion Criteria
(1) All patients with AS and spinal fractures, (2) Spinal fractures as a primary cause of admission, age > 18 years.
3. Exclusion Criteria
Spinal fractures are not a primary cause of admission.
4. Data Extraction
The data was extracted from the NIS data based on the ICD-10 diagnostic and procedural codes. NIS data provides weighted frequencies allowing to extrapolate national estimates. The diagnostic and procedural codes used to extract AS, spinal fractures at various levels, and complications of the surgical treatment were detailed in Table 1. The data were grouped based on the fracture level (i.e., cervical, thoracic, etc.).
Table 1.
Details of the ICD-10 codes used for data extraction
| Diagnosis | ICD-10 code |
|---|---|
| Ankylosing spondylitis | M45.(1-9) |
| Cervical fractures and dislocations | Base codes: S12.0(X), S12.1(X), S12.2X, S12.3(X), S12.4(X), S12.5(X), S12.6(X), S12.8(X), S12.9(X) |
| Thoracic fractures and dislocations | Base codes: S22.00(x), S22.01(x), S22.02(x), S22.03(x), S22.04(x), S22.05(x), S22.06(x), S22.07(x), S22.08(x) |
| Lumbar fracture | Base codes: S32.00(x), S32.01(X), S32.02(X), S32.03(X), S32.04(X), S32.05(X) |
| Sacral level | Base codes: S32.11(X), S32.12(X), S32.13(X), S32.14(X), S32.15(X), S32.16(X), S32.17(X), S32.19(X) |
| Spinal cord injury | S14(X), S24(X), S34(X) |
| Fusion | 0RG0070,0RG0071,0RG007J,0RG00A0,0RG00AJ,0RG00J0,0RG00J1,0RG00JJ,0RG00K0,0RG00K1,0RG00KJ,0RG0370,0RG0371,0RG037J,0RG03A0,0RG03AJ,0RG03J0,0RG03J1,0RG03JJ,0RG03K0,0RG03K1,0RG03KJ,0RG0470,0RG0471,0RG047J,0RG04A0,0RG04AJ,0RG04J0,0RG04J1,0RG04JJ,0RG04K0,0RG04K1,0RG04KJ,0RG1070,0RG1071,0RG107J,0RG10A0,0RG10AJ,0RG10J0,0RG10J1,0RG10JJ,0RG10K0,0RG10K1,0RG10KJ,0RG1370,0RG1371,0RG137J,0RG13A0,0RG13AJ,0RG13J0,0RG13J1,0RG13JJ,0RG13K0,0RG13K1,0RG13KJ,0RG1470,0RG1471,0RG147J,0RG14A0,0RG14AJ,0RG14J0,0RG14J1,0RG14JJ,0RG14K0,0RG14K1,0RG14KJ,0RG2070,0RG2071,0RG207J,0RG20A0,0RG20AJ,0RG20J0,0RG20J1,0RG20JJ,0RG20K0,0RG20K1,0RG20KJ,0RG2370,0RG2371,0RG237J,0RG23A0,0RG23AJ,0RG23J0,0RG23J1,0RG23JJ,0RG23K0,0RG23K1,0RG23KJ,0RG2470,0RG2471,0RG247J,0RG24A0,0RG24AJ,0RG24J0,0RG24J1,0RG24JJ,0RG24K0,0RG24K1,0RG24KJ,0RG4070,0RG4071,0RG407J,0RG40A0,0RG40AJ,0RG40J0,0RG40J1,0RG40JJ,0RG40K0,0RG40K1,0RG40KJ,0RG4370,0RG4371,0RG437J,0RG43A0,0RG43AJ,0RG43J0,0RG43J1,0RG43JJ,0RG43K0,0RG43K1,0RG43KJ,0RG4470,0RG4471,0RG447J,0RG44A0,0RG44AJ,0RG44J0,0RG44J1,0RG44JJ,0RG44K0,0RG44K1,0RG44KJ,0RG6070,0RG6071,0RG607J,0RG60A0,0RG60AJ,0RG60J0,0RG60J1,0RG60JJ,0RG60K0,0RG60K1,0RG60KJ,0RG6370,0RG6371,0RG637J,0RG63A0,0RG63AJ,0RG63J0,0RG63J1,0RG63JJ,0RG63K0,0RG63K1,0RG63KJ,0RG6470,0RG6471,0RG647J,0RG64A0,0RG64AJ,0RG64J0,0RG64J1,0RG64JJ,0RG64K0,0RG64K1,0RG64KJ,0RG7070,0RG7071,0RG707J,0RG70A0,0RG70AJ,0RG70J0,0RG70J1,0RG70JJ,0RG70K0,0RG70K1,0RG70KJ,0RG7370,0RG7371,0RG737J,0RG73A0,0RG73AJ,0RG73J0,0RG73J1,0RG73JJ,0RG73K0,0RG73K1,0RG73KJ,0RG7470,0RG7471,0RG747J,0RG74A0,0RG74AJ,0RG74J0,0RG74J1,0RG74JJ,0RG74K0,0RG74K1,0RG74KJ,0RG8070,0RG8071,0RG807J,0RG80A0,0RG80AJ,0RG80J0,0RG80J1,0RG80JJ,0RG80K0,0RG80K1,0RG80KJ,0RG8370,0RG8371,0RG837J,0RG83A0,0RG83AJ,0RG83J0,0RG83J1,0RG83JJ,0RG83K0,0RG83K1,0RG83KJ,0RG8470,0RG8471,0RG847J,0RG84A0,0RG84AJ,0RG84J0,0RG84J1,0RG84JJ,0RG84K0,0RG84K1,0RG84KJ,0SG0070,0SG0071,0SG007J,0SG