Abstract
Objective:
To evaluate longitudinal changes of the hyoid bone position and pharyngeal airway space after bimaxillary surgery in mandibular prognathism patients.
Materials and Methods:
Cone-beam computed tomography scans were taken for 25 mandibular prognathism patients before surgery (T0), 2 months after surgery (T1), and 6 months after surgery (T2). The positional displacement of the hyoid bone was assessed using the coordinates at T0, T1, and T2. Additionally, the volume of each subject's pharyngeal airway was measured.
Results:
The mean amount of posterior maxilla impaction was 3.76 ± 1.33 mm as the palatal plane rotated 2.04° ± 2.28° in a clockwise direction as a result of bimaxillary surgery. The hyoid bone moved backward (P < .05, P < .001) and downward (P > .05, P < .05) at 2 months and 6 months after surgery, while the total volume of the pharyngeal airway significantly decreased at the same time points (P < .001, P < .001). There was significant relationship between the changes of the hyoid bone position and airway volume at 2 months after surgery (P < .05). The change of the palatal plane angle was positively correlated to the decrease in the total airway volume (P < .001).
Conclusions:
The null hypothesis was rejected. The hyoid bone moved inferoposteriorly, and the pharyngeal airway volume decreased for up to 6 months after bimaxillary surgery. The decrease in the pharyngeal airway volume was correlated to the changes in the palatal plane inclination and the positional change of the hyoid bone.
Keywords: Hyoid bone, Pharyngeal airway, Orthognathic surgery, Skeletal Class III malocclusion, CBCT
INTRODUCTION
Treatment options for surgery in mandibular prognathism patients include single jaw surgery involving maxillary advancement or mandibular setback and double jaw surgery, in which the maxillomandibular complex undergoes rotational and horizontal changes.1,2 Currently, bimaxillary surgery has been preferred in those who have severe skeletal discrepancy because facial esthetic changes are often more favorable, treatment outcome is stable, and the respiratory anatomy is less affected in comparison with those who have undergone isolated mandibular setback surgery.3,4
The effect of bimaxillary surgery on respiratory function and its relationship with posttreatment stability have been controversial. The oropharyngeal complex consists of the hyoid bone, its connecting muscles, and the pharyngeal airway, and it undergoes significant changes after orthognathic surgery because it is anatomically and functionally associated with the jaws. Pharyngeal airway volume has been reported5 to decrease to a lesser amount following bimaxillary surgery, compared to results in those who have undergone mandibular setback surgery only. In addition, authors of previous studies1,6 reported that the anteroposterior dimension of the upper pharyngeal airway increases after bimaxillary surgery, which may have a minimal effect on reduction of the pharyngeal airway space.
The position of the hyoid bone is determined by supra- and infra-hyoid muscles and ligaments,7 and the hyoid bone does not articulate with any other bone.8 The hyoid bone has been reported to move inferoposteriorly after mandibular setback surgery, and this movement may be caused by the surrounding muscles compensating for the reduction in the oral volume and adapting physiologically to the soft tissue changes after the surgery.9,10 Several studies5,10–12 reported that mandibular setback surgery reduces the volume of the pharyngeal airway. However, as a result of physiologic adaptations of the soft tissues, the oropharyngeal complex reverts to its original condition during the retention period, and skeletal relapse has been observed.13,14 Therefore, conducting a positional assessment of the hyoid bone and maintaining the pharyngeal airway space are important for evaluating treatment changes and for predicting postoperative stability.15
To evaluate the positional and morphologic changes of the oropharyngeal complex following bimaxillary surgery, past studies8,10,12,16 have used two-dimensional (2D) imaging, in particular, lateral cephalographs. Although lateral cephalographs are useful for analyzing the airway measurements on the sagittal plane, they do not reflect the three-dimensional (3D) airway structure.15 Moreover, these images can provide only a limited assessment of hyoid bone position because of the difference between left and right magnification.17 Cone-beam computed tomography (CBCT) offers a more precise anatomical assessment through 3D reconstructed models and multi-planar reformatted views.5 Additionally, 3D volumetric images also provide visualization of the internal structures by eliminating the external structures,18 allowing for measurement of airway volume.19 With CBCT, it is possible to evaluate the changes in hyoid bone position by establishing the reference coordinates precisely.20
The purpose of this study was to evaluate the longitudinal changes in the hyoid bone position and the pharyngeal airway space following bimaxillary surgery in mandibular prognathism patients. Postsurgical changes were measured and compared at 2 and 6 months after surgery, and the relationship between changes of the hyoid bone and the pharyngeal airway volume was evaluated. In addition, the relationship among skeletal horizontal plane changes, airway volume, and hyoid bone position was evaluated. The null hypothesis was that the hyoid bone position and the pharyngeal airway volume do not change at 2 and 6 months after surgery.
