Abstract
Objective:
To analyze the effect of low-level laser therapy (LLLT) on perception of pain after separator placement and compare it with perceptions of control and placebo groups using a frequent irradiation protocol.
Materials and Methods:
Eighty-eight patients were randomly allocated to a laser group, a light-emitting diode (LED) placebo group, or a control group. Elastomeric separators were placed on the first molars. In the laser and LED groups, first molars were irradiated for 30 seconds every 12 hours for 1 week using a portable device. Pain was marked on a visual analog scale at predetermined intervals. Repeated measure analysis of variance was performed for statistical analysis.
Results:
The pain scores of the laser group were significantly lower than those of the control group up to 1 day. The pain scores in the LED group were not significantly different from those of the laser group during the first 6 hours. After that point, the pain scores of the LED group were not significantly different from those of the control.
Conclusions:
Frequent LLLT decreased the perception of pain to a nonsignificant level throughout the week after separator placement, compared with pain perception in the placebo and control groups. Therefore, LLLT might be an effective method of reducing orthodontic pain.
Keywords: Low-level laser therapy (LLLT), Light-emitting diode (LED), Orthodontic pain, Elastomeric separator, Placebo, Visual analog scale (VAS), Laser irradiation
INTRODUCTION
Pain or discomfort during orthodontic treatment is a major concern for clinicians and patients. It may discourage patients from seeking or continuing treatment.1 The incidence and severity of pain have been reported to be higher than those of extractions.2 Several patients have reported that orthodontic pain disturbed their sleep during the first week after initial wire placement.3 The peak of pain occurred approximately 24 hours after separator/initial wire placement and decreased over the next 6 to 8 days.2,4–7
To control the pain, analgesics or anti-inflammatory agents have been prescribed, and the initial arch wire has often been limited to light force only.8,9 Preemptive ibuprofen significantly reduced the pain 2 hours after separator placement compared with a placebo. However, a significant amount of pain was reported at 24 hours.6 Another option, the use of nonsteroidal anti-inflammatory drugs, is still controversial because of their potential influence on tooth movement and their adverse systemic side effects.10–13
Recently, low-level laser therapy (LLLT) has been used to control pain because of its anti-inflammatory properties and regenerative effect on neurons.14–17 These effects have been attributed to photobioactive reaction that stimulates the proliferation and differentiation of cells.18 Previous studies have shown that LLLT may increase the blood supply and promote recovery of dental tissue.19 In addition, several studies have shown that LLLT reduced orthodontic pain.20–22 Other studies showed no significant reduction of pain with lasers compared to a placebo.16,23 Moreover, laser therapy had no impact on time of pain initiation and maximum pain.21
Interestingly, in previous LLLT studies, clinicians directly performed a single-session laser irradiation in their office.17,21,24 Other studies recalled the participants to the office several times for laser application.20,25 This limitation might have decreased the efficacy of the therapy. It is hypothesized that a more frequent application of laser therapy during the pain/discomfort period might lead to a greater reduction in the perception of pain in orthodontic patients. However, no study has evaluated the effect of frequent LLLT. Currently, a compact, battery-operated, handheld device that produces a low-level aluminum-gallium-indium-phosphide semiconductor (AlGaInP) laser has been developed for use by patients at home. These devices have been found to be safe and effective in the management of dentin hypersensitivity.26
The purpose of this study was to analyze the effect of a more frequent LLLT protocol on the perception of pain from immediately up to 7 days after separator placement and to compare it to the perception of pain in control and placebo groups.
MATERIALS AND METHODS
One hundred and twenty patients were assessed in a private clinic from May 2010 to January 2012. Of these, 88 patients (23 males, 65 females; mean age, 22.7 years) met the following inclusion criteria: complete eruption of the second molars and no open interproximal contacts of the first molar. In addition, patients with previous orthodontic treatment, metabolic and periodontal diseases, or medication were excluded. The study was approved by the institutional review board of the Catholic University of Korea. Sample-size calculation was performed based on previous results.20
Subjects were assigned randomly to three test groups: laser irradiation group (n = 28), light-emitting diode (LED) group as a placebo (n = 30), and a control group receiving no irradiation (n = 30). Subjects assigned to the laser and LED groups were blinded to their assignment.
