Abstract
As per the World Health Organization, a disaster is defined as “an event that occurs in most cases suddenly and unexpectedly, causing severe disturbances to people or objects affected by it, resulting in the loss of life and harm to the health of the population.” A number of health issues are often reported following disasters, such as physical and psychological trauma, infections, malnutrition, and cardiovascular events. Among these, venous thromboembolism is deemed serious and thus should be taken into consideration. Indeed, its risk has been demonstrated to increase following earthquakes, floods, burns, and intoxications. The recent coronavirus pandemic summarizes some of the main triggering factors involved in acute and chronic venous disease development in a disaster setting: inflammation, infection, lockdown-induced reduced mobility, potential malnutrition, and overweight.
Proper venous risk assessment and guideline application have been determined to be essential in disaster management, particularly in the current time in which sheltering could lead to a potential exacerbation of the pandemic, which can only increase the risk for venous thrombotic diseases.
Global scientific teamwork is needed to make the recommendations as evidence-based and as homogeneous as possible among continents.
In this present review, we focus on how earthquakes impact venous thromboembolism, including an analysis of other disaster-related conditions, such as burns and intoxication. (This is a review article based on the informative seminar of the 40th Annual Meeting of Japanese Society of Phlebology.)
Keywords: disasters, earthquake, burns, intoxication, venous disease
Introduction
According to the World Health Organization, a disaster is defined as a “sudden phenomenon of sufficient magnitude to overwhelm the resources of a hospital, region, or location requiring external support.”1)
Disasters are defined as “natural” whenever related to geophysical, meteorological, hydrological, climatological, or biological phenomena. On the contrary, disasters can be “man-made” if related to criminal terrorist attacks or technological incidents.
The latter may be referred in an industrial or transportation context.2) The different types of disaster can be interconnected, for example, the 2011 Tohoku earthquake that led to a tsunami, which consequently led to the Fukushima Daiichi nuclear disaster.
Disasters are far more frequent than usually thought. In fact, more than 20,000 mass disasters have occurred since 1900, which resulted in 1.3 million deaths and 4.4 billion individuals in need of emergent assistance.
Floods, storms, droughts, heatwaves, and other extreme weather events have been accounted for 91% of these disasters.3)
The disasters may impact global health at multiple levels: direct trauma, challenging weather conditions, and direct contact with animals and insects in precarious sheltering leading to possible outbreaks of contagious infections. Foodborne illnesses, malnutrition, and psychological casualties should also to be taken into consideration. Lower limb chronic venous disease is an extremely frequent pathology, affecting more than half of the adult population in various severities.4)
This condition leads to a significantly increased risk of venous thrombosis.5,6) An increased incidence of venous thromboembolism in subjects exposed to disasters, in particular of geophysical nature (earthquakes and tsunami), has been reported for decades now.7)
Thus, in this present review, we aim to analyze the available literature on the topic of how disasters impact venous disease, focusing on earthquakes, while also examining the roles of burns and intoxications.
Materials and Methods
This present review methodology was done in accordance to the Quality of Reporting of Meta-analyses (QUOROM) indications8) together with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement9) and its most recent update.10)
Searching
The literature search was performed in PubMed, Embase, Cinahl, and the Cochrane Library up to May 30, 2020. It focused on all papers dealing with disaster conditions and venous disease by using the following mesh terms: “disasters,” “venous thrombosis,” “varicose veins,” “embolism,” “embolism and thrombosis,” and “pulmonary embolism.” The papers were screened on their abstracts and, if considered suitable, entirely reviewed for inclusion. “Related articles” links and references of the assessed papers were evaluated as well.
Selection
The review focused on topics dealing with venous disease (thromboembolism and/or chronic venous disease) and earthquakes or tsunami or flood. Further narrative search was performed on the topic on how burns and intoxication impact lower limb venous disease. No specific restrictions were made on the population type, number of enrolled subjects, follow-up length, and publication year. Only papers written in English were included.
Contributions coming from not indexed and/or from not English written journals were included only if considered of significant value for the revision.
Venous thromboembolism incidence and risk were considered as the main outcome.
Validity assessment
Maximum validity was given to randomized trials including concealed allocation, assessors blinding, and longer than 1-week follow-up.
Data abstraction
A reviewer (SG) independently screened the titles and abstracts for eligibility. The selected full papers are then assessed by three independent authors (SG, YWC, and EM).
Eventual disagreement between the reviewers was solved by a fourth reviewer (OB).
Data extraction was performed in duplicate by both reviewers using a standardized form, reporting the study description, type, and main results.
Study characteristics
The review included randomized controlled trials, non-randomized controlled trials, cohort and case-control studies, retrospective investigations, and expert opinion articles.
