Abstract
Objectives
This study aimed to evaluate the prevalence and incidence of herpes zoster (HZ) events and describe its associated factors in a study of patients with SLE.
Methods
491 consecutive SLE participants were screened for HZ events using a patient-reported questionnaire to capture outcomes on pain and other characteristics associated with HZ events. Sociodemographic, clinical and laboratory measures were also analysed, and time-dependent Cox regression survival analyses were performed to investigate factors associated with HZ events.
Results
Prevalence of HZ was 30.5%, incidence was 14.3 cases per 1000 person-years. Lymphopenia and glucocorticoid dosing were significantly associated with HZ events.
Conclusions
HZ is highly prevalent in SLE, which may be linked to disease-related and treatment-related effects on cellular immunity. Our results suggest that the presence of certain risk factors may be useful to allow identification of patients at risk of HZ and improve its management in patients with SLE.
Keywords: systemic lupus erythematosus, glucocorticoids, outcome assessment, health care
Key messages.
What is already known about this subject?
Higher prevalence and incidence of herpes zoster (HZ) events are present in patients with SLE compared with the general population—thought to be a result of differences in cell-mediated immunity. Certain risk factors have been identified in the literature, including disease activity and immunosuppressive therapies, though findings have been inconsistent.
What does this study add?
This study assesses the prevalence and incidence of HZ events in a lupus cohort using data from a novel questionnaire developed to assess patient-reported outcomes on characteristics related to HZ events, including pain, vaccination status, hospitalisations, treatments, complications of HZ events and onset after SLE diagnosis.
A significant association exists between the development of HZ events in patients with SLE and lymphopenia, as well as glucocorticoid dosing.
How might this impact on clinical practice or future developments?
The identification of associated factors from this study will allow targeted screening of patients at higher risk to allow for earlier diagnosis and improved management of HZ events in patients with SLE.
Furthermore, risk factors identified give insight into the pathophysiology behind opportunistic infections in SLE and may allow improved treatment modalities, as well as a more complete understanding of HZ events in patients with SLE.
Introduction
Herpes zoster (HZ) is caused by the reactivation of latent varicella-zoster virus (VZV) in patients that may have experienced an exposure up to decades prior.1 The infection can manifest as an acute painful vesicular rash that presents in a dermatomal pattern and can be followed by a persistent postzoster pain (postherpetic neuralgia).1 HZ and the occurrence of postzoster pain have also been shown to have significant impacts on healthcare costs,2 3 loss of productivity4 5 and patients’ health-related quality of life.6 7
Recurrent infection is most commonly seen in elderly and immunocompromised populations—including patients with malignancies,8 9 acquired immune deficiency syndrome, autoimmune diseases such as rheumatoid arthritis9–12 and SLE).9 13 14 In the general population, HZ incidence ranges between 1.2 and 4.9 cases per 1000 person-years.15 16 In comparison, the incidence is increased sixfold in SLE, where the incidence ranges from 6.4 to 37.7 cases per 1000 person-years.13 14 Across all age groups in SLE, an age-adjusted HZ incidence rate has been shown to be 12 cases per 1000 patient-years.1
HZ incidence has been attributed to declining VZV-specific cell-mediated immunity.17 As a result, it would also explain the increased incidence in SLE, where patients have been shown to have abnormal T cell mediated cytotoxicity and suppression of cellular immunity from both disease activity and immunosuppressive therapies, including glucocorticoids.18 Other risk factors for developing HZ in patients with SLE have been studied, though findings have been inconsistent.19–21 In this study, we aimed to evaluate the prevalence and incidence of HZ, and describe its associated factors in a study of patients with SLE. We also determined patient-reported outcomes on pain and other characteristics related to HZ events based on a questionnaire developed for this study.
Methods
Study design and patient selection
In this prospective cross-sectional study, a patient-reported questionnaire was developed by the Toronto Lupus Clinic (figure 1) to investigate HZ events in patients with SLE, capturing items related to patients’ demographics, HZ symptoms, onset, recurrence, vaccinations or hospitalisations related to HZ, and other factors associated with HZ events. This questionnaire was distributed to patients visiting the clinic between May 2016 to November 2018. All patients fulfilled ≥4 of the American College of Rheumatology (ACR) revised criteria for the classification of SLE, or 3 ACR criteria and a typical biopsy lesion of SLE.22 All patients provided informed written consent for participation in this study.
Figure 1.
Herpes zoster (HZ) survey.
Patient assessment
SLE Disease Activity Index 2000 (SLEDAI-2K, SLEDAI-2K glucocorticoid index (SLEDAI-2KG), and the Systemic Lupus International Collaborating Clinics/ACR Damage Index (SDI) were determined for each patient.23–25 The clinical variables evaluated in this study were SLEDAI-2K scores at each visit, SDI scores at each visit, presence of fibromyalgia within the past 6 months and SLEDAI-2K manifestations at each study visit.24 25 SLE clinical phenotypes were stratified based on the nine organ systems of SLEDAI-2K, including skin (skin rash, alopecia and mucosal ulcers), central nervous system (seizure, psychosis, organic brain syndrome, cranial nerve involvement, visual disturbance, lupus headache, cerebrovascular accident and vasculitis), musculoskeletal (MSK) (arthritis and myositis), renal (proteinuria, hematuria, pyuria and urinary casts), serosal (pleuritis and pericarditis), haematological (leucopenia and thrombocytopenia), immunological (low complements and positive anti-dsDNA antibodies), and constitutional (fever) symptoms.25 Other variables included age, gender, ethnicity, demographic characteristics such as disease duration, age at SLE diagnosis, SLE disease duration at first HZ event and recurrent HZ events.
