Abstract
Background
In the Veneto Region, 421,000 coronavirus 2019 disease (COVID-19) cases and 11,000 deaths have been reported since 21 February 2020. The pandemic spread particularly in nursing homes (NH).
Objective
This study estimated the impact of SARS-CoV-2 infection among NH residents, focusing on the risk of hospitalisation and death due to COVID-19 compared with the general older population. It also provided evidence of risk changes over time.
Methods
Older people, resident in Veneto, were enrolled from the regional registry of the population. We collected also information about demographic characteristics, chronic diseases, COVID-19 positivity, NH institutionalization, hospitalisation and date of death. Patients were assigned to NH or non-NH residents groups through a propensity score 1:1 matching. The follow-up period was defined as 21 February 2020 – 3 May 2021 and then divided into three waves. Risk ratios (RRs) and 95% confidence interval were estimated by using Poisson models with robust estimation of variance.
Results
NH residents showed a higher risk of COVID-19 infection (RR = 6.28; 6.03–6.54), hospitalisation for COVID-19 (RR = 2.20; 2.05–2.36) and death with COVID-19 (RR = 6.07; 5.58–6.61).
Conclusion
NH residents shared common spaces with other patients and healthcare professionals and were more exposed to infections. Nonetheless, in Italy from late December 2020 to May 2021, 95% of NH residents and their healthcare professionals received at least one vaccine dose and RRs for all outcomes decreased in NH.
Keywords: nursing homes, coronavirus 2019 disease (COVID-19), older people, vaccination, north-east Italy
Key Points
More than 421,000 cases of SARS-CoV-2 infection and about 11,000 COVID-19 patients’ deaths were reported since the beginning of the pandemic in the Veneto Region.
NH residents showed a higher risk of COVID-19(COVID-19_ infection, of hospitalisation for COVID-19 and of death with COVID-19).
By the end of the COVID-19 vaccination programme in NH, the risk of SARS-CoV-2 infection in NH residents was significantly reduced, in particular for severe forms of COVID-19.
Background
The first cases of coronavirus 2019 disease (COVID-19) reported in Italy were detected on 21 February 2020 in Codogno (Lombardy) and in Vo’ (Veneto) [1]. In February 2020, the first death due to COVID-19 in Europe was reported in Schiavonia Hospital, near Padua [2]. At the time of writing, more than 421,000 cases of SARS-CoV-2 infection [3] and about 11,000 COVID-19 patients’ deaths [4] were reported since the beginning of the pandemic in the Veneto Region, a large area in North-East Italy with more than 4.9 million inhabitants.
Most people affected by COVID-19 are asymptomatic or oligosymptomatic [5], but a small proportion of patients experience a severe interstitial pneumonia and multiple organ failure, especially older people or patients with chronic conditions. Many researchers [6–9] reported—for these categories—higher risks of hospitalisation and admission to intensive care units.
The COVID-19 pandemic in Italy has challenged the national and regional health systems. The Veneto Region was one of the most affected areas from March to May 2020 and from November 2020 to January 2021. The pandemic spread particularly in nursing homes (NH); the older people admitted in these facilities experienced the highest figures of severe subjects and deaths due to COVID-19 [10], because of their frail conditions and the spread within the care setting [11, 12]. In 2018, the Italian National Statistics Institute (ISTAT) reported about 35,000 subjects in NH in the Veneto Region (about 31 per 1,000 inhabitants over 65 years) [13].
The first aim of this study was to estimate the impact of SARS-CoV-2 infection among NH residents in the Veneto Region, focusing on the risk of hospitalisation and death due to COVID-19, in comparison with the general older population. The second aim was to estimate the change of these risks over time (i.e. different waves of infection), as well as the impact of vaccination on NH residents.