Results
Figure 1 reports the systematic selection process for publications related to earthquakes and venous thromboembolism. From an initial pool of 1483 references, 22 represented articles were deemed worthy to be assessed in their entireness. After a detailed revision, the final selection included 17 publications.
Fig. 1 Systematic selection of publications related to earthquakes and venous thromboembolism.
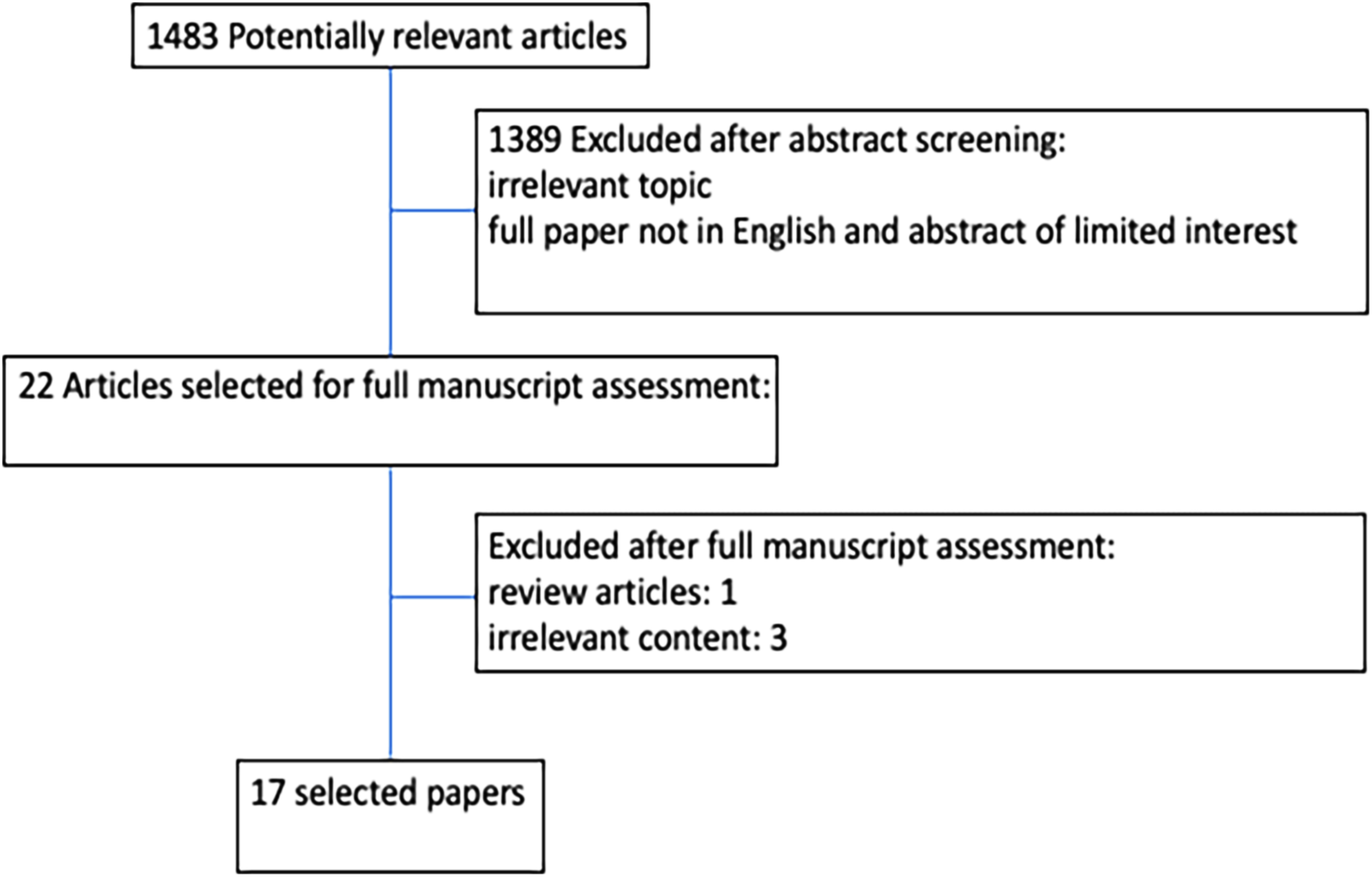
Table 1 shows the main features of the selected investigations. These publications focused on deep venous thromboembolism incidence following earthquakes. Among these papers, 11 also included analysis on the possible risk factors associated with thromboembolism following the disaster.11–21)
Table 1 Selected publications dealing with earthquake impact on venous disease.