Statistical methodology
Description of cohort and HZ events
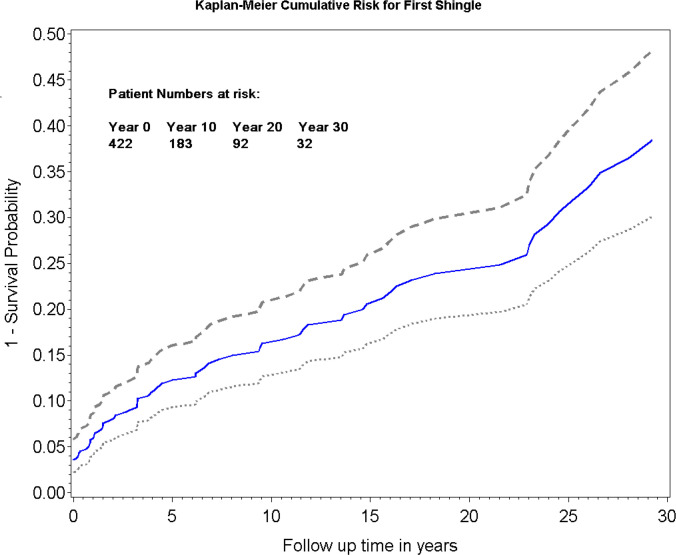
Patients were classified based on the presence of HZ symptoms over the duration of the study. Demographic, clinical and laboratory data for patients with and without HZ events, at their first visit to clinic, were described using mean±SD and count (percentage) to represent continuous and categorical variables, respectively. The incidence rates for the first and all HZ events were calculated using follow-up person-years from the patients’ first clinic visit to the date of survey completion. The CI of the incidence rate was estimated based on the assumption that the number of events occurring in a fixed interval of time follow a Poisson distribution. A Kaplan-Meier curve was created for the cumulative probability to first HZ event with 95% CIs and number of patients at risk over time.
Association between demographics, clinical and laboratory variables with HZ events
Three time-dependent survival analyses were performed to investigate factors associated with first or recurrent HZ events. The same variables were included in all three models: the first model with SLEDAI-2K, the second model with SLEDAI-2KG and a third model focused on studying the association with nine organ systems based on SLEDAI-2K. SLEDAI-2K and SLEDAI-2KG were completed at each clinical visit including the visit of the questionnaire fulfilment, while the SDI was performed annually. Counting process survival data were constructed for the three time-dependent Cox regressions (for the first event and repeated events). This was calculated from the date of first visit to the date of the first HZ event, or until the most recent visit for which the patient remained HZ-free. Explanatory variables in the models were included based on clinical relevance and literature review. Variables with potential collinearities were not included into the same regression model; these included the individual SLEDAI-2K organ systems, as well as SLEDAI-2K scores and glucocorticoid dosing in the SLEDAI-2KG model. A stepdown variable selection method was used in the multivariable model-building process; variables with highest p values were selected out using the Akaike Information Criterion as the model fitting statistic. The collinearities between total SLEDAI-2K Score and three relevant laboratory tests, including leucopenia, neutropenia and lymphopenia were assessed and demonstrated low correlations. As a result, the positive or negative laboratory results were entered into the three multivariable regressions as binary covariates.
The counting process model for recurrent data in survival analysis was used, where each HZ event was assumed to be independent and the subject contributes to the risk set if the subject was under observation at the time the event occurred.26 All analyses were performed in SAS V.9.3 with statistical significance deemed to be under 0.05.
Results
Cohort characteristics
Over the duration of the study, from May 2016 to November 2018, there were a total of 956 patients that attended the Toronto Lupus Clinic; each of them was approached to participate in the study. Of those, 491 patients completed the study questionnaire, 2 of which did not complete the first question ‘Have you ever had painful vesicular skin rash (shingles=herpes zoster virus) as shown in this picture’ and were excluded from the analysis. Of the 489 remaining patients, 149 reported having an HZ event and 340 never experienced an HZ event. Among the 149 patients with an HZ event, 26 did not report the year of the HZ event and were excluded from further analyses. Furthermore, 41 participants reported their HZ event prior to their first visit to the clinic—these patients were also excluded from the analyses. The final cohort therefore comprised of 422 patients with SLE.
In this cohort of 422 patients, the majority were female and Caucasian, followed by Black, Chinese and others. This was balanced across both the patients that reported HZ events and those that did not. The average ages at SLE diagnosis for patients with HZ and patients without HZ events were 29.3±12.0 years and 31.0±11.4 years, respectively. The mean age at the patient’s first clinic visit was 33.4±12.8 years for patients reporting HZ events and 35.2±11.6 years for patients that did not report HZ. The mean SLE disease duration at the time of study was 4.2±6.4 years for both groups.
The prevalence of HZ in our cohort was 30.5% and the incidence was 14.0 cases per 1000 person-years (95% CI 11.5 to 17.7), with 82 reporting occurrence of HZ since following at the clinic, and 340 patients that did not develop HZ. Among the 82 patients with HZ, 16 reported recurrence of HZ within 8.7±10.4 years from the initial event; including these recurrent events, this resulted in an HZ incidence rate of 17.0 cases per 1000 person-years (95% CI 14.0 to 20.8).
MSK involvement was significantly higher among patients reporting HZ events, though this was not statistically significant after Bonferroni adjustment. No statistically significant differences were found in the prevalence of other SLEDAI-2K manifestations, including central nervous system (CNS), vascular, renal, skin, serosal, immunological, haematological or constitutional symptoms. Demographics of patients with SLE with and without HZ included in our study are presented in tables 1 and 2.
Table 1.
