Abstract
Background
Oblique lateral interbody fusion (OLIF) is a new and minimally invasive surgery. This study aimed to compare the clinical efficacy and safety of oblique lateral interbody fusion with anterolateral screw fixation and with posterior percutaneous screw fixation in treating single-segment mild degenerative lumbar diseases.
Material/Methods
A retrospective analysis was performed on 51 patients with single-segment mild degenerative lumbar diseases who received OLIF from April 2017 to January 2020 in Hong Hui Hospital, Xi’an Jiao Tong University; 24 and 27 patients received OLIF with anterolateral screw fixation (OLIF+AF) and OLIF with posterior percutaneous screw fixation (OLIF+PF), respectively. Anesthesia time, operation time, intraoperative blood loss, intraoperative fluoroscopy number, hospital stay, postoperative complications, Visual Analog Scale (VAS) score, Oswestry Disability Index (ODI) score, anterior and posterior disc heights, foraminal height, and fusion rate of the 2 groups were compared to assess clinical and radiological outcomes.
Results
Anesthesia time, operation time, intraoperative blood loss, number of intraoperative fluoroscopy, and VAS score in the OLIF+AF group were significantly better than those in the OLIF+PF group (P<0.05). There were no significant differences in ODI score, anterior and posterior disc heights, foraminal height, fusion rate, and incidence of complications between the 2 groups (P<0.05).
Conclusions
OLIF+AF in treating single-segment mild degenerative lumbar diseases produces a satisfactory clinical effect. Moreover, OLIF+AF does not invade the paraspinal muscle group, thereby reducing trauma, postoperative residual low back pain, operation time, bleeding, and frequency of fluoroscopy. Thus, OLIF+AF is a feasible treatment method for single-segment mild degenerative lumbar diseases.
Keywords: Lumbar Vertebrae, Pedicle Screws, Intervertebral Disc Degeneration
Background
Along with the recent extension of people’s lifespan and changes in lifestyle, the annual incidence of lumbar degenerative diseases has also been increasing, becoming a leading public health problem endangering human health [1]. Posterior lumbar interbody fusion and transforaminal lumbar interbody fusion are common treatments for lumbar degenerative diseases. Posterior fusion has good clinical efficacy, but it can cause significant damage to paraspinal tissue, causing long-term chronic low back pain. Moreover, posterior fusion is an intraspinal procedure with a risk of nerve root and dural injury [2].
With the development of minimally invasive fusion technology, oblique lateral interbody fusion (OLIF) has been applied clinically. OLIF is a new and minimally invasive surgery proposed by Silvestre in 2012, and since then, it has been widely used in treating lumbar diseases [3–5]. OLIF enters through the peritoneum behind the natural space between the psoas major muscle and the abdominal aorta, and directly exposes the target vertebral body and the anterior side of the intervertebral disc. It avoids damaging the muscles, ligaments, and bones behind the lumbar spine. It also reduces bleeding, trauma, and operation and postoperative recovery times, significantly reducing the risk of complications [6]. Most patients with lumbar degenerative diseases are elderly. Affected by osteoporosis, complications such as cage displacement and cage subsidence after OLIF cannot be ignored. At present, OLIF with posterior percutaneous pedicle screw fixation (OLIF+PF) is widely used and can reconstruct spinal stability, restore the normal spinal sequence, and improve intervertebral fusion rates [7]. However, the combined procedure requires the intraoperative change of patient position, significantly increasing the operative time and amount of intraoperative bleeding and fluoroscopy [8]. To reduce these problems, some scholars have proposed OLIF with anterolateral screw fixation (OLIF+AF) instead for treating lumbar degenerative diseases. Because the cage used in OLIF is larger and spans the bilateral epiphyseal ring, the stability of the fixation interface is significantly enhanced so that the effective fixation strength can be achieved with lateral screw-assisted fixation of the vertebral body [9,10]. However, there are few reports on the clinical efficacy and safety of OLIF+AF in treating lumbar degenerative diseases. This study aimed to investigate the feasibility and safety of OLIF+AF in treating lumbar degenerative diseases, compared with OLIF+PF.
Material and Methods
Study Design and Patients
This study was approved by the Ethics Committee of the Hong Hui Hospital, Xi’an Jiao Tong University (no. 202105001). Retrospective analysis was performed on 51 patients with single-level lumbar degenerative diseases who received OLIF at Hong Hui Hospital, Xi’an Jiao Tong University from April 2017 to January 2020. They were then divided into the OLIF+AF (24 patients, 11 men) and OLIF+PF (27 patients, 12 men) groups, with a mean age of 57.2±9.4 (range, 51–79) and 59.7±8.9 (range, 52–77) years, respectively. The inclusion criteria were as follows: (1) L2–L5 single-level lumbar degenerative disease; (2) mild lumbar spondylolisthesis (Meyerding spondylolisthesis grades I–II) and low back pain, with ineffective conservative treatment for >3 months; (3) discography-confirmed low back pain lasting >6 months (diagnostic for discogenic back pain); (4) lumbar instability on dynamic radiography, with associated low back pain, and ineffective conservative treatment for >3 months; and (5) no obvious signs of neurological impairment. The exclusion criteria were as follows: (1) ≥2 levels with lumbar degenerative diseases; (2) severe slippage (Meyerding grades III–IV); (3) severe osteoporosis with a bone mineral density (BMD) T-score <−3.5; (4) morbid obesity (body mass index [BMI] >35 kg/m2); (5) large free disc herniation in the affected segment; (6) lumbar trauma, infection, and tumor; (7) intervertebral space fused spontaneously or with osteophyte formation anterior to the vertebral body; (8) a history of left abdominal surgery within the past year; and (9) incomplete medical records.
