Abstract
COPD is complex and heterogeneous with respect to its aetiology, clinical presentation, phenotypes and biological mechanisms. Despite this, COPD is still diagnosed and treated according to simple clinical measures, including airflow limitation, symptoms and exacerbation frequency, leading to failure to recognise the disease's heterogeneity and/or to provide targeted interventions. COPD continues to have a very large burden of disease with suboptimal outcomes for people with the disease, including frequent hospitalisation with exacerbations, rapid lung function decline, multimorbidity and death from respiratory failure. In light of this, there have been increasing calls for a renewed taxonomy with better characterisation of COPD phenotypes and endotypes. This would allow the unravelling of COPD's complexity and heterogeneity, the implementation of targeted interventions and improved patient outcomes. The treatable traits strategy is a proposed vehicle for the implementation of precision medicine in chronic airway diseases. In this review, in addition to summarising the key knowledge on the heterogeneity of COPD, we refer to the existing evidence pertaining to the treatable traits strategy as applied in COPD and discuss implementation in different settings.
Short abstract
COPD is a heterogeneous clinical syndrome, which requires deconstruction of its individual components to facilitate targeted treatment and improve individual patient outcomes. https://bit.ly/2YXWgHN
Educational aims
To describe COPD as a syndrome encompassing a heterogeneous group of aetiologies, clinical phenotypes and endotypes.
To introduce the treatable traits strategy as a tool for the diagnosis and management of patients with COPD, allowing implementation of precision medicine in chronic airway diseases.
To describe existing evidence on the treatable traits approach, including the most prevalent traits identified in COPD populations, traits associated with important clinical outcomes, and efficacy of the treatable traits approach in the management of COPD.
To discuss implementation of the treatable traits approach in various settings.
Introduction
COPD is a leading cause of mortality and disability globally [1]. Its estimated global prevalence reaches 13% and is projected to rise due to ongoing exposure to COPD risk factors and an ageing population [2]. COPD is associated with high personal and socioeconomic costs and represents a major global health need [1]. There is, therefore, a pressing need for improved approaches to diagnosing and managing this prevalent and costly disease. We argue that the key to improving diagnosis, management and patient outcomes in COPD is recognising its heterogeneity and complexity and departing from old “disease label” based approaches. Complexity in the context of COPD means that it has several pulmonary and extrapulmonary components with nonlinear dynamic interactions over time, and heterogeneity implies that not all those components are present in all individuals at any given time point [3]. The treatable traits strategy offers a personalised, “label-free” approach to chronic airway disease management, that recognises the disease's heterogeneity and complexity and addresses individual patient needs (figure 1).
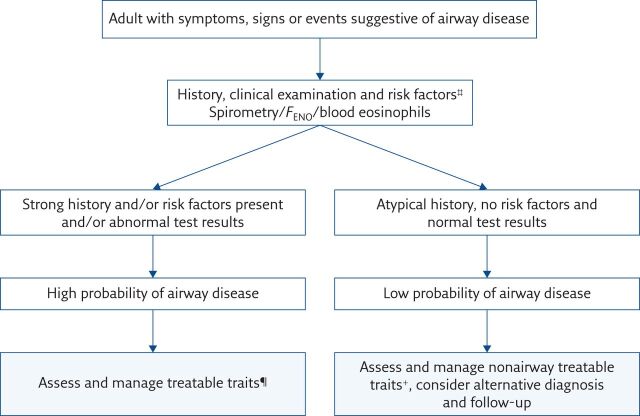
Figure 1.
Summary of the treatable traits strategy applied in clinical practice. Content has been reproduced with permission from the Centre of Excellence in Treatable Traits, originally developed as part of the Centre of Excellence in Treatable Traits (https://treatabletraits.org.au).
Increasing knowledge of the heterogeneity of the genetic makeup, aetiologies, endotypes and lung function trajectories in patients with COPD has led to calls for COPD to be redefined as a syndrome rather than a singular disease as well as the development of new diagnosis and treatment approaches [4]. Precision medicine, defined as “treatments targeted to the needs of individual patients on the basis of their genetic, biomarker, phenotypic, or psychosocial characteristics that distinguish a given patient from other patients with similar clinical presentations”, has been widely advocated as a new approach to chronic disease management [5]. The key goal of applying precision medicine to patients’ management is to improve their clinical outcomes and minimise side-effects associated with unnecessary treatments, reserving treatments for patients who are most likely to respond [5].
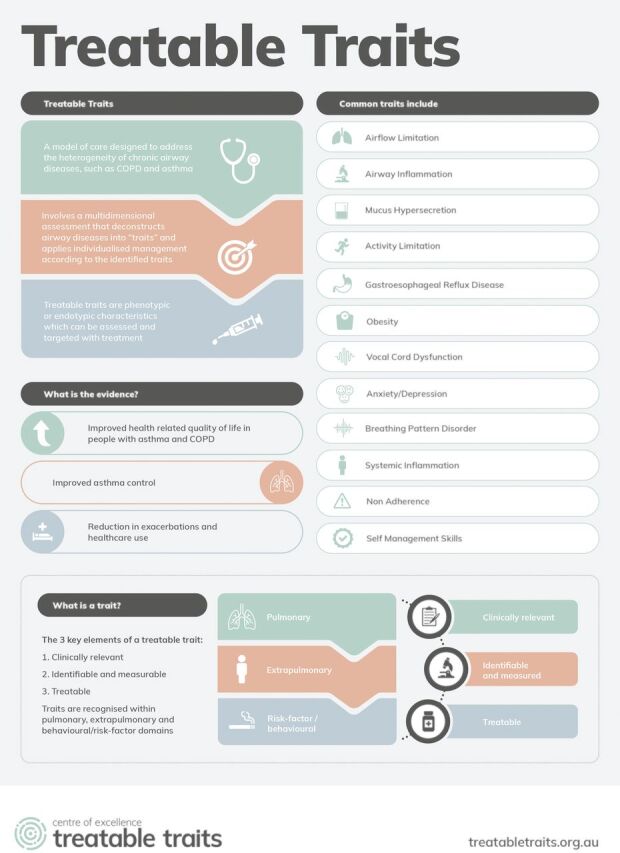
The treatable traits strategy offers hope as a vehicle for the implementation of precision medicine in chronic airway diseases, including asthma and COPD [6, 7]. This approach allows for the deconstruction of chronic airway diseases into components that are measurable, clinically significant and treatable [6]. Such an approach allows for departure from traditional disease labels, which often fail to reflect the heterogeneity, complexity and individual treatment needs of patients. The treatable traits approach utilises multidimensional assessment (MDA) of every patient with chronic airway disease to determine the core traits associated with disease outcomes, followed by the application of targeted and evidence-based treatments founded on the assessment outcome. Traits are classified under three domains: pulmonary (table 1), extrapulmonary (table 2) and behavioural/risk factors (table 3). An algorithm enabling the identification of treatable traits in patients with chronic airway disease was published by Agusti et al. [6], in 2016 (figure 2). The first step of this algorithm seeks to determine if the patient has airway disease; this is achieved through an assessment of the patient's clinical history, risk factors and exposures, and assessment of objective measures including spirometry, exhaled nitric oxide fraction (FENO) and blood eosinophils [6]. Such an assessment aims to yield a probability (high or low) of airway disease being present. High probability of airway disease is followed by an MDA of treatable traits of each individual and treatment targeted to the traits identified.