Methods
All residents in the Veneto Region aged between 70 and 100 and alive on 21 February 2020 were anonymously tracked from the regional electronic registry of the resident population. The information about NH institutionalization was retrieved from the regional NH archive, described in a previous study [14]. The admission in NH follows a comprehensive assessment of the health and functional status and a social support evaluation; a definitive transition into the NH is usually planned for the eligible residents. Regional NH archive also provided information on admission and discharge dates, demographic data and clinical functional assessment before entry. SARS-CoV-2 infection was retrieved from the regional archive of SARS-CoV-2 RT-PCR tests. Information about COVID-19 patients’ hospitalisation for SARS-CoV-2 infection and date of death related to SARS-CoV-2 infection were updated by hospitals and the public health local services. COVID-19-related deaths were attributed following the guidelines defined by the World Health Organization and the National Health Institute [15].
Evidence about previous chronic diseases (present on 31 December 2019) was retrieved from the regional Johns Hopkins’ Adjusted Clinical Groups (ACG©) archive. The ACG© regional archive, adopted to assess comorbidities affecting study subjects, provides several risk assessment measures using diagnosis codes obtained from multiple sources and assigning patients to categories, strictly associated with specific disease conditions [16]. It also provides the presence of the most important chronic diseases for subjects in the archive at the end of each calendar year.
The follow-up period was determined between 21 February 2020 and 3 May 2021. We also defined three different waves for the pandemic spread in the Veneto Region: the first from 21 February to 31 August 2020, the second from 1 September 2020 to 1 January 2021 and the third from 1 February to 3 May 2021.
Patients were assigned to two main groups (NH residents vs. non-NH residents) through a propensity score 1:1 matching [17] to provide unbiased estimates. We matched the patients for age group, gender, province of domicile, presence of legal disability (over 66%) and the most common chronic diseases: hypertension (HT), diabetes (DM), ischemic heart disease (IHD), chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), chronic renal failure (CRF), dementia (D).
The main outcome of this study was the risk of having a SARS-CoV-2 infection; two secondary outcomes were the risk of hospitalisation due to COVID-19 and the risk of death with COVID-19. We analysed the outcomes considering both the whole period of pandemic and the previously described three waves.
To avoid biased estimations of the total number of subjects at risk, the subjects who died (for any cause of death) or were affected by COVID-19 during the first wave were not included in the following waves, as well as the ones who died or were affected by COVID-19 in the second wave were not included in the third. We estimated risk ratios (RRs) and confidence intervals (CIs) at 95% level for the outcomes. The analysis was performed by Poisson models with robust estimation of variance. We analysed the data using SAS Enterprise Guide 6.1 and STATA/IC 16.0 software for Windows.
Results
Overall, 852,211 living subjects at 21 February 2020, residents in Veneto Region and aged between 70 and 100 years were included in the study; 495,774 subjects (58.2%) were aged 70–79, 292,055 (34.3%) were aged 80–89 and 64,382 (7.6%) 90–100. 491,458 (57.7%) were females and 360,753 were males (42.3%), as shown in Table 1.
Table 1.
