Key Points
Cancer-associated thrombosis (CAT) is increasing over time and is driven by an increase in PE±DVT.
CAT varies based on tumor type and stage and individual risk factors and is associated with increased risk of mortality.
Visual Abstract
Abstract
Cancer-associated thrombosis (CAT) is an important cause of morbidity and mortality for patients with malignancy and varies by primary cancer type, stage, and therapy. We aimed to characterize the incidence, risk factors, temporal trends, and the effect on mortality of CAT. The California Cancer Registry was linked to the statewide hospitalization database to identify individuals with the 13 most common malignancies diagnosed between 2005 and 2017 and determine the 6- and 12-month cumulative incidence of CAT by venous thromboembolism (VTE) location, tumor type, and stage after adjusting for competing risk of death. Cox proportional hazard regression models were used to determine risk factors associated with CAT and the effect of CAT on all-cause mortality. 942 019 patients with cancer were identified; 62 003 (6.6%) had an incident diagnosis of CAT. Patients with pancreatic, brain, ovarian, and lung cancer had the highest, and patients with breast and prostate cancer had the lowest 12-month cumulative incidence of CAT. For most malignancies, men, those with metastatic disease and more comorbidities, and African Americans (vs non-Hispanic Whites) were at highest risk for CAT. Patients diagnosed with cancer between 2014 and 2017 had a higher risk of CAT compared with those diagnosed between 2005 and 2007. CAT was associated with increased overall mortality for all malignancies (HR ranges 1.89 to 4.79). The incidence of CAT increased over time and was driven by an increase in pulmonary embolism±deep vein thrombosis (PE±DVT). CAT incidence varies based on tumor type and stage and on individual risk factors including gender, race/ethnicity, and comorbidities. For all tumor types, CAT is associated with an increased mortality.
Introduction
Cancer is a well-established risk for both arterial and venous thromboembolism (VTE). Prior studies have shown the high incidence of VTE in the cancer population varies widely by tumor type, cancer stage, cancer-directed therapy, and comorbidities.1-3 Thromboembolism is a leading cause of death for patients with malignancy.1,4-6
The reported incidence of cancer-associated venous thrombosis (CAT) varies widely between studies (1.6% to 6%) due to differences in ascertainment and the underlying populations represented.1,3,7 Multiple studies have suggested an increase in the incidence of CAT over time,3,5 with some investigators suggesting a 3-fold increase in the 12-month cumulative incidence of CAT over the past decade.3
The incidence of CAT varies greatly by primary tumor site, with most studies showing the highest risk of VTE in patients with pancreatic, lung, stomach, brain, and ovarian cancer.1,3,8 Other contributing factors for CAT include age, use of chemotherapy, and comorbidities.3,5 Cancer stage also significantly associates with increased risk for CAT, with patients with metastatic disease known to be at the highest risk of VTE.1,3,4,8
Our group previously determined the 12- and 24-month cumulative incidence of CAT, risk factors associated with CAT, and effect of CAT on survival using data from the California Cancer Registry linked to the California hospitalization data from 1993 to 1995.1 Since then, cancer-directed therapy has changed for many tumor subtypes and mortality rates have improved due to advances in both early detection and therapy. Simultaneously, more frequent use of high-resolution imaging for staging and assessment of treatment response has coincided with an increase in incidental VTE diagnoses, particularly pulmonary embolism (PE).2,3,9,10
Given these changes and the availability of diagnoses from California emergency department visits not resulting in inpatient admission starting in 2005, the aim of the current study is to determine the 6- and 12-month cumulative incidences of CAT (overall and by CAT location) in the 13 most common malignancies diagnosed in California between 2005 and 2017 stratified by tumor site, cancer stage, and year of cancer diagnosis. In addition, we investigated risk factors associated with the development of CAT and the impact of CAT on mortality.
Methods
This was a retrospective observational cohort study that linked the California Cancer Registry (CCR) and the California Patient Discharge Database (PDD), and the Emergency Department Utilization (EDU) Database. The CCR is a statewide population-based cancer surveillance system that has collected data on cancer incidence and mortality rates and captures >98% of all cancer diagnoses in the state. Date of cancer diagnosis, primary site, stage at diagnosis, initial course of treatment, and patient demographics (race/ethnicity, gender, age at diagnosis, neighborhood socioeconomic status,11 and insurance type12) can be ascertained from the CCR. The PDD captures all discharge diagnoses from nonfederal hospitals in California since 1991. The EDU database includes diagnosis information from all hospital-associated emergency department visits since 2005. These databases were linked using unique patient identifiers (ie, social security number, date of birth, sex, and zip code). All cancer patients who did not have a PDD or EDU admission (n = 155 075) or who received care through the Department of Veterans Affairs (which does not send data to the PDD or EDU) were excluded. Both PDD and EDU datasets include up to 25 diagnoses and up to 21 procedures associated with each admission, coded using the International Classification of Diseases, Ninth and Tenth Revision, Clinical Modification (ICD-9-CM, ICD-10-CM). All procedures in the EDU, including their associated dates, were coded using the Current Procedural Terminology (CPT).
We identified first primary cancer patients diagnosed between 2005 and 2017 with one of the 13 most common invasive cancers (breast, prostate, lung and bronchus, colorectal, non-Hodgkin lymphoma [NHL], urinary bladder, uterine, kidney, pancreas, stomach, ovarian, myeloma, and brain) using the SEER (Surveillance, Epidemiology, and End Results) Program site recode.13 Patients with a VTE in the PDD or EDU prior to their cancer diagnosis or patients whose cancer was diagnosed at autopsy or only noted on their death certificate were excluded from analysis (supplemental Figure 1).
From the CCR, stage at diagnosis was obtained using American Joint Commission on Cancer (AJCC) staging for all cancers except brain and myeloma (no staging information is available). Initial course of treatment was identified from CCR and included radiation (yes, no/unknown), chemotherapy (yes, no/unknown), and surgery (yes, no/unknown). Comorbidities were captured from the PDD or EDU up to 2 years prior to the malignancy diagnosis date. They were identified using the Elixhauser index, excluding cancer,14 and categorized as no admissions in PDD within the 2 prior years, 0 comorbidities, 1 to 2 comorbidities, and ≥3 comorbidities.
The primary outcomes included incidence of CAT (overall and by CAT location) and all-cause mortality. CAT location was identified from specific ICD-9-CM/ICD-10-CM codes (supplemental Table 1) for: pulmonary embolism with or without deep vein thrombosis (PE±DVT), proximal DVT (pDVT), isolated distal DVT (iDDVT), or unspecified leg DVT (LE-DVT, NOS). The CAT location was assigned in a hierarchical fashion: PE (± DVT), then pDVT (± iDDVT), then iDDVT. CAT diagnoses were obtained from the PDD and EDU dataset with follow-up data complete through 2018. The cumulative incidence and 95% confidence intervals of CAT, adjusted for the competing risk of death, was calculated from cancer diagnosis date to first CAT event date, death date, last known contact date, or study cutoff (12/31/2018), whichever occurred first. We determined the cumulative incidence of CAT by year of cancer diagnosis for each individual tumor site, dividing the time periods into quartiles (2005-2007, 2008-2010, 2011-2013, and 2014-2017). The in-hospital case fatality rate of PE was calculated for each of the 13 malignancies and by year of cancer diagnosis.
Multivariable Cox proportional hazards regression models, using the methods of Fine and Gray to adjust for competing risk of death, was used to analyze risk factors for incident CAT and evaluated association of CAT and mortality.15,16 Incident CAT was included as a time-dependent variable in the mortality analyses to adjust for immortal time bias.17-19 Mortality data captured by the CCR database is complete through 2017. Person time was calculated from cancer diagnosis date to death date, last known contact, or mortality cutoff (12/31/2017), whichever occurred first. Median potential follow-up time was calculated using reverse Kaplan Meier method.20 Proportional hazard assumptions for all Cox models were evaluated using the Schoenfeld Residuals Test.21 Covariates violating the proportional hazard assumption were included as stratification variables. Analyses were done for each cancer site separately. P values were considered significant if P < .05. This study was approved by the California Health and Human Services Agency Committee for the Protection of Human Subjects, and the University of California, Davis Institutional Review Boards. It was performed in accordance with the Declaration of Helsinki.
Results
We identified 942 109 first primary cancer patients with the 13 most common malignancies, and among those, 62 003 patients (6.6%) had a diagnosis of CAT (Table 1) with a median follow-up time of 89 months (95% CI 83.13 months to 89.52 months). Median age at time of cancer diagnosis was 65 years (quartile range: 56 years to 75 years); most patients identified as non-Hispanic White (63.1%), followed by Hispanic (18.6%), Asian/Pacific Islander (11.8%), and African American (7.3%). Twenty-four percent of the CAT patients had 3 or more comorbidities prior to their malignancy diagnosis compared with 17.3% in the overall cohort. In the overall cohort, 22.2% of patients had breast cancer, 19.2% prostate, and 14.3% lung cancer. The most common tumor types in patients who developed CAT were lung (20.1%) followed by colorectal (13.4%) and breast (12.3%) cancer. One-third of CAT patients had metastatic disease as compared with 20% in the entire cohort.