Table 1.
List of potential treatable traits within the pulmonary domain to consider in patients with chronic airway disease
| Trait | Trait identification marker/diagnostic criteria | Possible treatments | Evidence level I–IV # |
| Airway smooth muscle contraction | Bronchodilator reversibility, peak expiratory flow variability, airway hyperresponsiveness | Bronchodilators: Maintenance: LABA/LAMA; Rescue: SABA/SAMA/rapid-acting LABA |
I |
| Systemic allergic inflammation | Elevated serum IgE | Anti-IgE monoclonal antibody therapy | I |
| Dyspnoea | Dyspnoea score ≥2, modified Medical Research Council scale | Pulmonary rehabilitation, breathing retraining | I |
| Emphysema (loss of elastic recoil) | Chest CT, plethysmography, lung compliance | Smoking cessation, lung volume reduction surgery, lung transplantation, α1-antitrypsin replacement if deficient | I |
| Airway inflammation (eosinophilic) | Sputum eosinophils ≥3% and/or FENO ≥30 ppb and/or blood eosinophils ≥0.3×109 cells·L−1 | Corticosteroids, anti-IL-5, -13, -4 monoclonal antibody therapy | I-II |
| Pulmonary hypertension | Doppler echocardiography, brain natriuretic peptide, right heart catheterisation | Oxygen therapy, pulmonary vasodilator therapy, lung transplantation | I-II |
| Bronchiectasis | High-resolution chest CT | Physiotherapy, mucociliary clearance techniques, macrolides, pulmonary rehabilitation, vaccination | I–II¶ |
| Bacterial colonisation | Presence of a recognised bacterial pathogen in sputum (sputum culture, quantitative PCR) | Antibiotics and tailored antibiotic written action plan for infections | II |
| Airway inflammation (neutrophilic) | Sputum neutrophils ≥61% | Macrolides, tetracyclines, roflumilast | II |
| Cough reflex hypersensitivity | Capsaicin challenge, cough counts, cough questionnaire | Speech pathology intervention, gabapentin | II |
| Mucus hypersecretion | Volume ≥25 mL of mucus produced daily for the past week in the absence of an infection | Mucociliary clearance techniques with a physiotherapist, inhaled hypertonic saline, macrolides | II |
| Hypoxaemia | PaO2 ≤55 mmHg; PaO2 56–59 mmHg and evidence of complications of hypoxaemia (e.g. pulmonary hypertension, polycythaemia, right-sided heart failure) | Domiciliary oxygen therapy | II |
LABA: long-acting β2-agonists; LAMA: long-acting muscarinic antagonist; SABA: short-acting β2-agonists; SAMA: short-acting muscarinic antagonist; IgE: immunoglobulin E; CT: computed tomography; IL: interleukin; PaO2: partial pressure of oxygen. #: National Health and Medical Research Council (NHMRC) level of evidence currently available for the management/treatment of each trait; ¶: studies examining the effectiveness of different treatments in bronchiectasis in general, not specifically in chronic airways disease patients with coexisting bronchiectasis. Content has been reproduced with permission from the Centre of Excellence in Treatable Traits, originally developed as part of the Centre of Excellence in Treatable Traits (https://treatabletraits.org.au).
Table 2.
List of potential treatable traits within the extrapulmonary domain to consider in patients with chronic airway disease
| Trait | Trait identification marker/diagnostic criteria | Possible treatments | Evidence level I–IV # |
| Depression | Questionnaires (e.g. HADS depression domain score ≥8, GADS score >5), psychologist/liaison psychiatrist assessment | CBT, pharmacotherapy | I |
| Anxiety | Questionnaires (e.g. HADS anxiety domain score ≥8), psychologist/liaison psychiatrist assessment | Pharmacotherapy (i.e., anxiolytics/antidepressants), breathing retraining, CBT | I |
| Dysfunctional breathing | Nijmegen Questionnaire Total score ≥23, B-PAT (breathing pattern assessment tool) score >4, breath holding time, manual assessment of respiratory motion (MARM) | Breathing retraining | I |
| Physical inactivity and sedentary behaviour | Actigraphy, International Physical Activity Questionnaire | Pulmonary rehabilitation, physical activity, breaking bouts of sedentary activity | I |
| Overweight/obesity | Overweight: BMI 25–29.9 kg·m−2 Obesity: BMI ≥30 kg·m−2 |
Caloric restriction, exercise, bariatric surgery, pharmacotherapy | I–II |
| Deconditioning | Cardiopulmonary exercise testing, 6MWT | Structured exercise programme, rehabilitation | I+, II |
| Rhinosinusitis | History and examination, imaging (sinus CT), Sino-Nasal Outcome Test (SNOT-22) | Topical corticosteroids, leukotriene receptor antagonists, antihistamines, surgery, intranasal saline lavage | II |
| VCD | Questionnaires (e.g. Pittsburgh ≥4), laryngoscopy, dynamic neck CT, inspiratory flow–volume curve | Speech pathology intervention, laryngeal botulinum toxin, gabapentin/pregabalin, psychology/psychiatry | II |
| Systemic inflammation | Leukocyte count >9×109 cells·L−1or high-sensitivity CRP >3 mg·L−1 | Statins¶ | II |
| Anaemia | Males: Hb <140 g·L−1 Females: Hb <120 g·L−1 |
Haematinic (iron/B12) supplementation | I+, IV |
| Cardiovascular disease | Doppler echocardiography, Electrocardiogram, brain natriuretic peptide | Pharmacotherapy (β-blockers, diuretics, angiotensin-converting enzyme inhibitors), surgery | II |
| GORD | Questionnaires, gastrointestinal endoscopy, pH monitoring | Anti-reflux lifestyle measures, antacids, proton pump inhibitors, fundoplication surgery | II |
| OSA | Questionnaires (i.e., STOP-Bang Questionnaire), polysomnography | CPAP, mandibular advancement splint, positional therapy, weight loss | III-2 |
HADS: hospital anxiety and depression scale; GADS: Goldberg Anxiety and Depression Scale; CBT: cognitive behavioural therapy; BMI: body mass index; 6MWT: 6-min walk test; VCD: vocal cord dysfunction; CRP: C-reactive protein; Hb: haemoglobin; GORD: gastro-oesophageal reflux disease; OSA: obstructive sleep apnoea; CPAP: continuous positive airway pressure. #: NHMRC level of evidence currently available for the management/treatment of each trait; ¶: currently research only; +: evidence from the general population. Content has been reproduced with permission from the Centre of Excellence in Treatable Traits, originally developed as part of the Centre of Excellence in Treatable Traits (https://treatabletraits.org.au).
