Abstract
Objectives:
To determine whether a text message reduces the severity of patient self-reported levels of pain and anxiety following initial placement of orthodontic appliances.
Materials and Methods:
Thirty-nine orthodontic patients were randomly assigned to one of two groups and matched for age, gender, and bracket type (self-ligating vs conventional). The subjects completed baseline questionnaires to ascertain their levels of pain and anxiety before initiating orthodontic treatment. Following the initial appointment, subjects completed the pain questionnaire and anxiety inventory at the same time daily for 1 week. One group received a structured text message showing concern and reassurance, while the second group served as a control and received no postprocedural communication.
Results:
There was a statistically significant difference in pain in relation to time between the text message group and the control group as it was demonstrated that demonstrated that compared with the text message group, mean pain intensity increased and selfreported discomfort was longer in the control group. Anxiety was determined to be at its peak the day following initial orthodontic appliance placement and gradually tapered off from that time point. No intergroup difference was noted when analyzing anxiety.
Conclusions:
This study demonstrated that a text message sent from an orthodontic office following initial appliance placement resulted in a lower level of patient's self-reported pain. Additionally, patient anxiety is at its peak the day following the initial appointment and decreases from that point forward.
Keywords: Text message, Pain, Anxiety
INTRODUCTION
The initial placement of orthodontic appliances can cause discomfort, and patients must undergo a number of substantial adaptations in a relatively short period of time. According to several investigations1–4 that examined factors deterring individuals from undergoing orthodontic treatment, it was reported that the pain related to orthodontic appliances appeared to be the primary complaint of patients, more notably in adults than in adolescents,5 and that this discomfort was a major determining factor for avoiding orthodontic treatment.6 It has been reported that pain intensity was greater following placement of an orthodontic arch wire than after routine dental extractions7 and that this discomfort could adversely affect patient compliance during treatment.8,9 From these studies,1–4 approximately 94% of patients experienced some amount of pain during orthodontic appliance wear and average pain reported, measured at time points varying from 1 week to several months following initial appliance placement, was 42 on a 100-mm visual analog scale.10,11 Scheurer et al.12 demonstrated that the amount of actual tissue injury is not the only factor determining the severity of the pain and that there may be only a mild association between the pain stimulus and the patient's response to that pain incitement. Other factors, including anxiety, could be a primary contributor to the severity of pain experienced following initial bonding as this relationship has been adequately demonstrated in both medicine and dentistry.13,14
It has also been suggested that there may be a difference between the amount of pain experienced when using self-ligating brackets as opposed to conventional brackets. For instance, some studies of short duration15,16 showed that patients treated with self-ligating brackets reported, on average, lower pain intensity. However, in a systematic review conducted by Fleming and Johal,17 it was concluded that insufficient evidence exists to make the claim that one bracket system results in lower perceived pain levels than another.17
Although not a new idea, the concept of bibliotherapy,18 defined as “an adjunct to psychological treatment that incorporates appropriate books or other written materials, usually intended to be read outside of psychotherapy sessions, into the treatment regiment,”18 emphasizes the power of the written word on the human psyche. It is believed that through active participation in one's treatment, behavioral attitudes can be shaped. Jamison and Scogin19 studied a group of 80 individuals undergoing treatment for psychiatric disorder. They divided this group in half and, as part of their treatment, instructed one group (experimental) to read a psychological “self-help” book, while the other group (control) refrained from the assigned reading. They reported that those in the experimental group demonstrated clinically significant improvement in their overall well-being simply by reading and gaining a greater understanding of their condition. Neurolinguistic programming,20 or NLP, is another concept showing the effect of words, from a positive and negative aspect, on one's internal dialogue and external communication as well as on our nervous system. The potent ability of words to both heal and harm cannot be denied.
It has been reported21 that a telephone call from a healthcare provider leads to a reduction in pain intensity and anxiety during the initial phases of comprehensive orthodontic treatment. Bartlett et al.21 showed that the mere act of a phone call placed to a patient in the hours following orthodontic appliance placement resulted in a statistically significant reduction in postprocedural pain and anxiety. It was further noted that the content of the call was irrelevant to the patient's self-reported pain and anxiety levels. Detailed phone calls such as this have been shown to be helpful in both dental22 and medical settings.23
The number of individuals using text message as their primary means of communication is at an all-time high, even outnumbering phone calls by a rate of nearly two to one.24 In a recent survey conducted by Nielsen, the American teenage population is sending and receiving an average of 3339 texts per month.24 That figure, established in 2010, is up 8% from the previous year, and one can only speculate that usage will grow at an even greater rate in the years to come.