Surgical Technique
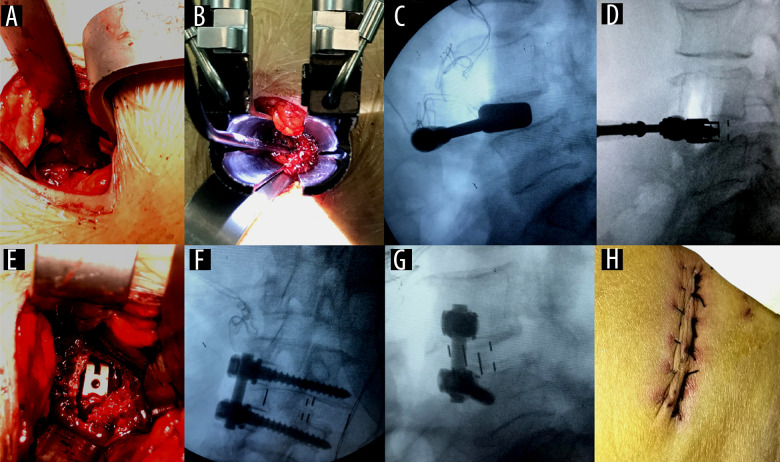
The surgery was performed according to the methods introduced by Sato et al [11]. Intraoperative neurophysiological monitoring was not required. The same experienced clinician performed the surgery for all patients. Preoperatively, the patient, under general anesthesia, was placed in the right decubitus position, and the target segment was identified by C-arm fluoroscopy. The abdominal muscles were bluntly dissected ventrally from the target intervertebral space to the retroperitoneal space (Figure 1A). The fingers pushed the peritoneum forward to the anterior edge of the psoas major and ventrally to expose the space between the psoas major and the abdominal aorta. The target intervertebral disc was touched, and a needle and the C-arm were positioned. After the target intervertebral disc was confirmed, the OLIF tubular retractor system was placed (Figure 1B). Finally, the expanding trocar was connected to the serpent arm and fixed on the operating table. Stabilizing pins were placed at the lower endplate level of the upper vertebral body to secure the working channel, which was moderately extended to fully expose the target disc. Residual disc tissue was treated with a reamer and the endplate cartilage was processed. The mold of the cage was tested and examined under a fluoroscope (Figure 1C). A suitable cage mixed with allograft bone was loaded into the target intervertebral space and positioned through fluoroscopy (Figure 1D, 1E).
Figure 1. Surgical technique.
(A) A 3.0-cm centered skin incision was made in projection of the target segment; (B) the tubular retractor system was placed in the targeting disc; (C) the mold of the cage was tested and examined under a fluoroscope; (D) the cage was placed and examined under a fluoroscope; (E) the cage was directly observed in the intervertebral space; (F) intraoperative fluoroscopy in the anteroposterior position; (G) intraoperative fluoroscopy in the lateral position; and (H) the surgical wound after suturing.
In the OLIF+AF group, a small hole was drilled with an opening device near the center of the vertebral body in the target intervertebral space, and an open-path vertebra and wire tap were used for drilling into the cancellous bone and tapping, respectively. Two screws were inserted to the areas at which the screws just penetrated the contralateral cortex, and the connecting rod was locked and fixed. Fluoroscopy then confirmed the position (Figure 1F, 1G), after which the abdominal muscle, fascia, subcutaneous tissue, and skin were sutured layer by layer (Figure 1H).
Patients in the OLIF+PF group were positioned prone. Four pedicle screws were placed percutaneously, as assisted by the C-arm. After the C-arm fluoroscopy proved correct, the screw-rod system was installed, and the incisions were closed layer by layer.
Perioperative Management
Cephalosporins were administered intravenously 30 min before surgery and 24 h after surgery to prevent infection. Regular postoperative analgesic treatment was conducted, with appropriately selected drugs and dosage, according to the patients’ pain levels. On the third postoperative day, the patients could walk out of bed with the protection of lumbar braces and the assistance of a walker.
Clinical Evaluation
Demographic data, including sex, age, height, weight, and BMD measured by dual-energy X-ray absorptiometry, and clinical data, including anesthesia time, operative time, intraoperative blood loss, intraoperative X-ray examination, and hospital stay, were recorded. Complications, including abdominal vascular injury, ventral dural tear, ureteral injury, sympathetic nerve injury, screw malposition, wound infection, paralytic ileus, donor site pain, thigh pain/numbness, iliopsoas/quadriceps weakness, and cage subsidence, were also recorded. The clinical results of the patients were routinely assessed based on Visual Analog Scale (VAS) scores for low back pain and the Oswestry Disability Index (ODI) before surgery, 1 week, 3 months, and 12 months after surgery, and on the final follow-up. The VAS score indicated the patients’ subjective pain by using a 10-cm line with values from 0 on one end, indicating no pain, to 10 on the other end, indicating severe pain. The ODI score evaluates the degree of back and leg pain, as well as self-care, heavy-lifting, standing, walking, sleeping, socializing, and traveling abilities. Each question has 6 options ranging from 0 (no dysfunction) to 5 (severe pain or dysfunction).
Radiographic Evaluation
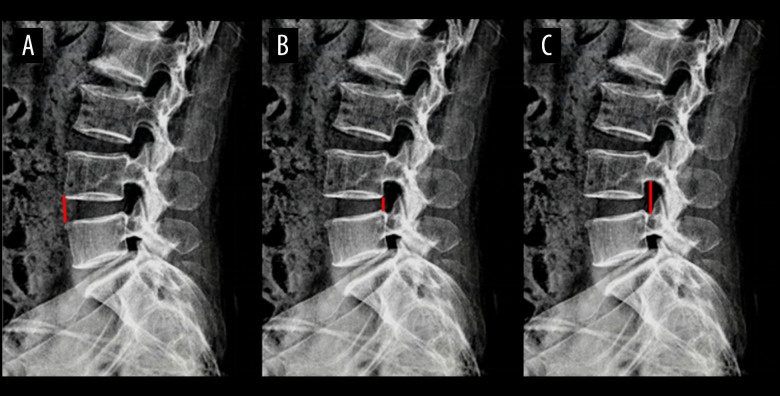
Imaging data, including X-ray scanning and computed tomography (CT), were collected before surgery, at 1 week, 3 months, and 12 months after surgery, and on the final follow-up. Figure 2 shows the method of radioactivity measurement. Anterior disc height (ADH), posterior disc height (PDH), and foraminal height (FH) were obtained by lateral X-ray imaging. In the case of L4–L5, ADH and PDH are the anterior and posterior distances, respectively, between the lower-end L4 plate and upper-end L5 plate (Figure 2A, 2B), and FH is the distance between the lower edge of the L4 pedicle and the upper edge of the L5 pedicle (Figure 2C). The fusion rates were obtained by CT at final follow-up, and the scoring standard of fusion rate was based on the Bridwell interbody fusion scoring system. The intervertebral fusion was evaluated of as follows: grade I, fusion with trabeculae reconstruction; grade II, graft intact, not fully trabeculae reconstruction but with no lucencies at the top or bottom of the graft; grade III, graft intact, but a certain lucency at the top or bottom of the graft; grade IV, certainly not fusion with resorption of bone graft and collapse. The first and second levels are considered as successful fusions [12]. All imaging scans were read by 2 independent and blinded physicians with ≥10 years of experience, and the average measurements of the physicians were calculated and analyzed.
