Abstract
Most studies only describe mental health indicators (anxiety, depression, insomnia, and stress) and the risk factors associated with these indicators during the pandemic (sex, student status, and specific physical symptoms). However, no explanatory studies have been found that assess the impact of variables associated with COVID-19. Against this background, the objective of the study was to evaluate the impact of the fear of catching COVID-19 on the level of anxiety, depression, and insomnia in 947 university students of both sexes (41.6% males and 58.4% females) between the ages of 18 and 35 (M = 21.6; SD = 3.4). The Fear of catching COVID-19 Scale, the Generalized Anxiety Disorder Scale (GAD-7), the Patient Health Questionnaire (PHQ-9), and the Insomnia Severity Index (ISI) were used to measure the variables. The results of the study show that the fear of catching COVID-19 significantly influences the level of anxiety (β = .52; p < .01), insomnia (β = .44; p<.01), and depression (β = .50; p < .01) experienced by university students (χ2 = 2075.93; df = 371; p = .000; RMSEA = .070 [CI 90% .067–.073]; SRMR = .055; CFI = .95; TLI = .94). The descriptive results show that a notable percentage of university students present significant symptoms of anxiety (23%), depression (24%), and insomnia (32.9%). It is concluded that the fear of catching COVID-19 is a serious health problem since it influences the appearance of anxiety, depression and insomnia symptoms.
Keywords: Fear of catching COVID-19, COVID-19, Anxiety, Depression, Insomnia, Undergraduate students, Predictive Model
Introduction
The SARS-CoV-2 (COVID-19) pandemic is the largest public health emergency the world has ever faced in recent memory. Various studies have described the mental health problems associated with this pandemic in different groups such as healthcare workers (Muller et al., 2020), clinic patients (Hu et al., 2020), adults (Wang et al., 2020; Xiong et al., 2020), police (Caycho-Rodríguez et al., 2020), school children (Chen et al., 2020), and university students (Khan et al., 2020). In this context, university students are a particularly vulnerable group to develop mental health problems, such as depression, anxiety (Auerbach et al., 2019), and insomnia (Sivertsen et al., 2018) since they are generally in a transition stage in their academic, professional and personal life (Acharya et al., 2018; Zivin et al., 2009). Added to this, the closure of universities, social isolation, the switch to virtual learning platforms, difficulties in accessing technology, economic problems, and family members' deaths due to COVID-19 have exacerbated the risk of suffering mental health issues.
A study carried out in China on medical students reported that 21.3% of those surveyed experienced moderate anxiety (Cao et al., 2020). Another longitudinal study, also conducted in China, estimated a prevalence of 12.4% and 16.8% for anxiety and insomnia respectively in university students (Ge et al., 2020). Similarly, another study conducted in China on university students from the arts and humanities areas evidenced significantly higher anxiety scores than the national average (Wang & Zhao, 2020). In Bangladesh, a study reported that 33.3% of university students surveyed experienced anxiety and 46.9% experienced depression (Khan et al., 2020). Similarly, another study in New Jersey reported high levels of anxiety and depression (Kecojevic et al., 2020). In Germany, a study showed that 35.9% of university students evaluated had a moderate to severe level of depression, and 27.7% reported moderate to severe anxiety symptoms (Karing, 2021). Studies carried out in France also showed that university students experienced a significant increase in anxiety and stress during confinement (Essadek & Rabeyron, 2020; Husky et al., 2020). Another study in Argentina reported that 23% of the university students evaluated had moderate insomnia and 4% severe insomnia (Scotta et al., 2021). In Peru, a study carried out on dentistry students showed that 47.4% had moderate anxiety, and 8.4% had severe anxiety (Cayo-Rojas et al., 2021). In previous epidemics, acute infectious diseases such as SARS and H1N1 were also associated with high levels of anxiety, depression, and stress in the university population (Main et al., 2011; Wu et al., 2005a, b).
