Abstract
This study of healthy adults revealed no major changes in the bacterial community of the respiratory tracts following RSV inoculation, suggesting that the adult respiratory microbial community is resilient to viral perturbations https://bit.ly/3AwnMc8
To the Editor:
Respiratory syncytial virus (RSV) is the commonest cause of acute lower respiratory tract infection (RTI) in infants, resulting in seasonal surges in hospital admissions [1]. In addition to its impact in childhood, RSV is increasingly recognised as a cause of morbidity and mortality in elderly persons [2]. The virus is highly contagious and regularly causes reinfections, despite limited genetic diversity [3]. Safe and effective vaccines have so far proven elusive [2].
Severe infantile bronchiolitis is associated with recurrent wheeze and asthma in later childhood [4]. One possible explanation is that RSV infection causes lasting changes in the respiratory microbial community leading to secondary effects on physiology and immunity. Alternatively, it has been proposed that disordered microbial communities predispose to severe RSV disease [5].
Longitudinal birth cohort studies have demonstrated that frequent RTIs in early life are associated with a perturbed respiratory microbiota, dominated by Moraxella, that may precede viral infections. These studies indicate associations between the respiratory microbiota and viral infection [6]. Nonetheless, the issues of cause and effect have been difficult to resolve in observational studies.
To determine the effect of RSV infection on the respiratory microbiome, we inoculated 37 healthy non-smoking adults between 18 and 50 years of age with an established RSV challenge inoculum, Memphis 37 (RSV-A M37) [7]. We anticipated that infection would result in significant changes in the bacterial community within the upper respiratory tract.
Baseline samples were collected prior to participant inoculation by intranasal drops of Memphis 37 [8]. Subjects were quarantined for 10 days post-infection and sampled daily [9]. Participants returned post-quarantine for further sampling at days 14 and 28. The study was approved by the UK National Research Ethics Services (study numbers 10/H0711/94 and 11/LO/1826) and written informed consent was provided by all subjects [10].
Endpoint titre of IgA against RSV was determined from nasal wash samples [7]. Cytokine and chemokine inflammatory mediators within nasosorption eluates were quantified by MSD multiplex immunoassay [10] (MesoScale Discovery, Rockville, MD, USA).
DNA was extracted from oropharyngeal swabs; SYBR green qPCR and 16S rRNA gene sequencing was performed [11]. Sequences were submitted to the European Nucleotide Database, project number PRJEB28323. Sequence processing was carried out as previously described [11]. All further analysis was carried out in R, version 3.3.2.
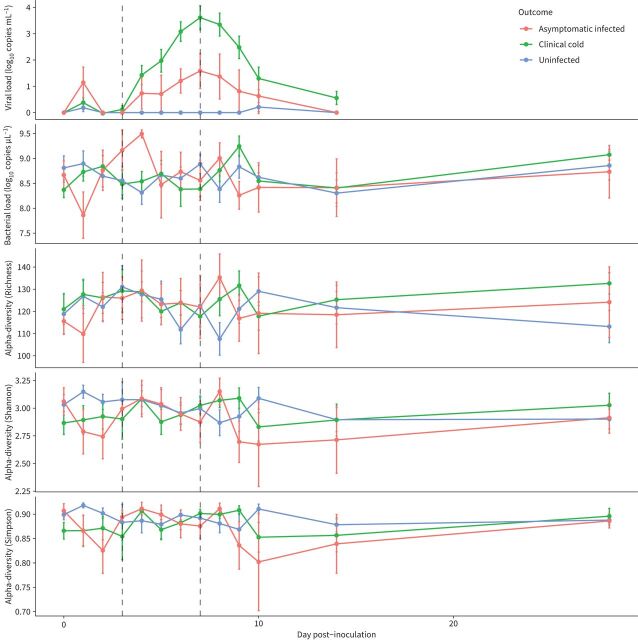
Enrolled volunteers showed one of three outcomes: clinical cold with RSV detection (determined by qPCR [10]) and/or virus-specific IgA production alongside a cumulative self-reported symptom score over a 14-day period (n=17) [7]; asymptomatic infection (n=6) or no infection (n=14) (figure 1). No significant differences in participant demographics (age, sex, ethnicity; p>0.05) were observed between outcome groups [10]. Between viral inoculation and day 3, only low levels of RSV were detected in the participants’ respiratory tracts. At day 3 viral load increased in patients who went on to develop symptoms. Day 7 was the peak of viral infection and viral load fell thereafter. At day 28, no patients had any sign of clinical infection and viral load was not measured [10].
FIGURE 1.
Mean change in viral load (by qPCR), bacterial load (by qPCR) and alpha diversity (three measures Richness, Shannon, Simpson) over the course of the study for the three groups: clinical cold (infected), asymptomatic infected, and uninfected. Error bars represent the standard error of the mean.
Prior to viral inoculation, there were no significant differences in bacterial alpha diversity (Richness, p=0.948; Shannon, p=0.263; Simpsons, p=0.166) or beta diversity (Bray–Curtis dissimilarity, R2=0.055, p=0.087) between the three outcome groups [10].