Table 1.
Baseline characteristics among California cancer patients with 13 common cancers by CAT, 2005-2017
| All | CAT | No CAT | P value | ||||
|---|---|---|---|---|---|---|---|
| Characteristics | n (%) | n (%) | n (%) | ||||
| All | 942 109 (100.0) | 62 003 (100.0) | 880 106 (100.0) | ||||
| Gender | |||||||
| Male | 443 089 (47.0) | 29 589 (47.7) | 413 500 (47.0) | 0.0003 | |||
| Female | 498 898 (53.0) | 32 402 (52.3) | 466 496 (53.0) | ||||
| Race/Ethnicity | |||||||
| Non-Hispanic White | 573 453 (60.9) | 39 135 (63.1) | 534 318 (60.7) | <.0001 | |||
| African American | 68 336 (7.3) | 6585 (10.6) | 61 751 (7.0) | ||||
| Hispanic | 175 521 (18.6) | 10 780 (17.4) | 164 741 (18.7) | ||||
| Asian/Pacific Islander | 110 895 (11.8) | 4931 (8.0) | 105 964 (12.0) | ||||
| Other/Unknown | 13 904 (1.5) | 572 (0.9) | 13 332 (1.5) | ||||
| Median age at cancer diagnosis (q1, q3) | 65 (56, 75) | 66 (57, 75) | 65 (56, 75) | <.0001 | |||
| Cancer site | |||||||
| Breast | 209 444 (22.2) | 7642 (12.3) | 201 802 (22.9) | <.0001 | |||
| Prostate | 180 807 (19.2) | 7271 (11.7) | 173 536 (19.7) | ||||
| Lung | 135 075 (14.3) | 12 442 (20.1) | 122 633 (13.9) | ||||
| Colorectal | 121 874 (12.9) | 8321 (13.4) | 113 553 (12.9) | ||||
| NHL | 56 771 (6.0) | 3951 (6.4) | 52 820 (6.0) | ||||
| Bladder | 24 964 (2.6) | 2295 (3.7) | 22 669 (2.6) | ||||
| Uterine | 47 295 (5.0) | 3560 (5.7) | 43 735 (5.0) | ||||
| Kidney | 44 345 (4.7) | 2781 (4.5) | 41 564 (4.7) | ||||
| Pancreatic | 36 679 (3.9) | 4604 (7.4) | 32 075 (3.6) | ||||
| Stomach | 24 689 (2.6) | 2162 (3.5) | 22 527 (2.6) | ||||
| Ovarian | 22 528 (2.4) | 2876 (4.6) | 19 652 (2.2) | ||||
| Brain | 19 039 (2.0) | 2249 (3.6) | 16 790 (1.9) | ||||
| Myeloma | 18 599 (2.0) | 1849 (3.0) | 16 750 (1.9) | ||||
| Year of cancer diagnosis | |||||||
| 2005-2007 | 230 451 (24.5) | 16 161 (26.1) | 214 290 (24.3) | <.0001 | |||
| 2008-2010 | 234 624 (24.9) | 16 232 (26.2) | 218 392 (24.8) | ||||
| 2011-2013 | 216 707 (23.0) | 14 301 (23.1) | 202 406 (23.0) | ||||
| 2014-2017 | 260 327 (27.6) | 15 309 (24.7) | 245 018 (27.8) | ||||
| Stage at diagnosis | |||||||
| Stage I | 255 374 (27.1) | 10 232 (16.5) | 245 142 (27.9) | <.0001 | |||
| Stage II | 256 524 (27.2) | 12 296 (19.8) | 244 228 (27.7) | ||||
| Stage III | 139 226 (14.8) | 11 052 (17.8) | 128 174 (14.6) | ||||
| Stage IV | 188 956 (20.1%) | 20 736 (33.4%) | 168 220 (19.1%) | ||||
| Stage Unknown | 102 023 (10.8%) | 7687 (12.4%) | 94 336 (10.7%) | ||||
| Initial course of cancer treatment | |||||||
| Chemotherapy | |||||||
| Yes | 312 233 (33.1) | 29 764 (48.0) | 282 469 (32.1) | <.0001 | |||
| No | 607 189 (64.4) | 30 662 (49.5) | 576 527 (65.5) | ||||
| Radiation | |||||||
| Yes | 260 948 (27.7) | 17 946 (28.9) | 243 002 (27.6) | <.0001 | |||
| No | 681 152 (72.3) | 44 057 (71.1) | 634 913 (72.1) | ||||
| Surgery | |||||||
| Yes | 588 227 (62.4) | 34 030 (54.9) | 554 197 (63.0) | <.0001 | |||
| No | 353 882 (37.6) | 27 973 (45.1) | 324 019 (36.8) | ||||
| Comorbidities (≤2 y prior) | |||||||
| NA/no admissions | 603 622 (64.1) | 32 611 (52.6) | 571 011 (64.9) | <.0001 | |||
| 0 comorbidities | 51 381 (5.5) | 3601 (5.8) | 47 780 (5.4) | ||||
| 1-2 comorbidities | 123 754 (13.1) | 10 722 (17.3) | 113 032 (12.8) | ||||
| ≥3 comorbidities | 163 352 (17.3) | 15 069 (24.3) | 148 283 (16.8) | ||||
Models are stratified by cancer site and adjusted for the competing risk of death using Fine and Gray methodologies.
Models are additionally adjusted for age at cancer diagnosis, stage at cancer diagnosis, initial course of treatment (chemotherapy, radiation, and surgery), neighborhood socioeconomic status, and health insurance at diagnosis or initial treatment. Variables that violated proportional hazard assumption were included as a stratification variable.
Most VTE events were PE±DVT (58.7%), followed by pDVT (22.1%), iDDVT (11%), and LE-DVT NOS (8.2%); therefore, 41.3% were lower extremity venous thrombosis without PE (Table 2). For almost all malignancies, patients with CAT were most likely to have PE±DVT as compared with proximal or distal DVT, except in bladder cancer, in which 43.4% of patients had PE±DVT compared with 56.6% with LE-DVT alone. In those with CAT and metastatic disease, 61.1% had PE±DVT, 21.2% pDVT, and 10.8% iDDVT. When examining trends in location of CAT over time, the proportion presenting as PE±DVT events increased from 55.7% between 2005 and 2007 to 60.5% for those diagnosed with cancer between 2014 and 2017.
Table 2.
Characteristics among CAT patients in California with 13 common cancers by CAT location, 2005-2017
| PE±DVT | pDVT | iDDVT | LE-NOS DVT | |
|---|---|---|---|---|
| Variables | n (%) | n (%) | n (%) | n (%) |
| All | 36 379 (58.7) | 13 717 (22.1) | 6841 (11.0) | 5066 (8.2) |
| Cancer site | ||||
| Breast | 4663 (61.0) | 1467 (19.2) | 776 (10.2) | 736 (9.6) |
| Prostate | 3877 (53.3) | 1769 (24.3) | 918 (12.6) | 707 (9.7) |
| Lung | 8838 (71.0) | 1714 (13.8) | 1156 (9.3) | 734 (5.9) |
| Colorectal | 4682 (56.3) | 2039 (24.5) | 880 (10.6) | 720 (8.7) |
| NHL | 2038 (51.6) | 1054 (26.7) | 509 (12.9) | 350 (8.9) |
| Bladder | 996 (43.4) | 793 (34.6) | 279 (12.2) | 227 (9.9) |
| Uterine | 1900 (53.4) | 968 (27.2) | 373 (10.5) | 319 (9.0) |
| Kidney | 1508 (54.2) | 792 (28.5) | 311 (11.2) | 170 (6.1) |
| Pancreatic | 2660 (57.8) | 1040 (22.6) | 553 (12.0) | 351 (7.6) |
| Stomach | 1315 (60.8) | 456 (21.1) | 237 (11.0) | 154 (7.1) |
| Ovarian | 1708 (59.4) | 633 (22.0) | 302 (10.5) | 233 (8.1) |
| Brain | 1269 (56.4) | 515 (22.9) | 280 (12.4) | 185 (8.2) |
| Myeloma | 925 (50.0) | 477 (25.8) | 267 (14.4) | 180 (9.7) |
| Year of cancer diagnosis | ||||
| 2005-2007 | 8999 (55.7) | 3606 (22.3) | 2001 (12.4) | 1555 (9.6) |
| 2008-2010 | 9434 (58.1) | 3671 (22.6) | 1876 (11.6) | 1251 (7.7) |
| 2011-2013 | 8677 (60.7) | 3155 (22.1) | 1580 (11.0) | 889 (6.2) |
| 2014-2017 | 9269 (60.5) | 3285 (21.5) | 1384 (9.0) | 1371 (9.0) |
| Stage at diagnosis | ||||
| Stage I | 5987 (58.5) | 2219 (21.7) | 1130 (11.0) | 896 (8.8) |
| Stage II | 6909 (56.2) | 2838 (23.1) | 1424 (11.6) | 1125 (9.1) |
| Stage III | 6646 (60.1) | 2373 (21.5) | 1119 (10.1) | 914 (8.3) |
| Stage IV | 12 671 (61.1) | 4401 (21.2) | 2232 (10.8) | 1432 (6.9) |
| Stage Unknown | 4166 (54.2) | 1886 (24.5) | 936 (12.2) | 699 (9.1) |
Models are stratified by cancer site and adjusted for the competing risk of death using Fine and Gray methodologies.