Pre-matching distribution of study subjects. Absolute frequencies, percentages and P values according to the characteristics of all NH and non-NH residents
| Total | Non-NH residents | NH residents | P value | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Total | 852,211 | 818,619 | 33,592 | |||
| Gender | <0.001 | |||||
| Females | 491,458 | 466,006 | 56.9 | 25,452 | 75.8 | |
| Males | 360,753 | 352,613 | 43.1 | 8,140 | 24.2 | |
| Age group (years) | <0.001 | |||||
| 70–79 | 495,774 | 489,875 | 59.8 | 5,899 | 17.6 | |
| 80–89 | 292,055 | 278,887 | 33.7 | 16,168 | 48.1 | |
| 90–100 | 64,382 | 52,857 | 6.5 | 11,525 | 34.3 | |
| Province of domicile | <0.001 | |||||
| Belluno | 40,335 | 37,820 | 4.6 | 2,515 | 7.5 | |
| Padua | 158,950 | 154,030 | 18.8 | 4,920 | 14.7 | |
| Rovigo | 45,948 | 43,901 | 5.4 | 2,047 | 6.1 | |
| Treviso | 147,514 | 141,116 | 17.2 | 6,398 | 19.1 | |
| Venice | 161,321 | 156,503 | 19.1 | 4,818 | 14.3 | |
| Vicenza | 142,719 | 135,732 | 16.6 | 6,987 | 20.8 | |
| Verona | 155,424 | 149,517 | 18.3 | 5,907 | 17.6 | |
| Legal disability | 138,167 | 112,665 | 13.8 | 25,502 | 75.9 | <0.001 |
| Chronic disease | ||||||
| HT | 624,965 | 601,893 | 73.5 | 23,072 | 68.7 | <0.001 |
| DM | 148,918 | 141,713 | 17.3 | 7,205 | 21.5 | <0.001 |
| IHD | 99,397 | 94,648 | 11.6 | 4,749 | 14.1 | <0.001 |
| COPD | 58,268 | 55,410 | 6.8 | 2,858 | 8.5 | <0.001 |
| CHF | 51,453 | 45,637 | 5.8 | 5,816 | 17.3 | <0.001 |
| CRF | 25,619 | 23,694 | 2.9 | 1,925 | 5.7 | <0.001 |
| D | 39,647 | 23,107 | 2.8 | 16,540 | 49.2 | <0.001 |
| SARS-CoV-2 Infection | ||||||
| Total | 65,897 | 50,467 | 100.0 | 15,430 | 100.0 | |
| 1st wave | 7,062 | 3,447 | 6.8 | 3,615 | 23.4 | |
| 2nd wave | 47,800 | 36,121 | 71.6 | 11,679 | 75.7 | |
| 3rd wave | 11,035 | 10,899 | 21.6 | 136 | 0.9 | |
A total of 65,897 subjects (7.7%) were infected by SARS-CoV-2 during the follow-up time. The total number of reported COVID-19 infections was 7,062 (10.7%) in the first wave, 47,800 (72.5%) in the second wave and 11,035 (16.8%) during the third wave. From 21 February 2020 to 3 May 2021 18,574 (28.2%) COVID-19 patients were hospitalised and 9,914 (15.0%) died.
Table 1 compares the main characteristics of NH versus non-NH study subjects: 33,592 study patients lived in NH on 21 February 2020 and 15,430 (23.4%) of them were infected by SARS-CoV-2 during the follow-up time. The proportion of cases infected with SARS-CoV-2 who were NH residents in the three waves were, respectively, 51.2, 24.4 and 1.2%.
NH patients were more frequently affected by severe chronic diseases than the general older population: they showed a higher prevalence of CHF, DM, CRF and D. People living in NH were also older (mean age 86.1 years, 95% CI: 86.1–86.2) than non-NH residents (78.6 years, 95% CI: 78.5–78.6). A non-homogeneous geographical distribution of NH in the seven provinces of the Veneto Region was found: i.e. the proportion of NH residents on the total number of subjects included in the study was 6.2% for the Belluno province and 3.0% for the Venice province.
After the 1:1 propensity score matching, the size of the two groups was equal to 31,922 cases. Homogeneous distribution was reached for gender (P = 0.16) and province of domicile (P = 0.24), whereas the distribution for age group, legal disability and all the considered chronic conditions remained different (P < 0.01). NH residents were slightly younger and healthier than non-NH selected patients, displaying lower prevalence of legal disability and all chronic conditions, except for D (46.6% among NH residents vs. 42.1% among non-NH residents), as shown in Table 2.
Table 2.
