ABSTRACT
Food systems are at the center of a brewing storm consisting of a rapidly changing climate, rising hunger and malnutrition, and significant social inequities. At the same time, there are vast opportunities to ensure that food systems produce healthy and safe food in equitable ways that promote environmental sustainability, especially if the world can come together at the UN Food Systems Summit in late 2021 and make strong and binding commitments toward food system transformation. The NIH-funded Nutrition Obesity Research Center at Harvard and the Harvard Medical School Division of Nutrition held their 22nd annual Harvard Nutrition Obesity Symposium entitled “Global Food Systems and Sustainable Nutrition in the 21st Century” in June 2021. This article presents a synthesis of this symposium and highlights the importance of food systems to addressing the burden of malnutrition and noncommunicable diseases, climate change, and the related economic and social inequities. Transformation of food systems is possible, and the nutrition and health communities have a significant role to play in this transformative process.
Keywords: food systems, transformation, sustainable diets, affordable diet, inequity, food environments, food governance, double burden of malnutrition, stunting, obesity
Why Food Systems?
Global food systems are at a pivotal turning point, and there is increased attention to transforming food systems so that they benefit nature, ensure healthy and safe diets, provide fair wages and livelihoods, and are prosperous (1–5). In late 2021, the world will come together to discuss and commit to this transformation at the UN Food Systems Summit (UNFSS).
Historically, there have been many calls, summits, and goal-setting exercises to address hunger and malnutrition through food policy and dialog (6, 7). Nevertheless, malnutrition and hunger remain unacceptably high in many parts of the world, with every country affected by some form of malnutrition (8). This year, 2021, is no exception. The UNFSS will focus its efforts to ensure that firm commitments are made by nation-states, donors, and private-sector actors to improve food systems amid increasingly alarming climate change, growing inequities, and a global pandemic. The clarion call leading up to the UNFSS is for food systems to become more sustainable while providing better nutrition and health outcomes (9). The Committee on World Food Security (CFS) Voluntary Guidelines on Food Systems and Nutrition define sustainable food systems as, “food systems that enable food safety, food security and nutrition for current and future generations in accordance with the three dimensions (economic, social and environmental) of sustainable development. In addition, sustainable food systems must be inclusive, equitable, and resilient” (10).
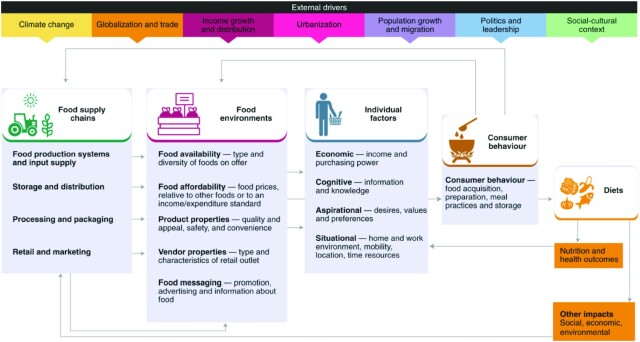
Food systems encompass everything from food production (and the ecological systems that underlie it) to the processing, packaging, distribution, retail, and consumption of foods, with many critical outcomes vital to sustainable development. Such outcomes include providing diets for nutrition, supporting livelihoods, and contributing to environmental and social benefits (Figure 1) (11). Many components of food supply chains and food environments influence food systems’ functionality, efficiency, and their relations with other health, education, and economic systems (12). Food systems are complex. They have many moving parts where diverse actors pull various levers and push food systems in different directions (13).
FIGURE 1.
Food Systems Framework. Source: Fanzo et al. (162).
Food systems affect everyone, in that they involve ∼1.5 billion producers (with one-third being smallholder farmers managing <2 hectares of land) that feed almost 8 billion people (14). Although the number of producers is significant, there is increasingly a smaller number of actors and organizations that control the inputs to produce food (e.g., seeds, chemicals, animal breeds) and the trading, processing, packaging, distributing, and selling of food (15).
Food systems are critical to the types of foods that are available and accessible to consumers. They are the backbone of global diets and have become more connected, globalized, and efficient at moving a diversity of food worldwide. Although food systems have reaped many benefits for society, there are alarming trends that are affecting human health and the environment. As diets have become more diverse in terms of foods offered, a healthy diet remains unaffordable for many individuals (16). The composition of diets has also become increasingly made up of highly processed, packaged foods that consist of added sugars, high amounts of sodium, and unhealthy fats and chemical additives that are detrimental to human health (17–21). The quality of the world's diets influences health outcomes: the Global Burden of Disease identifies the makeup of diets as a significant risk factor for mortality and morbidity, with 11 million deaths and 255 million disability-adjusted life years attributable to dietary risk factors including high intake of sodium and low intake of whole grains and fruits (22). Diets—and the operationalization of food systems—also contribute to significant environmental degradation and climate change (1, 4, 23, 24). Demand for animal-source foods is also increasing, particularly in emerging economies, which entails risks for the environment, including biodiversity loss, deforestation, and nutrient runoff into waterways, as well as animal welfare concerns (25, 26).
Over the past decades, there have been improvements in overall human longevity as well as substantial reductions in poverty but, especially in this era of the pandemic, there is also increasing disparity in health and economic status. Many people are still being left behind—many of whom are growing our food. Many working in food systems cannot afford a healthy diet and are left vulnerable to climate change and will continue to be at risk (16, 27–30). The prevalence of malnutrition has also not declined fast enough and, in many pockets of the planet, undernutrition, overweight, and diet-related noncommunicable diseases (NCDs), such as cardiovascular disease, diabetes, and hypertension, are worsening (8, 31–34).
Considering these challenges, the Nutrition Obesity Research Center at Harvard and the Harvard Medical School Division of Nutrition held their 22nd annual Harvard Nutrition Obesity Symposium entitled “Global Food Systems and Sustainable Nutrition in the 21st Century” in June 2021. This article brings together the speakers from the Symposium and presents a synthesis and summary of 3 of the world's biggest problems in the 21st century: the burden of malnutrition and NCDs, the consequences of climate change, and the massive economic and social inequities within and among nations. All 3 are directly related to sustainable food systems that are shared collectively and globally.
What Is Inhibiting Improvements in Nutrition and Diets from a Food System Perspective?
Several key food system issues are stymieing progress to improve diets and nutrition for many populations. Although the multiple forms of malnutrition are universal and significant, systemic inequities across food systems and overall societal structures influence who has access to healthy diets and who is at risk of foodborne illnesses and zoonotic diseases.
The multiple forms of malnutrition are worsening
Malnutrition encompasses undernutrition, including childhood stunting, wasting, and micronutrient deficiencies; overweight and obesity; and diet-related NCDs. Many countries have undergone what has been called the “nutrition transition” over the past 30 y, in which countries that have become more industrialized and urbanized shift away from traditional diets to diets high in fats, sodium, and sugar, and including more meat, and increasingly sedentary lifestyles (35, 36). This transition has resulted in populations struggling with the “double burden” of malnutrition (see below) (31).
There are some promising trends. There has been almost a 20% decline worldwide in the prevalence of stunting—or chronic undernutrition—since the 1990s (8, 37). However, in more recent years, progress has slowed in some countries. For example, India, where one-quarter of all malnourished children worldwide live, had the slowest rate of decline in stunting (only 1%/y) among emerging countries before the COVID-19 pandemic (38). According to India's 2019 National Family Health Survey, stunting was not on a downward trend and, instead, was increasing in several states, including Kerala, Gujarat, Maharashtra, and Goa (39).
The prevalence of wasting—or acute undernutrition—is much lower than stunting for children, although the number of children affected by wasting has remained essentially unchanged over the last decade (8). In Guatemala, for example, there is a high prevalence of stunting (47%) but a low prevalence of wasting (<1%) (8, 40) and increases in overweight in both children and adults have been noted. Thus, Guatemala is an example of a country undergoing a nutrition transition in that high consumption of highly processed foods and beverages has led to poor-quality diets (and shifts away from traditional diets), stagnation in the decline of stunting, and increasing burdens of obesity (41, 42).
Overweight and obesity have doubled since the 1980s and now exceed the proportion of the global population considered underweight as well as the proportion of adults who are of healthy weight (43–46). However, there are some regional differences in these trends. In many high-income countries, the Pacific Islands, and some regions of Latin and South America, North Africa, and the Middle East, the proportion of overweight and obesity actually exceeds those with a healthy BMI (45, 46). In East Africa and Southeast Asia, the proportion of overweight and obesity has risen but remains less than the proportion who are underweight (46, 47).
The global prevalence of the double burden of malnutrition—which is measured at the population level as having a prevalence of child wasting > 15%, child stunting > 30%, thinness in women > 20%, and adult overweight > 20%—has remained at ∼40% since the 1990s (31). However, there has been a regional shift. In the 1990s, the burden was mainly in the Middle East, North Africa, and Latin America, whereas in the 2010s, the prevalence declined in those regions but increased in South and South-East Asia. An increase in the prevalence of overweight drove the increases in the prevalence of the double burden in these regions (31). The reasons for the increased prevalence of the double burden and its shift to low- and middle-income countries (LMICs) are multifactorial; however, changing food systems, sedentary lifestyles, economic growth, and globalization trends have led to nutrition transitions in almost every country (20, 21, 31).
What are the consequences of this double burden? Data suggest that children born to women with a low BMI are at an increased risk of developing cardiometabolic diseases as adults (48, 49). A recent study in Ethiopia showed that children exposed to famine early in life (including prenatally and before age 2 y) had an increased propensity of decreased adult height and increased waist-to-height ratio [a marker of abdominal obesity and increased risk of cardiometabolic disease (50)], further strengthening the evidence that nutritional life cycle contributes to the developmental origins of adult diseases (51).
The economic, food, education, and health systems disruptions resulting from the COVID-19 pandemic will continue to exacerbate all forms of malnutrition. Models suggest that by 2022, COVID-19-related disruptions in LMICs could result in an additional 9.3 million wasted children, 2.6 million stunted children, 2.1 million women with anemia, 2.1 million children born to women with a low BMI, and 168,000 additional child deaths (34). In addition, in the first year of the pandemic, the proportion of those living in LMICs who could not afford a healthy diet increased from 43% to 50% (52). Food systems have been affected by the pandemic on multiple levels. In almost every country worldwide, segments of the population have lost their jobs and are relying on food assistance to feed their families. There is also an increase in comfort food eating, including fried foods and sweets high in fat, sugar, and salt, as well as increases in alcohol consumption, which could contribute to malnutrition and diet-related diseases (53, 54).
To address the multiple forms of malnutrition, a multitude of actions across food systems must be taken that will be articulated throughout this article. Double-duty interventions and policies that are actions (e.g., exclusive breastfeeding in the first 6 mo of life) that could simultaneously reduce the risk or burden of undernutrition, overweight and obesity, and diet-related NCDs are critical (55). Some of these actions that signal food systems include reorienting agriculture policies toward producing more nutritious crops, and redesigning school meal programs (56).
