Abstract
The authors present a case of a Baker's cyst in the right leg of an 86-year-old woman, whose presentation was more typical for a deep venous thrombosis. Both conditions have inflammation and acute calf pain. The clinical manifestations, imaging findings, and treatment of this common emergency department presentation are discussed.
Keywords: knee pain, emergency medicine, ultrasonography, popliteal cyst, baker's cyst
Introduction
A Baker's cyst, also known as a popliteal cyst, is caused by fluid distention of the gastrocnemio-semimembranosus bursa and results in a painful synovial-lined fluid sac outside the knee joint due to its communication with the knee cavity [1]. Most often it presents in adults aged 35-70 years. A popliteal cyst is associated with commonly found intra-articular knee disorders, such as osteoarthritis and meniscus tears [2]. Other underlying conditions can include Charcot joint [1], degenerative arthropathy [3], and post-traumatic injury in athletes [4]. Most patients with a popliteal cyst have no symptoms. When symptomatic, the most common complaint is a palpable swelling at the popliteal area with associated vague pain [5]. The incidence of Baker's cyst ranges from 5-38% [6]. In a population of 399 patients with knee pain, the prevalence of popliteal cysts was noted to be 25.8%, increasing in frequency with age [7]. The authors present a classic case of Baker's cyst on the degenerative knee of an elderly woman.
Case presentation
The patient is a healthy 86-year-old lady with no medical problems, who does not take any medications. She presents to the emergency department with right knee pain and swelling. It does not hurt to touch it, but it is difficult to bend it. The patient explained she had been on a long car ride of 16 hours the previous day. She denies any fevers, chills, chest pain, shortness of breath, nausea, vomiting, diarrhea, abdominal pain, headache, or urinary symptoms. She has no history of blood clots and has never been on a blood thinner.
Her vitals are within normal limits, with temperature 98.3ºF, heart rate 85 beats per minute, blood pressure 147/75 mmHg, respiratory rate 16 breaths per minute, and oxygen saturation of 98% on room air.
Physical examination demonstrates swelling, reduced range of motion, and joint effusion of the right knee. There are no signs of erythema, and the skin is intact. There is no tenderness to palpation of the effusion. The right lower extremity is slightly warmer than the left, and attempting to bend the knee beyond 30 degrees results in pain. The calf itself is non-tender, and there are no palpable cords. The thigh area also is non-tender to palpation. The patient has normal femoral, popliteal, and dorsalis pedis pulses. There are no signs or symptoms of compartment syndrome in the right lower extremity. Any pain the patient has is in proportion to the edema, the peripheral circulation is intact, capillary refill is not delayed, and there is no numbness, tingling, or paresthesia. Her laboratory evaluation is unremarkable except for a mildly elevated c-reactive protein and is summarized in Table 1.
Table 1. Patient's laboratory values.
BUN: blood urea nitrogen; GFR: glomerular filtration rate
| Lab | Reference range | Value |
| Sodium | 135-145 mmol/L | 131 L |
| Potassium | 3.5-5.3 mmol/L | 4.1 |
| Chloride | 98-107 mmol/L | 104 |
| Carbon Dioxide | 21-32 mmol/L | 24 |
| Anion Gap | 3 | |
| BUN | 7-18 mg/dL | 10 |
| Creatinine | 0.6-1.3 mg/dL | 0.6 |
| Estimated GFR | < 60 | >60 |
| Glucose | 74-106 mg/dL | 208 H |
| Calcium | 8.4-10.2 mg/dL | 9.2 |
| C-Reactive Protein | 0-0.300 mg/dL | 7.12 H |
| White blood cell count | 4.1-9.3 K/mm3 | 6.9 |
| Hemoglobin | 12.1-15.1 gm/dL | 12.1 |
| Hematocrit | 35.5-46.9 % | 35.9 |
| Platelet Count | 150-450 K/mm3 | 234 |
| Erythrocyte sedimentation rate | 0-20 mm/hr | 12 |
Radiograph of the right knee demonstrates mild osteoarthritis of the medial and lateral knee compartments of the right knee, and a small joint effusion in the suprapatellar recess (Figure 1).