Post-matching distribution of study subjects. Absolute frequencies, percentages and P values according to the characteristics used for matching in NH and not NH residents
| Total | Non-NH residents | NH residents | P value | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Total | 63,884 | 31,922 | 100.0 | 31,922 | 100.0 | |
| Gender | 0.157 | |||||
| Females | 47,546 | 23,695 | 74.2 | 23,851 | 74.7 | |
| Males | 16,298 | 8,227 | 25.8 | 8,071 | 25.3 | |
| Age group (years) | <0.001 | |||||
| 70–79 | 11,163 | 5,264 | 16.5 | 5,899 | 18.5 | |
| 80–89 | 31,809 | 16,049 | 50.3 | 15,760 | 49.4 | |
| 90–100 | 20,872 | 10,609 | 33.2 | 10,263 | 32.2 | |
| Province of domicile | 0.244 | |||||
| Belluno | 4,496 | 2,276 | 7.1 | 2,220 | 6.9 | |
| Padua | 9,796 | 4,961 | 15.5 | 4,835 | 15.2 | |
| Rovigo | 3,815 | 1,910 | 6.0 | 1,905 | 6.0 | |
| Treviso | 11,994 | 6,004 | 18.8 | 5,990 | 18.8 | |
| Venice | 9,276 | 4,596 | 14.4 | 4,680 | 14.7 | |
| Vicenza | 13,150 | 6,624 | 20.8 | 6,526 | 20.4 | |
| Verona | 11,317 | 5,551 | 17.4 | 5,766 | 18.1 | |
| Legal disability | 48,864 | 25,032 | 78.4 | 23,832 | 74.7 | <0.001 |
| Chronic disease | ||||||
| HT | 45,631 | 23,216 | 72.7 | 22,415 | 70.2 | <0.001 |
| DM | 14,239 | 7,274 | 22.8 | 6,965 | 21.8 | 0.003 |
| IHD | 9,627 | 4,99 | 15.7 | 4,628 | 14.5 | 0.006 |
| COPD | 5,865 | 3,064 | 9.6 | 2,801 | 8.8 | <0.001 |
| CHF | 11,368 | 5,853 | 18.3 | 5,515 | 17.3 | <0.001 |
| CRF | 3,902 | 2,035 | 6.4 | 1,867 | 5.8 | 0.006 |
| D | 28,301 | 13,430 | 42.1 | 14,871 | 46.6 | <0.001 |
NH residents showed a higher risk of COVID-19 infection (RR = 6.28; 95% CI: 6.03–6.54), hospitalisation for COVID-19 (RR = 2.20; 95% CI: 2.05–2.36) and death with COVID-19 (RR = 6.07; 95% CI: 5.58–6.61), as shown in Table 3. RRs were also calculated distinctly for the three pandemic waves.
Table 3.
Absolute frequencies (N), crude rates (%), and RRs with 95% Confidence Intervals for post-matching outcomes: SARS-CoV-2 infection, hospitalisation for COVID-19, death with COVID-19, overall and by pandemic wave
| Non-NH residents | NH residents | RR (95%CI) NH residents versus non-NH residents | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Wave | N | % | N | % | ||
| COVID-19 infection | 1 | 237 | 0.7 | 3,446 | 10.8 | 14.54 | (12.76–16.57) |
| 2 | 1,687 | 5.9 | 11,205 | 46.4 | 7.93 | (7.56–8.32) | |
| 3 | 431 | 1.7 | 127 | 1.2 | 0.69 | (0.57–0.84) | |
| Overall | 2,355 | 7.4 | 14,779 | 46.3 | 6.28 | (6.03–6.54) | |
| Hospitalisation for COVID-19 | 1 | 179 | 0.6 | 876 | 2.7 | 4.89 | (4.17–5.74) |
| 2 | 697 | 2.4 | 1,460 | 6.1 | 2.50 | (2.29–2.73) | |
| 3 | 210 | 0.8 | 22 | 0.2 | 0.25 | (0.16–0.38) | |
| Overalla | 1,103 | 3.5 | 2,425 | 7.6 | 2.20 | (2.05–2.36) | |
| Death with COVID-19 | 1 | 94 | 0.3 | 949 | 3.0 | 10.10 | (8.17–12.48) |
| 2 | 381 | 1.3 | 2,544 | 10.5 | 7.97 | (7.16–8.88) | |
| 3 | 88 | 0.4 | 22 | 0.2 | 0.48 | (0.30–0.77) | |
| Overalla | 604 | 1.9 | 3.668 | 11.5 | 6.07 | (5.58–6.61) | |
The number of events in each wave did not include people who experienced COVID-19 infection or death in previous waves: the overall number of events for the secondary outcomes could be higher than the sum of the events recorded in the three waves.