Against this backdrop, the review of the scientific literature reported some limitations in studies conducted in university populations. First, most studies only describe mental health indicators (anxiety, depression, insomnia, and stress) and the risk factors associated with these indicators during the pandemic (sex, student status, specific physical symptoms, and self-rated health status). However, no explanatory studies have been found that assess the impact of variables associated with COVID-19, such as fear or concern about its contagiousness. Second, no explanatory studies assessing the impact of variables associated with COVID-19 on mental health status have been found in the Latin American region, despite the fact that to date, as of the time of the submission of this article, there are 71,055,452 confirmed cases of COVID-19 in the Americas, the region with the highest infection rates (World Health Organization, 2020). Fourth, no reports were found regarding the level of anxiety, depression and insomnia in undergraduate students in the Latin American region.
In this context, it is essential not only to collect information on the rates of anxiety, depression, and other mental health indicators but also to determine causal mechanisms that explain mental health problems during and after the pandemic (Holmes et al., 2020). Especially in vulnerable groups like university students.
Concerning this, no theoretical models have been found to explain emotional reactions during pandemics (Taylor, 2019). However, a definition has recently been proposed that attempts to explain the fear of COVID-19. This construct called coronaphobia is defined as the intense fear of catching COVID-19, which causes a physiological response (palpitations, tremors, shortness of breath, dizziness, change in appetite, and sleep) accompanied by catastrophic thoughts that trigger emotional responses such as sadness, guilt, and anger. All this causes avoidance behaviors that interfere with the person's quality of life (Arora et al., 2020). Therefore, to measure the state of mental health, three principal indicators usually reported in the scientific literature will be used: anxiety, depression, and insomnia (Korkeila et al., 2003; Lin et al., 2020; Pigeon et al., 2017). Based on the exposed gaps in the literature, this study aims to (a) measure the levels of fear of catching COVID-19, anxiety, depression, and insomnia in university students and any possible differences depending on gender and (b) assess the impact of the fear of catching COVID-19 on the level of anxiety, depression, and insomnia in undergraduate students.
Method
Participants
A non-probability sample was used for data collection, employing the following inclusion criteria: (a) informed consent of participants, (b) no more than 40 years old, (c) ability to read and write in Spanish, (d) being enrolled in a university program. A sample of 947 Peruvian undergraduate students of both sexes (41.6% males and 58.4% females) between 18 and 35 years old was collected (M = 21.6; SD = 3.4). The professional careers most studied by the university students in the sample were psychology (49.8%), food engineering (12.5%), and communication sciences (6%). The study was carried out in three cities in Peru: Lima, Tarapoto, and Juliaca.
Instruments
The Fear of Catching COVID-19 Scale
Created by Caycho-Rodríguez et al. (2021) with the objective of evaluating the concern about the spread of COVID-19 and the impact that this concern can have on people's daily functioning (specifically on their mood and their ability to carry out their daily activities). It is made up of six items that have four response options (1 = Never or rarely to 4 = Nearly all the time), where high scores indicate more frequent concern. In the present study, the one-dimensional model presented adequate indices of reliability (α = 0.92; ω = 0.89) and validity based on internal structure (χ2 = 163.76; df = 9; p = 0.000; CFI = 0.99; TLI = 0.98; RMSEA = 0.131; SRMR = 0.037).
Generalized Anxiety Disorder Scale (GAD-7)
Developed by Spitzer et al. (2006) and adapted to Spanish by García-Campayo et al. (2010), this scale is made up of seven items that have four response categories ranging from "never" (0) to "almost every day" (3), where a higher score indicates a greater presence of the disorder. A cut-off point of 10 points was used to assess the presence of significant symptoms of generalized anxiety disorder (García-Campayo et al., 2010). In the present study, the one-dimensional model presented adequate indices of reliability (α = 0.93; ω = 0.89) and validity based on internal structure (χ2 = 174.73; df = 14; p = 0.000; CFI = 0.99; TLI = 0.99; RMSEA = 0.107; SRMR = 0.033).