Figure 1. Knee radiograph demonstrating small joint effusion in the suprapatellar recess (arrow).
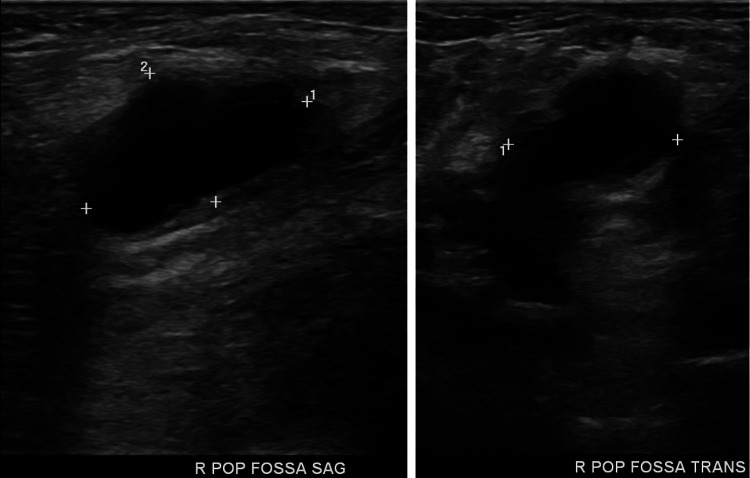
Ultrasonography of the right lower extremity reveals no deep vein thrombosis from the mid-calf to the common femoral vein. Observed is a popliteal cyst in sagittal and transverse views (Figure 2).
Figure 2. Ultrasonography of lower extremity reveals a popliteal cyst (crosshatches).
The patient was given Ketorolac in the emergency department and was discharged home with detailed information on her condition given to both her and her spouse, as well as follow-up with primary care.
Discussion
The diagnosis of a popliteal cyst is most easily made via ultrasonography. Typical findings include anechoic or hypoechoic fluid between the semimembranosus and medial gastrocnemius tendons, and a posterior soft tissue mass or cyst, with an average size of 10cm3 [8]. Magnetic resonance imaging (MRI) will depict a Baker's cyst as a well-defined unilocular or multilocular cystic mass, located posteromedially, arising between the tendon of the semimembranosus and the medial head of gastrocnemius [9,10]. Fluid signal intensity is seen in all sequences in cases of popliteal cysts [10,11].
The most common differential diagnoses include deep vein thrombosis (DVT), cystic masses such as synovial or ganglion cysts, solid masses such as sarcoma and lymphoma, and popliteal artery aneurysms. Of these, DVT is the most common differential diagnosis, especially in the emergency department. In situations where ready imaging is not available, sometimes low molecular weight heparin is administered empirically for presumed DVT. If it is in fact a Baker's cyst rather than a DVT, heparin treatment can actually result in compartment syndrome [12].