MATERIALS AND METHODS
Twenty-five consecutive mandibular prognathism patients (14 men, 11 women; mean age, 30.04 ± 13.08 years; range, 17.2–48.1 years) who had undergone orthognathic surgery at the Kangdong Sacred Heart Hospital were included in this study. The ethics review committee at Kangdong Sacred Heart Hospital and the Hallym University Medical Center approved the study protocol (IRB12-1-011), and all patients provided informed consent. Diagnostic inclusion criteria were an overjet of 0 mm or less, a unilateral or bilateral Angle Class III molar relationship, and an ANB of 0° or less. Patients who had craniofacial syndromes, such as cleft lip and palate, and those with symptoms related to pharyngeal pathology or with a history of an adenoidectomy/tonsillectomy were excluded.
Surgical techniques were identical for all of the patients. After the LeFort I osteotomy, the posterior maxilla was impacted (mean, 3.76 ± 1.33 mm) by rotating it in a clockwise direction with a center of rotation at either the anterior nasal spine (ANS) or upper incisal tip, along with rigid fixation. The mean amount of maxillary advancement was measured based on the changes of ANS point in a 3D coordinate system. The mandible was set back (mean, 8.25 ± 2.12 mm) with a sagittal split osteotomy, and the proximal segment was stabilized by semirigid fixation. Nine of the patients had advancement genioplasty as an adjunctive procedure. To discriminate the possible effects of genioplasty, both the amount of setback and the positional changes of menton were calculated. Surgical wafers were placed for 3–4 weeks after surgery, and interarch elastics were used to stabilize the interarch relationship after removal of the surgical wafers. Postoperative orthodontic treatment was provided to all patients to achieve functional occlusion. After debonding, a circumferential retainer was placed in the upper arch, and a fixed retainer was applied on the lower arch for retention.
CBCT Image Acquisition
CBCT scans were acquired at an average of 2 weeks (range, 0–3 weeks) before surgery (T0) and again 2 months (range, 2–4 months) and 6 months (range, 5–8 months) after surgery (T2). CBCT volume scans of all subjects at Kangdong Sacred Heart Hospital were obtained using the Master 3D dental-imaging system (Vatech Inc, Seoul, South Korea), and the imaging protocol used a 19 cm × 20 cm in-field of view to include the entire craniofacial anatomy. The axial slice thickness was 0.3 mm, and the voxels were isotropic. All patients were sitting upright with a natural head position, and the jaws were at maximum intercuspation, with the lips and tongue in a resting position.21
Hyoid Bone Position and Airway Parameters
The digital image files were exported using the Digital Imaging and Communications in Medicine (DICOM) format and imported into the InVivoDental 3D imaging software (Anatomage, San Jose, Calif). Because the airway volume and hyoid bone position are influenced by the head posture,9 angulation of the Frankfort Horizontal (FH) plane in reference to the true vertical line of all scans was recorded to see if there were any significant changes in the head posture.22 Each 3D-rendered image was then reoriented using the FH plane as its horizontal reference plane, which was constructed from right and left poria that are located in the most laterosuperior point of the external auditory meatus and the right orbital, the most inferior point of the lower margin of the bony orbit.
A 3D coordinate system was used to determine the positional changes of the hyoid bone. The nasion was set as the origin, and the coordinates of the most anterosuperior point of the hyoid bone (Hb) were identified in pre- and postoperative 3D models of the patients (Figure 1). Volumetric analysis of the airway was performed by isolating the upper pharyngeal airway (Figure 2).5 Because the airway is a void space surrounded by hard and soft tissues, an inversion of the 3D-rendered image was taken to convert a negative value to a positive value, and vice versa. A targeted airway section was isolated by removing unnecessary structures, such as the paranasal sinuses; subsequently, threshold values were set at a range of −1024 to −300 Hounsfield units to eliminate imaging artifacts and to refine the selected airway region. Finally, the volume of the designated airway was calculated in cubic millimeters.
