ABSTRACT
Background
The coronavirus disease 2019 (COVID-19) pandemic is placing a significant strain on healthcare. We conducted a national survey of the UK nephrology workforce to understand its impacts on their working lives.
Methods
An online questionnaire incorporating the Maslach Burnout Inventory score was distributed between 31 March and 1 May 2021, with a focus on COVID-19 and long COVID incidence, vaccine uptake, burnout and working patterns. Data were analysed qualitatively and quantitatively; multivariable logistic regression was used to identify associations.
Results
A total of 423 responses were received. Of them, 29% had contracted COVID-19, which was more common among doctors and nurses {odds ratio [OR] 2.18 [95% confidence interval (CI) 1.13–4.22]} and those <55 years of age [OR 2.60 (95% CI 1.38–4.90)]. Of those who contracted COVID-19, 36% had symptoms of long COVID, which was more common among ethnicities other than White British [OR 2.57 (95% CI 1.09–6.05)]. A total of 57% had evidence of burnout, which was more common among younger respondents [OR 1.92 (95% CI 1.10–3.35)] and those with long COVID [OR 10.31 (95% CI 1.32–80.70)], and 59% with reconfigured job plans continued to work more hours. More of those working full-time wished to retire early. A total of 59% experienced remote working, with a majority preference for continuing this in the future. In terms of vaccination, 95% had received one dose of a COVID-19 vaccine and 86% had received two doses by May 2021.
Conclusions
Burnout and long COVID is prevalent with impacts on working lives. Some groups are more at risk. Vaccination uptake is high and remote and flexible working were well received. Institutional interventions are needed to prevent workforce attrition.
Keywords: burnout, COVID-19, healthcare professionals, long COVID, survey, workforce, working patterns
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic is having a major impact on healthcare delivery. Hospitals have been placed under unprecedented strain and roles and working patterns of healthcare professionals (HCPs) have been reconfigured to adapt. For nephrology HCPs in the UK, this included reassignments to intensive care and internal medicine, altered shift patterns and remote working [1]. These reconfigurations were needed to maintain safe care, protect vulnerable HCPs and lower the risk of healthcare settings becoming hubs of transmission.
The impact of these pandemic-driven reconfigurations on nephrology HCPs has not been well described. To address this, we surveyed the UK nephrology workforce in July 2020, following the first surge of COVID-19 in the UK. We reported fatigue, burnout and compromises to work–life balance and training [1]. We did not investigate the proportion that suffered with COVID-19, nor its impacts on their lives. It is also uncertain if our early findings are sustained in the second year of the pandemic.
The aim of this study was to identify the impact of the pandemic on the nephrology workforce, 12 months on, with regards to the incidence of COVID-19 and long COVID and its impacts on working lives, the uptake of COVID-19 vaccinations, burnout and the impact of COVID-19 on working patterns and training opportunities. The findings may promote the modification of practices that have had a negative impact on HCPs and utilize positive experiences to better support the workforce.
MATERIALS AND METHODS
An online questionnaire was developed by the UK Kidney Association (UKKA). The UKKA represents nephrology-affiliated HCPs including doctors, nurses, technicians, pharmacists, psychologists and social workers [2]. The questionnaire was distributed via two e-mails sent 3 weeks apart to all members of professional nephrology groups, through social media and was cascaded regionally by HCPs. Responses were accepted between 31 March and 1 May 2021.
Questions were grouped into demographics, COVID-19 exposures and vaccinations, burnout, working patterns, remote working, training, perceived future impacts and overall experience. Questions were predominantly closed, with optional free-text responses. A decision tree configuration allowed questions to be skipped if not relevant. Completion was voluntary and not incentivized. Responses were anonymous.
Data regarding ethnicity were collected according to the UK government classification [3]. Regions were designated by catchments for national medical training programmes [4]. Age was collected categorically.
Burnout was assessed using the Maslach Burnout Inventory (MBI) score [5], which comprises three scales. The scores from emotional exhaustion, depersonalization and personal accomplishment scales determined to represent burnout were >26, >9 and <34, respectively [6].
For analyses examining COVID-19 and long COVID, a COVID-19 diagnosis was taken as a respondent self-reporting a confirmed infection following testing or COVID-19 antibodies presence prior to vaccination. For analyses examining burnout and working patterns, symptoms consistent with COVID-19 prior to community testing becoming available were included with confirmed diagnoses; this required 10 days of self-isolation and thus could impact workforce well-being. Long COVID was defined as persistent symptoms following acute COVID-19. Those with symptom resolution within 3 months were excluded.
Quantitative data are presented using descriptive statistics with proportions. Denominators are the total number of eligible responses. Comparisons were made using the chi-squared test or Fisher's exact test for categorical variables. Multivariable logistic regression models were performed to examine associations with contracting COVID-19, self-isolation, working patterns and burnout. Covariates were selected a priori to include age, sex, ethnicity, occupation, working pattern (in-hospital or remote working), living arrangement and COVID-19 status. Categories for ethnicity, occupation, age, living status and working pattern were pooled due to the limited sample size (White versus all other ethnicities, doctors and nurses versus other HCPs, age <55 versus ≥55 years, living alone versus not alone, and exclusively in-hospital versus remote working). Burnout was analysed against those who did not contract COVID-19, had COVID-19 and recovered and had long COVID. To avoid multiple testing, burnout was considered present if a score on any one of the three scales exceeded its threshold.
All models included complete cases only, with results reported as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was determined as P-values <0.05. Analyses were performed in Stata version 15 (StataCorp, College Station, TX, USA) or SPSS version 26 (IBM, Armonk, NY, USA).