Models are additionally adjusted for age at cancer diagnosis, stage at cancer diagnosis, initial course of treatment (chemotherapy, radiation, and surgery), neighborhood socioeconomic status, and health insurance at diagnosis or initial treatment. Variables that violated proportional hazard assumption were included as a stratification variable.
LE-NOS DVT, lower extremity, not otherwise specified deep vein thrombosis.
Cumulative incidence of CAT
The 12-month cumulative incidence of CAT, without stratification for stage, ranged from 1% (prostate and breast cancer) to 10.7% (pancreatic cancer) (Table 3). Malignancies associated with the highest cumulative incidence included pancreatic, brain, ovarian, and lung cancer. The lowest 12-month cumulative incidence of CAT occurred in patients with prostate, breast, kidney, and uterine cancers. Most CAT events occurred within 6 months of cancer diagnosis (supplemental Table 2) and continued to increase through 12 months (Figure 1).
Table 3.
12-month cumulative incidence, adjusted for the competing risk of death, of overall CAT and CAT location among California cancer patients with 13 common cancers, 2005-2017
| Overall CAT | PE±DVT | pDVT | iDDVT | LE-NOS, DVT | ||
|---|---|---|---|---|---|---|
| Cancer site | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Breast | ||||||
| Overall | 1.04 (1.00, 1.09) | 0.65 (0.62, 0.69) | 0.17 (0.15, 0.19) | 0.10 (0.09, 0.12) | 0.12 (0.11, 0.14) | |
| Stage I | 0.53 (0.48, 0.58) | 0.33 (0.29, 0.37) | 0.08 (0.06, 0.10) | 0.06 (0.05, 0.08) | 0.06 (0.04, 0.07) | |
| Stage II | 0.92 (0.85, 0.99) | 0.56 (0.51, 0.62) | 0.15 (0.12, 0.18) | 0.09 (0.07, 0.11) | 0.12 (0.10, 0.15) | |
| Stage III | 1.53 (1.38, 1.68) | 1.01 (0.89, 1.14) | 0.19 (0.14, 0.25) | 0.11 (0.07, 0.15) | 0.22 (0.17, 0.29) | |
| Stage IV | 4.79 (4.40, 5.20) | 2.94 (2.64, 3.27) | 0.94 (0.78, 1.14) | 0.52 (0.40, 0.66) | 0.39 (0.29, 0.52) | |
| Prostate | ||||||
| Overall | 1.01 (0.97, 1.06) | 0.55 (0.52, 0.58) | 0.24 (0.22, 0.26) | 0.13 (0.11, 0.15) | 0.10 (0.08, 0.11) | |
| Stage I | 0.52 (0.43, 0.63) | 0.25 (0.19, 0.33) | 0.15 (0.10, 0.21) | 0.07 (0.04, 0.12) | 0.06 (0.03, 0.10) | |
| Stage II | 0.76 (0.71, 0.82) | 0.45 (0.42, 0.49) | 0.14 (0.12, 0.16) | 0.10 (0.08, 0.12) | 0.07 (0.05, 0.08) | |
| Stage III | 1.09 (0.94, 1.26) | 0.67 (0.56, 0.80) | 0.21 (0.15, 0.29) | 0.10 (0.06, 0.16) | 0.11 (0.07, 0.17) | |
| Stage IV | 3.31 (3.04, 3.60) | 1.45 (1.28, 1.65) | 1.09 (0.94, 1.26) | 0.43 (0.34, 0.54) | 0.34 (0.26, 0.44) | |
| Lung | ||||||
| Overall | 6.75 (6.62, 6.89) | 4.85 (4.74, 4.97) | 0.91 (0.86, 0.96) | 0.63 (0.59, 0.68) | 0.37 (0.33, 0.40) | |
| Stage I | 2.51 (2.31, 2.72) | 1.80 (1.64, 1.99) | 0.29 (0.22, 0.36) | 0.27 (0.21, 0.34) | 0.15 (0.11, 0.21) | |
| Stage II | 4.09 (3.66, 4.56) | 3.16 (2.78, 3.58) | 0.51 (0.37, 0.70) | 0.28 (0.18, 0.43) | 0.13 (0.07, 0.24) | |
| Stage III | 6.67 (6.37, 6.98) | 4.93 (4.67, 5.20) | 0.79 (0.68, 0.90) | 0.57 (0.48, 0.66) | 0.39 (0.32, 0.47) | |
| Stage IV | 8.98 (8.77, 9.20) | 6.39 (6.21, 6.58) | 1.27 (1.18, 1.35) | 0.86 (0.80, 0.94) | 0.46 (0.41, 0.51) | |
| Colorectal | ||||||
| Overall | 3.89 (3.79, 4.00) | 2.28 (2.19, 2.36) | 0.88 (0.83, 0.93) | 0.43 (0.40, 0.47) | 0.31 (0.28, 0.34) | |
| Stage I | 1.58 (1.43, 1.73) | 0.91 (0.81, 1.03) | 0.35 (0.29, 0.43) | 0.18 (0.13, 0.24) | 0.13 (0.09, 0.18) | |
| Stage II | 3.02 (2.83, 3.22) | 1.71 (1.56, 1.86) | 0.74 (0.65, 0.85) | 0.37 (0.30, 0.44) | 0.20 (0.16, 0.26) | |
| Stage III | 3.99 (3.78, 4.21) | 2.37 (2.21, 2.54) | 0.85 (0.75, 0.96) | 0.44 (0.37, 0.51) | 0.33 (0.28, 0.40) | |
| Stage IV | 7.55 (7.22, 7.88) | 4.55 (4.30, 4.81) | 1.64 (1.49, 1.80) | 0.77 (0.67, 0.89) | 0.59 (0.50, 0.69) | |
| NHL | ||||||
| Overall | 4.34 (4.17, 4.51) | 2.25 (2.13, 2.38) | 1.14 (1.06, 1.23) | 0.59 (0.53, 0.66) | 0.35 (0.31, 0.41) | |
| Stage I | 3.21 (2.92, 3.51) | 1.77 (1.57, 2.00) | 0.67 (0.55, 0.82) | 0.46 (0.36, 0.58) | 0.30 (0.22, 0.40) | |
| Stage II | 4.17 (3.76, 4.61) | 2.20 (1.90, 2.52) | 1.02 (0.82, 1.25) | 0.58 (0.44, 0.76) | 0.37 (0.26, 0.52) | |
| Stage III | 4.72 (4.30, 5.17) | 2.51 (2.21, 2.85) | 1.26 (1.05, 1.50) | 0.53 (0.40, 0.70) | 0.41 (0.30, 0.56) | |
| Stage IV | 5.42 (5.11, 5.74) | 2.70 (2.48, 2.93) | 1.56 (1.39, 1.74) | 0.76 (0.64, 0.88) | 0.40 (0.32, 0.50) | |
| Uterine | ||||||
| Overall | 3.73 (3.56, 3.90) | 2.15 (2.02, 2.28) | 0.94 (0.86, 1.03) | 0.37 (0.32, 0.42) | 0.27 (0.23, 0.33) | |