The purpose of this study was to determine if there is a difference in self-reported pain and anxiety after initial placement of orthodontic appliances between patients who receive a postprocedural text message and those who receive no correspondence post appointment.
MATERIALS AND METHODS
This research protocol was approved by the Seton Hill University Institutional Review Board and was conducted on a convenience sample of 39 consecutively treated patients. Guidelines as described by CONSORT 201025 were followed, including consent forms that were completed by the subject and parent prior to participation. Inclusion criteria were patients between 10 and 18 years of age, access to a cellular telephone, orthodontic treatment with fixed maxillary edgewise appliances, no previous orthodontic treatment, no reported chronic usage of analgesic medications, and no pain-related pathology or disease. The text message group comprised 15 female and 5 male patients with a mean age of 12.6 years, while the control group included 10 female and 9 male patients with a mean age of 14.2 years. Race of subjects was white. In order to maintain a type I alpha risk of .05 and power of 80%, it was previously21 determined that 36 subjects would be needed in each of the two groups. Given the patient population that met this study's inclusion criteria and a timeline for this study, a sample size of 20 and 19 (text message and control group, respectively) subjects per group was achieved.
In accordance with CONSORT 201025 and randomized sequencing guidelines,26 subject group assignment was done by preassigning the first 20 subjects to either group 1 (text message) or group 2 (control). This random subject assignment that occurred for the first 20 individuals enrolled in the study was done in two groupings: the first group received a structured, standardized text message offering the patient encouragement and concern as to their well-being following initial treatment; the second group, serving as a control, received no text message.
Subjects were blinded as to group status and were not made aware that a text message was part of the study. The additional 19 study participants were then assigned to the experimental and control groups in an attempt to closely approximate the trial arms based on a minimization protocol as described by Pandis.26 Prognostic factors such as age, gender, and bracket type were taken into account when determining subject group assignment. Although all patients were bonded with fixed edgewise maxillary appliances, some variation of the initial arch wire may have occurred, and this was not accounted for during the minimization26 process. However, a systematic review conducted by Wang et al.27 concluded that patient discomfort does not appear to be significantly altered by the type or size of the initial aligning arch wire.
At the initial treatment appointment, a questionnaire was used to assess each subject's baseline level of pain. This questionnaire consisted of a number of inquiries, including whether the patient experienced any pain the day prior to initial bonding, the subject's current level of discomfort (as measured on a 100-mm visual analog scale), and the number of analgesics taken during the previous 24 hours. A similar questionnaire was filled out by the subjects at their homes approximately 4 hours after bonding and daily for the next 7 days.
In keeping consistent with the study protocol of Bartlett et al.,21 the Spielberger State-Trait Anxiety Inventory for Children (STAIC)28 was also completed by each subject at baseline and daily for 7 days following appliance placement. This questionnaire uses a three-point Likert scale to evaluate present levels of patient anxiety (state)28 in addition to examining other personality features (trait).28
Following initial placement of fixed edgewise maxillary appliances and aligning arch wires, patients received postoperative instructions and a reminder regarding how and when to fill out the aforementioned questionnaires. Since previous studies5,7 have reported average patient discomfort following initial archwire placement to last up to 5 days, a period of 1 week for analysis aptly covers that time frame and allows for individual patient variation. Patients were further instructed to avoid taking pain medication unless necessary.
RESULTS
All data were analyzed using SPSS version 19. Pain and state-anxiety were analyzed as 2 × 8R analysis of variance (ANOVA), and the total number of pain medications taken was analyzed using a Student's t-test for independent means.
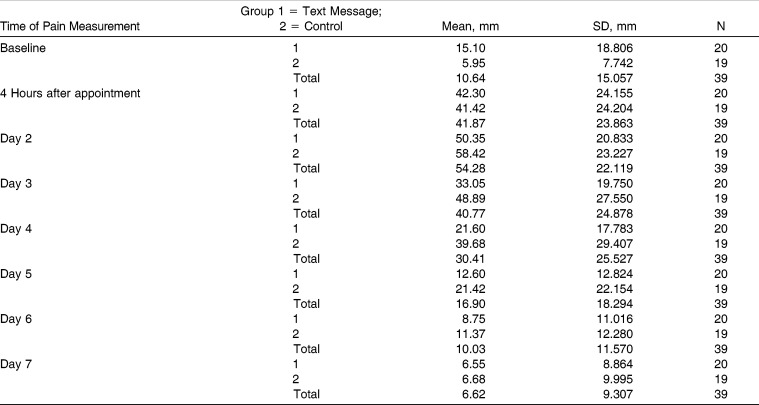
When following these subjects for a 7-day period after placement of the initial orthodontic appliance, both groups reported some degree of pain and anxiety. Upon comparison, the levels of overall self-reported pain changed depending on the group assignment (text message vs control) when using time as the comparative factor (F = 3.28, P = .002) (Figure 1; Table 1).
