Abstract
Objectives
The onset of the national stay-at-home orders accompanied by a surge in firearm sales has elevated the concerns of clinicians and public health authorities. The purpose of this study was to examine the impact of the stay-at-home orders among gunshot wound (GSW) trauma admissions.
Methods
This was a retrospective cohort study at six level I trauma centers across four states. Patients admitted after the onset of COVID-19 restrictions (March 16, 2020–June 30, 2020) were compared with those admitted during the same period in 2019. We compared (1) rate of patients with GSW and (2) characteristics of patients with GSW, by period using Χ2 tests or Fisher’s exact tests, as appropriate.
Results
There were 6996 trauma admissions across the study period; 3707 (53%) in 2019 and 3289 (47%) in 2020. From 2019 to 2020, there was a significant increase in GSW admissions (4% vs. 6%, p=0.001); 4 weeks specifically had significant increases (March 16–March 23: 4%, April 1–April 8: 5%, April 9–April 16: 6%, and May 11–May 18: 5%). Of the 334 GSWs, there were significant increases in patients with mental illness (5% vs. 11%, p=0.03), alcohol use disorder (2% vs. 10%, p=0.003), substance use disorder (11% vs. 25%, p=0.001), and a significant decrease in mortality (14% vs. 7%, p=0.03) in 2020. No other significant differences between time periods were identified.
Conclusion
Our data suggest that trauma centers admitted significantly more patients with GSW following the national guidelines, including an increase in those with mental illness and substance use-related disorders. This could be attributable to the stay-at-home orders.
Level of evidence
Level III, retrospective study.
Keywords: COVID-19, firearms, wounds, gunshot
Introduction
Following the March 16, 2020 White House announcement calling for a nationwide ‘social distancing’ order (NPR 2020), many states issued stay-at-home orders to slow the spread of COVID-19. Social distancing guidelines were recommended for 15 days and then subsequently extended until April 30, 2020 (CNN 2020). Though stay-at-home orders are a long-standing public health tool to curtail infection spread,1 they have led to unforeseen consequences across patient populations including increases in substance abuse,2 3 mental illness,4 and assaults.5 More specifically, there has been a surge in penetrating trauma by gun violence across many trauma centers,6 7 potentially due to a surge in firearm sales during the COVID-19 pandemic.
Studies show that emergencies and other potentially stressful national events are associated with more violent crime as well as surges in gun sales.7 8 Data on firearm sales from the Brookings Institute suggest that nearly 3 million more firearms were purchased during the COVID-19 pandemic than in the same period in 2019.9 Of particular concern was the finding that more than 8 million firearm purchases in 2020, deemed by some as ‘panic purchases’, were often by first-time owners for protection for the family.10 This increase in firearm sales could potentially have led to increases in accidental gun-related injuries during the pandemic as around 70% of all homicides and 83% of suicides are gun related; living in a home with a gun doubles your risk of a gun-related injury and triples your risk of suicide.11 Because of this surge in gun violence injuries, it is pertinent that trauma centers better understand these patient populations in the wake of the pandemic. This study further explores and describes characteristics of gun violence admissions across trauma centers before and during the national stay-at-home orders were implemented.
Methods
The study included trauma patients ≥18 years admitted across six level I trauma centers within our collaborative research network. Patients were compared between two admission time periods: period 1 (pre-COVID-19, March 16, 2019–June 30, 2019); and period 2 (COVID-19 with stay-at-home orders, March 16, 2020–June 30, 2020).
The proportion of patients admitted with a gunshot wound (GSW) was examined by admission period to determine changes in rates and patient characteristics during the pandemic. Covariates collected on each patient from the trauma registry included sex, age, race, Injury Severity Score (ISS, 1–15, ≥16), hospital length of stay (LOS), intensive care unit (ICU) stay (yes/no), injury location (unspecified, public, residential, car, other), type of injury (accidental, self-harm, domestic violence, police related, other intentional crime), and comorbid conditions (mental illness, alcoholism, substance abuse, history of smoking, hypertension). The presence of domestic violence (yes/no) was collected from the patient’s electronic medical record.