Patient Health Questionnaire (PHQ-9)
Developed by Spitzer et al. (1999) and adapted into Spanish by Zhong et al. (2014), this questionnaire consists of nine items that have four categories ranging from "not at all" (0) to "almost every day" (3). A 10-point cut-off point was used to assess the presence of significant symptoms of depression (Manea et al., 2012). In the present study, the one-dimensional model presented adequate indices of reliability (α = 0.92; ω = 0.90) and validity based on internal structure (χ2 = 132.39; df = 27; p = 0.000; CFI = 0.99; TLI = 0.98; RMSEA = 0.062; SRMR = 0.032).
Insomnia Severity Index (ISI)
Developed by Bastien et al. (2001) and adapted into Spanish by Fernandez-Mendoza et al. (2012), this instrument consists of seven items that have five response categories ranging from "nothing" (0) to "very much" (4). A 10-point cut-off was used to assess the presence of significant symptoms of insomnia (Morin et al., 2011). In the present study, the one-dimensional model presented adequate indices of reliability (α = 0.88; ω = 0.91) and validity based on internal structure (χ2 = 503.58; df = 14; p = 0.000; CFI = 0.94; TLI = 0.91; RMSEA = 0.187; SRMR = 0.072).
Procedure
For this study, the approval of the ethics committee of the Center for Research and Innovation in Health (CIISA) of the Universidad Peruana Unión and was obtained and the standards of the Declaration of Helsinki (Rickman, 1964; World Medical Association, 2013) were met. The data collection was done through a virtual form, using the digital platform Google Forms. In the first part of the virtual form, the objectives of the study were explained, the time required to complete the form was presented and informed was requested, where the confidentiality of the information was assured with the assurance that the participants could withdraw at any time. Only participants who gave their informed consent could complete the following sections of the form. The virtual form was applied during the virtual classes of the university students, and it was also sent to their emails.
Data Analysis
For the Structural Equation Model (SEM) the WLSMV estimator was used and to evaluate the adjustment of the proposed model the CFI (> 0.90), TLI (> 0.90), RMSEA (< 0.08) and SRMR (< 0.08) coefficients were used. In order to evaluate the adjustment indexes, the criteria proposed by Kline (2015) and Schumacker and Lomax (2015) were used. As for the measurement models, a Confirmatory Factor Analysis (CFA) was carried out using the WLSMV estimator and the adjustment indicators carried out in the SEM model were taken into account.
The lavaan package (Rosseel, 2012) was used for the Structural Equation Model (SEM), the semTools package (Jorgensen et al., 2018) for factorial invariance and the ggstatsplot package (Patil, 2018) for the comparative analysis by sex. For all statistical analyses, the RStudio environment was used (RStudio Team, 2018) for R (R Core Team, 2019).
Results
Descriptive Analysis of Anxiety, Depression and Insomnia in University Students
Table 1 shows that 23% of university students presented significant symptoms of anxiety. Similarly, 24% and 32.9% showed significant symptoms of depression and insomnia, respectively.
Table 1.
Descriptive analysis of anxiety, depression and insomnia
| Absence / Minimal symptoms | Significant symptoms | |||
|---|---|---|---|---|
| n | % | n | % | |
| Anxiety | 729 | 77% | 218 | 23% |
| Depression | 720 | 76% | 227 | 24% |
| Insomnia | 635 | 67.1% | 312 | 32.9% |
Fear of Catching COVID-19 Based on Sex
Before performing the comparative analysis, the factorial structure of the scale was verified to be invariant for the groups of men and women in the sequence of invariance models proposed: metric (ΔCFI = -0.002), scalar (ΔCFI = -0.003) and strict invariance (ΔCFI = 0.001). No significant difference was found in men’s (M = 5.51, DS = 3.77) and women’s (M = 5.74, DS = 3.45) scores for the fear of catching COVID-19 (tWelch (799.52) = -0.97, p = 0.331, dCohen = 0.07, CI99% [-0.23 – 0.10]).