Figure 2. Radiographic evaluation.
(A) In the case of L4–5, anterior disc height is the anterior distance between the lower-end L4 plate and upper-end L5 plate (red line). (B) In the case of L4–5, posterior disc height is the posterior distance between the lower-end L4 plate and upper-end L5 plate (red line). (C) In the case of L4–5, foraminal height is the distance between the lower edge of the L4 pedicle and the upper edge of the L5 pedicle (red line).
Statistical Methods
SPSS version 24.0 (IBM Corp, Armonk, NY, USA) was used for statistical analysis. Continuous normal distribution data are expressed as means with standard deviations, and analyzed using the t test. Nonnormally distributed continuous data are represented as medians with ranges and analyzed using the Wilcoxon test. Enumeration data were represented as frequencies, and analyzed using the chi-squared test. Statistical significance was set at P<0.05.
Results
Demographic Data
From April 2017 to January 2020, a total of 51 patients were enrolled in this retrospective study, with 24 and 27 patients in the OLIF+AF and OLIF+PF groups, respectively. As shown in Table 1, there were no statistically significant differences between the groups in terms of age, sex, BMD, BMI, preoperative diagnosis, and follow-up time (P<0.05).
Table 1.
Comparision of demographic OLIF+AF group and OLIF+PF group.
| OLIF+AF | OLIF+PF | p value | |
|---|---|---|---|
| Number | 24 | 27 | |
| Mean age: years (mean±SD) | 57.2±9.4 | 59.7±8.9 | p=0.671 |
| Sex (n, %) | p=0.921 | ||
| Male | 11 (45.8%) | 12 (44.4%) | |
| Female | 13 (54.2%) | 15 (55.6%) | |
| BMI: Kg/m2 (mean±SD) | 22.7±2.5 | 24.1±2.3 | p=0.264 |
| BMI: T-score (mean±SD) | −1.7±1.1 | −1.9±1.3 | p=0.463 |
| Preoperative diagnosis | p=0.721 | ||
| Lumbar spondylolysthesis | 18 (75.0%) | 19 (70.4%) | |
| Lumbar instability | 4 (16.7%) | 4 (18.5%) | |
| Discogenic low back pain | 2 (8.3%) | 3 (11.1%) | |
| Follow-up time (months) | 18.6±6.2 | 17.9±5.7 | p=0.579 |
Clinical Outcomes
All surgeries in this study were successfully completed, with no complications of permanent nerve injury. As shown in Table 2, the OLIF+AF group had a significantly shorter anesthesia time (132.5±23.4 min) and operation time (56.3±17.2 min), and less intraoperative blood loss (31.4±8.2 mL) and X-ray examination frequency (9.7±2.1) than the OLIF+PF group (183.5±42.7 min, 127.3±34.1 min, 75.1±14.3 mL, and 56.2±13.9, respectively; P<0.05). There was no significant difference in the duration of hospitalization between the 2 groups (8.4±1.6 days [OLIF+AF] vs 7.9±2.1 days [OLIF+PF], P<0.05). However, the OLIF+AF group was superior in terms of anesthesia time, operation time, intraoperative blood loss, and intraoperative X-ray examination.
Table 2.
Comparision of clinical data between OLIF+AF group and OLIF+PF group.
| OLIF+AF | OLIF+PF | p value | |
|---|---|---|---|
| Anesthesia time: minutes | 132.5±23.4 | 183.5±42.7 | p=0.000 |
| Operation time: minutes | 56.3±17.2 | 127.3±34.1 | p=0.000 |
| Intraoperative blood loss: ml | 31.4±8.2 | 75.1±14.3 | p=0.000 |
| Intraoperative X-ray examination: frequency | 9.7±2.1 | 56.2±13.9 | p=0.000 |
| Hospital stay: days | 8.4±1.6 | 7.9±2.1 | p=0.477 |
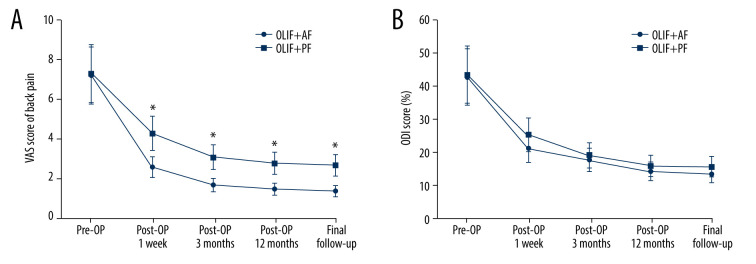
The preoperative VAS scores for the OLIF+AF group and the OLIF+PF group were similar (Figure 3A, P<0.05), with decreased scores from 7.2±1.6 and 7.3±1.7 before surgery to 1.4±0.3 and 2.7±0.5 at final follow-up, respectively. However, the OLIF+AF group reported significantly lower postoperative VAS scores for low back pain than did the OLIF+PF group (Figure 3A, P<0.05). The preoperative ODI scores for the OLIF+AF group and the OLIF+PF group were also similar, with improved scores from 42.7±3.4% and 43.4±2.7% before surgery to 13.4±1.9% and 15.6±1.5% at final follow-up, respectively. The differences in ODI scores during follow-up between the 2 groups were not significantly different (Figure 3B, P<0.05).