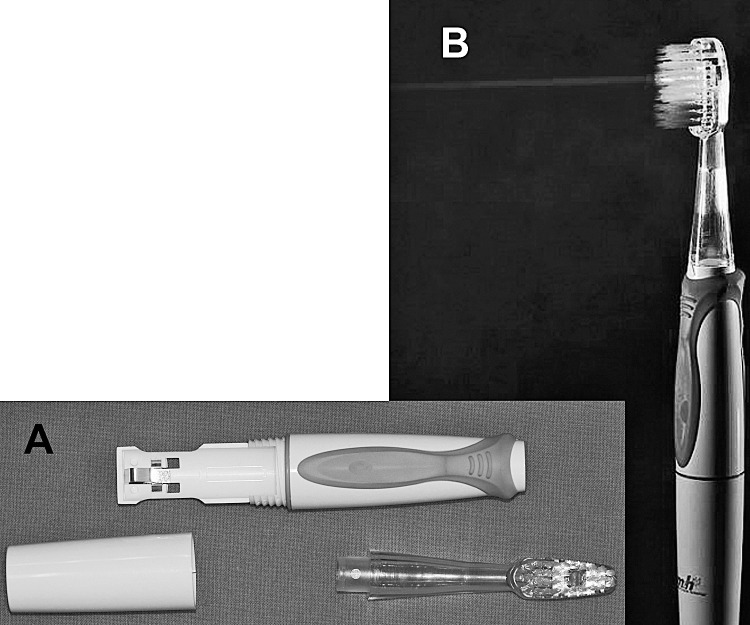
A low-level medical semiconductor laser device with an AlGaInP diode, wavelength of 635 nm, energy of 10 mJ, field diameter of 5.6 mm, and output potency of 6 mW (Figure 1) and an LED device with wavelength of 635 nm and output of 12.9 µW of the same exterior design (Dental.M, M&H Co, Hwaseong, Korea) were used. After placement of 2.1 mm elastomeric separators (Dentalastics Separators, Dentaurum, Ispringen, Germany) mesially and distally on both maxillary first molars, subjects in the laser and LED groups were taught to use the device and asked to apply it for 30 seconds on each area immediately then every 12 hours for 1 week with close contact between the tip and mucosa to irradiate the mesiobuccal, mesiolingual, distobuccal, and distolingual areas.
Figure 1.
A compact, battery-operated, handheld AlGaInP laser device for home use. (A) Disassembled. (B) Activated.
The three groups were asked to mark pain severity on a questionnaire containing 11 copies of a 10 cm visual analog scale (VAS) at 5 minutes, 1 hour, 6 hours, 12 hours and then at days 1, 2, 3, 4, 5, 6, and 7 after the separators were applied.
Statistical Analysis
Statistical evaluation was performed by SPSS 16.0 (SPSS Inc, Chicago, Ill). Two-way analysis of variance (ANOVA) was performed to compare age of subjects according to group and gender. Repeated measures ANOVA was conducted to evaluate the differences in pain scores at each time point as the within-subjects variable and between groups and gender as the between-subjects variables. Age was used as a covariant. The alpha level was 0.05.
RESULTS
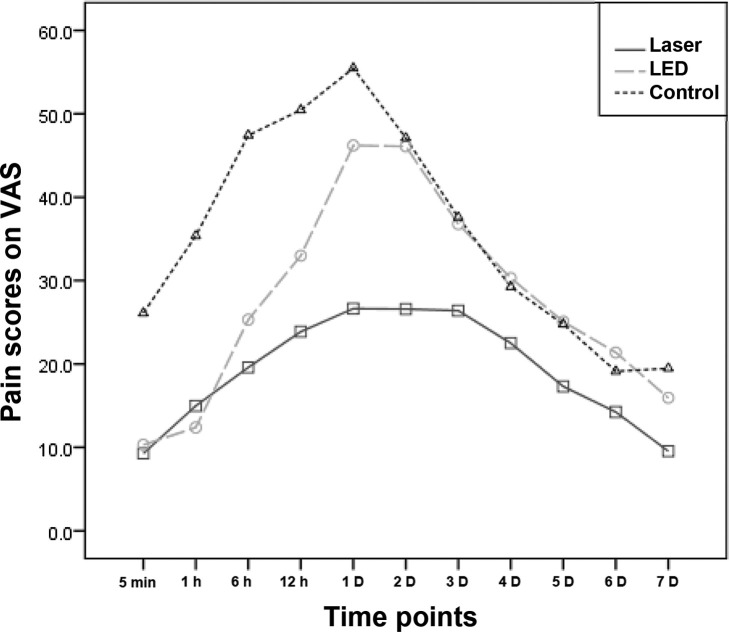
There were no significant differences in age among the laser, LED placebo, and control groups (P = .069) or between genders (P = .094). Also, no significant interaction between groups and gender was found (P = .30) (Table 1).