| First author, year | Disaster | Population | DVT | PE | Assessment | F-up | Identified risk factors | Study design |
|---|---|---|---|---|---|---|---|---|
| Sato K, 2019 | 2016 Kumamoto Earthquake | 1663 | 10.3% | NR | Questionnaire Portable US D-dimer | 1 m | Age ≥70 y.o. Sleep medication Edema Varicose veins | Consecutive case series |
| Watanabe H, 2008 | 2004 Niigata earthquake | NR | NR | 9 times increase | CT | 1 m | No statistical calculation performed. Suggested role of: Automobile sheltering | Consecutive case series |
| Inoue K, 2006 | 2004 Chuetsu District earthquake | NR | NR | 9 cases | CT | NR | No statistical calculation performed. Suggested role of: Automobile sheltering | Consecutive case series |
| Shibata M, 2014 | 2011 Japan earthquake and tsunami | 269 | 24% Calf DVT | NR | Questionnaire Physical exam Calf ultrasonography | 1 m | Lower limb trauma Reduced frequency of urination Sleeping in a vehicle | Consecutive case series |
| Sakuma M, 2006 | 2004 Mid Niigata earthquake | 117 | NR | 10 cases | Questionnaire CT Population divided in high (>5%) and low evacuee area | 1 m | High evacuee Female Suggested role of automobile sheltering | Retrospective analysis |
| Shibata M, 2017 | 2011 Japan earthquake and tsunami | 3316 | 11.85% distal DVT | NR | US | 26 m | -Older -Symptomatic -Female -VTE history -Attempting to perform daily exercise | Consecutive case series |
| Tauqir SF, 2007 | Pakistan 2005 earthquake | 194 | 2% | 1 case | US | 2 m | NR | Cross-sectional retrospective |
| Guner SI, 2014 | 2011 Van earthquake | 46 affected by crush syndrome | NR | 1 case | US, CT | NR | NR | Descriptive analysis |
| Sueta D, 2017 | 2016 Kumamoto earthquake | 1 | NR | 1 case | CT | NR | -Vehicle sheltering -Oral contraception | Clinical case |
| Aoki T, 2013 | 2011 Japan earthquake and tsunami | NR | 52 not specified pulmonary thromboembolism cases | NR | 1 y | NR | Retrospective analysis | |
| Ueda S, 2012 | 2011 Japan earthquake and tsunami | 8630 | 2.2% | NR | US | 3 m | -Flooded shelters | Consecutive case series |
| Rathore MF, 2008 | Pakistan 2005 earthquake | 187 survivors with acute spinal injury | 4.8% | NR | US | 2.5 m | -No influence of age, gender (P=0.4), spinal injury grade, fracture | Prospective observational |
| Matsukawa M, 2018 | Kumamoto 2016 earthquake | 76 | 32 | 54 | US, CT | 4 m | NR -DOACS found to be safe and effective in reducing recurrence, without increasing bleeding | Prospective observational |
| Modena MG, 2017 | 2012 Modena earthquake | 1401 | DVT-PE reported together: 64 vs 9 of the year before | US, CT | 1 y | Female | Retrospective analysis | |
| Groves CC, 2017 | 2015 Nepal earthquake | 117 spinal cord injuries | 6% | NR | US | 14 m | NR | Descriptive |
| Terakami T, 2009 | 2007 Ishikawa earthquake | 198 | 10.6% | NR | Questionnaires US D-dimer | NR | NR | Descriptive |
| Ueda S, 2014 | 2011 Japan earthquake and tsunami | 701 | 190 | NR | US | 9 m | -Flooded shelters -Temporary emergency houses | Consecutive case series |
DVT: deep venous thrombosis; PE: pulmonary embolism; F-UP: follow-up; NR: not reported; m: months; CT: computed tomography; US: ultrasound; y: year; DOACS: direct oral anticoagulants; VTE: venous thromboembolism
The total study population in this review included 16,916 subjects who were exposed to the earthquake. In three papers, information on the number of subjects was not reported. Mean follow-up after the disaster was 6 months, ranging from 1 to 26 months. No further details were provided regarding gender, age, and comorbidities distribution. No randomized comparative trials were found on the topic. All the identified investigations were consecutive case series or cross-sectional retrospective analysis.11–27)
An assessment of homogeneity at baseline of the herein reported scientific works was not feasible. Following the 2020 Cochrane Handbook for Systematic Reviews of Interventions publication on how to report risk of bias in scientific literature review,28) an evaluation of the bias risk assessment for the reviewed papers was performed: the reviewed publications showed lacking random sequence generation and allocation concealment, partly due to the unpredictable nature of the disaster and partly because of lacking study design (e.g., possible randomization in use of graduated elastic stockings for thrombosis prevention following an earthquake).
Blinding of participants, personnel was missing as well. Outcome assessment was deemed to be extremely incomplete, as exemplified by the lack of screening for distal deep venous thrombosis rather than full leg assessment. The vast presence of these biases made the creation of a detailed risk bias table futile, considering all the investigations would have resulted in high risk of bias.