Free-text answers were analysed qualitatively to identify key themes using the following steps: (i) comments were categorized as positive/negative, (ii) inductive codes were derived and applied to relevant comments using ‘keywords in context’ and ‘repetition of words’ techniques, (iii) codes sharing similar meaning were amalgamated into subthemes and frequencies were measured and (iv) descriptive analyses were applied to describe free-text respondents’ demographics in accordance with reported best practice techniques [7, 8]. Themes and codes were analysed independently by M.S. and H.B. and discrepancies were resolved by discussion to enhance the reliability of results.
RESULTS
Demographics
A total of 423 responses were received. The majority were female (74%), of White ethnicity (80%) and were nurses (36%) or doctors (34%) predominantly caring for adults (90%). Consultants (attending clinicians) were the most frequent respondents among doctors (64%) and dialysis nurses the most frequent among nurses (29%) (Table 1, detailed breakdown in Supplementary Table S1).
Table 1.
Demographics of survey respondents
| Characteristics | n (%) |
|---|---|
| Sex | 423 (100) |
| Male | 110 (26) |
| Female | 313 (74) |
| Age group (years) | 422 (100) |
| <25 | 2 (0.4) |
| 25–34 | 63 (15) |
| 35–44 | 110 (26) |
| 45–54 | 151 (36) |
| 55–64 | 91(22) |
| ≥65 | 5 (1) |
| Ethnicity | 416 (100) |
| Asian/Asian British | 69 (17) |
| Black/Black British | 8 (1) |
| Mixed | 6 (1) |
| White | 329 (80) |
| Other | 4(1) |
| Region | 417 (100) |
| England | 343 (82) |
| Northern Ireland | 11 (3) |
| Scotland | 49 (12) |
| Wales | 14 (3) |
| Profession | 420 (100) |
| Doctor | 144 (34) |
| Nurse | 150 (36) |
| Other multidisciplinary professional | 125 (30) |
| Retired | 1 (0) |
| Living situation | 421 (100) |
| Alone | 58 (14) |
| Not alone | 363 (86) |
| Remote working | 321 (100) |
| Yes, all the time | 27 (8) |
| Yes, some of the time | 167 (52) |
| No | 127 (40) |
Incidence of COVID-19 and its impacts on working lives
Approximated incidence of COVID-19
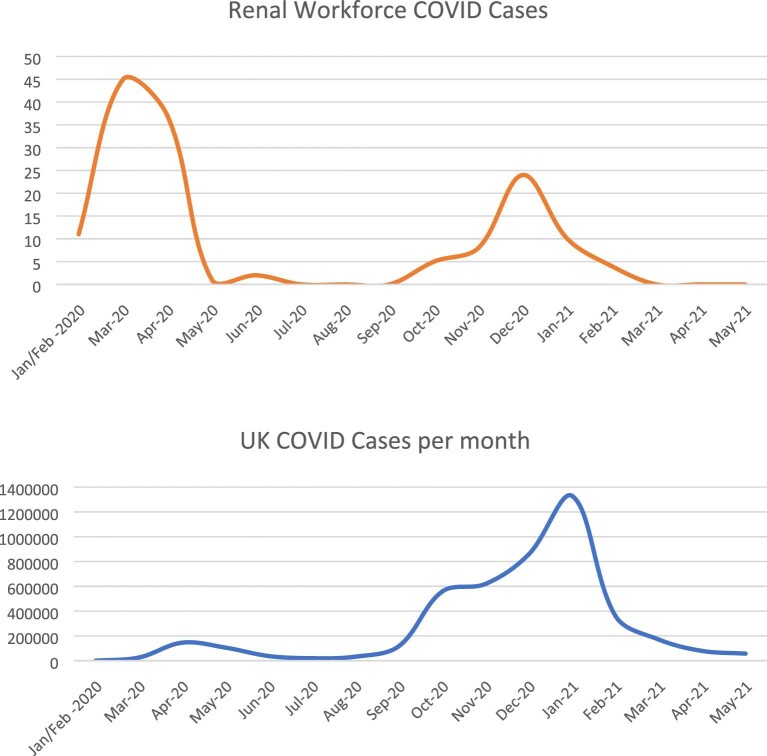
By 1 May 2021, 29% (120/421) reported a diagnosis of COVID-19. A further 8% (33/421) reported symptoms consistent with COVID-19 but were not tested, as symptoms occurred prior to May 2020, when community testing became available. Peaks occurred in March/April 2020 and December 2020/January 2021, mirroring national cases [9] (Figure 1).
FIGURE 1:
Cases of COVID-19 in the UK nephrology workforce compared with UK national cases.
On adjusted analyses, identifying as male [OR 2.03 (95% CI 1.13–3.65)], a doctor or a nurse [OR 2.60 (95% CI 1.38–4.90)] or <55 years of age [OR 2.18 (95% CI 1.13–4.22)] associated with COVID-19 (Table 2).
Table 2.
Univariable and multivariable logistic regression models examining factors associated with COVID-19, isolation episodes and long COVID
| COVID positive (n = 87/281) | ||||
|---|---|---|---|---|
| Variables | Unadjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
| Age <55 years (Ref: ≥55) | 1.94 (1.04–3.61) | 0.04 | 2.18 (1.13–4.22) | 0.02 |
| Male sex (Ref: female) | 2.13 (1.21–3.73) | 0.01 | 2.03 (1.13–3.65) | 0.02 |
| Non-White ethnicity (Ref: White) | 1.36 (0.73–2.56) | 0.34 | 0.97 (0.50–1.90) | 0.92 |
| Doctor/nurse (Ref: other professions) | 2.60 (1.40–4.81) | >0.01 | 2.60 (1.38–4.90) | >0.01 |
| Living alone (Ref: with others) | 1.03 (0.50–2.16) | 0.93 | 1.10 (0.50–2.39) | 0.82 |
| On site working (Ref: remote working) | 1.12 (0.67–1.88) | 0.67 | 1.08 (0.63–1.87) | 0.77 |
| Isolation (n = 171/311) | ||||
| Unadjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value | |
| Age <55 years (Ref: ≥55) | 2.82 (1.35–3.85) | >0.01* | 2.37 (1.37–4.08) | >0.01* |
| Male sex (Ref: female) | 1.45 (0.86–2.46) | 0.17 | 1.44 (0.83–2.50) | 0.19 |
| Non-White ethnicity (Ref: White) | 1.54 (0.85–2.81) | 0.16 | 1.91 (0.63–2.23) | 0.59 |
| Doctor/nurse (Ref: other professions) | 1.76 (1.08–2.89) | 0.02* | 1.83 (1.10–3.04) | 0.02* |
| Living alone (Ref: with others) | 0.99 (0.51–1.90) | 0.98 | 1.05 (0.53–2.10) | 0.89 |
| On site working (Ref: remote working) | 1.23 (0.78–1.95) | 0.37 | 1.14 (0.71–1.85) | 0.58 |
| Long COVID (n = 41/117) | ||||
| Unadjusted odds ratio (95% CI) | P-value | Adjusted odds ratio (95% CI) | P-value | |
| Age <55 years (Ref: ≥55) | 1.63 (0.54–4.89) | 0.39 | 1.42 (0.45–4.50) | 0.55 |
| Male sex (Ref: female) | 1.86 (0.83–4.13) | 0.13 | 1.75 (0.76–4.03) | 0.19 |
| Non-White ethnicity (Ref: White) | 2.93 (1.28–6.71) | 0.11 | 2.57 (1.09–6.05) | 0.03* |
| Doctor/nurse (Ref: other professions) | 1.77 (0.59–5.28) | 0.31 | 1.71 (0.55–5.33) | 0.35 |
*P < 0.05
Self-isolation
Self-isolation episodes were reported by 59% (242/411) of respondents due to confirmed or suspected COVID-19 or a possible exposure. A total of 517 episodes were reported; 44% (106/242) of respondents isolated once while 29% (69/242) isolated at least three times.
On adjusted analyses, being a doctor or a nurse [OR 1.83 (95% CI 1.10–3.04)], or <55 years of age [OR 2.37 (95% CI 1.37–4.08)] associated with needing to self-isolate (Table 2).
Long COVID
Of those who had COVID-19, 36% (43/120) had persistent symptoms consistent with long COVID. Fatigue was most common [70% (30/43)], followed by mood changes (19%) and ageusia/anosmia (14%). Major impacts of long COVID on quality of life and work were reported (Supplementary Table S2).
Among those who had COVID-19, those who self-reported an ethnicity other than White were more likely to have developed long COVID on adjusted analysis [OR 2.57 (95% CI 1.09–6.05)] (Table 2). Living and remote working status were not included in this adjusted analysis to preserve the sample size.
Uptake of COVID-19 vaccination
By May 2021, 95% (398/419) had received a first dose of a COVID-19 vaccine. Of the 21 not vaccinated, 48% (10/21) were intending to get vaccinated. Of the remaining 11, 6 declined due to pregnancy, 2 cited the presence of COVID-19 antibodies, 2 did not provide a reason and 1 cited lack of rigour surrounding vaccine data. Those declining vaccinations were from varying age groups, occupations, regions and ethnicities.
A second vaccine dose had been received by 86% (340/396). Of those yet to receive their second dose, 96% (54/56) intended to. Two respondents intended to decline their second dose, citing pregnancy and a vaccine reaction, respectively.
Burnout
Burnout questions were completed by 363 respondents (86%). Approximately 57% had evidence of burnout. When examining individual burnout subscales, 14% (49/363) scored for depersonalization, 32% (116/363) scored for low personal accomplishment and 41% (148/363) scored for emotional exhaustion; some participants had evidence of burnout in more than one subscale.
On adjusted analysis, burnout associated with age [less likely in those >55 years of age; OR 0.52 (95% CI 0.39–0.91) and long COVID [OR 10.31 (95% CI 1.32–80.70)] (Table 3).
Table 3.
Univariable and multivariable logistic regression models examining factors associated with burnout on any of the MBI subscales
| Burnout on MBI score (n = 207/363) | ||||
|---|---|---|---|---|
| Variables | Unadjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
| Age <55 years (Ref: ≥55) | 1.71 (1.06–2.77) | 0.03* | 1.92 (1.10–3.35) | 0.02* |
| Male sex (Ref: female) | 1.16 (0.72–1.88) | 0.54 | 1.01 (0.54–1.89) | 0.97 |
| Non-White ethnicity (Ref: White) | 1.65 (0.93–2.93) | 0.09 | 1.57 (0.81–3.02) | 0.18 |
| Other profession (Ref: doctor/nurse) | 1.45 (0.95–2.21) | 0.08 | 1.72 (0.98–3.03) | 0.06 |
| Living alone (Ref: with others) | 1.38 (0.73–2.60) | 0.34 | 1.42 (0.68–2.97) | 0.36 |
| Remote working (Ref: on-site work) | 1.08 (0.69–1.69) | 0.74 | 1.04 (0.63–1.74) | 0.87 |
| COVID-19 (Ref: not had COVID) | ||||
| COVID-19 and recovered | 0.78 (0.50–1.22) | 0.28 | 0.62 (0.37–1.02) | 0.06 |
| Long COVID | 12.82 (1.68–97.94) | 0.02* | 10.31 (1.32–80.70) | 0.03* |
*P < 0.05
Implications of the COVID-19 pandemic on training and working patterns
New patterns of working
Patterns of work changed in 65% (233/360) of respondents between March and August 2020. Approximately 43% reported changes after August 2020. Changes were most commonly due to departmental restructuring due to the pandemic (79%), with personal health vulnerabilities, caregiver responsibilities and personal choice comprising the remainder. More of the nephrology workforce worked in intensive care units (12% versus 4%), remote settings (11% versus 3%) and acute internal medicine (20% versus 10%) during the pandemic. Fewer were involved in academic work (3% versus 9% pre-pandemic).
Approximately 75% of those who underwent role reconfigurations felt they received adequate preparation, despite the same proportion receiving <2 weeks’ notice of working pattern or role changes. Approximately 60% of all respondents reported working more hours and 67% worked more frequently out-of-hours.
By May 2021, 61% (140/228) of respondents had returned to their pre-pandemic work role and pattern. A return to normal working patterns occurred before August 2020 in 26% (33/125), between August and December 2020 in 27% (32/125) and between January and May 2021 in 48% (60/125). Of those still in adapted roles at the time of the survey, 59% reported continuing to work more hours overall and more frequently out-of-hours.
Fatigue increased after the first wave (March–May 2020 peak in UK COVID-19 cases [10]) and second wave (November 2020–April 2021 peak in UK COVID-19 cases [10]) in 54% and 59% of respondents, respectively. A total of 22% (n = 88) of respondents noted increased aggression displayed by patients towards staff at work. Fewer educational opportunities were reported by 66% after the first wave and by 46% by the end of the second wave. Difficulties in accessing development opportunities compared with pre-pandemic levels were reported by 61% after the first wave and 46% after the second wave. Approximately 79% of the workforce felt supported overall and a stronger sense of team was reported by 70% after both waves. There was no difference in perceived education and development opportunities reported by those working remotely, but they had a diminished sense of team compared with those working on-site (59% versus 24%; chi-squared P = 0.01).
Effect on training
Of the 35 respondents in a training (fellows) programme (24 females, 11 males), nearly one-third (n = 11) reported extension to training or being unable to complete training when planned. More than 20% (n = 8) reported that time worked during the pandemic would not count towards training, mainly by those who returned to clinical work from research or who were working from home.
Remote working and learning
A total of 51% (167/327) moved to partial remote working and 8% (27/327) moved to complete remote working. Remote working was adopted to minimize staff contact/enable social distancing in the workplace (47%), to provide remote clinic services for patients (26%) and for medical/personal reasons. While 75% felt they were adequately resourced, there were concerns regarding internet/computer software reliability and inadequate phlebotomy services to facilitate telephone clinics. Approximately 84% experienced job satisfaction and felt their work was valued and 80% wanted to preserve an element of remote working in the future. These findings mirrored feedback from fellows following a national fellows virtual seminar (Renal SpR Club, March 2021) in which only 24% (19/78) expressed a preference to continue with exclusive face-to-face events.
Career plans
The pandemic affected career plans for 22% (72/321) of respondents. More than 50% of participants want to retire early (Fisher's exact test, P <0.001), but numbers considering leaving nephrology did not change (Table 4). Full-time workers, those closer to retirement, doctors and nurses and those with long COVID were more likely to want to retire early (Table 5).
Table 4.
Factors associated with contemplating changing career changes
| Pre-pandemic | Post-pandemic | ||||
|---|---|---|---|---|---|
| Had you considered: | Yes | No | Yes | No | P-value |
| Leaving healthcare | 53 | 249 | 66 | 236 | 0.22 |
| Retraining | 34 | 265 | 42 | 255 | 0.33 |
| Undertaking research | 105 | 193 | 95 | 202 | 0.44 |
| Undertaking an academic qualification | 102 | 197 | 94 | 203 | 0.54 |
| Retiring early | 77 | 227 | 121 | 188 | <0.001* |
Statistical analyses are performed using the two-tailed Fisher's exact test.
*P < 0.05
Table 5.
Factors associated with contemplating retiring early
| Pre-pandemic | Post-pandemic | ||||
|---|---|---|---|---|---|
| Retiring early | Yes | No | Yes | No | P-value |
| Gender | |||||
| Male | 22 | 53 | 35 | 41 | 0.04* |
| Female | 55 | 174 | 86 | 147 | 0.003* |
| Age (years) | |||||
| 25–34 | 9 | 33 | 14 | 29 | 0.33 |
| 35–44 | 13 | 69 | 20 | 63 | 0.24 |
| 45–54 | 33 | 73 | 49 | 57 | 0.03* |
| 55–64 | 22 | 49 | 37 | 36 | 0.02* |
| Working status | |||||
| Less than full time | 18 | 61 | 27 | 54 | 0.16 |
| Full time | 59 | 162 | 94 | 130 | 0.001* |
| Occupation | |||||
| Doctor | 34 | 78 | 59 | 55 | 0.001* |
| Nurse | 24 | 80 | 39 | 67 | 0.04* |
| Other | 15 | 60 | 19 | 57 | 0.56 |
| Ethnicity | |||||
| White | 60 | 190 | 96 | 155 | <0.001* |
| Non-White | 16 | 34 | 23 | 30 | 0.31 |
| Long COVID | |||||
| Yes | 11 | 17 | 19 | 10 | 0.07 |
| No | 66 | 210 | 102 | 178 | 0.002* |
| Remote working | |||||
| Yes, all the time | 4 | 20 | 7 | 17 | 0.49 |
| Yes, sometimes | 48 | 111 | 74 | 87 | 0.004* |
| No | 25 | 92 | 40 | 80 | 0.04* |
| Burnout | |||||
| Yes | 51 | 125 | 78 | 99 | 0.004* |
| No | 26 | 102 | 43 | 89 | 0.03* |
Statistical analyses are performed using the two-tailed Fisher's exact test.
*P < 0.05
Thematic analysis
Free-text questions were completed by 64% (Supplementary Table S3). Thematic analysis identified four themes: support, working relationships, workload and impacts on care provision, and changes in working conditions (Table 6).
Table 6.
Thematic analysis of free-text responses
| Category | Sub-themes | Quote |
|---|---|---|
| Support received | Management support | ‘Our trust management have left us to it. Within the renal team, the support we have given and received from each other has been incredible, but the trust has supported the staff who have been burdened with dealing with Covid extremely badly.’ (Female, 35–44 years) |
| ‘Professionally we (our department) had to be more proactive in sourcing PPE and developing isolation and protocols—we good not rely on the machinery of the Trust which moved more slowly. However, the Trust were fantastic in ensuring that our vulnerable patients were vaccinated promptly.’ (Male, 55–64 years) | ||
| Training | ‘Training severely disrupted and little communication initially regarding going forward. This is a function of degree of knowledge about the disease and the impact of COVID on the population.’ (Male, 35–44 years) | |
| ‘Charities have had a reduction in funding available to support clinical academic career pathways which has altered the ability to apply and gain access to training programmes. Alongside this the nature of work during COVID has meant there has been less time to focus on your own personal and professional development.’ (Female, 25–34 years) | ||
| Expectations from managers | ‘Barely any emotional support from seniors. Unreal expectations of performance in extremely stressful circumstances. GMC as per usual absolutely useless—a dire institution.’ (Male, 25–34 y) | |
| ‘Overall yes—although during times when my child's nursery was shut I was expected to look after him and work from home. This was an extremely difficult and stressful time as I felt like I was unable to perform either task adequately.’ (Female, 35–44 years) | ||
| Working relationships with colleagues | Teamwork | ‘Strong feeling of camaraderie in 1st wave replaced by exhaustion as the pandemic continued with having to cover for sick or shielding staff and extra clinical duties.’ (Male, 55–64 years) |
| ‘More remote working makes the team more distant, and communication can suffer. Also, close teams provide support and good moral, this has been more difficult. Covering people who have to isolate can be tiring and stressful.’ (Female, 45–54 years) | ||
| Feeling of ‘tiredness’ | ‘We are all tired and need a break but we keep going!’ (Female, 45–54 years) | |
| ‘Not so much during the first wave but I think definitely by the later waves people were beginning to get tired and becoming shorter with each other—especially without the ability to unwind in our usual ways when on annual leave or away from work.’ (Female, 25–34 years) | ||
| ‘Tiredness, some staff refusing to care for suspected or confirmed infected patients.’ (Male, 45–54 years) | ||
| Workload and ability to deliver timely and effective care to patients | Staff shortage | ‘1st wave—I was redeployed to the acute dialysis team. With 2 staff also not present due to non-covid sickness and 1 shielding, the team was severely short-handed. Quality of care suffered. This did not occur in following waves as there was no redeployed staff or shielding.’ (Male, 35–44 years) |
| ‘We have not been able to order our usual cleaning products for the unit. We have struggled with staffing levels due to colleagues shielding, plus increased workload with additional testing of patients and COVID restrictions. We have relied a lot on bank staff, however, have been running some shifts with less staff than usual.’ (Female, 35–44 years) | ||
| ‘Not enough staff or time to cover all covid policies throughout the pandemic, especially when we have had our own staff off sick covid related.’ (Female, 45–54 years) | ||
| Lack of face-to-face outpatient activity | ‘Difficult to get face to face appointments. Specialist nurses unable to see patients and reduced in numbers leading to poor patient preparation for dialysis.’ (Female, 35–44 years) | |
| ‘Less patients in clinic due to social distancing means longer waits for clinic appointments’ (Male, 44–54 years) | ||
| ‘In some gen neph clinics especially difficult to have appropriate discussions on the phone and assess complications appropriately.’ (Female, 25–34 years) | ||
| Working patterns and conditions | Flexibility/remote working | ‘Some working from home is good as there are (generally!) less interruptions and the lack of commute makes it less tiring. However, working from home has an impact on the team atmosphere in the workplace which is detrimental. I think it is only because we were such a strong team before the pandemic that this hasn't destroyed us!’ (Female, 35–44 years) |
| ‘Huge numbers of MS teams meetings which can be easily set up (as you don't need a room)—these impact massively on availability of non-structured time’ (Female, 45–54 years) | ||
| ‘There is some merit to virtual working—not every patient needs to attend clinics and if the infrastructure is in place to get tests, blood organised in advance its more efficient. Less hassle for patients than attending in person and greener nephrology! Zoom access to meetings/didactic teaching/conferences is also very efficient and easier to access.’ (Male, 55–64 years) | ||
| ‘Clinicians working from home—doctoring cannot be done remotely unfortunately. Now only consultants are allowed to work from home. This means more responsibilities are shifted towards more junior grade doctors. 2. Low threshold for absence from home…’ (Male, 35–44 years) | ||
| Face masks and personal protective equipment | ‘Wearing masks, some patients are unable to hear and lip read. Unable to give patients a reassuring smile.’ (Female, 25–34 years) | |
| ‘Wearing masks and visors—frightening and impersonal for patients, restricts communication, uncomfortable…’ (Female, 35–44 years) | ||
| ‘Mask wearing. It is a barrier to communication, even more so in the hard of hearing.’ (Male, 55–64 years) |
Support received
Support at a departmental level was considered positive, but perception of support from higher level management was negative. Trainees highlighted the lack of support for professional development. Managers were perceived to have high expectations, with little empathy for strain on personal lives.
Working relationships
Camaraderie reported early in the pandemic decreased over time, due to persistently tiring working conditions. Fatigue is a persistent theme; staff shortages were seen as a leading cause of tension among staff.
Workload and impacts on care provision
Understaffing due to isolation and sick leave leads to increased workloads for those on front-line duty. Reducing outpatient clinical activity was also considered a risk to the adequacy of patient care.
Changes in working patterns and conditions
While remote working was considered positive for flexibility and in some cases patient care, there is a growing urge to return to face-to-face interactions where needed. Hybrid forms of work were proposed. While the initial concern regarding personal protective equipment was a lack of provisions, concerns are now the physical barriers they present to interacting with patients.
DISCUSSION
We report the impact of the COVID-19 pandemic on the UK nephrology workforce. We found persisting burnout, a presence of long COVID—particularly among non-White HCPs—and a higher proportion of staff intending to retire early. Reassuringly, we also report high vaccine uptake and describe positive experiences with remote and flexible working.
Following the UK's first COVID-19 wave, 54% of the nephrology workforce had evidence of burnout [1]. This issue persists a year later as measured by the MBI score [5, 11–19]. This rate (57%) is higher compared with before the pandemic (∼35%) [20–25]. HCP burnout is dangerous. It associates with stress [26], suicidal ideation [18, 27], motor vehicle accidents [28], decreased productivity [29, 30], decreased empathy [15], increased medical errors [15, 17, 28], suboptimal care [19, 31–33] and increased costs [34, 35]. This finding is a critical issue that needs addressing.
Burnout in the context of this pandemic is multifactorial. Burnout associates with fatigue and workload, particularly when working longer and out-of-hours [11, 36]. Nearly 12 months on from our initial work, working pattern alterations remain common; 59% of those in adapted roles continue to work longer shifts with more out-of-hour shifts compared with pre-pandemic, with associated fatigue. We also report 517 episodes of staff self-isolation among 411 respondents, which may have contributed to increased workloads.
As Sever et al. [37] explore in their review of burnout among nephrology personnel during mass disasters, HCPs had to manage multiple roles during this pandemic, beyond that of their professions. This ranged from being parents and caregivers themselves, to being patients affected or recovering from COVID-19. Indeed, we found a high prevalence of long COVID in our workforce. Long COVID refers to a constellation of symptoms that persist following the resolution of acute COVID-19 [38, 39]. Of our respondents, 29% contracted COVID-19, with 36% describing persistent symptoms consistent with long COVID. This proportion is higher than that reported in the general population [40–42]. Free-text comments highlighted the negative impacts of long COVID on personal and professional lives, which are similar to those reported by HCPs in other settings [43]. Crucially, those with long COVID were 10 times more likely to experience burnout. Although pathways for managing long COVID are beginning to emerge [43], institutional support for HCPs with long COVID is needed to prevent workforce attrition.
Distinct groups within the workforce are more at risk of contracting COVID-19 and developing long COVID. We found those <55 years of age, doctors and nurses and males were all at least twice as likely to have had COVID-19, while respondents of non-White ethnicity were more than twice as likely to have had long COVID. An association between ethnicity and long COVID among HCPs has not been previously reported and we note that this finding is at odds with larger studies of the general population [39, 44, 45]. Recognizing the limited number of participants in our study, these findings need to be further investigated.
Despite these stark findings, we found a series of promising results. Most of our workforce had received both doses of a COVID-19 vaccine by May 2021. This should be reassuring to both patients and staff. Only 1.2% of respondents declined the vaccine for reasons other than pregnancy, citing lack of adequate data or a belief that the vaccination may not be needed following a COVID infection. At the time of the survey, guidance regarding vaccinations in those who are pregnant was ambiguous: this has since changed, underscoring the importance of the presentation of clear evidence about COVID-19 to HCPs to allow them to make informed decisions and counsel those around them.
We also found that a shift to remote working was well received. Remote working offers flexibility, affording an improved work–life balance [44, 45]. Staff who worked remotely felt their work was valued and experienced job satisfaction. Approximately 80% wanted to preserve an element of remote working. Although there is unlikely to be a ‘one-size-fits-all’ answer for managing burnout [13], remote working may prove an efficient solution in part, if feasible. Other solutions may include flexible working patterns, autonomy regarding job structure, protected time for personal and professional development and normalizing individualized burnout management plans [11, 46–48]. Support for those with long COVID is also critical and should complement interventions to promote well-being. Measures such as these will be imperative to preventing workforce attrition.
Our findings also highlight the need to ensure that sufficient measures are in place during times of prosperity to prevent burnout among staff during times of unprecedent disruption. This includes preparing staff to manage stress and workloads effectively, as well as organizational relief plans that could be implemented during periods of disruption. Such plans could involve periodically rotating staff from high-stress roles to low-stress roles, distributing the burden of excessive working during crises and designating supervisors with the specific role of monitoring staff for exhaustion and excessive workloads [37].
Our work has limitations. Data were self-reported and non-identifiable to preserve anonymity. This aimed to facilitate honest responses, but meant confirmatory cross-checks against national databases were not possible. It was also not possible to identify an appropriate denominator to calculate a response rate given the open methods by which the survey was distributed, which included social media platforms and regional distribution via HCPs. Our survey disproportionately represented the views of doctors, nurses, those of White ethnicity and those residing in England, and selection bias must be considered when interpreting findings. Further, there are limitations to the use of the MBI score when measuring burnout, including the inability to separate the influence of personal and work life on burnout, the quantitative nature of the tool that limited the ability to examine the narrative behind responses and a focus on negative rather than positive emotions [49]. Finally, our sample size limited our ability to probe for deeper associations and adjust our models for further covariates.
Our work highlights a concerning, persisting issue of staff burnout following the COVID-19 pandemic and a prevalence of long COVID directly impacting the working lives of those in the UK nephrology workforce. Our findings are likely translatable to other healthcare workforces who have had to adapt their service provision in response to the pandemic. These findings suggest a risk of workforce attrition that requires addressing at an institutional level. We celebrate the comradery our colleagues felt despite the challenging months that have passed and encourage the implementation of programmes to continue to foster this positivity, support those in the workforce with long COVID and encourage job plans and patterns that are sustainable.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank all survey respondents.
Contributor Information
Haresh Selvaskandan, John Walls Renal Unit, University Hospitals of Leicester NHS Trust, Leicester, UK; Department of Cardiovascular Sciences, University of Leicester, Leicester, UK.
Ailish Nimmo, Renal Department, Southmead Hospital, Bristol, UK.
Manuela Savino, UK Renal Registry, Renal Association, Bristol, UK.
Sarah Afuwape, Kidney and Urology Department, Royal Free London NHS Foundation Trust, London, UK.
Sarah Brand, Department of Renal Medicine, Nottingham University Hospitals NHS Trust, Nottingham, UK.
Matthew Graham-Brown, John Walls Renal Unit, University Hospitals of Leicester NHS Trust, Leicester, UK; Department of Cardiovascular Sciences, University of Leicester, Leicester, UK.
James Medcalf, John Walls Renal Unit, University Hospitals of Leicester NHS Trust, Leicester, UK; Department of Cardiovascular Sciences, University of Leicester, Leicester, UK; UK Renal Registry, Renal Association, Bristol, UK.
Paul Cockwell, Department of Renal Medicine, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Hannah Beckwith, Institute of Clinical Sciences, Imperial College London, London, UK; Imperial College Renal and Transplant Centre, Imperial College Healthcare NHS Trust, Hammersmith Hospital, London, UK.
FUNDING
Licences for use of the MBI proprietary questions were purchased from mindgarden.com with research funds provided by the UK Kidney Association.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the design of the survey. Survey analysis was performed by H.S., A.N., M.S. and H.B. All authors contributed to manuscript preparation.
CONFLICT OF INTEREST STATEMENT
P.C. has received grants from Kidney Research UK and the National Institute of Health Research and personal fees from Gilead, Napp Pharmaceuticals and Janssen Pharmaceuticals, all outside the submitted work. M.G.B. has received grants from Kidney Research UK and the British Heart Foundation and speaker honoraria from Napp Pharmaceuticals outside the submitted work. H.B., A.N., M.S., H.S., S.A., S.B. and J.M. report no conflicts of interest.
REFERENCES
- 1. Beckwith H, Nimmo A, Savino Met al. Impact of the COVID-19 pandemic on training, morale and well-being among the UK renal workforce. Kidney Int Rep 2021; 6: 1433–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. UK Kidney Association. Who we are . https://ukkidney.org/about-us/who-we-are (31 December 2021, date last accessed) [Google Scholar]
- 3. List of Ethnic Groups . https://www.ethnicity-facts-figures.service.gov.uk/style-guide/ethnic-groups#list-of-ethnic-groups (31 December 2021, date last accessed) [Google Scholar]
- 4. Training Deaneries in the UK . https://specialtytraining.hee.nhs.uk/portals/1/Content/Resource%20Bank/Inter-Deanery%20Transfer/UK%20Training%20Region%20Websites.pdf [Google Scholar]
- 5. Maslach C, Jackson S, Leiter M. The Maslach Burnout Inventory manual. In: Zalaquett CP, Wood RJ, eds. Evaluating Stress: A Book of Resources. New York: Scarecrow Press, 1997: 191–218 [Google Scholar]
- 6. Rotenstein LS, Torre M, Ramos MAet al. Prevalence of burnout among physicians: a systematic review. JAMA 2018; 320: 1131–1150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clarke V, Braun V.. Teaching thematic analysis: overcoming challenges and developing strategies for effective learning. Psychologist 2013; 26: 120–123 [Google Scholar]
- 8. Ryan GW, Bernard HR. Techniques to identify themes. Field Methods 2003; 15: 85–109 [Google Scholar]
- 9. Coronavirus cases . https://coronavirus.data.gov.uk (31 December 2021, date last accessed) [Google Scholar]
- 10. ONS . Office for national statistics: an analysis of published data on the waves and lags of coronavirus (COVID-19) from the coronavirus (COVID-19) infection survey, the Scientific Advisory Group for Emergencies (SAGE) and Public Health England (PHE). This analysis has been produced in partnership with University of Oxford [Google Scholar]
- 11. West CP, Dyrbye LN, Shanafelt TD.. Physician burnout: contributors, consequences and solutions. J Intern Med 2018; 283: 516–529 [DOI] [PubMed] [Google Scholar]
- 12. Panagopoulou E, Montgomery A, Benos A.. Burnout in internal medicine physicians: differences between residents and specialists. Eur J Intern Med 2006; 17: 195–200 [DOI] [PubMed] [Google Scholar]
