Abstract
Background:
A combined injury to the anterior cruciate ligament (ACL) and medial collateral ligament (MCL) is a common injury pattern encountered during clinical practice. Recent systematic reviews have found no consensus on the optimal method of managing this combined ligament injury pattern, and no long-term studies with modern techniques are available in the literature.
Purpose:
To compare 2 groups of patients who underwent isolated ACL reconstruction in terms of failures and clinical scores at long-term follow-up. In the first group were patients with isolated ACL tears (ACL group), while the second was composed of patients with combined ACL and MCL grade 2 tears (ACL + MCL group).
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A total of 57 patients (37 in the ACL group and 20 in the ACL + MCL group) underwent isolated ACL reconstruction with a double-bundle technique between January and December 2005. Patients were contacted for scores on the International Knee Documentation Committee subjective form, Western Ontario and McMaster Universities Osteoarthritis Index, and Tegner activity scale as well as data regarding ipsilateral or contralateral revision ACL surgery. A 2-way analysis of variance for repeated measures was used to statistically assess the differences between the groups.
Results:
Overall, 49 patients (86%) completed the survey and were therefore included in the study. The minimum follow-up was 14.6 years (range, 14.1-15.2 years). There was a significant reduction in both groups of all the outcome scores between the intermediate and final-follow-up. The number of failures was 3 of 31 (9.7%) in the ACL group and 1 of 18 (5.5%) in the ACL + MCL group; this difference was not significant. Moreover, there were no clinical differences between the groups in terms of graft failures, contralateral lesions, and clinical scores.
Conclusion:
At 14-year follow-up, no clinical difference or increased failure rate was observed between the study groups, suggesting that isolated ACL reconstruction could represent an appropriate treatment for a combined ACL and MCL grade 2 lesion.
Keywords: anterior cruciate ligament (ACL), medial collateral ligament (MCL), combined injury conservative treatment, long-term, failure, Telos, PROM
The medial collateral ligament (MCL) is one of the most commonly injured ligaments of the knee. 13,14 Most of those lesions are isolated MCL tears; however, with the increased severity of trauma, the anterior cruciate ligament (ACL) can be involved in a combined pattern of injury. 20
The treatment includes several options: ACL reconstruction alone, ACL reconstruction associated with MCL repair, or nonoperative treatment. 13,20 Recent systematic reviews 17,20 have found no consensus on optimal methods to manage this combined pattern of ligament injury. Moreover, most of the orthopaedic literature on the outcomes of combined ACL + MCL injury is based on isolated case series of surgical or nonoperative treatment at a short-term follow-up. 13 The only study that reached a long-term follow-up 10 presented mixed groups of patients treated with open surgical techniques, making these conclusions less applicable to current clinical practice.
The present study represents the third prospective evaluation of patients with isolated ACL lesion or combined ACL + MCL grade 2 tears who underwent isolated double-bundle ACL reconstruction. The aim of the research was to compare the 2 groups in terms of failures, clinical scores, and activity level at long-term follow-up to provide more insights regarding the management and long-term consequences of this injury pattern. The hypothesis of the present study was that the patients with combined ACL + MCL tears would present lower clinical scores and higher failure at long-term follow-up.
Methods
Patient Selection and Evaluation in the Previous Follow-up
The study protocol was approved by an institutional review board, and each patient gave informed consent. A total of 57 patients were recruited from a previous study 23 that assessed intraoperative valgus and anteroposterior laxity between patients with isolated ACL tears (ACL group) and those with combined ACL + MCL grade 2 injuries (ACL + MCL group). The MCL tear grade was determined through clinical examination using the International Knee Documentation Committee (IKDC) knee ligament standard evaluation. All patients had undergone isolated, over-the-top double-bundle, ACL reconstruction 15 (Figure 1) with hamstring tendons between January and December 2005.