Inequities exacerbate burdens of malnutrition and unhealthy diets
Socioeconomic inequities are associated with nutrition outcomes and are widening in some countries (8, 57, 58). However, there has been little focus on inequities beyond income levels, and attention should be broadened to include and examine social and economic differences related to gender, race, ethnicity, or disability (59, 60). Other inequities exist beyond who people are and where they live globally. For example, in countries and cities further along on the nutrition transition spectrum, multiple deprivations in people's living environments are also associated with poor nutrition outcomes such as obesity and diet-related NCDs. There are significant power differentials between sizable private-sector entities and consumers regarding unhealthy food marketing and policy shaped by corporate lobbying (61).
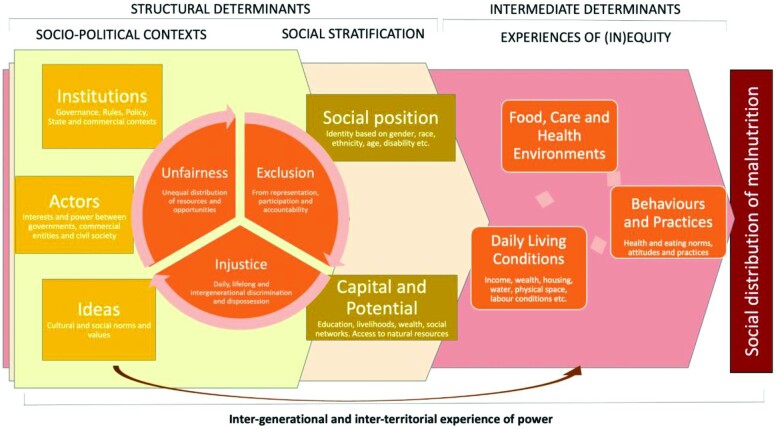
The UNICEF malnutrition framework and the WHO Commission on the Social Determinants of Health frameworks have mapped the causal factors that affect malnutrition when it is rooted in socioeconomic inequities (Figure 2) (8, 59). The immediate causes of inequities that affect nutrition are food, care, and health environments. These affect social conditions such as income, housing, water, behaviors, and practices—such as health and eating norms and attitudes. Underlying those immediate causes are structural causes and interactions such as social stratification (social positioning based on gender, race, ethnicity, age, or disability), capital, and potential. Finally, the sociopolitical context supports those structural causes and consists of institutions, actors, and ideas that influence the engine of inequity—what people experience daily and throughout their lives and across generations. These experiences perpetuate inequities such as the unequal distribution of resources and opportunities, exclusion from representation and participation, and ongoing social injustices that are both personal and geopolitical such as racism and colonialism.
FIGURE 2.
Inequities across nutrition. Source: Nisbett et al. (163).
Many factors lead to nutrition inequities. They include greater vulnerability to food shocks (i.e., loss of a crop or livestock due to an extreme event such as a climate disaster, pandemic, or conflict), discrimination in accessing health services or food safety nets/social assistance, and differential exposure to unhealthy food advertising faced by disadvantaged socioeconomic and ethnic groups (62, 63). Inequities also stem from fundamental social injustice which can take different forms in different countries: racism, casteism, patriarchy, and ableism. These forms often intersect and reinforce each other—limiting life opportunities (64) and access to essential goods, services, and education—and are associated with poor nutrition outcomes (65).
There are several recommendations to improve equity in nutrition and food systems. First, the people most affected by malnutrition and associated inequities must be involved in how food and health policies are formulated and enacted to ensure that rights, power, and sovereignty are prioritized. Second, food and nutrition actors must recognize and begin to understand some of the root causes of malnutrition (66), including some of the entrenched forms of discrimination that lie upstream from nutrition outcomes, and the power asymmetries that lie in deciding on nutrition policy, particularly that of the private sector (19). Finally, nutrition actors can support initiatives that strengthen the data used to measure and understand equity. For example, these data might incorporate determinants such as age, sex, ethnicity, education, wealth, disability, migration status, and geographic location into health, food, and nutrition surveys (8). However, given the nature of inequity, it also requires qualitative accounts of inequities at the community level to understand the root causes of malnutrition across multiple societal systems.
Healthy diets are not affordable for many people in the world
The real cost of acquiring enough nutrient-rich food to meet national dietary guidelines for a healthy diet exceeds the available income for ∼3 billion people (38% of the world's population) (Figure 3) (32). Market prices fluctuate over time and vary in space, but costs per unit of dietary energy are higher for fruits and vegetables, fish, eggs, dairy, nuts, and seeds than for cereal grains and other starchy staples, vegetable oils, and raw sugar. Even if one tries to eat the cheapest form of a nutrient-adequate diet, it is still more expensive than a diet made up mainly of starchy staples, oils, and sugar. This is because nutrient-rich foods are inherently more expensive because they are more difficult to grow, store, and transport than these shelf-stable, low-cost products. A balanced diet that meets food-based dietary guidelines calls for even larger quantities of these more costly food groups than would be needed just for nutrient adequacy, owing to their many functional attributes beyond just the essential nutrients that they contain.
FIGURE 3.
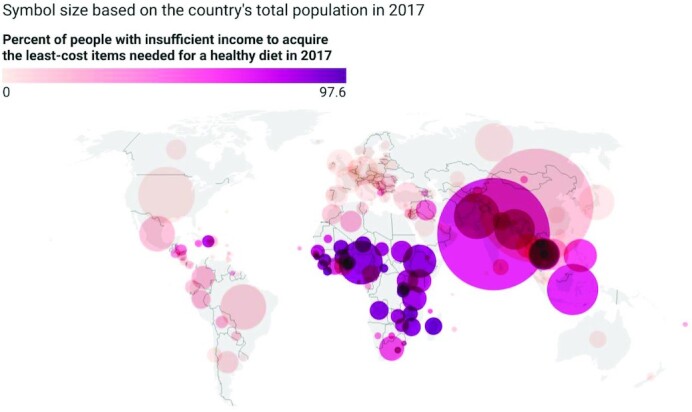
Global population unable to afford a healthy diet in 2017. Source: Herforth et al. (16). Map available online at: https://www.datawrapper.de/_/6LhIP.
The consistently high cost of nutrient-rich foods, combined with low and variable incomes around the world, ensures that making healthy diets affordable for all requires safety nets to supplement income when needed, and public investment to improve productivity and lower the real cost of production, storage, and distribution for popular, low-cost items in each food group. In addition, a wide range of supply chain innovations from the farm to the end-user can help reduce consumer costs while reducing the food system's environmental footprint by reducing the land, water, and energy needed per unit of the nutritious foods needed for a healthy diet (16).
Whereas ∼38% of the world's people have incomes too low to afford a healthy diet, the remaining majority could afford to do so but often consume fewer healthy items instead. Many factors drive food sales and purchases beyond the affordability of healthy foods in local markets. Even if consumers cared only about health, they would face a variety of constraints in meal preparation, including cooking time and other costs, as well as knowledge about and predictability of how much of each ingredient should be purchased and used for a low-cost healthy diet. In addition, people have many goals other than health when making food choices. Actual food consumption behavior is heavily influenced by other factors, including a person's biology of taste and satiation, family history and household circumstances, and food companies’ enormous advertising and marketing investments in the promotion of branded foods instead of generic items that come directly from farms (67). Affordability of low-cost healthy items is a necessary but far from sufficient condition for healthy diets to be consumed. As with transportation, housing, and other sectors of the economy, a wide range of policy interventions are needed to ensure that items being sold meet consumer needs safely, without causing harm to the purchaser or others.
Structural and systemic inequities paralyze progress
In addition to economic barriers, physical access to healthy foods can also significantly affect the ability to eat healthily. Food deserts—geographic areas that lack an adequate supply of affordable healthy foods, such as fresh fruit and vegetables—disproportionately affect low-income, nonwhite, and rural households in the United States (68). Despite local and federal efforts, such as the Healthy Food Financing Initiative (69), to address food deserts in the United States, the effects of the Great Recession exacerbated conditions for low-income households in the last decade (70). Food deserts are not unique to the United States and are prevalent worldwide (71, 72). Regardless of country or global region, food deserts are more likely to affect high-poverty communities.
People living in food deserts often face structural barriers that limit access to healthy diets: an overabundance of small food stores (i.e., convenience stores, dollar stores, and liquor stores), structural racism, and community violence. As a result, many low-income communities have excess unhealthy retailers. These retailers are often called food swamps—areas where unhealthy retailers are more abundant than healthy retailers (68, 73). However, low-income communities of color across the United States are taking steps to increase the healthfulness of their retail food environment, which include implementing novel policies that regulate the number of unhealthy retailers (74) and partnering with local growers to offer alternative options at farmers’ markets (75).
Structural racism describes systems and societal practices that oppress groups, given their race or ethnicity. This form of racism is difficult to document and measure because it is embedded in law, policy, and institutional culture. However, it is considered a root cause of racial health inequity (76) and contributes to disparities in healthy food availability. For example, redlining is an illegal and discriminatory practice of denying services (e.g., financial) to residents of certain areas based on race or ethnicity. Although it was banned in 1968 in the United States, it still takes place. Supermarket redlining occurs when a supermarket (often a national chain) closes a store in a minority community and relocates the store to a more affluent area. The closing is not prompted by economic duress or market competition but is instead driven by urban and logistical obstacles such as perceived crime, cultural biases, and profitability, often targeting minority, disadvantaged, and poor populations (77). Supermarket redlining can create food deserts and increase food insecurity rates in underserved communities (77).
Violence is widely considered a social determinant of health. Violence and threats to personal safety could be a potential deterrent to the access and purchase of healthy food options. The availability and density of certain food retailers such as liquor stores, convenience stores, fast-food restaurants, dollar stores, and supercenters (e.g., Wal-Mart) have been linked to higher violent crime rates in the United States (78). Violence may deter the retailer's customer base from patronizing the business and influence the owner's decision-making around store offerings and financial success (78). Overall, these examples demonstrate that structural barriers can increase inequities in nutrition and health.
Zoonotic and food safety risks are universal
Zoonoses—diseases transmitted from animals to humans—and foodborne illnesses are often ignored by the nutrition community, although they contribute significantly to the burden of disease. The increase in zoonoses can originate from environmental changes (e.g., climate change or pastureland change), human activity (e.g., increases in population density and pressure on landscapes), and animal ecosystem changes (e.g., mammalian biodiversity) (79). Of the 60% of human diseases shared with animals, 75% are zoonotic (80); about half of these are considered to be related to agriculture (81). There are 2 types of zoonotic diseases: neglected zoonoses (e.g., brucellosis, bovine tuberculosis, and leptospirosis) and emerging zoonoses [e.g., mad cow, bird flu, Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), and COVID-19 (SARS-CoV-2)]. Neglected zoonoses are well-controlled in wealthy countries because they can be easily prevented with financial inputs into interventions and surveillance. However, in low-income countries, they are widely prevalent and can lead to high morbidity and mortality. Emerging zoonoses are newly arrived diseases which can spill over from a reservoir species to multiple hosts, and (based on their level of transmissibility) have significant geographical spread. These zoonoses can have a large impact on high-income countries because of a lack of preparedness for such disease emergence. These diseases can be sporadic (e.g., rabies) or sustained (e.g., SARS-CoV-2).