Table 1.
Descriptive Data for the Laser, LED, and Control Groupsa
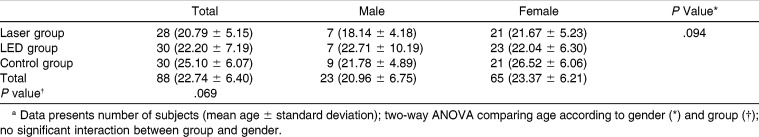
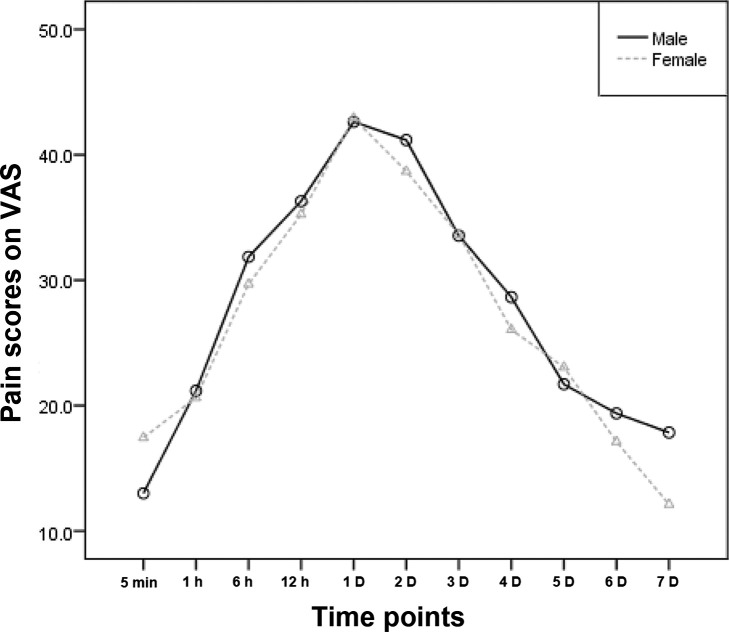
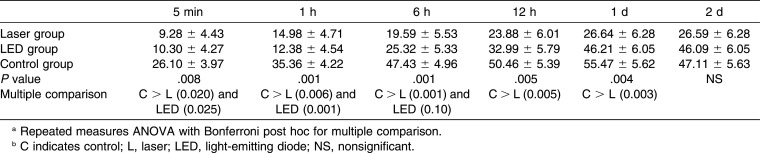
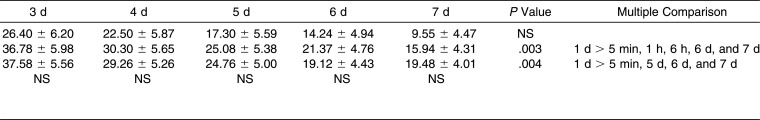
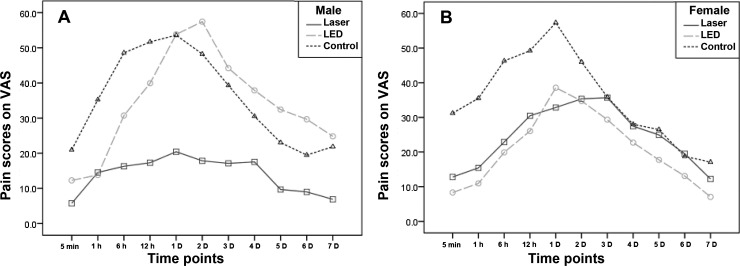
There was a significant difference in pain perception among the three groups (P = .004). The laser group showed a statistically significant decrease in pain scores compared with the control group (P = .003). The placebo group demonstrated no significant differences from the laser and control groups (P = .28 and P = .26, respectively; Figure 2). However, gender had no significant effect on scores of pain perception (P = .81; Figure 3). In addition, there was a borderline significance of the interaction between the gender and groups (P = .05).