Figure 3. Clinical outcomes.
(A) Back pain Visual Analog Scale (VAS) scores of patients who received oblique lateral interbody fusion and either anterolateral screw fixation or posterior percutaneous screw fixation before surgery, 1 week, 3 months, and 12 months after surgery, and at the final follow-up (* P<0.05). (B) Oswestry Disability Index (ODI) scores of patients who received oblique lateral interbody fusion and either anterolateral screw fixation or posterior percutaneous screw fixation before surgery, 1 week, 3 months, and 12 months after surgery, and at the final follow-up (* P<0.05).
Radiological Outcomes
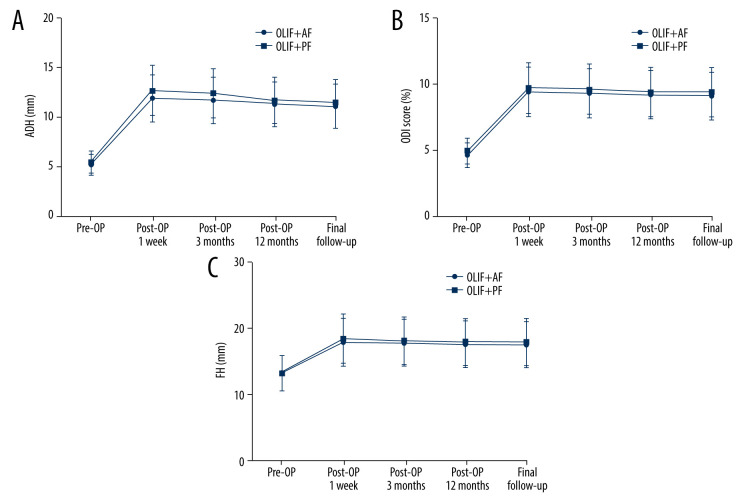
There were no significant differences between the OLIF+AF and OLIF+PF groups in terms of preoperative ADH (5.2±1.3 mm vs 5.5±1.4 mm), PDH (4.6±1.7 mm vs 4.9±1.6 mm), and FH (13.2±2.3 mm vs 13.2±2.7 mm), respectively (Figure 4, P<0.05). There were also no significant differences between the OLIF+AF and OLIF+PF groups in terms of ADH (11.3±1.4 mm vs 11.5±1.9 mm), PDH (9.1±1.6 mm vs 9.4±1.5 mm), and FH (17.5±2.7 mm vs 17.9±2.8 mm) at final follow-up. All postoperative radiographic outcomes, including the ADH, PDH, and FH, were also similar between the OLIF+AF group and the OLIF+PF group (Figures 4–6, P<0.05). The fusion rates in the OLIF+AF and OLIF+PF groups were 87.5% (21/24) and 92.6% (25/27), respectively, showing no significant differences (Figure 7 and Table 3, P<0.05). These results indicated that the AF produces the same radiological outcomes as PF in treating single-segment mild degenerative lumbar diseases.
Figure 4. Radiological outcomes.
(A) Anterior disc height (ADH) of patients who received oblique lateral interbody fusion and either anterolateral screw fixation or posterior percutaneous screw fixation before surgery, 1 week, 3 months, and 12 months after surgery, and at the final follow-up. (B) Posterior disc height (PDH) of patients who received oblique lateral interbody fusion and either anterolateral screw fixation or posterior percutaneous screw fixation before surgery, 1 week, 3 months, and 12 months after surgery, and at the final follow-up. (C) Foraminal height (FH) of patients who received oblique lateral interbody fusion and either anterolateral screw fixation or posterior percutaneous screw fixation before surgery, 1 week, 3 months, and 12 months after surgery, and at the final follow-up.
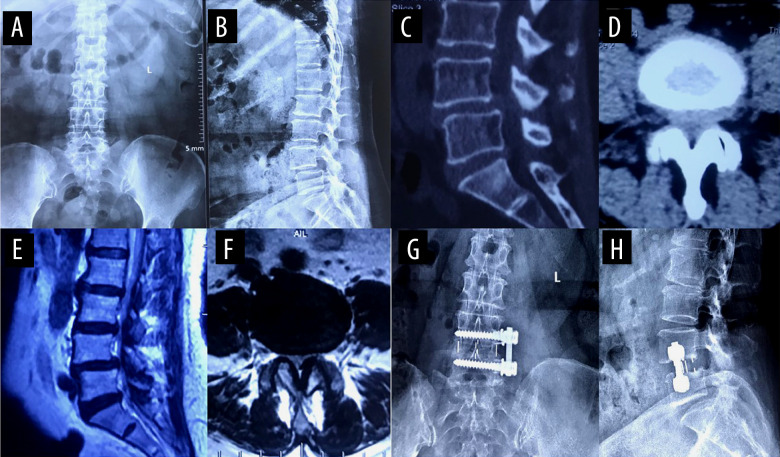
Figure 5. A typical case of oblique lateral interbody fusion with anterolateral screw fixation (OLIF+AF).
A 65-year-old woman had low back pain for 4 years, aggravated for 3 months. OLIF+AF was employed to treat lumbar spondylolisthesis at L4/5. (A) Preoperative anteroposterior radiograph. (B) Preoperative lateral radiograph shows L4 vertebral body I° anterior spondylolisthesis and loss of intervertebral disc height at L4/5. Before surgery, the anterior disc height (ADH) was 5.3 mm, the posterior disc height (PDH) was 4.9 mm, and the foraminal height (FH) was 13.2 mm. (C) Preoperative sagittal computed tomography (CT). (D) Preoperative cross-section CT shows disc herniation, obvious proliferation of the ligamentum flavum, and spinal canal stenosis at L4/5. (E) Preoperative sagittal magnetic resonance imaging (MRI). (F) Preoperative cross-section MRI shows disc herniation, obvious proliferation of the ligamentum flavum, and spinal canal stenosis at L4/5. (G) Postoperative anteroposterior radiograph. (H) Postoperative lateral radiograph shows the intervertebral cage at L4/5 was well in place, and the ADH, PDH, and FH were significantly increased. After surgery, the ADH was 10.4 mm, the PDH was 9.7 mm, and the FH was 18.3 mm.