Categorical variables were analyzed with χ2 tests and Fisher’s exact tests and continuous data were analyzed using Wilcoxon Mann-Whitney U tests and Kruskal-Wallis tests, as necessary. GSW injuries were also compared against the national firearm sales from the Federal Bureau of Investigations National Instant Criminal Background Check System report, where a background check is performed with every attempt at a firearm purchase and then recorded in the system.12 Poisson regression was used to further examine the association between firearm sales and GSWs. A significance level of α=0.05 and SAS V.9.4 were used to conduct all statistical analyses.
Results
Of the 6994 trauma patients admitted across the study period, there were 53% in period 1 (pre-COVID-19) and 47% in period 2 (COVID-19 with social distancing). Five percent (n=334) of all admissions resulted from GSW. From period 1 to period 2, there was a statistically significant increase in GSW admissions (4% vs. 6%, p=0.001) but an overall 11% decrease in trauma admissions.
The top three reasons for GSW admissions were other intentional crime (86%), followed by accidental (14%), and then self-harm (8%). The patients were predominantly male (82%), black (52%), young (median (IQR) of 30 (23–40) years old), had an ISS ≤15 (71%), and spent 3 (1–7.5) days hospitalized on average. Table 1 reports any differences in GSW admissions from period 1 to period 2. From period 1 to period 2, GSW admissions were similar, except for comorbidities, where in period 2, there were significantly more patients admitted with a history of mental illness (5% vs. 11%, p=0.03), alcoholism (2% vs. 10%, p=0.003), and the single largest increase in substance abuse (11% vs. 25%, p=0.001).
Table 1.
Overall characteristics of gunshot wound admissions by COVID-19 time period
| Characteristics, n (%) | Period 1, 147 (4%) | Period 2, 184 (6%) | P value |
| Sex, (male) | 118 (80) | 156 (83) | 0.46 |
| Race (white) (missing 29) | 0.54 | ||
| White | 56 (42) | 62 (36) | |
| Black | 68 (51) | 92 (54) | |
| Other | 10 (7) | 17 (10) | |
| Age, median (IQR) years | 31 (23–44) | 29 (23–39) | 0.11 |
| Age range, years | 0.66 | ||
| 18–30 | 73 (50) | 102 (55) | |
| 31–50 | 54 (37) | 67 (36) | |
| 51–70 | 18 (12) | 16 (9) | |
| ≥71 | 2 (1) | 2 (1) | |
| Injury location | |||
| Unspecified place/unknown | 47 (32) | 58 (31) | 0.85 |
| Public | 34 (23) | 47 (25) | 0.67 |
| Residential | 47 (32) | 57 (30) | 0.77 |
| Car | 13 (9) | 7 (4) | 0.05 |
| Other | 6 (4) | 18 (10) | 0.05 |
| Characterization of injury | |||
| Unintentional/accidental | 19 (13) | 26 (14) | 0.75 |
| Self-harm | 10 (7) | 16 (9) | 0.52 |
| Domestic violence | 3 (4) | 4 (4) | >0.99 |
| Police | 3 (2) | 2 (1) | 0.66 |
| Other intentional crime | 115 (78) | 140 (76) | 0.64 |
| Injury Severity Score | 0.55 | ||
| 1–9 | 81 (55) | 114 (61) | |
| 10–15 | 21 (14) | 22 (12) | |
| ≥16 | 35 (31) | 51 (27) | |
| Comorbidities | |||
| Mental illness | 7 (5) | 21 (11) | 0.03 |
| Alcoholism | 3 (2) | 19 (10) | 0.003 |
| Substance abuse | 16 (11) | 46 (25) | 0.001 |
| Smoker | 71 (48) | 108 (59) | 0.06 |
| Hypertension | 11 (7) | 13 (7) | 0.88 |
| State | |||
| Colorado | 20 (14) | 28 (15) | 0.72 |
| Texas | 22 (15) | 41 (22) | 0.11 |
| Missouri | 74 (50) | 90 (48) | 0.69 |
| Kansas | 31 (21) | 28 (15) | 0.15 |
| Average monthly firearm sales by state | |||
| Colorado | 39 484 (5309) | 61 390 (12 766) | 0.02 |
| Texas | 114 173 (18 100) | 219 495 (41 508) | 0.003 |
| Missouri | 38 525 (8736) | 64 775 (8996) | 0.01 |
| Kansas | 12 862 (3044) | 22 918 (4873) | 0.01 |
| HLOS | 3 (1–7) | 4 (1–8) | 0.54 |
| ICULOS | 2 (1–5) | 2 (1–4) | 0.39 |
| In-hospital mortality | 21 (14) | 13 (7) | 0.03 |
Period 1: March 16, 2019–June 30, 2019; period 2: March 16, 2020–June 30, 2020.
