Abstract
Background: An increasing number of lumbar spine conditions are treated surgically. Such intervention, however, is commonly thought to be more effective in addressing leg pain than low back pain. Patient expectations may also contribute to self-reported surgical outcomes. Questions/Purposes: We sought to compare the expectations of patients in 2 groups undergoing lumbar spine surgery: those with predominantly low back pain and those with predominantly leg pain. We also sought to evaluate how these expectations were fulfilled for each group. Methods: We carried out a retrospective analysis of prospectively collected data from a prior study in which patients scheduled for lumbar spine surgery at a single institution completed validated surveys preoperatively and at 2 years postoperatively, including a 20-item survey on expectations for lumbar spine surgery. The patients were enrolled in the study between February 2010 and August 2012, and were divided into 2 cohorts: a “Back > Leg” group that consisted of patients with back pain that was isolated or greater than leg pain, and a “Leg ≥ Back” group that consisted of patients with leg pain that equaled or exceeded back pain. The primary analysis compared composite expectation scores (range, 0–100) between groups. Results: A total of 366 patients were deemed eligible for the study; of these, 162 patients were allocated to the Back > Leg group and 204 patients were allocated to the Leg ≥ Back group. Patients in the Leg ≥ Back group had a greater mean preoperative expectation score compared with those in the Back > Leg group. Multivariate analysis demonstrated that higher preoperative expectations were associated with leg pain symptoms after controlling for disease diagnosis. Both groups reported similar proportions of fulfilled expectations. Conclusion: Patients with predominantly leg pain hold greater preoperative expectations for lumbar spine surgery than do patients with predominantly back pain. That these patient groups reported similar fulfillment of their expectations at 2 years postoperatively illustrates the greater clinical outcomes achieved among patients who presented with predominantly leg pain.
Keywords: patient expectations, lumbar spine surgery, low back pain, leg pain, patient-reported outcomes
Introduction
Pathologies of the lumbar spine can manifest as incapacitating low back and/or leg pain with all-encompassing debilitations in patients’ quality of life. Patients entering a spine clinic with low back pain and associated leg pain are more likely to be female and of an older age than those with isolated low back pain [10]. Patients with low back pain associated with radiating leg pain have increased disability, worse quality of life, and use more health care resources compared with patients with isolated low back pain [6,11,12]. Advancements in diagnostic and treatment technologies have expanded the role of surgery to address a variety of lumbar spine conditions [9,20]. Surgical interventions are commonly thought to more reliably address leg pain symptoms than low back pain.
The elective nature of many lumbar spine procedures requires surgeons to appreciate patients’ knowledge, attitudes, and expectations of surgical treatment. Patients derive their preoperative expectations for lumbar spine surgery from diverse sources, including prior experiences receiving treatment, interactions with the treating surgeon, and a variety of self-sought online information [16]. Furthermore, clinical and demographic differences also account for discrepancies in patients’ expectations [18]. In fact, although complex, patients’ expectations are increasingly recognized as an important and potentially modifiable component to patient-reported surgical outcomes [13].
Despite demographic and clinical differences between patients with predominantly leg pain and those with predominantly back pain, the relative expectations of lumbar spine surgery across these groups are heretofore unknown. We hypothesized that, among patients indicated for lumbar spine surgery, those with leg pain greater than or equal to low back pain have higher preoperative expectations than those with predominantly low back pain. The purpose of the present analysis was to compare patient expectations prior to lumbar spine surgery between patients with predominantly low back pain and those with equal or greater leg pain and, secondarily, to evaluate how patients’ expectations were fulfilled in each patient group.
Methods
Approval from the institutional review board was obtained prior to performing the study. The current analysis uses data from a prospective study that has characterized a large series of patient expectations for lumbar spine surgery [13–18]. We conducted a secondary retrospective analysis on the prospectively collected data.