Table 3.
List of potential treatable traits within the behaviour/risk-factor domain to consider in patients with chronic airway disease
| Trait | Trait identification marker/diagnostic criteria | Possible treatments | Evidence level I–IV # |
| Suboptimal inhaler technique | Direct observation and standardised assessment checklists, assessment via chipped inhalers | Education including demonstration and regular reassessment | I |
| Suboptimal adherence | Prescription refill rates, self-reported use of <80% of prescribed medication, chipped inhalers, FENO suppression test, measurement of drug concentrations | Self-management support, education, simplification of medication regime (i.e., reduce number of medications, frequency of doses and number of devices) | I |
| Smoking | Self-reported current smoking, elevated exhaled carbon monoxide, urinary cotinine | Smoking cessation counselling ± pharmacotherapy | I |
| Side-effects of treatments | Patient report, monitored withdrawal | Optimisation of treatment, alternative therapy, change device | I |
| Absence of a written action plan | Patient does not possess a written action plan, or reports not using the prescribed plan during exacerbations | Individualised self-management education with a written action plan | I |
| Exercise intolerance | <350 m on 6MWT | Pulmonary rehabilitation | I |
| Decreased bone mineral density (osteoporosis) | T-score ≤−2.5 | Pharmacotherapy based on osteoporosis guidelines, vitamin D supplementation, resistance training | I¶, II |
| Sarcopenia | Appendicular skeletal muscle mass index: Males <7.26 kg·m−2 Females <5.45 kg·m−2 |
Diet (high protein), resistance training | I¶, II |
#: NHMRC level of evidence currently available for the management/treatment of each trait; ¶: evidence from the general population. Content has been reproduced with permission from the Centre of Excellence in Treatable Traits, originally developed as part of the Centre of Excellence in Treatable Traits (https://treatabletraits.org.au).
Figure 2.
Proposed diagnostic strategy for adults with symptoms, signs or events suggestive of airway disease. #: smoking, allergies, sputum production, occupation, lung development and growth; ¶: tables 1–3; +: tables 2 and 3. Reproduced from [6] with permission.
To better illustrate and strengthen the argument regarding the heterogeneity and complexity of COPD, which was the catalyst for the renewed approach to its diagnosis and management, the following section of this review outlines key evidence pertaining to its genetic basis, aetiological factors, lung function trajectories, endotypes and acute exacerbations followed by current evidence regarding the efficacy of the treatable traits strategy in COPD, and the implementation challenges of treatable traits across different settings.
Heterogeneity and natural history of COPD
Genetic basis for COPD
The causative relationship between a single genetic defect leading to α1-antitrypsin deficiency and COPD is well established and was first reported by Laurell and Eriksson [8] in 1963. A more recent genetic association study, led by Hobbs et al. [9], conducted in a large number of COPD patients (n=15 256) and controls (n=47 936), identified a further 22 genetic loci of significance in COPD; highlighting that it is a polygenic disease. However, the individual odds ratio for any single genetic locus was small (OR 1.1), suggesting that several of them need to co-occur to result in phenotypic expression when exposed to environmental risk factors [9]. COPD, therefore, like the majority of complex disease models, has variable genetic contributions.
Aetiologies of COPD
Although COPD is conventionally thought of as a disease caused by cigarette smoke, there is significant heterogeneity in its aetiology. Biomass fuel exposure, recurrent pulmonary infections, abnormal lung development and poorly controlled asthma can all lead to chronic airflow limitation in the absence of exposure to cigarette smoke [4]. All of these pathways to COPD probably represent different clinical entities. For example, analyses of patients with COPD developed through biomass fuel exposure revealed their disease is characterised by less emphysema and more airway predominant involvement, with less rapid lung function decline, when compared with patients with COPD developed through cigarette smoking [10, 11]. Furthermore, patients with severe, uncontrolled asthma can develop fixed chronic airflow limitation with varying degrees of loss of lung elastic recoil and emphysema, in the absence of exposure to high-risk environmental risk factors seen in other patients with COPD [12].
As illustrated, varying histopathological expression of COPD according to its aetiology and overlapping of pathology despite distinct disease labels supports the argument for “label-free” approaches to chronic airway diseases. Furthermore, systematic recognition of varying aetiologies of COPD will facilitate better characterisation of the respective patient subgroups and create opportunities for the investigation of targeted interventions. This is inherent to the treatable traits approach.
Lung function trajectories in COPD
Heterogeneity is also displayed in the lung function trajectories of patients with COPD. Unravelling individual patient's lung function trajectories carries prognostic and potential therapeutic implications. Contrary to the most frequently cited model of lung function trajectory in COPD proposed by Fletcher and Peto [13], which was characterised by accelerated lung function decline from peak normal lung function reached in adulthood, 4–12% of the general population do not reach their predicted forced expiratory volume in 1 s (FEV1) by 20 years of age [5]. This patient subgroup develops COPD through submaximal lung function achieved in early adulthood without an enhanced rate of lung function decline thereafter [5]. This group of individuals is also reported to have an increased burden of comorbidities, with a higher prevalence and earlier incidence of comorbid cardiac and metabolic disorders and an increased risk of premature death [5, 14]. The differential lung function trajectories leading to COPD development raises the question of whether they represent different diseases? Should this hypothesis be true, it is possible that they could respond differently to treatment. This raises the question, however, as to how lung function trajectories may be differentiated when first diagnosing the patient aged in their 50s or 60s, without prior knowledge of their past lung function. The answer might be in the identification of a biomarker which would differentiate between the trajectories. Furthermore, screening lung function in early adulthood or earlier in life could enable the identification of susceptible individuals and create an opportunity to provide timely interventions to halt disease progression.