Figure 2.
Comparison of mean pain scores on the VAS among the laser, LED, and control groups over time.
Figure 3.
Comparison of mean pain scores on the VAS between male and female subjects over time.
The maximum level of pain was reached 1 day after separator placement. The laser group showed a maximum level of (26.6 ± 6.3), which was significantly lower than those of the LED placebo and control groups (46.2 ± 6.1 and 55.5 ± 5.6, respectively) (Table 2 and Figure 2).
Table 2.
Pain Perception Scores of the Laser, LED, and Control Groups at Each Time Pointa,b
Table 2.
Extended
During the first 6 hours, the pain scores in the placebo group were not significantly different from those of the laser group. Furthermore, at 12 and 24 hours after placement of separators, the pain scores of the placebo group were not significantly different from those of the control group. From day 2 to day 7 after separators placement, the pain scores of all three groups decreased. Pain scores were still lower at day 2 in the laser group; however, the difference was not statistically significant. A decrease was seen in the control and placebo groups, which reached a level that was not significantly different from the laser group (Table 2 and Figure 2).
In the laser group, there were no significant differences between pain scores at different time points. However, in the placebo group, the maximum pain score occurred at 1 day and was significantly higher than at 5 minutes, 1 hour, 6 hours, or day 6 or 7; whereas in the control group it was higher than at 5 minutes and at days 5, 6, and 7 (Table 2).
Because of the borderline significance (P = .05) of interaction between groups and gender, the groups were compared within each gender independently. In male subjects, the pain scores in the laser group were lower than those in the placebo and control groups, which showed a similar pain perception trend. In female subjects, pain scores in the placebo group showed a similar trend to those in the laser group (Figure 4).
Figure 4.
Comparison of mean pain scores on the VAS among laser, LED, and control groups over time according to gender. (A) Male subjects. (B) Female subjects.
DISCUSSION
The aim of this study was to evaluate the effect of frequent laser irradiation on the perception of pain caused by orthodontic forces. The pain perception ranged widely depending on individualized pain thresholds, age, and gender.2–5,27,28
In agreement with previous studies, pain reached a maximum level 24 hours after separator placement.14,22,28 The maximum pain level in the laser group was similar to the initial pain level in the control group. The pain scores were decreased and were not significantly different among all time points. This might indicate the laser blunts the peak of the pain compared with the peak pain experienced by the placebo and control groups (Figure 2).
It was presumed that a score of 0 to 30 score is the mild pain range, whereas a score of 31 to 69 is moderate pain.29 In our study, the laser group's pain was 20 scores lower than pain scores in the other groups. This decrease that changes the level of pain from moderate to mild might be clinically significant.
Less pain and faster recovery have been reported with the CO2 laser than with the Nd∶YAG laser group, suggesting a longer-lasting analgesic effect with CO2 laser therapy.30 Meanwhile, Dilsiz et al.31 demonstrated that the Nd∶YAG laser was more effective in desensitizing teeth than the 685 nm diode laser. In our study, the AlGaInP diode laser was applied whereas in several studies a gallium-aluminum-arsenide diode laser was used.19,24,32 Thus far, no study has compared the effect of different laser types with different treatment settings.