Patients were recruited from the clinical practices of 4 fellowship-trained spine surgeons at our institution. English-speaking patients at least 18 years of age and without cognitive deficit who were indicated for lumbar spine surgery were deemed eligible. Two groups were established based on participants’ preoperative self-assessments of their back pain and leg pain, which was defined by a 10-point numerical rating score. The “Back > Leg” group consisted of patients with back pain only or with back pain rated more severe than leg pain. The “Leg ≥ Back” group consisted of patients with leg pain equal to or exceeding back pain. Patients who rated their leg pain equal to their back pain were deemed to have clinically relevant leg pain and were therefore included in the Leg ≥ Back group.
At enrollment, all patients completed assessments of demographic and clinical characteristics. They also reported their expectations of surgery with the Hospital for Special Surgery Lumbar Spine Surgery Expectations Survey, a validated instrument providing a comprehensive assessment of patients’ preoperative expectations for pain relief, functional abilities, capacity for employment, and psychological well-being [13,18]. The development, validation, and a detailed description of this novel instrument has been described [13,15,17,18]. In brief, patients’ responses to a series of 20 items generate a composite score between 0 and 100, with a higher score reflecting greater overall expectations.
Patients also were screened for depressive symptoms using the Geriatric Depression Scale (GDS), a validated 30-item survey in which a score of ≥11 indicates a positive screening for depressive symptoms [22]. The State-Trait Anxiety Inventory (STAI) was also used as a validated instrument for assessing general anxiety [21]. Interpreting results from the STAI consisted of comparing population norms with composite scores between 20 and 80. Both instruments have been used previously to characterize patients undergoing lumbar spine surgery [17].
Clinical characteristics were recorded, including symptom duration, opioid use, the presence and type of prior treatment modalities, major comorbidity, and physical examination findings. To assess the severity of patients’ preoperative lumbar spine symptoms, participants completed a modified version of the Oswestry Disability Index (ODI). From this 10-item instrument, a score was calculated between 0 and 100, with higher scores indicative of greater disability [4,8]. Patients also completed assessment of back and leg pain severity according to numerical rating scale, ranging from 0 to 10, higher meaning more pain. Major comorbidity was assessed via the Charlson Comorbidity Index (CCI), a validated summary comorbidity measure that assigns points based on conditions associated with increased 1-year mortality, such as diabetes mellitus and congestive heart failure [2,3].
A senior spine surgeon blinded to all patients’ survey data provided a specific lumbar spine diagnosis based on the review of presenting symptoms, physical exam, and available imaging. Diagnoses were grouped as an acute condition (ie, herniated nucleus pulposus) or a degenerative condition (ie, spondylolisthesis, stenosis, degenerative disc disease).
Approximately 2 years following lumbar spine surgery, patients again completed several survey instruments, including the numerical rating scales for back and leg pain, as well as the ODI. To avoid biasing subsequent responses, patients were not provided with their preoperative survey responses. Patients were asked how much improvement they received for items they cited preoperatively on the Expectations Survey, with response options ranging from “no improvement at all” (0 points) to “back to normal or complete improvement” (4 points). A proportion of expectations fulfilled (described below) was then calculated. Patients were also asked to report any complications from their lumbar spine surgery, additional surgeries performed, and additional spine pathologies.
Back and leg groups were compared according to baseline demographic and clinical characteristics, and associations among variables were ascertained to identify potential covariates. Data were assessed for normality with univariate analyses for distributions, means, medians, and interquartile ranges, and then by confirming symmetry in residual plots. Expectations Survey scores were compared between groups with a t-test and then assessed in a linear regression model with scores as the dependent variable and group as the independent variable, controlling for acute versus degenerative diagnosis.
Additional properties of the survey were ascertained with factor analysis to determine whether items clustered based on response patterns or covariance structures. Using principal components analysis and varimax rotation, 4 domains (ie, factors) were discerned: daily function (6 items), personal function (6 items), psychosocial well-being (4 items), and skeletal function (2 items). Two items were not included, 1 about pain because it did not cluster to any specific domain and 1 about employment because it was not applicable to most patients.