Demographic and clinical description of patients at fulfilment of the questionnaire, n=422
| Variable | Value | No HZ n=340 |
HZ event n=82 |
P value | |
| Demographics | Sex |
F | 308 (90.6%) | 78 (95.1%) | 0.19 |
| M | 32 (9.4%) | 4 (4.9%) | |||
| Age at SLE diagnosis |
Mean±SD | 31.0±11.4 | 29.3±12.0 | 0.22 | |
| Min, Max | 8–66 | 8–76 | |||
| Age at first visit to the clinic |
Mean±SD | 35.2±11.6 | 33.4±12.8 | 0.22 | |
| Min, Max | 16–68 | 14–76 | |||
| SLE duration at first visit to the clinic |
Mean±SD | 4.2±6.4 | 4.2±6.4 | 0.94 | |
| Min, Max | 16–68 | 0–32 | |||
| Ethnicity | Black | 72 (21.2%) | 8 (9.8%) | 0.03 | |
| Caucasian | 196 (57.6%) | 60 (73.2%) | |||
| Chinese | 27 (7.9%) | 8 (9.8%) | |||
| Others | 45 (13.2%) | 6 (7.3%) | |||
| Caucasian | Yes (%) | 196 (57.6%) | 60 (73.2%) | 0.01 | |
| Black | Yes (%) | 72 (21.2%) | 8 (9.8%) | 0.02 | |
| SLE duration at first HZ event | Mean±SD | N/A | 12.5±10.6 | N/A | |
| HZ events | Age at first HZ event | Mean±SD | N/A | 41.8±15.4 | N/A |
| Recurrent HZ infection | Yes (%) | N/A | 16 (19.5%) | N/A | |
| Years between first and second HZ event | Mean±SD | N/A | 8.7±10.4 | N/A | |
| SDI score | Mean±SD | 0.2±0.6 | 0.2±0.5 | 0.52 |
HZ, herpes zoster; SDI, Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index.
Table 2.
SLE clinical manifestations stratified by organ systems of SLEDAI-2K
| Variable | Value | No HZ n=340 |
HZ event n=82 |
P value | Bonferroni adjusted |
| Central nervous system | Yes (%) | 32 (9.4%) | 9 (11.0%) | 0.67 | 1.00 |
| Vasculitis | Yes (%) | 25 (7.4%) | 8 (9.8%) | 0.47 | 1.00 |
| Musculoskeletal | Yes (%) | 65 (19.1%) | 24 (29.3%) | 0.04 | 0.33 |
| Renal | Yes (%) | 78 (22.9%) | 16 (19.5%) | 0.50 | 1.00 |
| Skin | Yes (%) | 139 (40.9%) | 41 (50.0%) | 0.13 | 0.72 |
| Serosal | Yes (%) | 26 (7.6%) | 7 (8.5%) | 0.79 | 1.00 |
| Immunological | Yes (%) | 229 (67.4%) | 51 (62.2%) | 0.38 | 0.98 |
| Constitutional | Yes (%) | 30 (8.8%) | 8 (9.8%) | 0.79 | 1.00 |
| Haematological | Yes (%) | 36 (10.6%) | 8 (9.8%) | 0.83 | 1.00 |
| SLEDAI-2K | Mean±SD | 7.7±6.8 | 8.5±7.8 | 0.32 | – |
| SLEDAI-2KG | Mean±SD | 5.5±3.0 | 5.9±3.1 | 0.34 | – |
HZ, herpes zoster; SLEDAI-2K, SLE Disease Activity Index 2000; SLEDAI-2KG, SLEDAI-2K Glucocorticoid Index.
Description of HZ events
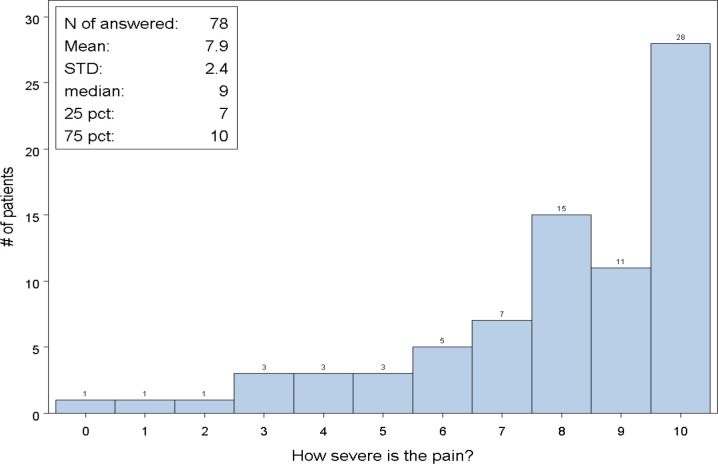
Among the 82 patients that reported HZ events, 35.4% reported HZ occurrence within the first 5 years of initial SLE diagnosis, 14.6% after 6–10 years of diagnosis and 50% occuring more than 10 years after SLE diagnosis. Mean SLE duration at first HZ event was 12.5±10.6 years. The majority of patients (98.8%) had their HZ event confirmed by a physician, with 80% receiving antiviral therapy and 15.9% requiring hospitalisation for severe HZ. Most patients (84.2%) who developed HZ never received a varicella zoster vaccine. HZ symptoms, involving rash with associated pain, itching or tingling, occurred in 95.1% of patients, with 74% rating the pain between 7 and 10 (figure 2). More than half (55.7%) of the patients experienced severe pain after HZ infection, lasting up to 3 months in duration in 48.8%, 3–6 months in 17.1%, and beyond 6 months in 34.2% of patients. There was no correlation between pain severity and ‘time since HZ event’, with a Spearman correlation coefficient 0.18 (p=0.16, n=65/82), suggesting that the time since HZ event had no significant impact on the recall of pain severity. Survival analyses showed that the cumulative risk of developing HZ increased with time after diagnosis of SLE (figure 3). Description of HZ events have been presented in table 3.