In our study, the LED group showed lower pain scores than the control group during the first 6 hours, and then the scores increased and showed no significant difference from those of the control group. The decreased scores could be attributed to the placebo effect. Several mechanisms have been suggested to explain the placebo effect, such as emotional modulation and reduction of subjective stress during painful stimulation.33
In a previous study, pain reduction was reported by 39% of the subjects after administration of analgesic placebo.34 However, the increased fear of pain after a previous placebo experience was found to reduce the placebo analgesic effect.35 This might explain the increased pain scores in our study after the second LED application. In addition, evidence supported the hypothesis that placebo and treatment effects are not cumulative and that they have mutually exclusive mechanisms.36 Esper et al.23 showed that pain scores decreased significantly in the LED group between 2 and 120 hours compared with scores of the control and laser groups. They attributed their result to the high-potency and high-energy LED (0.1 W and 7 J, respectively) applied in their study. Consequently, this inconsistency between the investigations might be due to the differences in the properties of the LED and laser used.
In our study, the pattern of the placebo effect over time seemed different between genders. The pain scores in male subjects in the placebo group followed the same pattern as the control group whereas in females, pain scores appeared to more closely follow the trend in the laser group. In agreement, Saxon et al.37 reported that female patients were more affected by placebo treatment, although an effective response to the analgesic placebo treatment was demonstrated in males only.38 Another study demonstrated no gender dimorphism in relation to the placebo analgesic effect.39 Nevertheless, our results should be interpreted with caution due to the relatively small size of the male group.
In concordance, no significant difference was reported in the discomfort level after placement of separators and initial arch wire, according to age and gender.7,28 A group of environmental, sociocultural, and genetic factors are responsible for these differences.40–43 Therefore, the present study might have been affected by these individual variations. A future study applying a split-mouth method might be required to remove bias. Also, a study evaluating the effect of laser application on the pain produced by the initial wire is recommended. In addition, a comparison between the pain that resulted from separator placement and from arch wire change is warranted.
CONCLUSIONS
The laser group showed a significant main effect compared with the control group only.
The perception of pain was not significantly different based on age or gender. However, the effect of laser irradiation was more pronounced in male subjects.
The placebo treatment was more effective after the first irradiation than after the following sessions and was more effective in female subjects than in males.
Therefore, frequent low-level laser irradiation may be an effective way to reduce orthodontic pain during the first day after separator placement.
REFERENCES
- 1.Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–188. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 2.Jones ML, Chan C. Pain in the early stages of orthodontic treatment. J Clin Orthod. 1992;26:311–313. [PubMed] [Google Scholar]
- 3.Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop. 1992;102:373–381. doi: 10.1016/0889-5406(92)70054-e. [DOI] [PubMed] [Google Scholar]
- 4.Jones ML. An investigation into the initial discomfort caused by placement of an archwire. Eur J Orthod. 1984;6:48–54. doi: 10.1093/ejo/6.1.48. [DOI] [PubMed] [Google Scholar]
- 5.Scheurer PA, Firestone AR, Burgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–357. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 6.Steen Law SL, Southard KA, Law AS, Logan HL, Jakobsen JR. An evaluation of preoperative ibuprofen for treatment of pain associated with orthodontic separator placement. Am J Orthod Dentofacial Orthop. 2000;118:629–635. doi: 10.1067/mod.2000.110638. [DOI] [PubMed] [Google Scholar]