Figure 1.
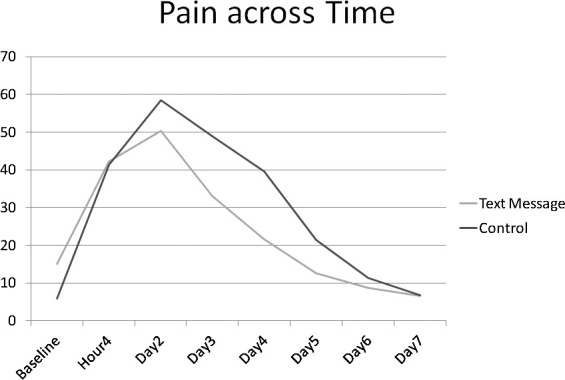
Mean pain measurements (in millimeters) of the text message and control groups over the 7-day trial period.
Table 1.
Pain vs Time Group Means and Standard Deviations
A Bonferroni post hoc analysis revealed that the control group reported statistically significant levels of pain that were greater (P < .05) at days 2, 3, 4, and 5, as compared to the text message group. The text group also reported a slightly greater amount of pain at baseline and 4 hours following initial appliance placement, but these measurements were reported prior to text message receipt and were not significantly different from the control group. Additionally, using time as a key comparative measurement, the text message group exhibited pain for a shorter period of time (Figure 1; Table 1).
Maximum mean pain intensity for both groups was at its highest level at day 2 as the text message group reported an average 50.35 mm and the control group reported an average of 58.42 (Figure 1; Table 1). At the time of maximum discomfort, it was shown that the text message group reported a 16% reduction in pain as compared to the controls, which was deemed statistically significant. Pain was also analyzed by looking at overall usage of analgesics during the 7-day period. No significant group differences were noted.
The Spielberger State-Trait Inventory was used to evaluate the differences in anxiety between the groups during the research period. State-anxiety was noted to be highest at day 2 and gradually decreased during days 4, 5, 6, and 7; however, post hoc analysis showed no significant differences from the perspective of an intergroup comparison (F = 1.907, P = .069) (Figure 2).
Figure 2.
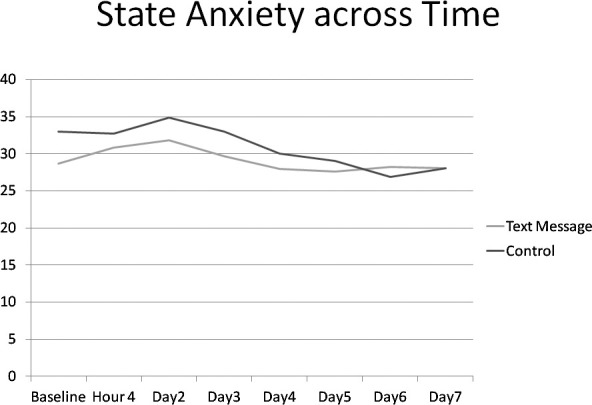
Mean anxiety measurements of the text message and control groups over the 7-day trial period.
DISCUSSION
The aim of this investigation was to evaluate whether the written word (text messaging) has the same impact as the spoken word (telephone call).21 To our knowledge, this was the first clinical trial comparing the effect of a text message on patients' self-reported levels of pain and anxiety. We found that a text message sent following initial appliance placement resulted in decreased perception of pain. This finding is similar to that reported by Bartlett et al.21 in which it was found that the mere act of a telephone call to patients following an initial orthodontic procedure resulted in reduced levels of pain. Our results differ from that study, however, in the fact that we did not find reduced levels of anxiety when comparing the text message and control groups.
The power of the spoken word, or in this instance the written word, appears invaluable when it comes to serving as a means of reducing the pain that may be experienced by patients when undergoing some form of medical-related procedure. Using this form of technology for communication purposes is not the only advantage, however. Text messaging was used recently as part of a smoking cessation program29 in which motivational messages were sent to a group of smokers and a control group. After a 6-month correspondence period, nearly double the number of individuals who received the text message quit smoking as opposed to those who did not receive any contact.