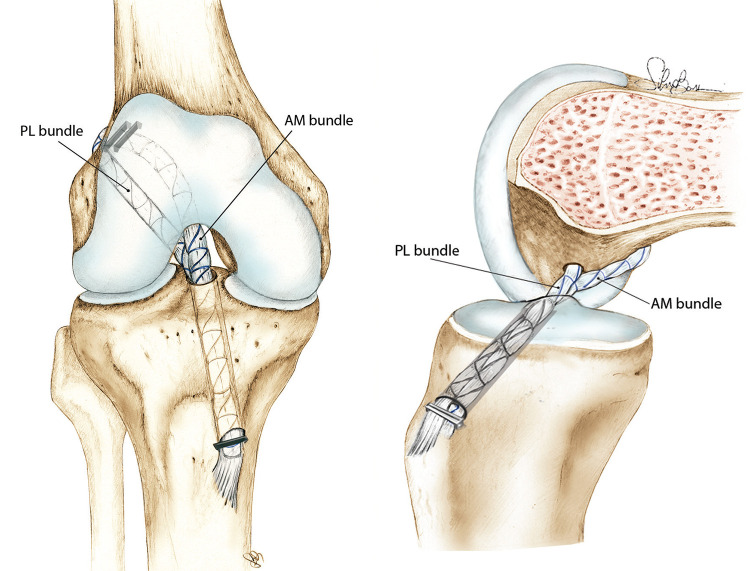
Figure 1.
Anterior and lateral views of the anterior cruciate ligament reconstruction surgical technique performed in the 2 groups of the present study. AM, anteromedial; PL, posterolateral.
The ACL + MCL group followed an MCL nonoperative treatment protocol before ACL surgery: bracing with the knee in extension and full weightbearing for 3 weeks. After the first week, the knee brace could be removed 2 times a day to perform knee flexion-extension; then, after 3 weeks, bracing was definitively removed, and the patients began muscular strengthening with isometric quadriceps exercises, cycling, and swimming. The postsurgical rehabilitation program was the same for both groups. Exclusion criteria were bilateral insufficiency of the ACL, previous ligament reconstruction of either knee, and a meniscal tear of the affected knee. In the first study of this patient cohort, 23 postsurgical laxity was intraoperatively quantified with a navigation system 16 (Polaris; NDI). Patients from the ACL + MCL group showed greater valgus laxity at 30° as compared with patients in the ACL group (5.47° ± 1.82° vs 4.41° ± 1.42°; P = .016).
A second evaluation was performed at a minimum 3-year follow-up. 24 We obtained scores on patient-reported outcome measures (PROMs)—Lysholm, Tegner, IKDC subjective form, and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)—and conducted valgus laxity evaluation with Telos stress radiographs (METAX Kupplungs und Dichtungs technik). In this setting, a significant difference occurred between the groups in the mean medial joint space opening during valgus stress (50 N), with a side-to-side difference of 0.9 mm in the ACL group and 1.7 mm in the ACL + MCL group (P = .013).
In the present study, patients from the original cohort were prospectively recruited at a minimum 14-year follow-up. The patients were contacted via telephone between April 2020 and June 2020 and completed the same PROMs as those used at 3-year follow-up (Lysholm, Tegner, IKDC, WOMAC); moreover, patients were asked about graft failure or contralateral ACL tear. The patients were carefully interviewed, and if a history of trauma or instability were reported, they were invited for a clinical and imaging evaluation.
Statistical Analysis
The normal distribution of the data was verified through the Shapiro-Wilk test. Normally distributed continuous variables are presented as means and standard deviations, while categorical variables are presented as a percentage over the total. A 2-way analysis of variance for a repeated measures test was performed to assess the between-group differences of continuous variables, while the Student t test was used to compare each group with the other. The chi-square test was performed to assess the differences in categorical variables. Differences between the groups were considered statistically significant if P < .05. For the multiple comparisons, P values were adjusted using the Bonferroni post hoc correction. An a priori power analysis was performed to calculate an adequate sample size based on the results of a previous study. 24 Considering a reduction of 3 points in clinical outcomes with a standard deviation of 3.5 points, at least 17 patients were required to have a power of 90% and a type 1 error of 0.05. All statistical analyses were performed in SPSS (Version 26; IBM).
Results
A total of 49 patients (86%) were included in the current evaluation; the mean follow-up was 14.6 years (range, 14.1-15.2 years). Of these patients, we excluded 4 from the final evaluation because they had experienced ACL graft failure (1 in the ACL + MCL group, 3 in the ACL group; P = .62). This left 45 patients available for subjective clinical score evaluation: 17 in the ACL + MCL group and 28 in the ACL group. No differences were found between the groups in age, sex distribution, time injury to surgery, or contralateral ACL injury (Table 1).
Table 1.