The frequency of zoonosis emergence is accelerated by environmental change, including agricultural expansion, increasing human population and density, changing human behavior, and intensifying livestock production to meet the growing demand for meat products driving deforestation and increased contact between humans and animals (both wild and domesticated). This increasing contact between humans and animals creates opportunities for spillover events in which infectious diseases can transfer from one species to another.
There is also growing concern about food safety, and consumers will pay more to ensure their food is safe. Younger, wealthier, town-residing supermarket shoppers are willing to pay more for safety and will not eat food that is deemed unsafe (82). In the global South and indigenous contexts, food safety concerns may drive people away from domesticated meats and lead people to consume more wildlife because of the lack of a secure cold chain. Most years of life lost from foodborne disease come from pathogens, and >50% of those cases are from zoonotic sources (83, 84). Foodborne illnesses significantly influence individuals’ nutritional status (85–87). Diarrheal disease is a major risk factor for undernutrition, and poor nutritional status affects immunity and can predispose individuals to more severe and/or more frequent infectious diseases (88, 89). Accidental ingestion of fecal material from food exposed to unsafe water may cause foodborne illness and contribute to enteric dysfunction, reducing the absorption of critical nutrients (78, 79).
To remedy these threats, a One Health or planetary health approach is indicated, requiring collaborative, multisectoral, and transdisciplinary approaches—working at the local, regional, national, and global levels—to achieve optimal health outcomes recognizing the interconnection between people, animals, plants, and their shared environment (90, 91). This approach is critical to minimize the emergence of future zoonotic disease and food safety threats. The health of humans, animals, and the environment are interdependent and self-reinforcing. Although an important strategy, this approach has been less integrated into the field of nutrition.
What Is Inhibiting Food Systems and Nutrition from Being Sustainable from Climate and Ecological Perspectives?
Climate change will continue to alter the environmental conditions under which food systems operate, reducing food production (92). At the same time, food systems have consequences for climate change through greenhouse gas emissions associated with food production and transport and alteration of soil and surface properties (93). Food systems are also reliant on a range of environmental factors and ecosystem health. At the same time, current food system practices in some parts of the world are degrading natural resources and biodiversity at an alarming rate (92, 94). Agriculture uses 40% of arable land, 70% of freshwater resources, and contributes ≤30% of total greenhouse gas emissions (1, 4, 95). These emissions are wreaking havoc on the planet, particularly via global warming, rising sea levels, and climate-related natural disasters (92, 96). The impacts of climate change also bring inequities, with low-income regions and populations being more severely affected by climate change shocks, resulting in higher risk of food insecurity and decreased capacity to respond and adapt to climate change (97).
Climate change is affecting food systems and agricultural productivity
Relative to 2005 levels, global food demand is expected to grow by 50%–100% by 2050 owing to an increase in per capita consumption (98). However, historical food production yield trends have only partially covered increased demand, such that between 2002 and 2014, for example, 85% of global soybean production and 66% of global maize production increases were attributable to expansion of the harvested crop area (99). Another important consideration is that food prices have been higher and more volatile since 2000 (100), where price spikes are at least partly attributable to a short-term reduction in supply because of adverse weather events as well as policy responses such as trade caps and biofuel prioritization (63, 101). Increased food prices have also been accompanied by a reversal in decades of declines in undernutrition, with undernutrition prevalence increasing since 2015 in places such as India and Ethiopia (102, 103). Increased prices of certain foods such as animal source-foods including dairy are associated with childhood stunting in LMICs (104).
Even under stable environmental agricultural conditions, the ability to meet rising food demand and ensure consistent food security is questionable. In this context, the effects of climate change are a potentially destabilizing factor in ensuring sufficient food consistently as well as the nutritional quality of crops (105–107). The global temperature has warmed by ∼1°C over the last 50 y and 1.5°C over land (108). Under a high emissions scenario, the same increment of warming is expected in the next 30 y (109). The 2021 Inter-Governmental Panel on Climate Change Report showed that average global temperatures have now reached 1.1°C above the historical norm and under every future scenario modeled from optimal to worst case, the world will reach a global temperature rise of 1.5°C in the next 20 y. Precipitation and soil moisture patterns are also expected to change but, whereas warming is essentially global, changes in water availability will be regional (110). A warmer atmosphere holds more water vapor and, thus, can evaporate more when dry and rain more when wet, leading to enhanced extremes, and frequent droughts and floods that are already being experienced in different parts of the world. Furthermore, changes in atmospheric circulation patterns will change how moisture moves in and out of croplands.
The consequence of a warmer world with a changing hydrological cycle for food production will depend on a host of factors. In general, studies have found that higher temperatures are detrimental to crop yields (111, 112), raising concerns that climate change will suppress the growth in yields needed to meet rising demand. Of further concern is that this is coupled with a rapidly growing population, especially in sub-Saharan Africa. The implications of changes in hydrology are less well understood, with some studies suggesting low sensitivity to precipitation and others indicating that precipitation is a poor proxy for available water supply and that soil moisture is a first-order control on yields (113). Another important consideration is the ability to adapt agriculture to altered climates, including selecting cultivars, timing of planting, and water application or retention techniques (114). There is little margin between needs and supply of food for too much of the world, and it will be essential to develop better insights into how climate change will alter food production in the coming decades.
Climate change is affecting food security, diets, and nutrition outcomes
There are different ways to understand how climate will affect food security and nutrition outcomes by pulling together different data types at different scales, including individual nutrition information (115), rainfall (precipitation), temperature data (116), and regional livelihood zones (117). Observing climate change can be performed by measuring temperature, rainfall, and vegetation through remote sensing data and models (118, 119). Food security and nutrition outcomes can be measured by the Food Insecurity Experience Scale, food access, and anthropometric nutrition indicators (120).
A literature review of 90 studies assessed the relations between potential factors and significant indicators of child malnutrition of 107,000 children living in 19 LMICs across 6 global regions. The review determined that shocks—deviations in conditions compared with long-run average conditions due to variations in climate conditions (as measured by temperature and rainfall) and violent conflict—were consistent predictors of child malnutrition (121).
When examining the impact of precipitation and temperature extremes on children's diets in 19 countries, higher long-term temperatures were associated with lower dietary diversity, whereas higher rainfall than the long-term average was associated with higher dietary diversity (122). At the regional level, 5 of the 6 regions (Asia, Central America, North Africa, South America, Southeast Africa, and West Africa) examined had significant reductions in dietary diversity associated with higher temperatures. Conversely, 3 regions had significant increases in dietary diversity associated with higher precipitation. In some regions, the statistical effect of climate on dietary diversity was comparable with or greater than other factors such as increased access to education, improved water and toilets, and poverty reduction interventions (122).
A related study that examined 53 LMICs found that periods of minor to severe drought and severe wetness were correlated with lower height-for-age z scores (a measure of stunting) among children (123). In addition, a study found that increased temperatures and decreased precipitation was associated with low birth weight outcomes in newborns, and this relation was mediated by where a pregnant woman lived, and her income, education, and access to electricity (124). These studies show the importance of tracking and responding to climate extremes as they happen and the potential to move toward timely, targeted food security and nutrition interventions to limit malnutrition (121).
Food systems and diets are affecting climate change and environmental degradation
Many studies have demonstrated the impacts of climate change on food production, crop nutrient quality, food security, diet, and nutrition outcomes (93, 125, 126). At the same time, there is increasing concern about how food systems are affecting human health and planetary health. The EAT–Lancet Commission was charged with identifying a path to nourish a global population of 10 billion people by 2050 with a diet that is healthy and produced from sustainable food systems (1).
The EAT–Lancet Commission proceeded in 4 steps. It 1) defined a healthy reference diet using the best available evidence (controlled feeding studies, long-term cohort studies, and randomized trials) (127); 2) defined planetary boundaries (a set of earth system boundaries that, if transgressed, could be catastrophic for the planet and human populations) for 6 critical environmental systems and processes including greenhouse gases, cropland use, water use, nitrogen and phosphorus application, and species extinction rate (128); 3) applied a global food systems modeling framework to analyze what combinations of readily implementable measures are needed to stay within food production boundaries while still delivering healthy diets by 2050; and 4) outlined strategies to achieve the necessary changes to meet the goal of healthy diets from sustainable food systems.
Based on evidence for health outcomes, the reference diet has been described as a “flexitarian” diet because it is mainly plant-based, emphasizing whole grains, fruits, vegetables, nuts, soy, and other legumes. It also includes optional intakes of animal-source foods in modest quantities: ∼1 serving/d of dairy and 1 serving/d of poultry, fish, eggs, or red meat (with red meat at ∼1 serving/wk). The possible ranges include the option of a vegan diet. This flexitarian dietary pattern describes the traditional Mediterranean diet, which has well-documented health benefits and is compatible with traditional diets worldwide (129, 130).
Using 3 different modeling approaches to assess the health benefits of global adoption of the reference diet, each model predicted annual reductions of ∼11 million premature adult deaths averted from the consumption of the usual diet, or ∼19%–24% of all deaths. However, the Commission demonstrated that most of the world is quite far from consuming this diet, with some countries consuming high amounts of red and processed meats and others consuming excess intakes of starchy staples. In addition, most countries consume suboptimal amounts of fruits, vegetables, nuts, legumes, fish, and whole grains (Figure 4).
FIGURE 4.
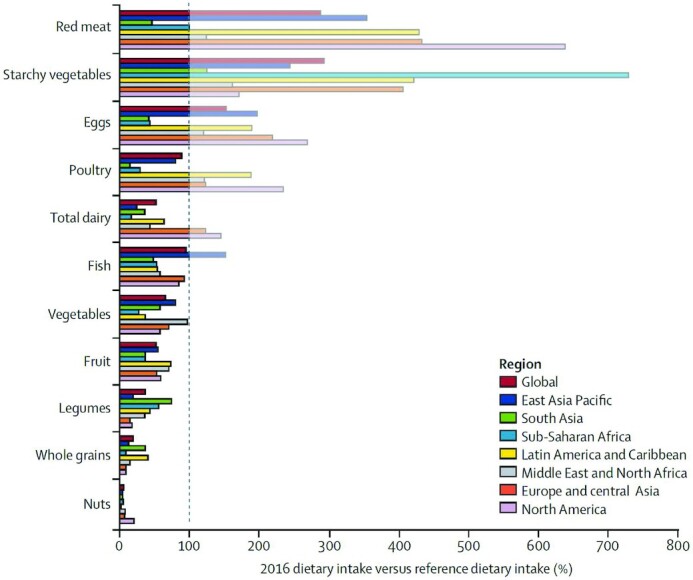
The dietary consumption of food groups regionally as compared to the EAT–Lancet reference diet. The graph shows the gap between global and regional dietary patterns in 2016 and reference diet intakes of food. The dotted line represents reference diet intakes. Data on 2016 intakes are from the Global Burden of Disease database. Source: Willett et al. (1).
By incorporating data on projected increases in population growth and dietary trends, the world is on track to exceed environmental boundaries by 2050, including greenhouse gas emissions by 2-fold if food systems do not change. However, we could stay within planetary environmental boundaries for food production by adopting the dietary reference targets, reducing food loss and waste, and improving agricultural methods using more sustainable practices (21). These changes are required to meet the Paris Climate Agreement targets (131).