In recent years, e-mail has been used by orthodontic offices as either a replacement or adjunct to telephone calls as a means of patient appointment reminders. Given that virtually every cellular telephone has the ability to receive a text message, it would be reasonable to think that this may be the preferred method of communication while being cognizant of patient privacy as dictated by HIPAA. Furthermore, the number of individuals owning a cell phone is greater than the number of individuals owning a computer.24 Ease of usage and accessibility appear to be the key issues. Some might argue that texting is just for the teenage population, but that is not the case. On comparing individuals from Generation X (those born between the 1960s and 1980s) and Generation Y (those born between the 1980s and 2000s), reports state that 43% of those in Generation Y are texting daily, while 31% of Generation X have adopted this method of communication.24 Clearly, texting is not merely a youth movement.
Since introducing text confirmations into their patient reminder armamentarium, US communication company Televox has seen effective response rates ranging from 48%–61%, which, in comparison, was greater than that seen by phone and e-mail message reminders.24 In contrast, a study30 comparing the effectiveness of a text message to a voice reminder regarding patient appointments found that text messaging resulted in more than twice as many missed appointments. As both times and generations change, and based on current trending, one might expect that the number of individuals using text messaging as a primary means of correspondence will only grow.
Contact with the patient following initial placement of orthodontic archwires can serve as an effective means of alleviating a number of measures that cause undue pain, anxiety, and stress among orthodontic patients. Given that pain and discomfort are frequent accompaniments to a number of orthodontic procedures, the orthodontic professional and/or staff should make the patient as comfortable as possible. One way to accomplish this is via increased office-patient communication. In doing so, not only is treatment completed at a higher rate, but it is also finished with a greater degree of efficiency, compliance, and, most importantly, patient satisfaction.
In the conduction of any randomized controlled trial, a certain degree of bias, which is inherent in each study, exists. In order to maximize the reliability and validity of the results, it is imperative that the researchers attempt to minimize the influence various factors such as random error, bias, and confounding have on the trial's outcome. As delineated by Pandis,31 four types of bias are commonly discussed, and they include selection bias, performance bias, detection bias, and subject attrition (postrandomization bias). In this study, we attempted to account for each form in various manners. To ensure that proper statistical reporting was completed, all results were analyzed independently and computed by the university's statistical department.
Given the patient population that met this study's inclusion criteria and a timeline for this study, a sample size of 20 and 19 (text message and control group, respectively) subjects per group was achieved; however, a larger sample size would have been preferred in order to achieve an ideal type I alpha risk and power. This would have allowed for an increase in generalizability of this study's results. Future studies may look at using three groups: (1) text message follow-up, (2) phone call follow-up (to compare effectiveness of phone call vs text message), and (3) control group.
CONCLUSIONS
This study established that a text message sent from the orthodontic office following the initial appliance placement resulted in a lower level of self-reported pain.
It was also noted that patient anxiety is at its peak the day following the initial appointment and decreases from that point forward. Overall anxiety, however, did not change as a result of postprocedural communication.
REFERENCES
- 1.Sergl HG, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofacial Orthop. 1998;114:684–691. doi: 10.1016/s0889-5406(98)70201-x. [DOI] [PubMed] [Google Scholar]
- 2.Brattstrom V, Ingelsson M, Aberg E. Treatment co-operation in orthodontic patients. Br J Orthod. 1991;18:37–42. doi: 10.1179/bjo.18.1.37. [DOI] [PubMed] [Google Scholar]
- 3.Gosney MB. An investigation into factors which may deter patients from undergoing orthodontic treatment. Br J Orthod. 1985;12:133–138. doi: 10.1179/bjo.12.3.133. [DOI] [PubMed] [Google Scholar]
- 4.Tayer BH, Burek MJ. A survey of adults' attitudes toward orthodontic therapy. Am J Orthod. 1981;79:305–315. doi: 10.1016/0002-9416(81)90078-6. [DOI] [PubMed] [Google Scholar]