Figure 1.
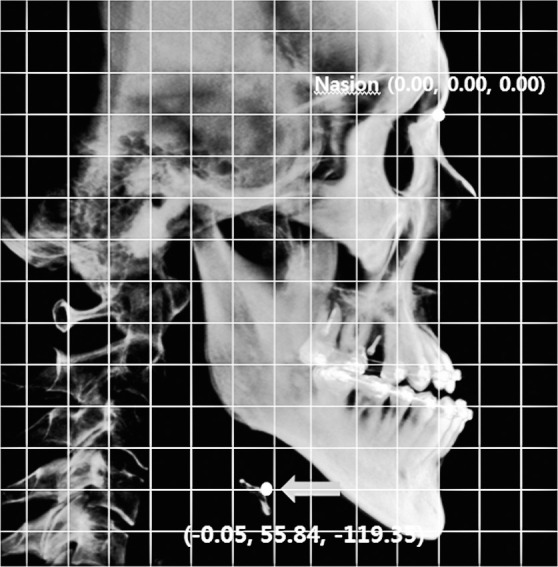
Measurement of hyoid bone position. Nasion was set up as a reference point. The coordinate of the most anterosuperior point of the hyoid bone (Hb) was marked.
Figure 2.
Volumetric measurements of pharyngeal airway space. (A) Reference planes: A, posterior nasal spine (PNS) plane (axial plane passing through PNS); B, soft palate plane (axial plane passing through most inferior point of soft palate); and C, epiglottis plane (axial plane passing through base of epiglottis on anterior pharyngeal wall). (B) ‘a’ indicates the naso-pharyngeal airway; ‘b’ indicates the oro-pharyngeal airway; and; ‘c’ indicates the hypo-pharyngeal airway. The red arrows indicating the borders were planes through the PNS and the most inferior point of the soft palate parallel to the Frankfort Horizontal plane.
Skeletal Horizontal Planes
We measured horizontal plane angles on 2D cephalometric images derived from the reoriented 3D images using InVivoDental software.23 Palatal plane angle was defined as the angle formed by the FH plane and the line through ANS and posterior nasal spine (PNS). Occlusal plane angle was formed by the FH plane and the line through the midpoint of the maxillomandibular central incisors and the intersection point of the first molars of maxilla and mandible on the midsagittal plane. Finally, the mandibular plane angle was defined as the angle by the FH plane and the line through the menton and the most inferoposterior point of the gonial angle.24
Statistical Analysis
SPSS 17.0 software for Windows (SPSS Inc, Chicago, Ill) was used for all statistical analyses. To evaluate the systemic error of the employed method, 10 CBCT scans were randomly selected and measured two times on each scan by the same investigator. A paired t-test was used. The random error for the measurements was calculated with Dahlberg's formula (Standard error = ∑d2/2n), where d is the difference between the repeated measurements and n is the number of double recordings.25
Descriptive statistics were calculated, including the mean and standard deviations for each group. The Wilcoxon signed-rank test was used to assess the significant differences among the head positions at every CBCT scan time point. Additionally, this test was used to compare the preoperative changes with the 2- and 6-month postoperative changes. The Spearman's correlation coefficient was determined to obtain the correlation among the changes in horizontal plane angles, the hyoid bone position, and the pharyngeal airway volume. A P value of less than .05 was considered significant for all of the analyses.
All of the measurements were free of any systemic error. The random error varied from 1054.47 to 1418.88 mm3 for the volumetric measurements.