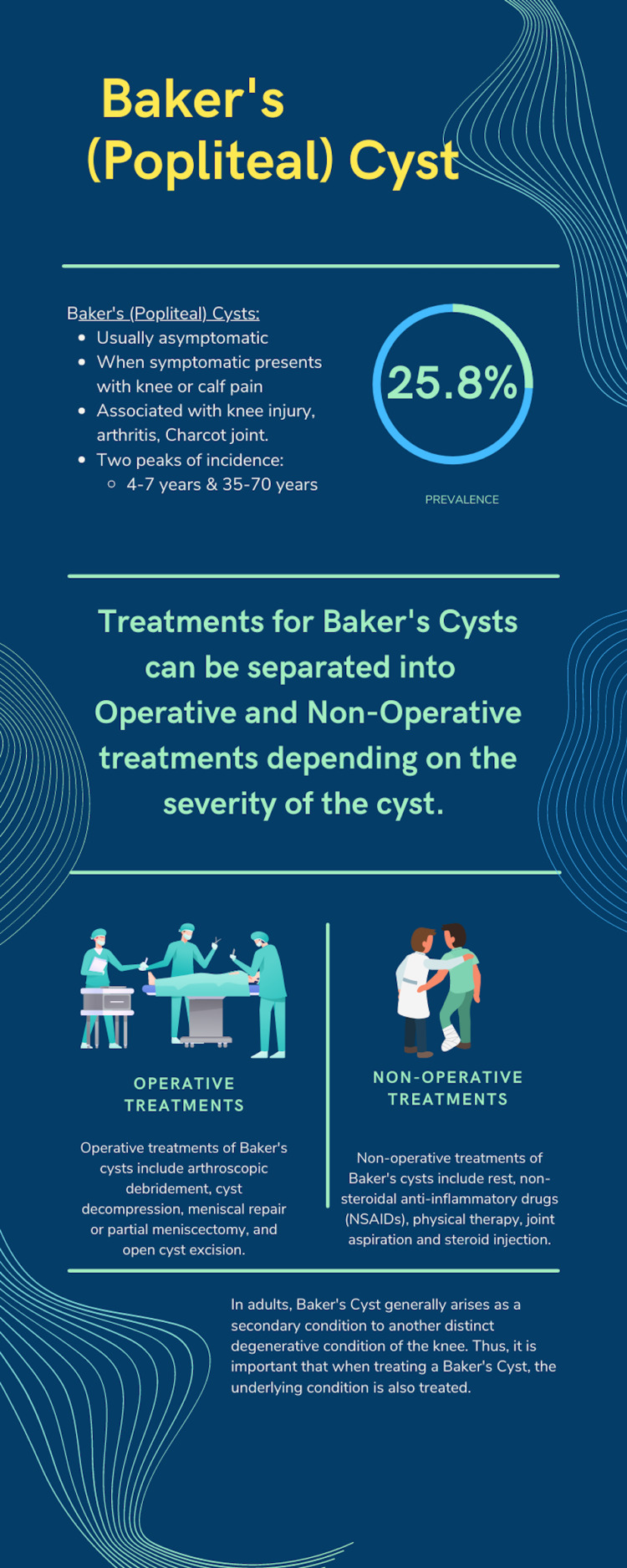
No treatment is necessary for asymptomatic Baker's cysts. Treatment for symptomatic Baker's cysts can be operative or non-operative (Figure 3) [13].
Figure 3. Infographic describing Baker's (popliteal) cyst.
Created by Arjun Nanduri on canva.com (Canva Pty Ltd, Surry Hills, Australia)
Initially, conservative non-operative management is preferred. Options include rest and activity restriction, oral or topical non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, and joint aspiration. Operative management includes arthroscopic debridement, cyst decompression, open cyst excision to surgically remove the cyst, and meniscal repair or partial meniscectomy. The latter often results in cyst recurrence [1]. An important detail to note is the existence of an underlying knee-joint disorder that caused the cyst. Successfully resolving the underlying disorder would reduce the amount of synovial fluid reaching the cyst, thus alleviating the condition. A systematic review of non-operative and operative treatment [13] found that that intracystic corticosteroid injection with cyst fenestration is an effective non-operative treatment method.
Conclusions
A Baker's or popliteal cyst is a benign condition that often presents with acute knee or calf pain. The diagnosis is easily made with imaging and helps to distinguish it from a deep venous thrombosis. Acute management is generally conservative with rest, ice, elevation, and analgesics. Addressing the underlying condition can be curative. Occasionally, surgical intervention may be warranted and is typically performed arthroscopically.