The risk of being infected by SARS-CoV-2 among NH residents (compared with non-NH residents) showed a decreasing trend: in the first wave, it was equal to 14.54 (95% CI: 12.76–16.57), in the second it was equal to 7.93 (95% CI: 7.56–8.32) and decreased to 0.69 (95% CI: 0.57–0.84) in the third wave (Figure 1).
Figure 1.
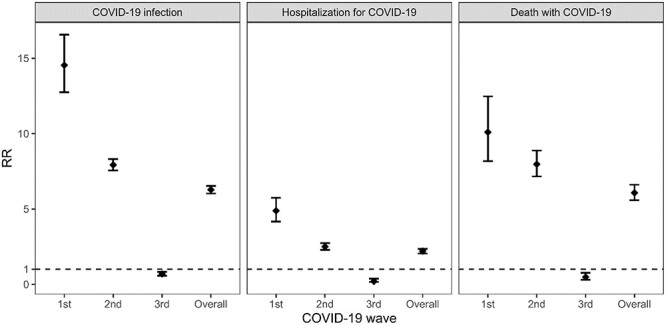
RRs (NH residents vs. non-NH residents) and 95% Confidence Intervals for post-matching outcomes (SARS-CoV-2 infection, hospitalisation for COVID-19, death with COVID-19), three pandemic waves and overall period of follow-up: 21 February 2020–3 May 2021.
Similar paths were also found for the RRs of hospitalisation for COVID-19: −4.89 (95% CI: 4.17–5.74), 2.50 (95% CI: 2.29–2.73) and 0.25 (95% CI: 0.16–0.38), respectively. The RRs of death with COVID-19 were, respectively, 10.10 (95% CI: 8.17–12.47), 7.97 (95% CI: 7.17–8.87) and 0.48 (95% CI: 0.30–0.77).
Discussion
At the best of our knowledge, this is one of the first detailed population-based analyses on COVID-19 infection and mortality from a large area comparing NH residents with matched subjects. Few reports compared the mortality of NH residents to the general population in Italy. De Girolamo et al. [18] used aggregated administrative data from the ISTAT to compare the figures in Lombardy versus Veneto Region and reported a significantly higher rate in the former (12.9 vs. 6.5 per 100 residents). Estimates were provided also in Ciminelli et al. [19]: they found that mortality doubled in municipalities where 10% of older people live in NH, compared with the ones without NH in town. A recent analysis focused on NH settled in the Venice area [20] and showed that the presence of COVID-19 increased the risk of death by 1.85 times for NH residents.
A Spanish study underlined that the main factors associated with mortality for NH residents were being male, older than 80 years, admitted to a hospital for COVID-19 and being affected by cardiovascular disease, kidney disease or D [21]. Sepulveda et al. [22] estimated a risk of mortality in NH residents of about 24.3 times higher than non-NH residents. Moreover, a recent US study provided estimates for the second wave of the pandemic and showed from April to early November 2020 a decline in adjusted mortality rates [23]. A comprehensive British study also evidenced a significant excess (65%) of deaths in care homes’ residents due to COVID-19 [24].
This study showed that NH residents suffered the COVID-19 pandemic more than the non-NH residents: considering the overall study period, they had a greater risk of SARS-CoV-2 infection, hospitalisation for COVID-19 and COVID-19-related death. This happened particularly in the first wave of the pandemic, when a great number of SARS-CoV-2 infections were reported in the NHs. NH residents represented more than 50% of the COVID-19 total cases and their risk of being infected with SARS-CoV-2, of hospitalisation and of death were respectively 14, 5 and 10 times higher than non-NH residents. Such increased risk could be partially due to a surveillance bias related to the periodic screening for COVID-19 infection among NH residents, which was recommended by the Italian Ministry of Health on 27 February 2020 [25]. In addition, Italy experienced a general lockdown from 8 March to 3 May 2020, which drastically reduced the chances of infection in the general population.
