Abstract
Background:
With an increase in the treatment options available for massive rotator cuff tears, understanding the long-term outcomes of the chosen modality is important.
Questions/Purpose:
The purpose of this study was to systematically review the available literature on repair of massive rotator cuff repairs and learn the longevity of outcomes, the failure rate, outcomes after failure, and any contributing factors to poor outcomes or failure.
Methods:
We conducted a systematic review of the MEDLINE, Cochrane, and Embase databases to find studies that investigated the long-term results of repair of massive rotator cuff repairs. Studies were excluded if they did not stratify results of massive tears, provide a definition for a massive rotator cuff tear, or report isolate patients with long-term follow-up.
Results:
Six studies met the inclusion criteria, for a total of 472 shoulders; average patient age was 57.6 years. Follow-up ranged from 119 to 240 months. Outcome scores improved significantly following repair and were maintained throughout follow-up. The repair failure rate across studies was 39.2%. Patients who suffered retear had significantly worse outcome scores than patients with intact tendons at long-term follow-up.
Conclusions:
The existing literature on long-term follow-up after massive rotator cuff repair is scarce and not of high level of evidence. This review found repair of massive rotator cuff tears leads to long-term maintained improvements in outcome measures. Failure of repair is quite common, but results following failure are superior to preoperative outcomes.
Keywords: rotator cuff repair, massive rotator cuff, reverse total shoulder arthroplasty, repair failure, retear rate, long-term outcomes
Introduction
Rotator cuff tears are the most common shoulder pathology to cause disability and constitute a major portion of orthopedic care [6]. Rotator cuff tears account for nearly 4.5 million physician visits annually, and 54% of patients above the age of 60 years have a tear apparent on imaging [31]. Massive rotator cuff tears (MRCTs) make up 20% of all rotator cuff tears and 80% of all recurrent tears [5,32]. These tears are classically defined as over 5 cm in the coronal plane or a tear that compromises 2 or more tendons of the rotator cuff [8,16].
Massive rotator cuff tears present a treatment challenge as there are multiple treatment modalities available including shoulder replacement [36], partial [3] or complete [15,26] repair, tendon transfer [7], graft augmentation [24], or debridement alone [3]. Reverse total shoulder arthroplasty has gained popularity due to the fear of poor outcomes and primary repair failure when treating MRCT [1,13,23,40]. However, these studies did not take into account the long-term results of primary repair, an especially important consideration with a younger patient population. Reverse total shoulder replacements in younger patients can lead to reduced range of motion, potential need for revision, and a significant impact on normal activities.
To evaluate the long-term outcomes of primary repair of MRCTs, we aimed to systematically review the literature to learn the longevity of outcomes, the rupture rate, outcomes after rupture, and any contributing factors to poor outcomes or failure. We hypothesize that the failure rate, while high, would not be shown necessarily to prognosticate poor outcomes.
Methods
This systematic review was performed on the published outcomes of MRCT repair with a minimum of 10-year follow-up while following the Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement (http://www.prisma-statement.org/).
With the assistance of a medical librarian a comprehensive search of online databases was conducted on July 13, 2020, which included PubMed, Cochrane, and EMBASE databases. The key terms included for the PubMed search query were as follows: “Rotator Cuff Injuries”[Mesh] OR “Rotator Cuff/surgery”[Mesh] OR “Rotator Cuff Tear Arthropathy”[Mesh] OR “Rotator Cuff Tear Arthropathy/surgery”[Mesh] OR massive cuff tear arthropathy[tiab] OR massive rotator cuff tear injuries[tiab] OR massive rotator cuff tear*[tiab] OR massive cuff tear*[tiab]. Full search criteria for the 3 databases ares available in the Supplemental Appendix. This search yielded a total of 5114 results across the PubMed, Cochrane, and Embase databases.