Bolded p-values indiciate statistical signifiance at p≤0.05.
HLOS, hospital length of stay; ICU, intensive care unit; IQR, Interquartile range.
Although the median hospital LOS (3 vs. 4 days, p=0.54) and median ICULOS (2 days for both periods, p=0.39) were statistically similar, there was a significant decrease in the proportion of patients who died in-hospital during period 2 (14% vs. 7%, p=0.03). Although there were no significant differences in the proportion of GSWs from 2019 to 2020 by state, there was a trend towards significantly more GSWs in Texas (p=0.11). Whereas the proportion of GSWs in Colorado only slightly increased and the proportion of GSWs occurring in Kansas and Missouri decreased. There were significant increases in the average monthly firearm sales from period 1 to period 2 across all states. However, Texas observed the largest and most significant increase in firearm sales from period 1 to period 2.
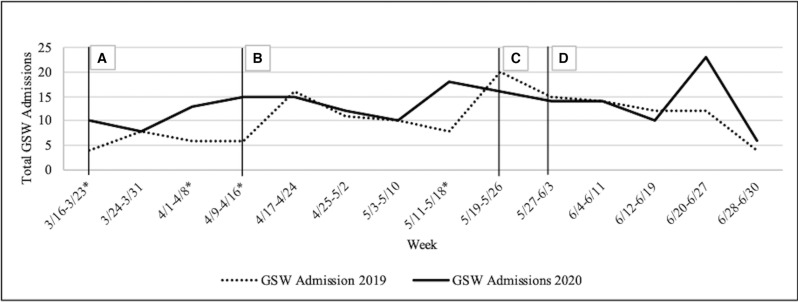
Figure 1 shows the total GSW admissions by week during period 1 and period 2. Compared with 2019, the rates of GSW admissions increased significantly from March 16, 2020 to March 23, 2020 (2% vs. 6%, p=0.01). The largest increases in GSW admissions occurred between April 1, 2020–April 8, 2020 (2% vs. 7%, p=0.02) and April 9, 2020–April 16, 2020 (2% vs. 8%, p=0.005). The last two increases occurred the weeks of May 11, 2020–May 18, 2020 (3% vs. 8%, p=0.008) and June 20, 2020–June 27, 2020 (4% vs. 7%, p=0.16). No other significant differences were observed by admission week.
Figure 1.
The total GSW admissions by week during period 1 and period 2 with specific national events marked by letters: (A) March 16, 2020: White House recommends national stay-at-home orders; (B) April 21, 2020: Centers for Disease Control and Prevention director warns of second wave of COVID-19; (C) May 28, 2020: the Minneapolis Police Station burns down following George Floyd’s death; (D) June 1, 2020: Lafayette Square, Washington DC BLM protests begin. Asterisks indicate significant differences in GSW admissions weeks from period 1 to period 2. BLM, Black Lives Matter; GSW, gunshot wound.