During the second wave, a different scenario showed up. From November 2020 to January 2021 the pandemic stressed the regional Health System severely and hardly hit both NH residents and home-based older people. Nonetheless, COVID-19 swab tests became widespread, increasing the chances to identify most of the SARS-CoV-2 infection cases also among the general population. During the second wave, NH residents represented less than 25% of the COVID-19 reported cases and their RRs for all the study outcomes decreased. The severe health conditions of NH residents and their constant healthcare surveillance could partly explain why they were more often treated inside the NHs and were less frequently hospitalised.
From late December 2020, the Italian COVID-19 vaccination programme started for NH residents and healthcare professionals. This represented an important chance to enhance the health conditions of NH residents. By the end of the third wave, almost 95% of NH residents and their healthcare professionals received at least one vaccine dose [26] and NH residents seemed to have developed widespread immunity against the COVID-19. The risk of SARS-CoV-2 infection was significantly reduced, in particular for severe forms of COVID-19, which were frequently associated with hospitalisation and death. In fact, during the third wave, the number of NH patients who had the SARS-CoV-2 infection significantly decreased. They represented only 1% of the total number of reported COVID-19 cases and their RRs for all the study outcomes declined below 1. The risk of SARS-CoV-2 infection was 30% lower among NH residents than the general older population with similar personal and health characteristics. The reduction in the risk of hospitalisation and death in NH residents was even larger (−75 and −62%, respectively), which likely reflects an effective lower risk for these individuals, coupled by a protective effect of the continuity of healthcare experienced in NHs.
It is not a chance that in Italy the vaccination campaign started from NH residents and their healthcare professionals. During the first two pandemic waves, the virus hardly hit these facilities [20, 27] and their hosts represented one of the frailest categories of COVID-19 susceptible subjects [28, 29]. In a representative sample of European countries, the range of deaths among NH residents has been estimated (in May 2020) between 37 and 66% of all COVID-19-related deaths [30]. NH residents are also more exposed to infection than the general population because they share common spaces with other patients and healthcare professionals [19, 31]. Moreover, the integration between hospitals and other care services in Italy is far from being completed and emerged as one of the most striking issues during the pandemic, in particular for NH healthcare management [32].
This study has some limitations. First, it analysed a large sample of subjects in North-East Italy and focused on a regional healthcare policy behaviour. However, it does not allow comparing different healthcare models, which in Italy were defined on a regional basis. In addition, the socioeconomic status of study subjects was not taken into account. We also underline that because of the exclusion of dead and infected subjects in the second and third wave, the 1:1 matching pairing proportion could not be assured in these phases. Finally, the distribution for age group, sex and health condition of the group of patients who survived and never had the COVID-19 infection at the end of the third wave, could have been different than the whole set of subjects included in the study.
In conclusion, this study showed the effect of the COVID-19 vaccination programme on the risk of SARS-CoV-2 infection, hospitalisation and death among NH residents. Besides vaccination, a more comprehensive organization for NH management is needed [33, 34] in order to promote improved handling of COVID-19 and possibly of other epidemics in these facilities. Special attention should be paid also to enhance the engagement of physicians and nurse practitioners [35], with the aim to improve care for NH residents [36, 37], also with prehospital interventions [38].
Contributor Information
Silvia Pierobon, Epidemiological Department, Azienda Zero, Veneto Region, Padova 35132, Italy.
Marco Braggion, Epidemiological Department, Azienda Zero, Veneto Region, Padova 35132, Italy.
Ugo Fedeli, Epidemiological Department, Azienda Zero, Veneto Region, Padova 35132, Italy.
Maurizio Nordio, Unit of Nephrology, General Hospital, Treviso 31100, Italy.
Cristina Basso, Epidemiological Department, Azienda Zero, Veneto Region, Padova 35132, Italy.
Manuel Zorzi, Epidemiological Department, Azienda Zero, Veneto Region, Padova 35132, Italy.