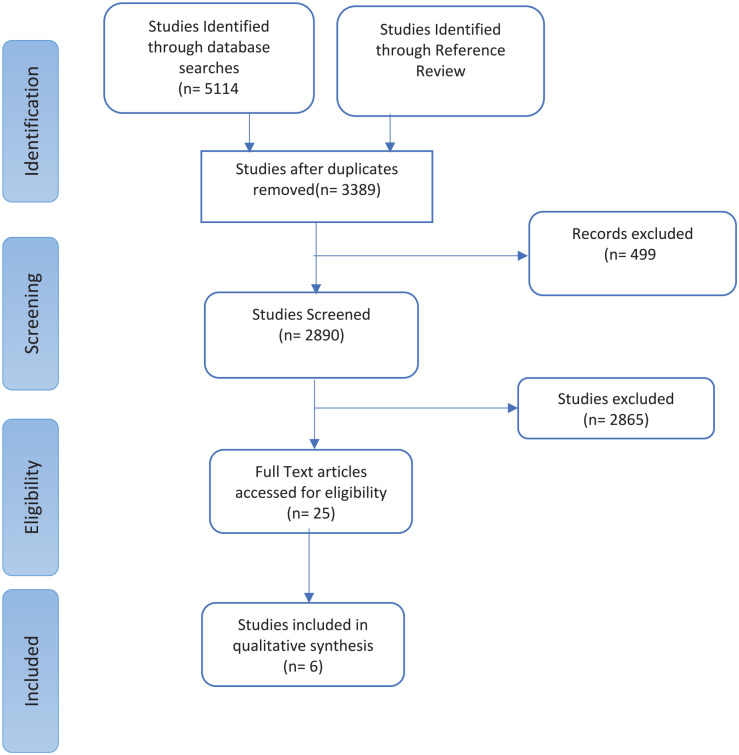
After the search was initially performed, the titles of the articles were read to eliminate duplicates. The remaining 3389 articles were screened for articles with follow-up of less than 10 years, articles without English translation available, containing less than level IV evidence, case reports, literature reviews, editorials, and abstracts without full-text availability. Following the exclusion of 499 articles, the remaining titles and abstracts were reviewed by 2 independent authors (E.S.P., Y.U.). Inclusion criteria included articles that reported outcomes of patients being treated for an MRCT. Exclusion criteria included articles that reported less than 10-year follow-up and articles that did not contain details about MRCT. Any differences were resolved through discussion. The remaining studies were further screened to eliminate those that did not report results of primary rotator cuff tear or did not stratify results to isolate massive tear repair results. A total of 25 studies from the primary literature search and zero from a secondary literature search were selected for full-text review (Fig. 1).
Fig. 1.
PRISMA flow diagram for study selection. PRISMA Preferred Reporting Items for Systematic Reviews and Meta-analyses.
The following demographic data were extracted: first author, year of publication, level of evidence, type of study, initial population size, number available for end point of follow-up, number of patients who suffered repair failure, patient report outcome measures (PROMs), and fatty infiltration. Multiple validated PROMs were extracted from the studies including the total Constant Score, the Simple Shoulder Test (SST), the Subjective Shoulder Value (SSV), American Shoulder and Elbow Society (ASES) score, and the Disabilities of the Arm, Shoulder and Hand (DASH) [2,11,17,18,30]. A subjective evaluation of outcomes was performed and described below. Included studies were evaluated for bias using the validated MINORS (methodological index for non-randomized studies) criteria by 2 authors (E.S.P and Y.U.) [38]. Discrepancies in scoring were resolved through discussion. All included studies scored at least 75%.
To determine the average follow-up and age of included patients, retear rate and reoperation rate data were pooled across the studies. Due to study design, there was potential for inclusion of studies that are heterogeneous in clinical and methodological quality. Therefore, we quantitatively explored the heterogeneity through Cochrane Q and I2 values. Cochrane Q was less than the critical χ2 value (35.17), and thus suggested that there is homogeneity in the effect sizes of the included studies. I2 values for variables of interest were also negative, which by convention is expressed as low heterogeneity, and confirmed the Cochrane Q value.
Results
Twenty-five studies were identified, with 19 not meeting the full inclusion criteria, leaving 6 for inclusion in this review (Fig. 1). The most common reasons for exclusion were lack of long-term follow-up, lack of subgroup analysis to isolate results of MRCTs, and lack of inclusion of definition of MRCT. Two of the included studies were of level III evidence [25,28] and 4 were of level IV evidence [9,10,33,47]. All studies performed complete rotator cuff repair and no studies performed partial repair. Studies mixed open, mini-open, and arthroscopic approaches. In addition, results of adjunctively performed biceps pathology treatment or acromioplasty were not reported. There were a total of 472 shoulders that underwent primary repair of rotator cuff tears, with 336 massive tears that were available for long-term follow-up and thus included in this review (Table 1). The range of sample size was from 7 to 130, with an average age of 57.6 years. Weighted average of follow-up was 139.4 (range: 119–240 months). A massive rotator tear was defined as 5 cm or more by one study [28] and by 2 torn tendons in the 5 other studies [9,10,25,33,47].