| Stage I | 1.47 (1.34, 1.61) | 0.92 (0.82, 1.03) | 0.31 (0.25, 0.38) | 0.15 (0.11, 0.20) | 0.09 (0.06, 0.13) | |
| Stage II | 3.80 (3.11, 4.57) | 2.09 (1.59, 2.69) | 0.95 (0.63, 1.38) | 0.53 (0.31, 0.87) | 0.23 (0.10, 0.48) | |
| Stage III | 6.61 (5.99, 7.26) | 3.72 (3.26, 4.23) | 1.90 (1.58, 2.28) | 0.51 (0.36, 0.73) | 0.47 (0.32, 0.67) | |
| Stage IV | 15.40 (14.3, 16.5) | 8.61 (7.77, 9.52) | 3.99 (3.41, 4.63) | 1.67 (1.31, 2.11) | 1.12 (0.83, 1.49) | |
| Bladder | ||||||
| Overall | 5.10 (4.83, 5.37) | 2.26 (2.08, 2.45) | 1.82 (1.65, 1.99) | 0.60 (0.51, 0.71) | 0.42 (0.35, 0.51) | |
| Stage I | 1.70 (1.47, 1.96) | 0.92 (0.75, 1.12) | 0.52 (0.40, 0.67) | 0.15 (0.09, 0.24) | 0.11 (0.06, 0.19) | |
| Stage II | 5.69 (5.11, 6.31) | 2.50 (2.12, 2.93) | 2.07 (1.73, 2.47) | 0.66 (0.48, 0.90) | 0.45 (0.30, 0.66) | |
| Stage III | 8.16 (7.06, 9.35) | 3.55 (2.84, 4.39) | 3.06 (2.40, 3.84) | 0.91 (0.58, 1.38) | 0.64 (0.37, 1.05) | |
| Stage IV | 12.30 (11.3, 13.3) | 5.16 (4.51, 5.87) | 4.42 (3.82, 5.08) | 1.62 (1.26, 2.04) | 1.13 (0.84, 1.49) | |
| Stomach | ||||||
| Overall | 6.68 (6.37, 7.00) | 4.17 (3.93, 4.43) | 1.31 (1.17, 1.46) | 0.76 (0.65, 0.87) | 0.45 (0.37, 0.54) | |
| Stage I | 3.36 (2.88, 3.90) | 2.07 (1.69, 2.50) | 0.69 (0.48, 0.96) | 0.42 (0.26, 0.63) | 0.19 (0.09, 0.35) | |
| Stage II | 5.23 (4.47, 6.08) | 3.33 (2.72, 4.02) | 1.02 (0.71, 1.44) | 0.68 (0.43, 1.03) | 0.20 (0.09, 0.43) | |
| Stage III | 6.65 (5.90, 7.46) | 4.09 (3.50, 4.74) | 1.33 (1.01, 1.73) | 0.72 (0.49, 1.03) | 0.51 (0.33, 0.78) | |
| Stage IV | 10.30 (9.64, 10.9) | 6.51 (6.01, 7.04) | 1.93 (1.66, 2.23) | 1.09 (0.89, 1.33) | 0.73 (0.57, 0.92) | |
| Pancreatic | ||||||
| Overall | 10.70 (10.4, 11.1) | 6.30 (6.05, 6.55) | 2.41 (2.26, 2.57) | 1.26 (1.15, 1.37) | 0.79 (0.70, 0.88) | |
| Stage I | 5.28 (4.53, 6.11) | 3.28 (2.69, 3.96) | 0.99 (0.68, 1.39) | 0.49 (0.29, 0.79) | 0.52 (0.31, 0.83) | |
| Stage II | 7.68 (7.12, 8.26) | 4.26 (3.84, 4.71) | 1.71 (1.45, 2.01) | 1.13 (0.92, 1.38) | 0.58 (0.43, 0.76) | |
| Stage III | 7.81 (6.88, 8.83) | 4.42 (3.72, 5.21) | 2.02 (1.56, 2.58) | 0.65 (0.41, 1.00) | 0.72 (0.46, 1.08) | |
| Stage IV | 15.00 (14.5, 15.5) | 8.95 (8.54, 9.38) | 3.27 (3.01, 3.53) | 1.74 (1.56, 1.94) | 1.02 (0.88, 1.17) | |
| Ovarian | ||||||
| Overall | 8.18 (7.83, 8.54) | 5.17 (4.88, 5.46) | 1.59 (1.43, 1.76) | 0.83 (0.72, 0.96) | 0.59 (0.50, 0.70) | |
| Stage I | 3.55 (3.06, 4.09) | 2.12 (1.74, 2.55) | 0.69 (0.48, 0.95) | 0.38 (0.24, 0.59) | 0.37 (0.23, 0.57) | |
| Stage II | 5.49 (4.49, 6.63) | 3.37 (2.60, 4.30) | 1.26 (0.81, 1.87) | 0.34 (0.15, 0.73) | 0.51 (0.26, 0.95) | |
| Stage III | 8.52 (7.91, 9.16) | 5.50 (5.01, 6.03) | 1.50 (1.25, 1.80) | 1.03 (0.83, 1.28) | 0.49 (0.35, 0.66) | |
| Stage IV | 12.50 (11.6, 13.3) | 7.90 (7.25, 8.59) | 2.43 (2.07, 2.83) | 1.22 (0.97, 1.52) | 0.90 (0.69, 1.16) | |
| Kidney | ||||||
| Overall | 3.57 (3.40, 3.75) | 1.99 (1.86, 2.12) | 1.04 (0.95, 1.14) | 0.35 (0.30, 0.41) | 0.19 (0.15, 0.23) | |
| Stage I | 1.58 (1.42, 1.74) | 1.05 (0.93, 1.19) | 0.29 (0.22, 0.36) | 0.18 (0.13, 0.24) | 0.06 (0.04, 0.10) | |
| Stage II | 1.78 (1.40, 2.22) | 0.84 (0.59, 1.15) | 0.50 (0.31, 0.75) | 0.32 (0.18, 0.54) | 0.12 (0.05, 0.28) | |
| Stage III | 5.22 (4.69, 5.79) | 2.44 (2.08, 2.85) | 2.01 (1.68, 2.38) | 0.41 (0.28, 0.60) | 0.35 (0.23, 0.53) | |
| Stage IV | 9.02 (8.40, 9.66) | 4.88 (4.42, 5.37) | 2.82 (2.47, 3.20) | 0.89 (0.70, 1.11) | 0.43 (0.31, 0.60) | |
| Myeloma | ||||||
| Overall | 5.34 (5.03, 5.67) | 2.76 (2.53, 3.01) | 1.32 (1.16, 1.49) | 0.84 (0.72, 0.98) | 0.42 (0.34, 0.52) | |
| Brain | ||||||
| Overall | 9.70 (9.28, 10.1) | 5.47 (5.15, 5.80) | 2.20 (1.99, 2.41) | 1.26 (1.11, 1.42) | 0.78 (0.66, 0.91) | |
Models are stratified by cancer site and adjusted for the competing risk of death using Fine and Gray methodologies.
Models are additionally adjusted for age at cancer diagnosis, stage at cancer diagnosis, initial course of treatment (chemotherapy, radiation, and surgery), neighborhood socioeconomic status, and health insurance at diagnosis or initial treatment. Variables that violated proportional hazard assumption were included as a stratification variable.
All P values are significant <.01 by cancer site and stage at diagnosis and CAT location except: NHL (P value = .6025) and pancreas (P value = .0594).
LE-NOS DVT, lower extremity, not otherwise specified deep vein thrombosis.
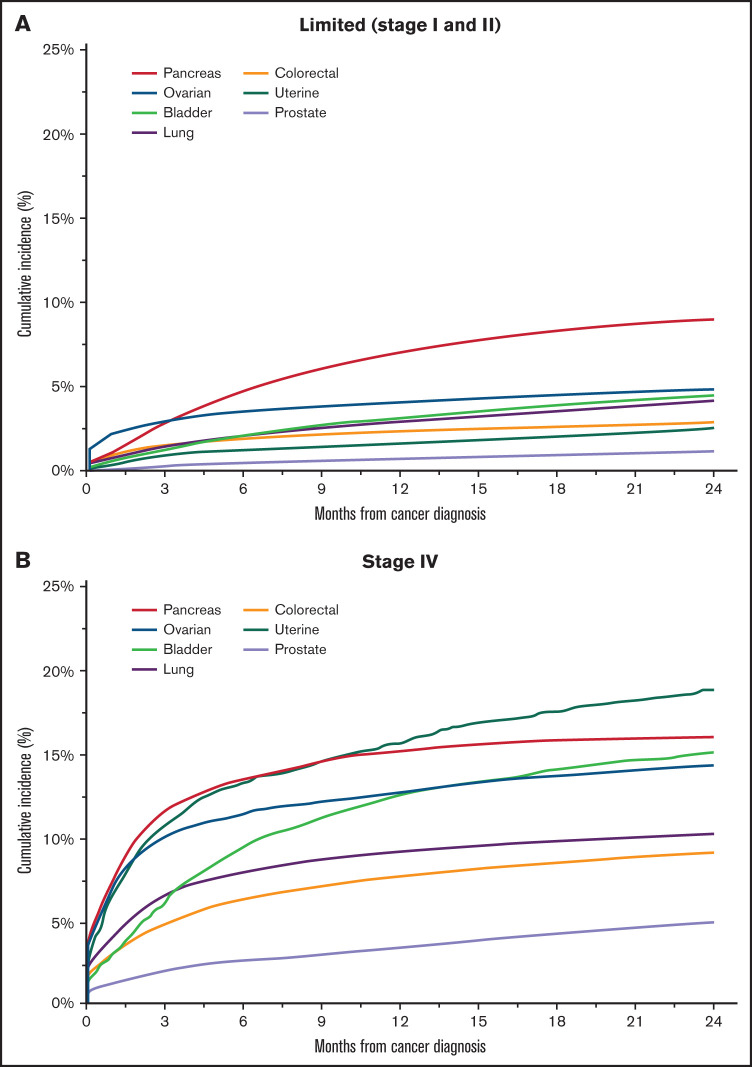
Figure 1.