Predictive Model
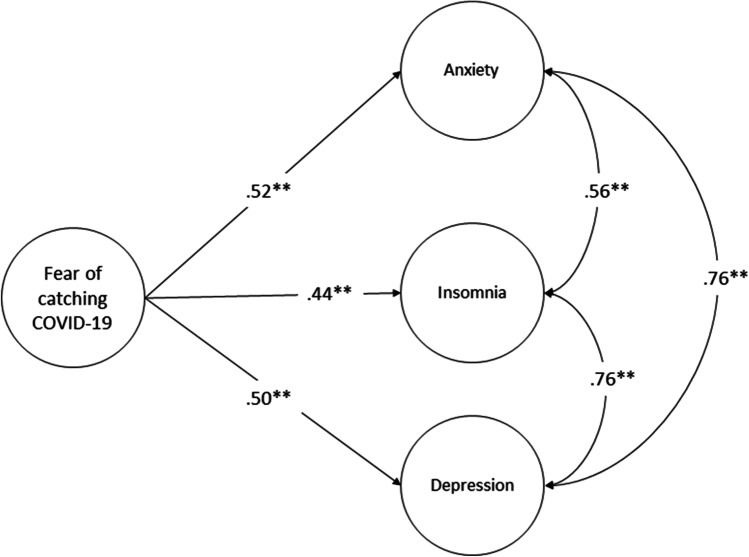
Table 2 shows that the structural model has adequate adjustment indexes (χ2 = 2075.93; df = 371; p = 0.000; RMSEA = 0.070 [CI 90% 0.067–0.073]; SRMR = 0.055; CFI = 0.95; TLI = 0.94) and the measurement models are adequately represented by their items. Figure 1 shows that the degree of concern about getting COVID-19 significantly influences the level of anxiety (β = 0.52; p < 0.01), insomnia (β = .44; p < .01) and depression (β = .50; p < .01) experienced by university students.
Table 2.
Structural model and measurement models
| Structural model | ||||||||
| X2 | df | p | RMSEA | 90% CI | SRMR | CFI | TLI | |
| 2075.93 | 371 | .000 | .070 | .067–.073 | .055 | .95 | .94 | |
| Measurement models | ||||||||
| Items | Fear of catching COVID-19 | Anxiety | Depression | Insomnia | ||||
| λ (error) | λ (error) | λ (error) | λ (error) | |||||
| 1 | .78 (.39) | .81 (.34) | .73 (.47) | .85 (.28) | ||||
| 2 | .88 (.22) | .82 (.33) | .82 (.33) | .83 (.32) | ||||
| 3 | .81 (.34) | .94 (.12) | .81 (.35) | .54 (.71) | ||||
| 4 | .88 (.22) | .83 (.31) | .77 (.41) | .72 (.48) | ||||
| 5 | .91 (.18) | .79 (.38) | .73 (.47) | .79 (.38) | ||||
| 6 | .75 (.44) | .73 (.46) | .81 (.34) | .76 (.42) | ||||
| 7 | .82 (.33) | .76 (.43) | .81 (.34) | |||||
| 8 | .77 (.40) | |||||||
| 9 | .68 (.53) | |||||||
Note: λ: Factorial load
Fig. 1.
Predictive model of fear of catching COVID-19
Discussion
The results of this study show that a notable percentage of university students present significant symptoms of anxiety (23%), depression (24%) and insomnia (32.9%). It was found that the prevalence of anxiety is higher than that reported by Ge et al. (2020) and Cao et al. (2020) in China (12.4% and 21.3% respectively) and it is also higher than the levels reported by Saraswathi et al. (2020) in India (21.2%). However, it is lower than that found by Khan et al. (2020) in Bangladesh (33.3%) and Cayo-Rojas et al. (2021) in Peru (47.4%). Regarding the prevalence of depression, the present results are lower than those reported by Khan et al. (2020) and Saraswathi et al. (2020) in Bangladesh (46.9%) and India (33.2%), respectively. The prevalence of insomnia was found to be higher than that estimated by Ge et al. (2020) in China (16.8%) and Scotta et al. (2021) in Argentina (23%). It is worth noting that there are few studies that evaluate the prevalence of insomnia in the university population.