Multiple actions by governments and the private sector will be needed. For example, both hard regulations (e.g., high-carbon food or soda tax; restricting marketing of unhealthy foods) and soft behavior change nudges (e.g., changes to the choice architecture of retail outlets) should be considered by governments. In addition, many food environments can be redesigned by changing the choice architecture to make changes more manageable and accessible at workplaces, schools, and hospitals. However, any nudge or behavior change may have trade-offs and not achieve positive outcomes across every spectrum of health, the environment, the social, or the economic. What is critical is that the collective aggregate of these changes result in positive outcomes. It should also be noted that some individuals and some countries need to make more significant changes toward human and planetary health than others (132). The conference did not deeply delve into behavior change and the “demand” side of food systems and there is a need for more research and focus on behavior economics related to food system transformation (4).
The cost of meeting the EAT–Lancet dietary targets will vary among countries, but the average cost is not significantly different from meeting current national dietary guidelines. In other words, consuming a sustainable diet does not add to the cost of a healthy diet because the lowest-cost items for healthy and sustainable diets include relatively few animal-source foods (16). Unsustainable and unhealthy choices can be driven by factors other than prices, such as cultural and social norms and aggressive marketing by corporations (67).
The EAT–Lancet Commission report was important in that it established global targets that governments could consider when taking action to improve food systems for both human and planetary health. The report was limited on recommendations for individuals, and specificities of local action and context, but the goal of the report was to recommend grand-scale changes that must take place over the next decade amid a rapidly changing climate.
How to Move toward Sustainable Food System Transformation?
Moving toward food system transformation
How should food systems be transformed, and can these changes be completed in the near term? In the process leading up to the UNFSS, many involved have championed the idea that transformation must achieve appropriate levels of availability, access, and affordability to a sufficient, nutritious, desirable, and safe diet for everyone. At the same time, such diets should be produced from sustainable and resilient food systems that promote fair and equitable livelihoods and benefit nature in positive ways (9). There is no single solution to enable all nations and regions to achieve this transformation (5). What are required are end-to-end thinking and end-to-end action across the entirety of food systems. There is potential to manage this transformation through the coproduction of actors that are working on food systems. Coproduction is the collaboration of practice and research that could help reframe power, empower voices, give agency, and navigate differing world views and trade-offs (133).
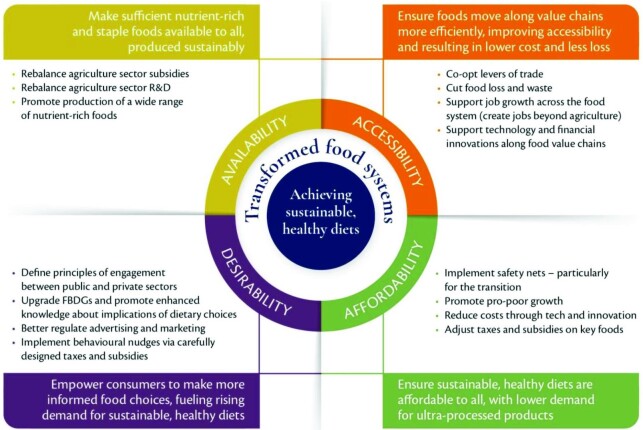
Figure 5 shows the significant areas of transformation necessary across food systems and the policy entry points to do so (2). The first domain is availability: ensuring nutrient-rich and staple foods are available for everyone and produced in sustainable ways. What is currently grown on the finite arable land around the world is a mismatch with what comprises an optimal diet. Of what is grown around the world, 36% of the calories produced go to feed animals, and only 12% of those calories contribute to the human diet (134). Models suggest that if the global population were to consume the WHO-recommended amount of 400 g of fruits and vegetables per capita per day, the world currently cannot now nor in the future provide that supply of fruits and vegetables in the global supply chain (135). There is a need to rebalance the agriculture sector's research and development toward healthy crops, repurpose the sector's subsidy policies toward nutrient-rich foods, scale-up incentives for nature-positive on-farm technologies, and focus on new job creation of nonfarm rural food services. International trade is also critical—without it, there would be an increase in micronutrient deficiencies such as iron, zinc, and folate worldwide (136). However, there is a trade-off to trade. Trade also moves unhealthy foods around the world (137, 138).
FIGURE 5.
Necessary food system transformations and policy entry points. Source: Glopan (2). FBDG, food-based dietary guideline; R&D, research and development.
The second area is to improve the accessibility of food for everyone no matter where they live and who they are. The more efficiently food moves along supply chains, accessibility is improved, costs are lowered, and food losses are lessened. Readily available technologies can reduce food loss and waste. Currently, ∼9%–20% of food is lost on farms and in movement along supply chains (139). In high-income countries and settings, most food is wasted or thrown out at retail outlets, restaurants, and homes (140, 141). In addition to bulk food wasted, 18%–41% of nutrients are lost when food is processed (142, 143). The amount of food loss and waste varies at different stages of the supply chains. Food losses occur mainly at the food transformation and packaging level in Africa, Central and Southeast Asia, and Latin America. In Europe, North America, and Oceania, most food is wasted at the consumer level (144).
The third area is affordability. As discussed earlier, healthy diets are unaffordable for almost half of the world, and that cost does not factor in environmental sustainability traits (16). The cost of a diet of minimum nutrient adequacy can be 200% of a household's food expenditure in countries like Niger or the Democratic Republic of the Congo (145). Ultra-processed foods—highly processed foods with high amounts of added sugars, sodium, and unhealthy fats—are readily available and traded, cheap, tasty, and have a long shelf-life (19). These foods are also associated with an increased risk of NCDs and weight gain (146–149).
The fourth area is desirability. There is a need to empower people to make choices that inform and empower them toward healthy, sustainable diets. Merely making foods available and affordable does not mean that people will choose them. Although there are significant social and cultural norms to acknowledge and build on, encouragement to shift dietary norms will have to come in many forms (150). The latter will include behavioral nudges based on changes in the relative price of different food categories, use of consumer price subsidies and taxes where appropriate, informational gains through front-of-package labeling, advertising of prohealth diets and sustainability rather than cheap empty calories, and more. In other words, the various domains of food systems must work together rather than in siloes, and the many instruments of policy and investment, retail, and marketing practices must be coherent and consistently pointing toward the common goals embedded in the transformation agenda.
Managing transformation
Food systems need to be better managed and governed to ensure that food system transformation is redesigned to improve nutrition and health, ensure environments are sustainable and resilient, promote fair and equitable livelihoods, and mitigate climate change (2, 151). The first step is to identify multiple wins across policy and investment decisions that strive for outcomes where no harm is done. One such example is the restoration of China's Loess Plateau that had benefits for poverty reduction, natural resource restoration, and more jobs (5). The second step is to make transparent, evidence-based policy decisions and investments that systematically analyze trade-offs and choices. The third step is to strengthen institutions and the capacity for implementing those relevant decisions. The fourth step is to establish feedback mechanisms by allowing for real-time adjustments to policy and process, unforeseen consequences, and changing circumstances. And the last step is to identify bundles of mechanisms for more coherent system-wide actions rather than minor changes at the margins (132).
At the country level, cross-ministerial working groups could identify ways to reconcile trade-offs across sectors, short- and long-term gains, and constituency impacts. Ministries of finance could revise calculations of national poverty lines to focus on the affordability of healthy diets to guide safety nets, minimum wages, and propoor growth policies. Subnational authorities and city leaders should explore vertical/horizontal coordinating mechanisms and ways to bring local voices to national prominence and translate national goals into local agency. Civil society should be fully engaged to build momentum across all stakeholders via constituent group dialogs, whereas business leaders and networks should commit to functional accountability mechanisms for private-sector activity across all food domains. Finally, national statistical agencies can set and support targets and metrics for food system–wide transformation.
Trade-offs (political, economic, societal) are inevitable and must be effectively managed. Examining trade-offs through coproduction as aforementioned or sustainability indexes to understand which drivers move food transformation in different directions could help navigate decisions to address those trade-offs (152, 153). Transformation requires coherent actions (policies, investments, engagement) across the whole food system. It requires country-level and global efforts framed by a vision of the destination and the path to get there. The current UNFSS process is the first time that efforts are being framed around a shared vision of food systems transformation at country and global levels. For food systems transformation, there is a need to address realities of sectoral and interest trade-offs and limits to policy development and analytical capacity in LMICs. The UNFSS could provide some of this support, but what happens at the country level will be critical. The roadmaps and food systems transformation pathways the countries have developed will need to be informed by a shared vision to align the actions of all food systems actors. Adequate resourcing and accountability mechanisms are also essential.
Connecting up systems
There is currently sufficient food available for everyone to be well-fed and well-nourished, yet we still have many people who suffer from hunger (32). This approach could be partly due to the systemic failure in how we grow, process, distribute, market, eat, and dispose of food, disregarding equity and meeting basic human needs (154). Key components of human health are underpinned by and dependent on the determinants of health, which depend on ecological and animal health. The degradation of the underlying ecological systems that support food production can lead to adverse nutritional outcomes, and it is critical to support the social-ecological systems of food production (155).
Several factors determine whether we experience good physical and mental health and well-being, such as safe food and water, culturally respectful and nutritious diets, empowerment, and integrated government action. Underpinning all of these is the other ecological and animal health systems that include connections to climate, soil quality, water quality, biodiversity, pollination, pests and diseases, nutrient cycling, and animal welfare. Taking a multisystems approach to policy and practice ensures these relations are not underestimated or separated.
Taking a business-unusual approach
The current industrialized food systems are premised on economies of scale that reduce prices, incentivize the externalization of costs, and create growth in consumption and demand. This vicious cycle—supply creating demand leading to intensification of supply—is a classic Jevons’ paradox (wherein a technological improvement in the processing of a resource leads to increased demand for this resource) and, in turn, creates a greater need for land and intensifies competition for water, energy, and inputs (156).
Greater focus should be on the efficiency of the overall food systems transformation rather than the primary focus being on the efficiency of agricultural productivity (157). The policy focus should be broadened to, “What should we grow, in what quantities, and how?” and away from simply, “How do we grow more?” For this to happen, there needs to be greater recognition of the values associated with food and the true cost of food instead of driving to minimize food prices and maximize consumption (158). Diets based on the principles of improved nutrition, in turn, could spur more diversified and circular agriculture systems, which improve the heterogeneity of production systems (and the environmental benefits this brings) and increase the sustainability of agriculture (157).
However, getting the incentives right is vital: encouraging healthy dietary patterns with less reliance on animal-source foods; reducing food waste; allowing land use to become more sustainable; and reducing future impacts from climate change and biodiversity loss. Reorienting incentives, in essence, can create virtuous and less vicious cycles—a business-unusual approach.
Changing social narratives
Social narratives are deeply embedded mental models that influence how we think and what we do. Transformational change in food systems will not occur without a shift of narrative, mindsets, assumptions, and, most importantly, an inspirational vision of what is possible. For example, today, 1 prevailing narrative underpins and enables the current industrial food system to focus solely on the quantity of food and calories produced and is based on assumptions that we need to maximize yields by “doubling food production by 2050” (159). Efforts to minimize the social, health, or ecological costs are considered but seen as less important than the goal of increasing food production to “feed the world” (7, 160, 161).
This narrative shapes how food is produced, harvested, processed, distributed, marketed, disposed of, and eaten. It influences research, investments, policy priorities, and practices across the food sector, from governments and research establishments to educational curricula, investors, and businesses. Table 1 highlights several more examples of how we need to shift the prevailing social narratives to new narratives.
TABLE 1.
Changing the prevailing social narratives1
| Prevailing narrative | New narrative |
|---|---|
| “We” feed the world, often driven by the Global North. | The world feeds itself: citizens and communities grow their foods with dignity, retaining rights to their products and access to markets. |
| Food is seen as a commodity. | Healthy and sustainable diets are seen as a public good with farmers, producers, citizens, and health care professionals supported and incentivized to promote health. In addition, local and regional food systems and resilience are prioritized. |
| Policy addresses hunger in isolation. | Hunger is addressed with a healthy, nutrient-dense diet–centered approach that addresses malnutrition in all its forms (hunger, obesity, micronutrient deficiencies). |
| Unhealthy, unsustainable, culturally inappropriate food choices are an unavoidable by-product of prevailing food environments, economics, and what people want to eat. | Food environments enable and motivate people to eat a diversity of foods in healthy proportions, sustainably, and in culturally respectful ways. |
| Systems and practices treat ill-health and take a curative approach to health care provisions on diet-related health problems. | Conditions promote good health and a preventative approach to health care provisions, and there is a focus on preventing diet-related diseases through healthier consumption patterns. |
| The responsibility falls on the individual, with little focus on addressing food environments and underlying determinants of health. | Focus is on health and sustainable diets as a public good, healthy food environments, and underlying determinants of health with all food systems actors striving to make a positive contribution. |
| Emphasis is on a global search for single solutions. | A diversity of contexts requires a diversity of solutions with multiple food systems entry points aligned by a shared food systems vision. |
| LMICs should not be burdened with climate mitigation when hunger is still a huge priority. | All countries must contribute to climate mitigation; otherwise, we will not meet the Paris targets, and climate change's devastation will make LMIC settings worse with a limited resource base for coping strategies. |
1LMIC, low- and middle-income country.
In the COVID-19 context, there is an urgent need for a new narrative and vision for global food systems. Equally at the heart of this vision is that all actors actively shape and contribute to healthy, equitable, renewable, resilient, just, inclusive, and culturally diverse food systems. It is not the privilege of any single stakeholder group to determine the future of food. Such a new narrative would enable and inspire diverse actors to identify and prioritize the policies, practices, and business models that align human, ecological, and animal health outcomes.
Conclusion
The 22nd annual Harvard Nutrition Obesity Symposium highlighted the importance of the nutrition and health communities in contributing to this transformative food systems agenda. Therefore, it will be necessary for these communities to engage in the UNFSS. The Summit aims to launch bold new actions to transform how the world produces and consumes food, delivering progress on all 17 Sustainable Development Goals as part of food system transformation. There are 5 main action tracks: 1) ensuring access to safe and nutritious food for all; 2) shifting to sustainable consumption patterns; 3) boosting nature-positive production; 4) advancing equitable livelihoods; and 5) building resilience to vulnerabilities, shocks, and stresses. The solutions derived from these action tracks and coalitions need to address the profound global and local problems linked to food systems, widespread poor diets, and different forms of malnutrition; the climate crisis and environmental degradation; and the challenges of inequities, safety, and sustainability of livelihoods.
The ambitious aims of these action tracks reflect the urgency needed by every actor who engages with food systems; however, the nutrition community has a leadership role to play (4). Now is the time for nutrition scientists to collaborate with other sectors, disciplines, and experts to make shifts in food systems and put them on a trajectory toward lasting sustainable development.
Acknowledgments
The authors’ responsibilities were as follows—JF and CR: wrote the paper; JF and SG: had primary responsibility for the final content; SG and IS: oversaw the organization of the meeting; IS: managed the content contributions from all authors; and all authors: read an earlier draft, suggested revisions, and read and approved the final manuscript. CDG is a science advisor for Oceana. SG has consulted for Viiv and Theratechnologies, and received support from Kowa Pharmaceuticals, Theratechnologies, Viiv, and Gilead, all unrelated to the present study. PH has served as a consultant to Mahi Pono Agriculture regarding impacts of climate on crop production. NN has received support from UK Research and Innovation, the International Food Policy Research Institute, and BMGF India. CR has consulted for Alcresta Pharmaceuticals. PW declares that he has no competing financial interests or personal relationships that could appear to have influenced the work reported in this article; he is a consultant technical adviser to the Global Panel on Agriculture and Food Systems for Nutrition. WCW has received research funding from GlaxoSmithKline. All other authors report no conflicts of interest.
Notes
MEB acknowledges that the work was a product of the Modelling Early Risk Indicators to Anticipate Malnutrition (MERIAM) project, funded by the UK Foreign, Commonwealth and Development Office via Strengthening Data for Nutrition Programme contract #7442; work was also supported by subcontracts from Action Against Hunger to the University of Maryland. CDG was supported by National Science Foundation grant CNH 1826668. WAM was supported by Bill & Melinda Gates Foundation and UKAid grant INV-016158 for the Food Prices for Nutrition project; US Agency for International Development (USAID) grant OAA-18-LA-00003, through the Feed the Future Policy Research Consortium; and USAID grant OAA-L-10-00006, through the Feed the Future Innovation Lab for Nutrition. DG was supported by Action Against Stunting Hub, funded by UK Research and Innovation through the Global Challenges Research Fund. PW was supported by USAID through Feed the Future Innovation Lab for Nutrition award AID-OAA-LA-14-00012, through the Friedman School of Nutrition Science and Policy at Tufts University. This symposium was a collaboration between the Nutrition Obesity Research Center at Harvard (NORC-H) through NIH grant P30 DK040561 (to SG) and the Division of Nutrition at Harvard Medical School. The symposium is available online at: http://healthcare.partners.org/streaming/Live/MGH/Endocrine/2021_NORCH_Global_Symposium.html.
CR and IS contributed equally to this work.
Abbreviations used: LMIC, low- and middle-income country; NCD, noncommunicable disease; UNFSS, UN Food Systems Summit.
Contributor Information
Jessica Fanzo, Nitze School of Advanced International Studies, Johns Hopkins University, Baltimore, MD, USA; Berman Institute of Bioethics, Johns Hopkins University, Baltimore, MD, USA; Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA.
Coral Rudie, Division of Gastroenterology, Hepatology and Nutrition, Boston Children's Hospital, Boston, MA, USA.
Iman Sigman, Metabolism Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA.
Steven Grinspoon, Metabolism Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA.
Tim G Benton, Energy, Environment and Resources Programme, Chatham House, London, United Kingdom.
Molly E Brown, Department of Geographical Sciences, University of Maryland College Park, College Park, MD, USA.
Namukolo Covic, International Food Policy Research Institute, Addis Ababa, Ethiopia.
Kathleen Fitch, Metabolism Unit, Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA.
Christopher D Golden, Department of Nutrition, Harvard TH Chan School of Public Health, Boston, MA, USA.
Delia Grace, Natural Resources Institute, University of Greenwich, Chatham Maritime, United Kingdom; Animal and Human Health, International Livestock Research Institute, Nairobi, Kenya.
Marie-France Hivert, Department of Population Medicine, Harvard Pilgrim Health Care Institute, Harvard Medical School, Boston, MA, USA.
Peter Huybers, Department of Earth and Planetary Sciences, Harvard University, Boston, MA, USA.
Lindsay M Jaacks, Global Academy of Agriculture and Food Security, The University of Edinburgh, Edinburgh, United Kingdom.
William A Masters, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA.
Nicholas Nisbett, Health and Nutrition Cluster, Institute of Development Studies, Falmer, United Kingdom.
Ruth A Richardson, Global Alliance for the Future of Food, Toronto, Ontario, Canada.
Chelsea R Singleton, Department of Social, Behavioral, and Population Sciences, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA.
Patrick Webb, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA.
Walter C Willett, Department of Epidemiology, Harvard TH Chan School of Public Health, Boston, MA, USA.