Cumulative incidence of CAT among California cancer patients with select cancer site by stage, 2005-2017. (A) Limited (stage I and II). (B) Stage IV.
For all malignancies, the 12-month cumulative incidence of CAT increased with stage (Table 3; Figure 1). Among patients with limited-stage disease (stage I/II), pancreatic cancer, followed by ovarian, stomach, and NHL were associated with the highest incidence of CAT (range: 3.21% to 7.68%) (Figure 1A), while those with prostate and breast cancer (range: 0.52% to 0.92%) had the lowest.
For patients with stage III disease, those with ovarian, bladder, pancreas, and stomach cancer had the highest cumulative incidence of CAT (range: 6.65% to 8.52%). Among those with stage IV disease, uterine cancer had the highest 12-month cumulative incidence of CAT (15.4%), followed closely by pancreatic (15%), ovarian (12.5%), and bladder cancer (12.3%), while those with breast and prostate cancer had the lowest 12-month cumulative incidence of CAT at 4.79% and 3.31%, respectively (Figure 1B).
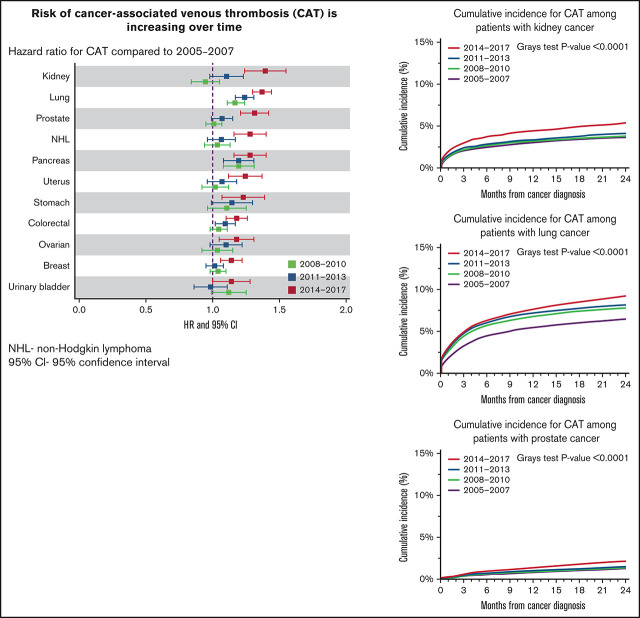
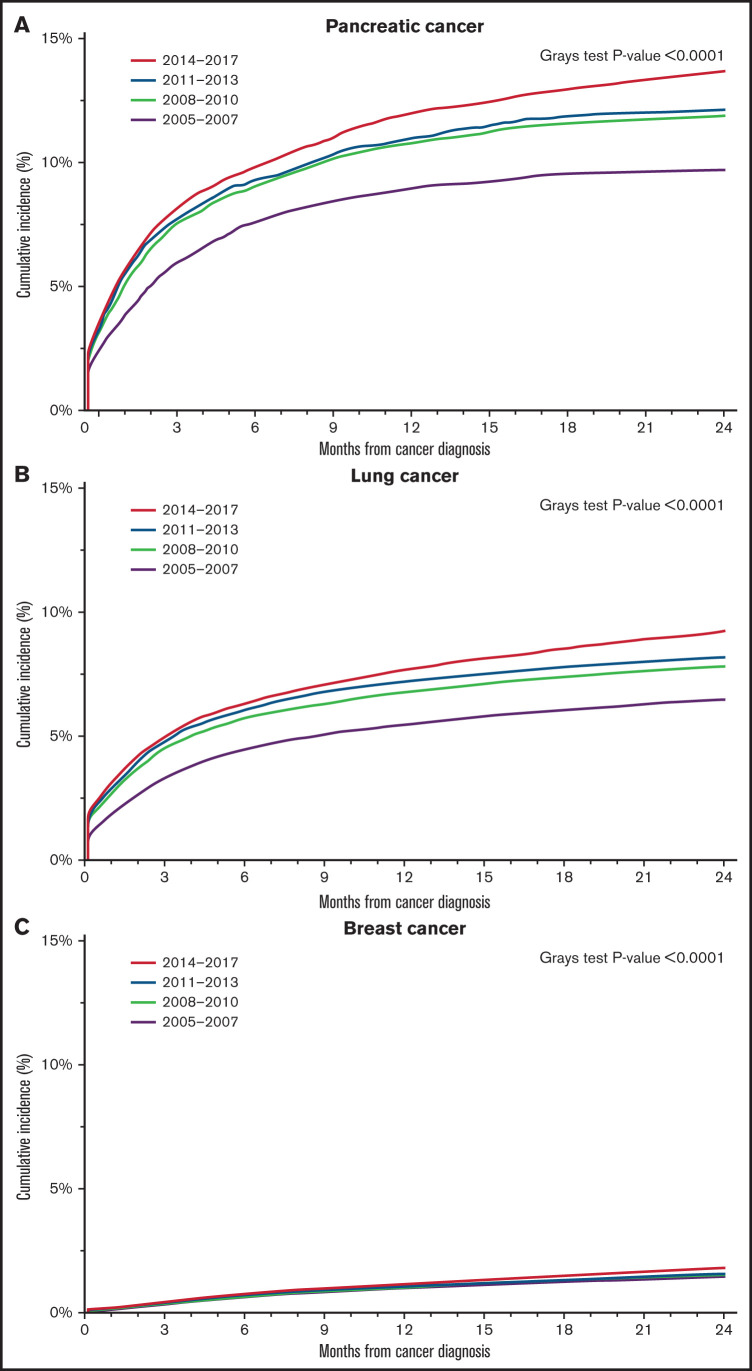
For most malignancies, the cumulative incidence of CAT was highest in the most recent time period (2014-2017) when compared with prior years (supplemental Figure 2). For example, the 12-month cumulative incidence of overall CAT in pancreatic cancer patients was 8.92% (95% CI 8.31% to 9.56%) in those diagnosed between 2005 and 2007 compared with 11.9% (95% CI 11.3% to 12.5%) in the 2014-2017 era (Figure 2A). A similar increase was also noted in patients with lung cancer, where the 12-month cumulative incidence of CAT in those diagnosed between 2005 and 2007 was 5.44% (95% CI 5.21% to 5.69%) vs 7.66% (95% CI 7.39% to 7.94%) between 2014 and 2017 (Figure 2B). For patients with breast cancer, the change in CAT incidence over time was less pronounced (12-month CI 0.99% [95% CI 0.9% to 1.08%] 2005-2007 vs 1.12% [95% CI 1.04% to 1.21%] 2014-2017) but was still statistically significantly different (Figure 2C).
Figure 2.
Cumulative incidence of CAT among California cancer patients with select cancer site, 2005-2017. (A) Pancreatic cancer. (B) Lung cancer. (C) Breast cancer.
Risk factors for CAT
Using multivariable models, we determined risk factors for CAT for each tumor site after adjusting for clinical and sociodemographic characteristics (Table 4). Women were at lower risk of CAT for most cancer types except for colorectal cancer, NHL, pancreatic cancer, stomach cancer, and myeloma, in which gender was not associated with risk factor for CAT. For almost all cancer sites (with the exception of myeloma), African Americans had a higher risk of CAT compared with non-Hispanic Whites, with the highest hazard ratio seen in uterine cancer (HR 1.69, 95% CI 1.52-1.89, P < .0001). Asian/Pacific Islanders were at decreased risk of CAT for all malignancies (HR 0.48-0.84) when compared with non-Hispanic Whites.
Table 4.