00A0,0SG00AJ,0SG00J0,0SG00J1,0SG00JJ,0SG00K0,0SG00K1,0SG00KJ,0SG0370,0SG0371,0SG037J,0SG03A0,0SG03AJ,0SG03J0,0SG03J1,0SG03JJ,0SG03K0,0SG03K1,0SG03KJ,0SG0470,0SG0471,0SG047J,0SG04A0,0SG04AJ,0SG04J0,0SG04J1,0SG04JJ,0SG04K0,0SG04K1,0SG04KJ,0SG1070,0SG1071,0SG107J,0SG10A0,0SG10AJ,0SG10J0,0SG10J1,0SG10JJ,0SG10K0,0SG10K1,0SG10KJ,0SG1370,0SG1371,0SG137J,0SG13A0,0SG13AJ,0SG13J0,0SG13J1,0SG13JJ,0SG13K0,0SG13K1,0SG13KJ,0SG1470,0SG1471,0SG147J,0SG14A0,0SG14AJ,0SG14J0,0SG14J1,0SG14JJ,0SG14K0,0SG14K1,0SG14KJ,0SG3070,0SG3071,0SG307J,0SG30A0,0SG30AJ,0SG30J0,0SG30J1,0SG30JJ,0SG30K0,0SG30K1,0SG30KJ,0SG3370,0SG3371,0SG337J,0SG33A0,0SG33AJ,0SG33J0,0SG33J1,0SG33JJ,0SG33K0,0SG33K1,0SG33KJ,0SG3470,0SG3471,0SG347J,0SG34A0,0SG34AJ,0SG34J0,0SG34J1,0SG34JJ,0SG34K0,0SG34K1,0SG34KJ,0SG5070,0SG5071,0SG507J,0SG50A0,0SG50AJ,0SG50J0,0SG50J1,0SG50JJ,0SG50K0,0SG50K1,0SG50KJ,0SG5370,0SG5371,0SG537J,0SG53A0,0SG53AJ,0SG53J0,0SG53J1,0SG53JJ,0SG53K0,0SG53K1,0SG53KJ,0SG5470,0SG5471,0SG547J,0SG54A0,0SG54AJ,0SG54J0,0SG54J1,0SG54JJ,0SG54K0,0SG54K1,0SG54KJ,0SG6070,0SG6071,0SG607J,0SG60A0,0SG60AJ,0SG60J0,0SG60J1,0SG60JJ,0SG60K0,0SG60K1,0SG60KJ,0SG6370,0SG6371,0SG637J,0SG63A0,0SG63AJ,0SG63J0,0SG63J1,0SG63JJ,0SG63K0,0SG63K1,0SG63KJ,0SG6470,0SG6471,0SG647J,0SG64A0,0SG64AJ,0SG64J0,0SG64J1,0SG64JJ,0SG64K0,0SG64K1,0SG64KJ |
| Corpectomy | 0P540ZZ,0P840ZZ,0PB40ZX,0PB40ZZ,0PC40ZZ,0PD40ZZ,0PH404Z,0PN40ZZ,0PR407Z,0PR40JZ,0PR40KZ,0PU407Z,0PU40JZ,0PU40KZ,0R560ZZ,0RB60ZX,0RB60ZZ,0RC90ZZ,0RG6070,0RG607J,0RG60A0,0RG60AJ,0RG60Z0,0RG60JJ,0RG60K0,0RG60KJ,0RH604Z,0RH608Z,0RR607Z,0RR60JZ,0RR60KZ,XRG6092,XRG60F3,XRG7092,XRG70F3,XRG8092,XRG80F3,0Q500ZZ,0Q800ZZ,0QB00ZX,0QB00ZZ,0QC00ZZ,0QD00ZZ,0QH004Z,0QH005Z,0QN00ZZ,0QR007Z,0QR00JZ,0QR00KZ,0QS004Z,0QS00ZZ,0QS0XZZ,0QU007Z,0QU00JZ,0QU00KZ,0S500ZZ,0SB00ZX,0SB00ZZ,0SC00ZZ,0SG0070,0SG007J,0SG00A0,0SG00AJ,0SG00J0,0SG00JJ,0SG00K0,0SG00KJ,0SH004J,0SH008Z,0SN00ZZ,0SR007Z,0SR00JZ,0SR00KZ,0SU007Z,0SU00JZ,0SU00KZ,0P530ZZ,0P830ZZ,0PB30ZX,0PB30ZZ,0PC30ZZ,0PD30ZZ,0PH304Z,0PN30ZZ,0PR307Z,0PR30JZ,0PR30KZ,0PU307Z,0PU30JZ,0PU30KZ,0R500ZZ,0RB00ZX,0RB00ZZ,0RB10ZX,0RB10ZZ,0RC00ZZ,0RC10ZZ,0RG0070,0RG0071,0RG007J,0RG00A0,0RG00AJ,0RG00J0,0RG00JJ,0RG00K0,0RG00KJ,0RG1070,0RG107J,0RG10A0,0RG10AJ,0RG10J0,0RG10JJ,0RG10K0,0RG10KJ,0RH004Z,0RR007Z,0RR00JZ,0RR00KZ,0RR107Z,0RR10JZ,0RR10KZ,0RU007Z,0RU00ZJ,0RU00KZ,0RU107Z,0RU10JZ,0RU10KZ,XRG0092,XRG00F3,XRG1092,XRG10F3 |
| Wound complications, including CSF leak | T81.3,T81.30,T81.30XA,T81.30XD,T81.30XS,T81.31,T81.31XA,T81.31XD,T81.31XS,T81.32,T81.32XA,T81.32XD, T81.32XS, G97.0 |
| Respiratory complications | J81.0,J80,J96.00,J96.90,J96.91,J96.92,J96.01,J96.02,J95.89,J95.859,T8.182XA,J18,J18.0,J18.1,J18.2,J18.8,J18.9 |
| Acute Kidney Injury | N17.0,N17.1,N17.2,N17.8,N17.9 |
| UTI | N39.0 |
| Cardiac complications | 197.710, I97.790, I97.88, I97.89 Nerve root injuries S14.2(X), S24.2(X), S34.2(X) |
| Sepsis and septic shock | A410,A4101,A4102,A411,A412,A413,A414,A415,A4150,A4151,A4152,A4153,A4159,A418,A4181,A4189,A419, T81.12, T81.12XA, T81.12XD, T81.12XS |
| Ventilation | 5A1935Z, 5A1945Z, 5A1955Z |
| DVT | I82.2(X) |
ICD-10, International Statistical Classification of Diseases, 10th revision; CSF, cerebrospinal fluid; UTI, urinary tract infection; DVT, deep venous thrombosis.