Table 1.
Characteristics of included studies.
| Study | Total rotator cuff tears | Massive tear definition | Massive tears, N | Study type | LOE | % male | Age, y | Follow-up, mo | MINORS criteria, % |
|---|---|---|---|---|---|---|---|---|---|
| Collin et al [10] | 130 | 2 tendon | 130 | Case Series | IV | 68 | 56.1 (26–79) | 120 | 81 |
| Paxton et al [33] | 15 | 2 tendon | 15 | Case Series | IV | 67 | 74.6 (63–90) | 127 | 75 |
| Collin et al [9] | 53 | 2 tendon | 53 | Case Series | IV | 64 | 54 (33–73) | 240 | 88 |
| Matsuba et al [28] | 86 | >5 cm | 7 | Retrospective Cohort | III | 53 | 60.4 ± 7.3 | 133 | 88 |
| König et al [25] | 165 | 2 tendon | 108 | Retrospective Cohort | III | 60 | 57.5 (45–74) | 120 | 83 |
| Zumstein et al [47] | 23 | 2 tendon | 23 | Case Series | IV | 65 | 54 (42–67) | 119 | 94 |
Massive tear definition refers to how massive rotator cuff tears were defined in each study.
MINORS methodological index for non-randomized studies, LOE level of evidence.
Four studies reported outcome scores preoperatively and at long-term follow-up [9,10,33,47], and 3 provided outcome scores at medium-term follow-up for the same cohort of patients [25,33,47] (Table 2). Three studies reported significantly higher total Constant scores at 10-year follow-up compared with preoperative (P < .05) [9,10,47]. One study that investigated long-term outcomes of repair failure reported significantly higher ASES scores and lower visual analog scale (VAS) pain scores at 10-year follow-up (P < .05) [33]. König et al reported ASES, DASH, and Constant scores at a follow-up of 60 to 72 months and 108 to 120 months; they reported no significance between the 2 time points for all scores [25]. Similarly, a study that evaluated results preoperatively and at 3.1 and 9.9 years after surgery found no differences between total Constant scores and SSV at the 2 time points. The same finding was true regardless of tear integrity with ASES and VAS having no significant differences between short-term follow-up and long-term follow-up in patients with ultrasound confirmed rotator cuff repair failure [33].
Table 2.
Outcome scores reported at different points in follow-up.
| Study | Variable | Preoperative | Short term (2–3 years) | Medium term (5–7 years) | Long term (9–10 years) |
|---|---|---|---|---|---|
| König et al [25] | ASES | — | 23.3 ± 3.3 | 24.3 ± 1.7 | 21.7 ± 0.5 |
| Constant Score | — | 66.6 ± 13.6 | 68.3±5.2 | 60.7±2.6 | |
| DASH | — | 22.3 ± 11.0 | 24.3 ± 10.1 | 25.0 ± 1.4 | |
| Paxton et al [33] | VAS Pain | 5.2 | 2.3 | — | 2.2 |
| ASES | 48.3 | 79.9 | — | 79.4 | |
| Constant Score | — | — | — | 65.3 | |
| SST | — | — | — | 9.2 | |
| Zumstein et al [47] | Constant Score | 51 | 70 | — | 71 |
| SSV | — | 80 | — | 82 | |
| Collin et al [10] | Constant Score | 53.1 ± 15.9 | — | — | 78.5 ± 11.3 |
| Collin et al [9] | Constant Score | 44.5 ± 15.3 | — | — | 68 ± 17.7 |
ASES American Shoulder and Elbow Society, DASH Disabilities of the Arm, Shoulder and Hand, SST Simple Shoulder Test, SSV Subjective Shoulder Value, VAS visual analog scale.
Complications following repair were not consistently reported. One study reported that 10 patients had postoperative stiffness and 4 had infections [10]. Another study reported that 4 patients developed stiffness and 2 patients had a complication labeled as “other” [9].