Figure 2.
Herpes zoster pain severity as reported by patients with SLE (n=138). STD, standard deviation.
Figure 3.
Kaplan-Meier cumulative risk for first herpes zoster event.
Table 3.
Results of the HZ Questionnaire
| Onset after SLE diagnosis | Frequency (%) | |||||||
| 1–5 years post-SLE diagnosis | 29 (35.4) | |||||||
| 6–10 years post-SLE diagnosis | 12 (14.6%) | |||||||
| >10 years post-SLE diagnosis | 41 (50.0%) | |||||||
| HZ symptoms: occurrence of pain, itching, tingling with rash | ||||||||
| No | 4 (4.9%) | |||||||
| Yes | 78 (95.1%) | |||||||
| Confirmed of HZ diagnosis by physician | ||||||||
| No | 1 (1.2%) | |||||||
| Yes | 81 (98.8%) | |||||||
| Vaccination history: ever received varicella zoster vaccine | ||||||||
| No | 69 (84.2%) | |||||||
| Yes | 13 (15.9%) | |||||||
| Hospitalisations: ever hospitalised for severe HZ? | ||||||||
| No | 69 (84.2%) | |||||||
| Yes | 13 (15.9%) | |||||||
| Treatment for HZ : ever received treatments (eg, antivirals) for HZ? | ||||||||
| No | 16 (20%) | |||||||
| Yes | 64 (80%) | |||||||
| Missing | 2 | |||||||
| Postherpetic neuralgia: history of severe pain after HZ infection? | ||||||||
| No | 35 (44.3%) | |||||||
| Yes | 44 (55.7%) | |||||||
| Missing | 3 | |||||||
| Duration of postherpetic neuralgia, if present | ||||||||
| 3 months | 20 (48.8%) | |||||||
| 3–6 months | 7 (17.1%) | |||||||
| >6 months | 14 (34.2%) | |||||||
| Missing | 3 | |||||||
| SLE treatments at time of HZ infection? | ||||||||
| Prednisone | 59 (71.9%) | |||||||
| Hydroxychloroquine | 50 (61%) | |||||||
| Azathioprine | 29 (35%) | |||||||
| Mycophenolate mofetil or mycophenolic acid | 14 (17.1%) | |||||||
| Cyclophosphamide | 2 (2.4%) | |||||||
| Belimumab | 0 (0%) | |||||||
| Rituximab | 2 (2.4%) | |||||||
| Methotrexate | 4 (4.9%) | |||||||
| Other treatment | 15 (18.3%) | |||||||
| Prednisone dose in mg/day, if taken | ||||||||
| Frequency | Missing | Minimum dose | Mean dose | SD | Median dose | Lower quartile | Upper quartile | Maximum dose |
| 23 | 36 | 1 | 22.3 | 19.5 | 15 | 5 | 30 | 60 |
HZ, herpes zoster.
Fifty-nine patients (71.9%) reported being on prednisone for SLE at the time of the HZ event. Of those, 43 patients reported a mean prednisone dose of 22.3 mg/day (range, 1–60 mg/day) (table 3). Fourty-nine patients (59.4%) were on immunosuppressant therapy, including azathioprine (35%), mycophenolate mofetil (17.1%), methotrexate (4.9%) and cyclophosphamide (2.4%) (table 3).
Association between HZ events and patient characteristics, clinical and laboratory variables
No demographic characteristics, including gender, age at diagnosis, age at first visit or ethnicity were associated with development of HZ in either the univariable or the three multivariable models (table 4).
Table 4.
Time-dependent survival analyses using three regression models with SLEDAI-2K, SLEDAI-2KG and SLEDAI organ systems
| Univariable cox regression | Multivariable analysis with SLEDAI-2K | Multivariable analysis with SLEDAI-2KG | |||||
| HR (95% CI) |
P value | HR (95% CI) |
P value | HR (95% CI) | P value | ||
| Demographics | Female sex | 1.89 (0.69 to 5.17) | 0.22 | 2.41 (0.76 to 7.67) | 0.13 | 2.51 (0.79 to 7.98) | 0.12 |
| Age at SLE diagnosis | 1.00 (0.98 to 1.02) | 0.77 | |||||
| Age at first visit | 1.00 (0.98 to 1.02) | 0.73 | |||||
| Caucasian | 1.46 (0.89 to 2.38) | 0.13 | 1.41 (0.85 to 2.32) | 0.18 | |||
| Study protocol | SLEDAI-2KG at each visit | 1.21 (1.10 to 1.33) | <0.0001 | 1.178 (1.06 to 1.31) | 0.002 | ||
| SLEDAI-2K at each visit | 1.06 (1.02 to 1.11) | 0.004 | 1.04 (0.99 to 1.09) | 0.11 | |||
| SDI score | 0.87 (0.72 to 1.10) | 0.14 | 0.84 (0.69 to 1.02) | 0.10 | 0.84 (0.69 to 1.02) | 0.09 | |
| Fibromyalgia | 0.94 (0.48 to 1.85) | 0.86 | |||||
| Treatment | Glucocorticoid Use | 1.66 (1.04 to 2.66) | 0.03 | Not entered into multivariable analysis, part of SLEDAI-2KG | |||
| Glucocorticoid dose (mg/day) | 1.02 (1.01 to 1.02) | 0.0001 | 1.01 (1.001 to 1.02) | 0.03 | |||
| Antimalarial | 1.19 (0.75 to 1.90) | 0.46 | |||||
| Treated with Immunosuppressives | 1.52 (0.98 to 2.36) | 0.06 | |||||
| Laboratory markers | Antiphospholipid antibody at any time | 0.94 (0.48 to 1.85) | 0.86 | ||||
| Leucopenia (WBC<4.0*10∧9 /L) | 1.27 (0.51 to 3.2) | 0.60 | |||||
| Neutropenia (<1.5* 10∧9) | 0.83 (0.40 to 1.73) | 0.62 | |||||
| Lymphopenia (<1.0* 10∧9) | 1.78 (1.12 to 2.80) | 0.01 | 1.63 (1.02 to 2.59) | 0.041 | 1.56 (0.98 to 2.49) | 0.06 | |
| Anaemia | 1.25 (0.78 to 2.02) | 0.36 | |||||
| Low IgA | 1.52 (0.21 to 10.10) | 0.68 | |||||
| Low IgG | 1.61 (0.39 to 6.58) | 0.51 | |||||
| Low IgM | 1.12 (0.35 to 3.55) | 0.85 | |||||
*All of the above variables were time-dependent with the exception of: female sex, age at SLE diagnosis, age at first visit and Caucasian ethnicity.