The patient-level comorbidities were extracted based on the Elixhauser comorbidity algorithm [8] provided on the Healthcare Cost and Utilization Project website (https://www.hcup-us.ahrq.gov/nisoverview.jsp). Along with these variables, patient-level factors like race, socioeconomic characteristics, location of the patient, and hospital and patient’s zip code’s median income were also analyzed and described in the descriptive fashion. Complications were calculated for the patients who underwent surgical treatment.
5. Statistical Analysis
All variables were described in a standard descriptive fashion. Continuous variables are described as mean, standard deviation (SD), and median as appropriate and categorical variables as frequencies. Logistic regression analysis was used to calculate the odds ratios for the mutually exclusive levels and probability of the complications after adjusting for the SCI, Elixhauser comorbidities score and used Wald statistics to test the differences between them. Statistical significance was considered if the p-value (2-tailed) is 0.05. NIS discharge weights were used to extrapolate at the national level. All the analysis was performed using IBM SPSS Statistics ver. 27.0 (IBM Co., Armonk, NY, USA).
RESULTS
1. Clinical Characteristics
1) Overall patient cohort
A total of 5,385 patients were included. The mean age was 71.63 years (SD, 13.21), with male predominance (83.8%). The most common population is Whites (77.4%), followed by Hispanics (7.9%). The most common fracture level was thoracic level (58.3%), followed by cervical level (38%). Multiple fracture levels were found in 13.3% of the patients. SCI was associated with 15.8% of the patients. The cervical level had a higher proportion of SCI (26.5%), followed by thoracic level (9.2%). The mean Elixhauser comorbidity score was 4.82 (SD, 2.17). Complete details are listed in Table 2.
Table 2.
Demographics and discharge dispositions of the cohorts (weighted frequencies)
| Variable | Overall (n = 5,385) | Cervical (n = 2,055) | Thoracic (n = 3,140) | Lumbar (n = 955) | Sacral (n = 120) | |
|---|---|---|---|---|---|---|
| Age (yr) | 71.63 ± 3.21 | 69.88 ± 13.58 | 72.20 ± 12.85 | 71.30 ± 13.4 | 69.54 ± 15.75 | |
| Sex | ||||||
| Male | 83.8 | 88.6 | 83.4 | 82.2 | 45.8 | |
| Female | 16.2 | 11.4 | 16.6 | 17.8 | 54.2 | |
| Race | ||||||
| White | 4,170 (77.4) | 1,520 (74) | 2,455 (78.2) | 740 (77.5) | 100 (83.3) | |
| African Americans | 265 (4.9) | 145 (7.3) | 110 (3.5) | 65 (6.8) | N/A | |
| Hispanics | 265 (7.9) | 185 (9.3) | 250 (8) | 55 (5.8) | 10 (8.3) | |
| Asian/Pacific Islander | 165 (3.1) | 90 (4.4) | 75 (2.4) | 25 (2.6) | N/A | |
| Native Americans | 30 (0.6) | 5 (0.2) | 25 (0.8) | 5 (0.5) | 5 (4.2) | |
| Others | 110 (2) | 40 (1.9) | 65 (2.1) | 30 (3.1) | N/A | |
| Spinal cord injury | 850 (15.8) | 545 (26.5) | 290 (9.2) | 45 (4.7) | N/A | |
| Elixhauser comorbidity score | 4.82 ± 2.14 | 4.45 ± 2.05 | 5.13 ± 2.14 | 4.67 ± 2.28 | 6± 0 | |
| Insurance | ||||||
| Medicare | 3,820 (70.9) | 1,375 (66.9) | 2,265 (72.1) | 675 (70.7) | 70 (58.3) | |
| Medicaid | 225 (4.2) | 130 (6.3) | 80 (2.5) | 35 (3.7) | 10 (8.3) | |
| Private | 970 (18) | 380 (18.5) | 580 (18.5) | 180 (18.8) | 35 (29.2) | |
| Self-pay | 100 (1.9) | 65 (3.2) | 35 (1.1) | 15 (1.6) | 5 (4.2) | |
| No charge | 10 (0.2) | 10 (0.5) | N/A | N/A | N/A | |
| Others | 250 (4.6) | 90 (4.4) | 175 (5.6) | 50 (5.2) | N/A | |
| Patient location | ||||||
| “Central” counties of metro areas of ≥ 1 million population | 1,335 (24.8) | 470 (22.9) | 785 (25) | 270 (28.3) | 50 (41.7) | |
| “Fringe” counties of metro areas of ≥ 1 million population | 1,335 (24.8) | 520 (25.3) | 785 (25) | 240 (25.1) | 30 (25) | |
| Counties in metro areas of 250,000–999,999 population | 1,185 (22) | 515 (25.1) | 635 (20.2) | 175 (18.3) | 15 (12.5) | |