RESULTS
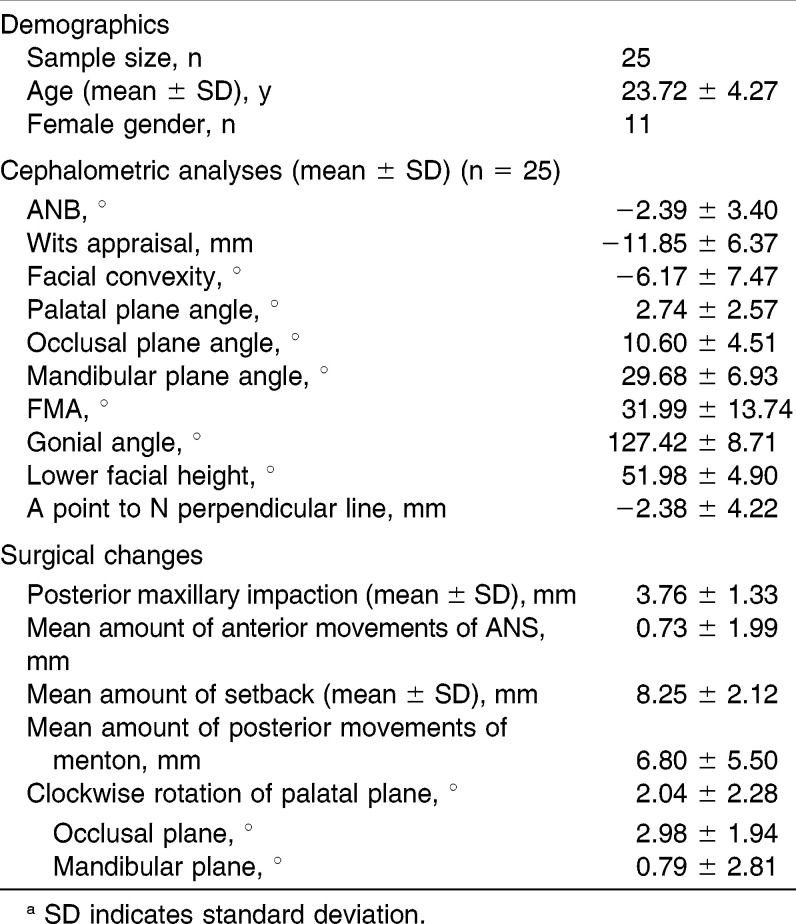
Sample Characteristics and Surgical Changes
The head postures of each patient at T0, T1, and T2 were not significantly different. As a result of surgery, the posterior maxilla was impacted 3.76 ± 1.33 mm as the mean amount of advancement of ANS was 0.79 ± 1.99 mm. The mean amount of mandibular setback was 8.25 ± 2.12 mm, while menton shifted 6.80 ± 5.50 mm posteriorly. Other sample characteristics and the mean amount of clockwise rotation of the horizontal planes are shown in Table 1.
Table 1.
Sample Characteristics and Surgical Changesa
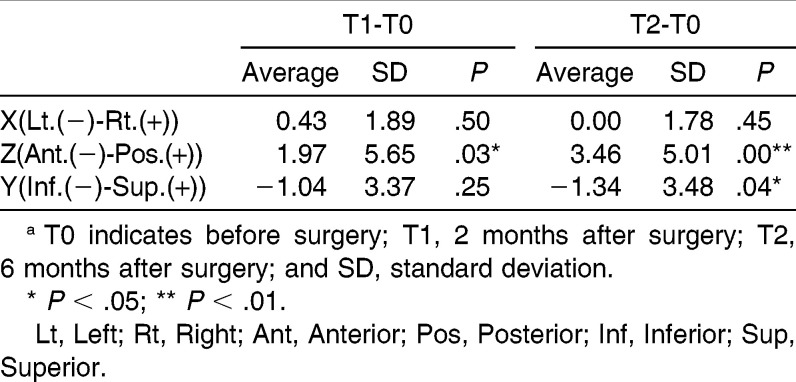
Positional Changes of the Hyoid Bone
At 2 months after surgery, the hyoid bone showed a posterior displacement of 1.97 ± 5.65 mm. However, at 6 months after surgery, the hyoid bone moved more posteriorly and was located 3.46 ± 5.01 mm posterior to the presurgical position. In addition, an inferior movement of 1.34 ± 3.48 mm was observed (Table 2).
Table 2.
Displacement of Hyoid Bone in X, Y, and Z Axes (mm)a
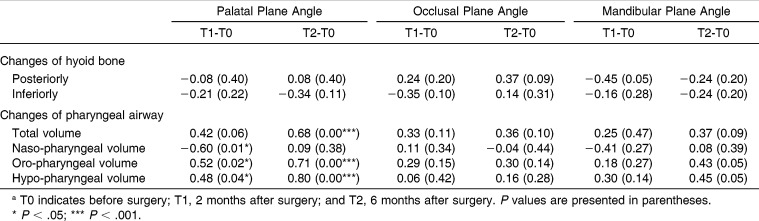
Changes in Pharyngeal Airway Measurements
The total volume of the upper pharyngeal airway significantly decreased from T0 to T1 and T2. Of the three subregions of the airway, the naso- and hypo-pharyngeal airway volume decreased at 2 months and 6 months after surgery (P < .05), but the oro-pharyngeal airway showed no significant changes in volume (P > .05; Table 3).