*In the third multivariable regression model with SLEDAI organ systems, lymphopenia was the only statistically significant predictor of HZ events (HR=1.64, 95% CI 1.03 to 2.95, p=0.037), the other adjusted variables in the model included SLEDDAI-2K organ systems, SDI and glucocorticoid dose which did not sustain significance. As a result this was not included in the above table.
HZ, herpes zoster; SLEDAI-2K, SLEDAI-2K, SLE Disease Activity Index 2000; SLEDAI-2KG, SLEDAI-2K Glucocorticoid Index; WBC, white blood cells.
Model with SLEDAI-2K
Lymphopenia was associated with HZ events in the univariable analysis (HR=1.77; 95% CI 1.12 to 2.80; p=0.01) and in the multivariable analysis (HR=1.63; 95% CI 1.02 to 2.59; p=0.04). There was an association between HZ events and SLEDAI-2K Score, though only for the univariable analysis (HR=1.06; CI 1.02 to 1.11; p=0.004). No association was found between SDI scores and HZ events in either the univariable or multivariable models (table 4).
Glucocorticoid dosing was associated with HZ events in the univariable (HR=1.02; 95% CI 1.01 to 1.02; p=0.0001) and multivariable analysis with SLEDAI-2K (HR=1.01; 95% CI 1.00 to 1.02; p=0.03).
Model with SLEDAI-2KG
In this model, lymphopenia did not sustain significance (HR=1.56; 95% CI 0.98 to 2.49; p=0.06). There was an association between HZ events and SLEDAI-2KG scores in both the univariable (HR=1.21; CI 1.1 to 1.33; p<0.0001) and multivariable analysis with SLEDAI-2KG (HR=1.18; CI 1.06 to 1.31; p=0.002) (table 4).
Model with SLEDAI-2K organ systems
In this model, the only variable that was associated with HZ events was lymphopenia (HR=1.64; 95% CI 1.03 to 2.60; p=0.04). Neither SLEDAI-2K organ scores or SDI scores were associated with HZ events. Furthermore, glucocorticoid dosing did not sustain significance (HR=1.01; 95% CI 1.00 to 1.02; p=0.06) (data not shown in table 3).
Discussion
The prevalence and incidence of HZ in this study were 30.5% and 14.3 cases per 1000 person-years, respectively. This is in keeping with findings published in the literature of prevalence varying from 13.5% to 46.6% of adult patients with SLE,27 and incidence in SLE ranging from 6.3 to 37.7 cases per 1000 person-years.13 14 Furthermore, the HZ recurrence rate in our study was 1.7%. This is similar to results from a study by Yawn et al, where they demonstrated a recurrence rate of 1.4%, within 3 years, in a general population-based study of 1669 adult residents.28 In SLE, it is recognised that HZ is a late complication—with one study showing two-thirds of patients with an SLE disease duration greater than 5 years.13 In our study, the SLE disease duration at the time of the first HZ infection was 12.5±10.6 years.