Repair failure at long-term follow-up was evaluated using magnetic resonance imaging in 4 studies [10,28,47] and ultrasound in 1 study [33] (Table 3). All studies used validated methods of assessing cuff integrity [27,32,35,42,46]. Four studies reported rate of tear failure [9,10,28,47]. The pooled rate of repair failure was 39.2% (68/168) (Table 2); 48.4% (34/68) of patients had reoperation after their repair failure.
Table 3.
The number of patients who suffered repair failure in each study.
| Study | N | Failure | Reoperation | Diagnosis | Definition |
|---|---|---|---|---|---|
| Collin et al [10] | 130 | 32/102 (31%) | 19 (59.4%) a | MRI | Sugaya IV/V |
| Paxton et al [33] | 15 | — | 2 (13.3%) | Ultrasound | Institutional |
| Collin et al [9] | 53 | 17/36 (47%) | 13 (68.4%) a | MRI | Sugaya IV/V |
| Matsuba et al [28] | 7 | 4/7 (57%) | — | MRI | Sugaya IV/V |
| König et al [25] | 165 | — | — | — | — |
| Zumstein et al [47] | 23 | 13/23 (57%) | 0 (0%) | MRI | MRI Grading |
Four studies reported outcome scores at long-term follow-up after repair failure [9,10,33,47] (Table 4). Total Constant scores were significantly lower in the 3 studies that compared repair integrity at long-term follow-up with those who had an intact repair [9,10,47]. Paxton et al reported a mean total Constant score of 65.3 for those who had repair failure, which was comparable with the other 2 studies [33]. Two studies reported results of the SSV, with 1 showing significantly worse results in those who suffered a failure of tear and the other showing a value that approached significance [9,47]. Two studies reported the results of SST with one showing significantly worse results in retear. The score reported by Paxton et al in patients who had failure of tear was comparable with the 1 reported in intact patients by Collin et al [9,33].
Table 4.
Outcome scores in patients who had failure of their repair at long-term follow-up.
| Collin et al [10] | Paxton et al [33] | Collin et al [9] | Zumstein et al [47] | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intact | Failure | Significance | Failure | Intact | Failure | Significance | Intact | Failure | Significance | |
| Constant Score | — | — | 0.004 | 65.3 | 75 ± 11.1 | 57.8 ± 21.2 | 0.01 | 81 | 64 | 0.02 |
| SSV Score | — | — | — | — | 79 ± 16 | 64 ± 23 | 0.03 | 89.5 | 76.5 | 0.06 |
| SST Score | — | — | — | 9.2 | 9.9 ± 2.0 | 7.3 ± 3.6 | 0.01 | — | — | — |
Paxton et al studied a cohort of patients who had repair failure.
SSV Subjective Shoulder Value, SST Simple Shoulder Test.
Fatty infiltration was reported in 4 studies [9,10,33,47]. Magnetic resonance imaging was used to assess fatty infiltration based on the criteria described by Goutallier et al and modified by Fuchs et al in all 4 of the studies [14,19]. Only 1 study reported preoperative fatty infiltration of the supraspinatus and infraspinatus and found that it had no impact on long-term outcome scores; however, only 2 patients had greater than grade 2 fatty infiltration [10]. The average Goutallier classification [19] of fatty infiltration significantly progressed in both the supraspinatus and infraspinatus according to Zumstein et al (P = .004) [47]. When the repaired tendon was intact, there was significantly less progress when compared with those with a retear (P = .004) in the supraspinatus; however, this was not significant in the infraspinatus (P = .10) [47]. Collin et al reported advanced infiltration (Goutallier III/IV) in 15 shoulders (42%) in one of their studies, concluding that postoperative fatty infiltration of the supraspinatus can be used as a predictive measure for tendon retear 20 years after operation (P < .001) [9]. One study of patients with tear failure at 2 years had a severe fatty infiltration rate of 40% (6/15) and 53.3% (8/15) for the supraspinatus and infraspinatus, respectively, at 10 years [33].
Discussion
Massive rotator cuff tears are a treatment challenge for shoulder surgeons. The surgical options for managing an MRCT include shoulder replacement [36], partial [3] or complete [15,26] repair, tendon transfer [7], graft augmentation [24], or debridement [3]. Primary repair has become a more studied treatment option for these injuries. However, these previous studies have concentrated on techniques and short-term outcomes while reporting high retear rates [15,45]. With arthroplasty gaining traction as a treatment choice for MRCT due to fears of repair failure, it is important to evaluate the long-term outcomes of repair [13]. The purpose of this review was to evaluate the available evidence on long-term outcomes and the impact of repair failure.