Table 3.
Changes in Airway Volume Before (T0) and 2 Months (T1) and 6 Months (T2) After Surgery (mm3)a
The Relationship Among Skeletal Changes, Airway, and Hyoid Bone Position
The Spearman's correlation coefficient was performed to discover any significant relationships among horizontal plane changes, airway volumes, and hyoid bone displacements (Table 4). The changes in the palatal plane angle were positively correlated to those in the pharyngeal airway volume at 6 months after surgery (P < .001). The changes in pharyngeal airway volume did not relate to those in the occlusal plane and mandibular plane angles (P > .05).
Table 4.
Correlation With Inferoposterior Changes of Hyoid Bone Position, Changes in Airway Volume, and Those of Palatal, Occlusal, and Mandibular Plane Angle (n = 25)a
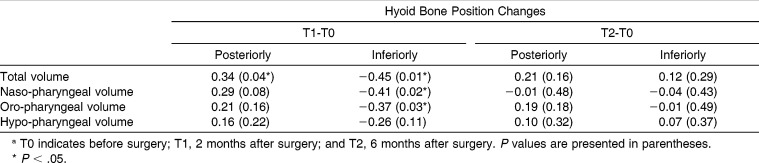
Significant correlations between the hyoid position and airway volume were observed only at 2 months after surgery. The changes in the total pharyngeal airway volume were positively correlated to the posterior movement of the hyoid bone (P < .05), whereas these changes were negatively correlated to the inferior displacement (P < .05; Table 5) at 2 months after surgery. In addition, the changes in the naso- and oro-pharyngeal airway volume were related to the inferior movement of the hyoid bone (P < .05; Table 5). The changes in the hypo-pharyngeal airway volume did not show any significant correlation with the inferoposterior movements of the hyoid bone (P > .05; Table 5).
Table 5.
Correlation With Inferoposterior Changes of Hyoid Bone Position and Changes in Airway Volume (n = 25)a
At 6 months after surgery, the changes in all subregions of the pharyngeal airway volume as well as those associated with total pharyngeal airway volume had no correlation with inferoposterior displacements of the hyoid bone (P > .05; Table 5).
DISCUSSION
The purpose of this study was to evaluate postoperative changes in the hyoid bone position and the pharyngeal airway space following bimaxillary surgery. The hyoid bone moved inferoposteriorly from 2 months to 6 months after surgery (Table 2), and the pharyngeal airway volume generally decreased in the same time periods (Table 3).
Because an individual's natural head posture may vary at different time points,26–28 which can affect the accuracy of the analysis of airway and hyoid bone position,5,22 head postures were measured at all time points. We have confirmed that there were no significant differences in head orientations between presurgery values and values at 2 and 6 months after surgery.
As the hyoid bone moves backward and downward after the mandibular setback, the changes in the supra-hyoid and infra-hyoid muscle tension may be related to the skeletal relapse.11,29 According to Degerliyurt et al.,30 the position of the hyoid bone was highly unstable for 1 year after surgery. Gu et al.9 reported that the hyoid bone tended to return to its original position after mandibular setback surgery, and this result is related to the relapse tendency of the anteroposterior position of the mandible. However, Eggensperger et al.11 observed progressive posterior movements of the hyoid bone during 11 years of postoperative follow-up. In our study, the hyoid bone continuously moved inferoposteriorly until 6 months after surgery (Table 2). We also found that both posterior movement of menton and the amount of mandibular setback were positively correlated to posterior displacement of the hyoid bone. This indicates that the position of hyoid bone after surgery is affected by the amount of mandibular setback or the amount of advancement with genioplasty.
The authors of previous reports5,30 concluded that the postoperative pharyngeal airway space decreases following mandibular setback surgery; however, the reduction is more marked in those who undergo mandibular setback surgery only. With regard to changes in the three subregions of the airway, the volume of the naso- and hypo-pharyngeal airway and the total volume significantly decreased at 2 and 6 months after surgery. According to our data, impaction of the posterior maxilla with a small amount of maxillary advancement may be associated with a decrease of naso-pharyngeal airway volume (Table 3).