| Counties in metro areas of 50,000–249,999 population | 495 (9.2) | 205 (10) | 275 (8.8) | 80 (8.4) | 10 (8.3) | |
| Micropolitan counties | 555 (10.3) | 210 (10.2) | 325 (10.4) | 100 (10.5) | 15 (12.5) | |
| Not metropolitan or micropolitan counties | 465 (8.6) | 125 (6.1) | 325 (10.4) | 90 (9.4) | N/A | |
| Discharge disposition | ||||||
| Routine | 1,040 (19.3) | 445 (21.7) | 585 (18.6) | 165 (17.3) | 10 (8.3) | |
| Transfer to short-term hospital | 240 (4.5) | 110 (5.4) | 160 (5.1) | 20 (2.1) | N/A | |
| Transfer other: includes skilled nursing facility, intermediate care facility, another type of facility | 3,115 (57.8) | 1,065 (51.8) | 1,860 (59.2) | 595 (62.3) | 95 (79.2) | |
| Home Health Care | 640 (11.9) | 235 (11.4) | 370 (11.8) | 125 (13.1) | 15 (12.5) | |
| Against Medical Advice | 10 (0.2) | 5 (0.2) | 5 (0.2) | 50 (5.2) | N/A | |
| Died | 335 (6.2) | 190 (9.2) | 160 (5.1) | N/A | N/A | |
| Hospital charges (US dollar) | 162,423.63 ± 16,7112 | 184,558.78 ± 183,818 | 163,523.38 ± 161,991 | 150,966.64 ± 136,839 | 142,685.26 ± 241,209 | |
| Median household income | ||||||
| 0–25th percentile | 1,180 (21.9) | 470 (22.9) | 670 (21.3) | 225 (23.6) | 30 (25.0) | |
| 26th–50th percentile (median) | 1,400 (26.0) | 580 (28.2) | 815 (26.0) | 260 (27.2) | 20 (16.7) | |
| 51st–75th percentile | 1,490 (27.7) | 580 (28.2) | 870 (27.7) | 220 (23.0) | 30 (25.0) | |
| 76th–100th percentile | 1,215 (22.6) | 385 (18.7) | 730 (23.2) | 220 (23.0) | 40 (33.3) | |
Values are presented as mean±standard deviation or number (%).
NA, not available.
2) Socioeconomic characteristics
Overall Central counties (24.8%) and Fringe counties (24.8%) are the predominant locations of the patients. Twenty-seven point seven percent of the patients fell in the 51st to 75th percentile of the zip codes’ median household income. The most common insurance availed was Medicare (70.9%), followed by private insurance (18%) (Table 2).
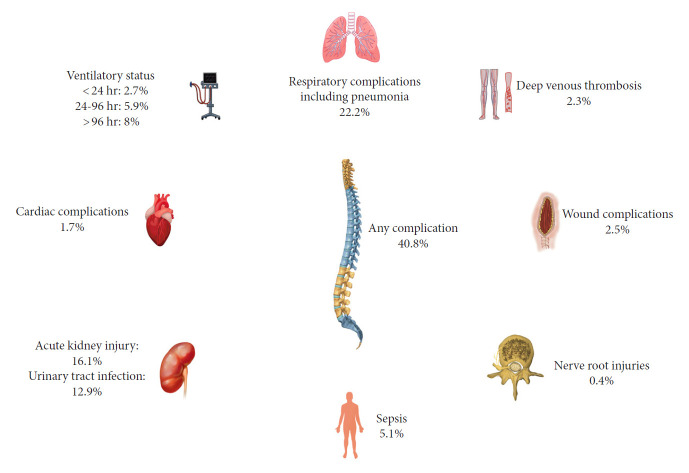
3) Surgical treatment and complications
A total of 2,365 patients (43.9%) underwent surgical treatment for the fractures. The most common surgery was fusion (71%), followed by corpectomy (29%). Fusion was the predominant surgery in all the groups. In the cervical level, 64.4% of the patients underwent 2 or more levels fusion. In thoracic fractures, 76.1% patients underwent 2 to 7 levels of fusion and 0.4% of the patients underwent more than 8 levels of the fusion. In lumbar fractures, 9.2% of the patients underwent 2 or more levels of fusion. The overall complication rate was 40.8% (Table 3). Respiratory complications, including pneumonia and respiratory insufficiency, were the predominant complications in the overall cohort (22.2%) as well cervical (27.7%), thoracic (21.5%), and lumbar (13%) levels (Fig. 2). Sacral fractures had lesser respiratory complications (13%). Cervical fracture patients (10.9%) required ventilatory support for more than 96 hours. The next common complication was acute kidney injury (AKI) (16.1%). Thoracic levels (18.3%) and lumbar levels (18.2%) had a higher proportion of AKI. Urinary tract infections (UTI) were found in 12.9% of the patients. Wound complications were found in 2.5% of the patients overall, with the lumbar level having the highest rate (5.2%). The cardiac complication rate was 1.7%, and the deep venous thrombosis rate was 2.3%. Sepsis was found in 5.1% of patients overall. The mean hospital stay was 11.44 days (SD, 12.57) overall. The in-hospital mortality rate was 5.7% overall, with the cervical level (7.9%) being higher than other levels. The mean hospital charges were $162,423.63 (SD, 167,112), with the cervical level having the highest charges ($184,558). Overall, the most common discharge disposition was to a skilled nursing facility or another type of facility for rehabilitation (57.8%), followed by discharge to home (19.3%).
