Abstract
Aims
Delivery of cardiac rehabilitation (CR) was challenged during the pandemic caused by the Coronavirus disease (COVID-19), due to government stay-at-home directives which restricted in-person programmes. The Australian state of Victoria experienced the longest and most severe COVID-19 restrictions and was in lockdown for ∼6 months of 2020. We aimed to explore (i) clinicians’ experiences and perceptions and (ii) identify barriers and enablers, for delivering CR during the COVID-19 pandemic.
Methods and results
Victorian members of the Australian Cardiovascular Health and Rehabilitation Association (ACRA) were invited to attend an exploratory qualitative online consultation in November 2020. An inductive thematic analysis was undertaken, before deductively applying the Non-adoption, Abandonment, Scale-up, Spread, and Sustainability (NASSS) framework to identify barriers and enablers for technology adoption in CR. Thirty members participated in a 106-min consultation. Seventeen members who provided demographics represented multiple disciplines (nursing n = 13, exercise physiology n = 3, and physiotherapy n = 1) and geographical settings (metropolitan n = 10, regional n = 4, and rural n = 3). Four main themes were inductively identified: consequences of change; use of technology; capacity; and the way forward. The deductive NASSS analysis demonstrated the main challenges of continuing remotely delivered CR lie with adopters (staff, patients, and carers) and with organizations.
Conclusion
The COVID-19 pandemic expedited significant changes to CR delivery models. While clinicians are eager to retain technology-enabled delivery in addition to resuming in-person CR, it is now timely to review remote models of care, tools used and plan how they will be integrated with traditional in-person programmes.
Keywords: Cardiac rehabilitation, COVID-19, telehealth, telerehabilitation, models of care, qualitative
Implications for practice
While clinicians are eager to continue to integrate telehealth into cardiac rehabilitation (CR) programmes, staff, and programme capacity are significant issues that need to be addressed if multimodal programmes are to be integrated into practice long term.
Initial experience in the use of telehealth in CR has been gained. Evaluation is now needed to refine telehealth technologies, develop local policies and guidelines, and secure long-term sustainable funding.
Using the Non-adoption, Abandonment, Scale-up, Spread, and Sustainability framework to guide future telehealth adoption, particular focus is required for the adopter system, particularly for staff in the form of resources, training, and support. Focus is also required for organizations, particularly for changes in team interactions and routines.
Introduction
Cardiac rehabilitation (CR) is a complex intervention comprising education, tailored and supervised exercise, and psychological support.1 It is strongly recommended for all patients following a cardiac event or diagnosis, based on Level I evidence,1 demonstrating significant improvements in cardiovascular mortality, hospitalization, and quality of life.1–4 Cardiac rehabilitation is typically delivered in-person.5 Emerging alternatives, such as home and telehealth delivery models, are seldom adopted despite increasing availability, capability to address traditional participation barriers, and evidence demonstrating similar improvements in cardiovascular disease risk as in-person programmes.6–8
Australian delivery of CR was challenged during the Coronavirus disease (COVID-19) pandemic due to government enforced restrictions and lockdowns; the state of Victoria experienced restrictions of the longest duration with ∼6 months spent under stay-at-home directives in 2020.9 Approximately 136 public, community, and private programmes provide CR in the state of Victoria where the age-standardized rate for heart disease admissions is 117 per 10 000 persons.10,11 During lockdown, many CR staff were redeployed into COVID-related roles and outpatient services, such as CR, were required to be delivered remotely. This required a significant and rapid change to existing models of care. The aims of this study were to (i) explore clinicians’ experiences and perceptions and (ii) identify barriers and enablers, for delivering CR during COVID-19.
Methods
Setting
This study focused on outpatient Phase II CR, which in Australia (including Victoria), is predominantly co-ordinated by nurses and run by multidisciplinary teams.5 Programmes are delivered across diverse health settings, such as public and private hospitals, community health services, and private clinics. On average, Australian CR programmes provide nine sessions and include exercise training12 in addition to education on heart disease, physical activity, diet, and depression.5 From the last documented national CR survey in 2014, telephone support was used in 58% of programmes. However, the use of the internet for video conferencing to deliver CR was only used in 2.4% of programmes.5 This may have increased slightly over recent years, but anecdotally very few CR programmes in Victoria used models of care that included telehealth prior to COVID-19.
Design
We undertook an exploratory qualitative study to understand the experiences of CR clinicians delivering CR during the COVID-19 pandemic, and have reported findings according to the Consolidated Criteria for Reporting Qualitative Studies (COREQ).13 The Non-adoption, Abandonment, Scale-up, Spread, and Sustainability (NASSS) Framework14 was used to understand adoption of barriers and enablers to technology use for CR delivery.
Participant selection and recruitment
Australian Cardiovascular Health and Rehabilitation Association (ACRA) members in the state of Victoria (n = 155) were invited to an online consultation held in November 2020, via member newsletters, with a link to access the study information. The ACRA is the peak organization for CR healthcare professionals in Australia.15
Data collection
Feedback on priority discussion topics was received via an online poll distributed in the members’ newsletter. This was reviewed by two investigators (M.T. and P.R.) and synthesized into 10 key questions (Supplementary material online). Participants contributed to the online consultation by speaking or using the written chat function. An overall facilitator (J.C.R.) guided the conversation according to these key questions. A second facilitator (M.T.) moderated the chat. Field notes were taken (S.C.) to augment videoconference data.