The palatal plane angle, which is a lateral cephalometric variable used to represent the maxillary changes, has shown significant correlation with the airway changes. Volumetric changes of the oro-pharyngeal, hypo-pharyngeal, and total airway were positively correlated to the palatal plane angle in the present study (Table 4). This finding indicates that the pharyngeal airway volume is greatly affected by the rotational movement of the maxilla. In addition, we have found a significant relationship between the airway volume changes and the vertical movements of the hyoid bone (Table 5). Our results indicate that a more inferior displacement of the hyoid was associated with less airway volume reduction, which may be explained by the compensatory rearrangement of the oro-pharyngeal complex.
Our null hypothesis—that the pharyngeal airway volume and the hyoid bone position do not change after bimaxillary surgery—was rejected.
CONCLUSIONS
The hyoid bone moved backward and downward, and the amount of displacement increased with time.
The total pharyngeal airway space progressively decreased for up to 6 months after surgery.
The amount of the clockwise rotation of the palatal plane was positively correlated to the decrease in total airway volume.
The amount of airway volume reduction was negatively associated with the inferior movement of the hyoid bone.
REFERENCES
- 1.Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am J Orthod Dentofacial Orthop. 2007;131:372–377. doi: 10.1016/j.ajodo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 2.Jakobsone G, Stenvik A, Sandvik L, Espeland L. Three-year follow-up of bimaxillary surgery to correct skeletal Class III malocclusion: stability and risk factors for relapse. Am J Orthod Dentofacial Orthop. 2011;139:80–89. doi: 10.1016/j.ajodo.2009.03.050. [DOI] [PubMed] [Google Scholar]
- 3.Kim YI, Sp JK. A study of upper airway dimensional change according to maxillary superior movement after orthognathic surgery. Korean J Orthod. 2008;38:121. [Google Scholar]
- 4.Bailey LT, Proffit WR, White RP., Jr Trends in surgical treatment of Class III skeletal relationships. Int J Adult Orthod Orthognath Surg. 1995;10:108–118. [PubMed] [Google Scholar]
- 5.Hong JS, Park YH, Kim YJ, Hong SM, Oh KM. Three-dimensional changes in pharyngeal airway in skeletal Class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 2011;69:e401–e408. doi: 10.1016/j.joms.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Marsan G, Vasfi Kuvat S, Oztas E, Cura N, Susal Z, Emekli U. Oropharyngeal airway changes following bimaxillary surgery in Class III female adults. J Craniomaxillofac Surg. 2009;37:69–73. doi: 10.1016/j.jcms.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Bibby RE, Preston CB. The hyoid triangle. Am J Orthod. 1981;80:92–97. doi: 10.1016/0002-9416(81)90199-8. [DOI] [PubMed] [Google Scholar]
- 8.Marsan G, Oztas E, Cura N, Kuvat SV, Emekli U. Changes in head posture and hyoid bone position in Turkish Class III patients after mandibular setback surgery. J Craniomaxillofac Surg. 2010;38:113–121. doi: 10.1016/j.jcms.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Gu G, Nagata J, Suto M, et al. Hyoid position, pharyngeal airway and head posture in relation to relapse after the mandibular setback in skeletal Class III. Clin Orthod Res. 2000;3:67–77. [PubMed] [Google Scholar]
- 10.Kitahara T, Hoshino Y, Maruyama K, In E, Takahashi I. Changes in the pharyngeal airway space and hyoid bone position after mandibular setback surgery for skeletal Class III jaw deformity in Japanese women. Am J Orthod Dentofacial Orthop. 2010;138:708 e701–e710; discussion 708–709. doi: 10.1016/j.ajodo.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 11.Eggensperger N, Smolka W, Iizuka T. Long-term changes of hyoid bone position and pharyngeal airway size following mandibular setback by sagittal split ramus osteotomy. J Craniomaxillofac Surg. 2005;33:111–117. doi: 10.1016/j.jcms.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Tselnik M, Pogrel MA. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000;58:282–285; discussion 285–287. doi: 10.1016/s0278-2391(00)90053-3. [DOI] [PubMed] [Google Scholar]