The variability observed concerning the different studies could be explained by the differences in the sample size used in the previous studies. The range of sample sizes varied between 217 (Saraswathi et al., 2020) and 7143 students (Cao et al., 2020). Also, it could be explained by the type of instruments used to measure the variables (Bukumiric et al., 2016; Guerra et al., 2016) and the cultural context to which the university students belong (Hofmann & Hinton, 2014; Smith et al., 2016).
Regarding the level of fear of catching COVID-19 according to sex, it was found that there are no significant differences between men and women. This result differs from what was found in another study (Rodríguez-Hidalgo et al., 2020). This could be explained by the sample size and age range of the evaluated participants in each study. In the study by Rodríguez-Hidalgo et al. (2020) there is a higher proportion of women (72%) than men (28%) and the age range is wider (18–47 years). In contrast, in the present study the proportion of women (58.4%) and men (41.6%) was more balanced and the age range was smaller (18 to 35 years). Furthermore, it is important to mention that the present study corroborated the factorial invariance of the scale, to avoid a possible bias in the comparison of the scores.
The main result of this study shows that the concern about COVID-19 has a negative impact on some mental health indicators in university students. This result is consistent with previous studies that indicate that long periods of infectious epidemics can negatively affect the people’s psychological states (Lee et al., 2007; Pappas et al., 2009; Wu et al., 2005a; Yang et al., 2021). Specifically, it was found that the concern about catching the virus explains 52% of the anxiety symptoms and 50% of the depression symptoms experienced by undergraduate students. These symptoms could be explained by the negative consequences that getting COVID-19 would have on one’s own health, their family's health, their educational progress and their professional future. Also, it could be related to the fear of being stigmatized by their social circle.
It was also found that the fear of catching the virus explains 44% of the symptoms of insomnia. This is because fear and constant worry cause a serious cognitive disturbance which affects the quality of sleep (Kalmbach et al., 2018). In addition, this result coincides with that found in an adult population (Kokou-kpolou et al., 2020; Voitsidis et al., 2020).
Regarding the limitations of this study, firstly, non-probabilistic sampling was used, which limits the generalizability of the results. Future studies should use representative samples to confirm the results. Second, only self-report measures were used, which can be affected by the participants’ perception of social desirability. Thus future studies should use qualitative interviews or case studies to overcome this limitation. Third, a cross-sectional design was used, so the model should be studied using a longitudinal design in future studies in order to better understand the variables. Fourth, the model did not include variables such as cognitive flexibility (Pakenham et al., 2020), social support (Lee & You, 2020), and knowledge about COVID-19 (Rodríguez-Rey et al., 2020) which could mediate the effect of concern about becoming infected on mental health indicators. Despite these limitations, this study provides a conceptual and statistical basis for a better understanding of the psychological impact of COVID-19 in the university population.
In conclusion, worrying about getting COVID-19 is a serious health problem since it influences the appearance of symptoms of anxiety, depression and insomnia. In addition, it was found that a significant percentage of university students present clinical symptoms of anxiety, depression and insomnia. Therefore, governments and universities should work together to provide timely and quality psychological services to address this public health problem.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors state that they have no real, potential or apparent conflict of interest.
Ethical approval
All procedures performed in the study were approved by the university's ethics committee and conformed to the requirements of the 1975 Declaration of Helsinki.