Risk factors associated with CAT development among California cancer patients with 13 common cancers, 2005-2017
| HR | Gender | Race/Ethnicity | Year of cancer diagnosis | Comorbidities (≤2 y prior) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | (vs male) | (vs non-Hispanic White) | (vs 2005-2007) | (vs 0 comorbidities) | ||||||
| P value | ||||||||||
| Cancer | Female | African American | Hispanic | Asian/PI | 2008-2010 | 2011-2013 | 2014-2017 | NA | 1-2 | ≥3 |
| Breast | 0.67 | 1.59 | 0.92 | 0.48 | 1.04 | 1.01 | 1.14 | 1.09 | 1.35 | 1.45 |
| (0.54, 0.83) | (1.48, 1.71) | (0.86, 0.98) | (0.44, 0.53) | (0.98, 1.10) | (0.95, 1.08) | (1.06, 1.22) | (0.96, 1.24) | (1.16, 1.57) | (1.25, 1.68) | |
| 0.0002 | <.0001 | 0.0084 | <.0001 | 0.2056 | 0.7252 | 0.0005 | 0.1935 | <.0001 | <.0001 | |
| Prostate | NA | 1.43 | 0.75 | 0.49 | 1.01 | 1.07 | 1.31 | 0.92 | 1.08 | 1.17 |
| (1.33, 1.54) | (0.70, 0.80) | (0.43, 0.55) | (0.95, 1.07) | (0.99, 1.15) | (1.21, 1.42) | (0.82, 1.04) | (0.94, 1.24) | (1.02, 1.35) | ||
| <.0001 | <.0001 | <.0001 | 0.834 | 0.0752 | <.0001 | 0.2021 | 0.2911 | 0.0303 | ||
| Lung | 1.06 | 1.27 | 1.05 | 0.78 | 1.17 | 1.24 | 1.37 | 0.95 | 1.01 | 0.87 |
| (1.02, 1.10) | (1.19, 1.35) | (0.99, 1.12) | (0.73, 0.82) | (1.11, 1.24) | (1.17, 1.31) | (1.30, 1.44) | (0.87, 1.03) | (0.93, 1.11) | (0.79, 0.94) | |
| 0.0018 | <.0001 | 0.0954 | <.0001 | <.0001 | <.0001 | <.0001 | 0.2041 | 0.785 | 0.0011 | |
| Colorectal | 1.03 | 1.47 | 0.86 | 0.50 | 1.04 | 1.09 | 1.18 | 1.02 | 1.13 | 1.2 |
| (0.98, 1.07) | (1.36, 1.58) | (0.81, 0.92) | (0.46, 0.55) | (0.98, 1.11) | (1.02, 1.17) | (1.10, 1.26) | (0.93, 1.13) | (1.02, 1.26) | (1.08, 1.34) | |
| 0.2617 | <.0001 | <.0001 | <.0001 | 0.1998 | 0.0078 | <.0001 | 0.6433 | 0.0244 | 0.0006 | |
| NHL | 0.96 | 1.59 | 0.9 | 0.67 | 1.03 | 1.06 | 1.27 | Stratification | ||
| (0.90, 1.03) | (1.41, 1.81) | (0.82, 0.98) | (0.59, 0.76) | (0.94, 1.13) | (0.96, 1.17) | (1.16, 1.40) | ||||
| 0.2763 | <.0001 | 0.0168 | <.0001 | 0.565 | 0.2495 | <.0001 | ||||
| Bladder | 0.89 | 1.69 | 0.96 | 0.6 | 1.11 | 0.98 | 1.13 | 1.1 | 1.08 | 1.06 |
| (0.80, 0.98) | (1.44, 1.98) | (0.84, 1.09) | (0.49, 0.73) | (0.99, 1.25) | (0.86, 1.11) | (1.00, 1.28) | (0.91, 1.33) | (0.88, 1.33) | (0.87, 1.31) | |
| 0.0199 | <.0001 | 0.5116 | <.0001 | 0.0801 | 0.7276 | 0.0471 | 0.3205 | 0.4638 | 0.5527 | |
| Uterine | 1.69 | 0.98 | 0.73 | 1.02 | 1.07 | 1.24 | 1.11 | 1.26 | 1.17 | |
| NA | (1.52, 1.89) | (0.89, 1.07) | (0.65, 0.82) | (0.92, 1.12) | (0.96, 1.18) | (1.12, 1.37) | (0.95, 1.30) | (1.06, 1.51) | (0.98, 1.40) | |
| <.0001 | 0.6484 | <.0001 | 0.7594 | 0.2166 | <.0001 | 0.1985 | 0.0095 | 0.0891 | ||
| Kidney | 0.91 | 1.53 | 0.91 | 0.69 | 0.94 | 1.09 | 1.38 | 1.28 | 1.35 | 1.48 |
| (0.84, 0.99) | (1.34, 1.76) | (0.83, 1.00) | (0.59, 0.81) | (0.84, 1.05) | (0.98, 1.23) | (1.24, 1.55) | (1.09, 1.50) | (1.14, 1.60) | (1.25, 1.75) | |
| 0.0223 | <.0001 | 0.0494 | <.0001 | 0.2912 | 0.1238 | <.0001 | 0.003 | 0.0005 | <.0001 | |
| Pancreatic | 1.03 | 1.36 | 0.93 | 0.67 | 1.19 | 1.19 | 1.27 | 1.11 | 1.19 | 1.03 |
| (0.96, 1.09) | (1.23, 1.51) | (0.85, 1.01) | (0.60, 0.75) | (1.08, 1.31) | (1.08, 1.31) | (1.16, 1.40) | (0.97, 1.28) | (1.03, 1.38) | (0.89, 1.18) | |
| 0.4141 | <.0001 | 0.0815 | <.0001 | 0.0005 | 0.0005 | <.0001 | 0.1255 | 0.018 | 0.7277 | |
| Stomach | 1.05 | 1.39 | 0.88 | 0.56 | 1.1 | 1.14 | 1.22 | 1.23 | 1.19 | 1.17 |
| (0.96, 1.15) | (1.19, 1.63) | (0.79, 0.98) | (0.49, 0.65) | (0.96, 1.25) | (0.99, 1.30) | (1.07, 1.39) | (0.99, 1.53) | (0.94, 1.50) | (0.93, 1.48) | |
| 0.2803 | <.0001 | 0.0189 | <.0001 | 0.1832 | 0.0635 | 0.0037 | 0.0658 | 0.1565 | 0.1741 | |
| Ovarian | 1.57 | 1.10 | 0.84 | 1.03 | 1.09 | 1.17 | 1.2 | 1.21 | 1.23 | |
| NA | (1.35, 1.83) | (1.00, 1.22) | (0.74, 0.96) | (0.92, 1.15) | (0.98, 1.22) | (1.05, 1.31) | (1.05, 1.37) | (1.06, 1.39) | (1.06, 1.43) | |
| <.0001 | 0.0543 | 0.0084 | 0.623 | 0.1216 | 0.0061 | 0.0058 | 0.006 | 0.0057 | ||
| Brain | 0.82 | 1.29 | 0.87 | 0.53 | 1.11 | 1.02 | 1.05 | 1.07 | 1.20 | 1.22 |
| (0.75, 0.90) | (1.06, 1.58) | (0.78, 0.98) | (0.44, 0.65) | (0.98, 1.25) | (0.89, 1.15) | (0.93, 1.19) | (0.93, 1.24) | (1.06, 1.37) | (1.05, 1.41) | |
| <.0001 | 0.0119 | 0.0242 | <.0001 | 0.1077 | 0.8143 | 0.4049 | 0.3131 | 0.0046 | 0.0085 | |
| Myeloma | 0.92 | 1.13 | 0.81 | 0.48 | 0.94 | 0.89 | 0.94 | Stratification | ||
| (0.84, 1.01) | (0.98, 1.30) | (0.72, 0.93) | (0.38, 0.59) | (0.82, 1.07) | (0.77, 1.02) | (0.82, 1.08) | ||||
| 0.085 | 0.0874 | 0.0019 | <.0001 | 0.3369 | 0.09 | 0.3793 | ||||
Models are stratified by cancer site and adjusted for the competing risk of death using Fine and Gray methodologies.
Models are additionally adjusted for age at cancer diagnosis, stage at cancer diagnosis, initial course of treatment (chemotherapy, radiation, and surgery), neighborhood socioeconomic status, and health insurance at diagnosis or initial treatment. Variables that violated proportional hazard assumption were included as a stratification variable.
PI, Pacific Islander.
Consistent with the increased cumulative incidence of CAT in more recent times, the risk of CAT was higher if the diagnosis was 2014-2017 vs 2005-2007 for all cancers in multivariable models, except brain cancers and myeloma. This was particularly noticeable in kidney cancer (HR 1.38, 95% CI 1.24-1.55 for 2014-2007 vs 2005-2007). In those with lung cancer, the risk of CAT was also significantly higher in all time periods of cancer diagnosis as compared with 2005-2007 (HR 2008-2010: 1.17; HR 2011-2013: 1.24; HR 2014-2017: 1.37; all P < .0001).
Concurrent comorbidities were significantly associated with CAT risk in patients with breast, prostate, colorectal, kidney, ovarian, and brain cancer, but were not significant in those with bladder and stomach cancers. In those with kidney and breast cancer, the risk of CAT was highest in those with 3 or more comorbidities (kidney HR 1.48, 95% CI 1.25-1.75, P < .0001; breast: HR 1.45, 95% CI 1.25-1.68, P < .0001).
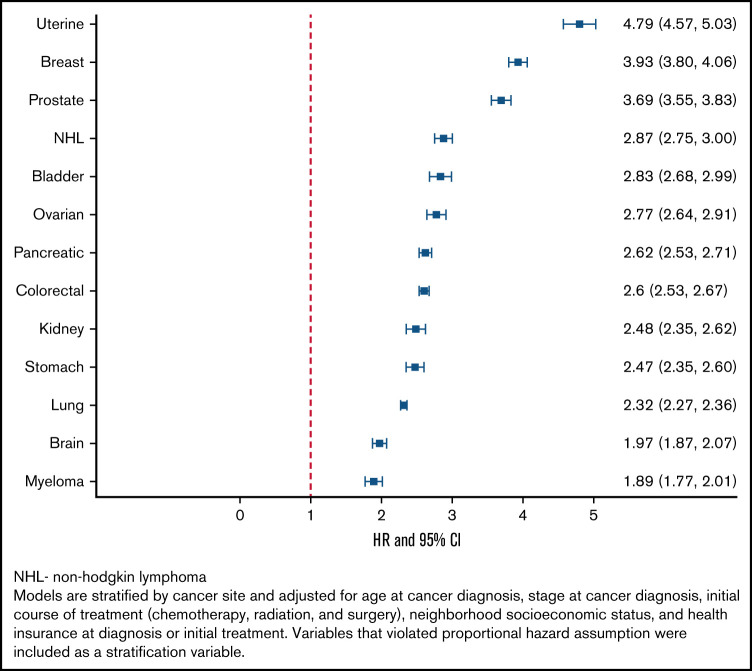
Impact of CAT on mortality
CAT in any location was associated with an increased all-cause mortality across all malignancies (Figure 3). For example, patients with CAT and uterine (HR 4.79, 95% CI 4.57-5.03), breast (HR 3.93, 95% CI 3.8-4.06), and prostate cancer (HR 3.69, 95% CI 3.55-3.83) all had a 3- to nearly 5-fold increased risk of mortality compared with those without CAT. By comparison, patients with CAT and myeloma (HR 1.89, 95% CI 1.77-2.01) and brain cancer (HR 1.97, 95% CI 1.87-2.07) had a nearly 2-fold increased risk of mortality.
Figure 3.
Effect of CAT on mortality among California cancer patients with 13 common cancers, 2005-2017.
The in-hospital case fatality rate of PE was obtained for each malignancy (supplemental Figure 3) and by era. The overall in-hospital case fatality rate of PE was 11.36% (95% CI 11% to 11.7%) for all malignancies. The case fatality rate varied widely by malignancy, with the lowest in prostate cancer (8.19%; 95% CI 7.3% to 9.1%) to the highest in stomach cancer (15.36%; 95% CI 13.4% to 17.3%). When examining case fatality rate of PE by era, 2005-2007 had the highest rate of 12.83% (95% CI 12.1% to 13.5%), followed by 2008-2010 at 11.21% (95% CI 10.6% to 11.8%), 2011-2013 was 10.71% (95% CI 10.1% to 11.4%), and the 2014-2017 case fatality rate of PE was 10.67% (95% CI 10% to 11.3%).
Discussion
In this large population-based study of cancer patients in California spanning 13 years, we describe the epidemiology of CAT from 2005 through 2017. Similar to prior studies, the results show most CAT events are PE±DVT.3 The incidence of CAT was highest in those with pancreatic, brain, ovarian, and lung cancer and lowest in those with breast and prostate cancer. The incidence of CAT increased with stage, with the highest incidence observed among those with metastatic disease. Men, African Americans, and those with multiple comorbidities were at increased risk for CAT, consistent with risk factors for VTE in the general population.22 For most malignancies, patients diagnosed with cancer more recently were at higher risk of CAT, findings that may relate to improved diagnostic technology or changes in therapy. CAT was associated with an increased risk of mortality across all malignancies; therefore, it is important to understand the contribution of tumor-specific risk factors (ie, primary tumor site and stage) as well as individual patient risk factors on the development of CAT.
PE±DVT was the most common location of CAT for most malignancies, followed by pDVT and then iDDVT. The rate of PE±DVT increased over time. This increase may relate to increased sensitivity of CT angiography in the last decade.23 In addition, it is possible the increase in PE±DVT over time may be related to changes in cancer-directed systemic therapy therapeutics. Prior studies have suggested a significantly higher risk of VTE in patients undergoing chemotherapy, protein kinase-inhibitors, antiangiogenic drugs, and immunotherapy, and this has increased over the last 2 decades.3,24
As previously published, pancreatic cancer was associated with the highest incidence of CAT, followed by brain and ovarian cancer.1,3,25 These malignancies may be associated with a higher risk for thrombosis due to upregulated expression of procoagulant proteins expressed by the tumor itself.26,27 Consistent with our findings, most CAT events have been found to occur within the first 6 months after diagnosis of malignancy,10,28,29 and continued to rise in the first 12 months after diagnosis. This is a time when tumor burden is the highest and in which patients are undergoing cancer-directed therapy that contribute a prothrombotic state.29,30
Stage at time of malignancy diagnosis has a significant impact on the incidence of thrombosis for all tumor types.1,3 For example, patients with uterine cancer and limited stage disease had a relatively low incidence compared with those with stage IV disease, a finding consistent with prior studies suggesting CAT may be a surrogate for aggressive tumor behavior in gynecologic malignancies.31 It is worth noting that cancer stage is not a component in many current predictive models for CAT,25,32 and incorporation of the extent of disease may improve predictive value in the future.
Several studies have shown an increase in the incidence of CAT over time.2,3,10 We confirm this temporal trend of increasing incidence of CAT for most malignancies except brain and myeloma. The increases were particularly striking in lung and pancreatic cancer and may be due to increased detection during routine disease assessment with more sensitive CT scans, immunotherapy in lung cancer and more intensive combination chemotherapies, and improved survival. For patients with myeloma, we may not have observed changes in CAT risk over time because CAT is highly associated with the use of high-dose steroids and lenalidomide that was introduced in 2006, near the beginning of our study period.33 Similarly, for patients with glioma, the risk of VTE appears most related to recent surgical resection and comorbidities.34
As previously shown, patients with CAT were at increased risk of mortality.1,4,5 The association with mortality varied significantly depending on primary tumor site, as those with uterine cancer and CAT had a nearly 5-fold increased risk of mortality compared with approximately 2-fold increased risk of mortality in those with brain cancer or myeloma. The association of CAT with mortality may be directly related to the VTE or as a clinical biomarker for more aggressive underlying malignancy and/or poor underlying health. As expected in this cohort of patients with advanced cancer, the case fatality rate of PE was much higher than the 3.9% case fatality rate reported in the general population.35 Cause of death can be difficult to ascertain in those with malignancy, but the high in-hospital mortality rate of PE across all cancer sites underscores the clinical importance of this complication. Primary and secondary prevention of CAT has not been shown to improve survival.36-39
There are several limitations to this study. While the California Cancer Registry does have robust data regarding stage and cancer-directed treatment, we do not have doses of medications or treatment dates. Patient characteristics which could impact VTE risk such as body mass index, hereditary thrombophilia, or smoking history are not available. In addition, we lack data regarding the use of prophylactic anticoagulation, though this was likely a limited clinical practice during the study period as it was prior to the publication of 2 trials using direct oral anticoagulants for primary prophylaxis in high-risk cancer patients.36,37 In terms of CAT diagnosis, we relied upon diagnostic coding performed in the emergency department and inpatient settings; therefore, the incidence of CAT may be underestimated if patients were diagnosed and treated only as an outpatient. Lastly, we were unable to ascertain if the VTE events included were symptomatic or incidental, which is often of particular interest for PE. However, prior literature has shown incidental PE to be clinically relevant with recurrence rates similar to symptomatic PE,40 and society guidelines recommend treatment regardless of symptoms associated with VTE.41,42
To our knowledge, this is one of the largest studies to examine CAT in a racially and ethnically diverse population of patients by location of VTE, tumor site, and stage. The incidence of CAT increased over time, and CAT was associated with an increased risk of mortality for all malignancies. Recent studies have shown the use of prophylactic anticoagulation in high-risk cancer patients undergoing chemotherapy decreases the risk of CAT,36,37 however, this is underused in practice.43 The data presented here serves as an important updated reference for CAT in the modern treatment era and will help guide discussions between providers and cancer patients regarding the risk of CAT and the risk/benefit ratio of primary prophylaxis.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885, Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 5NU58DP006344, the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201800032I awarded to the University of California, San Francisco, contract HHSN261201800015I awarded to the University of Southern California, and contract HHSN261201800009I awarded to the Public Health Institute.
This work was supported by a grant from the National Center for Advancing Translational Science (NCATS), National Institutes of Health, UL1 00001860.
Authorship
Contribution: A.M., A.B., and T.W. designed the study, acquired and analyzed the data, and drafted the manuscript; and all authors made revisions and approved the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Corresponding Author: Anjlee Mahajan, Division of Hematology Oncology, UC Davis Comprehensive Cancer Center, 4501 X Street, Sacramento, CA 95817, anmahajan@ucdavis.edu.
References
- 1.Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. Feb 27 2006;166(4):458-464. [DOI] [PubMed] [Google Scholar]
- 2.Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007;110(10):2339-2346. [DOI] [PubMed] [Google Scholar]
- 3.Mulder FI, Horvàth-Puhó E, van Es N, et al. Venous thromboembolism in cancer patients: a population-based cohort study. Blood. 2021;137(14):1959-1969. [DOI] [PubMed] [Google Scholar]
- 4.Sørensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000;343(25):1846-1850. [DOI] [PubMed] [Google Scholar]
- 5.Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5(3):632-634. [DOI] [PubMed] [Google Scholar]
- 6.Naess IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrøm J. Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost. 2007;5(4):692-699. [DOI] [PubMed] [Google Scholar]
- 7.Cohen AT, Katholing A, Rietbrock S, Bamber L, Martinez C. Epidemiology of first and recurrent venous thromboembolism in patients with active cancer. A population-based cohort study. Thromb Haemost. 2017;117(01):57-65. [DOI] [PubMed] [Google Scholar]
- 8.Horsted F, West J, Grainge MJ. Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLoS Med. 2012;9(7):e1001275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006;119(1):60-68. [DOI] [PubMed] [Google Scholar]
- 10.Walker AJ, Card TR, West J, Crooks C, Grainge MJ. Incidence of venous thromboembolism in patients with cancer - a cohort study using linked United Kingdom databases. Eur J Cancer. 2013;49(6):1404-1413. [DOI] [PubMed] [Google Scholar]
- 11.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12(8):703–711. [DOI] [PubMed] [Google Scholar]
- 12.Parikh-Patel A, Morris CR, Martinsen R, Kizer KW. Disparities in Stage at Diagnosis, Survival, and Quality of Cancer Care in California by Source of Health Insurance. Sacramento, CA: California Cancer Reporting and Epidemiologic Surveillance Program, Institute for Population Health Improvement, University of California Davis; 2015. [Google Scholar]
- 13.Surveillance E; and End Results Program . Site Recode ICD-O-3/WHO 2008 Definition. Accessed 23 March 2015. http://seer.cancer.gov/siterecode/icdo3_dwhoheme/index.html
- 14.Schoenman JA, Sutton JP, Elixhauser A, Love D. Understanding and enhancing the value of hospital discharge data. Med Care Res Rev. 2016; 64(4):449-468. [DOI] [PubMed] [Google Scholar]
- 15.Gray R. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Statist. 1988;16(3):1141-1154. [Google Scholar]
- 16.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496-509. [Google Scholar]
- 17.Lévesque LE, Hanley JA, Kezouh A, Suissa S. Problem of immortal time bias in cohort studies: example using statins for preventing progression of diabetes. BMJ. 2010;340(mar12 1):b5087. [DOI] [PubMed] [Google Scholar]
- 18.Liu J, Weinhandl ED, Gilbertson DT, Collins AJ, St Peter WL. Issues regarding ‘immortal time’ in the analysis of the treatment effects in observational studies. Kidney Int. 2012;81(4):341-350. [DOI] [PubMed] [Google Scholar]
- 19.Giobbie-Hurder A, Gelber RD, Regan MM. Challenges of guarantee-time bias. J Clin Oncol. 2013;31(23):2963-2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17(4):343-346. [DOI] [PubMed] [Google Scholar]
- 21.Allison PD. Survival Analysis Using SAS: A Practical Guide, 2nd ed. SAS Institute; 2010 [Google Scholar]
- 22.White RH, Zhou H, Murin S, Harvey D. Effect of ethnicity and gender on the incidence of venous thromboembolism in a diverse population in California in 1996. Thromb Haemost. 2017;93(02):298-305. [DOI] [PubMed] [Google Scholar]
- 23.Wang RC, Miglioretti DL, Marlow EC, et al. Trends in imaging for suspected pulmonary embolism across US Health Care Systems, 2004 to 2016. JAMA Netw Open. 2020;3(11):e2026930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moik F, Chan WE, Wiedemann S, et al. Incidence, risk factors, and outcomes of venous and arterial thromboembolism in immune checkpoint inhibitor therapy. Blood. 2021;137(12):1669-1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood. 2008;111(10):4902-4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khorana AA, Ahrendt SA, Ryan CK, et al. Tissue factor expression, angiogenesis, and thrombosis in pancreatic cancer. Clin Cancer Res. 2007; 13(10):2870-2875. [DOI] [PubMed] [Google Scholar]
- 27.Riedl J, Preusser M, Nazari PM, et al. Podoplanin expression in primary brain tumors induces platelet aggregation and increases risk of venous thromboembolism. Blood. 2017;129(13):1831-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alcalay A, Wun T, Khatri V, et al. Venous thromboembolism in patients with colorectal cancer: incidence and effect on survival. J Clin Oncol. 2006;24(7):1112-1118. [DOI] [PubMed] [Google Scholar]
- 29.Moore RA, Adel N, Riedel E, et al. High incidence of thromboembolic events in patients treated with cisplatin-based chemotherapy: a large retrospective analysis. J Clin Oncol. 2011;29(25):3466-3473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293(6):715-722. [DOI] [PubMed] [Google Scholar]
- 31.Matsuo K, Ross MS, Im DD, et al. Significance of venous thromboembolism in women with uterine carcinosarcoma. Gynecol Oncol. 2018;148(2):267-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ay C, Dunkler D, Marosi C, et al. Prediction of venous thromboembolism in cancer patients. Blood. 2010;116(24):5377-5382. [DOI] [PubMed] [Google Scholar]
- 33.Schoen MW, Carson KR, Luo S, et al. Venous thromboembolism in multiple myeloma is associated with increased mortality. Res Pract Thromb Haemost. 2020;4(7):1203-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Semrad TJ, O’Donnell R, Wun T, et al. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg. 2007; 106(4):601-608. [DOI] [PubMed] [Google Scholar]
- 35.Alotaibi GS, Wu C, Senthilselvan A, McMurtry MS. Secular trends in incidence and mortality of acute venous thromboembolism: The AB-VTE Population-Based Study. Am J Med. 08 2016;129(8):879.e19-25. [DOI] [PubMed] [Google Scholar]
- 36.Khorana AA, Soff GA, Kakkar AK, et al. Rivaroxaban for thromboprophylaxis in high-risk ambulatory patients with cancer. N Engl J Med. 02 2019;380(8):720-728. [DOI] [PubMed] [Google Scholar]
- 37.Carrier M, Abou-Nassar K, Mallick R, et al. Apixaban to prevent venous thromboembolism in patients with cancer. N Engl J Med. 02 2019; 380(8):711-719. [DOI] [PubMed] [Google Scholar]
- 38.Lee AY, Levine MN, Baker RI, et al. ; Randomized Comparison of Low-Molecular-Weight Heparin versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer (CLOT) Investigators . Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-153. [DOI] [PubMed] [Google Scholar]
- 39.Lee AYY, Kamphuisen PW, Meyer G, et al. ; CATCH Investigators . Tinzaparin vs warfarin for treatment of acute venous thromboembolism in patients with active cancer: A Randomized Clinical Trial. JAMA. 2015;314(7):677-686. [DOI] [PubMed] [Google Scholar]
- 40.Kraaijpoel N, Bleker SM, Meyer G, et al. ; UPE investigators . Treatment and long-term clinical outcomes of incidental pulmonary embolism in patients with cancer: An International Prospective Cohort Study. J Clin Oncol. 2019;37(20):1713-1720. [DOI] [PubMed] [Google Scholar]
- 41.Di Nisio M, Lee AY, Carrier M, Liebman HA, Khorana AA; Subcommittee on Haemostasis and Malignancy . Diagnosis and treatment of incidental venous thromboembolism in cancer patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2015;13(5):880-883. [DOI] [PubMed] [Google Scholar]
- 42.Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis , 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S-e496S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martin KA, Molsberry R, Khan SS, Linder JA, Cameron KA, Benson A III. Preventing venous thromboembolism in oncology practice: use of risk assessment and anticoagulation prophylaxis. Res Pract Thromb Haemost. 2020;4(7):1211-1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.