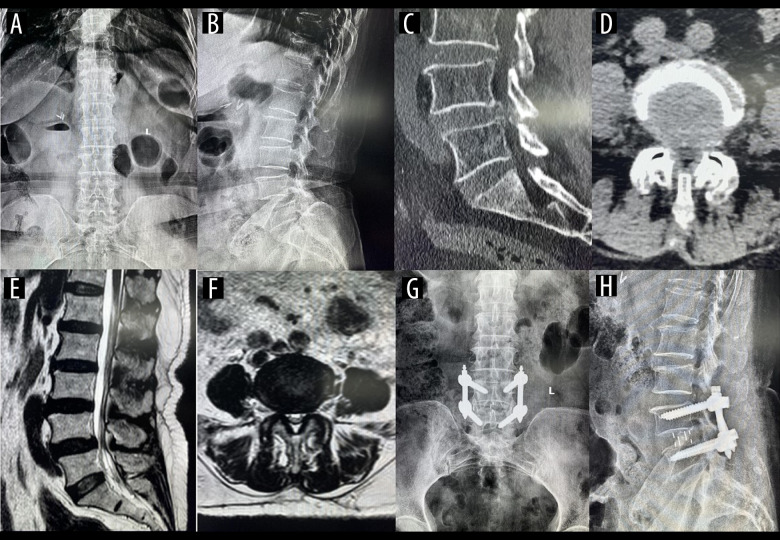
Figure 6. A typical case of oblique lateral interbody fusion with percutaneous pedicle screw fixation (OLIF+PF).
A 57-year-old man had low back pain for 3 years, aggravated for 5 months. OLIF+PF was employed to treat lumbar spondylolisthesis at L4/5. (A) Preoperative anteroposterior radiograph. (B) Preoperative lateral radiograph shows L4 vertebral body I° anterior spondylolisthesis and loss of intervertebral disc height at L4/5. Before surgery, the anterior disc height (ADH) was 5.7 mm, the posterior disc height (PDH) was 5.1 mm, and the foraminal height (FH) was 13.9 mm. (C) Preoperative sagittal computed tomography (CT). (D) Preoperative cross-section CT shows disc herniation, obvious proliferation of the ligamentum flavum, and spinal canal stenosis at L4/5. (E) Preoperative sagittal magnetic resonance imaging (MRI). (F) Preoperative cross-section MRI shows disc herniation, obvious proliferation of the ligamentum flavum, and spinal canal stenosis at L4/5. (G) Postoperative anteroposterior radiograph. (H) Postoperative lateral radiograph shows the intervertebral cage at L4/5 was well in place, and the ADH, PDH, and FH were significantly increased. After surgery, the ADH was 11.2 mm, the PDH was 10.5 mm, and the FH was 19.1 mm.
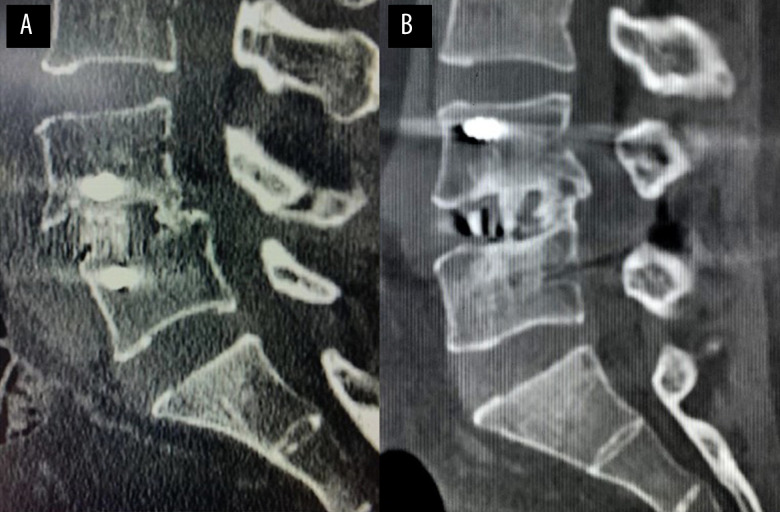
Figure 7. The typical case of postoperative fusion in the OLIF+AF and OLIF+PF groups.
(A) Postoperative sagittal computed tomography (CT) in OLIF+AF case shows intervertebral fusion with trabeculae reconstruction and no lucencies at the top or bottom of the graft at L4/5. (B) Postoperative sagittal CT in OLIF+PF case shows intervertebral fusion with trabeculae reconstruction and no lucencies at the top or bottom of the graft at L4/5.
Table 3.
Comparision of fusion rate between OLIF+AF group and OLIF+PF group.
| OLIF+AF | OLIF+PF | p value | |
|---|---|---|---|
| Total fusion rate | 21/24 (87.5%) | 25/27 (92.6%) | p=0.706 |
| Grade I | 18 | 21 | |
| Grade II | 3 | 4 | |
| Grade III | 3 | 2 | |
| Grade IV | 0 | 0 |
Complications
There were no vascular, ureteral, lumbar plexus, sympathetic nerve, and abdominal organ injuries or other serious complications in both groups (Table 4). In the OLIF+AF group, the incidence of complications was 45.8% (11/24). One patient experienced incomplete paralytic intestinal obstruction after surgery but recovered after fasting and water intake for 3 days. Postoperative pain in the donor bone area was observed in 4 patients, which disappeared within 1 month after symptomatic treatment. Postoperative anterior thigh pain and numbness and weakness in the psoas major and/or quadriceps femoris muscles were observed in 2 and 1 patients, respectively, all of which spontaneously resolved within 2 months after surgery without special treatment. There were 2 cases of cage subsidence, both observed in patients with high BMI. In the OLIF+PF group, 48.1% (13/27) of patients had complications. There were 2 cases of screw malposition, which were adjusted intraoperatively. Postoperative pain in the donor bone area was observed in 5 patients, which disappeared within 1 month after symptomatic treatment. Postoperative anterior thigh pain and numbness and weakness in psoas major and/or quadriceps femoris muscles were observed in 3 and 2 patients, respectively, all of which disappeared spontaneously within 2 months postoperatively without special treatment. One patient with a high BMI showed cage subsidence. Overall, the incidence of complications was similar between the 2 groups, without statistical significance (Table 4, P<0.05).