This systematic review has limitations. First, this study’s findings are not applicable to populations for which MRCT primary repair is not indicated. Repair is best suited for patients without evidence of arthritis, those who are not willing to undergo a joint-replacement procedure, or patients who have more labor-intensive lifestyles. Patients with associated conditions such as cuff tear arthropathy, pseudoparalysis with or without anterior-superior escape, or lower demand lifestyles are more likely to be suited for treatment with reverse shoulder arthroplasty or debridement [36]. In addition, there is a paucity of literature on the long-term outcomes of massive rotator cuff failure and an even more overwhelming lack of high-level evidence. For that reason, the articles in this study were all of level III and IV evidence. Many of the included studies did not report on all of the outcomes included in this review, leading conclusions to be drawn from 1 or 2 studies at a time. While all massive tears in this review were reported as being repaired, there was a variety of surgical approaches and concurrent procedures; it is possible that this definition varied between authors and the intervention left a defect that could constitute a partial rather than a total repair. This can be seen as a different treatment modality for the treatment of MRCT and would certainly skew comparison of results. Finally, while the definition for MRCT and fatty infiltration remained fairly constant, the integrity of the tendon was evaluated using the Sugaya criteria in 3 studies [9,10,28] and other methods in 2 studies [33,47].
Our results demonstrated that the treatment of MRCT with primary repair results in excellent outcomes at long-term follow-up. The long-term repair failure rate was 39% across 5 studies. Repair failure led to lower outcome scores, though still appreciably greater than preoperative values. The outcomes at long-term follow-up changed minimally when compared with shorter-term follow-up. Fatty infiltration below grade 3 was not predictive of decreased outcomes, but repair failure did lead to significantly increased fatty degeneration. Preoperative fatty infiltration was found to be significantly associated with repair failure at long-term follow-up [9].
A previous long-term study on patient satisfaction after MRCT repair found that 80% of patients were not satisfied at 13-year follow-up [39]. The studies included in our review indicated that outcome scores significantly improve and are maintained in the long term. The overall rate of failure seen across the included studies was 39%, and although this is still a high retear rate it is much lower than previously reported (rates as high as 79% [20]). However, this included studies that investigated repair of chronic and retracted or irreparable rotator cuff tears [34,43] and on patients who had stage 3 and stage 4 fatty degeneration [4]. It has been well established that these factors of retraction [21,41,45] along with fatty degeneration [12,29,41,45] are highly predictive of poorer outcomes. One article included in our review found a significant association of long-term repair failure in patients and fatty degeneration of the supraspinatus at the time of repair [9]. The rate seen in our study is comparable with that of some studies; Sugaya et al reported 40% for MRCTs at 36-month follow-up when excluding patients with retracted tendons and severe fatty infiltration [40].
Patients who had repair failure showed significantly lower outcome measures for the Constant score, SSV, and SST [9,10,47], indicating that the known worsening in an unhealed or retorn rotator cuff tears [37] is still apparent at long-term follow-up. When comparing these values with preoperative scores, however, there is still an improvement in VAS pain, ASES, and Constant scores [9,10,33,47]. The benefit of partial repair has been established [3,22,34,44,45], and it is likely that patients are benefiting from having the partial portion of the repair intact.
In conclusion, repair of MRCTs leads to long-term maintained improvements in outcome measures. Failure of repair is quite common, although the results following failure are still superior to preoperative outcomes. The existing literature on long-term follow-up after massive rotator cuff repair is scarce and not of high level of evidence.
Supplemental Material
Supplemental material, sj-pdf-1-hss-10.1177_15563316211008137 for Long-Term Outcomes of Massive Rotator Cuff Tear Repair: A Systematic Review by Nihar S. Shah, Emil Suriel Peguero, Yuta Umeda, Zachary T. Crawford and Brian M Grawe in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-pdf-2-hss-10.1177_15563316211008137 for Long-Term Outcomes of Massive Rotator Cuff Tear Repair: A Systematic Review by Nihar S. Shah, Emil Suriel Peguero, Yuta Umeda, Zachary T. Crawford and Brian M Grawe in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Level of Evidence: Level IV, systematic review of Level IV or higher studies.