- 5.Jones ML. An investigation into the initial discomfort caused by placement of an arch wire. Eur J Orthod. 1984;6:48–54. doi: 10.1093/ejo/6.1.48. [DOI] [PubMed] [Google Scholar]
- 6.Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–188. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 7.Jones M, Chan C. The pain and discomfort during orthodontic treatment: a randomized controlled clinical trial of two aligning arch wires. Am J Orthod Dentofacial Orthop. 1992;102:373–381. doi: 10.1016/0889-5406(92)70054-e. [DOI] [PubMed] [Google Scholar]
- 8.White LW. Toothbrush pressures of orthodontic patients. Am J Orthod. 1983;83:109–113. doi: 10.1016/s0002-9416(83)90295-6. [DOI] [PubMed] [Google Scholar]
- 9.White LW. Pain and cooperation in orthodontic treatment. J Clin Orthod. 1984;18:572–575. [PubMed] [Google Scholar]
- 10.Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–188. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 11.Kvam E, Gjerdet NR, Bondevik O. Traumatic ulcers and pain during orthodontic treatment. Community Dent Oral Epidemiol. 1987;15:104–107. doi: 10.1111/j.1600-0528.1987.tb00493.x. [DOI] [PubMed] [Google Scholar]
- 12.Scheurer PA, Firestone AR, Burgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–357. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 13.Litt MD. A model of pain and anxiety associated with acute stressors: distress in dental procedures. Behav Res Ther. 1996;34:459–476. doi: 10.1016/0005-7967(96)00015-0. [DOI] [PubMed] [Google Scholar]
- 14.Van Buren J, Kleinknecht R. An evaluation of the McGill pain questionnaire for use in dental pain assessment. Pain. 1979;6:23–33. doi: 10.1016/0304-3959(79)90137-4. [DOI] [PubMed] [Google Scholar]
- 15.Tecco S, D'Attilio M, Tete S, Festa F. Prevalence and type of pain during conventional and self-ligating orthodontic treatment. Eur J Orthod. 2009;31:380–384. doi: 10.1093/ejo/cjp003. [DOI] [PubMed] [Google Scholar]
- 16.Pringle AM, Petrie A, Cunningham SJ. Prospective randomized clinical trial to compare pain levels associated with 2 orthodontic fixed bracket systems. Am J Orthod Dentofacial Orthop. 2009;136:160–167. doi: 10.1016/j.ajodo.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 17.Fleming PS, Johal A. Self-ligating brackets in orthodontics: a systematic review. Angle Orthod. 2010;80:575–584. doi: 10.2319/081009-454.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fitzgerald J. Bibliotherapy. Encyclopedia of Mental Disorders. Available at: http://www.minddisorders.com/A-Br/Bibliotherapy.html Accessed May 3, 2012. [Google Scholar]
- 19.Jamison C, Scogin F. The outcome of cognitive bibliotherapy with depressed adults. J Consult Clin Psychol. 1995;63:644–650. doi: 10.1037//0022-006x.63.4.644. [DOI] [PubMed] [Google Scholar]
- 20.Grinder J, Bandler R. The Structure of Magic A Book About Language and Therapy. Palo Alto, Calif: Science and Behavior Books; 1975. [Google Scholar]
- 21.Bartlett BW, Firestone AR, Vig KWL, Beck FM, Marucha PT. The influence of a structured telephone call on orthodontic pain and anxiety. Am J Orthod Dentofacial Orthop. 2005;128:435–441. doi: 10.1016/j.ajodo.2004.06.033. [DOI] [PubMed] [Google Scholar]
- 22.Martinez-Urratia A. Anxiety and pain in surgical patients. J Consult Clin Psychol. 1975;43:437–442. doi: 10.1037/h0076898. [DOI] [PubMed] [Google Scholar]
- 23.Greenhouse DL, Probst JC. After-hours telephone calls in a family practice residency: volume, seriousness, and patient satisfaction. Fam Med. 1995;27:525–530. [PubMed] [Google Scholar]
- 24.Hamilton JY. Orthodontists shd B txtN Patients. The Progressive Orthodontist. 2011;Q2:42–44. [Google Scholar]
- 25.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trial. BMJ. 2010;340:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandis N. Randomization. Part 1: sequence generation. Am J Orthod Dentofacial Orthop. 2011;140:747–748. doi: 10.1016/j.ajodo.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 27.Wang Y, Jian F, Lai W, et al. Initial arch wires for alignment of crooked teeth with fixed orthodontic braces. Cochrane Database Syst Rev. 2010;(4):CD007859. doi: 10.1002/14651858.CD007859.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Spielberger C, Gorsuch R, Lushene R, Vagg R, Jacobs G. STAI Manual for the StateTrait Anxiety Inventory (Form Y) Palo Alto, Calif: Consulting Psychologists Press; 1983. [Google Scholar]
- 29.Free C, Knight R, Robertson S, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet. 2011;378:49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nelson TM, Berg JH, Bell JF, Leggott PJ, Seminario AL. Assessing the effectiveness of text messages as appointment reminders in a pediatric dental setting. J Am Dent Assoc. 2011;142:397–405. doi: 10.14219/jada.archive.2011.0194. [DOI] [PubMed] [Google Scholar]
- 31.Pandis N. Sources of bias in clinical trials. Am J Orthod Dentofacial Orthop. 2011;140:595–596. doi: 10.1016/j.ajodo.2011.06.013. [DOI] [PubMed] [Google Scholar]