Table 4.
Comparision of complication between OLIF+AF group and OLIF+PF group.
| OLIF+AF | OLIF+PF | p value | |
|---|---|---|---|
| Total | 11 | 13 | 0.869 |
| Abdominal vascular injury | 0 | 0 | |
| Ventral dular tear | 0 | 0 | |
| Ureteral injury | 0 | 0 | |
| Sympathetic nerve injury | 0 | 0 | |
| Wound infection | 0 | 0 | |
| Screw malposition | 0 | 2 | 0.174 |
| Paralytic ileus | 1 | 0 | 0.284 |
| Donor site pain | 4 | 5 | 0.862 |
| Thigh pain/numbness | 3 | 3 | 0.878 |
| Iliopsoas/quadriceps weakness | 1 | 2 | 0.623 |
| Cage subsidence | 2 | 1 | 0.483 |
Discussion
OLIF is a new minimally invasive lumbar surgery proposed by Silvestre et al in 2012, which has been widely used in treating lumbar degenerative diseases [5]. The surgical approach in OLIF is between the psoas major muscle and the abdominal aorta, avoiding the risk of injury to the paravertebral muscle, psoas major muscle, and lumbar plexus nerve. OLIF provides adequate intervertebral space extension for indirect decompression by inserting with a wide cage, as well as less surgical trauma and intraoperative blood loss, and short operation time, hospital stay, and recovery time [6]. OLIF has become a new choice for spinal surgeons in the treatment of degenerative diseases of the lumbar spine. At present, OLIF with posterior percutaneous pedicle screw fixation (OLIF+PF) is widely used and can reconstruct spinal stability, restore the normal spinal sequence, and improve intervertebral fusion rates [7]. However, the combined procedure requires the intraoperative change of patient position, significantly increasing the operative time and amount of intraoperative bleeding and fluoroscopy [8]. To reduce these problems, some scholars have proposed OLIF with anterolateral screw fixation (OLIF+AF) instead for treating lumbar degenerative diseases. Because the cage used in OLIF is larger and spans the bilateral epiphyseal ring, the stability of the fixation interface is significantly enhanced so that the effective fixation strength can be achieved with lateral screw-assisted fixation of the vertebral body [9,10]. This study aimed to investigate the feasibility and safety of OLIF+AF in treating lumbar degenerative diseases, compared with OLIF+PF.
Single-level lumbar degenerative disease of L2–3, L3–4, and L4–5, which have similar structural and biomechanical characteristics and provide adequate operation windows for OLIF, were included in the present study. For the limitation of the rib arch and iliac crest, the applications of OLIF in L1–2 level and L5–S1 level do not have enough operation window and were excluded from the study. In addition, it is known that the decompression effect of OLIF on nerve roots are indirect; therefore, the indications of OLIF are limited. Indications of OLIF are mild degenerative lumbar diseases with low back pain, such as mild lumbar spondylolisthesis (Meyerding spondylolisthesis grades I–II), discogenic low back pain, and lumbar instability. Severe degenerative lumbar diseases with radiculopathy, such as severe lumbar spondylolisthesis (Meyerding grades III–IV), large free disc herniation, and severe lumbar spinal stenosis, are not good indications of OLIF [5,6]. Treatment of severe degenerative disease with OLIF will fail to achieve surgical efficacy and relieve symptoms; therefore, we excluded severe degenerative lumbar diseases in the study. To ensure surgical efficacy, we included mild degenerative lumbar diseases with low back pain and excluded severe degenerative lumbar diseases in the study.
OLIF has the advantages of a small incision, short operation time, and less bleeding. Silvestre et al retrospectively analyzed the data of 179 patients treated with OLIF, showing an average intraoperative blood loss, operative time, and hospital stay of 57 mL, 32.5 min, and 7.1 days, respectively. Woods et al reported an average intraoperative blood loss of 83.2 mL (range, 10–300 mL) in 137 patients treated with OLIF, and Ohtori et al reported an average operative time and intraoperative blood loss of 350 min and 350 mL, respectively, in 12 patients with scoliosis treated with OLIF [13]. The operative time and intraoperative blood losses reported above are significantly different, which may be attributed to differences in conditions and in the skill levels of the surgeons. In the present study, we were able to complete screw placement with OLIF+AF under direct vision at the same incision, avoiding intraoperative postural changes and frequent intraoperative fluoroscopies. There was no difference in hospital stay between the 2 groups. However, the anesthesia time, operation time, intraoperative blood loss, and intraoperative fluoroscopy times of OLIF+AF were better than those of OLIF+PF.
After removing the intervertebral disc tissue via the anterior approach, a sufficient size cage was placed. OLIF can increase the intervertebral space, FHs, and the central canal area by applying tension between the annulus fibrosus, ligamentum flavum, and posterior longitudinal ligament, achieving indirect decompression [14,15]. It has been reported that after OLIF, the intervertebral space height, intervertebral foramen area, and vertebral canal area can increase by 42% to 89%, 25% to 66%, and 30% to 43%, respectively [16,17]. Sato et al performed OLIF on 20 patients with lumbar degenerative diseases, showing a satisfactory postoperative clinical effect, with the intervertebral space height and vertebral canal diameter increased by 61% and 21%, respectively [11]. In their study, intervertebral space height, foramina height, and anteroposterior diameter of the thecal sac were significantly increased after surgery in both groups. However, there were no significant differences between the groups in terms of these variables, suggesting that OLIF+AF can maintain stability after lumbar fusion and achieve similar imaging outcomes as OLIF+PF.