- 13. Shanafelt TD, Boone S, Tan Let al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012; 172: 1377–1385 [DOI] [PubMed] [Google Scholar]
- 14. Shanafelt TD, Hasan O, Dyrbye LNet al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90: 1600–1613 [DOI] [PubMed] [Google Scholar]
- 15. West CP, Huschka MM, Novotny PJet al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA 2006; 296: 1071–1078 [DOI] [PubMed] [Google Scholar]
- 16. West CP, Tan AD, Habermann TMet al. Association of resident fatigue and distress with perceived medical errors. JAMA 2009; 302: 1294–1300 [DOI] [PubMed] [Google Scholar]
- 17. Shanafelt TD, Balch CM, Bechamps Get al. Burnout and medical errors among American surgeons. Ann Surg 2010; 251: 995–1000 [DOI] [PubMed] [Google Scholar]
- 18. Shanafelt TD, Balch CM, Dyrbye Let al. Special report: suicidal ideation among American surgeons. Arch Surg 2011; 146: 54–62 [DOI] [PubMed] [Google Scholar]
- 19. Shanafelt TD, Bradley KA, Wipf JEet al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002; 136: 358–367 [DOI] [PubMed] [Google Scholar]
- 20. Khan A, Teoh KR, Islam Set al. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open 2018; 8: e018720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bourne T, Shah H, Falconieri Net al. Burnout, well-being and defensive medical practice among obstetricians and gynaecologists in the UK: cross-sectional survey study. BMJ Open 2019; 9: e030968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Balendran B, Bath MF, Awopetu AIet al. Burnout within UK surgical specialties: a systematic review. Ann R Coll Surg Engl 2021; 103: 464–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sharma A, Sharp DM, Walker LGet al. Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology 2008; 17: 570–576 [DOI] [PubMed] [Google Scholar]
- 24. Ross J, Jones J, Callaghan Pet al. A survey of stress, job satisfaction and burnout among haemodialysis staff. J Ren Care 2009; 35: 127–133 [DOI] [PubMed] [Google Scholar]
- 25. Ong J, Swift C, Ong Set al. Burnout in gastroenterology registrars: a feasibility study conducted in the East of England using a 31-item questionnaire. BMJ Open Gastroenterol 2020; 7: e000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lloyd C, King R, Chenoweth L.. Social work, stress and burnout: a review. J Ment Health 2002; 11: 255–265 [Google Scholar]
- 27. Dyrbye LN, Thomas MR, Massie FSet al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 2008; 149: 334–341 [DOI] [PubMed] [Google Scholar]
- 28. West CP, Tan AD, Shanafelt TD.. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc 2012; 87: 1138–1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shanafelt TD, Mungo M, Schmitgen Jet al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc 2016; 91: 422–431 [DOI] [PubMed] [Google Scholar]
- 30. Dewa CS, Loong D, Bonato Set al. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res 2014; 14: 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dewa CS, Loong D, Bonato Set al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open 2017; 7: e015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hall LH, Johnson J, Watt Iet al. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One 2016; 11: e0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Halbesleben JRB, Rathert C.. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev 2008; 33: 29–39 [DOI] [PubMed] [Google Scholar]
- 34. Han S, Shanafelt TD, Sinsky CAet al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med 2019; 170: 784–790 [DOI] [PubMed] [Google Scholar]
- 35. Dewa CS, Jacobs P, Thanh NXet al. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res 2014; 14: 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hu N, Chen J, Cheng T.. The associations between long working hours, physical inactivity, and burnout. J Occup Environ Med 2016; 58: 514–518 [DOI] [PubMed] [Google Scholar]
- 37. Sever MS, Ortiz A, Maggiore Uet al. Mass disasters and burnout in nephrology personnel: from earthquakes and hurricanes to COVID-19 pandemic. Clin J Am Soc Nephrol 2021; 16: 829–837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Proal AD, VanElzakker MB.. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front Microbiol 2021; 12: 698169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Garg M, Maralakunte M, Garg Set al. The conundrum of ‘long-COVID-19’: a narrative review. Int J Gen Med 2021; 14: 2491–2506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Whitaker M, Elliot J, Chadeau-Hyam Met al. Persistent symptoms following SARS-CoV-2 infection in a random community sample of 508,707 people. medRxiv 2021; doi: 10.1101/2021.06.28.21259452. [DOI] [Google Scholar]
- 41. O'Dowd A. Covid-19: third of people infected have long term symptoms. BMJ 2021; 373: n1626. [DOI] [PubMed] [Google Scholar]
- 42. Sudre CH, Murray B, Varsavsky Tet al. Attributes and predictors of long COVID. Nat Med 2021; 27: 626–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ladds E, Rushforth A, Wieringa Set al. Developing services for long COVID: lessons from a study of wounded healers. Clin Med 2021; 21: 59–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Felstead A, Henseke G.. Assessing the growth of remote working and its consequences for effort, well-being and work-life balance. New Technol Work Employ 2017; 32: 195–212 [Google Scholar]
- 45. Como R, Hambley L, Domene J. An exploration of work-life wellness and remote work during and beyond COVID-19. Can J Career Dev 2021; 20: 46 [Google Scholar]
- 46. Regehr C, Glancy D, Pitts Aet al. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis 2014; 202: 353–359 [DOI] [PubMed] [Google Scholar]
- 47. West CP, Dyrbye LN, Erwin PJet al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016; 388: 2272–2281 [DOI] [PubMed] [Google Scholar]
- 48. Panagioti M, Panagopoulou E, Bower Pet al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017; 177: 195–205 [DOI] [PubMed] [Google Scholar]
- 49. Brindley PG, Olusanya S, Wong Aet al. Psychological ‘burnout’ in healthcare professionals: updating our understanding, and not making it worse. J Intensive Care Soc 2019; 20: 358–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.