Informed consent
Informed consent was obtained from all participants included in the study.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Acharya L, Jin L, Collins W. College life is stressful today–Emerging stressors and depressive symptoms in college students. Journal of American College Health. 2018;66(7):655–664. doi: 10.1080/07448481.2018.1451869. [DOI] [PubMed] [Google Scholar]
- Arora A, Kumar A, Alat P, Sekhar S. Understanding coronaphobia Alisha. Asian Journal of Psychiatry. 2020;54:102384. doi: 10.1016/j.ajp.2020.102384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach R, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, Demyttenaere K, Ebert D, Green J, Murray E, Nock M, Pinder-amaker S, Sampson N, Stein D, Vilagut G, Zaslavsky A, Kessler R. Student Project : Prevalence and Distribution of Mental Disorders. Journal of Abnormal Psychology. 2019;127(7):623–638. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine. 2001;2(4):297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bukumiric Z, Starcevic V, Stanisavljevic D, Marinkovic J, Milic N, Djukic-Dejanovic S, Janjic V, Corac A, Ilic A, Kostic M, Nikolic I, Trajkovic G. Meta-analysis of the changes in correlations between depression instruments used in longitudinal studies. Journal of Affective Disorders. 2016;190:733–743. doi: 10.1016/j.jad.2015.10.054. [DOI] [PubMed] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research Journal. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T, Carbajal-León C, Vilca LW, Heredia-Mongrut J, Gallegos M. COVID-19 y salud mental en policías peruanos: resultados preliminares. Acta Médica Peruana. 2020;37(3):396–398. doi: 10.35663/amp.2020.373.1503. [DOI] [Google Scholar]
- Caycho-Rodríguez T, Ventura-León J, Barboza-Palomino M. Design and validation of a scale to measure worry for contagion of the COVID-19 (PRE-COVID-19) Enfermeria Clinica. 2021;31(3):175–183. doi: 10.1016/j.enfcli.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cayo-Rojas CF, Castro-Mena MJ, Agramonte-Rosell RC, Aliaga-Mariñas AS, Ladera-Castañeda MI, Cervantes-Ganoza LA, Cervantes-Liñán LC. Impact of COVID-19 Mandatory Social Isolation on the Development of Anxiety in Peruvian Dentistry Students: A Logistic Regression Analysis. Journal of International Society of Preventive & Community Dentistry. 2021;11(2):222–229. doi: 10.4103/jispcd.JISPCD_52_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Liang S, Peng Y, Li X, Chen J, Tang S, Zhao J. Mental health status and change in living rhythms among college students in China during the COVID-19 pandemic: A large-scale survey. Journal of Psychosomatic Research. 2020;137(August):110219. doi: 10.1016/j.jpsychores.2020.110219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essadek A, Rabeyron T. Mental health of French students during the Covid-19 pandemic. Journal of Affective Disorders. 2020;277:392–393. doi: 10.1016/j.jad.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Mendoza J, Rodriguez-Muñoz A, Vela-Bueno A, Olavarrieta-Bernardino S, Calhoun SL, Bixler EO, Vgontzas AN. The Spanish version of the Insomnia Severity Index: A confirmatory factor analysis. Sleep Medicine. 2012;13(2):207–210. doi: 10.1016/j.sleep.2011.06.019. [DOI] [PubMed] [Google Scholar]
- García-Campayo, J., Zamorano, E., Ruiz, M. A., Pardo, A., Pérez-Páramo, M., López-Gómez, V., Freire, O., & Rejas, J. (2010). Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes, 8(8). 10.1186/1477-7525-8-8 [DOI] [PMC free article] [PubMed]
- Ge F, Zhang D, Wu L, Mu H. Predicting psychological state among chinese undergraduate students in the covid-19 epidemic: A longitudinal study using a machine learning. Neuropsychiatric Disease and Treatment. 2020;16:2111–2118. doi: 10.2147/NDT.S262004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra M, Prina AM, Ferri CP, Acosta D, Gallardo S, Huang Y, Jacob KS, Jimenez-Velazquez IZ, Llibre Rodriguez JJ, Liu Z, Salas A, Sosa AL, Williams JD, Uwakwe R, Prince M. A comparative cross-cultural study of the prevalence of late life depression in low and middle income countries. Journal of Affective Disorders. 2016;190:362–368. doi: 10.1016/j.jad.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann, S. G., & Hinton, D. E. (2014). Cross-cultural aspects of anxiety disorders. Current Psychiatry Reports, 16(6). 10.1007/s11920-014-0450-3 [DOI] [PMC free article] [PubMed]