In the present study, we found that the postoperative VAS and ODI scores of both groups improved, compared with their corresponding preoperative scores. There was no statistical difference in ODI scores between the groups. However, the postoperative VAS score in the OLIF+AF group was significantly better than that in the OLIF+PF group, confirming the importance of paravertebral muscle injury reduction for postoperative rehabilitation of patients in terms of minimally invasive surgeries. Postoperative paravertebral muscle atrophy is closely related to paravertebral muscle denervation and postoperative residual low back pain [18]. OLIF+PF requires incision of the paravertebral muscle for screw positioning, inevitably leading to paravertebral muscle injury and denervation, and subsequent failure of lumbar surgery in some patients. In contrast, OLIF+AF does not require paravertebral muscle dissection, leading to the significantly lower postoperative VAS score.
OLIF in the space between the psoas major muscle and the greater vessels reduces the risk of injury to the psoas major muscle and the lumbar plexus, avoiding damage to the posterior structure of the lumbar spine and injury to the spinal canal. However, some intraoperative complications can occur, such as great vessel, ureter, lumbar plexus, sympathetic nerve, and abdominal organ injuries [19,20]. According to the study of Fujibayashi et al, the complication rate of OLIF was 15.3%, with the most common complications being sensory nerve injury and psoas major weakness, most of which gradually resolved spontaneously [21]. According to the results of a multi-center retrospective study by Abe et al, the incidence of complications in OLIF was 48.3%, most of which were surgery-related and usually self-limiting. The most common complications were endplate injury collapse (18.7%) and temporary psoas major muscle weakness and thigh numbness (13.5%). The incidence of serious surgical complications, such as vascular, nerve, and ureteral injuries, in OLIF was lower (1.9%) [6].
In the present study, the absence of postoperative injuries and other serious complications as well as the similar incidence of complications in the 2 groups indicates that the safety of the 2 procedures is similar. There were 3 cases of cage subsidence (2 and 1 in the OLIF+AF and OLIF+PF groups, respectively), all of which were in patients with a high BMI. Therefore, a high BMI may be a factor affecting cage subsidence, and further studies are needed to prove this. Biomechanical stability may influence interbody fusion rate [22]. St Clair et al conducted a biomechanical experimental study after OLIF on cadaver specimens and obtained dynamic and static biomechanical data. They found that the biomechanical properties of the lumbar spine after OLIF were similar to those of the normal lumbar spine, but that activity decreased by more than 50%, indicating that the interbody fusion was stable enough to withstand the exercise load [23]. Biomechanical studies of the artificial intervertebral disc showed that the cages with a larger contact area with the endplate were more consistent with physiological stress distribution. Compared with the cage implanted in traditional interbody fusion, the OLIF-implanted cage was taller, and its cross-sectional area was several times larger than that of the common cage, increasing the contact area with the endplate. Moreover, it plays a role in supporting the interbody axial pressure of the interbody, stabilizing the anterior and central spinal columns, providing a good environment for interbody fusion, and improving the interbody fusion rate [24,25]. We found that OLIF+AF produced slightly lower fusion rates than OLIF+PF, with no significant difference. However, this indicates that OLIF+PF may be better in terms of stability and interbody fusion promotion. It is possible that the follow-up period was not long enough to detect a significant change in fusion rates. It may also be due to the inability of anterior vertebral fixation to effectively avoid lumbar spinal lateral flexion and extension. Therefore, it is recommended to routinely monitor the waist circumference as well as avoid lateral flexion and extension activities within 3 months after surgery.
Limitations
This study analyzed the clinical efficacy, technical safety, early clinical results, and complications of OLIF in 51 patients treated at a single center and had the following limitations: (1) the retrospective study design made it difficult to avoid selective bias; (2) L2–L5 single-level lumbar degenerative diseases were included in the study and were not the same segment; the different segments may affect the parameters, complications, and outcome analysis and evaluation of OLIF; (3) the number of samples was small, and the follow-up time was short; and (4) the improvement in early patients with low back pain was obvious, but assessing long-term clinical effects needs further follow-up, which can be performed in a multi-center systematic study with a large sample size.
Conclusions
Our study suggests that OLIF+AF in treating single-segment mild degenerative lumbar diseases produces the same radiological outcomes, ODI scores, and incidence of complications as those in OLIF+PF. However, compared with posterior percutaneous screw fixation, anterolateral screw fixation reduces anesthesia and operation times, bleeding, fluoroscopy time, trauma, and postoperative residual back pain. On the premise that the indications for fixation are strictly followed, OLIF+AF is a feasible treatment method for single-segment mild degenerative lumbar diseases, with good short-term efficacy. The checking of long-term effects still warrants further follow-up and future studies with a large number of cases.