From our questionnaire, most patients who developed HZ had not been vaccinated against varicella zoster, which may suggest a clinical gap that can be addressed to reduce susceptibility to HZ infections. However, while guidelines recommend live attenuated vaccines for prevention of HZ in healthy adults over 60 years of age, the use of live vaccines has been limited in SLE due to evidence of increased risk of severe adverse events in immunocompromised patients.29–31 Newer recombinant zoster vaccines, such as the non-live Varicella zoster vaccine recombinant, adjuvanted, have shown utility in patients with SLE32 and may provide an alternate option to circumvent the need for live HZ vaccines. This is in keeping with the 2019 EULAR guidelines for vaccinations in patients with autoimmune inflammatory rheumatic diseases, including SLE. Large retrospective studies have shown the effectiveness of the HZ vaccine in reducing incidence of HZ over a 2-year follow-up period, regardless of medication use, offering protection for approximately 5 years in those with autoimmune diseases.33
Postherpetic neuralgia is the most common complication of HZ, and in our study, 34% of patients developed severe pain lasting beyond 90 days of their initial HZ infection. This prevalence is similar to what is reported in the literature for the general population, with studies reporting 22%–48% of adult patients reporting symptoms of postherpetic neuralgia.28 34–36 Overall, less than 20% required hospitalisation for severe HZ, which is also in keeping with other studies.13
Over half of our patients who developed HZ were on immunosuppressant therapy, with 72% of patients on glucocorticoids at the time of the HZ event, and a mean dose of 22.3 mg/day. Our analyses confirmed the association of glucocorticoid dosing with HZ events, a finding that is in keeping with similar studies that have shown immunosuppressive therapies to be risk factors for development of HZ infections in patients with SLE.8 12 14 37–40 This is thought to be mediated through effects on inhibiting T-lymphocyte-mediated and B-lymphocyte-mediated immune responses, as well as their suppressive effects on monocytes and neutrophils.41 42 In one study by Shah et al, a mean daily dose greater than 7.5 mg of prednisone resulted in increased susceptibility of opportunistic infection such as HZ, pneumonia and other fungal infections;43 with evidence of a strong dose-response relationship for glucocorticoids.39 It is worth noting that glucocorticoid dosing may also be an indication of the level of SLE disease activity, which in itself may be a risk factor for HZ events—independent of immunosuppressive therapy.44 Another factor associated with HZ events across both univariable and multivariable regression analyses included lymphopenia—which has been shown in literature to be an independent risk factor for HZ in patients with SLE20 45–48 and may be a result of both lupus-related and treatment-related effects on lymphocyte-mediated immune responses. Both Ng et al and Hu et al showed that frequency of lymphopenia was higher in patients with SLE that developed HZ. The exact mechanism of this is not well understood, and it is hypothesised that this may be a result of defective cell-mediated immunity, an integral component of defence against VZV reactivation.45 49 50
In our univariable and multivariable analyses, we found an association between SLEDAI-2KG scores and development of HZ. The literature surrounding the association between HZ events and disease activity is mixed, with some studies showing that the majority of zoster reactivation occurs during mild or inactive disease;37 49 51 for example, in a study by Borba et al, nearly half of their patients with HZ reactivation had a SLEDAI score of 0—with most patients (82.4%) exhibiting a SLEDAI <8 (13). Contrary to this, other studies have demonstrated HZ association with higher disease activity.20 52 In this study, association of HZ events with SLEDAI-2KG scores is likely due to the accounting of glucocorticoid dosing, a factor that is independently associated with HZ events. This hypothesis is supported by the fact that SLEDAI-2K scores, that do not account for glucocorticoid dosing, were not associated with HZ events in our multivariable analysis.
Possible limitations of this study include that only half of the approached patients agreed to participate in the study. Although further data were not collected around reasons for declining participation, this was most often related to patients’ limited time and commitment to other activities after their clinic visit. While this may possibly introduce a selection bias resulting in an overestimation of prevalence, our results are consistent with those found in literature. Furthermore, HZ events were patient-reported and physician-confirmed. As we do not have details surrounding the method of confirmation, this may contribute to possible bias which could also affect the estimation of HZ prevalence and incidence. However, studies have shown that the accuracy of self-reported HZ can be quite reliable, which helps to mitigate this risk.53 As we did not have a control group in this study, further studies will have to be performed to validate these findings in other SLE cohorts and to compare them with an immunocompetent group to determine their generalisability and possible use for predicting patients at high risk for HZ reactivation.
Conclusion
In conclusion, this study highlights the prevalence of HZ in an SLE patient cohort, while investigating the relationships among sociodemographic, clinical and laboratory variables. Measures such as lymphopenia and glucocorticoid dosing were associated with HZ development and are consistent with results of other reports suggesting an increased risk for HZ development in SLE that may be linked to both disease-specific immunological imbalances, as well as treatment regimens. Together, these risk factors may serve as useful indicators to be considered in patients with SLE to allow for closer monitoring for earlier diagnosis and improved management of HZ.
Footnotes