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Cohen Silver, R., Everall, I., Ford, T., John, A., Kabir, T., King, K., Madan, I., Michie, S., Przybylski, A. K., Shafran, R., Sweeney, A., … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed]
- Hu Y, Chen Y, Zheng Y, You C, Tan J, Hu L, Zhang Z, Ding L. Brain, Behavior, and Immunity Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behavior and Immunity. 2020;89(May):587–593. doi: 10.1016/j.bbi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husky MM, Kovess-Masfety V, Swendsen JD. Stress and anxiety among university students in France during Covid-19 mandatory confinement. Comprehensive Psychiatry. 2020;102:152191. doi: 10.1016/j.comppsych.2020.152191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorgensen, T. D., Pornprasertmanit, S., Schoemann, A. M., & Rosseel, Y. (2018). semTools: Useful tools for structural equation modeling. R package version 0.5–1. https://cran.r-project.org/package=semTools
- Kalmbach DA, Cuamatzi-Castelan AS, Tonnu CV, Tran KM, Anderson JR, Roth T, Drake CL. Hyperarousal and sleep reactivity in insomnia: Current insights. Nature and Science of Sleep. 2018;10:193–201. doi: 10.2147/NSS.S138823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karing C. Prevalence and predictors of anxiety, depression and stress among university students during the period of the first lockdown in Germany. Journal of Affective Disorders Reports. 2021 doi: 10.1016/j.jadr.2021.100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Basch CH, Sullivan M, Davi NK. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS ONE. 2020;15(9):e0239696. doi: 10.1371/journal.pone.0239696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. Journal of A ff ective Disorders The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. Journal of Affective Disorders. 2020;277(May):121–128. doi: 10.1016/j.jad.2020.07.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 4. The Guilford Press; 2015. [Google Scholar]
- Kokou-kpolou CK, Megalakaki O, Laimou D, Kousouri M. factors in French population. Psychiatry Research. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkeila J, Lehtinen V, Bijl R, Dalgard OS, Kovess V, Morgan A, Salize HJ. Review Article: Establishing a set of mental health indicators for Europe. Scandinavian Journal of Public Health. 2003;31(6):451–459. doi: 10.1080/14034940210165208. [DOI] [PubMed] [Google Scholar]
- Lee AM, Wong JGWS, McAlonan GM, Cheung V, Cheung C, Sham PC, Chu NM, Wong PC, Tsang KWT, Chua SE. Stress and psychological distress among SARS survivors 1 year after the outbreak. Canadian Journal of Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lee M, You M. Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19) International Journal of Environmental Research and Public Health. 2020;17(9):2977. doi: 10.3390/ijerph17092977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YH, Chiang TW, Lin YL. Increased internet searches for insomnia as an indicator of global mental health during the COVID-19 pandemic: Multinational longitudinal study. Journal of Medical Internet Research. 2020;22(9):1–7. doi: 10.2196/22181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main A, Zhou Q, Ma Y, Luecken LJ, Liu X. Relations of sars-related stressors and coping to chinese college students’ psychological adjustment during the 2003 beijing sars epidemic. Journal of Counseling Psychology. 2011;58(3):410–423. doi: 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. Canadian Medical Association Journal. 2012;184(3):191–196. doi: 10.1503/cmaj.112004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SO, Stroobants S, Van de Velde S, Vist GE. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research. 2020;293(August):113441. doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakenham KI, Landi G, Boccolini G, Furlani A, Grandi S, Tossani E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science. 2020;17(July):109–118. doi: 10.1016/j.jcbs.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas G, Kiriaze IJ, Giannakis P, Falagas ME. Psychosocial consequences of infectious diseases. Clinical Microbiology and Infection. 2009;15(8):743–747. doi: 10.1111/j.1469-0691.2009.02947.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil, I. (2018). ggstatsplot: “ggplot2” Based Plots with Statistical Details. https://cran.r-project.org/web/packages/ggstatsplot/index.html