Declaration of Sources of Funding
None.
Declaration of Conflicts of Interest
None.
References
- 1. Romagnani P, Gnone G, Guzzi F et al. The COVID-19 infection: lessons from the Italian experience. J Public Health Policy 2020; 41: 238–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pasin L, Sella N, Correale C et al. Regional COVID-19 network for coordination of SARS-CoV-2 outbreak in Veneto, Italy. J Cardiothorac Vasc Anesth 2020; 34: 2341–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Italian National Health Institute . COVID-19 National Report, updated on May, 19th 2021 (in Italian). https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_19-maggio-2021.pdf (6 June 2021, date last accessed)
- 4. Italian National Health Institute . Characteristics of COVID-19 Patients Dying in Italy, Report Based on Available Data on April 28th, 2021 https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_28_april_2021.pdf. (6 June 2021, date last accessed).
- 5. Nikolai LA, Meyer CG, Kremsner PG et al. Asymptomatic SARS coronavirus 2 infection: invisible yet invincible. Int J Infect Dis 2020; 100: 112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. CDC . Coronavirus Disease 2019 (COVID-19): People Who Need to Take Extra Precautions. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html. (6 June 2021, date last accessed). [Google Scholar]
- 7. Heras E, Garibaldi P, Boix M et al. COVID-19 mortality risk factors in older people in a long-term care center. Eur Geriatr Med 2020; 12: 601–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ho FK, Petermann-Rocha F, Gray SR et al. Is older age associated with COVID-19 mortality in the absence of other risk factors? General population cohort study of 470,034 participants. PLoS One 2020; 15: e0241824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Perrotta F, Corbi G, Mazzeo G et al. COVID-19 and the elderly: insights into pathogenesis and clinical decision-making. Aging Clin Exp Res 2020; 32: 1599–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lombardo FL, Bacigalupo I, Salvi E et al. The Italian national survey on coronavirus disease 2019 epidemic spread in nursing homes. Int J Geriatr Psychiatry 2021; 36: 873–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abrams HR, Loomer L, Gandhi A et al. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc 2020; 68: 1653–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bielza R, Sanz J, Zambrana F et al. Clinical characteristics, frailty, and mortality of residents with COVID-19 in nursing homes of a region of Madrid. J Am Med Dir Assoc 2021; 22: 245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Italian National Statistics Institute , I presidi residenziali socio-assistenziali e socio-sanitari, updated on 2018, May 23. (in Italian). https://www.istat.it/it/files/2018/05/Presidi-residenziali_2015.pdf. (6 June 2021, date last accessed).
- 14. Braggion M, Pellizzari M, Basso C et al. Overall mortality and causes of death in newly admitted nursing home residents. Aging Clin Exp Res 2020; 32: 275–80. [DOI] [PubMed] [Google Scholar]
- 15. Italian National Health Institute . COVID-19: Interim Report on definItion, Certification and Classification of Causes of Death. Version of June 8, 2020. Gruppo di Lavoro ISS Cause di morte COVID-19, Gruppo di lavoro Sovrintendenza sanitaria centrale - INAIL, ISTAT; 2020, 15 p. Rapporto ISS COVID-19 n. 49/2020 (in Italian). https://www.iss.it/rapporti-covid-19/-/asset_publisher/btw1J82wtYzH/content/rapporti-iss-covid-19-n.-49-2020-covid-19-rapporto-ad-interim-su-definizione-certificazione-e-classificazione-delle-cause-di-morte.-versione-dell-8-giugno-2020. (6 June 2021, date last accessed). [Google Scholar]
- 16. Corti MC, Avossa F, Schievano E et al. A case-mix classification system for explaining healthcare costs using administrative data in Italy. Eur J Intern Med 2018; 54: 13–6. [DOI] [PubMed] [Google Scholar]