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211–220. 10.5312/wjo.v6.i2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–146. [PubMed] [Google Scholar]
- 3. Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11(1):13–20. 10.1007/s10195-010-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Burkhart SS, Barth JRH, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(4):347–354. 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 5. Burkhart SS, Danaceau SM, Pearce CE. Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17(9):905–912. 10.1053/jars.2001.26821. [DOI] [PubMed] [Google Scholar]
- 6. Chakravarty K, Webley M. Shoulder joint movement and its relationship to disability in the elderly. J Rheumatol. 1993;20(8):1359–1361. [PubMed] [Google Scholar]
- 7. Clark NJ, Elhassan BT. The role of tendon transfers for irreparable rotator cuff tears. Curr Rev Musculoskelet Med. 2018;11(1):141–149. 10.1007/s12178-018-9468-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cofield RH. Current concepts review. Rotator cuff disease of the shoulder. J Bone Jt Surg Am. 1985;67(6):974–979. 10.2106/00004623-198567060-00024. [DOI] [PubMed] [Google Scholar]
- 9. Collin P, Betz M, Herve A, et al. Clinical and structural outcome 20 years after repair of massive rotator cuff tears. J Shoulder Elb Surg. 2020;29(3):521–526. 10.1016/j.jse.2019.07.031. [DOI] [PubMed] [Google Scholar]
- 10. Collin P, Colmar M, Thomazeau H, et al. Clinical and MRI outcomes 10 years after repair of massive posterosuperior rotator cuff tears. J Bone Jt Surg Am. 2018;100(21):1854–1863. 10.2106/JBJS.17.01190. [DOI] [PubMed] [Google Scholar]
- 11. Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. 10.1097/00003086-198701000-00023. [DOI] [PubMed] [Google Scholar]
- 12. Dwyer T, Razmjou H, Henry P, Gosselin-Fournier S, Holtby R. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):415–422. 10.1007/s00167-013-2745-z. [DOI] [PubMed] [Google Scholar]
- 13. Ernstbrunner L, Suter A, Catanzaro S, Rahm S, Gerber C. Reverse total shoulder arthroplasty for massive, irreparable rotator cuff tears before the age of 60 years: long-term results. J Bone Joint Surg Am. 2017;99(20):1721–1729. 10.2106/JBJS.17.00095. [DOI] [PubMed] [Google Scholar]
- 14. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elb Surg. 1999;8(6):599–605. 10.1016/S1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 15. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219–224. 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 16. Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 17. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elb Surg. 2007;16(6):717–721. 10.1016/j.jse.2007.02.123. [DOI] [PubMed] [Google Scholar]
- 18. Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: psychometric properties by age and injury type. J Shoulder Elb Surg. 2007;16(3):260–267. 10.1016/j.jse.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 19. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 20. Henry P, Wasserstein D, Park S, et al. Arthroscopic repair for chronic massive rotator cuff tears: a systematic review. Arthroscopy. 2015;31(12):2472–2480. 10.1016/j.arthro.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 21. Holtby R, Razmjou H. Relationship between clinical and surgical findings and reparability of large and massive rotator cuff tears: a longitudinal study. BMC Musculoskelet Disord. 2014;15:180. 10.1186/1471-2474-15-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28(6):761–768. 10.1016/j.arthro.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 23. Kluger R, Bock P, Mittlböck M, Krampla W, Engel A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med. 2011;39(10):2071–2081. 10.1177/0363546511406395. [DOI] [PubMed] [Google Scholar]
- 24. Kokubu T, Mifune Y, Inui A, Kuroda R. Arthroscopic rotator cuff repair with graft augmentation of fascia lata for large and massive tears. Arthrosc Tech. 2016;5(6):e1235–e1238. 10.1016/j.eats.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. König MA, Braunstein VA. Tendon repair leads to better long-term clinical outcome than debridement in massive rotator cuff tears. Open Orthop J. 2017;11(1):546–553. 10.2174/1874325001611010546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lo IKY, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy. 2004;20(3):250–267. 10.1016/j.arthro.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 27. Magee TH, Gaenslen ES, Seitz R, Hinson GA, Wetzel LH. MR imaging of the shoulder after surgery. Am J Roentgenol. 1997;168(4):925–928. 10.2214/ajr.168.4.9124141. [DOI] [PubMed] [Google Scholar]