Contributors: All authors contributed towards the study design, analysis and development of the manuscript. Dr Zahi Touma has access to the data.
Funding: ZT is supported by the Arthritis Society, Young Investigator Award and the Canadian Rheumatology Association (CIORA) - Arthritis Society Clinician Investigator Award and by the Department of Medicine, University of Toronto. The Toronto Lupus Program and ZT’s laboratory are supported by donations from the Kathi and Peter Kaiser family, the Lou and Marissa Rocca family and the Bozzo family.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the University Health Network Research Ethics Board, CAPCR ID: 11-0397. Participants gave informed consent to participate in the study before taking part.
References
- 1.Chakravarty EF, Michaud K, Katz R, et al. Increased incidence of herpes zoster among patients with systemic lupus erythematosus. Lupus 2013;22:238–44. 10.1177/0961203312470186 [DOI] [PubMed] [Google Scholar]
- 2.Dworkin RH, White R, O'Connor AB, et al. Health care expenditure burden of persisting herpes zoster pain. Pain Medicine 2008;9:348–53. 10.1111/j.1526-4637.2006.00196.x [DOI] [PubMed] [Google Scholar]
- 3.White RR, Lenhart G, Singhal PK, et al. Incremental 1-year medical resource utilization and costs for patients with herpes zoster from a set of US health plans. Pharmacoeconomics 2009;27:781–92. 10.2165/11317560-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 4.Drolet M, Levin MJ, Schmader KE, et al. Employment related productivity loss associated with herpes zoster and postherpetic neuralgia: a 6-month prospective study. Vaccine 2012;30:2047–50. 10.1016/j.vaccine.2012.01.045 [DOI] [PubMed] [Google Scholar]
- 5.Singhal PK, Makin C, Pellissier J, et al. Work and productivity loss related to herpes zoster. J Med Econ 2011;14:639–45. 10.3111/13696998.2011.607482 [DOI] [PubMed] [Google Scholar]
- 6.Katz J, Cooper EM, Walther RR, et al. Acute pain in herpes zoster and its impact on health-related quality of life. Clin Infect Dis 2004;39:342–8. 10.1086/421942 [DOI] [PubMed] [Google Scholar]
- 7.Schmader KE, Sloane R, Pieper C, et al. The impact of acute herpes zoster pain and discomfort on functional status and quality of life in older adults. Clin J Pain 2007;23:490–6. 10.1097/AJP.0b013e318065b6c9 [DOI] [PubMed] [Google Scholar]
- 8.Habel LA, Ray GT, Silverberg MJ, et al. The epidemiology of herpes zoster in patients with newly diagnosed cancer. Cancer Epidemiol Biomarkers Prev 2013;22:82–90. 10.1158/1055-9965.EPI-12-0815 [DOI] [PubMed] [Google Scholar]
- 9.Hata A, Kuniyoshi M, Ohkusa Y. Risk of herpes zoster in patients with underlying diseases: a retrospective hospital-based cohort study. Infection 2011;39:537–44. 10.1007/s15010-011-0162-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonald JR, Zeringue AL, Caplan L, et al. Herpes zoster risk factors in a national cohort of veterans with rheumatoid arthritis. Clin Infect Dis 2009;48:1364–71. 10.1086/598331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smitten AL, Choi HK, Hochberg MC, et al. The risk of herpes zoster in patients with rheumatoid arthritis in the United States and the United Kingdom. Arthritis Rheum 2007;57:1431–8. 10.1002/art.23112 [DOI] [PubMed] [Google Scholar]
- 12.Strangfeld A, et al. Risk of herpes zoster in patients with rheumatoid arthritis treated with anti-TNF-α agents. JAMA 2009;301:737–44. 10.1001/jama.2009.146 [DOI] [PubMed] [Google Scholar]
- 13.Borba EF, Ribeiro ACM, Martin P, et al. Incidence, risk factors, and outcome of herpes zoster in systemic lupus erythematosus. J Clin Rheumatol 2010;16:119–22. 10.1097/RHU.0b013e3181d52ed7 [DOI] [PubMed] [Google Scholar]
- 14.Chen H-H, Chen Y-M, Chen T-J, et al. Risk of herpes zoster in patients with systemic lupus erythematosus: a three-year follow-up study using a nationwide population-based cohort. Clinics 2011;66:1177–82. 10.1590/S1807-59322011000700009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jih J-S, Chen Y-J, Lin M-W, et al. Epidemiological features and costs of herpes zoster in Taiwan: a national study 2000 to 2006. Acta Derm Venereol 2009;89:612–6. 10.2340/00015555-0729 [DOI] [PubMed] [Google Scholar]
- 16.Thomas SL, Hall AJ. What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect Dis 2004;4:26–33. 10.1016/S1473-3099(03)00857-0 [DOI] [PubMed] [Google Scholar]
- 17.Levin MJ. Immune senescence and vaccines to prevent herpes zoster in older persons. Curr Opin Immunol 2012;24:494–500. 10.1016/j.coi.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 18.Kang I, Park SH. Infectious complications in SLE after immunosuppressive therapies. Curr Opin Rheumatol 2003;15:528–34. 10.1097/00002281-200309000-00002 [DOI] [PubMed] [Google Scholar]
- 19.Hu SC-S, Lin C-L, Lu Y-W, SC H, YW L, et al. Lymphopaenia, anti-Ro/anti-RNP autoantibodies, renal involvement and cyclophosphamide use correlate with increased risk of herpes zoster in patients with systemic lupus erythematosus. Acta Derm Venereol 2013;93:314–8. 10.2340/00015555-1454 [DOI] [PubMed] [Google Scholar]
- 20.Lee PPW, Lee T-L, Ho MH-K, et al. Herpes zoster in juvenile-onset systemic lupus erythematosus: incidence, clinical characteristics and risk factors. Pediatr Infect Dis J 2006;25:728–32. 10.1097/01.inf.0000226841.03751.1f [DOI] [PubMed] [Google Scholar]
- 21.Wu S-A, Yeh K-W, Yao T-C, et al. Association of herpes zoster infection with clinical characteristics and MBL2 gene polymorphisms in Chinese children with systemic lupus erythematosus. Pediatr Infect Dis J 2011;30:656–60. 10.1097/INF.0b013e3182127b67 [DOI] [PubMed] [Google Scholar]
- 22.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1982;25:1271–7. 10.1002/art.1780251101 [DOI] [PubMed] [Google Scholar]
- 23.Brunner HI, Silverman ED, Bombardier C, et al. European consensus lupus activity measurement is sensitive to change in disease activity in childhood-onset systemic lupus erythematosus. Arthritis Rheum 2003;49:335–41. 10.1002/art.11111 [DOI] [PubMed] [Google Scholar]
- 24.Gladman D, Ginzler E, Goldsmith C, et al. The development and initial validation of the systemic lupus international collaborating clinics/American College of rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 1996;39:363–9. 10.1002/art.1780390303 [DOI] [PubMed] [Google Scholar]