- 7.Wilson S, Ngan P, Kess B. Time course of the discomfort in young patients undergoing orthodontic treatment. Pediatr Dent. 1989;11:107–110. [PubMed] [Google Scholar]
- 8.Bird SE, Williams K, Kula K. Preoperative acetaminophen vs ibuprofen for control of pain after orthodontic separator placement. Am J Orthod Dentofacial Orthop. 2007;132:504–510. doi: 10.1016/j.ajodo.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 9.Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR. The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop. 2001;120:20–27. doi: 10.1067/mod.2001.115616. [DOI] [PubMed] [Google Scholar]
- 10.Kyrkanides S, O'Banion MK, Subtelny JD. Nonsteroidal anti-inflammatory drugs in orthodontic tooth movement: metalloproteinase activity and collagen synthesis by endothelial cells. Am J Orthod Dentofacial Orthop. 2000;118:203–209. doi: 10.1067/mod.2000.105872. [DOI] [PubMed] [Google Scholar]
- 11.Walker JB, Buring SM. NSAID impairment of orthodontic tooth movement. Ann Pharmacother. 2001;35:113–115. doi: 10.1345/aph.10185. [DOI] [PubMed] [Google Scholar]
- 12.Gameiro GH, Pereira-Neto JS, Magnani MB, Nouer DF. The influence of drugs and systemic factors on orthodontic tooth movement. J Clin Orthod. 2007;41:73–78; quiz 71. [PubMed] [Google Scholar]
- 13.Krishnan V, Davidovitch Z. The effect of drugs on orthodontic tooth movement. Orthod Craniofac Res. 2006;9:163–171. doi: 10.1111/j.1601-6343.2006.00372.x. [DOI] [PubMed] [Google Scholar]
- 14.Harazaki M, Isshiki Y. Soft laser irradiation effects on pain reduction in orthodontic treatment. Bull Tokyo Dent Coll. 1997;38:291–295. [PubMed] [Google Scholar]
- 15.Harazaki M, Takahashi H, Ito A, Isshiki Y. Soft laser irradiation induced pain reduction in orthodontic treatment. Bull Tokyo Dent Coll. 1998;39:95–101. [PubMed] [Google Scholar]
- 16.Lim HM, Lew KK, Tay DK. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofacial Orthop. 1995;108:614–622. doi: 10.1016/s0889-5406(95)70007-2. [DOI] [PubMed] [Google Scholar]
- 17.Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon HP. Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2006;130:371–377. doi: 10.1016/j.ajodo.2005.04.036. [DOI] [PubMed] [Google Scholar]
- 18.Verschueren RC, Koudstaal J, Oldhoff J. The carbon dioxide laser; some possibilities in surgery. Acta Chir Belg. 1975;74:197–204. [PubMed] [Google Scholar]
- 19.Abi-Ramia LB, Stuani AS, Stuani MB, Mendes Ade M. Effects of low-level laser therapy and orthodontic tooth movement on dental pulps in rats. Angle Orthod. 2010;80:116–122. doi: 10.2319/120808-619.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141:289–297. doi: 10.1016/j.ajodo.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Tortamano A, Lenzi DC, Haddad AC, Bottino MC, Dominguez GC, Vigorito JW. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009;136:662–667. doi: 10.1016/j.ajodo.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 22.Fujiyama K, Deguchi T, Murakami T, Fujii A, Kushima K, Takano-Yamamoto T. Clinical effect of CO(2) laser in reducing pain in orthodontics. Angle Orthod. 2008;78:299–303. doi: 10.2319/033007-153.1. [DOI] [PubMed] [Google Scholar]
- 23.Esper MA, Nicolau RA, Arisawa EA. The effect of two phototherapy protocols on pain control in orthodontic procedure—a preliminary clinical study. Lasers Med Sci. 2011;26:657–663. doi: 10.1007/s10103-011-0938-6. [DOI] [PubMed] [Google Scholar]
- 24.Bicakci AA, Kocoglu-Altan B, Toker H, Mutaf I, Sumer Z. Efficiency of low-level laser therapy in reducing pain induced by orthodontic forces. Photomed Laser Surg. 2012;30:460–465. doi: 10.1089/pho.2012.3245. [DOI] [PubMed] [Google Scholar]
- 25.Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008;23:27–33. doi: 10.1007/s10103-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 26.Kook YA, Beak SH. A Comparative MultiCenter Double Blind Randomized Clinical Trial to Assess the Safety and Efficacy of the “Laser Toothbrush” a LowLevel Laser Therapy Toothbrush for the Treatment of Dentin Hypersensitivity. Seoul, Korea: The Catholic University of Korea, Seoul, St Mary's Hospital and Seoul National University Dental Hospital; 2009. [Google Scholar]