Table 3.
Surgical management, complications, length of stay, and mortality (weighted frequencies)
| Variable | Overall | Cervical (n = 2,055) | Thoracic (n = 3,140) | Lumbar (n = 955) | Sacral (n = 120) |
|---|---|---|---|---|---|
| Surgery | 2,365 (43.9) | 1,010 (49.1) | 1,420 (45.2) | 385 (40.3) | 20 (16.6) |
| Fusion | 1,680/2,365 (71) | 625/1,010 (61.9) | 1,100/1,420 (77.5) | 225/385 (58.4) | 15/20 (75) |
| Corpectomy | 685/2,365 (29) | 385/1,010 (38.1) | 320/1,420 (22.5) | 160/385 (41.6) | 5/20 (25) |
| No. of levels fused | NA | 2/more = 64.4% | 2 to 7 levels = 76.1% | 2/more levels = 9.2% | NA |
| > 8 levels = 0.4% | |||||
| Any complication | 40.8% | 435/1,010 (43.1) | 590/1,420 (41.5) | 145/385 (37.7) | 5/20 (25) |
| Wound complications | 2.5% | 15/1,010 (1.5) | 40/1,420 (2.8) | 20/385 (5.2) | 5/20 (25) |
| Respiratory including pneumonia | 22.2% | 280/1,010 (27.7) | 305/1,420 (21.5) | 50/385 (13) | 0% |
| Ventilation < 24 hr | 2.7% | 30/1,010 (3) | 40/1,420 (2.8) | 10/385 (2.6) | 0% |
| Ventilation 24 hr–96 hr | 5.9% | 90/1,010 (8.9) | 65/1,420 (4.6) | 70/385 (7.8) | 0% |
| Ventilation > 96 hr | 8% | 110/1,010 (10.9) | 110/1,420 (7.7) | 10/385 (2.6) | 0% |
| Cardiac complications | 1.7% | 10/1,010 (1) | 35/1,420 (2.5) | 5/385 (1.3) | 0% |
| Acute kidney injury | 16.1% | 125/885 (12.4) | 260/1,420 (18.3) | 70/385 (18.2) | 0% |
| UTI | 12.9% | 105/1,010 (10.4) | 195/1,420 (13.7) | 45/385 (11.7) | 5/20 (25) |
| Nerve root injuries | 0.4% | 5/1,010 (0.5) | 5/1,420 (0.4) | 0% | 0% |
| DVT | 2.3% | 20/1,010 (2) | 35/1,420 (2.5) | 15/385 (3.9) | 5/20 (25) |
| Sepsis | 5.1% | 30/1,010 (3) | 75/1,345 (5.3) | 45/385 (5.2) | 5/20 (25) |
| In-hospital mortality | 135/2,365 (5.7) | 80/1,010 (7.9) | 70/1,420 (4.9) | 25/385 (6.5) | |
| Hospital stay (day) | 11.44 ± 12.57 | 12.17 ± 14.9 | 11.13 ± 11.16 | 12.65 ± 17.2 | 41.75 ± 54 (median, 13) |
Values are presented as number (%) or mean±standard deviation unless otherwise indicated.
NA, not available; UTI, urinary tract infection; DVT, deep venous thrombosis.
Fig. 2.
Distribution of overall cohort, spinal cord injury, and surgical treatments. NIS, Nationwide Inpatient Sample.
Logistic regression analysis was used after adjusting for the Elixhauser comorbidities and SCI, predominantly affecting the complication rate (Table 4). The probability of the complications by the fracture level was computed through the odds ratio with the lumbar level as the reference. Based on the regression analysis, there was no significant difference (p=0.45) in the complication rates based on the levels. The odds ratio of having a complication in the cervical level patients was 1.308 (95% confidence interval [CI], 0.829–2.064; p=0.247), 1.141 (95% CI, 0.722–1.803; p=0.5721) in the thoracic level, and 1.119 (95% CI, 0.698–1.795; p=0.6395) in the lumbar level; however, none of them were statistically significant. The presence of SCI increased the odds of having a complication by 2.164 times (95% CI, 1.722–2.72; p≤0.001), and a unit increase in Elixhauser comorbidity score increased the odds of having complications (p≤0.001). Age (p=0.296) and the presence of multiple fracture levels (odds ratio [OR], 1.073; 95% CI, 0.643–1.792; p=0.786) did not predict the complication rate. In-hospital mortality was predicted only by Elixhauser comorbidity score (p≤0.001) (Table 4).
Table 4.
Logistic regression analysis of factors predicting complications and in-hospital mortality
| Variable | Any complication |
In-hospital mortality |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age | NA | NA | 0.0518 | NA | NA | 0.0518 |
| Elixhauser comorbidity score | NA | NA | < 0.001 | NA | NA | < 0.001 |
| Presence of spinal cord injury | 2.164 | 1.722–2.72 | < 0.001 | Excluded in the model | ||
| Multiple levels | 1.073 | 0.643–1.792 | 0.7866 | 2.527 | 0.913–6.998 | 0.0743 |
| Cervical level | 1.308 | 0.829–2.064 | 0.2472 | 1.761 | 0.714–4.341 | 0.2186 |
| Thoracic level | 1.141 | 0.722–1.803 | 0.5721 | 0.536 | 0.211–1.362 | 0.1894 |
| Lumbar level | 1.119 | 0.698–1.795 | 0.6395 | 1.26 | 0.513–3.098 | 0.6131 |
OR, odds ratio; CI, confidence interval; NA, not available.