- 17. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 2011; 46: 399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. De Girolamo G, Bellelli G, Bianchetti A et al. Older people living in long-term care facilities and mortality rates during the COVID-19 pandemic in Italy: preliminary epidemiological data and lessons to learn. Front Psych 2020; 11: 586524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ciminelli G, Garcia-Mandicó S. COVID-19 in Italy: an analysis of death registry data. J Public Health (Oxf) 2020; 42: 723–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Veronese N, Koyanagi A, Stangherlin V et al. Mortality attributable to COVID-19 in nursing home residents: a retrospective study. Aging Clin Exp Res 2021; 33: 1745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. España PP, Bilbao A, García-Gutiérrez S et al. Predictors of mortality of COVID-19 in the general population and nursing homes. Intern Emerg Med 2021; 16: 1487–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sepulveda ER, Stall NM, Sinha SK. A comparison of COVID-19 mortality rates among long-term care residents in 12 OECD countries. J Am Med Dir Assoc 2020; 21: 1572–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kosar CM, White EM, Feifer RA et al. COVID-19 mortality rates among nursing home residents declined from March to November 2020. Health Aff (Millwood) 2021; 40: 655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Morciano M, Stokes J, Kontopantelis E et al. Excess mortality for care home residents during the first 23 weeks of the COVID-19 pandemic in England: a national cohort study. BMC Med 2021; 19: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Italian Ministry of Health , Documento relativo ai criteri per sottoporre soggetti clinicamente asintomatici alla ricerca d'infezione da SARS-CoV-2 attraverso tampone rino-faringeo e test diagnostico, 2020. (in Italian). https://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=73444&parte=1%20&serie=null. (6 June 2021, date last accessed).
- 26. Veneto Region , COVID-19 vaccination plan monitoring tool web page (in Italian). 2021. https://regione.veneto.it/dati-vaccinazioni/. (6 June 2021, date last accessed).
- 27. Trabucchi M, de Leo D. Nursing homes or besieged castles: COVID-19 in Italy. Lancet Psychiatry 2020; 7: 387–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. White EM, Kosar CM, Feifer RA et al. Variation in SARS-CoV-2 prevalence in U.S. skilled nursing facilities. J Am Geriatr Soc 2020; 68: 2167–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ouslander JG, Grabowski DC. COVID-19 in nursing homes: calming the perfect storm. J Am Geriatr Soc 2020; 68: 2153–62. [DOI] [PubMed] [Google Scholar]
- 30. Public ECDC. Health emergency team, Danis K, Fonteneau L et al. high impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA. Euro Surveill 2020; 25: 2000956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Powell T, Bellin E, Ehrlich AR. Older adults and Covid-19: the most vulnerable, the hardest hit. Hastings Cent Rep 2020; 50: 61–3. [DOI] [PubMed] [Google Scholar]
- 32. Cesari M, Proietti M. Editorial: geriatric medicine in Italy in the time of COVID-19. J Nutr Health Aging 2020; 24: 459–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rolland Y, Benetos A, Villars H et al. A COVID-19 support platform for long term care facilities. J Nutr Health Aging 2020; 24: 461–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ioannidis JPA, Axfors C, Contopoulos-Ioannidis DG. Second versus first wave of COVID-19 deaths: shifts in age distribution and in nursing home fatalities. Environ Res 2021; 195: 110856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spilsbury K, Devi R, Griffiths A et al. SEeking AnsweRs for care homes during the COVID-19 pandemic (COVID SEARCH). Age Ageing 2021; 50: 335–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gordon AL, Goodman C, Achterberg W et al. Commentary: COVID in care homes—challenges and dilemmas in healthcare delivery. Age Ageing 2020; 49: 701–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Grabowski DC, Mor V. Nursing home care in crisis in the wake of COVID-19. JAMA 2020; 324: 23–4. [DOI] [PubMed] [Google Scholar]
- 38. Dolveck F, Strazzulla A, Noel C et al. COVID-19 among nursing home residents: results of an urgent pre-hospital intervention by a multidisciplinary task force. Braz J Infect Dis 2021; 25: 101039. [DOI] [PMC free article] [PubMed] [Google Scholar]