Main findings on earthquake impact on venous disease
In 2006, Sakuma et al. have reported an increased incidence of pulmonary embolism following the 2004 Mid Niigata Prefecture earthquake in Japan. The investigation focused on the high pulmonary embolism rate in evacuees. Moreover, female gender and the use of the automobile as night shelter were found to be potentially associated with increased venous thromboembolic risk.15)
The role of automobile sheltering in thromboembolism was highlighted by the Inoue in 2006, following their analysis of the 2004 Chuetsu District earthquake.13)
In 2007, the analysis of Tauqir et al. on the 2005 earthquake in Pakistan has pointed out an increased percentage of venous thrombosis in the population hit by the disaster, but no risk factor analysis was performed.23) Following the same event, Rathore et al. focused on 187 patients with spinal cord injuries due to disaster-related direct trauma. No influence on the thrombotic risk was reported for age, gender, spinal injury grade, or eventual fractures.19) Examining the patients affected by post-traumatic spinal cord injuries, Groves et al. have confirmed the increased venous thrombosis incidence after the 2015 earthquake in Nepal.26) In 2008, Watanabe et al., who conducted a study on the 2004 Niigata earthquake, confirmed the possible role of automobile sheltering in the increased incidence of pulmonary embolism.12) In 2009, Terakami et al. reported a significantly increased deep venous thrombosis incidence rate (10.6% of the affected population) following the 2007 Ishikawa earthquake.27) In 2012, Ueda et al. pointed out the role of flooded shelters on the increasing risk of venous thrombosis after the 2011 Japan earthquake and tsunami.18) The Shibata analysis on the same event highlighted lower limb trauma, reduced frequency of urination, and sleeping in an automobile as conditions associated with a significant increase in calf deep venous thrombosis.14) In 2014, another study from Ueda confirmed the role of flooded shelters and temporary emergency housing in the increased venous thrombosis rate after the 2011 Japan earthquake.21) A subsequent publication of Shibata analysis of the same 2011 Japan earthquake confirmed advanced age and the female gender as potential risk factors for venous thrombosis following the geophysical disaster. In the same publication, potential risk factors were also identified in the symptomatic cases as well as those with a history of venous thromboembolism.16) Pulmonary embolism risks were analyzed by Sueta et al. on the Kumamoto 2016 earthquake, wherein it was confirmed that automobile sheltering and oral contraceptives are potential risk factors.17)
Matsukawa et al. have also examined the same catastrophic event, but focusing on the use of direct oral anticoagulants in post-disaster thromboprophylaxis, highlighting their safety and potentials in reducing thrombotic recurrence, without increase in bleeding.25) In 2019, Sato et al. assessed 1663 subjects exposed to the Kumamoto 2016 earthquake and reported a deep venous thrombosis incidence of 10.3%; potential risk factors identified were as follows: age >70, use of sleep medication, edema, and varicose veins.11)
Main findings on how burns and intoxications impact venous disease
Table 2 presents the results of the search on the topic of how burns and intoxication impact venous thromboembolism risk. Potential risk factors for venous thrombosis following burns were identified as follows: wound infections, prolonged hospital stay, obesity, total body surface area affected by burn, prolonged immobility, and D-dimer elevation.29–31) Harrington et al. have looked into the risk of pulmonary embolism after burns, wherein advanced age and total body surface area were identified as two potential factors.32) Organophosphate or carbon monoxide intoxication was categorized in the disaster category as “man-made” event, following, for example, an industrial accident. A longitudinal cohort study demonstrated the increased risk of both deep venous thrombosis and pulmonary embolism associated with organophosphate intoxication.33) A retrospective case-control study demonstrated carbon monoxide intoxication was associated with an increased risk only of venous thrombosis.34)
Table 2 Selected publications dealing with burns and intoxication impact on venous disease.