DISCUSSION
Spinal fractures are a relatively rare complication of AS patients. Since AS is a relatively less common rheumatological disease, the literature describing the patterns of spinal fractures and complications of surgical management is mainly in the form of single-center studies and systematic reviews. Through the NIS database, we aim to review the treatment patterns and complications for traumatic fractures in AS patients at the national level. In our study, the majority of the patients underwent nonoperative management (56.1%). Our data is not granular enough to distinguish different types of nonoperative management due to the coding bias. Our study's most common fracture level was thoracic, followed by cervical level, although it differs with a few studies [9-13] (Table 5). In the operated patients, 40.8% had at least one complication, with respiratory (22.2%) being the most common complication. The presence of the complications did not depend upon the fracture level rather dependent upon the Elixhauser comorbidities (p≤0.001) and the presence of the SCI (OR, 2.164; 95% CI, 1.722–2.72; p≤0.001). In our study, age was not a predictor of complication rate (p=0.296).
Table 5.
Literature review of ankylosing spondylitis with spinal fractures
| Study | Total no. of patients | Average age (yr) | Patients with fractures | Total fracture incidents | Fracture location | Complications with rates (%) | Median length of stay (day) | Mortality rate (%) |
|---|---|---|---|---|---|---|---|---|
| Teunissen et al. [10] (2017) | 2,089 | 69.3 | 172 | 189 | C: 104 (60.8) | Pneumonia (50.6), respiratory failure (6.4), altered mental status (6.4), UTI (4.3), wound infection (2.1) | 7 (3–15) | 24.6 |
| T: 72 (42.1) | ||||||||
| L: 26 (15.2) | ||||||||
| S: 3 (1.8) | ||||||||
| Longo et al. [11] (2015) | 110 | 59.2 | 86 | 110 | C: 110 (100.0) | Epidural (2.0) hematoma, pneumonia (5.0), infection (4.0), ARDS (2.0) | NA | 21.0 |
| T: 0 | ||||||||
| L: 0 | ||||||||
| S: 0 | ||||||||
| Rustagi et al. [12] (2017) | - | 63.4 | - | - | C: 53.0 | Overall 84.0: (pneumonia, respiratory failure) | NA | 32 |
| T: 41.9 | ||||||||
| L: 18.2 | ||||||||
| S: 1.5 | ||||||||
| Lukasiewicz et al. [9] (2016) | 939 | 68.4 | 939 | 1,076 | C: 53.0 | UTI (9.6), AKI (7), pneumonia (6.3) | NA | 6.6 |
| T: 41.9 | ||||||||
| L: 18.2 | ||||||||
| S: 1.5 | ||||||||
| Sedney et al. [17] (2016) | 38 | 74.0 | 38 | 38 | T: 87.0 | Reoperation (13) | NA | 13 |
| Multilevel: 13.0 | ||||||||
| Moussallem et al. [18] (2016) | 41 | 75.56 | 17 | 17 | C: 0 | Overall 67.5 (wound infection, DVT, PE, pneumonia) | NA | 5.0 |
| T: 30.0 | ||||||||
| L: 65.0 | ||||||||
| S: 2.5 | ||||||||
| Altun et al. [13] (2016) | 30 | 70.4 | 30 | 42 | C: 60.0 | Pseudoarthrosis (3.3), wound infection (3.3), pneumonia (3) | NA | 3.3 |
| T: 33.0 | ||||||||
| L: 3.0 | ||||||||
| S: 4.0 | ||||||||
| Robinson et al. [14] (2015) | 17,297 | 65.7 | 990 | 1131 | C: 53.9 | Pseudoarthrosis, wound infection | NA | 17 |
| T: 36.5 | ||||||||
| L: 25.0 | ||||||||
| S: 6 | ||||||||
| Lu et al. [19] (2013) | 28 | 54.2 | 25 | 25 | C: 7.0 | Overall 66.7 (respiratory failure, empyema, osteomyelitis) | NA | 0 |
| T: 52.0 | ||||||||
| L: 36.0 | ||||||||
| S: 5.0 | ||||||||
| Kouyoumdjian et al. [20] (2012) | 19 | 60.84 | 19 | 19 | C: 100.0 | Hematoma (5.3) | NA | 26 |
| T: 0 | ||||||||
| L: 0 | ||||||||
| S: 0 | ||||||||
| Backhaus et al. [21] (2011) | 119 | 67.0 | 119 | 129 | C: 39.5 | Wound infection (14), Pseudoarthrosis requiring revision (15) | NA | NA |
| T: 42.6 | ||||||||
| L: 17.8 | ||||||||
| S: 0 | ||||||||
| Caron et al. [5] (2010) | 112 | 62.4 | 112 | 122 | C: 55.0 | UTI (35), Wound infection (16), DVT (8) | NA | NA |
| T: 21.0 | ||||||||
| L: 8.0 | ||||||||
| S: 0 | ||||||||
| TL Jxn: 16.0 | ||||||||
| Sapkas et al. [22] (2009) | 20 | 55.4 | 20 | 20 | C: 35.0 | Wound infection (5), Hardware loosening (10) | NA | NA |
| T: 45.0 | ||||||||
| L: 5.0 | ||||||||
| S: 0 | ||||||||
| TL Jxn: 15.0 | ||||||||
| Kanter et al. [23] (2008) | 13 | 60.4 | 13 | 13 | C: 53.8 | Hardware failure (15), neurological decline (8) | NA | 8 |
| T: 46.2 | ||||||||
| L: 0 | ||||||||
| S: 0 | ||||||||
| Thumbikat et al. [24] (2007) | 18 | 56.2 | 18 | 18 | C: 78.0 | Neurologic decline after surgery (17) | 63–204 | 28 |
| T: 14.0 | ||||||||
| L: 5.5 | ||||||||
| S: 5 |
C, cervical; T, thoracic; L, lumbar; S, sacral; PE, pulmonary embolism; ARDS, acure respiratory distress syndrome; UTI, urinary tract infections; NA, not available; AKI, acute kidney injury; DVT, deep venous thrombosis.