- 28. Matsuba T, Hata Y, Ishigaki N, Nakamura K, Kato H. Osteoarthritis progression of the shoulder: a long-term follow-up after mini-open rotator cuff repair. J Orthop Surg. 2018;26(2):1–6. 10.1177/2309499018768106. [DOI] [PubMed] [Google Scholar]
- 29. Mellado JM, Calmet J, Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. Am J Roentgenol. 2005;184(5):1456–1463. 10.2214/ajr.184.5.01841456. [DOI] [PubMed] [Google Scholar]
- 30. Michener LA, McClure PW, Sennett BJ. American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elb Surg. 2002;11(6):587–594. 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 31. Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007;455:52–63. 10.1097/BLO.0b013e31802fc175. [DOI] [PubMed] [Google Scholar]
- 32. Owen RS, Iannotti JP, Kneeland JB, Dalinka MK, Deren JA, Oleaga L. Shoulder after surgery: MR imaging with surgical validation. Radiology. 1993;186(2):443–447. 10.1148/radiology.186.2.8421748. [DOI] [PubMed] [Google Scholar]
- 33. Paxton ES, Teefey SA, Dahiya N, Keener JD, Yamaguchi K, Galatz LM. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: minimum ten-year follow-up. J Bone Joint Surg Am. 2013;95(7):627–632. 10.2106/JBJS.L.00255. [DOI] [PubMed] [Google Scholar]
- 34. Porcellini G, Castagna A, Cesari E, Merolla G, Pellegrini A, Paladini P. Partial repair of irreparable supraspinatus tendon tears: clinical and radiographic evaluations at long-term follow-up. J Shoulder Elb Surg. 2011;20(7):1170–1177. 10.1016/j.jse.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 35. Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003;85(6):1084–1089. 10.2106/00004623-200306000-00016. [DOI] [PubMed] [Google Scholar]
- 36. Sellers TR, Abdelfattah A, Frankle MA. Massive rotator cuff tear: when to consider reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2018;11(1):131–140. 10.1007/s12178-018-9467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Slabaugh MA, Nho SJ, Grumet RC, et al. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010;26(3):393–403. 10.1016/j.arthro.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 38. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 39. Sperling JW, Cofield RH, Schleck C. Rotator cuff repair in patients fifty years of age and younger. J Bone Joint Surg Am. 2004;86(10):2212–2215. 10.2106/00004623-200410000-00012. [DOI] [PubMed] [Google Scholar]
- 40. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89(5):953–960. 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 41. Sugihara T, Nakagawa T, Tsuchiya M, Ishizuki M. Prediction of primary reparability of massive tears of the rotator cuff on preoperative magnetic resonance imaging. J Shoulder Elb Surg. 2003;12(3):222–225. 10.1016/S1058-2746(02)86888-4. [DOI] [PubMed] [Google Scholar]
- 42. Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears: comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86(4):708–716. 10.2106/00004623-20040400000007. [DOI] [PubMed] [Google Scholar]
- 43. Van Der Zwaal P, Pool LD, Hacquebord ST, Van Arkel ERA, Van Der List MPJ. Arthroscopic side-to-side repair of massive and contracted rotator cuff tears using a single uninterrupted suture: the shoestring bridge technique. Arthroscopy. 2012;28(6):754–760. 10.1016/j.arthro.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 44. Wellmann M, Lichtenberg S, Da Silva G, Magosch P, Habermeyer P. Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy. 2013;29(8):1275–1282. 10.1016/j.arthro.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 45. Yoo JC, Ahn JH, Koh KH, Lim KS. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009;25(10):1093–1100. 10.1016/j.arthro.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 46. Yoshida M, Collin P, Josseaume T, et al. Post-operative rotator cuff integrity, based on Sugaya’s classification, can reflect abduction muscle strength of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):161–168. 10.1007/s00167-017-4608-5. [DOI] [PubMed] [Google Scholar]
- 47. Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90(11):2423–2431. 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-hss-10.1177_15563316211008137 for Long-Term Outcomes of Massive Rotator Cuff Tear Repair: A Systematic Review by Nihar S. Shah, Emil Suriel Peguero, Yuta Umeda, Zachary T. Crawford and Brian M Grawe in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-pdf-2-hss-10.1177_15563316211008137 for Long-Term Outcomes of Massive Rotator Cuff Tear Repair: A Systematic Review by Nihar S. Shah, Emil Suriel Peguero, Yuta Umeda, Zachary T. Crawford and Brian M Grawe in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery