Abstract
Background
Older women have faced significant disruptions in social connections during the coronavirus disease 2019 pandemic. Whether loneliness increased or whether a change in loneliness from pre- to intrapandemic period was associated with mental health during the pandemic is unknown.
Methods
Older women (n = 27 479; mean age 83.2 [SD: 5.4] years) completed surveys in mid-2020, including questions about loneliness, living arrangements, changes in social connections, and mental health. Loneliness was also previously assessed in 2014–2016. We examined whether loneliness changed from the pre- to intrapandemic period and explored factors associated with this change. In multivariable models, we investigated the association of changes in loneliness and social connections with mental health.
Results
Loneliness increased from pre- to intrapandemic levels. Factors associated with worsening loneliness included older age, experiencing stressful life events, bereavement, histories of vascular disease and depression, and social connection disruptions. Factors associated with a decrease in loneliness included identifying as Black, engaging in more frequent physical activity, being optimistic, and having a higher purpose in life. A 3-point increase in loneliness scores was associated with higher perceived stress, higher depressive, and higher anxiety symptoms. Social connection disruptions showed modest or no associations with mental health.
Conclusions
Loneliness increased during the pandemic in older women and was associated with higher stress, depressive, and anxiety symptoms. Our findings point to opportunities for interventions targeting lifestyle behaviors, well-being, disrupted social connections, and paying closer attention to those with specific medical and mental health histories that may reduce loneliness and improve mental health.
Keywords: Anxiety, Depression, Loneliness, SARS-CoV-2, Social connection, Stress, Women
Loneliness—the subjective feeling of being isolated—was highly prevalent among older adults even before the coronavirus disease 2019 (COVID-19) pandemic (1,2). Pre-COVID-19 data indicated that over 40% of Americans aged 60 and older were lonely (2–4), with 1 in 5 expressing frequent and severe feelings of loneliness (2). While loneliness decreases with age through the mid-70s, an overall increase is observed after age 75 (5). Loneliness is an important public health priority among older adults as it is associated with a myriad of long-term negative physical, cognitive, and mental health consequences and premature all-cause mortality (2,6–8).
Loneliness was widely anticipated to intensify among older adults during the COVID-19 pandemic, due to the national and self-imposed physical distancing and stay-at-home measures. However, studies of loneliness that included older cohorts are limited and have produced mixed findings (9–16). While a handful of investigations reported an increase in loneliness in older adults during the earlier months of the pandemic compared with the prepandemic levels (12,13), one study found no change (14). In contrast, a larger number of COVID-19 surveys in mixed-age cohorts have reported that younger individuals express greater loneliness than their older counterparts (9–11,15,16). Despite these discrepancies, older women consistently expressed more loneliness than older men during the pandemic (12,17–19), though explanatory factors are unknown. Also unclear is whether the degree of loneliness changed among the oldest-old women during COVID-19 compared with their prepandemic levels.
Older adults, especially the oldest old, are particularly vulnerable to becoming severely ill and succumbing to COVID-19 because of multiple factors, including having more cardiovascular risk factors and other chronic health conditions. Significant precautions are therefore taken to protect them from virus exposure, bringing unprecedented disruptions to their daily social connections. In older women, changes in loneliness levels and disruptions in objective social connections from the pre- to intrapandemic period may adversely influence mental health outcomes during the pandemic; however, no study has evaluated this link.
We, therefore, utilized data collected from the Women’s Health Initiative (WHI) participants (age range: 71–104 years) who completed surveys prepandemic (2014–2016) and during the earlier months of the pandemic (ie, between February and October 2020) to examine (a) the changes in loneliness scores from the prepandemic to intrapandemic period; (b) factors associated with changes in loneliness from the pre- to intrapandemic period and loneliness severity during the pandemic; and (c) the associations of changes in loneliness and social connection disruptions from the pre- to intrapandemic period with mental health outcomes during the pandemic. We further explored if the loneliness–mental health associations were modified by specific factors (ie, age, reported race, life events, physical activity, depression history, and disruptions in social connection). While this study is not designed to examine the impact of the pandemic on non-White, financially insecure, and poorly educated subgroups, the WHI is one of the largest and more diverse cohorts of oldest-old women available; thus, this data set provides a unique opportunity to examine the associations as described above.
Method
Study Population
The WHI is a longitudinal study of 161 808 postmenopausal women aged 50–79 years originally recruited between 1993 and 1998 at 40 clinical centers across the United States. WHI participants were enrolled in an observational study (OS) or randomized into one or more of 3 clinical trials (CTs)—hormone therapy (ie, estrogen plus progestin or estrogen alone arms), dietary modification, or calcium and vitamin D supplementation. The WHI study design and methods are detailed elsewhere (20). In 2005, either after the completion or early termination of all WHI CTs, women in both OS and CT components were consented to the first (2005–2010) and second (2010–2020) extension studies, which collected health updates and outcomes annually in active participants. WHI is now in its third extension (2020–2027). All participants provided written informed consent, according to the Institutional Review Board-approved protocols.
Cohort Selection for This Substudy
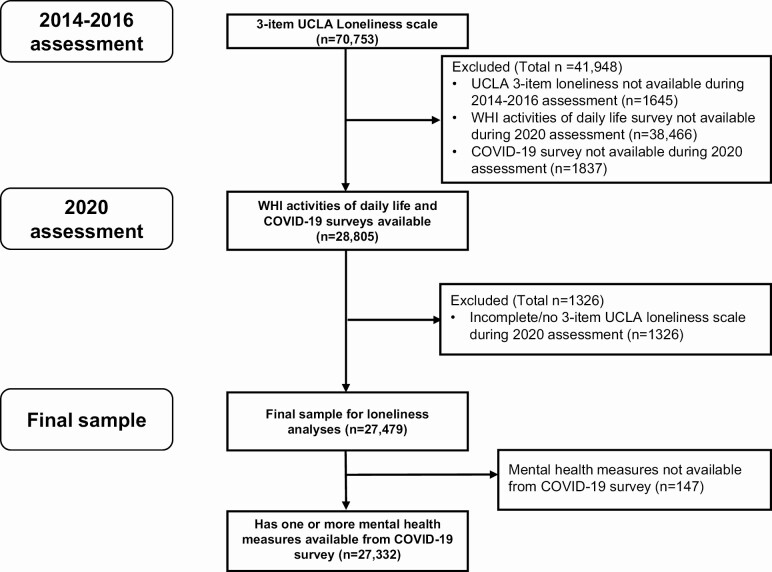
Women who are still participating in WHI were included in this study if they completed the (a) 3-item UCLA Loneliness Scale during the 2014–2016 assessment and (b) 2 surveys during the COVID-19 pandemic as of October 30, 2020. The 2 surveys were the “Activities of Daily Life,” completed between February 6, 2020 and October 30, 2020, in which the 3-item UCLA Loneliness Scale was repeated and the “COVID-19 Impact Survey,” completed between June 5, 2020 and October 29, 2020 (see Figure 1 for details).
Figure 1.
STROBE flow diagram. Notes: WHI activities of daily life survey were received between February 6, 2020 and October 30, 2020. WHI COVID-19 survey was received between June 5, 2020 and October 29, 2020. WHI = Women Health Initiative; COVID-19 = coronavirus disease 2019.
Loneliness Measure Before and During COVID-19
Loneliness was measured twice (once during 2014–2016, and then in 2020 during the COVID-19 pandemic) using the 3-item version of the UCLA Loneliness Scale. This self-reported instrument has demonstrated good reliability and both concurrent and discriminant validity and has been used in several aging studies (3,21–23). This scale assesses subjective feelings of loneliness on a 3-point Likert scale ranging from 1 (hardly ever) to 3 (often). The 3 items are (a) How often do you feel that you lack companionship? (b) How often do you feel left out? and (c) How often do you feel isolated from others? The scores range from 3 to 9; higher scores indicate greater perceived loneliness (21,24), with women categorized as no/minimal loneliness (score of 3), some loneliness (score of 4–5), and severe loneliness (score ≥6).
Psychological and Mental Health Assessments During COVID-19
Perceived stress
The 4-item perceived stress scale (25), a widely used instrument, was completed on a COVID-19 survey. The items included in the past 4 weeks how often have you felt that (a) you were unable to control the important things in your life, (b) confident about your ability to handle your personal problems, (c) things were going your way, and (d) difficulties were piling up so high that you could not overcome them. The total scores range from 0 to 16, with higher scores indicating greater levels of perceived stress.
Current depressive symptoms
Current depressive symptoms were assessed on a COVID-19 survey using the 6-item Center for Epidemiologic Studies—Depression scale (CES-D short form) (26,27). This scale has been widely utilized in previous aging studies (27,28). Participants are asked about their feelings during the past week, and the scores range from 0 to 18. Higher scores indicate greater levels of depressive symptoms, with a score ≥5 indicative of clinically significant depressive symptoms.
Current anxiety symptoms
The PROMIS Anxiety Short Form 4a questionnaire, which included 4 questions related to anxious mood in the past 7 days, was used to measure current anxiety symptoms in the past 7 days during COVID-19 (29,30). Participants rated each item on a 5-point scale (from 1 [never] to 5 [always]), with the total score ranging from 4 to 20. Total raw scores were then converted to a standardized T-score to generate a final score. The standardized T-score on this scale ranges from 40.3 to 81.6, with a mean of 50 (SD of 10) for the general population. Higher scores indicate greater anxiety symptom severity, with PROMIS T-score ≥60 indicative of clinically significant anxiety symptoms.
Living Arrangement and Changes in Objective Social Connections During COVID-19
Living alone status
This variable was assessed by asking the question, “Do you live alone?” with participants answering either yes or no.
Changes in living arrangements due to the COVID-19 pandemic were assessed using the question, “Has your living arrangement, including the place where you live and the people that live with you, changed since March 2020 due to the COVID-19 pandemic?” with participants answering yes or no.
Living situation restrictions were indicated as yes if a participant lived in a care facility where residents were either not allowed to leave their home/apartment/room, have visitors, or leave the property except for emergencies, and/or food was delivered to their home/apartment/room. No living restrictions were indicated if a participant lived in a private home or endorsed that the care facility in which they lived had no restrictions on residents.
Social communication frequency during COVID-19 was assessed by the question: “How often do you communicate with others who live outside your home?” Participants were grouped into categories of every day or several times per week or 1–2 times per week or less.
Change in communication frequency during the pandemic compared with before the pandemic was assessed by the question: “Compared to months before the outbreak began, would you say this (ie, communication with others) is (1) about the same or more often than before, or (2) less often than before.”
In addition, the methods by which the participants communicated were assessed by “How are you staying in touch with others who do not live with you.” Because there were too few responses in certain groups (ie, speaking by telephone/video only), participants were grouped into speaking in person, or only by telephone/video/email/social media/postal mail but not in person.
Covariates
The following variables were assessed at the WHI baseline: race, ethnicity, and education. The 2020 WHI activities of daily life survey included life events measures over the past year (stressful life events, death or serious illness of close friend or family member, death of a pet, death of spouse or partner), optimism, the purpose in life construct (31,32)), and history of depression (using the 2-item National Institute of Mental Health’s Diagnostic Interview Schedule). The 2020 COVID-19 survey assessed lifestyle variables, including current walking/physical activity, alcohol intake, and smoking history. The annual WHI medical history updates included vascular risk factor variables (ie, cerebrovascular/cardiovascular disease [CVD], cancer, treated diabetes, treated hypertension, and body mass index [BMI]). The vascular risk factors score is a composite of treated diabetes, treated hypertension, current smoker, and BMI ≥30. The presence of each risk factor contributes one point to the score (range: 0–4). These variables came from the annual medical history assessment closest to the time of collection of the 2 2020 WHI surveys during COVID-19.
Statistical Analysis
We used a paired t-test to evaluate within-participant changes in the loneliness score between 2014–2016 and 2020. We used linear regression to examine changes in the loneliness scores using the participants’ age group at the 2014–2016 assessment (<70, 70–74, 75–79, 80–89, and ≥90 years).
We explored the factors related to (a) within-participant change in pre- to intrapandemic loneliness scores as well as (b) the loneliness score during the pandemic. Estimates of the associations were presented as beta coefficients and 95% confidence intervals (95% CIs), calculated from separate unadjusted linear regressions where the change in loneliness scores and the loneliness score during the pandemic were separately modeled as functions of each of the factors.
We conducted multivariable linear regression analyses to examine the associations of living alone during the pandemic, changes in loneliness and social connectedness from the pre- to intrapandemic period, and each mental health outcome (perceived stress, depressive symptoms, and anxiety symptoms) as separately modeled as a dependent variable. Loneliness change and all social connection variables were included in the same model, and all models were adjusted for sociodemographic factors (age, education, race, and ethnicity), lifestyle factors (physical activity, alcohol intake, number of life events), and medical history: CVD, cancer, vascular factors risk score, history of depression. Estimates, including beta coefficients (representing the strength of the association), and 95% CI from these models are presented. Odds ratio estimates from logistic regression models were also calculated where clinically significant depressive symptoms (ie, CES-D ≥5) and moderate to severe anxiety (ie, PROMIS T-score ≥60) were separately modeled as functions of change in loneliness score (intrapandemic minus prepandemic) and social connection variables, after adjusting for above-mentioned covariates.
Finally, we evaluated effect modification by age, race, objective social connection variables, physical activity, past depression history, and stressful life events. Models included main effects for change in loneliness score and the effect modifier variables further adjusted for education, Hispanic/Latina ethnicity, alcohol intake, and medical history (CVD history, cancer history, and vascular factors risk score). Interaction terms were created by multiplying the change in loneliness score by the potential effect modifier.
The p value was set a priori at <.0001 for statistical significance to minimize Type 1 error. Analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
Figure 1 is the STROBE flow diagram that outlines the methods used to arrive at the final sample (n = 27 479) for this WHI substudy.
The descriptive characteristics (frequencies and percentages) of the final WHI sample of participants (n = 27 479) who completed the loneliness questionnaire during the 2014–2016 and 2020 assessments respectively are summarized in Table 1. The mean age (SD) of the participants was 83.2 (5.4) years during the 2020 surveys. On the COVID-19 survey, most women reported being nonsmokers (97.7%), 12% reported a history of CVD, 25.8% cancer, 20% diabetes, 71% hypertension, and 4.6% a history of depression, and the mean (SD) BMI of the full cohort was 26.0 (5.2). Most women reported walking for at least 5 minutes without stopping 2–3 times or more per week (67.5%) and consuming 4 or fewer alcoholic drinks per week (81.4%). During the 1 year before completing the 2020 surveys, 37.6% of women either experienced death or serious illness of a close friend or family member, and about 5% experienced bereavement of a spouse or partner (Table 1).
Table 1.
Descriptive Characteristics
| Characteristic | All Participants (n = 27 479) | |
|---|---|---|
| n | % | |
| Demographics | ||
| Age at 2020 survey, mean (SD)* | 83.2 (5.4) | |
| Hispanic/Latina | 886 | 2.8 |
| Race | ||
| American Indian/Alaska Native | 57 | 0.2 |
| Asian/Pacific Islander | 624 | 2.3 |
| Black/African American | 1 324 | 4.8 |
| White | 24 959 | 90.8 |
| More than one race | 299 | 1.1 |
| Unknown/not reported | 216 | 0.8 |
| Education | ||
| High school diploma or less | 4 185 | 15.2 |
| School after high school | 9 386 | 34.2 |
| College degree or higher | 13 724 | 49.9 |
| Lifestyle | ||
| Walking continuously for 5 minutes or more | ||
| ≤1 time each week | 8 554 | 31.1 |
| 2–3 times each week | 6 368 | 23.2 |
| 4–6 times per week | 6 890 | 25.1 |
| 7 or more times per week | 5 277 | 19.2 |
| Alcoholic drinks per week | ||
| None | 13 758 | 50.1 |
| ≤4 | 8 611 | 31.3 |
| 5–7 | 3 846 | 14.0 |
| >7 | 985 | 3.6 |
| Currently smoke regular or electronic cigarettes | 348 | 1.3 |
| Life events † | ||
| Number of stressful life events (0–11), mean (SD) | 1.0 (1.1) | |
| Death or serious illness of a close friend or family member (other than spouse or partner) | 10 335 | 37.6 |
| Death of a pet | 1 848 | 6.7 |
| Death of spouse or partner | ||
| No | 24 183 | 88.0 |
| Yes | 1 306 | 4.8 |
| Intense longing or yearning for spouse/partner who died | ||
| Did not experience death of spouse/partner | 24 183 | 88.0 |
| Never/rarely | 374 | 1.4 |
| Sometimes/often | 775 | 2.8 |
| Always | 116 | 0.4 |
| Frequent thoughts about spouse/partner who died intrude on usual activities | ||
| Did not experience death of spouse/partner | 24 183 | 88.0 |
| Never/rarely | 787 | 2.9 |
| Sometimes/often | 459 | 1.7 |
| Always | 36 | 0.1 |
| Optimism construct, mean (SD) | 23.6 (3.6) | |
| Purpose in life construct (7-item scale), mean (SD) | 19.2 (4.8) | |
| Medical history ‡ | ||
| CVD | 3 288 | 12.0 |
| Cancer | 7 078 | 25.8 |
| Treated diabetes | 5 530 | 20.1 |
| Treated hypertension | 19 518 | 71.0 |
| Body mass index (BMI, kg/m2), mean (SD) | 26.0 (5.2) | |
| Vascular risk factors score (0–4), mean (SD)§ | 1.1 (0.8) | |
| History of depression (DIS)† | 1 274 | 4.6 |
| Social connection | ||
| Lives alone† | 12 857 | 46.8 |
| Living arrangement† | ||
| Independently in the community | 21 584 | 78.6 |
| With family other than spouse, assisted living or skilled nursing facility, other | 5 256 | 19.1 |
| Changes in living arrangement since March 2020, due to the COVID-19 pandemic | 1 676 | 6.1 |
| Living situation restrictions due to the COVID-19 pandemic | 3 795 | 13.8 |
| Communication with others outside the home | ||
| Every day or several times per week | 21 973 | 80.0 |
| 1–2 times per week, or less | 4 612 | 16.8 |
| Frequency of communication, compared to before the pandemic | ||
| About the same, or more often than before | 19 542 | 71.1 |
| Less often than before | 7 051 | 25.7 |
| Ways of staying in touch with others | ||
| Speaking in person | 10 684 | 38.9 |
| Telephone, video, social media, email or postal mail, but not in person | 16 257 | 59.2 |
| Psychological and mental health ‖ | ||
| Perceived stress 4-item score, mean (SD) | 4.6 (2.9) | |
| CES-D 6-item scale, mean (SD) | 2.8 (2.5) | |
| CES-D score ≥5 | 5 191 | 18.9 |
| PROMIS anxiety 4-item T-score, mean (SD) | 50.7 (8.2) | |
| PROMIS anxiety score ≥60 | 3 262 | 11.9 |
Notes: CVD = cardiovascular disease; COVID-19 = coronavirus disease 2019; CES-D = Center for Epidemiologic Studies—Depression scale; SD = standard deviation; DIS = Diagnostic Interview Schedule; PROMIS = Patient-Reported Outcomes Measurement Information System. Numbers and percentages do not always sum to the total, due to missing data.
*At the 2014–2016 assessment, mean age (SD) for this cohort: 78.0 (5.4).
†Life events items and history of depression were collected on the Activities of Daily Life survey in 2020, living alone and living arrangement status.
‡Medical history data (except history of depression) were collected as part of the ongoing WHI follow-up assessments; these variables come from the annual follow-up assessment closest to the time of collection of the 2020 surveys.
§Vascular risk factors score is a composite of treated diabetes, treated hypertension, current smoker, and BMI ≥30. Presence of each characteristic contributes one point to the score.
‖Perceived stress ranges from 0 (no stress) to 16 (greatest stress); CES-D ranges from 0 to 18 (≥5 considered to have depressive symptoms); PROMIS Anxiety T-score ranges from 40.3 to 81.6. General population mean is 50 (SD = 10). Higher score = greater anxiety.
During the earlier months of the COVID-19 pandemic, 46.8% reported living alone. About 82% of women reported no changes in their living alone status in 2020 compared with their 2014–2016 status (ie, those who answered “yes” to living alone in 2014–2016 reported the same in 2020, and those who reported “no” answered the same at both assessments). Due to the pandemic, 6.1% reported changes in their living arrangement, and 13.8% reported restrictions in their living situation. Although a vast majority (80%) reported communicating every day or several times per week with others outside their home, 25.7% reported that the communication frequency occurred less often than before the pandemic, and only 39% were staying in touch with others during the pandemic by physically speaking in person. During the pandemic, 19% of women reported clinically significant depressive symptoms (ie, CES-D score ≥5) and 12% endorsed moderate to severe anxiety symptoms (ie, PROMIS anxiety score ≥60; Table 1).
Loneliness Changes From Before to During the COVID-19 Pandemic
While only 10% reported severe loneliness scores (ie, UCLA 3-item loneliness scale score ≥6) prepandemic, approximately 19% reported severe loneliness during the pandemic (Table 2A). Compared with the prepandemic levels, the overall loneliness scores were higher during COVID-19 (mean change [SD]: 0.46 [1.4]; p < .0001). In the linear regression model with loneliness score changes modeled as a function of age in 2014–2016, feelings of loneliness were significantly higher during the pandemic than prepandemic in all age categories, except the youngest age group (<70 years; Table 2B).
Table 2.
Change in Loneliness Between Prepandemic and During the COVID-19 Pandemic
| A. Loneliness Scores as a Categorical Variable | ||||||
|---|---|---|---|---|---|---|
| 2014–2016 | 2020 | |||||
| UCLA 3-item loneliness score | N | % | N | % | p * | |
| 3 (no/minimal loneliness) | 18 980 | 69.1 | 14 896 | 54.2 | <.0001 | |
| 4–5 (some loneliness) | 5 834 | 21.2 | 7 458 | 27.1 | ||
| 6–9 (severe loneliness) | 2 665 | 9.7 | 5 125 | 18.7 | ||
| B. Loneliness Scores as a Continuous Variable | ||||||
| 2014–2016 | 2020 | Change | ||||
| UCLA 3-item loneliness score | N | Mean (SD) | Mean (SD) | Mean (SD) | p † | |
| Overall | 3.6 (1.1) | 4.1 (1.5) | 0.46 (1.4) | <.0001 | ||
| Age in 2014–2016 | ||||||
| <70 | 807 | 3.7 (1.3) | 3.9 (1.4) | 0.18 (1.3) | .0002 | |
| 70–74 | 7 332 | 3.6 (1.1) | 3.9 (1.4) | 0.34 (1.3) | <.0001 | |
| 75–79 | 9 151 | 3.6 (1.1) | 4.0 (1.5) | 0.43 (1.4) | <.0001 | |
| 80–89 | 9 494 | 3.7 (1.2) | 4.2 (1.6) | 0.57 (1.5) | <.0001 | |
| ≥90 | 695 | 3.8 (1.2) | 4.6 (1.8) | 0.77 (1.7) | <.0001 |
Note: COVID-19 = coronavirus disease 2019. The bold was used to highlight “significant findings.”
*p value is from Bowker’s test of symmetry and compares categorical loneliness scores from 2014 to 2016 and 2020, taking into account the paired data.
† p values test change in loneliness from 2014 to 2016 to 2020 and are from paired t-test (overall) or linear regression model with change in loneliness score modeled as a function of age in 2014–2016.
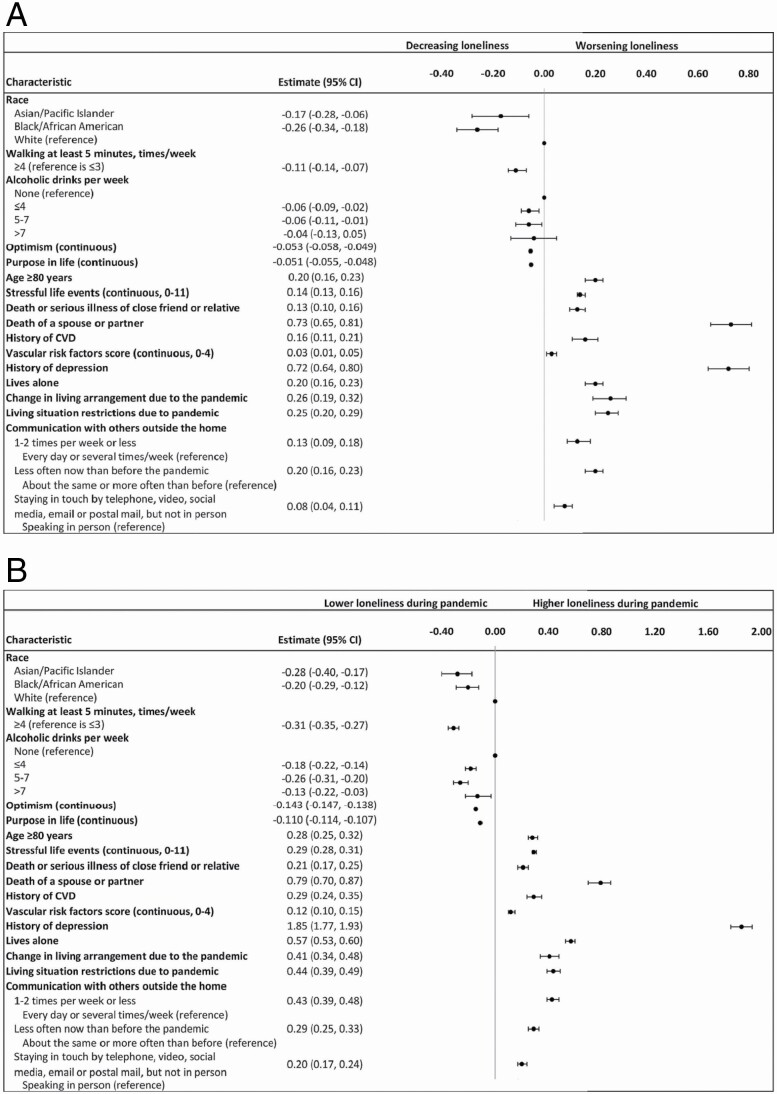
Factors Associated With Loneliness Changes
The factors associated with an intraparticipant change in loneliness scores from prepandemic to intrapandemic (Figure 2A) and loneliness scores during the pandemic were similar (Figure 2B and Supplementary Table 1).
Figure 2.
(A) Factors related to a within-participant change in loneliness from before the COVID-19 pandemic (2014–2016) to during the pandemic (2020). Notes: Estimates are the beta coefficients (slope) from unadjusted linear regression models where a change in loneliness is modeled as a function of each characteristic. (B) Factors related to loneliness during the COVID-19 pandemic. Notes: Estimates are the beta coefficients (slope) from unadjusted linear regression models where loneliness is modeled as a function of each characteristic. COVID-19 = coronavirus disease 2019; CVD = cardiovascular disease.
Older age (ie, ≥80 years of age), reporting more stressful life events, experiencing death or serious illness of a close friend or family member, experiencing the death of a spouse or partner, history of CVD, and depression history were associated with worsening of loneliness scores over time.
Living alone during the pandemic and changes in the objective social connection factors (ie, change in living arrangement, living situation restrictions, and less communication with others outside the home during the pandemic) were also associated with worsening of loneliness scores (Figure 2A; Supplementary Table 1).
Identifying as Black/African American (compared with White), walking continuously for at least 5 minutes 4 or more times per week (vs. ≤3 times/week), drinking ≤4 alcoholic drinks per week, being more optimistic, and having a higher sense of purpose in life score were associated with a decrease in loneliness scores from the pre- to intrapandemic period.
We further explored whether the month when and the region in the United States where the COVID-19 survey was completed were associated with changes in loneliness from the prepandemic to the intrapandemic period. We found no significant associations between the region or month of survey and change in loneliness.
Associations of Changes in Loneliness and Objective Social Connection With Mental Health
In multivariable models, changes in loneliness showed a stronger association than living alone and changes in objective social connections, with all 3 dependent variables, after full covariate adjustment: During the pandemic, a 3-point increase in feelings of loneliness from pre- to intrapandemic scores was associated with mean 0.56-point higher perceived stress (95% CI, 0.46–0.65), 1.02-point higher depressive symptom (95% CI, 0.95–1.09), and 1.78-point higher anxiety symptom (95% CI, 1.54–2.02) scores (p < .0001; Table 3). Because the rates of COVID-19 cases fluctuated on a month-to-month basis in different parts of the United States, we conducted additional analyses to explore whether the associations between loneliness changes and mental health outcomes were different, after including the month when and the U.S. region where the COVID survey was completed as covariates. The beta estimates and CIs were not appreciably different (data not shown).
Table 3.
Multivariable Associations Between Changes in Loneliness and Social Connection, and Mental Health During the COVID-19 Pandemic
| Perceived Stress 4-Item Score | CES-D Depression 6-Item Scale | PROMIS Anxiety 4-Item T-Score | ||||
|---|---|---|---|---|---|---|
| Characteristic | Estimate (95% CI) | p | Estimate (95% CI) | p | Estimate (95% CI) | p |
| Change in loneliness score, continuous (by increase of 3) | 0.56 (0.46, 0.65) | <.0001 | 1.02 (0.95, 1.09) | <.0001 | 1.78 (1.54, 2.02) | <.0001 |
| Lives alone | −0.06 (−0.14, 0.02) | .1528 | −0.02 (−0.08, 0.05) | .6127 | −0.29 (−0.51, −0.07) | .0089 |
| Changes in living arrangement due to the COVID-19 pandemic | 0.43 (0.26, 0.60) | <.0001 | 0.29 (0.15, 0.42) | <.0001 | 1.66 (1.19, 2.13) | <.0001 |
| Living situation restrictions due to the COVID-19 pandemic | 0.43 (0.31, 0.56) | <.0001 | 0.13 (0.03, 0.23) | .0083 | 0.53 (0.20, 0.86) | .0018 |
| Communication with others outside the home | ||||||
| Every day or several times per week | Reference | Reference | Reference | |||
| 1–2 times per week or less | 0.50 (0.38, 0.61) | <.0001 | 0.19 (0.11, 0.28) | <.0001 | −0.10 (−0.41, 0.20) | .5123 |
| Frequency of communication now, compared to before the pandemic | ||||||
| About the same or more often | Reference | Reference | Reference | |||
| Less often than before | 0.30 (0.21, 0.39) | <.0001 | 0.14 (0.07, 0.21) | .0001 | 1.22 (0.98, 1.47) | <.0001 |
| Ways of staying in touch with others | ||||||
| Speaking in person | Reference | Reference | Reference | |||
| Telephone, video, social media, email or postal mail, but not in person | 0.34 (0.26, 0.43) | <.0001 | 0.21 (0.14, 0.27) | <.0001 | 1.04 (0.82, 1.27) | <.0001 |
Notes: CVD = cardiovascular disease; COVID-19 = coronavirus disease 2019; CES-D = Center for Epidemiologic Studies—Depression scale; PROMIS = Patient-Reported Outcomes Measurement Information System. Estimates are the beta coefficients from linear regressions where stress, depression, and anxiety are separately modeled as functions of change in loneliness score (ie, within individual intrapandemic score minus prepandemic score) and social connection variables. Models include all variables shown in the table and are adjusted for sociodemographic factors (age, education, race, and ethnicity), lifestyle factors (physical activity, alcohol intake, number of stressful life events), and medical history (CVD history, cancer history, vascular factors risk score, past history of depression). Perceived stress ranges from 0 (no stress) to 16 (greatest stress); CES-D ranges from 0 to 18 (≥5 considered to have depressive symptoms); PROMIS anxiety T-score ranges from 40.3 to 81.6. General population mean is 50 (SD = 10). Higher score = greater anxiety.
After full covariate adjustment, a 3-point increase in loneliness score from pre- to intrapandemic period was associated with twofold increased odds of clinically significant depressive symptoms (odds ratio = 2.37 [95% CI: 2.18–2.57]; p < .0001) and 55% increased odds of moderate to severe anxiety (odds ratio = 1.55 [95% CI: 1.42–1.70]; p < .0001) during the pandemic (Supplementary Table 2).
While changes in living arrangement due to COVID-19 were significantly associated with 0.43-point higher perceived stress (95% CI, 0.26–0.60), 0.29-point higher depressive symptom (95% CI, 0.15–0.42), and 1.66-point higher anxiety symptom (95% CI, 1.19–2.13) scores (p < .0001), living alone did not significantly correlate with perceived stress or mental health measures. However, lack of in-person communication was associated with modestly higher perceived stress, depressive, and anxiety symptoms. Lower frequency of communication during COVID-19, relative to prepandemic levels, was associated with modestly higher perceived stress and anxiety, but not depressive symptoms (Table 3).
Associations of changes in loneliness and social connection measures and mental health during the pandemic did not significantly vary by age and racial subgroups, physical activity, history of depression, stressful life events, living alone, or social connection measures (Supplementary Table 3). Changes in living arrangement showed a trend toward modifying the association between loneliness and depressive symptoms: In participants who reported a change in living arrangement due to COVID-19, increases in loneliness over time were associated with a mean 1.45-point increase in depressive symptoms versus a mean 0.99-point increase in those who did not report a change (interaction p value = .0005).
Discussion
In a large sample of older women, significant increases in loneliness were observed during the earlier pandemic months, relative to prepandemic levels; this increase was more pronounced in those 70 years of age and older. Factors associated with increasing loneliness scores included older age, experiencing a greater number of life stressors (especially death of a spouse/partner) during the past year, having a history of CVD, a history of depression, and reporting social connection disruptions during the pandemic. The factors associated with decreases in loneliness over time included being Black/African American, being Asian/Pacific Islander, engaging in more frequent physical activity, being more optimistic, and having a higher purpose in life. Increasing feelings of loneliness were associated with higher perceived stress and depressive and anxiety symptoms during the pandemic. In contrast, living alone during the pandemic was not associated with mental health, and changes in objective social connection measures showed modest or no associations with these measures during the pandemic. These novel findings provide unique insights regarding loneliness and its association with mental health during COVID-19 and underscore the importance of developing strategies that mitigate loneliness to improve mental health in older women.
Recent longitudinal studies comprising older mixed-gender samples have reported an overall increase in loneliness during the earlier pandemic months compared with the prepandemic period (12,13). In a Dutch study among 1 679 community-dwelling older adults, when loneliness increased during the pandemic, overall mental health remained stable (13). In another cohort of 1 990 Swiss older adults, loneliness scores increased after their government recommended physical distancing policies to protect older adults (12). Studies comprising mixed-age samples, however, have reported variable findings. For example, data from the Health and Retirement Study of US adults older than age 50 years showed no change in loneliness levels despite experiencing increased physical isolation during COVID-19. Participants in that study stayed digitally connected, which may have protected them from feeling lonely (14). Large cross-sectional studies from across Europe also report higher loneliness levels in younger than older adults during the COVID-19 lockdown (9,10,16). In a nationwide sample of American adults, older adults also expressed less loneliness than their younger counterparts, though the former showed loneliness increases in response to the acute pandemic phase (11). In these prior investigations, few older women, especially those who belong to the oldest-old cohort, were included. This is pertinent because older women express more loneliness than older men during the pandemic (12,17–19). Furthermore, the National Social Life, Health and Aging Project of health and aging conducted pre-COVID-19 demonstrated that loneliness decreases with age until the mid-70s, but then increases after age 75 (5). Our findings suggest that older women express increased feelings of loneliness, particularly during unprecedented situations like the COVID-19 pandemic, and the importance of monitoring, preventing, and managing this silent epidemic during this and future similar crises. However, older women are not a monolithic group vulnerable to loneliness; certain factors may alter the risk.
Specific factors associated with worsening loneliness in our older women sample are mostly consistent with other pre- and intra-COVID-19 data from mixed-age and -gender studies. Older subgroups who reported greater loneliness during the pandemic included those living alone, having limited social contact, experiencing changes to their daily routine, and reporting poor health (12,18,33,34). Also, about two thirds of older adults with chronic health conditions (35) and over 50% of oncology patients (36) were found to experience at least moderate loneliness during the pandemic. Prior studies have also reported that experiencing bereavement and the presence of mental disorders is associated with higher loneliness during the COVID-19 lockdown (9,12).
Loneliness intensifies after bereavement and is a gateway symptom to subsequent depressive symptoms in grieving individuals (37). Moreover, intense loneliness is one of the main associated symptoms in the diagnostic criteria for prolonged grief disorder, a clinical condition that is diagnosed 12 months postloss in those experiencing protracted and disabling grief symptoms. Also, chronic medical conditions, including vascular factors, and CVD are associated with increased loneliness risk; those who have these health conditions have worse outcomes especially if they are lonely (2). Our data provide important clues as to the specific older women subgroups (ie, those experiencing disruptive life events such as bereavement, chronic medical and mental health conditions, living alone, and disruptions in social connections) who may benefit from targeted interventions to alleviate or prevent loneliness.
Few studies have examined the association between loneliness and race in older adults. Emerging COVID-19 data suggest that older persons of color with chronic conditions report lower loneliness (35). Lower odds of depression and anxiety have also been reported during COVID-19 in those identifying as Black; similar trends were also seen in those identifying as Asian (38). Similarly, young Asian Americans were less likely to report high levels of depressive and anxiety symptoms compared to Whites in another COVID-19 study (39). Our results suggest that, among older adults, identifying as Black or Asian/Pacific Islander (compared with White) is associated with decreases in loneliness from the pre- to intrapandemic period. Plausible explanations for racial differences may include greater social connections and support available to older Black and Asian/Pacific Islander women relative to their White counterparts. For instance, a pre-COVID-19 study found that non-Hispanic White persons are more likely to live alone, have limited social contact, and be childless than Black persons; in fact, being a Black woman was found to be associated with less social isolation (40).
We also observed that being more physically active and more optimistic, consuming moderate to no alcohol, and reporting a higher purpose in life are associated with a decrease in loneliness from the pre- to intrapandemic period. These associations are supported in the literature across men and women of different ages (2,41–43). Our findings raise the possibility that interventions focused on increasing physical activity, moderating alcohol intake, and cultivating positive psychological attributes such as optimism or purpose in life may serve to protect against detrimental loneliness changes in older women.
We found stronger positive associations of change in loneliness from the pre- to intrapandemic period were associated with higher perceived stress, depressive, and anxiety symptoms during the pandemic. These findings are in line with the published cross-sectional and longitudinal pre-COVID-19 literature (44–47). In the Chicago Health, Aging, and Social Relations Study, loneliness predicted subsequent changes in depressive symptoms in a young-old sample; however, this association did not vary based on objective social connection measures of social network and support (48). In a representative older adult sample, being lonely, but not socially isolated as determined by living alone, and having no direct social contacts were cross-sectionally associated with higher depressive symptoms during the COVID-19 lockdown (49). Consistent with these findings, living alone was not associated with mental health measures and did not modify the longitudinal loneliness–mental health associations in our study. However, modest positive associations were observed between disruptions in living arrangement due to COVID-19 and mental health variables in our study. Furthermore, women reporting living arrangement disruptions during COVID-19 showed a stronger loneliness–depressive symptom association in our study. Collectively, these results suggest that loneliness and disruptions in living arrangements increase vulnerability to stress and mental health issues. As older women belong to an age group vulnerable to experiencing COVID-19-related complications and deaths, the feeling of being protected against virus exposure while living alone may have alleviated depression and anxiety risk in this age cohort.
Such social exclusion, however, has led many older adults to rely heavily on digital and other non-in-person services to stay in touch with others in society (50). Among younger and middle-aged adults, modern information and communication technologies (ICTs) including smartphones, laptops, computers, and high-speed internet services have increased social networking during the pandemic by using video call apps and video conferencing platforms. On the contrary, older adults have been slower to adapt to these communication methods, even though their access to digital technologies has increased in recent years. Older adults use modern ICTs in more basic ways than their younger counterparts (51) and continue to prefer in-person contact and telephone communication methods as their primary modes of staying socially connected (50).
The older women in the WHI cohort are no exception to this digital gap. While over 90% of older women in our study stayed in touch via telephone, only one third also used video calls to stay in touch with others. These data, combined with our findings that a lack of in-person communication was associated with higher mental health symptoms, shed light on yet another adverse consequence of COVID-19 afflicting older adults. Factors associated with digital inequalities among older adults require additional research. The influence of staying in touch using different modalities of modern ICTs, rather than telephone, on mental health adversities in older adults should be addressed in future studies. These lines of research may aid in designing interventions to enhance digital technology adoption and use among older adults, especially in those with physical disabilities and cognitive impairment who are living alone or in long-term care facilities, to mitigate loneliness and mental health symptoms (50,52).
Multiple lifestyle behavioral and psychological mechanisms may increase the vulnerability of older women to feel lonely and link loneliness with poor mental health outcomes (1,2). Moreover, several plausible biological factors, including inflammation, activation of the hypothalamus–pituitary–adrenocortical axis, neurodegeneration, and brain amyloid burden, have been proposed as mechanisms linking loneliness with adverse mental health outcomes (2,53). These and other potential biological pathways should be the focus of future investigations.
Our study has several strengths, including the availability of longitudinal loneliness assessments both before and during the pandemic, change in objective social connection measures due to the pandemic, information on psychological and mental health measures during the pandemic, as well as several covariates in a large sample of older women. However, there are study limitations. Our study cohort is a subsample from a larger sample of women who participated in multiple WHI studies that spanned over several decades. Thus, selection bias is possible. Our sample is mostly White, highly educated and at the time of WHI study enrollment, had higher incomes; thus, our results may not be generalizable. Also, we do not have data on financial status/income during this study period. Nevertheless, we would like to highlight that the oldest-old age groups in the United States are less diverse than the younger age subgroups (54). Moreover, the WHI is one of the largest and more diverse cohorts of older women available, and major efforts were made at enrollment to recruit a diverse study population. Specifically, our sample comprised of 1 324 Black/African American and 624 Asian/Pacific Islander, as well as 886 Hispanic women older than the age of 70. Future studies are needed to specifically address the potential adverse impact of the pandemic on predominantly non-White, financially disadvantaged, and poorly educated oldest-old cohorts. The first loneliness measure was collected about 4–6 years before the intrapandemic assessment. Several factors could have contributed to changes in loneliness over this extended timeframe; we attempted to address this by adjusting for a robust set of covariates in our models. One major stressor, however, deserves special mention. Older women may have experienced the death of loved ones during this period. While we do not have bereavement data for the entire 4- to 6-year period, we collected this data for 1 year before the 2020 loneliness and mental health assessments. The relationship between the death of a spouse or partner over 1 year before the 2020 assessment and loneliness changes was examined (Figure 2 and Supplementary Table 1). The mental health variables were all self-report measures, which cannot replace clinician diagnoses of mental disorders. Also, other self-report scales that can assess depressive and anxiety symptoms in more detail than those used here are available (55,56). Cognitive assessments were not available; the effects of cognitive impairment on the loneliness–mental health associations remain to be elucidated. Finally, a small number of women in our study identified themselves as American Indian/Alaskan Native; however, we are unable to perform analyses or draw any conclusions in this specific racial subgroup due to the small sample size. Future studies with larger samples of Native American participants with different tribal affiliations should explore the associations between loneliness and mental health outcomes.
In summary, loneliness increased in older women during the COVID-19 pandemic. Loneliness worsening was associated with increased stress and higher depressive and anxiety symptoms during the pandemic. Several factors were associated with worsening and decreases of loneliness during the pandemic. Our preliminary findings thus point to opportunities for possible interventions targeting lifestyle behaviors (eg, physical activity, alcohol intake), optimism and purpose in life, disrupted social connections, and monitoring those with specific medical and mental health histories that may reduce loneliness and improve mental health in older women.
Supplementary Material
Acknowledgments
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Joan McGowan, Leslie Ford, and Nancy Geller.
Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg.
Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Jennifer Robinson; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker; (University of Nevada, Reno, NV) Robert Brunner.
Sponsorʼs role: The National Heart, Lung, and Blood Institute has representation on the Womenʼs Health Initiative Steering Committee, which governed the design and conduct of the study, the interpretation of the data, and preparation and approval of manuscripts.
Contributor Information
Joseph S Goveas, Department of Psychiatry and Behavioral Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin, USA.
Roberta M Ray, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA.
Nancy F Woods, University of Washington School of Nursing, Seattle, Washington, USA.
JoAnn E Manson, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, USA.
Candyce H Kroenke, Division of Research, Kaiser Permanente Northern California, Oakland, California, USA.
Yvonne L Michael, Department of Epidemiology and Biostatistics, Dornsife School of Public Health, Drexel University, Philadelphia, Pennsylvania, USA.
Aladdin H Shadyab, Herbert Wertheim School of Public Health and Human Longevity Science, University of California, San Diego, La Jolla, California, USA.
Jaymie R Meliker, Program in Public Health, Department of Family, Population and Preventive Medicine, Stony Brook University, Stony Brook, New York, USA.
Jiu-Chiuan Chen, Departments of Preventive Medicine and Neurology, University of Southern California Keck School of Medicine, Los Angeles, California, USA.
Lisa Johnson, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA.
Charles Mouton, Office of the Provost, University of Texas Medical Branch, Galveston, Texas, USA.
Nazmus Saquib, College of Medicine, Sulaiman AlRajhi University, Al Bukayriyah, Saudi Arabia.
Julie Weitlauf, Veterans Affairs Palo Alto Health Care System, Palo Alto, California, USA; Department of Psychiatry and Behavioral Sciences, Stanford University, Stanford, California, USA.
Jean Wactawski-Wende, Department of Epidemiology and Environmental Health, School of Public Health and Health Professions, University at Buffalo (SUNY), Buffalo, New York, USA.
Michelle Naughton, Ohio State University College of Medicine, Columbus, Ohio, USA.
Sally Shumaker, Department of Social Sciences and Health Policy, Wake Forest School of Medicine, Winston-Salem, North Carolina, USA.
Garnet L Anderson, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA.
Funding
We gratefully acknowledge the 161,808 women who enrolled in the Women’s Health Initiative almost 30 years ago, and those who are able to remain active and engaged partners in this journey to advance our understanding of the health and well-being of women. We are particularly grateful to the 49,695 women who participated in the WHI COVID-19 Survey – 1, launched during a disruptive period in their lives. Their generosity adds critical information on the impact of the pandemic on one of our most vulnerable populations. We also thank the WHI Clinical Coordinating Center at Fred Hutchinson Cancer Research Center for conducting the COVID survey and providing financial and statistical support for this effort, as well as the four WHI Regional Centers who assisted in conducting the COVID-19 Survey - 1 (Stanford School of Medicine, The Ohio State University College of Medicine, University at Buffalo School of Public Health & Health Professions, and Wake Forest University Health Sciences). Finally, we thank Wake Forest University Health Sciences for providing the financial support for publication costs that made this supplement possible.
Conflict of Interest
None declared.
Author Contributions
Conception or design of the work: J.S.G., R.M.R., S.S., and G.L.A. Acquisition and analysis of data: J.S.G., R.M.R., J.E.M., C.H.K., L.J., J.W.-W., M.N., S.S., and G.L.A. Preparation of the manuscript: J.S.G. and R.M.R. Interpretation of data, critical revision of the work for important intellectual content, and final approval of the version to be published: All authors.
References
- 1. Donovan NJ, Blazer D. Social isolation and loneliness in older adults: review and commentary of a national academies report. Am J Geriatr Psychiatry. 2020;28(12):1233–1244. doi: 10.1016/j.jagp.2020.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Academies of Sciences Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. The National Academies Press; 2020. [PubMed] [Google Scholar]
- 3. Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cudjoe TKM, Roth DL, Szanton SL, Wolff JL, Boyd CM, Thorpe RJ. The epidemiology of social isolation: National Health and Aging Trends Study. J Gerontol B Psychol Sci Soc Sci. 2020;75(1):107–113. doi: 10.1093/geronb/gby037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hawkley LC, Wroblewski K, Kaiser T, Luhmann M, Schumm LP. Are U.S. older adults getting lonelier? Age, period, and cohort differences. Psychol Aging. 2019;34(8):1144–1157. doi: 10.1037/pag0000365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- 7. Kuiper JS, Zuidersma M, Oude Voshaar RC, et al. Social relationships and risk of dementia: a systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2015;22:39–57. doi: 10.1016/j.arr.2015.04.006 [DOI] [PubMed] [Google Scholar]
- 8. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020;265:113521. doi: 10.1016/j.socscimed.2020.113521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291:113267. doi: 10.1016/j.psychres.2020.113267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Luchetti M, Lee JH, Aschwanden D, et al. The trajectory of loneliness in response to COVID-19. Am Psychol. 2020;75(7):897–908. doi: 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seifert A, Hassler B. Impact of the COVID-19 pandemic on loneliness among older adults. Front Sociol. 2020;5:590935. doi: 10.3389/fsoc.2020.590935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH. Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci. 2021;76(7):e249–e255. doi: 10.1093/geronb/gbaa111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Peng S, Roth AR. Social isolation and loneliness before and during the COVID-19 pandemic: a longitudinal study of US Adults over 50. J Gerontol B Psychol Sci Soc Sci. 2021. doi: 10.1093/geronb/gbab068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rumas R, Shamblaw AL, Jagtap S, Best MW. Predictors and consequences of loneliness during the COVID-19 pandemic. Psychiatry Res. 2021;300:113934. doi: 10.1016/j.psychres.2021.113934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Varga TV, Bu F, Dissing AS, et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg Health Eur. 2021;2:100020. doi: 10.1016/j.lanepe.2020.100020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hansen T, Nilsen TS, Yu B, et al. Locked and lonely? A longitudinal assessment of loneliness before and during the COVID-19 pandemic in Norway. Scand J Public Health. 2021;49:766–73. doi: 10.1177/1403494821993711 [DOI] [PubMed] [Google Scholar]