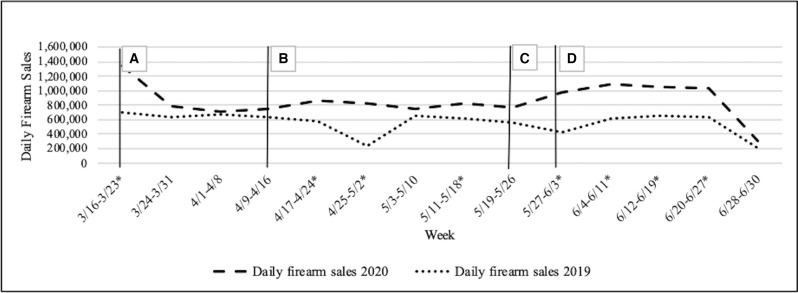
Figure 2 shows the total firearm sales by week during period 1 and period 2. Overall, there was a significant increase in the average firearm sales during the 14-week period from period 1 to period 2, (558 020 vs. 860 678, p=0.005). Significant increases in weekly firearm sales occurred in the following weeks: March 16–March 23 (p=0.0004), April 17–April 24 (p=0.0003), April 25–May 2 (p=0.03), May 11–May 18 (p=0.01), May 27–June 3 (p=0.001), June 4–June 11 (p=0.0001), June 12–June 19 (p=0.0003), and June 20–June 27 (p=0.0002) from period 1 to period 2.
Figure 2.
The total firearm sales by week during period 1 and period 2 with specific national events marked by letters: (A) March 16, 2020: White House recommends national stay-at-home orders; (B) April 21, 2020: Centers for Disease Control and Prevention director warns of second wave of COVID-19; (C) May 28, 2020: the Minneapolis Police Station burns down following George Floyd’s death; (D) June 1, 2020: Lafayette Square, Washington DC BLM protests begin. Asterisks indicate significant differences in daily firearm sales by weeks from period 1 to period 2. BLM, Black Lives Matter.
There were significant increases in both firearm sales and GSWs during the weeks of March 16–March 23, May 11–May 18, and June 20–June 27. The number of GSWs was significantly associated with number of firearm sales (p=0.02), without including the period. After adjustment, firearm sales were significantly associated with an increase in GSWs (p=0.04), however study period did not seem to alter the association (p=0.80), whereas admission week had a stronger impact on the association (p=0.02).
Discussion
After high stress events such as national emergencies, studies tend to show increases in firearm purchases, as well as an uptick in anxiety, depression, and acute stress disorder.7 13 Following the official recognition of the COVID-19 pandemic, firearm sales skyrocketed,9 14 and so did the number of people with mental illness and substance use disorders,2 creating a vulnerable and unique patient profile across hospitals in the USA. This study examined the effect of the stay-at-home orders on characteristics and rate of GSW admissions across level I trauma centers.
Among six level I trauma centers, the rate of GSW admissions significantly increased from period 1 to period 2, associated with particular weeks during the stay-at-home orders and other high stress national events of 2020. Following the national stay-at-home guidelines March 16, 2020–March 23, 2020, compared with 2019, the rates of GSW admissions and firearm sales increased. This is similar to other studies which also reported a significant increase in gun violence and firearm-related searches during the pandemic.14–16 Although we overall found that firearm sales and GSWs were significantly associated, COVID-19 did not impact that association whereas enrollment week did. The increases in GSWs may have been a result of the state of emergency declaration and resulting spike in firearm sales, or this increase may not have been related to the stay-at-home orders, and could have been a result of people buying guns for personal protection, the pandemic, or other reasons not examined. Additionally, the increase in GSW admissions may have been related to a larger number of people being out of work, resulting in an increase in poor mental health and substance abuse. Significant increases were also observed the weeks of April 1, 2020–April 8, 2020 and April 9, 2020–April 16, 2020, potentially following the Centers for Disease Control and Prevention’s official warning of a possible second wave of COVID-19. T The last two increases occurring May 11, 2020–May 18, 2020 and June 20, 2020–June 27, 2020 coincided with the wake of George Floyd’s death and Black Lives Matter protests.