- 13.Athanasiou AE, Toutountzakis N, Mavreas D, Ritzau M, Wenzel A. Alterations of hyoid bone position and pharyngeal depth and their relationship after surgical correction of mandibular prognathism. Am J Orthod Dentofacial Orthop. 1991;100:259–265. doi: 10.1016/0889-5406(91)70063-3. [DOI] [PubMed] [Google Scholar]
- 14.Liukkonen M, Vahatalo K, Peltomaki T, Tiekso J, Happonen RP. Effect of mandibular setback surgery on the posterior airway size. Int J Adult Orthod Orthognath Surg. 2002;17:41–46. [PubMed] [Google Scholar]
- 15.Park SB, Kim YI, Son WS, Hwang DS, Cho BH. Cone-beam computed tomography evaluation of short- and long-term airway change and stability after orthognathic surgery in patients with Class III skeletal deformities: bimaxillary surgery and mandibular setback surgery. Int J Oral Maxillofac Surg. 2011;41:87–93. doi: 10.1016/j.ijom.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Hwang S, Chung CJ, Choi YJ, Huh JK, Kim KH. Changes of hyoid, tongue and pharyngeal airway after mandibular setback surgery by intraoral vertical ramus osteotomy. Angle Orthod. 2010;80:302–308. doi: 10.2319/040209-188.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larson BE. Cone-beam computed tomography is the imaging technique of choice for comprehensive orthodontic assessment. Am J Orthod Dentofacial Orthop. 2012;141:402, 404, 406. doi: 10.1016/j.ajodo.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 18.Baik HS, Lee HJ, Lee KJ. A proposal for soft tissue landmarks for craniofacial analysis using 3-dimensional laser scan imaging. World J Orthod. 2006;7:7–14. [PubMed] [Google Scholar]
- 19.Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:468–479. doi: 10.1016/j.ajodo.2007.04.043. [DOI] [PubMed] [Google Scholar]
- 20.Lee H-sB YS, Lee KJ, Yu HS. The structural change in the hyoid bone and upper airway after orthognathic surgery for skeletal Class III anterior open bite patients using 3-dimensional computed tomography. Korea J Orthod. 2009;39:72. [Google Scholar]
- 21.Solow B, Sandham A. Cranio-cervical posture: a factor in the development and function of the dentofacial structures. Eur J Orthod. 2002;24:447–456. doi: 10.1093/ejo/24.5.447. [DOI] [PubMed] [Google Scholar]
- 22.Madsen DP, Sampson WJ, Townsend GC. Craniofacial reference plane variation and natural head position. Eur J Orthod. 2008;30:532–540. doi: 10.1093/ejo/cjn031. [DOI] [PubMed] [Google Scholar]
- 23.Oh KM, Seo SK, Park JE, Sim HS, Cevidanes LH, Kim YJ, et al. Post-operative soft tissue changes in patients with mandibular prognathism after bimaxillary surgery. J Craniomaxillofac Surg. In press. 2012:e1–e8. doi: 10.1016/j.jcms.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Won-Sik Yang T-WK, Seung-Hak Baek. Current Orthodontic Diagnosis. Seoul, Korea: Ji Sung Publications. 2007. [Google Scholar]
- 25.Springate SD. The effect of sample size and bias on the reliability of estimates of error: a comparative study of Dahlberg's formula. Eur J Orthod. 2012;34:158–163. doi: 10.1093/ejo/cjr010. [DOI] [PubMed] [Google Scholar]
- 26.Marcotte MR. Head posture and dentofacial proportions. Angle Orthod. 1981;51:208–213. doi: 10.1043/0003-3219(1981)051<0208:HPADP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Ozbek MM, Koklu A. Natural cervical inclination and craniofacial structure. Am J Orthod Dentofacial Orthop. 1993;104:584–591. doi: 10.1016/S0889-5406(05)80442-1. [DOI] [PubMed] [Google Scholar]
- 28.Cole SC. Natural head position, posture, and prognathism: the Chapman Prize Essay, 1986. Br J Orthod. 1988;15:227–239. doi: 10.1179/bjo.15.4.227. [DOI] [PubMed] [Google Scholar]
- 29.Chung DH, Hatch JP, Dolce C, Van Sickels JE, Bays RA, Rugh JD. Positional change of the hyoid bone after bilateral sagittal split osteotomy with rigid and wire fixation. Am J Orthod Dentofacial Orthop. 2001;119:382–389. doi: 10.1067/mod.2001.112670. [DOI] [PubMed] [Google Scholar]
- 30.Degerliyurt K, Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E. A comparative CT evaluation of pharyngeal airway changes in Class III patients receiving bimaxillary surgery or mandibular setback surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:495–502. doi: 10.1016/j.tripleo.2007.11.012. [DOI] [PubMed] [Google Scholar]