| First author, year | Disaster | Population | DVT | PE | Assessment tools | F-up | Identified risk factors | Study design |
|---|---|---|---|---|---|---|---|---|
| Wahl WL, 2001 | Burns | 327 | 2.4% | NR | US | NR | -Infections -Hospital length of stay | Review |
| Harrington D, 2001 | Burns | 1300 | 2.9% | 2.9% | US, CT | 5.5 y | -Age -TBSA | Retrospective analysis |
| Ahuja RB, 2016 | Burns | 50 | 8% | NR | US | Not specified | -BMI -TBSA -Prolonged immobility -Longer duration of stay -D-dimer (day 5) | Randomized controlled trial |
| Lim YP, 2015 | Organophosphate intoxication | 9223 | Adjusted hazard ratio=1.55 | Adjusted hazard ratio=1.44 | US | 11 y | OP intoxication | Longitudinal cohort study |
| Chung W, 2015 | Carbon monoxide poisoning | 8316 | 3.85-fold higher risk of DVT | Not significantly associated with risk of PE | US, CT | 11 y | Carbon monoxide intoxication | Retrospective case-control |
| Shen C, 2017 | Alcohol intoxication | 61,229 | Risk of DVT=3.40 higher | Risk of DVT=3.53 higher | US, CT | 10 y | Alcohol intoxication | Retrospective case-control |
DVT: deep venous thrombosis; PE: pulmonary embolism; F-UP: follow-up; NR: not reported; CT: computed tomography; US: ultrasound; y: year; BMI: body mass index; TBSA: total body surface area; OP: organophosphate intoxication
On the other hand, alcoholism should also be considered as a form of intoxication given its high prevalence in the society resembling a form of disaster.35) In a large population study, Shen et al. demonstrated an increased risk of both deep venous thrombosis and pulmonary embolism associated with alcoholism.36)
Discussion
A 2019 review has reported the association of earthquakes with a number of cardiovascular events: mainly sudden cardiac death, myocardial infarction, cardiomyopathy, heart failure, stroke, arrhythmias, hypertension, and pulmonary embolism. The increased incidence was evident in post-disaster time, ranging from few hours up to several months.37)
Disasters’ effects on the cardiovascular system were reported even 10 years after Hurricane Katrina.38)
Subjects hit by earthquakes and natural disasters often have be evacuated to emergency shelters, which, in turn, could lead to hypomobility and poor hygiene. In particular, crowded and/or flooded shelters can increase the risk of contagious diseases, as reported by Kawano research group following the Great Eastern Japan earthquake.39) In this sheltering scenario, acute respiratory infections and acute gastroenteritis were the most frequently reported conditions.40)
In these times of pandemic brought about by COVID-19, proper knowledge on the literature related to the topic and “preparedness” for facing the eventual disaster emergency is of paramount importance.
Indeed, sheltering in these times could represent an extremely challenging situation for an already strained public health system.41) This difficulty becomes even more evident as COVID-19 has been clearly associated with an increased risk of venous thrombosis per se,42) with 4.5% bilateral deep venous thrombosis reported even in patients hospitalized in non-intensive care units.43) Among the investigated disasters, earthquakes was determined to be the most common topic, with its significant increase in terms of risk for venous thrombosis. Experiencing sheltering after an earthquake in this pandemic would definitely stretch preparedness at multiple levels. An example of the need of having sonographers ready to detect the eventual thrombosis was nicely reported already by Shimura.44) A multispecialty approach to the disaster management was nicely outlined by Hata, focusing on the central role of the general practitioners as health professionals, as they are aware of patients’ risk factors, particularly in case of pro-thrombotic post-disaster scenarios.45) From the herein review, the same pro-thrombotic nature of the post-earthquake condition became as evident as the need of properly organized shelters allowing proper movement, distancing, and hygiene to their inhabitants. At the same time, the heterogeneity encountered in the currently available data collections on the topic rendered a meta-analysis impossible to be performed. The authors involved in all the assessed papers have to be congratulated for both their scientific effort and the will of collecting data in such a challenging context for the benefit of all, especially, the ones who will have to face upcoming disasters. The herein presented data suggest the importance of clear protocols of data collection for venous thromboembolism incidence assessment and related risk factor identification. An example of the unmet evidence-based need in this current literature is the lack of ultrasound screening performed along the limb rather than just at the calf region. While the below knee scanning demonstrated to be of great clinical use, particularly considering the difficulty of performing a whole leg scan in the real-world disaster environment,16) future investigations aimed to collect data suitable for meta-analysis should follow the same scanning protocol. In the papers assessed in this review, no data were found on the prophylactic/therapeutic measures adopted for thrombosis control in the study population after a disaster, with the exception of the investigation of Matsukawa which examined the potential role of direct oral anticoagulants.25)
Particularly in pandemic time, the possibility of using drugs not requiring constant monitoring and blood sampling is deemed appealing. Nevertheless, as per this present review, proper studies specifying a homogeneous protocol including drugs and/or graduated compression stocking use for venous thrombosis prevention/treatment are missing in the disaster context. Family history of thrombosis was recognized as a potential risk factor for post-disaster thrombosis by Shibata et al.16) This finding highlighted the importance of proper reporting of comorbidities in future investigations on the topic. Indeed, the currently available literature has failed to examine information as regards the personal thrombotic risk assessment of the subjects affected by thrombosis following a disaster.