In addition to the overall Expectations Survey score, additional scores were calculated for the 4 domains ascertained by factor analysis. The domain scores similarly were scored to range from 0 to 100, with higher scores reflecting greater expectations.
From postoperative data, a proportion of expectations fulfilled was calculated as the ratio of summed total points from the postoperative assessment (ie, reflecting amount of improvement received) divided by the summed total points from the preoperative assessment (ie, reflecting amount of improvement expected). Proportions ranged from 0 (no expectations fulfilled) to greater than 1 (expectations surpassed). To compare preoperative and postoperative values, the sample was also stratified into tiers based on preoperative and postoperative total points ranging from 0 to 50, 51 to 75, and 76 to 100, and percentages in each tier were calculated for both groups. This stratification was performed to depict the 3-way association of percentage of patients, preoperative score, and postoperative score. Additional outcomes were within-patient preoperative to postoperative change in ODI scores, and changes in back and leg pain were based on numerical rating scale values.
Results
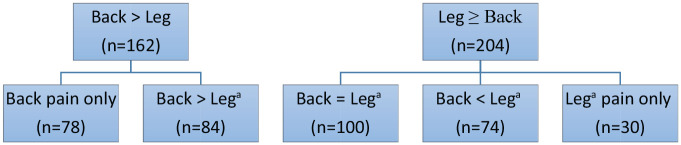
Of the 420 patients who enrolled between February 2010 and August 2012, 366 patients remained eligible and completed follow-up surveys. As previously reported, patients who did not complete follow-up surveys were similar to the final study population with respect to baseline depressive and anxiety scores, age, gender, diagnosis, and comorbidities [17]. The Back > Leg group comprised 162 patients, including 78 patients who reported isolated back pain and 84 patients who reported back pain that was more severe than leg pain. The Leg ≥ Back group comprised 204 patients, including 30 patients with leg pain only, 74 patients with leg pain worse than back pain, and 100 patients with leg pain equal to their back pain (Fig. 1).
Fig. 1.
Assignment of patient groups. aPain from more severely affected leg.
Baseline demographics and psychosocial characteristics were similar between groups (Table 1). Groups were similar with respect to several clinical characteristics, including prior spine surgery, ODI scores, and prior nonoperative treatment modalities (Table 2). Based on our group definitions, patients in the Back > Leg group had greater back pain than leg pain (P < .001), whereas patients in the Leg ≥ Back group had greater leg pain than back pain (P < .001). A higher percentage of patients in the Back > Leg group had a degenerative diagnosis (85% vs 73%, P < .008) as well as a higher percentage of symptom duration of more than 12 months (57% vs 465%, P = .03). Leg ≥ Back had a higher percentage of patients with abnormalities on physical exam. A greater percentage of patients in this group were unable to perform a heel walk (32% vs 18%, P = .05), had decreased quadriceps strength (15% vs 5%, P = .004), and decreased hamstring strength (13% vs 5%, P = .008) compared with patients with predominantly back pain.
Table 1.
Preoperative demographic and psychosocial characteristics.
| Characteristic | Back pain > leg pain (n = 162) | Leg pain ≥ back pain (n = 204) | P |
|---|---|---|---|
| Mean age (years) | 54 | 57 | .12 |
| Men | 59% | 56% | .52 |
| College graduate | 56% | 62% | .20 |
| Currently employed | 44% | 45% | .90 |
| Positive screen for depression a | 42% | 39% | .59 |
| Anxiety greater than population norms b | 61% | 59% | .75 |
| Any major comorbidity | 27% | 27% | .97 |
| Current smoker | 14% | 8% | .07 |
| Ever smoked | 43% | 34% | .07 |
As indicated by a score ≥11 on Geriatric Depression Scale.
Based on State-Trait Anxiety Inventory score in comparison with age- and gender-based population norms.
Table 2.