Patient Characteristics a
| ACL + MCL Grade 2 Tear (n = 17) | Isolated ACL Tear (n = 28) | P | |
|---|---|---|---|
| Sex, male:female | 16:1 | 27:1 | .72 |
| Age at final follow-up, y | 48.1 ± 10.2 | 43.7 ± 9.9 | .14 |
| Time from injury to surgery, mo | 9 ± 4.7 | 12 ± 12.8 | .82 |
| Contralateral ACL injury | 3 | 5 | .98 |
a Data are reported as No. of patients or mean ± SD. ACL, anterior cruciate ligament; MCL, medial collateral ligament.
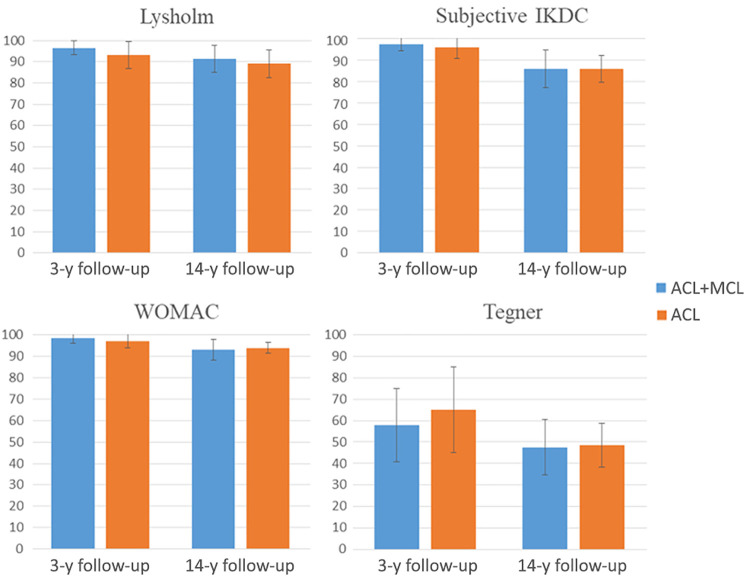
PROM Evaluations
A statistically significant effect for time (P < .001) was found for all the PROMs (Table 2). In particular, the ACL + MCL group showed a significant reduction from 3- to 14-year follow-up on the Lysholm (5.1 points; P < .012), IKDC (11.3 points; P < .001), and WOMAC (5.4 points; P < .001), while the ACL group showed a significant reduction on the IKDC (10 points; P < .001), WOMAC (3.2 points; P < .001), and Tegner (1.6 points; P < .001).
Table 2.
Patient-Reported Outcome Scores by Follow-up a
| ACL + MCL Grade 2 Tear | Isolated ACL Tear | |||
|---|---|---|---|---|
| 3 y | 14 y | 3 y | 14 y | |
| Lysholm | 96.5 ± 3.3 | 91.4 ± 6.2 b | 93.1 ± 6.3 | 89.0 ± 6.6 |
| IKDC | 97.3 ± 3.0 | 86.0 ± 8.8 b | 96.1 ± 5.3 | 86.1 ± 6.2 b |
| WOMAC | 98.5 ± 2.3 | 93.1 ± 5.0 b | 97.2 ± 3.3 | 94.0 ± 2.6 b |
| Tegner | 5.8 ± 1.7 | 4.8 ± 1.3 | 6.5 ± 2.0 | 4.9 ± 1.0 b |
a Values are presented as mean ± SD. ACL, anterior cruciate ligament; IKDC, International Knee Documentation Committee; MCL, medial collateral ligament; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
b Statistically significant within-group difference between 3- and 14-year follow-up (P < .05). No statistical differences were found between the groups at 14-year follow-up.
No statistically significant group or time × group effects were observed (P > .05). In particular, no differences between the groups were registered at 14-year follow-up (Table 2, Figure 2). Three patients required subsequent surgery: 1 for the ACL + MCL group (hardware removal) and 2 for the ACL group (1 hardware removal and 1 microfracture). All patients except 1 of ACL group were satisfied with the surgical procedure they underwent.
Figure 2.
Patient-reported outcome measures collected at 3- and 14-year follow-ups. A statistically significant effect for time was found for all measures; however, no differences were registered between the groups at the final follow-up. Values are presented as mean ± SD. ACL, anterior cruciate ligament; IKDC, International Knee Documentation Committee; MCL, medial collateral ligament; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Discussion
The most important finding of the present study is that the clinical results of a combined ACL + MCL grade 2 lesion managed with ACL reconstruction alone are comparable to the outcomes of an isolated ACL reconstruction, even at long-term follow-up.
Historically, the surgical management of this combined lesion has been advocated as the standard of care by many authors. 20 Among them, Fetto and Marshall 7 reported that 79% of combined ACL + MCL lesions treated nonoperatively led to unsatisfactory outcomes regardless of MCL tear grade, suggesting a more aggressive approach. Similarly, in 1994, Hughston 10 published results at long-term follow-up for 51 patients with grade 3 MCL tears treated with an acute repair of the MCL and the semimembranosus complex. The author described good results in physical activity, pain, stability, and osteoarthritic changes, with only 3 failures (7%). Among the cohort, 24 patients had a torn ACL, and the ligament was debrided or repaired with absorbable sutures using an open approach. Conversely, Shelbourne and Porter, 19 not mentioning MCL tear grade, reported excellent results in stability and return to sport in patients with a combined ligamentous injury who underwent isolated open ACL reconstruction with patellar tendon and no medial-side surgical treatment. However, these studies used old surgical techniques and different rehabilitation protocols, making the results less applicable to the current clinical practice.
More recently, Funchal et al 8 reported the 2-year outcomes of a cohort of 112 patients with combined ACL tears and MCL grade 2 lesions with a floating meniscus. The patients underwent either isolated ACL or combined ACL + MCL reconstruction. At the final follow-up, the latter group presented a lower failure rate, with only 2 cases (3%) as opposed to 16 (29%) in the nonoperative-MCL group, thus underlying that in the presence of a floating meniscus, an isolated ACL reconstruction may result in inferior outcomes. Similarly, a study from the Swedish National Knee Ligament Registry 21 found that patients undergoing ACL reconstruction for isolated ACL injury had lower revision rates (hazard ratio, 0.61) than patients with combined ACL + MCL injuries undergoing ACL reconstruction and nonoperative treatment of the MCL injury. Patients undergoing concomitant MCL repair/reconstruction had similar revision rates to those with isolated ACL reconstruction.
Conversely, in our study, the presence of combined ACL + MCL lesions treated nonoperatively did not result in an increased risk of failure with respect to an isolated ACL lesion. Thus, our results are in line with the study of Halinen et al, 9 who found no failure differences between those groups, even in the presence of associated grade 3 MCL tears. A possible explanation for the different failure results between our study and that by Funchal et al 8 is that they differ significantly in characteristics, surgical techniques adopted, and time from injury to surgery.
Unlike in our study, Funchal et al 8 reported a Tegner activity level of 9 at 24-month follow-up after ACL and MCL reconstruction, thus suggesting that the research was performed on elite athletes. Moreover, those authors performed surgery in an acute setting (3-6 weeks after injury), while in the present study, the mean time from injury to surgery was 9 months. According to biomechanical studies on animal models, at 6 weeks, the modulus and stiffness of the healing MCL are lower than the native state, 18 and the medial laxity could affect the healing process of the ACL graft. MCL tears also place more tension on the ACL, 1 and the load not controlled by the deficient MCL will be restrained by the ACL graft. 25 The high revision rate cited by Funchal et al could therefore be explained by the decision to perform surgery in the acute setting when a functionally unstable MCL could have placed excessive tension on the ACL graft.
Another important finding of our research was that no differences in clinical scores and sport-activity level occurred between the groups. Conversely, Funchal et al 8 noted lower clinical scores in patients who underwent nonoperative MCL treatment with respect to those who underwent combined ACL + MCL reconstruction (Lysholm scores, 78.1 vs 89.7; Tegner scores, 6.7 vs 9.0).
The evidence from the Swedish National Knee Ligament Registry 21 also showed reduced clinical scores when comparing patients with isolated ACL injury and patients with combined ACL + MCL injury treated nonoperatively (Knee injury and Osteoarthritis Outcome Score [KOOS], 70.7 vs 67.0, respectively). However, unlike the results by Funchal et al, 8 worse results were seen in patients with combined ACL + MCL treatment, with the KOOS dropping to 62.8 and with an extremely low score on the KOOS sport subscale.
Even if the Telos stress radiographs are considered the gold standard to quantify valgus instability, 11 there is a lack of studies investigating the effect of combined ligamentous injuries in vivo. Moreover, no studies have ever correlated valgus instability values with the Telos at short-term follow-up with the long-term outcomes. In summary, at the moment, the Telos radiographs performed pre- and postoperatively could provide to the surgeon only objective measurements of the raw reduction laxity without giving any additional prognostic information.