Although other petty crimes and trauma admissions overall have decreased, hospitals across the USA have seen an increase in admissions due to violent crimes during the pandemic.15 16 Similar to this study, Donnelly et al observed a significant increase in the number of firearm incidents per day, firearm deaths per day and firearm injuries per day during stay-at-home orders when compared with previous years, as well as an increase after reopening when compared with the stay-at-home order period.7
Noteworthy differences observed in this gun violence population included not only a significant increase in mental illness, but also increases in admissions with alcoholism and substance abuse during the pandemic compared with 2019. Yuen et al state panic purchasing is influenced by individuals' perception of a threat (such as a health crisis), scarcity of products, fear of the unknown, uncertainty, coping behaviors, and social psychological factors.17 Donnelly et al also reported a significant increase in gun-related incidents involving drugs during stay-at-home orders when compared with 2019.7 Olding et al observed an increase in self-harm and discussed how social isolation can increase the risk of mental health disorders and self-harm; it is possible that the increase in GSWs in this study could also be partially attributable to self-harm injuries driven by the increase of mental illnesses.18 Although we saw an increase in the proportion of self-inflicted GSWs, from 7% to 9%, the difference was not significant.
Limitations
There are several study limitations; COVID-19 testing results were not tracked at all participating centers and testing criteria changed over time across all centers. Each state had different start and stop dates for the stay-at-home order, which may have contributed to variation in trauma patterns and volume by state; however, we think the White House’s national date captured these trends and provided consistency across the study. States had differing definitions for essential businesses during the stay-at-home orders, such as the option to continue to purchase federal firearm licenses, which may have resulted in different rates of firearm sales and GSW admissions. Factors other than COVID-19 that we did not examine could have played a role in the increased rate of GSWs observed. This was also a retrospective study, and the results may not be generalizable to other locations. We did examine the GSW and firearm rate by state and observed that firearm sales increased in all states, but the greatest increases in GSWs and firearm sales occurred in Texas. The change in proportion of GSWs was not significantly different among any of the states, but the direction of the change in proportion of GSWs was different by state. The largest increase in proportion of GSWs by period occurred in Texas (in line with firearm arms), Colorado experienced a slight increase, and the proportion of GSWs occurring in Kansas and Missouri decreased from 2019 to 2020.
Conclusions
Patients admitted with GSWs during the pandemic were more likely to be admitted with a history of substance abuse, alcoholism, or a mental health illness than patients with GSWs in the comparison period. Following any traumatic injury, patients may experience acute stress disorder, but this is especially true for those with mental illness. Because this patient population requires distinct inpatient needs that may not be available with COVID-19 protocols in place, important supplemental resources may include social work consultations or psychiatric consultations. Furthermore, clinicians and lawmakers need to be aware of trends in GSW injuries to tailor impactful programs that protect these vulnerable populations given the increase in GSW trauma admissions observed, whereas overall trauma admissions decreased after stay-at-home orders were implemented.
Footnotes
Contributors: CM conceived of the study, conducted literature searches, data collection, data analyses, and data interpretation, drafted the article, provided critical article revisions, and approved the final article. SJ conducted literature searches, data collection, data analyses, and data interpretation, assisted with drafting of the article, provided critical article revisions, and approved the final article. MC, ML, RMM, GMB, KLB, and DH participated in data interpretation, provided critical article revisions, and approved the final article. DB-O supervised the study, participated in data interpretation, provided critical article revisions, and approved the final article.
Funding: This study was internally funded and received no external grants or funds.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and approval to conduct this retrospective study was obtained from the Institutional Review Boards of the six participating hospitals: HCA-HealthONE IRB, Denver, Colorado (Swedish Medical Center and Wesley Medical Center, 1602124-2), Medical City Institutional Review Board, Plano, Texas (1602123-2), Catholic Health Initiatives Institute for Research and Innovation Institutional Review Board, Englewood, Colorado (Penrose Hospital and St Anthony Hospital, 1602122-3), and Western Institutional Review Board (Research Medical Center, 1-1344386-1). The research involves no more than minimal risk to the subjects and the research could not practically be performed without the waiver or alteration since the study only involves collecting and reporting data originally collected in the patient medical charts during a previous hospital stay and the patients are no longer accessible to obtain consent.