A special focus should also be placed on the monitoring of patients affected by physical trauma following a disaster. According to Rathore paper, fractures and spinal injury grade were not associated with an increase in the thrombotic risk following the Pakistan 2005 earthquake.19)
Yet, Groves identified an increased thrombotic incidence in post-earthquake crash syndrome patients.26) Special care should also be placed in the detection of fat embolism after a fracture: a condition underestimated following earthquakes as per a study conducted by Wang et al.46) The potential benefits of proper rehabilitation following earthquake-induced physical trauma, including the venous thrombosis aspect, were described by Li et al.47) Another aspect that should not be underestimated is the disaster impact on mental health.48) One should always keep in mind that the most advanced stages of chronic venous disease are often characterized by a depressive symptomatology and related hypomobility, thus inducing a vicious circle that could lead to worsening lower limb function.49) Chronic venous disease per se is a significant risk factor for venous thromboembolism.50) As per the investigation published by Sato et al., varicose veins are considered a potential risk factor in the specific context of a disaster like the 2016 Kumamoto earthquake.11) Future investigations should always include an assessment of the study population characteristics in terms of chronic venous disease comorbidities. Moreover, they should include the details of disease stage, in order to create more homogenous groups at the baseline of the investigation. The same attention should also be given to gender and age, as potential risk factors.20)
For example, in the context of the female gender, thrombotic risk can change significantly with menopause; thus, assessing gender without considering age may lead to potential bias.51) The same need for homogenous data collection in order to generate strong evidence-based recommendations is important in the context of burn and intoxications as potential causes of thromboembolism. The amount of literature found on the topic in this review is extremely scarce, yet extremely interesting and useful for further research on the topic.
Indeed, as reported by Giarratano,52) disaster research remained an open field, full of difficulties, but also of opportunities for valuable data collection in hopes to improve assistance to patients afflicted by both the disease and the disaster.
Conclusion
Disasters are not rare events, and they require immediate action for containment due to devastating health threat. A literature body is identified by this review, pointing out the incidence of venous thromboembolism associated with earthquakes.
Burns and intoxications have only been partially investigated as potential risk factors for thromboembolism, but preliminary data clearly showed the need for further research on these topics considering their potential impact on venous health. Homogenous data collection protocols are needed in order to facilitate future meta-analysis on the topic of disaster and venous thromboembolism. The topic becomes of even greater importance considering the COVID-19 pandemic, its direct pro-thrombotic action and on top of a potentially catastrophic disaster, forcing those affected to aggregate in a poorly prepared shelter. The consequence is unimaginable.
Acknowledgments
The authors would like to thank Dr. Anselmo Pagani, a research fellow at Sant’Anna University Hospital of Ferrara-Italy, for his technical contribution to the manuscript editing.
Disclosure Statement (COI)
Gianesini Sergio: No conflict of interest in the subject matter or materials discussed in the manuscript.
Menegatti Erica: No conflict of interest in the subject matter or materials discussed in the manuscript.
Bottini Oscar: No conflict of interest in the subject matter or materials discussed in the manuscript.
Chi Yung Wei: No conflict of interest in the subject matter or materials discussed in the manuscript.
Author Contributions
Study conception: SG
Data collection: SG, YWC; EM
Analysis: SG, YWC, OB
Investigation: SG, YWC; EM
Writing: SG, YWC
Funding acquisition: no funding
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
This is a review article based on the informative seminar of the 40th Annual Meeting of Japanese Society of Phlebology.
References
- 1).Puryear B, Gnugnoli DM. Emergency Preparedness. 2020 Sep 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. [PubMed]
- 2).de Boer J. Definition and classification of disasters: introduction of a disaster severity scale. J Emerg Med 1990; 8: 591-5. [DOI] [PubMed] [Google Scholar]
- 3).The International Disaster Database. Available at: https://www.emdat.be