At the intermediate follow-up of 3 years, the Telos valgus stress radiographs revealed a mean medial joint space opening (side-to-side difference) of 0.9 mm in patients with isolated ACL and 1.7 mm in the combined group (P = .013). These midterm results revealed the persistence of a mild medial laxity at 3-year follow-up. Therefore, an increased rate of failures or lower clinical scores were expected in the combined group for future follow-up. Since those groups demonstrated no difference in PROMs or failures even after 14 years, it is possible that the magnitude of this medial instability was below a safety threshold and that the knee kinematics were not significantly affected. For this reason, a value of 1.7 mm of medial gapping at a short-term follow-up could be used as a reference for a favorable long-term prognosis.
The present study has several limitations. First, the surgical technique was a double-bundle ACL reconstruction; therefore, the decision to perform a more standard, single-bundle ACL reconstruction could lead to different results over time. However, there is no evidence that the double bundle is superior to the standard techniques in controlling the valgus laxity. 22 Conversely, biomechanical studies 2,3,6 showed that the main difference between these techniques is about controlling the rotational instability in terms of pivot shift. Moreover, Donaldson et al 5 stated that the pivot shift could be decreased if a concomitant injury to the medial compartment is present because of the reduced valgus force applied during the maneuver. It is therefore possible that the biomechanical differences between the techniques could be additionally smoothed out because of the reduced pivot shift in patients with this combined injury.
Second, the lack of objective evaluation could have underestimated the failure rate: Subclinical failures or mild instability not requiring an ACL revision could not have been detected. Yet, the patients were carefully interviewed, and if they indicated a history of trauma or instability, they were invited for a clinical and imaging evaluation. Third, there is a possible administration bias since the clinical scores were collected through a phone interview. However, the Lysholm and WOMAC scores have been cross-validated, and the telephone interview has demonstrated similar results as those of face-to-face administration. 4,12 Other limitations are the absence of a consistent number of female patients and the older age of our patients at the time of surgery. Females’ knees tend to be more valgus, which could have negatively influenced nonoperative MCL treatment. The advanced age could have affected the level of sports activity, potentially masking a higher risk of failure for the patients participating in higher-demand activity. Although this article gives information about the general surgical approach, treatment considerations in athletes should be performed with more selected samples. The final limitation is the lack of radiographical examination, which would allow a more objective evaluation of osteoarthritis progression in the 2 groups.
Conclusion
Nonoperative treatment of grade 2 MCL lesion with ACL reconstruction led to results comparable to isolated ACL reconstruction in terms of clinical scores, Tegner activity level, and failure rates at minimum 14-year follow-up.
Acknowledgment
The authors thank Silvia Bassini for the illustrations in Figure 1.
Footnotes
Final revision submitted June 15, 2021; accepted June 29, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.Z. is a consultant surgeon for DePuy Synthes and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Istituto Ortopedi Rizzoli.
References
- 1. Battaglia MJ, Lenhoff MW, Ehteshami JR, et al. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: a biomechanical evaluation in a cadaveric model. Am J Sports Med. 2009;37(2):305–311. [DOI] [PubMed] [Google Scholar]
- 2. Bedi A, Musahl V, O’Loughlin P, et al. A comparison of the effect of central anatomical single-bundle anterior cruciate ligament reconstruction and double-bundle anterior cruciate ligament reconstruction on pivot-shift kinematics. Am J Sports Med. 2010;38(9):1788–1794. [DOI] [PubMed] [Google Scholar]
- 3. Björnsson H, Desai N, Musahl V, et al. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):696–739. [DOI] [PubMed] [Google Scholar]
- 4. Carpenter CVE, Blackburn J, Jackson J, Blom AW, Sayers A, Whitehouse MR. Validated repeatability of patient-reported outcome measures following primary total hip replacement: a mode of delivery comparison study with randomized sequencing. Acta Orthop. 2018;89(6):628–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Donaldson WF, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations: initial versus examination under anesthesia. Am J Sports Med. 1985;13(1):5–10. [DOI] [PubMed] [Google Scholar]