Endotypes
COPD is heterogeneous not only at a phenotypic but also at a biological level [15]. Characterisation of underlying biological mechanisms (endotypes) is essential to improve therapeutic targets in COPD and is likely to improve patient outcomes. Endotype-directed diagnosis of chronic airway disease will facilitate treatment based on biological mechanisms and not solely on the clinical presentation of the disease, which has been a cornerstone of 19th century medicine based on an Oslerian paradigm. To date, the best described endotype of COPD is α1-antitrypsin deficiency, which has a well-validated biomarker at the genetic and protein level [8]. Emerging endotypes and biomarkers in COPD include eosinophilic inflammation, neutrophilic inflammation, persistent systemic inflammation, and abnormal tissue maintenance and repair resulting in severe emphysema and changes in the lung microbiome [15]. Eosinophilic inflammation in COPD carries important treatment implications and predicts treatment responses to corticosteroid therapy [16]. Eosinophilic inflammation was shown to be associated with a heightened risk of acute COPD exacerbations [17] and a reduced rate of emphysema progression compared with non-eosinophilic COPD individuals [18]. Furthermore, sputum eosinophil count-directed management compared with symptom-focused guideline-based care, essentially a treatable traits intervention, was shown to vastly reduce exacerbations requiring hospitalisation by 62% (95% CI 5–72%, p=0.037), in COPD patients with eosinophilic inflammation [19].
Many patients with COPD have neutrophilic inflammation, which is characterised by sputum with a predominance of neutrophils and macrophages. The role of bacterial colonisation in driving neutrophilic inflammation is not yet clear as neutrophilic inflammation occurs in both colonised and non-colonised patients. Approximately one-third of COPD patients have persistent bacterial colonisation of the lower airways, which has been proposed to reflect a defect in lung innate immunity such as bacterial phagocytosis by macrophages [20]. These colonised patients are more prone to frequent exacerbations, more rapid lung function decline, and chronic bronchitis with mucus hypersecretion [21]. Long-term antibiotic therapy may be indicated for chronically colonised patients; however, there is a need for further studies to define which patients would benefit the most from such an intervention.
Systemic inflammation, characterised by persistent elevation of high-sensitivity CRP, IL-6, IL-8, fibrinogen and tumour necrosis factor-α, has also been reported in COPD patients, and has been associated with a higher risk of all-cause mortality and frequent exacerbations compared to non-inflamed COPD patients, despite similar degrees of lung function impairment [22]. Although the biology of this complex inflammatory response in COPD is not yet fully understood, it raises the possibility of a distinct endotype amongst this patient subgroup and presents an opportunity for targeted treatment [22].
Finally, abnormal tissue maintenance and repair has been proposed as a distinct endotype driving severe emphysema [15]. The biomarker which identifies this endotype has not yet been described; however, it has been hypothesised that it may be the same endotype that drives concurrent extrapulmonary tissue loss in patients with emphysema (sarcopenia, osteopenia, fat loss) [15]. This hypothesis, however, requires further investigation.
The abovementioned list of possible endotypes in COPD is neither exhaustive nor entirely understood. These endotypes, however, do represent current treatable traits that can potentially be targeted with pharmacotherapy. Further research to advance our understanding of the complex molecular pathways in COPD will present an opportunity to further develop better treatments that address the underlying disease mechanisms, and arrest or reduce disease progression. Without a systematic recognition of patients’ individual endotypes we are missing opportunities to develop new therapies or repurpose current treatments in individuals that will benefit from them the most.
Extrapulmonary traits and behavioural/risk factors
Clinical phenotypes, treatment outcomes and the prognosis of patients diagnosed with COPD are not only determined by pulmonary characteristics such as airflow limitation, emphysema, and exacerbation history, but by a host of important extrapulmonary traits including, but not limited to, BMI, cardiac health, anxiety, depression, exercise capacity, treatment adherence, self-management ability and smoking status [23]. COPD patients are known to carry a large burden of coexisting comorbidities, which determine important patient-centred outcomes including health status, treatment responsiveness and frequency of hospitalisations [23].
The contribution of extrapulmonary traits to outcomes in patients with moderate-to-severe asthma was described by Freitas et al. [24], with physical inactivity, obesity, anxiety and depression associated with worse asthma outcomes and poorer asthma control. Although, to our knowledge, similar cluster analyses based on extrapulmonary traits have not yet been conducted in patients with COPD, a similar relationship is likely to hold in this patient population.
In light of the above, it is evident that the treatment of extrapulmonary comorbidities and behavioural risk factors in patients with COPD is integral to providing optimal care for this patient population. The treatable traits strategy addresses this care need by proposing systematic identification and treatment of traits within the pulmonary, extrapulmonary and behavioural/risk-factor domains.
Acute exacerbations
Heterogeneity of COPD also manifests at the time of acute exacerbations, with the “one-size-fits-all” approach to managing exacerbations unable to meet the care needs of all patients. Exacerbations of COPD vary with respect to their endotype and aetiology. A prospective observational cohort study, led by MacDonald et al. [25], described 26 distinct phenotypes of exacerbations amongst 146 patients with COPD, with only a quarter associated with a single aetiology. Patients were phenotyped for viral infection, bacterial infection, depression/anxiety, eosinophilic inflammation, cardiac dysfunction, and environmental factors. Although the number of patients ascribed to any individual phenotype was too small to conduct statistical analysis regarding their outcomes, the results brought to light the vast diversity of the aetiological factors driving individual patient's acute exacerbation using a relatively small number of easily accessible assessment tools. In another study by Bafadhel et al. [26], four distinct biologic COPD exacerbation clusters were identified: bacterial, viral, eosinophilic predominant and pauci-inflammatory. These biologic clusters could not be distinguished clinically or through Anthonisen criteria with similar exacerbation severity across the clusters [26]. The biomarkers that best-identified the clusters were sputum IL-1β, serum CXCL10 and percentage of peripheral blood eosinophils, respectively. These subgroups were found to be independent and had differential inflammatory profiles, which suggests that they could be amenable to more specific interventions, advancing their care closer towards precision medicine.
Unravelling the heterogeneity of COPD exacerbations should be at the forefront of our agenda as they are arguably the most sentinel events in the patient's disease trajectory. Patients experiencing frequent exacerbations of COPD have worse quality of life, accelerated lung function decline and a 12-month mortality risk post-hospitalisation for an acute exacerbation of approximately 25% [27, 28]. Sentinel events drive treatment decisions across various medical disciplines. In airway diseases, acute exacerbations are an opportunity to re-evaluate treatment and introduce targeted therapies to improve treatment efficacy and minimise the risk of acute exacerbation re-occurrence. It has been proposed that the application of a treatable traits strategy in the acute phase of illness can improve recovery and exacerbation prevention with an emphasis on precision medicine rather than a “one-size-fits-all” approach to treatment and secondary prevention [29, 30]. To date, there has been no published efficacy data on the treatable traits approach in acute exacerbations, hence future research in this area is needed.