References
- 1. Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood A et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447–92. [DOI] [PubMed] [Google Scholar]
- 2. Global Panel on Agriculture and Food Systems for Nutrition (Glopan). Future food systems: for people, our planet, and prosperity. [Internet]. London, United Kingdom: Glopan; 2020. Available from: https://foresight.glopan.org/ (Accessed 2021 Aug 5). [Google Scholar]
- 3. Searchinger T, Waite R, Hanson C, Ranganathan J, Dumas P, Matthews E. Creating a sustainable food future: a menu of solutions to feed nearly 10 billion people by 2050. [Internet]. Washington (DC): World Resources Institute; 2019. Available from: https://www.wri.org/research/creating-sustainable-food-future (Accessed 2021 Aug 5). [Google Scholar]
- 4. Fanzo J, Bellows AL, Spiker ML, Thorne-Lyman AL, Bloem MW. The importance of food systems and the environment for nutrition. Am J Clin Nutr. 2021;113(1):7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Webb P, Benton TG, Beddington J, Flynn D, Kelly NM, Thomas SM. The urgency of food system transformation is now irrefutable. Nature Food. 2020;1(10):584–5. [DOI] [PubMed] [Google Scholar]
- 6. Byerlee D, Fanzo J. The SDG of zero hunger 75 years on: turning full circle on agriculture and nutrition. Glob Food Sec. 2019;21:52–9. [Google Scholar]
- 7. Jurkovich M. Feeding the hungry: advocacy and blame in the global fight against hunger. Ithaca, NY: Cornell University Press; 2020. [Google Scholar]
- 8. Micha R, Mannar V, Afshin A, Allemandi L, Baker P, Battersby J, Bhutta Z, Chen K, Corvalan C, Di Cesare M et al. Global nutrition report: action on equity to end malnutrition. Behrman N, editor. Bristol, UK: Development Initiatives; 2020. [Google Scholar]
- 9. von Braun J, Afsana K, Fresco L, Hassan M, Torero M. Food systems – definition, concept and application for the UN Food Systems Summit. [Internet]. Scientific Group for the UN Food Systems Summit; 2020. Available from: https://knowledge4policy.ec.europa.eu/sites/default/files/food_systems_concept_paper_scientific_group_-_draft_oct_261.pdf. [Google Scholar]
- 10. Committee on World Food Security (CFS). CFS voluntary guidelines on food systems and nutrition. Rome, Italy: CFS; 2021. [Google Scholar]
- 11. HLPE. Nutrition and food systems: a report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security, September 2017. Rome, Italy: CFS; 2017. [Google Scholar]
- 12. Fanzo J. Strengthening the engagement of food and health systems to improve nutrition security: synthesis and overview of approaches to address malnutrition. Glob Food Sec. 2014;3(3–4):183–92. [Google Scholar]
- 13. Fanzo J, Davis C. Global food systems, diets, and nutrition: linking science, economics, and policy. Cham, Switzerland: Springer Nature; 2021. [Google Scholar]
- 14. Ricciardi V, Ramankutty N, Mehrabi Z, Jarvis L, Chookolingo B. How much of the world's food do smallholders produce?. Glob Food Sec. 2018;17:64–72. [Google Scholar]
- 15. Mooney P. Too big to feed: exploring the impacts of mega-mergers, consolidation and concentration of power in the agri-food sector. [Internet]. London, UK: IPES-Food; 2017. Available from: https://agris.fao.org/agris-search/search.do?recordID=XF2018001356. [Google Scholar]
- 16. Herforth A, Bai Y, Venkat A, Mahrt K, Ebel A, Masters W. Cost and affordability of healthy diets across and within countries: background paper for The state of food security and nutrition in the world 2020. FAO Agricultural Development Economics Technical Study No. 9. Rome, Italy: FAO; 2020. [Google Scholar]
- 17. Baker P, Friel S. Food systems transformations, ultra-processed food markets and the nutrition transition in Asia. Global Health. 2016;12(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khonje MG, Qaim M. Modernization of African food retailing and (un)healthy food consumption. Sustainability. 2019;11(16):4306. [Google Scholar]
- 19. Baker P, Machado P, Santos T, Sievert K, Backholer K, Hadjikakou M, Russell C, Huse O, Bell C, Scrinis G et al. Ultra-processed foods and the nutrition transition: global, regional and national trends, food systems transformations and political economy drivers. Obes Rev. 2020;21(12):e13126. [DOI] [PubMed] [Google Scholar]
- 20. Popkin BM, Reardon T. Obesity and the food system transformation in Latin America. Obes Rev. 2018;19(8):1028–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reardon T, Tschirley D, Liverpool-Tasie LSO, Awokuse T, Fanzo J, Minten B, Vos R, Dolislager M, Sauer C, Dhar R et al. The processed food revolution in African food systems and the double burden of malnutrition. Glob Food Sec. 2021;28:100466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, Mullany EC, Abate KH, Abbafati C, Abebe Z et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Springmann M, Clark M, Mason-D'Croz D, Wiebe K, Bodirsky BL, Lassaletta L, de Vries W, Vermeulen SJ, Herrero M, Carlson KM et al. Options for keeping the food system within environmental limits. Nature. 2018;562(7728):519–25. [DOI] [PubMed] [Google Scholar]
- 24. He P, Baiocchi G, Hubacek K, Feng K, Yu Y. The environmental impacts of rapidly changing diets and their nutritional quality in China. Nature Sustainability. 2018;1(3):122–7. [Google Scholar]
- 25. Perry BD, Grace DC. How growing complexity of consumer choices and drivers of consumption behaviour affect demand for animal source foods. Ecohealth. 2015;12(4):703–12. [DOI] [PubMed] [Google Scholar]
- 26. Kim BF, Santo RE, Scatterday AP, Fry JP, Synk CM, Cebron SR, Mekonnen MM, Hoekstra AY, De Pee S, Bloem MW et al. Country-specific dietary shifts to mitigate climate and water crises. Global Environ Change. 2020;62:101926. [Google Scholar]
- 27. Kharas H, McArthur JW, Ohno I. Leave no one behind: time for specifics on the Sustainable Development Goals. Washington (DC): Brookings Institution Press; 2019. [Google Scholar]
- 28. Tomich TP, Lidder P, Coley M, Gollin D, Meinzen-Dick R, Webb P, Carberry P. Food and agricultural innovation pathways for prosperity. Agric Syst. 2019;172:1–15. [Google Scholar]
- 29. Dennig F, Budolfson MB, Fleurbaey M, Siebert A, Socolow RH. Inequality, climate impacts on the future poor, and carbon prices. Proc Natl Acad Sci U S A. 2015;112(52):15827–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rozenberg J, Hallegatte S. Poor people on the front line: the impacts of climate change on poverty in 2030. In: Kanbur R, Shue H, editors. Climate justice: integrating economics and philosophy. Oxford, United Kingdom: Oxford University Press; 2018. p. 24–42. [Google Scholar]
- 31. Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. FAO, International Fund for Agricultural Development, UNICEF, World Food Programme, WHO. The state of food security and nutrition in the world 2020. Transforming food systems for affordable healthy diets. Rome, Italy: FAO; 2020. [Google Scholar]
- 33. Headey D, Heidkamp R, Osendarp S, Ruel M, Scott N, Black R, Shekar M, Bouis H, Flory A, Haddad L et al. Impacts of COVID-19 on childhood malnutrition and nutrition-related mortality. Lancet. 2020;396(10250):519–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Osendarp S, Akuoku JK, Black RE, Headey D, Ruel M, Scott N, Shekar M, Walker N, Flory A, Haddad L et al. The COVID-19 crisis will exacerbate maternal and child undernutrition and child mortality in low- and middle-income countries. Nature Food. 2021;2(7):476–84. [DOI] [PubMed] [Google Scholar]
- 35. Popkin BM. The implications of the nutrition transition for obesity in the developing world. In: Crawford D, Jeffery RW, Ball K, Brug J, editors. Obesity epidemiology: from aetiology to public health. Oxford, United Kingdom: Oxford University Press; 2010. p. 136–58. [Google Scholar]
- 36. Popkin BM. Relationship between shifts in food system dynamics and acceleration of the global nutrition transition. Nutr rev. 2017;75(2):73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Roediger R, Hendrixson DT, Manary MJ. A roadmap to reduce stunting. Am J Clin Nutr. 2020;112(Supplement_2):773S–6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gao L, Bhurtyal A, Wei J, Akhtar P, Wang L, Wang Y. Double burden of malnutrition and nutrition transition in Asia: a case study of 4 selected countries with different socioeconomic development. Adv Nutr. 2020;11(6):1663–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. International Institute for Population Sciences (IIPS). Key findings from NFHS-5. [Internet]. Mumbai, India: IIPS; 2020. Available from: http://rchiips.org/nfhs/factsheet_NFHS-5.shtml (Accessed 2021 Aug 5). [Google Scholar]
- 40. Martorell R, Young MF. Patterns of stunting and wasting: potential explanatory factors. Adv Nutr. 2012;3(2):227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ford ND, Martorell R, Ramirez-Zea M, Stein AD. The nutrition transition in rural Guatemala: 12 year changes in diet of adults. FASEB J. 2017;31(S1):147.3. [Google Scholar]
- 42. Mialon M, Gomes FS. Public health and the ultra-processed food and drink products industry: corporate political activity of major transnationals in Latin America and the Caribbean. Public Health Nutr. 2019;22(10):1898–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tzioumis E, Adair LS. Childhood dual burden of under- and overnutrition in low- and middle-income countries: a critical review. Food Nutr Bull. 2014;35(2):230–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, Laxmaiah A, Kengne A-P, Bentham J. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 2019;17(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, Adams RJ, Aekplakorn W, Afsana K, Aguilar-Salinas CA et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387(10026):1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Malik VS, Willet WC, Hu FB. Nearly a decade on — trends, risk factors and policy implications in global obesity. Nat Rev Endocrinol. 2020;16(11):615–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Jaacks LM, Kavle J, Perry A, Nyaku A. Programming maternal and child overweight and obesity in the context of undernutrition: current evidence and key considerations for low- and middle-income countries. Public Health Nutr. 2017;20(7):1286–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ashwell M, Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016;6(3):e010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Arage G, Belachew T, Hajmahmud K, Abera M, Abdulhay F, Abdulahi M, Abate KH. Impact of early life famine exposure on adulthood anthropometry among survivors of the 1983–1985 Ethiopian Great famine: a historical cohort study. BMC Public Health. 2021;21:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Laborde D, Herforth A, Headey D, de Pee S. COVID-19 pandemic leads to greater depth of unaffordability of healthy and nutrient-adequate diets in low- and middle-income countries. Nature Food. 2021;2(7):473–5. [DOI] [PubMed] [Google Scholar]
- 53. Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L, Mead BR, Noonan R, Hardman CA. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156:104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lin AL, Vittinghoff E, Olgin JE, Pletcher MJ, Marcus GM. Body weight changes during pandemic-related shelter-in-place in a longitudinal cohort study. JAMA Netw Open. 2021;4(3):e212536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2020;395(10218):142–55. [DOI] [PubMed] [Google Scholar]
- 56. Ruel M Sr, Hawkes C. Double duty actions to tackle all forms of malnutrition (P10-053-19). Curr Dev Nutr. 2019;3(Suppl 1):nzz034.P10–053-19. [Google Scholar]
- 57. Harris J, Nisbett N. The basic determinants of malnutrition: resources, structures, ideas and power. Int J Health Policy Manag. 2020; Dec 26 (Epub ahead of print; doi:10.34172/ijhpm.2020.259). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bell W, Lividini K, Masters WA. Global dietary convergence from 1970 to 2010 altered inequality in agriculture, nutrition and health. Nature Food. 2021;2(3):156–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nisbett N, Harris J. Equity in social and development studies research: insights for nutrition. [Internet]. In: UNSCN News 43. Advancing equity, equality and non-discrimination in food systems: pathways to reform. Rome, Italy: United Nations System Standing Committee on Nutrition Secretariat; 2018. p. 57–63.. Available from: https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/13991 (Accessed 2021 Aug 5). [Google Scholar]
- 60. Harris J, Tan W, Mitchell B, Zayed D. Equity in agriculture-nutrition-health research: a scoping review. Nutr Rev. 2021; Apr 28 (Epub ahead of print; doi:10.1093/nutrit/nuab001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Walls H, Nisbett N, Laar A, Drimie S, Zaidi S, Harris J. Addressing malnutrition: the importance of political economy analysis of power. Int J Health Policy Manag. 2020; Dec 16 (Epub ahead of print; doi:10.34172/ijhpm.2020.250). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Barrett CB. Actions now can curb food systems fallout from COVID-19. Nature Food. 2020;1(6):319–20. [DOI] [PubMed] [Google Scholar]
- 63. Koo J, Mamun A, Martin W. From bad to worse: poverty impacts of food availability responses to weather shocks. Agric Econ. 2021;52(5):833–47. [Google Scholar]
- 64. Crenshaw KW. On intersectionality: essential writings. New York: The New Press; 2017. [Google Scholar]
- 65. Headey D, Hoddinott J, Park S. Accounting for nutritional changes in six success stories: a regression-decomposition approach. Glob Food Sec. 2017;13:12–20. [Google Scholar]
- 66. Fraser N. Social justice in the age of identity politics: redistribution, recognition, participation. Discussion paper. Berlin, Germany: Wissenschaftszentrum Berlin für Sozialforschung (WZB); 1998. [Google Scholar]
- 67. Finaret AB, Masters WA. Beyond calories: the new economics of nutrition. Annu Rev Resour Econ. 2019;11:237–59. [Google Scholar]
- 68. Karpyn AE, Riser D, Tracy T, Wang R, Shen YE. The changing landscape of food deserts. UNSCN Nutr. 2019;44:46–53. [PMC free article] [PubMed] [Google Scholar]
- 69. Singleton CR, Li Y, Duran AC, Zenk SN, Odoms-Young A, Powell LM. Food and beverage availability in small food stores located in Healthy Food Financing Initiative eligible communities. Int J Environ Res Public Health. 2017;14(10):1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Rhone A, Ver Ploeg M, Dicken C, Williams R, Breneman V. Low-income and low-supermarket-access census tracts, 2010-2015. [Internet]. EIB-165. Washington (DC): USDA, Economic Research Service; 2017. Available from: https://ageconsearch.umn.edu/record/262134/files/eib-165.pdf (Accessed 2021 Aug 5). [Google Scholar]
- 71. Battersby J, Crush J. Africa's urban food deserts. Urban Forum. 2014;25(2):143–51. [Google Scholar]
- 72. Lu W, Qiu F. Do food deserts exist in Calgary, Canada?. Can Geogr. 2015;59(3):267–82. [Google Scholar]
- 73. Cooksey-Stowers K, Schwartz MB, Brownell KD. Food swamps predict obesity rates better than food deserts in the United States. Int J Environ Res Public Health. 2017;14(11):1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Chenarides L, Cho C, Nayga RM, Thomsen MR. Dollar stores and food deserts. Appl Geogr. 2021;134:102497. [Google Scholar]
- 75. Freedman DA, Vaudrin N, Schneider C, Trapl E, Ohri-Vachaspati P, Taggart M, Ariel Cascio M, Walsh C, Flocke S. Systematic review of factors influencing farmers’ market use overall and among low-income populations. J Acad Nutr Diet. 2016;116(7):1136–55. [DOI] [PubMed] [Google Scholar]
- 76. Bailey ZD, Feldman JM, Bassett MT. How structural racism works — racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2021;384(8):768–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhang M, Debarchana G. Spatial supermarket redlining and neighborhood vulnerability: a case study of Hartford, Connecticut. Trans GIS. 2016;20(1):79–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bernasco W, Block R. Robberies in Chicago: a block-level analysis of the influence of crime generators, crime attractors, and offender anchor points. J Res Crime Delinq. 2011;48(1):33–57. [Google Scholar]
- 79. Allen T, Murray KA, Zambrana-Torrelio C, Morse SS, Rondinini C, Di Marco M, Breit N, Olival KJ, Daszak P. Global hotspots and correlates of emerging zoonotic diseases. Nat Commun. 2017;8(1):1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, Daszak P. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Rohr JR, Barrett CB, Civitello DJ, Craft ME, Delius B, DeLeo GA, Hudson PJ, Jouanard N, Nguyen KH, Ostfeld RS et al. Emerging human infectious diseases and the links to global food production. Nature Sustainability. 2019;2(6):445–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Grace D. Food safety in low and middle income countries. Int J Environ Res Public Health. 2015;12(9):10490–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Gibb R, Browning E, Glover-Kapfer P, Jones KE. Emerging opportunities and challenges for passive acoustics in ecological assessment and monitoring. Methods Ecol Evol. 2019;10(2):169–85. [Google Scholar]
- 84. Havelaar AH, Brul S, de Jong A, de Jonge R, Zwietering MH, Ter Kuile BH. Future challenges to microbial food safety. Int J Food Microbiol. 2010;139:S79–94. [DOI] [PubMed] [Google Scholar]
- 85. Grace D, Alonso S, Bett BK, Lindahl JF, Patel E, Nguyen-Viet H, Roesel K, Unger F, Dominguez-Salas P. Food safety and nutrition. In: McIntire J, Grace D, editors. The impact of research at the International Livestock Research Institute. Nairobi, Kenya and Wallingford, United Kingdom: ILRI and CABI; 2020. p. 338–65. [Google Scholar]
- 86. Walls H, Baker P, Chirwa E, Hawkins B. Food security, food safety & healthy nutrition: are they compatible?. Glob Food Sec. 2019;21:69–71. [Google Scholar]
- 87. Grace D, Alonso S, Roesel K, Covic N, McDermott JJ. Sustained food safety action for improved nutrition and health of Africans. [Internet]. Background paper prepared for the 9th annual Africa Day for Food and Nutrition Security, Dar es Salaam, Tanzania, 4–5 December 2018. Nairobi, Kenya: International Livestock Research Institute; 2018. Available from: https://cgspace.cgiar.org/bitstream/handle/10568/98385/nutrition_security.pdf?sequence=4. [Google Scholar]
- 88. Schlaudecker EP, Steinhoff MC, Moore SR. Interactions of diarrhea, pneumonia, and malnutrition in childhood: recent evidence from developing countries. Curr Opin Infect Dis. 2011;24(5):496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Caulfield LE, de Onis M, Blössner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr. 2004;80(1):193–8. [DOI] [PubMed] [Google Scholar]
- 90. Franco-Martínez L, Martínez-Subiela S, Cerón JJ, Bernal LJ, Tecles F, Tvarijonaviciute A. Teaching the basics of the One Health concept to undergraduate veterinary students. Res Vet Sci. 2020;133:219–25. [DOI] [PubMed] [Google Scholar]
- 91. Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, Ezeh A, Frumkin H, Gong P, Head P et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation–Lancet Commission on planetary health. Lancet. 2015;386(10007):1973–2028. [DOI] [PubMed] [Google Scholar]
- 92. Mbow C, Rosenzweig C, Barioni LG, Benton TG, Herrero M, Krishnapillai M, Liwenga E, Pradhan P, Rivera-Ferre MG, Sapkota TB et al. Food security. In: Climate change and land: an IPCC Special Report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems. Geneva, Switzerland: IPCC; 2019. [Google Scholar]
- 93. Fanzo J, Davis C, McLaren R, Choufani J. The effect of climate change across food systems: implications for nutrition outcomes. Glob Food Sec. 2018;18:12–19. [Google Scholar]
- 94. Leibenath M, Kurth M, Lintz G. Science–policy interfaces related to biodiversity and nature conservation: the case of Natural Capital Germany—TEEB-DE. Sustainability. 2020;12(9):3701. [Google Scholar]
- 95. Crippa M, Solazzo E, Guizzardi D, Monforti-Ferrario F, Tubiello FN, Leip A. Food systems are responsible for a third of global anthropogenic GHG emissions. Nature Food. 2021;2(3):198–209. [DOI] [PubMed] [Google Scholar]
- 96. Watson RT, Noble IR, Bolin B, Ravindranath NH, Verardo DJ, Dokken DJ, editors. IPCC special report on land use, land-use change, and forestry. Geneva, Switzerland: IPCC; 2000. [Google Scholar]
- 97. Ray DK, West PC, Clark M, Gerber JS, Prishchepov AV, Chatterjee S. Climate change has likely already affected global food production. PLoS One. 2019;14(5):e0217148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Valin H, Sands RD, van der Mensbrugghe D, Nelson GC, Ahammad H, Blanc E, Bodirsky B, Fujimori S, Hasegawa T, Havlik P et al. The future of food demand: understanding differences in global economic models. Agric Econ. 2014;45(1):51–67. [Google Scholar]
- 99. Cassman KG, Grassini P. A global perspective on sustainable intensification research. Nature Sustainability. 2020;3(4):262–8. [Google Scholar]
- 100. Organisation for Economic Cooperation and Development (OECD)/FAO. FAO Food Price Index. [Internet]. In: OECD-FAO agricultural outlook 2021-2030. Paris, France: OECD; 2021. Available from: https://www.oecd-ilibrary.org/agriculture-and-food/fao-food-price-index_74b9be71-en (Accessed 2021 Aug 5). [Google Scholar]
- 101. Tadesse G, Algieri B, Kalkuhl M, von Braun J. Drivers and triggers of international food price spikes and volatility. Food Policy. 2014;47:117–28. [Google Scholar]
- 102. FAO, International Fund for Agricultural Development, UNICEF, World Food Programme, WHO. The state of food security and nutrition in the world 2018. Building climate resilience for food security and nutrition. Rome, Italy: FAO; 2018. [Google Scholar]
- 103. Vellakkal S, Fledderjohann J, Basu S, Agrawal S, Ebrahim S, Campbell O, Doyle P, Stuckler D. Food price spikes are associated with increased malnutrition among children in Andhra Pradesh, India. J Nutr. 2015;145(8):1942–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Headey DD, Alderman HH. The relative caloric prices of healthy and unhealthy foods differ systematically across income levels and continents. J Nutr. 2019;149(11):2020–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Myers SS, Zanobetti A, Kloog I, Huybers P, Leakey ADB, Bloom AJ, Carlisle E, Dietterich LH, Fitzgerald G, Hasegawa T et al. Increasing CO2 threatens human nutrition. Nature. 2014;510(7503):139–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Scheelbeek PFD, Tuomisto HL, Bird FA, Haines A, Dangour AD. Effect of environmental change on yield and quality of fruits and vegetables: two systematic reviews and projections of possible health effects. Lancet Glob Health. 2017;5:S21. [Google Scholar]
- 107. Beach RH, Sulser TB, Crimmins A, Cenacchi N, Cole J, Fukagawa NK, Mason-D'Croz D, Myers S, Sarofim MC, Smith M et al. Combining the effects of increased atmospheric carbon dioxide on protein, iron, and zinc availability and projected climate change on global diets: a modelling study. Lancet Planet Health. 2019;3(7):e307–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. National Oceanic and Atmospheric Administration (NOAA). Climate at a glance. [Internet]. Silver Spring, MD: NOAA; 2021[cited 9 August, 2021]. Available from: https://www.ncdc.noaa.gov/cag/global/time-series/globe/land/ytd/12/1880-2020. [Google Scholar]
- 109. Brunner L, Pendergrass AG, Lehner F, Merrifield AL, Lorenz R, Knutti R. Reduced global warming from CMIP6 projections when weighting models by performance and independence. Earth Syst Dyn. 2020;11(4):995–1012. [Google Scholar]