- 6. Ferretti A, Monaco E, Labianca L, Conteduca F, De Carli A. Double-bundle anterior cruciate ligament reconstruction: a computer-assisted orthopaedic surgery study. Am J Sports Med. 2008;36(4):760–766. [DOI] [PubMed] [Google Scholar]
- 7. Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;132:206–218. [PubMed] [Google Scholar]
- 8. Funchal LFZ, Astur DC, Ortiz R, Cohen M. The presence of the arthroscopic “floating meniscus” sign as an indicator for surgical intervention in patients with combined anterior cruciate ligament and grade II medial collateral ligament injury. Arthroscopy. 2019;35(3):930–937. [DOI] [PubMed] [Google Scholar]
- 9. Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and non-operative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34(7):1134–1140. [DOI] [PubMed] [Google Scholar]
- 10. Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament: results of long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1328–1344. [DOI] [PubMed] [Google Scholar]
- 11. James E, Williams B, LaPrade R. Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res. 2014;472(9):2644–2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kose O, Deniz G, Ozcan H, Guler F. A comparison of telephone interview versus on-site completion of Lysholm knee score in patients who underwent arthroscopic ACL reconstruction: are the results equivalent? Eur J Orthop Surg Traumatol Orthop Traumatol. 2015;25(6):1069–1072. [DOI] [PubMed] [Google Scholar]
- 13. Lind M, Jacobsen K, Nielsen T. Medial collateral ligament (MCL) reconstruction results in improved medial stability: results from the Danish knee ligament reconstruction registry (DKRR). Knee Surg Sports Traumatol Arthrosc. 2020;28(3):881–887. [DOI] [PubMed] [Google Scholar]
- 14. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. [DOI] [PubMed] [Google Scholar]
- 15. Marcacci M, Molgora AP, Zaffagnini S, Vascellari A, Iacono F, Presti ML. Anatomic double-bundle anterior cruciate ligament reconstruction with hamstrings. Arthrosc J Arthrosc Relat Surg. 2003;19(5):540–546. [DOI] [PubMed] [Google Scholar]
- 16. Martelli S, Zaffagnini S, Bignozzi S, Lopomo N, Marcacci M. Description and validation of a navigation system for intra-operative evaluation of knee laxity. Comput Aided Surg. 2007;12(3):181–188. [DOI] [PubMed] [Google Scholar]
- 17. Papalia R, Osti L, Del Buono A, Denaro V, Maffulli N. Management of combined ACL-MCL tears: a systematic review. Br Med Bull. 2010;93:201–215. [DOI] [PubMed] [Google Scholar]
- 18. Scheffler SU, Clineff TD, Papageorgiou CD, Debski RE, Ma CB, Woo SL. Structure and function of the healing medial collateral ligament in a goat model. Ann Biomed Eng. 2001;29(2):173–180. [DOI] [PubMed] [Google Scholar]
- 19. Shelbourne KD, Porter DA. Anterior cruciate ligament-medial collateral ligament injury: non-operative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med. 1992;20(3):283–286. [DOI] [PubMed] [Google Scholar]
- 20. Smyth MP, Koh JL. A review of surgical and nonsurgical outcomes of medial knee injuries. Sports Med Arthrosc Rev. 2015;23(2):e15–e22. [DOI] [PubMed] [Google Scholar]
- 21. Svantesson E, Hamrin Senorski E, Alentorn-Geli E, et al. Increased risk of ACL revision with non-surgical treatment of a concomitant medial collateral ligament injury: a study on 19,457 patients from the Swedish National Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2450–2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tsai AG, Wijdicks CA, Walsh MP, Laprade RF. Comparative kinematic evaluation of all-inside single-bundle and double-bundle anterior cruciate ligament reconstruction: a biomechanical study. Am J Sports Med. 2010;38(2):263–272. [DOI] [PubMed] [Google Scholar]
- 23. Zaffagnini S, Bignozzi S, Martelli S, Lopomo N, Marcacci M. Does ACL reconstruction restore knee stability in combined lesions? An in vivo study. Clin Orthop Relat Res. 2007;454:95–99. [DOI] [PubMed] [Google Scholar]
- 24. Zaffagnini S, Bonanzinga T, Marcheggiani Muccioli GM, et al. Does chronic medial collateral ligament laxity influence the outcome of anterior cruciate ligament reconstruction? A prospective evaluation with a minimum three-year follow-up. J Bone Joint Surg Br. 2011;93(8):1060–1064. [DOI] [PubMed] [Google Scholar]
- 25. Zhu J, Dong J, Marshall B, Linde MA, Smolinski P, Fu FH. Medial collateral ligament reconstruction is necessary to restore anterior stability with anterior cruciate and medial collateral ligament injury. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):550–557. [DOI] [PubMed] [Google Scholar]