Significant differences between viral loads were seen between the uninfected and clinical cold groups at days 5, 6, 7 and 8 (p(adjusted)<0.001) (figure 1). Significant differences were also seen between the asymptomatic infected group and the clinical cold group on days 7 and 8 (p(adjusted)=0.03 and 0.04, respectively); the mean viral load at day 2 was higher in the asymptomatic infected group, despite not going on to develop clinical colds.
Bacterial load in the asymptomatic infected group fluctuated more than in the other groups in the first 4 days of infection (figure 1); these changes were not significant and may reflect the low number of cases in the asymptomatic group (n=6).
No significant differences in bacterial load, alpha diversity measures or species turnover were observed between groups over the course of viral infection.
Repeated measure correlations were carried out between bacterial diversity measures and the full set of cytokine measurements. No significant correlations were observed when the whole dataset was compared or when it was subdivided based on clinical symptoms. In addition, no significant correlations were found between bacterial diversity measures and patient symptom score or viral load.
Analysis of the respiratory microbiome in healthy adults revealed that, contrary to results reported in children, no significant changes in the bacterial community were seen over the course of RSV infection.
Initial investigation of differences in the bacterial community at baseline revealed no significant differences in bacterial load, diversity or community composition, suggesting that the bacterial community at baseline did not have a significant effect on the course of viral infection. A post hoc power analysis based on the effect size seen in the baseline samples (f=0.23) suggested that using the conventional power of 0.80, n=62 per group would be required to identify significant differences in Shannon diversity between the three groups. It is possible therefore that a larger study would be able to detect more subtle changes in the bacterial community.
Indicator species analysis and DESeq2 were used to investigate operational taxonomic units (OTUs) that may influence the outcome of viral infection. This analysis was carried out at the key time points in the viral infection, baseline, days 3 (the start of concerted viral replication), 7 (peak viral replication) and 28. Although several OTUs were statistically significant by these analyses, none stood up to further OUT-specific investigation. Further analysis at phylum level revealed no significant differences between outcome groups.
No significant correlations between changes in the microbial community and changes in cytokine measurements were seen, suggesting that the microbial community within the respiratory tract is resilient to RSV-mediated changes in the inflammatory environment of the upper respiratory tract in healthy adult volunteers. Considering the number of participants within the present study, further investigation using a larger set of subjects would be needed to confirm these observations, although there are ethical challenges.
Previous studies have focused on exploring the microbiome in infants, showing a positive association between Haemophilus-, Moraxella- and Streptococcus-dominated nasal microbiota and infection severity [12–14]. Our study of healthy adults did not confirm these reported microbial changes. This may be due to the maturity and relative stability of the immune system and microbial community in these individuals, unlike those of the infant population, or the milder disease experienced by healthy adults.
In a human rhinovirus (HRV) challenge study of induced sputum, Molyneaux et al. [15] found that the bacterial communities of healthy individuals were stable during the course of infection. In contrast, using nasal lavage fluid, Allen et al. [16] found significant changes in two genera (Neisseria and Propionibacterium) between infected and non-infected adults. These divergent results may be in part be due to the sampling site, as it has been previously shown that the bacterial community of the throat is more closely related to the lower respiratory tract than the nasal community [17]. Including both nasal and throat samples may be of value in future studies.
Controlled human infection challenges are essential to understand disease pathogenesis and underpin eventual vaccine development. There are, however, substantial ethical issues associated with exposing healthy individuals to infectious risk. As a result, these studies must be conscientiously designed to minimise risks [18]. When considering these parameters, sample sizes are necessarily limited. This provides a challenge for the analysis of highly variable microbiome data, making interpretation difficult.
Despite these limitations, the present study provides important information about the resilience of the microbiome in healthy adults to RSV perturbations and suggests that comorbidities may have an important effect on the bacterial community within the lungs of vulnerable individuals, as observed in studies of natural infections.
Shareable PDF
Footnotes
Data availability: Sequences were submitted to the European Nucleotide Database and fully available under project number PRJEB28323.
Author contributions: P.J.M. Openshaw, C. Chiu and M.F. Moffatt conceived the study, with input from W.O.C. Cookson. M.S. Habibi, A. Paras and C. Chiu performed volunteer infections and collected samples. M.S. Habibi, R.S. Thwaites, L. Cuthbertson, P. James and C. Chiu collected human antibody and microbial data. Microbiome data was analysed by L. Cuthbertson and P. James. The manuscript was written by L. Cuthbertson with input from all authors.
Conflict of interest: L. Cuthbertson has nothing to disclose.
Conflict of interest: P. James has nothing to disclose.
Conflict of interest: M.S. Habibi has nothing to disclose.
Conflict of interest: R.S. Thwaites has nothing to disclose.
Conflict of interest: A. Paras has nothing to disclose.
Conflict of interest: C. Chiu has nothing to disclose.
Conflict of interest: P.J.M. Openshaw has nothing to disclose.
Conflict of interest: W.O.C. Cookson has nothing to disclose.
Conflict of interest: M.F. Moffatt has nothing to disclose.