- 18. Savage RD, Wu W, Li J, et al. Loneliness among older adults in the community during COVID-19: a cross-sectional survey in Canada. BMJ Open. 2021;11:e044517. doi: 10.1136/bmjopen-2020-044517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wickens CM, McDonald AJ, Elton-Marshall T, et al. Loneliness in the COVID-19 pandemic: associations with age, gender and their interaction. J Psychiatr Res. 2021;136:103–108. doi: 10.1016/j.jpsychires.2021.01.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Design of the Women’s Health Initiative clinical trial and observational study. The Women’s Health Initiative Study Group. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0 [DOI] [PubMed] [Google Scholar]
- 21. Sams N, Fisher DM, Mata-Greve F, et al. Understanding psychological distress and protective factors amongst older adults during the COVID-19 pandemic. Am J Geriatr Psychiatry. 2021;29(9):881–894. doi: 10.1016/j.jagp.2021.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosom Med. 2013;75(2):161–170. doi: 10.1097/PSY.0b013e31827f09cd [DOI] [PubMed] [Google Scholar]
- 24. Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 26. Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12(2):277–287. doi: 10.1037//0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- 27. Goveas JS, Espeland MA, Woods NF, Wassertheil-Smoller S, Kotchen JM. Depressive symptoms and incidence of mild cognitive impairment and probable dementia in elderly women: the Women’s Health Initiative Memory Study. J Am Geriatr Soc. 2011;59(1):57–66. doi: 10.1111/j.1532-5415.2010.03233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Borhani NO, Applegate WB, Cutler JA, et al. Systolic Hypertension in the Elderly Program (SHEP). Part 1: rationale and design. Hypertension. 1991;17:II2–15. doi: 10.1161/01.hyp.17.3_suppl.ii2 [DOI] [PubMed] [Google Scholar]
- 29. Patient-reported outcomes measurement information system; dynamic tools to measure health outcomes from the patient perspective. http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Adult_Profile_Scoring_Manual.pdf
- 30. Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D; PROMIS Cooperative Group. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ryff CD. In the eye of the beholder: views of psychological well-being among middle-aged and older adults. Psychol Aging. 1989;4(2):195–201. doi: 10.1037//0882-7974.4.2.195 [DOI] [PubMed] [Google Scholar]
- 32. Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727. doi: 10.1037//0022-3514.69.4.719 [DOI] [PubMed] [Google Scholar]
- 33. Losada-Baltar A, Jiménez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro MDS, Fernandes-Pires J, Márquez-González M. “We are staying at home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e10–e16. doi: 10.1093/geronb/gbaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tomaz SA, Coffee P, Ryde GC, et al. Loneliness, wellbeing, and social activity in Scottish older adults resulting from social distancing during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:4517. doi: 10.3390/ijerph18094517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Polenick CA, Perbix EA, Salwi SM, Maust DT, Birditt KS, Brooks JM. Loneliness during the COVID-19 pandemic among older adults with chronic conditions. J Appl Gerontol. 2021;40(8):804–813. doi: 10.1177/0733464821996527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Miaskowski C, Paul SM, Snowberg K, et al. Loneliness and symptom burden in oncology patients during the COVID-19 pandemic. Cancer. 2021;127(17):3246–3253. doi: 10.1002/cncr.33603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fried EI, Bockting C, Arjadi R, et al. From loss to loneliness: the relationship between bereavement and depressive symptoms. J Abnorm Psychol. 2015;124(2):256–265. doi: 10.1037/abn0000028 [DOI] [PubMed] [Google Scholar]
- 38. Kantor BN, Kantor J. Mental health outcomes and associations during the COVID-19 pandemic: a cross-sectional population-based study in the United States. Front Psychiatry. 2020;11:569083. doi: 10.3389/fpsyt.2020.569083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Taylor RJ, Chatters LM, Taylor HO. Race and objective social isolation: older African Americans, Black Caribbeans, and non-Hispanic Whites. J Gerontol B Psychol Sci Soc Sci. 2019;74(8):1429–1440. doi: 10.1093/geronb/gby114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol. 2009;28(3):354–363. doi: 10.1037/a0014400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rius-Ottenheim N, Kromhout D, van der Mast RC, Zitman FG, Geleijnse JM, Giltay EJ. Dispositional optimism and loneliness in older men. Int J Geriatr Psychiatry. 2012;27(2):151–159. doi: 10.1002/gps.2701 [DOI] [PubMed] [Google Scholar]
- 43. Kang Y, Cosme D, Pei R, Pandey P, Carreras-Tartak J, Falk EB. Purpose in life, loneliness, and protective health behaviors during the COVID-19 pandemic. Gerontologist. 2021;61(6):878–887. doi: 10.1093/geront/gnab081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Choi H, Irwin MR, Cho HJ. Impact of social isolation on behavioral health in elderly: systematic review. World J Psychiatry. 2015;5(4):432–438. doi: 10.5498/wjp.v5.i4.432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Beutel ME, Klein EM, Brähler E, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17(1):97. doi: 10.1186/s12888-017-1262-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Van As BAL, Imbimbo E, Franceschi A, Menesini E, Nocentini A. The longitudinal association between loneliness and depressive symptoms in the elderly: a systematic review. Int Psychogeriatr. 2021:1–13. doi: 10.1017/S1041610221000399 [DOI] [PubMed] [Google Scholar]
- 47. Domènech-Abella J, Mundó J, Haro JM, Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J Affect Disord. 2019;246:82–88. doi: 10.1016/j.jad.2018.12.043 [DOI] [PubMed] [Google Scholar]
- 48. Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25(2):453–463. doi: 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Muller F, Rohr S, Reininghaus U, Riedel-Heller SG. Social Isolation and Loneliness during COVID-19 Lockdown: associations with depressive symptoms in the German old-age population. Int J Environ Res Public Health. 2021;18:3615. doi: 10.3390/ijerph18073615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Seifert A, Cotten SR, Xie B. A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. J Gerontol B Psychol Sci Soc Sci. 2021;76(3):e99–e103. doi: 10.1093/geronb/gbaa098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. van Boekel LC, Peek ST, Luijkx KG. Diversity in older adults’ use of the internet: identifying subgroups through latent class analysis. J Med Internet Res. 2017;19(5):e180. doi: 10.2196/jmir.6853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Marston HR, Ivan L, Fernández-Ardèvol M, et al. COVID-19: technology, social connections, loneliness, and leisure activities: an international study protocol. Front Sociol. 2020;5:574811. doi: 10.3389/fsoc.2020.574811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Donovan NJ, Okereke OI, Vannini P, et al. Association of higher cortical amyloid burden with loneliness in cognitively normal older adults. JAMA Psychiatry. 2016;73(12):1230–1237. doi: 10.1001/jamapsychiatry.2016.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Roberts AW, Ogunwole SU, Blakeslee L, Rabe MA.. The Population 65 Years and Older in the United States: 2016. American Community Survey Reports, ACS-38. U.S. Census Bureau; 2018. [Google Scholar]
- 55. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pocklington C, Gilbody S, Manea L, McMillan D. The diagnostic accuracy of brief versions of the Geriatric Depression Scale: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2016;31(8):837–857. doi: 10.1002/gps.4407 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.