- 25.Touma Z, Urowitz MB, Ibañez D, et al. SLEDAI-2K 10 days versus SLEDAI-2K 30 days in a longitudinal evaluation. Lupus 2011;20:67–70. 10.1177/0961203310385163 [DOI] [PubMed] [Google Scholar]
- 26.Hosmer DWL S, May S. Applied survival analysis: regression modeling of Time-to-Event data. 2nd edn. Wiley, 2008. [Google Scholar]
- 27.Sayeeda A, Al Arfaj H, Khalil N. Herpes zoster infections in SLE in a university hospital in Saudi Arabia: risk factors and outcomes. Autoimmune Dis 2011;2010:174891. doi:10.4061%2F2010%2F174891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007;82:1341–9. 10.4065/82.11.1341 [DOI] [PubMed] [Google Scholar]
- 29.Millet A, Decaux O, Perlat A, et al. Systemic lupus erythematosus and vaccination. Eur J Intern Med 2009;20:236–41. 10.1016/j.ejim.2008.07.017 [DOI] [PubMed] [Google Scholar]
- 30.Abu-Shakra M. Safety of vaccination of patients with systemic lupus erythematosus. Lupus 2009;18:1205–8. 10.1177/0961203309346507 [DOI] [PubMed] [Google Scholar]
- 31.Cohen JI. Strategies for herpes zoster vaccination of immunocompromised patients. J Infect Dis 2008;197 Suppl 2:S237–41. 10.1086/522129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mok CC. Herpes zoster vaccination in systemic lupus erythematosus: the current status. Hum Vaccin Immunother 2019;15:45–8. 10.1080/21645515.2018.1514228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Furer V, Rondaan C, Heijstek MW, et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 2020;79:39–52. 10.1136/annrheumdis-2019-215882 [DOI] [PubMed] [Google Scholar]
- 34.Chen S-Y, Suaya JA, Li Q, et al. Incidence of herpes zoster in patients with altered immune function. Infection 2014;42:325–34. 10.1007/s15010-013-0550-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott FT, Leedham-Green ME, Barrett-Muir WY, et al. A study of shingles and the development of postherpetic neuralgia in East London. J Med Virol 2003;70 Suppl 1:S24–30. 10.1002/jmv.10316 [DOI] [PubMed] [Google Scholar]
- 36.Kost RG, Straus SE. Postherpetic neuralgia — pathogenesis, treatment, and prevention. N Engl J Med Overseas Ed 1996;335:32–42. 10.1056/NEJM199607043350107 [DOI] [PubMed] [Google Scholar]
- 37.Manzi S, Kuller LH, Kutzer J, et al. Herpes zoster in systemic lupus erythematosus. J Rheumatol 1995;22:1254–8. [PubMed] [Google Scholar]
- 38.Danza A, Ruiz-Irastorza G. Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus 2013;22:1286-94. 10.1177/0961203313493032 [DOI] [PubMed] [Google Scholar]
- 39.Hu SC-S, Yen F-L, Wang T-N, et al. Immunosuppressive medication use and risk of herpes zoster (Hz) in patients with systemic lupus erythematosus (SLE): a nationwide case-control study. J Am Acad Dermatol 2016;75:49–58. 10.1016/j.jaad.2015.12.059 [DOI] [PubMed] [Google Scholar]
- 40.Zhang J, Xie F, Delzell E, et al. Association between vaccination for herpes zoster and risk of herpes zoster infection among older patients with selected immune-mediated diseases. JAMA 2012;308:43–9. 10.1001/jama.2012.7304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luijten RKMAC, Cuppen BVJ, Bijlsma JWJ, et al. Serious infections in systemic lupus erythematosus with a focus on pneumococcal infections. Lupus 2014;23:1512–6. 10.1177/0961203314543918 [DOI] [PubMed] [Google Scholar]
- 42.Ruiz-Irastorza G, Olivares N, Ruiz-Arruza I, et al. Predictors of major infections in systemic lupus erythematosus. Arthritis Res Ther 2009;11:R109. 10.1186/ar2764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shah M, Chaudhari S, McLaughlin TP, et al. Cumulative burden of oral corticosteroid adverse effects and the economic implications of corticosteroid use in patients with systemic lupus erythematosus. Clin Ther 2013;35:486–97. 10.1016/j.clinthera.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 44.Duffy KN, Duffy CM, Gladman DD. Infection and disease activity in systemic lupus erythematosus: a review of hospitalized patients. J Rheumatol 1991;18:1180–4. [PubMed] [Google Scholar]
- 45.Chen D, Li H, Xie J, et al. Herpes zoster in patients with systemic lupus erythematosus: clinical features, complications and risk factors. Exp Ther Med 2017;14:6222–8. 10.3892/etm.2017.5297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ng WL, Chu CM, Wu AKL, et al. Lymphopenia at presentation is associated with increased risk of infections in patients with systemic lupus erythematosus. QJM 2006;99:37–47. 10.1093/qjmed/hci155 [DOI] [PubMed] [Google Scholar]
- 47.Pryor BD, Bologna SG, Kahl LE. Risk factors for serious infection during treatment with cyclophosphamide and high-dose corticosteroids for systemic lupus erythematosus. Arthritis Rheum 1996;39:1475–82. 10.1002/art.1780390906 [DOI] [PubMed] [Google Scholar]
- 48.Ferreira JCOA, Marques HH, Ferriani MPL, et al. Herpes zoster infection in childhood-onset systemic lupus erythematosus patients: a large multicenter study. Lupus 2016;25:754–9. 10.1177/0961203315627203 [DOI] [PubMed] [Google Scholar]
- 49.Nagasawa K, Yamauchi Y, Tada Y, et al. High incidence of herpes zoster in patients with systemic lupus erythematosus: an immunological analysis. Ann Rheum Dis 1990;49:630–3. 10.1136/ard.49.8.630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Park H-B, Kim K-C, Park J-H, et al. Association of reduced CD4 T cell responses specific to varicella zoster virus with high incidence of herpes zoster in patients with systemic lupus erythematosus. J Rheumatol 2004;31:2151–5. [PubMed] [Google Scholar]
- 51.Kahl LE. Herpes zoster infections in systemic lupus erythematosus: risk factors and outcome. J Rheumatol 1994;21:84–6. [PubMed] [Google Scholar]
- 52.Gladman DD, Hussain F, Ibañez D, et al. The nature and outcome of infection in systemic lupus erythematosus. Lupus 2002;11:234–9. 10.1191/0961203302lu170oa [DOI] [PubMed] [Google Scholar]
- 53.Schmader K, George LK, Newton R, et al. The accuracy of self-report of herpes zoster. J Clin Epidemiol 1994;47:1271–6. 10.1016/0895-4356(94)90132-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.