- Pigeon, W. R., Bishop, T. M., & Krueger, K. M. (2017). Insomnia as a Precipitating Factor in New Onset Mental Illness: a Systematic Review of Recent Findings. Current Psychiatry Reports, 19(8). 10.1007/s11920-017-0802-x [DOI] [PubMed]
- R Core Team. (2019). A language and environment for statistical computing (R version 3.6.1). R Foundation for Statistical Computing. http://www.r-project.org/
- Rickman PP. Human Experimentatio: Code of ethics of the world medical association. Declaration of Helsinki. British Medical Journal. 1964;2(5402):177. doi: 10.1136/bmj.2.5402.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Hidalgo, A. J., Pantaleón, Y., Dios, I., & Falla, D. (2020). Fear of COVID-19, Stress, and Anxiety in University Undergraduate Students: A Predictive Model for Depression. Frontiers in Psychiatry, 11(591797). 10.3389/fpsyg.2020.591797 [DOI] [PMC free article] [PubMed]
- Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological Impact and Associated Factors During the Initial Stage of the Coronavirus (COVID-19) Pandemic Among the General Population in Spain. Frontiers in Psychology. 2020;11(June):1540. doi: 10.3389/fpsyg.2020.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. lavaan: An R package for structural equation modeling. Journal of Statistical Software. 2012;48(2):1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- RStudio Team. (2018). RStudio: Integrated Development Environment for R. RStudio, Inc. http://www.rstudio.com/
- Saraswathi I, Saikarthik J, Kumar KS, Srinivasan KM, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study. Peer J. 2020;8:e10164. doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling: Fourth Edition. 4. Routledge; 2015. [Google Scholar]
- Scotta, A. V., Cortez, M. V., & Miranda, A. R. (2021). Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychology, Health and Medicine, 1–16. 10.1080/13548506.2020.1869796 [DOI] [PubMed]
- Sivertsen B, Vedaa Ø, Harvey AG, Glozier N, Pallesen S, Aarø LE, Lønning KJ, Hysing M. Sleep patterns and insomnia in young adults: A national survey of Norwegian university students. Journal of Sleep Research. 2018;28(2):1–10. doi: 10.1111/jsr.12790. [DOI] [PubMed] [Google Scholar]
- Smith PB, Easterbrook MJ, Celikkol GC, Chen SX, Ping H, Rizwan M. Cultural Variations in the Relationship Between Anger Coping Styles, Depression, and Life Satisfaction. Journal of Cross-Cultural Psychology. 2016;47(3):441–456. doi: 10.1177/0022022115620488. [DOI] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing; 2019. [Google Scholar]
- Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, Syngelakis M, Holeva V, Diakogiannis I. Letter to the Editor Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Research. 2020;289(May):113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Zhao H. The Impact of COVID-19 on Anxiety in Chinese University Students. Frontiers in Psychology. 2020;11(January):1–8. doi: 10.3389/fpsyg.2020.01168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Coronavirus Disease (COVID-19) Dashboard. Retrieved June 24, 2021 from https://covid19.who.int/
- World Medical Association World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. Clinical Review & Education Special. 2013;27(20):2191–2194. doi: 10.1001/jama.292.11.1359. [DOI] [PubMed] [Google Scholar]
- Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) Journal of Traumatic Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerging Infectious Diseases. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277(August):55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C, Chen A, Chen Y. College students’ stress and health in the COVID-19 pandemic: The role of academic workload, separation from school, and fears of contagion. PLoS ONE. 2021;16(2):e0246676. doi: 10.1371/journal.pone.0246676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Q, Gelaye B, Fann JR, Sanchez SE, Williams MA. Cross-cultural validity of the Spanish version of PHQ-9 among pregnant Peruvian women: A Rasch item response theory analysis. Journal of Affective Disorders. 2014;158:148–153. doi: 10.1016/j.jad.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin K, Eisenberg D, Gollust SE, Golberstein E. Persistence of mental health problems and needs in a college student population. Journal of Affective Disorders. 2009;117(3):180–185. doi: 10.1016/j.jad.2009.01.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.