- 4).Davies AH. The seriousness of chronic venous disease: a review of real-world evidence. Adv Ther 2019; 36 Suppl 1: 5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Müller-Bühl U, Leutgeb R, Engeser P, et al. Varicose veins are a risk factor for deep venous thrombosis in general practice patients. Vasa 2012; 41: 360-5. [DOI] [PubMed] [Google Scholar]
- 6).Chang SL, Huang YL, Lee MC, et al. Association of varicose veins with incident venous thromboembolism and peripheral artery disease. JAMA 2018; 319: 807-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Sakuma M, Nakamura M, Hanzawa K, et al. Acute pulmonary embolism after an earthquake in Japan. Semin Thromb Hemost 2006; 32: 856-60. [DOI] [PubMed] [Google Scholar]
- 8).Moher D, Cook DJ, Eastwood S, et al. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet 1999; 354: 1896-900. [DOI] [PubMed] [Google Scholar]
- 9).Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339 jul21 1: b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Page MJ, McKenzie JE, Bossuyt PM, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol 2021; 134: 103-12. [DOI] [PubMed] [Google Scholar]
- 11).Sato K, Sakamoto K, Hashimoto Y, et al. Risk factors and prevalence of deep vein thrombosis after the 2016 Kumamoto Earthquakes. Circ J 2019; 83: 1342-8. [DOI] [PubMed] [Google Scholar]
- 12).Watanabe H, Kodama M, Tanabe N, et al. Impact of earthquakes on risk for pulmonary embolism. Int J Cardiol 2008; 129: 152-4. [DOI] [PubMed] [Google Scholar]
- 13).Inoue K. Venous thromboembolism in earthquake victims. Disaster Manag Response 2006; 4: 25-7. [DOI] [PubMed] [Google Scholar]
- 14).Shibata M, Hanzawa K, Ueda S, et al. Deep venous thrombosis among disaster shelter inhabitants following the March 2011 earthquake and tsunami in Japan: a descriptive study. Phlebology 2014; 29: 257-66. [DOI] [PubMed] [Google Scholar]
- 15).Sakuma M, Nakamura M, Hanzawa K, et al. Acute pulmonary embolism after an earthquake in Japan. Semin Thromb Hemost 2006; 32: 856-60. [DOI] [PubMed] [Google Scholar]
- 16).Shibata M, Chiba H, Sasaki K, et al. The utility of on-site ultrasound screening in population at high risk for deep venous thrombosis in temporary housing after the great East Japan Earthquake. J Clin Ultrasound 2017; 45: 566-74. [DOI] [PubMed] [Google Scholar]
- 17).Sueta D, Akahoshi R, Okamura Y, et al. Venous thromboembolism due to oral contraceptive intake and spending nights in a vehicle—a case from the 2016 Kumamoto Earthquakes. Intern Med 2017; 56: 409-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Ueda S, Hanzawa K, Shibata M, et al. High prevalence of deep vein thrombosis in tsunami-flooded shelters established after the great East-Japan earthquake. Tohoku J Exp Med 2012; 227: 199-202. [DOI] [PubMed] [Google Scholar]
- 19).Rathore MF, Hanif S, New PW, et al. The prevalence of deep vein thrombosis in a cohort of patients with spinal cord injury following the Pakistan earthquake of October 2005. Spinal Cord 2008; 46: 523-6. [DOI] [PubMed] [Google Scholar]
- 20).Modena MG, Pettorelli D, Lauria G, et al. Gender differences in post-traumatic stress. Biores Open Access 2017; 6: 7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Ueda S, Hanzawa K, Shibata M. One-year overview of deep vein thrombosis prevalence in the Ishinomaki area since the great East Japan earthquake. Ann Vasc Dis 2014; 7: 365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Aoki T, Takahashi J, Fukumoto Y, et al. Effect of the Great East Japan Earthquake on cardiovascular diseases—report from the 10 hospitals in the disaster area. Circ J 2013; 77: 490-3. [DOI] [PubMed] [Google Scholar]
- 23).Tauqir SF, Mirza S, Gul S, et al. Complications in patients with spinal cord injuries sustained in an earthquake in Northern Pakistan. J Spinal Cord Med 2007; 30: 373-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Guner SI, Oncu MR. Evaluation of crush syndrome patients with extremity injuries in the 2011 Van Earthquake in Turkey. J Clin Nurs 2014; 23: 243-9. [DOI] [PubMed] [Google Scholar]
- 25).Matsukawa M, Miyamoto T, Yoshioka Y, et al. Efficacy of direct oral anticoagulant into the care of venous thromboembolism related to Kumamoto Earthquake. Ann Vasc Dis 2018; 11: 503-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26).Groves CC, Poudel MK, Baniya M, et al. Descriptive study of earthquake-related spinal cord injury in Nepal. Spinal Cord 2017; 55: 705-10. [DOI] [PubMed] [Google Scholar]
- 27).Terakami T, Ohba N, Morishita E, et al. Deep vein thrombosis in Noto Peninsula earthquake victims. Rinsho Byori 2009; 57: 411-6. (in Japanese) [PubMed] [Google Scholar]
- 28).Higgins JPT, Thomas J, Chandler J, et al. (eds.) Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
- 29).Wahl WL, Brandt MM. Potential risk factors for deep venous thrombosis in burn patients. J Burn Care Rehabil 2001; 22: 128-31. [DOI] [PubMed] [Google Scholar]
- 30).Ahuja RB, Bansal P, Pradhan GS, et al. An analysis of deep vein thrombosis in burn patients (part 1): comparison of D-dimer and Doppler ultrasound as screening tools. Burns 2016; 42: 1686-92. [DOI] [PubMed] [Google Scholar]