1. Age
The mean age in our study was 71.63 years (SD, 13.21) with the range of 23 years to 90 years. Most of the studies reported a mean age of > 65 years. Our study is in agreement with these studies [9-12,14]. As age increases, the severity of the disease increases and the chances of fall, predisposing to spinal fractures in these patients. Few single-center studies reported age as an independent predictor of mortality in AS patients with spinal fractures [5], the inherent limitations in the NIS data precludes us from doing a survival analysis. Also, in our study, the in-hospital mortality rate was not affected by age (p=0.051).
2. Sex
Our study showed a male predominance (83.8%), in line with the results of other studies. Interestingly in the sacral fractures, there was a female predominance (54.2%). Evidence shows the HLA-B27 allele (most important allele in AS) being less often positive in women, explaining the male predominance. Another interesting genetic study in AS patients showed 1,522 unique gene expressions in males and 291 genes in women compared to controls in the general population [15]. Hormones play an essential role in modulating the pain mechanisms, inflammation, and syndesmophytes development [16]. Rusman et al. [16] in their review, reported that although men have a higher radiological progression, the disease burden is equal.
3. Spinal Cord Injury
The rate of SCI was 15.8% in our study. SCI was associated with a higher chance of postoperative complications in our study. Westerveld et al. [4] reported an SCI incidence of 67.2% in 232 AS patients. Another study by Caron et al. [5] reported an incidence of 58%. In another older NIS database study, the incidence of SCI reported was 21.2%. There are significant discrepancies between the institutional cohorts and NIS data, reflecting the coding patterns and bias in the NIS sample. Also, the chance of having a delayed SCI in AS patients cannot be underestimated. Harboring an unstable fracture that was either missed in the initial evaluation or ignored by the patients as the injury is trivial can progress to a delayed SCI. Teunissen et al. [10] in their study, reported a delay in diagnosis of spinal fracture in 44.2% of the patients. The delay in diagnosis was associated with SCI in 4.1% of the cases. Similarly, Caron et al. [5] reported an incidence of 36.8% delayed diagnosis in their series. Hence it is recommended to evaluate for a spinal fracture in AS patients with persistent pain after minor fall/trauma even though the pain is not disabling.
4. Complication Rates
Our study showed that at least one complication was present in 40.8% of the patients who underwent surgical treatment. Respiratory complication was the most common (22.2%), followed by AKI (16.1%) and UTI (12.9%). Most of the studies showed significant morbidity and complications in the AS patients irrespective of the treatment [17-24]. Based on these studies, the complications might be a manifestation of physiological endpoints of organ modeling in AS rather than the procedures per se (Fig. 3). The majority of people are near 70 years with a mean comorbidity score of 4.82, predisposing them to multiple postoperative complications. Our study showed ventilator dependency of more than 96 hours in 8% of the people, with cervical patients being higher (10.9%) than others. A Danish National registry reported 57.6% of AS patients have at least one or more comorbidities [25]. Interestingly they also reported that AS with pneumonia as a cause of admission did not increase the mortality rates. Although intriguing, our study cannot be compared with this registry as they differ in population sets. Westerveld et al. reported higher complications than the control population (85.7% vs. 48.7%) in the AS patients [26]. Lukasiewicz et al. [9] reported that fracture location did not correlate with the adverse events in agreement with our study. However, we included only inpatient complications, which can underreport the delayed complications if post-discharge was also considered.
Fig. 3.
Showing the distribution of the complications.
5. Limitations
Our study has several limitations. The lack of SCI severity grading (pre-and postinjury), mechanism of the injury, readmission data due to complications, and long-term follow-up were a few, limiting us to discuss only the early complications in the postoperative period. Along with these, the preoperative comorbidities specific to AS which can influence the postoperative outcome were not available. We reduced this bias slightly by adjusting the Elixhauser comorbidities and SCI while calculating the odds of complication by the fracture level. Again, we do not have the information on the location of the fracture in the vertebrae (Denis 3 column-wise). Also, the NIS data comes with inherent selection and sampling bias along with interrater coding bias. The details regarding the nonoperative management in the data were also lacking.
CONCLUSION
AS patients with spinal fractures have higher postoperative complications. The most common fracture location was thoracic in our study, although it differs with few studies, with SCI occurring in 1/6th of the patients. Although with significant limitations, we intend to provide a bird's eye view of patterns, management, and complications in AS patients with spinal fractures.
Acknowledgments
This study was supported in part by U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center.
Footnotes
The authors have nothing to disclose.