- 110. Greve P, Gudmundsson L, Seneviratne SI. Regional scaling of annual mean precipitation and water availability with global temperature change. Earth Syst Dyn. 2018;9(1):227–40. [Google Scholar]
- 111. Porter JR. Rising temperatures are likely to reduce crop yields. Nature. 2005;436(7048):174. [DOI] [PubMed] [Google Scholar]
- 112. Lobell DB, Cahill KN, Field CB. Historical effects of temperature and precipitation on California crop yields. Clim Change. 2007;81(2):187–203. [Google Scholar]
- 113. Rigden AJ, Mueller ND, Holbrook NM, Pillai N, Huybers P. Combined influence of soil moisture and atmospheric evaporative demand is important for accurately predicting US maize yields. Nature Food. 2020;1(2):127–33. [DOI] [PubMed] [Google Scholar]
- 114. Butler EE, Huybers P. Adaptation of US maize to temperature variations. Nature Climate Change. 2013;3(1):68–72. [Google Scholar]
- 115. DHS [Internet]. Rockville, MD: ICF. Available from: https://www.dhsprogram.com/. [Google Scholar]
- 116. Funk C, Shukla S. Drought early warning and forecasting: theory and practice. Amsterdam, Netherlands: Elsevier; 2020. [Google Scholar]
- 117. Grillo J, Holt J. Application of the livelihood zone maps and profiles for food security analysis and early warning: guidance for Famine Early Warning Systems Network (FEWS NET) representatives and partners. Washington (DC): USAID FEWSNET; 2009. [Google Scholar]
- 118. Füssel H-M. Vulnerability: a generally applicable conceptual framework for climate change research. Global Environ Change. 2007;17(2):155–67. [Google Scholar]
- 119. Brown M. Food security, food prices and climate variability. Abingdon, United Kingdom: Routledge; 2014. [Google Scholar]
- 120. Brown ME, Grace K, Shively G, Johnson KB, Carroll M. Using satellite remote sensing and household survey data to assess human health and nutrition response to environmental change. Popul Environ. 2014;36(1):48–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Brown ME, Backer D, Billing T, White P, Grace K, Doocy S, Huth P. Empirical studies of factors associated with child malnutrition: highlighting the evidence about climate and conflict shocks. Food Security. 2020;12(6):1241–52. [Google Scholar]
- 122. Niles MT, Emery BF, Wiltshire S, Brown ME, Fisher B, Ricketts TH. Climate impacts associated with reduced diet diversity in children across nineteen countries. Environ Res Lett. 2021;16(1):015010. [Google Scholar]
- 123. Cooper MW, Brown ME, Hochrainer-Stigler S, Pflug G, McCallum I, Fritz S, Silva J, Zvoleff A. Mapping the effects of drought on child stunting. Proc Natl Acad Sci U S A. 2019;116(35):17219–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Grace K, Davenport F, Hanson H, Funk C, Shukla S. Linking climate change and health outcomes: examining the relationship between temperature, precipitation and birth weight in Africa. Global Environ Change. 2015;35:125–37. [Google Scholar]
- 125. Myers SS, Smith MR, Guth S, Golden CD, Vaitla B, Mueller ND, Dangour AD, Huybers P. Climate change and global food systems: potential impacts on food security and undernutrition. Annu Rev Public Health. 2017;38:259–77. [DOI] [PubMed] [Google Scholar]
- 126. Fanzo J, Hood A, Davis C. Eating our way through the Anthropocene. Physiol Behav. 2020;222:112929. [DOI] [PubMed] [Google Scholar]
- 127. Naghshi S, Sadeghi O, Willett WC, Esmaillzadeh A. Dietary intake of total, animal, and plant proteins and risk of all cause, cardiovascular, and cancer mortality: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2020;370:m2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Steffen W. Climate change, the Anthropocene and planetary boundaries. In: Qatar University Life Science Symposium 2016: biodiversity, sustainability and climate change, with perspectives from Qatar; 4–5 December 2016; Doha, Qatar. Doha, Qatar: Hamad bin Khalifa University (HBKU) Press; 2016. [Google Scholar]
- 129. Park J, Kim J. Meta analysis of relation between Mediterranean diet and overall mortality. Atherosclerosis. 2015;241(1):e195. [Google Scholar]
- 130. Kastorini C-M, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011;57(11):1299–313. [DOI] [PubMed] [Google Scholar]
- 131. Clark MA, Domingo NGG, Colgan K, Thakrar SK, Tilman D, Lynch J, Azevedo IL, Hill JD. Global food system emissions could preclude achieving the 1.5° and 2°C climate change targets. Science. 2020;370(6517):705–8. [DOI] [PubMed] [Google Scholar]
- 132. Barrett CB, Benton TG, Cooper KA, Fanzo J, Gandhi R, Herrero M, James S, Kahn M, Mason-D'Croz D, Mathys A et al. Bundling innovations to transform agri-food systems. Nature Sustainability. 2020;3(12):974–6. [Google Scholar]
- 133. Chambers JM, Wyborn C, Ryan ME, Reid RS, Riechers M, Serban A, Bennett NJ, Cvitanovic C, Fernández-Giménez ME, Galvin KA et al. Six modes of co-production for sustainability. Nature Sustainability. 2021; Aug 5 (Epub ahead of print; doi:10.1038/s41893-021-00755-x). [Google Scholar]
- 134. Cassidy ES, West PC, Gerber JS, Foley JA. Redefining agricultural yields: from tonnes to people nourished per hectare. Environ Res Lett. 2013;8(3):034015. [Google Scholar]
- 135. Mason-D'Croz D, Bogard JR, Sulser TB, Cenacchi N, Dunston S, Herrero M, Wiebe K. Gaps between fruit and vegetable production, demand, and recommended consumption at global and national levels: an integrated modelling study. Lancet Planet Health. 2019;3(7):e318–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Wood SA, Smith MR, Fanzo J, Remans R, DeFries RS. Trade and the equitability of global food nutrient distribution. Nature Sustainability. 2018;1(1):34–7. [Google Scholar]
- 137. Garton K, Thow AM, Swinburn B. International trade and investment agreements as barriers to food environment regulation for public health nutrition: a realist review. Int J Health Policy Manag. 2020; Oct 19 (Epub ahead of print; doi:10.34172/ijhpm.2020.189). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Thow AM, Nisbett N. Trade, nutrition, and sustainable food systems. Lancet. 2019;394(10200):716–18. [DOI] [PubMed] [Google Scholar]
- 139. Koester U, Galaktionova E. FAO Food Loss Index methodology and policy implications. Stud Agric Econ. 2021;123(1):1–7. [Google Scholar]
- 140. Schmidt K, Matthies E. Where to start fighting the food waste problem? Identifying most promising entry points for intervention programs to reduce household food waste and overconsumption of food. Resour Conserv Recycl. 2018;139:1–14. [Google Scholar]
- 141. Schneider F, Eriksson M. Food waste (and loss) at the retail level. In: Reynolds C, Soma T, Spring C, Lazell J, editors. Routledge handbook of food waste. Abingdon, United Kingdom: Routledge; 2020. p. 114–28. [Google Scholar]
- 142. Neff RA, Kanter R, Vandevijvere S. Reducing food loss and waste while improving the public's health. Health Aff. 2015;34(11):1821–9. [DOI] [PubMed] [Google Scholar]
- 143. Spiker ML, Hiza HAB, Siddiqi SM, Neff RA. Wasted food, wasted nutrients: nutrient loss from wasted food in the United States and comparison to gaps in dietary intake. J Acad Nutr Diet. 2017;117(7):1031–40.e22. [DOI] [PubMed] [Google Scholar]
- 144. Global Panel on Agriculture and Food Systems for Nutrition (Glopan). Preventing nutrient loss and waste across the food system: policy actions for high-quality diets. Policy Brief No. 12. London, United Kingdom: Glopan; 2018. [Google Scholar]
- 145. Bai Y, Alemu R, Block SA, Headey D, Masters WA. Cost and affordability of nutritious diets at retail prices: evidence from 177 countries. Food Policy. 2021;99:101983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Lawrence M. Ultraprocessed foods and cardiovascular health: it's not just about the nutrients. Am J Clin Nutr. 2021;113(2):257–8. [DOI] [PubMed] [Google Scholar]
- 147. Rolls BJ, Cunningham PM, Diktas HE. Properties of ultraprocessed foods that can drive excess intake. Nutr Today. 2020;55(3):109–15. [Google Scholar]
- 148. Elizabeth L, Machado P, Zinöcker M, Baker P, Lawrence M. Ultra-processed foods and health outcomes: a narrative review. Nutrients. 2020;12(7):1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Ludwig DS, Astrup A, Bazzano LA, Ebbeling CB, Heymsfield SB, King JC, Willett WC. Ultra-processed food and obesity: the pitfalls of extrapolation from short studies. Cell Metab. 2019;30(1):3–4. [DOI] [PubMed] [Google Scholar]
- 150. Constantinides SV, Turner C, Frongillo EA, Bhandari S, Reyes LI, Blake CE. Using a global food environment framework to understand relationships with food choice in diverse low- and middle-income countries. Glob Food Sec. 2021;29:100511. [Google Scholar]
- 151. Gillespie S, Haddad L, Mannar V, Menon P, Nisbett N, Maternal and Child Nutrition Study Group . The politics of reducing malnutrition: building commitment and accelerating progress. Lancet. 2013;382(9891):552–69. [DOI] [PubMed] [Google Scholar]
- 152. Béné C, Oosterveer P, Lamotte L, Brouwer ID, de Haan S, Prager SD, Talsma EF, Khoury CK. When food systems meet sustainability – current narratives and implications for actions. World Dev. 2019;113:116–30. [Google Scholar]
- 153. Béné C, Fanzo J, Prager SD, Achicanoy HA, Mapes BR, Toro PA, Cedrez CB. Global drivers of food system (un)sustainability: a multi-country correlation analysis. PLoS One. 2020;15(4):e0231071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Yambi O, Rocha C, Jacobs N, International Panel of Experts on Sustainable Food Systems (IPES-Food) . Unravelling the food-health nexus to build healthier food systems. In: Biesalski HK, editor. Hidden hunger and the transformation of food systems: how to combat the double burden of malnutrition?. World review of nutrition and dieteticsvol. 121. Basel, Switzerland: Karger; 2020. p. 1–8. [Google Scholar]
- 155. Golden CD, Gephart JA, Eurich JG, McCauley DJ, Sharp MK, Andrew NL, Seto KL. Social-ecological traps link food systems to nutritional outcomes. Glob Food Sec. 2021;30:100561. [Google Scholar]
- 156. Benton TG, Bieg C, Harwatt H, Pudasaini R, Wellesley L. Food system impacts on biodiversity loss. Three levers for food system transformation in support of nature. [Internet]. London, United Kingdom: Chatham House; 2021. Available from: https://action.ciwf.org/media/7443992/food-system-impacts-on-biodiversity-loss.pdf (Accessed 2021 Aug 5). [Google Scholar]
- 157. Benton TG, Bailey R. The paradox of productivity: agricultural productivity promotes food system inefficiency. Global Sustainability. 2019;2:E6. [Google Scholar]
- 158. Baker L, Castilleja G, De Groot Ruiz A, Jones A. Prospects for the true cost accounting of food systems. Nature Food. 2020;1(12):765–7. [DOI] [PubMed] [Google Scholar]
- 159. Ray DK, Mueller ND, West PC, Foley JA. Yield trends are insufficient to double global crop production by 2050. PLoS One. 2013;8(6):e66428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Wegner L, Zwart G. Who will feed the world? The production challenge. Food Chain. 2011;1(2):187–205. [Google Scholar]
- 161. Tamburino L, Bravo G, Clough Y, Nicholas KA. From population to production: 50 years of scientific literature on how to feed the world. Glob Food Sec. 2020;24:100346. [Google Scholar]
- 162. Fanzo J, Haddad L, McLaren R, Marshall Q, Davis C, Herforth A, Jones A, Beal T, Tschirley D, Bellows A et al. The Food Systems Dashboard is a new tool to inform better food policy. Nature Food. 2020;1(5):243–6. [Google Scholar]
- 163. Nisbett N, Harris J, Backholer K, Baker P, Friel S, Jernigan VBB. Holding no-one back: the nutrition equity framework in theory and practice. Glob Food Sec. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]