References
- 1.Strochlic N, Champine R. How some cities “flattened the curve” during the 1918 flu pandemic. National Geographic, 2020. [Google Scholar]
- 2.McGraw C, Salottolo K, Carrick M, Lieser M, Madayag R, Berg G, Banton K, Hamilton D, Bar-Or D. Patterns of alcohol and drug utilization in trauma patients during the COVID-19 pandemic at six trauma centers. Inj Epidemiol 2021;8:24. 10.1186/s40621-021-00322-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Correction: global changes and factors of increase in Caloric/Salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: survey study. JMIR Public Health Surveill 2021;7:e31906–9. 10.2196/31906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open 2020;3:e2019686. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salottolo K, Caiafa R, Mueller J, Tanner A, Carrick MM, Lieser M, Berg G, Bar-Or D. Multicenter study of US trauma centers examining the effect of the COVID-19 pandemic on injury causes, diagnoses and procedures. Trauma Surg Acute Care Open 2021;6:e000655. 10.1136/tsaco-2020-000655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeates EO, Grigorian A, Barrios C, Schellenberg M, Owattanapanich N, Barmparas G, Margulies D, Juillard C, Garber K, Cryer H, et al. Changes in traumatic mechanisms of injury in southern California related to COVID-19: penetrating trauma as a second pandemic. J Trauma Acute Care Surg 2021;90:714–21. 10.1097/TA.0000000000003068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donnelly MR, Grigorian A, Inaba K, Kuza CM, Kim D, Dolich M, Lekawa M, Nahmias J. A dual pandemic: the influence of coronavirus disease 2019 on trends and types of firearm violence in California, Ohio, and the United States. J Surg Res 2021;263:24–33. 10.1016/j.jss.2021.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kowohl W, Nordt C. COVID-19, unemployment and suicide. Br J Psychiatry 2020;216:189–96. 10.1192/bjp.2019.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levine P, McKnight R. Three million more guns: the spring 2020 spike in firearm sales. BROOKINGS. 2020.
- 10.Khubchandani J, Price JH. Public perspectives on firearm sales in the United States during the COVID‐19 pandemic. J Am Coll Emerg Physicians Open 2021;2. 10.1002/emp2.12293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu J, Murphy SL, Kochanek KD, Bastian B, Arias E. National Vital Statistics Reports Volume 67, Number 5 July 26, 2018, Deaths: Final Data for 2016. Vol 67. 2018. https://www.cdc.gov/. [PubMed]
- 12.FBI . FbI documents: NCIS firearm checks: Day/Month/Year.
- 13.Donnelly MR, Barie PS, Grigorian A, Kuza CM, Schubl S, de Virgilio C, Lekawa M, Nahmias J. New York state and the nation: trends in firearm Purchases and firearm violence during the COVID-19 pandemic. Am Surg 2021;87:690–7. 10.1177/0003134820954827 [DOI] [PubMed] [Google Scholar]
- 14.Caputi TL, Ayers JW, Dredze M, Suplina N, Burd-Sharps S. Collateral crises of gun preparation and the COVID-19 pandemic: Infodemiology study. JMIR Public Health Surveill 2020;6:e19369–12. 10.2196/19369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramos Perkis JP, Achurra Tirado P, Raykar N, Zinco Acosta A, Muñoz Alarcon C, Puyana JC, Ottolino Lavarte P. Different crises, different patterns of trauma. The impact of a social crisis and the COVID-19 health pandemic on a high violence area. World J Surg 2021;45:3–9. 10.1007/s00268-020-05860-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohler G, Bertozzi AL, Carter J, Short MB, Sledge D, Tita GE, Uchida CD, Brantingham PJ. Impact of social distancing during COVID-19 pandemic on crime in Los Angeles and Indianapolis. J Crim Justice 2020;68:101692. 10.1016/j.jcrimjus.2020.101692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yuen KF, Wang X, Ma F, Li KX. The psychological causes of panic buying following a health crisis. Int J Environ Res Public Health 2020;17:3513. 10.3390/ijerph17103513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olding J, Zisman S, Olding C, Fan K. Penetrating trauma during a global pandemic: changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. Surgeon 2021;19:e9–13. 10.1016/j.surge.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]