Preoperative clinical characteristics.
| Characteristic | Back pain > leg pain (n = 162) | Leg pain ≥ back pain (n = 204) | P |
|---|---|---|---|
| Back pain rating a | 7.2 | 5.2 | <.0001 |
| Leg pain rating a | 2.7 | 7.1 | <.0001 |
| Degenerative diagnosis | 85% | 73% | <.008 |
| Vertebral levels involved | |||
| <3 | 74% | 68% | .23 |
| ≥3 | 26% | 32% | |
| Currently taking opioids | 44% | 39% | .31 |
| Prior treatments | |||
| Epidural injection | 74% | 74% | .91 |
| Physical therapy | 57% | 62% | .29 |
| Acupuncture | 15% | 13% | .57 |
| Chiropractic care | 27% | 33% | .24 |
| Symptoms > 12 months | 57% | 46% | .03 |
| Oswestry Disability Index score, mean b | 55 | 56 | .46 |
| Prior spine surgery | 46% | 39% | .21 |
| Physical exam abnormal | |||
| Heel walk | 18% | 32% | .005 |
| Toe walk | 13% | 22% | .05 |
| List | 12% | 7% | .17 |
| Flexion | 76% | 57% | .001 |
| Extension | 83% | 71% | .03 |
| Straight leg raise | 31% | 35% | .48 |
| Contralateral straight leg raise | 6% | 9% | .51 |
| Gait | 27% | 37% | .06 |
| Balance | 17% | 12% | .35 |
| Patellar reflex | 18% | 25% | .16 |
| Achilles reflex | 40% | 45% | .35 |
| Lower extremity sensation | 25% | 31% | .24 |
| Quadriceps strength | 5% | 15% | .004 |
| Hamstring strength | 5% | 13% | .008 |
| Hallucis strength | 16% | 23% | .13 |
Possible range 0–10, higher is more pain.
Possible range 0–100, higher is more disability.
Finally, Leg ≥ Back patients had a greater mean preoperative Expectations Survey score compared with those with predominantly back pain (74 vs. 69, P = .02). Given that the group with predominantly leg pain had a higher percentage of patients with an acute spine condition, diagnosis was controlled for in further analysis. In a multivariate model with Expectations Survey score as the dependent variable, leg pain remained associated, controlling for diagnosis (Table 3). The difference in overall Expectations Survey scores between the 2 groups was driven mostly by the physical function and skeletal domains (Table 4). The items for the physical function domain address walking, standing, climbing stairs, exercising, stopping the condition from getting worse, and removing the control my spine condition has on my life. The items for the skeletal domain address regaining strength in legs and improving balance.
Table 3.
Expectations Survey score as a dependent variable in bivariate and multivariate analyses for leg pain ≥ back pain and acute diagnosis.
| Independent variables | Bivariate |
Multivariate |
||
|---|---|---|---|---|
| Estimate | P | Estimate | P | |
| Leg pain ≥ back pain | 4.8 | .02 | 4.1 | .05 |
| Acute spine diagnosis | 6.8 | .006 | 6.1 | .01 |
Group and acute spine diagnosis: Spearman’s correlation = .14 (P = .008).
Table 4.
Overall and domain scores for the Expectations Survey.
| Domains | Back pain > leg pain (n =162) | Leg pain ≥ back pain (n = 204) | P |
|---|---|---|---|
| Overall | 69 ± 19 | 74 ± 20 | .02 |
| Personal function | 62 ± 27 | 66 ± 28 | .14 |
| Physical function | 77 ± 19 | 82 ± 19 | .007 |
| Psychological well-being | 72 ± 23 | 77 ± 25 | .05 |
| Skeletal function | 63 ± 34 | 72 ± 30 | .007 |
The proportion of expectations fulfilled was .68 (range, 0–1.64) for Back > Leg and .65 (range, 0–2.00) for Leg ≥ Back (Table 5). Thus, because patients in Leg ≥ Back had a similar proportion of expectations fulfilled despite having greater preoperative expectations, they derived greater improvement than Back > Leg. This distinction is particularly noted when the 2 groups were compared for preoperative and postoperative total survey points (Fig. 2).
Table 5.
Postoperative outcomes.
| Characteristic | Back pain > leg pain (n = 162) | Leg pain ≥ back pain (n = 204) | P |
|---|---|---|---|
| Change in back pain a | 4.0 b | 2.5 | <.0001 |
| Change in leg pain c | 1.3 | 5.2 b | <.0001 |
| Change in disability | 0.30 | 0.32 | .50 |
| Proportion of expectations fulfilled | 0.68 | 0.65 | .44 |
ODI Oswestry Disability Index.
Based on mean within patient change in preoperative to postoperative numerical rating of pain.
P = .002 comparison of change in pain according to group.
Based on mean within patient change in preoperative to postoperative ODI score.
Fig. 2.
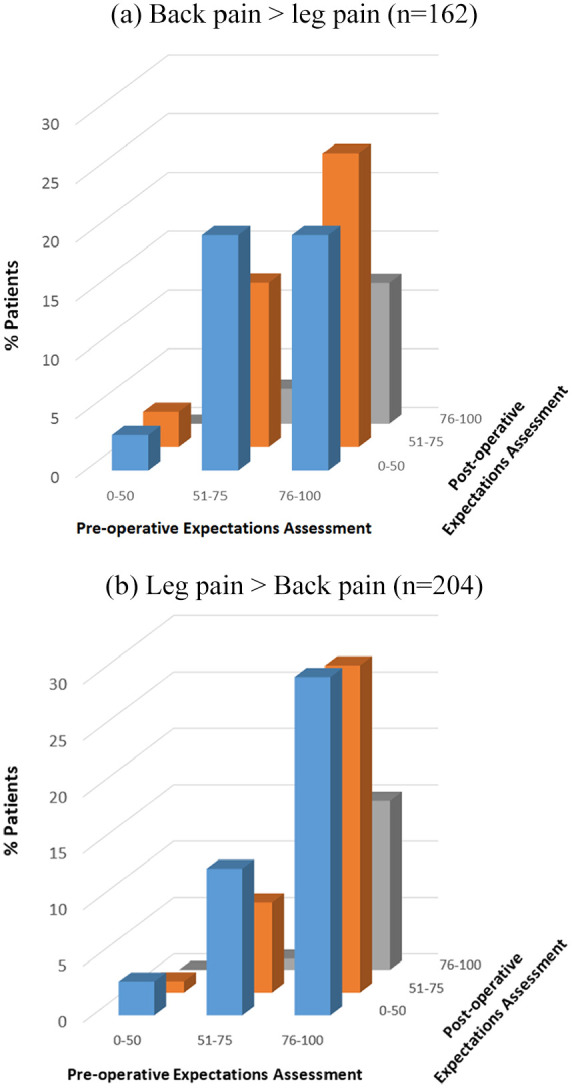
(a) Three-dimensional plot of preoperative expectations versus postoperative fulfillment of expectations for patients with predominantly back pain. Data stratified based on 3 tiers of preoperative and postoperative assessments. (b) In comparison, greater percentages of patients with predominantly leg pain had higher expectations.
At the postoperative evaluation, pain improved in both groups. The mean improvement in back pain was greater in the Back > Leg group, whereas the mean improvement in leg pain was greater among patients who presented with predominantly leg pain (Table 5). When the groups were compared, patients with predominantly leg pain had greater pain improvement than patients with predominantly back pain. There were no differences in change in preoperative to postoperative ODI scores between groups.
Discussion
The findings of the present analysis demonstrate that patients with predominantly leg pain undergoing lumbar spine surgery have greater preoperative expectations than do patients with predominantly back pain. Patients with primarily leg pain reported more benefit from surgery because they had greater preoperative expectations but not less fulfillment of expectations postoperatively. The study’s results are supported by its application of a validated instrument for evaluating patients’ expectations and fulfillment of expectations, a relatively large sample size, and 2-year follow-up data.
Patients with primarily leg pain reported a mean 5-point increase in preoperative expectations in the Hospital for Special Surgery Lumbar Spine Surgery Expectations Survey. Beyond its statistical significance, this corresponds to a 1-level difference in approximately 20% of a survey previously validated in multiple domains, including symptoms, physical function, and emotional well-being. Thus, the higher mean Expectations Survey score among patients with primarily leg pain indicates a greater breadth and amount of improvement expected compared with those patients with leg and back pain. Patients in the Leg ≥ Back group expected more improvement for all 20 items of the Expectations Survey. They were particularly more likely to expect more improvement for pain, walking, standing, regain strength in legs, activities of daily living, personal care, and exercise (P < .05). However, the strength of the Expectations Survey is in its composite value and not the performance of individual questions and associations with outcome. Given the likelihood of finding an association by chance due to multiple comparisons, we did not report scores on specific components of preoperative expectations. A much larger sample would be required if individual questions were required to stand alone as independent outcomes.
A key finding from our study was that multivariate analysis demonstrated that higher preoperative expectations were associated with leg pain symptoms even after controlling for the higher percentage of acute spine conditions present within this group. The presenting symptom of clinically meaningful leg pain, therefore, functions as more than a proxy for an underlying diagnosis. This finding may be especially helpful for surgeons in the earliest stages of a clinical encounter. In a patient’s first visit, when advanced imaging is not yet available and a definitive diagnosis has not been reached, the patient’s presenting symptoms and relative pain contributors are among the first pieces of clinical information the surgeon obtains and may therefore assist in early patient education efforts.
Our study identified that expectations pertaining to physical function (eg, walking, climbing stairs) and skeletal function (eg, leg strength and balance) were the domains that drove the meaningful difference in preoperative expectations between groups. This is consistent with our clinical experience, in which patients with primarily leg pain are more likely to derive such benefits from surgical intervention. In contrast, patients in both groups are more likely to expect similar improvement in psychological well-being and personal function.
After identifying differences in patients’ expectations for surgery, the logical next questions becomes, “Is the difference in expectations between groups warranted?” Our study demonstrates that both groups may have unjustifiably high expectations. However, at 2 years’ follow-up, despite higher initial expectations, patients with leg pain greater than or equal to back pain had a similar proportion of expectations fulfilled compared with the patients with predominantly back pain. Thus, both groups had similar fulfillment of expectations even though patients with predominantly leg pain set a higher bar for success. This finding is concordant with our clinical experience, which suggests that leg pain is often more amenable to surgical treatment. Whereas leg pain can frequently be attributable to a defined structural abnormality of the lumbar spine, the etiology of back pain is frequently multifactorial. It is critical to note that our study relies on patients’ direct feedback via the Expectations Survey to assess functional improvement, rather than the change in level of disability, as measured by the ODI.
This analysis builds upon recent work that has expanded our understanding of patients’ expectations prior to lumbar surgery. Younger patient age, worse ODI score, and worse mental health score have all been previously associated with a higher composite score on the Expectations Survey [18]. More than half of patients develop their preoperative expectations from information obtained from the Internet, while nearly 1 in 5 patients do not base their expectations exclusively from their treating surgeon [16]. Together, these data suggest room to actively increase engagement with patients, and address modifiable components of patients’ expectations. Such work at addressing patients’ attitudes in the perioperative setting is underway. Goz et al [5] used a mobile phone messaging tool to decrease patient anxiety following spine surgery. A preoperative educational class has been shown to modify patients’ expectations of their recovery time from total joint arthroplasty [19]. Improved understanding of patients’ nuanced baseline expectations and knowledge base, such as that gained from the present analysis, is critical to the success of new educational interventions.
Our study must be considered in the context of its limitations. As patients were recruited from a spine surgery clinic and indicated for lumbar spine surgery, the study’s results are not generalizable to a primary care setting in which the majority of patients are treated nonoperatively. To establish 2 patient cohorts for direct comparison, participants presenting with equivalent amounts of leg pain and back pain were allotted to the group with predominantly leg pain. This level of leg pain was deemed clinically substantial and therefore patients were considered to be more aligned with patients experiencing predominantly leg pain. As our study design was hypothesis-driven, we did not test a third group, in which patients with equal amounts of back pain and leg pain were assigned to the group with predominantly back pain. Finally, we did not categorize patients based on the nature of their leg pain. For example, patients in a primary care clinic with pain radiating below the knee have been demonstrated to have more severe symptoms than those with leg pain that does not radiate beyond the knee [1,7]. That all patients in our study were indicated for surgery may have diminished the heterogeneity within our study’s cohort of patients experiencing leg pain; however, future studies are needed to better characterize patients with leg pain of different quality and severity.
In conclusion, our analysis of 366 patients undergoing lumbar spine surgery demonstrated that patients whose leg pain equaled or exceeded their back pain had higher expectations than those patients with predominantly back pain, and at 2-year follow-up, both groups had similar fulfillment of their preoperative expectations. That these patient groups reported similar fulfillment of their expectations illustrates the greater clinical outcomes achieved among patients who presented with predominantly leg pain. Future interventions addressing patients’ expectations should be tailored based upon patients’ presenting symptoms.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Christopher M. Brusalis, MD, Roland Duculan, MD, and Carol A. Mancuso, MD, declare they have no conflicts of interests. Frank P. Cammisa, MD, reports relationships with Orthofix Medical, Inc; Nuvasive, Inc; Mallinckrodt Pharmaceuticals; Centinel Spine, Inc; Beatrice & Samuel A. Seaver Foundation; 4WEB Medical, Inc; 7D Surgical, Inc; Pfizer, Inc; Spine Biopharma, LLC; Vertical Spine, LLC; 4WEB Medical/4WEB, Inc; Woven Orthopedic Technologies; Orthobond Corporation; Healthpoint Capital Partners, LP; Ivy Healthcare Capital Partners, LLC; ISPH II, LLC; VBVP VI, LLC; Medical Device Partners III, LLC; Viscogliosi Brothers, LLC; and RTI Surgical, Inc, outside the submitted work. Andrew A. Sama, MD, reports relationships with Ortho Development Corp; Paradigm Spine, LLC; Spinal Kinectics; Vestia Ventures MiRus Investment; Integrity Implants; Clariance; Kuros Biosciences AG; DuPuy Spine Products & Medical Device Business Services; 4WEB, Inc; MiMedex Group; AO Spine North America; and South Carolina Spine Society, outside the submitted work. Alexander P. Hughes, MD, reports relationships with NuVasive, Inc; Mallinckrodt Pharmaceuticals; 4WEB Medical/4WEB, Inc; and Pfizer, Inc, outside the submitted work. Federico P. Girardi, MD, reports relationships with LANX, Inc; Ortho Development Corp; and Nuvasive, outside the submitted work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was waived from all patients included in this study.