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Abbreviations
- OLIF
oblique lateral interbody fusion
- OLIF+AF
OLIF with anterolateral screw fixation
- OLIF+PF
OLIF with posterior percutaneous screw fixation
- XLIF/DLIF
lateral lumbar interbody fusion
- BMD
bone mass density
- BMI
body mass index
- CT
computed tomography
- MRI
magnetic resonance imaging
- VAS
Visual Analog Scale
- ODI
Oswestry Disability Index
- ADH
anterior disc height
- PDH
posterior disc height
- FH
foraminal height
Footnotes
Conflict of interest: None declared
Ethics Approval
The study protocol was approved by the Ethics Committee of Hong Hui Hospital, Xi’an Jiao Tong University (no. 202105001). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part
Financial support: This study was supported by the National Natural Science Foundation of China (no. 81502330 and 81601938), the Natural Science Foundation of Shannxi Province (no. 2020JM-687), and the Science and Technology Plan of Xi’an City (no. 2020yb35)
References
- 1.Nasi D, Dobran M, Pavesi G. The efficacy of postoperative bracing after spine surgery for lumbar degenerative diseases: A systematic review. Eur Spine J. 2020;29(2):321–31. doi: 10.1007/s00586-019-06202-y. [DOI] [PubMed] [Google Scholar]
- 2.Lan T, Hu SY, Zhang YT, et al. Comparison between posterior lumbar interbody fusion and transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: A systematic review and meta-analysis. World Neurosurg. 2018;112:86–93. doi: 10.1016/j.wneu.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion – systematic review and meta-analysis. Br J Neurosurg. 2015;29(5):705–11. doi: 10.3109/02688697.2015.1036838. [DOI] [PubMed] [Google Scholar]
- 4.Goz V, Weinreb JH, Schwab F, et al. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: An analysis of the Nationwide Inpatient Sample database. Spine J. 2014;14(9):2019–27. doi: 10.1016/j.spinee.2013.11.050. [DOI] [PubMed] [Google Scholar]
- 5.Silvestre C, Mac-Thiong JM, Hilmi R, et al. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 2012;6(2):89–97. doi: 10.4184/asj.2012.6.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abe K, Orita S, Mannoji C, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: Perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976) 2017;42(1):55–62. doi: 10.1097/BRS.0000000000001650. [DOI] [PubMed] [Google Scholar]
- 7.Li HJ, Ge DW, Zhang S, et al. Comparative study between mini-open TLIF via Wiltse’s approach and conventional open TLIF in lumbar degenerative diseases. Eur Rev Med Pharmacol Sci. 2018;22(1 Suppl):53–62. doi: 10.26355/eurrev_201807_15364. [DOI] [PubMed] [Google Scholar]
- 8.He W, He D, Sun Y, et al. Standalone oblique lateral interbody fusion vs. combined with percutaneous pedicle screw in spondylolisthesis. BMC Musculoskelet Disord. 2020;21(1):184. doi: 10.1186/s12891-020-03192-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xie T, Wang C, Yang Z, et al. Minimally invasive oblique lateral lumbar interbody fusion combined with anterolateral screw fixation for lumbar degenerative disc disease. World Neurosurg. 2020;135:e671–78. doi: 10.1016/j.wneu.2019.12.105. [DOI] [PubMed] [Google Scholar]
- 10.Liu J, Feng H. Oblique lateral interbody fusion (OLIF) with supplemental anterolateral screw and rod instrumentation: a preliminary clinical study. World Neurosurg. 2020;134:e944–50. doi: 10.1016/j.wneu.2019.11.046. [DOI] [PubMed] [Google Scholar]
- 11.Sato J, Ohtori S, Orita S, et al. Radiographic evaluation of indirect decompression of mini -open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. 2017;26(3):671–78. doi: 10.1007/s00586-015-4170-0. [DOI] [PubMed] [Google Scholar]
- 12.Bridwell KH, Lenke LG, McEnery KW, et al. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patient with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20(12):1410–18. [PubMed] [Google Scholar]
- 13.Ohtori S, Mannoji C, Orita S, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J. 2015;9(4):565–72. doi: 10.4184/asj.2015.9.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim KT, Jo DJ, Lee SH, Seo EM. Oblique retroperitoneal approach for lumbar interbody fusion from L1 to S1 in adult spinal deformity. Neurosurg Rev. 2018;41(1):355–63. doi: 10.1007/s10143-017-0927-8. [DOI] [PubMed] [Google Scholar]
- 15.Ohtori S, Orita S, Yamauchi K, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J. 2015;56(4):1051–59. doi: 10.3349/ymj.2015.56.4.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel RS, Suh SW, Kang SH, et al. The Radiologic and Clinical Outcomes of Oblique Lateral Interbody Fusion for Correction of Adult Degenerative Lumbar Deformity. Indian J Orthop. 2019;53(4):502–9. doi: 10.4103/ortho.IJOrtho_655_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujibayashi S, Hynes RA, Otsuki B, et al. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 2015;40(3):E175–82. doi: 10.1097/BRS.0000000000000703. [DOI] [PubMed] [Google Scholar]
- 18.Ross JS, Robertson JT, Frederickson RC, et al. Association between peridural scar and recurrent radicular pain after lumbar discectomy: Magnetic resonance evaluation. ADCON-L European Study Group. Neurosurgery. 1996;38(4):855–61. [PubMed] [Google Scholar]
- 19.Mehren C, Mayer HM, Zandanell C, et al. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res. 2016;474(9):2020–27. doi: 10.1007/s11999-016-4883-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li HM, Zhang RJ, Shen CL. Radiographic and clinical outcomes of oblique lateral interbody fusion versus minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease. World Neurosurg. 2019;122:e627–38. doi: 10.1016/j.wneu.2018.10.115. [DOI] [PubMed] [Google Scholar]
- 21.Fujibayashi S, Kawakami N, Asazuma T, et al. Complications associated with lateral interbody fusion: Nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine (Phila Pa 1976) 2017;42(19):1478–84. doi: 10.1097/BRS.0000000000002139. [DOI] [PubMed] [Google Scholar]
- 22.Sembrano JN, Yson SC, Horazdovsky RD, et al. Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: Analysis of sagittal contour change. Int J Spine Surg. 2015;9:16. doi: 10.14444/2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.St Clair S, Tan JS, Lieberman I. Oblique lumbar interbody fixation: A biomechanical study in human spines. J Spinal Disord Tech. 2012;25(4):183–89. doi: 10.1097/BSD.0b013e318211fc6b. [DOI] [PubMed] [Google Scholar]
- 24.Ko MJ, Park SW, Kim YB. Effect of cage in radiological differences between direct and oblique lateral interbody fusion techniques. J Korean Neurosurg Soc. 2019;62(4):432–41. doi: 10.3340/jkns.2018.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soriano-Baron H, Newcomb AGUS, Malhotra D, et al. Biomechanical effects of an oblique lumbar PEEK cage and posterior augmentation. World Neurosurg. 2019;126:e975–81. doi: 10.1016/j.wneu.2019.02.200. [DOI] [PubMed] [Google Scholar]