Acknowledgments
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. HCA Centralized Algorithms for Research Rules on IRB Exemption issued approval 2021-524. HCA Centralized Algorithms for Research Rules on IRB Exemptions (CARRIE)/ IRB manager issued exemption [2021-524]. Based on the information provided and attested as true, the research plan described does not require IRB oversight. This is because the investigators are either a) not engaging in research with human subjects as defined by federal regulations; b) engaging in research with human subjects deemed excluded from IRB oversight per 45CFR46.102(l) OR c) engaging in research with sufficient human subject protections in the design to meet one or more IRB exemption criteria set forth in 45CFR46.104.
References
- 1.Baker's cyst imaging. Toussaint SP, McCabe S. Int J Emerg Med. 2010;3:469–470. doi: 10.1007/s12245-009-0157-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker's cyst: diagnostic and surgical considerations. Frush TJ, Noyes FR. Sports Health. 2015;7:359–365. doi: 10.1177/1941738113520130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MR imaging of Baker cysts: association with internal derangement, effusion, and degenerative arthropathy. Miller TT, Staron RB, Koenigsberg T, Levin TL, Feldman F. Radiology. 1996;201:247–250. doi: 10.1148/radiology.201.1.8816552. [DOI] [PubMed] [Google Scholar]
- 4.Longitudinal ultrasound and clinical follow-up of Baker's cysts injection with steroids in knee osteoarthritis. Bandinelli F, Fedi R, Generini S, et al. Clin Rheumatol. 2012;31:727–731. doi: 10.1007/s10067-011-1909-9. [DOI] [PubMed] [Google Scholar]
- 5.Ruptured Baker's cyst: a diagnostic dilemma. Bansal K, Gupta A. Cureus. 2021;13:0. doi: 10.7759/cureus.18501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Efficacy and safety of musculoskeletal ultrasound guided aspiration and intra-lesional corticosteroids injection of ruptured Baker's cyst: a retrospective observational study. Mortada M, Amer YA, Zaghlol RS. Clin Med Insights Arthritis Musculoskelet Disord. 2020;13:1179544120967383. doi: 10.1177/1179544120967383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prevalence of Baker's cyst in patients with knee pain: an ultrasonographic study. Picerno V, Filippou G, Bertoldi I, Adinolfi A, Di Sabatino V, Galeazzi M, Frediani B. Reumatismo. 2014;65:264–270. doi: 10.4081/reumatismo.2013.715. [DOI] [PubMed] [Google Scholar]
- 8.Sonographic detection of Baker's cysts: comparison with MR imaging. Ward EE, Jacobson JA, Fessell DP, Hayes CW, van Holsbeeck M. AJR Am J Roentgenol. 2001;176:373–380. doi: 10.2214/ajr.176.2.1760373. [DOI] [PubMed] [Google Scholar]
- 9.MR imaging of cysts, ganglia, and bursae about the knee. Beaman FD, Peterson JJ. https://pubmed.ncbi.nlm.nih.gov/17981178/ Radiol Clin North Am. 2007;45:969–982. doi: 10.1016/j.rcl.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 10.MRI features of cystic lesions around the knee. Marra MD, Crema MD, Chung M, et al. Knee. 2008;15:423–438. doi: 10.1016/j.knee.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Mimics of bone and soft tissue neoplasms. Stacy GS, Kapur A. https://pubmed.ncbi.nlm.nih.gov/22024298/ Radiol Clin North Am. 2011;49:1261–1286. doi: 10.1016/j.rcl.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Ruptured Baker's cyst: complications due to misdiagnosis [Article in English and Spanish] Tejero S, Fenero-Delgado BT, López-Lobato R, Carranza-Bencano A. https://pubmed.ncbi.nlm.nih.gov/30638346. Emergencias. 2018;30:412–414. [PubMed] [Google Scholar]
- 13.Popliteal cysts: a systematic review of nonoperative and operative treatment. Van Nest DS, Tjoumakaris FP, Smith BJ, Beatty TM, Freedman KB. JBJS Rev. 2020;8:0. doi: 10.2106/JBJS.RVW.19.00139. [DOI] [PubMed] [Google Scholar]