Treatable traits, a precision medicine approach for chronic airway disease management: the evidence
The complexity and heterogeneity of patients with COPD was demonstrated in a cross-sectional observational study led by McDonald et al. [31], which strengthened the discussion regarding the need for renewed approaches to the diagnosis and management of this patient population. In this study, patients’ clinical, functional, biological and behavioural characteristics, relevant to their airway disease diagnosis and management, were identified through an MDA [31]. The results of this analysis highlighted that people over 55 years of age with obstructive airway diseases experience multiple clinical management issues (traits), with a mean of 11 traits identified per patient. Although the traits identified were relevant to their airway disease diagnoses, they may not be addressed through the current management guidelines. Notably, the traits identified were similar irrespective of the type of chronic airway disease, and the degree of health status impairment correlated significantly with the number of traits detected through the MDA [31]. The most common traits identified were activity limitation (74%), airway inflammation (74%), airway hyperresponsiveness (80%) and systemic inflammation (60.5%). All the above traits were treatable and independent of the airway disease diagnoses. When treated, they had the capacity to improve health-related quality of life (HRQoL). In another study, van't Hul et al. [32] reported a high prevalence of traits amenable to nonpharmacological management in COPD patients upon their first assessment in a tertiary hospital respiratory clinic. Patients exhibited on average four treatable traits qualifying for nonpharmacological intervention, regardless of their COPD severity. The most prevalent traits were low activation for self-management, severe fatigue, low habitual physical activity and poor exercise tolerance. The identified treatable traits were independent of each other, occurred in unique combinations, and were clinically relevant as there was a significant positive association between the number of traits identified and health status impairment [32]. There was a poor correlation between the number of treatable traits identified and the FEV1 (%) predicted, illustrating heterogeneity of COPD beyond airflow limitation [32].
A treatable traits strategy provides the opportunity to identify and address those diverse clinical issues consistently and effectively, irrespective of the airway disease diagnostic label. A proof-of-concept pilot study evaluating the efficacy of a treatable traits approach for managing patients with COPD was conducted by McDonald et al. [33]. This study recruited older adults (>55 years) with stable COPD. The intervention (n=17) involved an MDA, inflammometry and individualised management supported by a case manager and a multidisciplinary team over 3 months and was compared with usual care in a tertiary hospital respiratory clinic (n=19). The authors reported that delivery of personalised treatment employing a treatable traits strategy resulted in significant improvements in health status compared with a standard care approach, with a mean (95% CI) difference in St George's Respiratory Questionnaire (SGRQ) of 14 (8.5–20.7) versus 3.5 (−3.8–10.8) in the control group (p=0.0003). The number needed to treat to achieve a clinically significant change in SGRQ was two in the intervention group. Health status continued to improve at 6-month follow-up, mean (95% CI) decrease of 17.1 (7.1–27.1) units, (p=0.002) and was maintained at 12 months with a 13.5 (4.7–22.3) unit decrease from baseline (p=0.005). There was no significant difference either at 6 months or 12 months in the control group. Furthermore, targeted inflammation-based management reduced eosinophilic and neutrophilic airway inflammation and systemic inflammation in the intervention group but not in the control group. Despite this intervention being delivered over 3 months, its benefits were sustained at 6 and 12 months in the intervention group. In addition, although this was only a small pilot study, the reported effect size was very promising and formed the basis for further work to investigate the real-world efficacy of the treatable traits approach. A multidimensional treatable traits intervention has also been tested in a severe asthma population compared with severe asthma usual care, and resulted in similar improvements in health status to that of the COPD proof-of-concept study [34], suggesting the approach is efficacious in both asthma and COPD.
Implementation of the treatable traits strategy across different settings
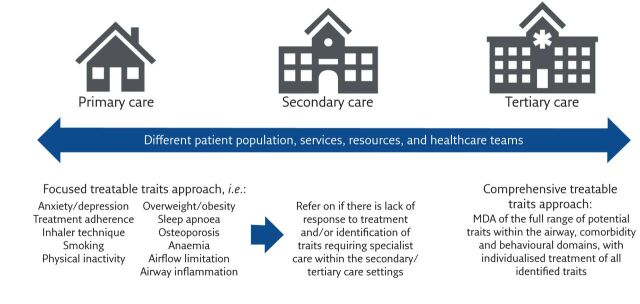
Evolving from “umbrella” terms for airway diseases to the implementation of a trait-based approach to guide treatment across multiple settings is a key goal in the landscape of chronic airway diseases moving forward [35]. However, while MDA has been implemented in severe asthma clinics within the tertiary care setting, a treatable traits approach has not yet been integrated into the care of patients with all subtypes and severity of chronic airway diseases, including COPD. Data on the feasibility and cost-effectiveness of implementing a treatable traits approach for the management of COPD across different healthcare settings are likely to lead to greater support of this approach. Effective implementation of this model of care will likely require adaptation of the approach to the healthcare setting which considers not only the needs of the population but also the accessibility and availability of healthcare services, resources, and healthcare professionals (figure 3). For instance, low-, middle- and high-income countries are likely to require considerably different treatable traits implementation approaches [36]. This is largely due to their disparate healthcare needs and systems [36], which will strongly influence the range of treatable traits that are feasible to target. Indeed, it is recognised that low- and middle-income countries may lack the resources required to assess and treat the full range of potential pulmonary, extrapulmonary and risk-factor/behavioural traits within this somewhat complex model of care, and therefore a simplified or “focused” approach targeting key traits (i.e., traits that have been identified as important and feasible to address in any setting: airflow limitation, airway inflammation, smoking, nutrition, physical inactivity, and self-management skills [35, 37]) may be more feasible (figure 3).
Figure 3.
Implementation of the treatable traits strategy across different healthcare settings. Effective implementation of this model of care for the management of patients with COPD will likely require adaptation of the approach to the healthcare setting, which considers not only the needs of the population but also the accessibility and availability of healthcare services, resources, and healthcare professionals. Content has been reproduced with permission from the Centre of Excellence in Treatable Traits, originally developed as part of the Centre of Excellence in Treatable Traits (https://treatabletraits.org.au).
The practical application of treatable traits across different settings within the healthcare system (i.e., primary, secondary, and tertiary care) also requires consideration. A large proportion of new COPD diagnoses occur within the primary care setting, as does the routine management of COPD patients with mild and moderate disease. Given that significant heterogeneity in COPD has been demonstrated irrespective of disease severity [38], the implementation of a treatable traits approach within the primary care setting has the potential to reduce the overall burden of COPD significantly. However, while the comprehensive treatable traits approach may be feasible in the well-resourced tertiary care setting, primary care is another under-resourced setting in which a more focused treatable traits approach may be required. One such approach that has been proposed involves individualising treatment based on two dominant pulmonary traits, airflow limitation and eosinophilic airway inflammation, which may be more feasible within the primary care setting [6]. However, whether focusing on only two traits reduces the potential benefit of the treatable traits approach is unknown. An alternative model of care may be to use a hierarchical approach to address traits that are already managed in primary care (i.e., anxiety and depression, treatment adherence, inhaler technique, smoking, physical inactivity, nutrition, and sleep apnoea, as well as the pulmonary traits of airflow limitation and airway inflammation), with an established referral pathway to specialist care within the secondary/tertiary settings for more complex patients who are unable to achieve an acceptable level of disease control within the primary care setting (figure 3).
The hierarchy of dominant and important treatable traits, however, is yet to be determined. One approach is to prioritise traits according to their prevalence, severity and/or impact on disease outcomes [37]. A study, by Hiles et al. [39], used a novel Bayesian model averaging technique to identify clinically impactful treatable traits in patients with chronic airway disease (severe asthma and COPD) by exploring which traits were associated with HRQoL. Of the 22 treatable traits identified, the best model for predicting HRQoL was comprised of five traits across the pulmonary, extrapulmonary and behavioural domains: frequent chest infections, inadequate inhaler technique, systemic inflammation, depression and breathing pattern disorder/dysfunctional breathing [39]. Traits that predict general quality of life and decline in lung function have also been explored in patients with COPD specifically [40]. In a 4-year longitudinal prospective evaluation of an English cohort of patients with COPD, seven traits that predicted quality of life were identified: chronic bronchitis, arthritis, depression, cardiovascular disease, anaemia, disability, and poor social and family support; while five traits were found to be associated with decline in lung function [40]. These included chronic bronchitis, breathlessness, sarcopenia, underweight, and current smoking [40]. This is not to say that the other treatable traits should not be considered priorities in the management of individuals with COPD, particularly given the absence of endotypes in this analysis. Indeed, it appears that different traits are likely to matter in different ways. This highlights the need to identify traits that impact a range of outcomes, including risk of future exacerbations, symptom control, mortality, and the development of new disease [37], to guide the prioritisation of traits using this approach.
Prioritisation of traits could also be based on treatment response [37]; that is, prioritising traits that when treated provide the greatest “bang for our buck”. For example, Hiles et al. [39] reported that treating systemic inflammation and eosinophilic airway inflammation were associated with the greatest improvements in HRQoL, while treatments for exercise intolerance, obesity and anxiety were also associated with HRQoL improvements, but to a lesser degree. A similar approach would be to prioritise traits based on their potential to create a domino effect when treated [37]. For example, it has been demonstrated that targeting obesity in patients with COPD using a weight loss intervention not only improved body weight, but also various other traits such as exercise tolerance, skeletal muscle strength and depression, as well a number of cardiovascular and metabolic markers [41]. Patients’ treatment priorities could also be used to guide the prioritisation of traits [37]. Indeed, in a population with chronic airway disease it has previously been demonstrated that clinicians and patients’ priorities do not always align [42]. While there was good concordance between patients and their physician regarding the importance of managing activity limitation, airway inflammation and dyspnoea, there was poor patient–physician agreement regarding the importance several other traits including inhaler technique adequacy, airflow limitation and obesity. Understanding treatment priorities of patients is an essential element of effective shared care [33], and therefore should be considered in the prioritisation of traits within this model of care.
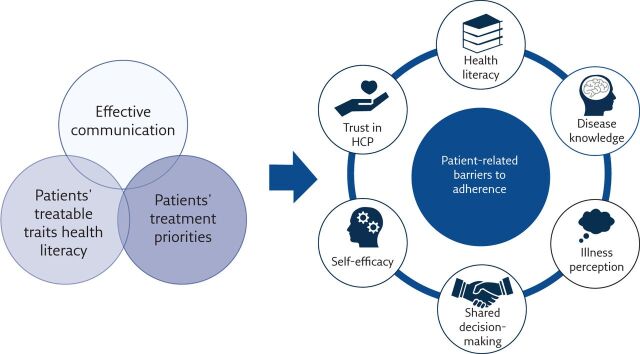
Successful implementation of new models of care within any healthcare setting also requires consideration of how to effectively engage key stakeholders in the approach. A key component of the treatable traits strategy is the coordination of care by a multidisciplinary team of healthcare professionals, including general practitioners, respiratory physicians, specialist nurses, dietitians, speech pathologists, psychologists/psychiatrists and physiotherapists. To ensure the smooth implementation of the model of care into usual clinical practice, it is important that healthcare professionals are provided with adequate training, education, and resources. Determination of what is needed to support healthcare professionals in the implementation of treatable traits in clinical practice is an important area for future research. Patient engagement is also integral in bridging the gap between the efficacy and effectiveness of an intervention or treatment. Indeed, patient adherence is one of the main contributors to suboptimal COPD management and subsequently poor clinical outcomes [43]. Shared decision-making which accommodates patients’ goals and priorities is a key strategy for engaging patients in their care. As discussed earlier, clinician and patients’ treatment priorities do not always align [42]. This supports the need for clinician–patient partnerships with shared decision-making, which has been shown improve treatment adherence and subsequently overall chronic disease management [44]. It is also important that the health literacy of the individual patient is taken into consideration, and that the treatable traits approach is communicated to patients using terminology they understand (figure 4) [42]. Other strategies which have been demonstrated to improve treatment adherence in COPD and which may assist the smooth implementation of this model of care into clinical practice include ensuring continuity of care, educating patients on the rationale behind the prescribed treatments, using written instructions, and ensuring regular follow-up assessments are conducted [43].
Figure 4.
A model for optimising patient engagement in the treatable traits model of care. To enhance patient engagement to this approach, we have developed a model of what we think is needed to address many patient-related barriers to adherence: effective communication of treatable traits using terminology patients understand, understanding and addressing patients’ treatable traits health literacy, and using shared decision-making to accommodate patients’ goals and priorities. Content has been reproduced with permission from the Centre of Excellence in Treatable Traits, originally developed as part of the Centre of Excellence in Treatable Traits (https://treatabletraits.org.au). HCP: healthcare professionals.
The cost-effectiveness of the treatable traits model of care is not yet established. However, given that the model of care provides a more rational approach to treatment with targeted interventions it is proposed that the approach may have an initial increase in cost that will become cost neutral due to the reduced healthcare utilisation requirements [33].
Future
In summary, evolving from “umbrella” terms for airway disease to implementation of a trait-based approach to guide treatment across multiple settings is the key goal in the landscape of chronic airway diseases in the next few years. Admittedly, we do not hold treatments or understand biological mechanisms underpinning all treatable traits in chronic airway diseases, such as fixed airflow limitation, systemic or neutrophilic inflammation. This, however, should not preclude the identification of these traits and presents an opportunity for their investigation and development of targeted treatments. Unravelling heterogeneity of chronic airway diseases in each patient during times of stability as well as during periods of acute exacerbations will form the platform for further research and progress precision medicine in chronic airway diseases. Furthermore, we need to generate more data to assess the longitudinal stability of treatable traits, which will likely inform important treatment decisions and shed further light on the complexity of chronic airway diseases in any individual patient. Real-world implementation studies which evaluate the effectiveness of different treatable traits models in different settings are now needed. This will constitute more generalisable evidence on effectiveness to inform policy change in the long-term.
Key points
COPD is a heterogeneous clinical syndrome, which requires deconstruction of its individual components to facilitate targeted treatment and improve individual patient outcomes.
The treatable traits strategy is a proposed vehicle for the implementation of precision medicine in chronic airway diseases which entails the application of multidimensional assessment to identify each patient's treatable traits and guides the application of individualised treatment.
The treatable traits strategy has been demonstrated to be efficacious in improving quality of life and other treatment outcomes in chronic airway diseases.
The treatable traits strategy can be applied to unravel heterogeneity and complexity of COPD during stability as well as during periods of acute exacerbations.
Implementation of the treatable traits strategy in a wide range of clinical settings will generate real-life data on its efficacy and will help to inform long-term policy change.
Self-evaluation questions
What is the basis for coining COPD as a syndrome rather than a single disease?
What is the treatable traits approach to chronic airway disease?
What evidence do we have to support the implementation of the treatable traits approach into clinical practice?
What considerations are needed when implementing a treatable traits approach in COPD management?
Suggested answers
This is due to the increased recognition of the heterogeneity in terms of the genetic makeup, aetiologies, endotypes and lung function trajectories in patients with COPD.
The treatable traits strategy is a model of care for the management of patients with chronic airway disease, allowing implementation of precision medicine in chronic airway diseases. This approach utilises multidimensional assessment of every patient to determine the core traits (classified under three domains: pulmonary, extrapulmonary and behavioural/risk-factors) associated with disease outcomes, followed by the application of targeted and evidence-based treatments founded on the assessment outcome.
Studies have demonstrated the complexity and heterogeneity of chronic airways diseases. Furthermore, treatable traits strategies have been tested and have demonstrated significant improvements in health status compared with a standard care approach, in both COPD and severe asthma.
Effective implementation of a treatable traits approach in COPD management will likely require adaptation of the approach to the healthcare setting which considers not only the needs of the population but also the accessibility and availability of healthcare services, resources, and healthcare professionals. Ways of engaging key stakeholders (i.e., healthcare professionals and patients) in the approach will also require careful consideration.
Footnotes
Author contributionsAll authors (K. Duszyk, R.F. McLoughlin, P.G. Gibson, V.M. McDonald) contributed to the conceptualisation and writing of the manuscript and have reviewed and approved the final submitted version.
Conflict of interest: K. Duszyk has nothing to disclose.
Conflict of interest: R.F. McLoughlin has nothing to disclose.
Conflict of interest: P.G. Gibson has received grants and consultancy fees from GlaxoSmithKline, Novartis and AstraZeneca.
Conflict of interest: V.M. McDonald has received grants and consultancy fees from GlaxoSmithKline and AstraZeneca.
References
- 1.Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J 2019; 53: 1900164. doi: 10.1183/13993003.00164-2019 [DOI] [PubMed] [Google Scholar]
- 2.Blanco I, Diego I, Bueno P, et al. Geographic distribution of COPD prevalence in the world displayed by geographic information system maps. Eur Respir J 2019; 54: 1900610. doi: 10.1183/13993003.00610-2019 [DOI] [PubMed] [Google Scholar]
- 3.Agusti A. The path to personalised medicine in COPD. Thorax 2014; 69: 857–864. doi: 10.1136/thoraxjnl-2014-205507 [DOI] [PubMed] [Google Scholar]
- 4.Celli BR, Agustí A. COPD: time to improve its taxonomy? ERJ Open Res 2018; 4: 00132-2017. doi: 10.1183/23120541.00132-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agustí A, Hogg JC. Update on the pathogenesis of chronic obstructive pulmonary disease. N Engl J Med 2019; 381: 1248–1256. doi: 10.1056/NEJMra1900475 [DOI] [PubMed] [Google Scholar]
- 6.Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 2016; 47: 410–419. doi: 10.1183/13993003.01359-2015 [DOI] [PubMed] [Google Scholar]
- 7.Agusti A. The disease model: implications for clinical practice. Eur Respir J 2018; 51: 1800188. doi: 10.1183/13993003.00188-2018 [DOI] [PubMed] [Google Scholar]
- 8.Laurell C, Eriksson S. The electrophoretic α1-globulin pattern of serum in α1-antitrypsin deficiency. Scand Clin Lab Invest 1963; 15: 132–140. doi: 10.1080/00365516309051324 [DOI] [Google Scholar]
- 9.Hobbs BD, De Jong K, Lamontagne M, et al. Genetic loci associated with chronic obstructive pulmonary disease overlap with loci for lung function and pulmonary fibrosis. Nat Genet 2017; 49: 426–432. doi: 10.1038/ng.3752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramírez-Venegas A, Sansores RH, Pérez-Padilla R, et al. Survival of patients with chronic obstructive pulmonary disease due to biomass smoke and tobacco. Am J Respir Crit Care Med 2006; 173: 393–397. doi: 10.1164/rccm.200504-568OC [DOI] [PubMed] [Google Scholar]
- 11.Hu G, Zhou Y, Tian J, et al. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest 2010; 138: 20–31. doi: 10.1378/chest.08-2114 [DOI] [PubMed] [Google Scholar]
- 12.Gelb AF, Zamel N. Unsuspected pseudophysiologic emphysema in chronic persistent asthma. Am J Respir Crit Care Med 2000; 162: 1778–1782. doi: 10.1164/ajrccm.162.5.2001037 [DOI] [PubMed] [Google Scholar]
- 13.Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J 1977; 1: 1645–1648. doi: 10.1136/bmj.1.6077.1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agustí A, Noell G, Brugada J, et al. Lung function in early adulthood and health in later life: a transgenerational cohort analysis. Lancet Respir Med 2017; 5: 935–945. doi: 10.1016/S2213-2600(17)30434-4 [DOI] [PubMed] [Google Scholar]
- 15.Agustí A, Celli B, Faner R. What does endotyping mean for treatment in chronic obstructive pulmonary disease? Lancet 2017; 390: 980–987. doi: 10.1016/S0140-6736(17)32136-0 [DOI] [PubMed] [Google Scholar]
- 16.Leigh R, Pizzichini M, Morris M, et al. Stable COPD: predicting benefit from high-dose inhaled corticosteroid treatment. Eur Respir J 2006; 27: 964–971. doi: 10.1183/09031936.06.00072105 [DOI] [PubMed] [Google Scholar]