Support statement: The authors gratefully acknowledge support from the Wellcome Trust (087805/Z/08/Z); The Medical Research Council HIC-Vac network (MR/R005982/1); RSV Consortium in Europe (RESCEU) Horizon 2020 Framework Grant 116019; the UK National Institute for Health Research (NIHR) Comprehensive Local Research Networks (CLRNs); an NIHR Senior Investigator award to P.J.M. Openshaw; the Biomedical Research Centre (NIHR Imperial BRC); and the Health Protection Research Unit in Respiratory Infections at Imperial College London (NIHR HPRU RI). Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Terletskaia-Ladwig E, Enders G, Schalasta G, et al. Defining the timing of respiratory syncytial virus (RSV) outbreaks: an epidemiological study. BMC Infect Dis 2005; 5: 20. doi: 10.1186/1471-2334-5-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coultas JA, Smyth R, Openshaw PJ. Respiratory syncytial virus (RSV): a scourge from infancy to old age. Thorax 2019; 74: 986–993. doi: 10.1136/thoraxjnl-2018-212212 [DOI] [PubMed] [Google Scholar]
- 3.Hall CB, Walsh EE, Long CE, et al. Immunity to and frequency of reinfection with respiratory syncytial virus. J Infect Dis 1991; 163: 693–698. [DOI] [PubMed] [Google Scholar]
- 4.Lynch JP, Sikder MA, Curren BF, et al. The influence of the microbiome on early-life severe viral lower respiratory infections and asthma-food for thought? Front Immunol 2017; 8: 156. doi: 10.3389/fimmu.2017.00156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Higgins D, Trujillo C, Keech C. Advances in RSV vaccine research and development – a global agenda. Vaccine 2016; 34: 2870–2875. doi: 10.1016/j.vaccine.2016.03.109 [DOI] [PubMed] [Google Scholar]
- 6.Bosch A, de Steenhuijsen Piters WAA, van Houten MA, et al. Maturation of the infant respiratory microbiota, environmental drivers, and health consequences. a prospective cohort study. Am J Respir Crit Care Med 2017; 196: 1582–1590. doi: 10.1164/rccm.201703-0554OC [DOI] [PubMed] [Google Scholar]
- 7.Habibi MS, Jozwik A, Makris S, et al. Impaired antibody-mediated protection and defective IgA B-cell memory in experimental infection of adults with respiratory syncytial virus. Am J Respir Crit Care Med 2015; 191: 1040–1049. doi: 10.1164/rccm.201412-2256OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thwaites RS, Jarvis HC, Singh N, et al. Absorption of nasal and bronchial fluids: precision sampling of the human respiratory mucosa and laboratory processing of samples. J Vis Exp 2018; 131: e56413. doi: 10.3791/56413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeVincenzo JP, Wilkinson T, Vaishnaw A, et al. Viral load drives disease in humans experimentally infected with respiratory syncytial virus. Am J Respir Crit Care Med 2010; 182: 1305–1314. doi: 10.1164/rccm.201002-0221OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Habibi MS, Thwaites RS, Chang M, et al. Neutrophilic inflammation in the respiratory mucosa predisposes to RSV infection. Science 2020; 370: 166. doi: 10.1126/science.aba9301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cuthbertson L, Craven V, Bingle L, et al. The impact of persistent bacterial bronchitis on the pulmonary microbiome of children. PLoS ONE 2017; 12: e0190075. doi: 10.1371/journal.pone.0190075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosas-Salazar C, Shilts MH, Tovchigrechko A, et al. Nasopharyngeal microbiome in respiratory syncytial virus resembles profile associated with increased childhood asthma risk. Am J Respir Crit Care Med 2016; 193: 1180–1183. doi: 10.1164/rccm.201512-2350LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sonawane AR, Tian L, Chu CY, et al. Microbiome-transcriptome interactions related to severity of respiratory syncytial virus infection. Sci Rep 2019; 9: 13824. doi: 10.1038/s41598-019-50217-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Steenhuijsen Piters WA, Heinonen S, Hasrat R, et al. Nasopharyngeal microbiota, host transcriptome, and disease severity in children with respiratory syncytial virus infection. Am J Respir Crit Care Med 2016; 194: 1104–1115. doi: 10.1164/rccm.201602-0220OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molyneaux PL, Mallia P, Cox MJ, et al. Outgrowth of the bacterial airway microbiome after rhinovirus exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2013; 188: 1224–1231. doi: 10.1164/rccm.201302-0341OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen EK, Koeppel AF, Hendley JO, et al. Characterization of the nasopharyngeal microbiota in health and during rhinovirus challenge. Microbiome 2014; 2: 22. doi: 10.1186/2049-2618-2-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson ES, Bittinger K, Haas AR, et al. Topographical continuity of bacterial populations in the healthy human respiratory tract. Am J Respir Crit Care Med 2011; 184: 957–963. doi: 10.1164/rccm.201104-0655OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bambery B, Selgelid M, Weijer C, et al. Ethical criteria for human challenge studies in infectious diseases. Public Health Ethics 2016; 9: 92–103. doi: 10.1093/phe/phv026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-01932-2021.Shareable (324.1KB, pdf)