Level of Evidence: Level III: retrospective comparative study with prospectively collected data
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
References
- 1. Ashworth J, Konstantinou K, Dunn KM. Prognostic factors in non-surgically treated sciatica: a systematic review. BMC Musculoskelet Disord. 2011;12:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Austin SR, Wong Y-N, Uzzo RG, Beck JR, Egleston BL. Why summary comorbidity measures such as the Charlson Comorbidity Index and Elixhauser Score work. Med Care. 2015;53:e65–e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 4. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–2952. [DOI] [PubMed] [Google Scholar]
- 5. Goz V, Anthony C, Pugely A, et al. Software-based postoperative communication with patients undergoing spine surgery. Glob Spine J. 2019;9:14–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hider SL, Whitehurst DGT, Thomas E, Foster NE. Pain location matters: the impact of leg pain on health care use, work disability and quality of life in patients with low back pain. Eur Spine J. 2015;24:444–451. [DOI] [PubMed] [Google Scholar]
- 7. Hill JC, Konstantinou K, Egbewale BE, Dunn KM, Lewis M, van der Windt D. Clinical outcomes among low back pain consulters with referred leg pain in primary care. Spine (Phila Pa 1976). 2011;36:2168–2175. [DOI] [PubMed] [Google Scholar]
- 8. Hudson-Cook N, Tomes-Nicholson K, Breen A. A revised Oswestry Disability Questionnaire. In: Roland M, Jenner JR, eds. Back Pain: New Approaches to Rehabilitation and Education. Manchester, England: Manchester University Press; 1989:187–204. [Google Scholar]
- 9. Kim CH, Chung CK, Kim MJ, et al. Increased volume of lumbar surgeries for herniated intervertebral disc disease and cost-effectiveness analysis: a nationwide cohort study. Spine (Phila Pa 1976). 2018;43:585–593. [DOI] [PubMed] [Google Scholar]
- 10. Kongsted A, Kent P, Albert H, Jensen TS, Manniche C. Patients with low back pain differ from those who also have leg pain or signs of nerve root involvement—a cross-sectional study. BMC Musculoskelet Disord. 2012;13:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Konstantinou K, Dunn KM, Ogollah R, Vogel S, Hay EM. Characteristics of patients with low back and leg pain seeking treatment in primary care: baseline results from the ATLAS cohort study. BMC Musculoskelet Disord. 2015;16:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Konstantinou K, Hider SL, Jordan JL, Lewis M, Dunn KM, Hay EM. The impact of low back-related leg pain on outcomes as compared with low back pain alone: a systematic review of the literature. Clin J Pain. 2013;29:644–654. [DOI] [PubMed] [Google Scholar]
- 13. Mancuso CA, Cammisa FP, Sama AA, Hughes AP, Ghomrawi HMK, Girardi FP. Development and testing of an Expectations Survey for patients undergoing lumbar spine surgery. J Bone Joint Surg Am. 2013;95:1793–1800. [DOI] [PubMed] [Google Scholar]
- 14. Mancuso CA, Duculan R, Cammisa FP, et al. Fulfillment of patients’ expectations of lumbar and cervical spine surgery. Spine J. 2016;16:1167–1174. [DOI] [PubMed] [Google Scholar]
- 15. Mancuso CA, Duculan R, Cammisa FP, et al. Proportion of expectations fulfilled: a new method to report patient-centered outcomes of spine surgery. Spine (Phila Pa 1976). 2016;41:963–970. [DOI] [PubMed] [Google Scholar]
- 16. Mancuso CA, Duculan R, Cammisa FP, et al. Sources of patients’ expectations of lumbar surgery. Spine (Phila Pa 1976). 2019;44:318–324. [DOI] [PubMed] [Google Scholar]
- 17. Mancuso CA, Duculan R, Cammisa FP, et al. Successful lumbar surgery results in improved psychological well-being: a longitudinal assessment of depressive and anxiety symptoms. Spine J. 2018;18:606–613. [DOI] [PubMed] [Google Scholar]
- 18. Mancuso CA, Duculan R, Stal M, Girardi FP. Patients’ expectations of lumbar spine surgery. Eur Spine J. 2015;24:2362–2369. [DOI] [PubMed] [Google Scholar]
- 19. Mancuso CA, Graziano S, Briskie LM, et al. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin Orthop Relat Res. 2008;466:424–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rajaee SS, Bae HW, Kanim LEA, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012;37:67–76. [DOI] [PubMed] [Google Scholar]
- 21. Spielberger C. State-Trait Anxiety Inventory for Adults (Form Y). Redwood City, CA: Mind Garden, Inc; 1983. [Google Scholar]
- 22. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982. –1983;17:37–49. [DOI] [PubMed] [Google Scholar]