- 31).Ahuja RB, Bansal P, Pradhan GS, et al. An analysis of deep vein thrombosis in burn patients (part II): a randomized and controlled study of thrombo-prophylaxis with low molecular weight heparin. Burns 2016; 42: 1693-8. [DOI] [PubMed] [Google Scholar]
- 32).Harrington DT, Mozingo DW, Cancio L, et al. Thermally injured patients are at significant risk for thromboembolic complications. J Trauma 2001; 50: 495-9. [DOI] [PubMed] [Google Scholar]
- 33).Lim YP, Lin CL, Hung DZ, et al. Increased risk of deep vein thrombosis and pulmonary thromboembolism in patients with organophosphate intoxication: a nationwide prospective cohort study. Medicine (Baltimore) 2015; 94: e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34).Chung WS, Lin CL, Kao CH. Carbon monoxide poisoning and risk of deep vein thrombosis and pulmonary embolism: a nationwide retrospective cohort study. J Epidemiol Community Health 2015; 69: 557-62. [DOI] [PubMed] [Google Scholar]
- 35).Axley PD, Richardson CT, Singal AK. Epidemiology of alcohol consumption and societal burden of alcoholism and alcoholic liver disease. Clin Liver Dis 2019; 23: 39-50. [DOI] [PubMed] [Google Scholar]
- 36).Shen CJ, Kao CH, Hsu TY, et al. Effect of alcohol intoxication on the risk of venous thromboembolism: a nationwide retrospective cohort study. Medicine (Baltimore) 2017; 96: e8041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37).Kloner RA. Lessons learned about stress and the heart after major earthquakes. Am Heart J 2019; 215: 20-6. [DOI] [PubMed] [Google Scholar]
- 38).Moscona JC, Peters MN, Maini R, et al. The incidence, risk factors, and chronobiology of acute myocardial infarction ten years after Hurricane Katrina. Disaster Med Public Health Prep 2019; 13: 217-22. [DOI] [PubMed] [Google Scholar]
- 39).Kawano T, Tsugawa Y, Nishiyama K, et al. Shelter crowding and increased incidence of acute respiratory infection in evacuees following the Great Eastern Japan Earthquake and tsunami. Epidemiol Infect 2016; 144: 787-95. [DOI] [PubMed] [Google Scholar]
- 40).Kawano T, Hasegawa K, Watase H, et al. Infectious disease frequency among evacuees at shelters after the great eastern Japan earthquake and tsunami: a retrospective study. Disaster Med Public Health Prep 2014; 8: 58-64. [DOI] [PubMed] [Google Scholar]
- 41).Khan Y, Brown AD, Gagliardi AR, et al. Are we prepared? The development of performance indicators for public health emergency preparedness using a modified Delphi approach. PLoS One 2019; 14: e0226489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42).Khan IH, Savarimuthu S, Leung MST, et al. The need to manage the risk of thromboembolism in COVID-19 patients. J Vasc Surg 2020; 72: 799-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43).Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res 2020; 192: 23-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44).Shimura H. Human resource development for Tohoku region after Great East Japan Earthquake: remarks of the chairperson. Rinsho Byori 2016; 64: 78-9. (in Japanese) [PubMed] [Google Scholar]
- 45).Hata T. The comprehensive role of general physicians is very important in the chronic phase of a disaster area: beyond and after the Great East Japan Earthquake. J Gen Fam Med 2017; 18: 212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46).Wang J, Yang H, Xiang J, et al. The early diagnosis and treatment of fat embolism syndrome caused by the injuries in Wenchuan earthquake. Zhonghua Wai Ke Za Zhi 2008; 46: 1856-8. (in Chinese) [PubMed] [Google Scholar]
- 47).Li Y, Reinhardt JD, Gosney JE, et al. Evaluation of functional outcomes of physical rehabilitation and medical complications in spinal cord injury victims of the Sichuan earthquake. J Rehabil Med 2012; 44: 534-40. [DOI] [PubMed] [Google Scholar]
- 48).Otsuka K, Sakai A, Nakamura H, et al. Mental health activities following the Great East Japan Earthquake in the stricken coastal area of Iwate Prefecture. Seishin Shinkeigaku Zasshi 2013; 115: 485-91. (in Japanese) [PubMed] [Google Scholar]
- 49).Zhou K, Jia P. Depressive symptoms in patients with wounds: a cross-sectional study. Wound Repair Regen 2016; 24: 1059-65. [DOI] [PubMed] [Google Scholar]
- 50).Chang SL, Huang YL, Lee MC, et al. Association of varicose veins with incident venous thromboembolism and peripheral artery disease. JAMA 2018; 319: 807-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51).Canonico M, Plu-Bureau G, O’Sullivan MJ, et al. Age at menopause, reproductive history, and venous thromboembolism risk among postmenopausal women: the Women’s Health Initiative hormone therapy clinical trials. Menopause 2014; 21: 214-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52).Giarratano G, Savage J, Barcelona-deMendoza V, et al. Disaster research: a nursing opportunity. Nurs Inq 2014; 21: 259-68. [DOI] [PMC free article] [PubMed] [Google Scholar]