- 17.Hastie AT, Martinez FJ, Curtis JL, et al. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. Lancet Respir Med 2017; 5: 956–967. doi: 10.1016/S2213-2600(17)30432-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh D, Kolsum U, Brightling CE, et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J 2014; 44: 1697–1700. doi: 10.1183/09031936.00162414 [DOI] [PubMed] [Google Scholar]
- 19.Siva R, Green RH, Brightling CE, et al. Eosinophilic airway inflammation and exacerbations of COPD: a randomised controlled trial. Eur Respir J 2007; 29: 906–913. doi: 10.1183/09031936.00146306 [DOI] [PubMed] [Google Scholar]
- 20.Donnelly LE, Barnes PJ. Defective phagocytosis in airways disease. Chest 2012; 141: 1055–1062. doi: 10.1378/chest.11-2348 [DOI] [PubMed] [Google Scholar]
- 21.Patel I, Seemungal T, Wilks M, et al. Relationship between bacterial colonisation and the frequency, character, and severity of COPD exacerbations. Thorax 2002; 57: 759–764. doi: 10.1136/thorax.57.9.759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agustí A, Edwards LD, Rennard SI, et al. Persistent systemic inflammation is associated with poor clinical outcomes in COPD: a novel phenotype. PLoS One 2012; 7: e37483. doi: 10.1371/journal.pone.0037483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Divo MJ, Casanova C, Marin JM, et al. COPD comorbidities network. Eur Respir J 2015; 46: 640–650. doi: 10.1183/09031936.00171614 [DOI] [PubMed] [Google Scholar]
- 24.Freitas PD, Xavier RF, McDonald VM, et al. Identification of asthma phenotypes based on extrapulmonary treatable traits. Eur Respir J 2021; 57: 2000240. doi: 10.1183/13993003.00240-2020 [DOI] [PubMed] [Google Scholar]
- 25.MacDonald MI, Osadnik CR, Bulfin L, et al. MULTI-PHACET-multidimensional clinical phenotyping of hospitalised acute COPD exacerbations. ERJ Open Res 2021; 7: 00198-2021. doi: 10.1183/23120541.00198-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bafadhel M, McKenna S, Terry S, et al. Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers. Am J Respir Crit Care Med 2011; 184: 662–671. doi: 10.1164/rccm.201104-0597OC [DOI] [PubMed] [Google Scholar]
- 27.García-Sanz M-T, Cánive-Gómez J-C, Senín-Rial L, et al. One-year and long-term mortality in patients hospitalized for chronic obstructive pulmonary disease. J Thorac Dis 2017; 9: 636–645. doi: 10.21037/jtd.2017.03.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho T-W, Tsai Y-J, Ruan S-Y, et al. In-hospital and one-year mortality and their predictors in patients hospitalized for first-ever chronic obstructive pulmonary disease exacerbations: a nationwide population-based study. PLoS One 2014; 9: e114866. doi: 10.1371/journal.pone.0114866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDonald VM, Osadnik CR, Gibson PG. Treatable traits in acute exacerbations of chronic airway diseases. Chron Respir Dis 2019; 16: 1479973119867954. doi: 10.1177/1479973119867954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mathioudakis AG, Janssens W, Sivapalan P, et al. Acute exacerbations of chronic obstructive pulmonary disease: in search of diagnostic biomarkers and treatable traits. Thorax 2020; 75: 520–527. doi: 10.1136/thoraxjnl-2019-214484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDonald VM, Simpson JL, Higgins I, et al. Multidimensional assessment of older people with asthma and COPD: clinical management and health status. Age Ageing 2011; 40: 42–49. doi: 10.1093/ageing/afq134 [DOI] [PubMed] [Google Scholar]
- 32.van't Hul AJ, Koolen EH, Antons JC, et al. Treatable traits qualifying for nonpharmacological interventions in COPD patients upon first referral to a pulmonologist: the COPD sTRAITosphere. ERJ Open Res 2020; 6: 00438-2020. doi: 10.1183/23120541.00438-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McDonald VM, Higgins I, Wood LG, et al. Multidimensional assessment and tailored interventions for COPD: respiratory utopia or common sense? Thorax 2013; 68: 691–694. doi: 10.1136/thoraxjnl-2012-202646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McDonald VM, Clark VL, Cordova-Rivera L, et al. Targeting treatable traits in severe asthma: a randomised controlled trial. Eur Respir J 2020; 55: 1901509. doi: 10.1183/13993003.01509-2019 [DOI] [PubMed] [Google Scholar]
- 35.Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases. Lancet 2018; 391: 350–400. doi: 10.1016/S0140-6736(17)30879-6 [DOI] [PubMed] [Google Scholar]
- 36.McDonald VM, Gibson PG. Treatable traits and their application in high-, middle- and low-income countries. Respirology 2019; 24: 942–943. doi: 10.1111/resp.13626 [DOI] [PubMed] [Google Scholar]
- 37.McDonald VM, Fingleton J, Agusti A, et al. Treatable traits: a new paradigm for 21st century management of chronic airway diseases: treatable traits down under international workshop report. Eur Respir J 2019; 53: 1802058. doi: 10.1183/13993003.02058-2018 [DOI] [PubMed] [Google Scholar]
- 38.Agusti A, Calverley PMA, Celli B, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res 2010; 11: 122. doi: 10.1186/1465-9921-11-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hiles SA, Gibson PG, Agusti A, et al. Treatable traits that predict health status and treatment response in airway disease. J Allergy Clin Immunol Pract 2021; 9: 1255–1264.e2. doi: 10.1016/j.jaip.2020.09.046 [DOI] [PubMed] [Google Scholar]
- 40.Sarwar MR, McDonald VM, Abramson MJ, et al. Treatable traits in an English cohort: prevalence and predictors of future decline in lung function and quality of life in COPD. ERJ Open Res 2021; 7: 00934-2020. doi: 10.1183/23120541.00934-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McDonald VM, Gibson PG, Scott HA, et al. Should we treat obesity in COPD? The effects of diet and resistance exercise training. Respirology 2016; 21: 875–882. doi: 10.1111/resp.12746 [DOI] [PubMed] [Google Scholar]
- 42.McDonald VM, Higgins I, Simpson JL, et al. The importance of clinical management problems in older people with COPD and asthma: do patients and physicians agree? Prim Care Respir J 2011; 20: 389–395. doi: 10.4104/pcrj.2011.00025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax 2008; 63: 831–838. doi: 10.1136/thx.2007.086041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med 2010; 181: 566–577. doi: 10.1164/rccm.200906-0907OC [DOI] [PMC free article] [PubMed] [Google Scholar]