- 27.Brown DF, Moerenhout RG. The pain experience and psychological adjustment to orthodontic treatment of preadolescents, adolescents, and adults. Am J Orthod Dentofacial Orthop. 1991;100:349–356. doi: 10.1016/0889-5406(91)70073-6. [DOI] [PubMed] [Google Scholar]
- 28.Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96:47–53. doi: 10.1016/0889-5406(89)90228-x. [DOI] [PubMed] [Google Scholar]
- 29.Garven A, Brady S, Wood S, et al. The impact of enrollment in a specialized interdisciplinary neuropathic pain clinic. Pain Res Manag. 2011;16:159–168. doi: 10.1155/2011/518710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lippert BM, Werner JA. Comparison of carbon dioxide and neodymium: yttrium-aluminum-garnet lasers in surgery of the inferior turbinate. Ann Otol Rhinol Laryngol. 1997;106:1036–1042. doi: 10.1177/000348949710601207. [DOI] [PubMed] [Google Scholar]
- 31.Dilsiz A, Canakci V, Ozdemir A, Kaya Y. Clinical evaluation of Nd:YAG and 685-nm diode laser therapy for desensitization of teeth with gingival recession. Photomed Laser Surg. 2009;27:843–848. doi: 10.1089/pho.2008.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altan BA, Sokucu O, Ozkut MM, Inan S. Metrical and histological investigation of the effects of low-level laser therapy on orthodontic tooth movement. Lasers Med Sci. 2012;27:131–140. doi: 10.1007/s10103-010-0853-2. [DOI] [PubMed] [Google Scholar]
- 33.Aslaksen PM, Flaten MA. The roles of physiological and subjective stress in the effectiveness of a placebo on experimentally induced pain. Psychosom Med. 2008;70:811–818. doi: 10.1097/PSY.0b013e31818105ed. [DOI] [PubMed] [Google Scholar]
- 34.Levine JD, Gordon NC, Bornstein JC, Fields HL. Role of pain in placebo analgesia. Proc Natl Acad Sci U S A. 1979;76:3528–3531. doi: 10.1073/pnas.76.7.3528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lyby PS, Aslaksen PM, Flaten MA. Variability in placebo analgesia and the role of fear of pain—an ERP study. Pain. 2011;152:2405–2412. doi: 10.1016/j.pain.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 36.van Die MD, Bone KM, Burger HG, Teede HJ. Are we drawing the right conclusions from randomised placebo-controlled trials? A post-hoc analysis of data from a randomised controlled trial. BMC Med Res Methodol. 2009;9:41. doi: 10.1186/1471-2288-9-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saxon L, Hiltunen AJ, Hjemdahl P, Borg S. Gender-related differences in response to placebo in benzodiazepine withdrawal: a single-blind pilot study. Psychopharmacology (Berl) 2001;153:231–237. doi: 10.1007/s002130000574. [DOI] [PubMed] [Google Scholar]
- 38.Aslaksen PM, Bystad M, Vambheim SM, Flaten MA. Gender differences in placebo analgesia: event-related potentials and emotional modulation. Psychosom Med. 2011;73:193–199. doi: 10.1097/PSY.0b013e3182080d73. [DOI] [PubMed] [Google Scholar]
- 39.Averbuch M, Katzper M. Gender and the placebo analgesic effect in acute pain. Clin Pharmacol Ther. 2001;70:287–291. doi: 10.1067/mcp.2001.118366. [DOI] [PubMed] [Google Scholar]
- 40.Salomons TV, Johnstone T, Backonja MM, Shackman AJ, Davidson RJ. Individual differences in the effects of perceived controllability on pain perception: critical role of the prefrontal cortex. J Cogn Neurosci. 2007;19:993–1003. doi: 10.1162/jocn.2007.19.6.993. [DOI] [PubMed] [Google Scholar]
- 41.Mogil JS. The genetic mediation of individual differences in sensitivity to pain and its inhibition. Proc Natl Acad Sci U S A. 1999;96:7744–7751. doi: 10.1073/pnas.96.14.7744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moore R, Miller ML, Weinstein P, Dworkin SF, Liou HH. Cultural perceptions of pain and pain coping among patients and dentists. Community Dent Oral Epidemiol. 1986;14:327–333. doi: 10.1111/j.1600-0528.1986.tb01084.x. [DOI] [PubMed] [Google Scholar]
- 43.Diatchenko L, Slade GD, Nackley AG, et al. Genetic basis for individual variations in pain perception and the development of a chronic pain condition. Hum Mol Genet. 2005;14:135–143. doi: 10.1093/hmg/ddi013. [DOI] [PubMed] [Google Scholar]