REFERENCES
- 1.Olivieri I, D'Angelo S, Palazzi C, et al. Diffuse idiopathic skeletal hyperostosis: differentiation from ankylosing spondylitis. Curr Rheumatol Rep. 2009;11:321–8. doi: 10.1007/s11926-009-0046-9. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs WB, Fehlings MG. Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Neurosurg Focus. 2008;24:E12. doi: 10.3171/FOC/2008/24/1/E12. [DOI] [PubMed] [Google Scholar]
- 3.Cooper C, Carbone L, Michet CJ, et al. Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol. 1994;21:1877–82. [PubMed] [Google Scholar]
- 4.Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18:145–56. doi: 10.1007/s00586-008-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caron T, Bransford R, Nguyen Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976) 2010;35:E458–64. doi: 10.1097/BRS.0b013e3181cc764f. [DOI] [PubMed] [Google Scholar]
- 6.Ahoniemi E, Alaranta H, Hokkinen EM, et al. Incidence of traumatic spinal cord injuries in Finland over a 30-year period. Spinal Cord. 2008;46:781–4. doi: 10.1038/sc.2008.53. [DOI] [PubMed] [Google Scholar]
- 7.Whang PG, Goldberg G, Lawrence JP, et al. The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. J Spinal Disord Tech. 2009;22:77–85. doi: 10.1097/BSD.0b013e3181679bcb. [DOI] [PubMed] [Google Scholar]
- 8.Moore BJ, White S, Washington R, et al. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55:698–705. doi: 10.1097/MLR.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 9.Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal fracture in patients with ankylosing spondylitis: cohort definition, distribution of injuries, and hospital outcomes. Spine (Phila Pa 1976) 2016;41:191–6. doi: 10.1097/BRS.0000000000001190. [DOI] [PubMed] [Google Scholar]
- 10.Teunissen FR, Verbeek BM, Cha TD, et al. Spinal cord injury after traumatic spine fracture in patients with ankylosing spinal disorders. J Neurosurg Spine. 2017;27:709–16. doi: 10.3171/2017.5.SPINE1722. [DOI] [PubMed] [Google Scholar]
- 11.Longo UG, Loppini M, Petrillo S, et al. Management of cervical fractures in ankylosing spondylitis: anterior, posterior or combined approach? Br Med Bull. 2015;115:57–66. doi: 10.1093/bmb/ldv010. [DOI] [PubMed] [Google Scholar]
- 12.Rustagi T, Drazin D, Oner C, et al. Fractures in spinal ankylosing disorders: a narrative review of disease and injury types, treatment techniques, and outcomes. J Orthop Trauma. 2017;31 Suppl 4:S57–74. doi: 10.1097/BOT.0000000000000953. [DOI] [PubMed] [Google Scholar]
- 13.Altun I, Yuksel KZ. Ankylosing spondylitis: patterns of spinal injury and treatment outcomes. Asian Spine J. 2016;10:655–62. doi: 10.4184/asj.2016.10.4.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson Y, Willander J, Olerud C. Surgical stabilization improves survival of spinal fractures related to ankylosing spondylitis. Spine (Phila Pa 1976) 2015;40:1697–702. doi: 10.1097/BRS.0000000000001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gracey E, Yao Y, Green B, et al. Sexual dimorphism in the Th17 signature of ankylosing spondylitis. Arthritis Rheumatol. 2016;68:679–89. doi: 10.1002/art.39464. [DOI] [PubMed] [Google Scholar]
- 16.Rusman T, van Bentum RE, van der Horst-Bruinsma IE. Sex and gender differences in axial spondyloarthritis: myths and truths. Rheumatology (Oxford) 2020;59:iv38–46. doi: 10.1093/rheumatology/keaa543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sedney CL, Daffner SD, Obafemi-Afolabi A, et al. A comparison of open and percutaneous techniques in the operative fixation of spinal fractures associated with ankylosing spinal disorders. Int J Spine Surg. 2016;10:23. doi: 10.14444/3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moussallem CD, McCutcheon BA, Clarke MJ, et al. Perioperative complications in open versus percutaneous treatment of spinal fractures in patients with an ankylosed spine. J Clin Neurosci. 2016;30:88–92. doi: 10.1016/j.jocn.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 19.Lu ML, Tsai TT, Lai PL, et al. A retrospective study of treating thoracolumbar spine fractures in ankylosing spondylitis. Eur J Orthop Surg Traumatol. 2014;24 Suppl 1:S117–23. doi: 10.1007/s00590-013-1375-y. [DOI] [PubMed] [Google Scholar]
- 20.Kouyoumdjian P, Guerin P, Schaelderle C, et al. Fracture of the lower cervical spine in patients with ankylosing spondylitis: retrospective study of 19 cases. Orthop Traumatol Surg Res. 2012;98:543–51. doi: 10.1016/j.otsr.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Backhaus M, Citak M, Kalicke T, et al. Spine fractures in patients with ankylosing spondylitis: an analysis of 129 fractures after surgical treatment. Orthopade. 2011;40:917-20, 22-4. doi: 10.1007/s00132-011-1792-8. (German) [DOI] [PubMed] [Google Scholar]
- 22.Sapkas G, Kateros K, Papadakis SA, et al. Surgical outcome after spinal fractures in patients with ankylosing spondylitis. BMC Musculoskelet Disord. 2009;10:96. doi: 10.1186/1471-2474-10-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanter AS, Wang MY, Mummaneni PV. A treatment algorithm for the management of cervical spine fractures and deformity in patients with ankylosing spondylitis. Neurosurg Focus. 2008;24:E11. doi: 10.3171/FOC/2008/24/1/E11. [DOI] [PubMed] [Google Scholar]
- 24.Thumbikat P, Hariharan RP, Ravichandran G, et al. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine (Phila Pa 1976) 2007;32:2989–95. doi: 10.1097/BRS.0b013e31815cddfc. [DOI] [PubMed] [Google Scholar]
- 25.Holland-Fischer M, Thomsen RW, Tarp U, et al. Ankylosing spondylitis and mortality following hospitalised pneumonia: a population-based cohort study. RMD Open. 2020;6:e001140. doi: 10.1136/rmdopen-2019-001140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Westerveld LA, van Bemmel JC, Dhert WJ, et al. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. 2014;14:729–40. doi: 10.1016/j.spinee.2013.06.038. [DOI] [PubMed] [Google Scholar]