Ethical considerations and data storage
This investigation conforms with the principles outlined in the Declaration of Helsinki16 and was approved by the Alfred Hospital Ethics Committee (756/20). Before initiating the recorded discussion, participants were reminded that consent was implied by attendance, provided an opportunity to ask questions, and reminded they could leave at any time. Data were stored on a secure server at Monash University. Data transfer for transcription was conducted via web-based end-to-end SSL encryption.
Data analysis
Demographic information collected via videoconference polling was analysed descriptively. The audio file was transcribed verbatim, while the chat text was downloaded and combined in a separate section of the transcript for analysis.
Analysis of the single transcript was conducted by hand using coloured highlighters, independently by two investigators (S.C. and A.J.). A third investigator (J.C.R.) assisted in refining themes. First, a thematic analysis using Braun and Clarke’s17 six steps was undertaken. Investigators increased familiarization with the data via multiple audio playbacks and repeatedly moved between reading, reflecting, and interpreting the transcript.18,19 Data were coded, and codes were categorized and grouped into themes. Investigators then met to discuss and compare codes, reflect, and begin to develop themes. Field notes were also reviewed during this time, which included initial thoughts on emerging themes and notes on group interaction.
Second, we anticipated technology would be a prominent theme in the setting of remotely delivered CR. Therefore, we planned to deductively apply the NASSS Framework14 to evaluate the complexity and future challenges of technology-enabled CR delivery. In brief, the NASSS Framework is an evidence-based, theory-informed pragmatic framework to predict and evaluate the success of technology-supported health programmes. The framework can be applied either prospectively or in our case, retrospectively. The NASSS comprises seven domains, where each is classified as simple (straightforward, predictable, and few components), complicated (multiple interacting components or issues), or complex (dynamic, unpredictable, not easily disaggregated into constituent components).14 Two investigators (S.C. and A.J.) mapped themes and subthemes into the seven NASSS domains and applied what were determined to be the appropriate classification. A third investigator (J.C.R.) reviewed decisions and settled any discrepancies. An example was used where it was not appropriate to map a theme.
Reflexivity and rigour
As qualitative researchers bring personal values, beliefs, and experiences to their research,20 self-reflection and reflexivity are critical to achieve high-quality data analysis. The analysts all had strong knowledge of CR, experience in conducting qualitative research, and diverse multidisciplinary backgrounds. S.C. is a cardiac nurse and researcher who has undertaken qualitative research training and conducted previous qualitative studies. A.J. and J.C.R. have backgrounds in behavioural science and psychology, and exercise science and health technology, respectively.
Group rapport was easily developed as all investigators were known to participants through clinical practice or ACRA membership. The rigour of this study was further addressed using several techniques. Two investigators (S.C. and A.J.) discussed coding and themes at length to provide analyst triangulation in order to reach consensus on a coding strategy.21,22 A third investigator (J.C.R.) was consulted where consensus was not reached. Initial results were presented back to participants at a subsequent ACRA member event, enabling member checking.18 Finally, the transferability of findings was increased through the inclusion of participants who represented multiple health disciplines, programme types, and geographic regions of Victoria.
Results
Sample characteristics
Thirty CR clinicians participated in the consultation, which went for 106 min. Demographics were provided by 17/30 participants (Table 1). Multiple disciplines (nursing n = 13, exercise physiology n = 3, and physiotherapy n = 1) and geographical settings (metropolitan n = 10, regional n = 4, and rural n = 3) were represented. Among the services in our sample, CR delivery during the peak of the pandemic was split between telehealth (n = 9) and hybrid in-person/telehealth (n = 7); only one programme retained in-person delivery.
Table 1.
Demographics of participants and cardiac rehabilitation programmes
|
n (%) |
|
|---|---|
| n = 17 (57) a | |
| Gender, female | 14 (82) |
| Profession | |
| Registered nurse | 13 (77) |
| Exercise physiologist | 3 (18) |
| Physiotherapist | 1 (6) |
| Location of programme | |
| Metropolitan | 10 (59) |
| Regional | 4 (24) |
| Rural | 3 (18) |
| Service type | |
| Public | 9 (53) |
| Private | 2 (12) |
| Community health | 7 (41) |
| Current alternative delivery CR service | |
| In-person only | 1 (6) |
| Telehealth/remote delivery only | 9 (53) |
| Combined face to face and telehealth | 7 (41) |
Not all participants completed the online demographic poll.
Thematic analysis
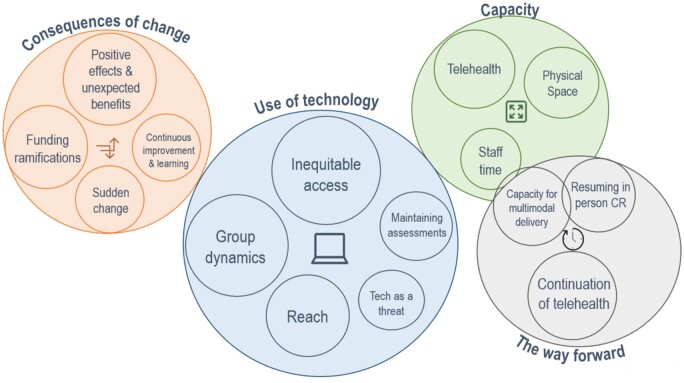
The inductive thematic analysis produced four key themes, each with several subthemes: (i) consequences of change; (ii) use of technology; (iii) capacity; and (iv) the way forward (Figure 1). Thematic analysis of themes and sub-themes is provided in Supplementary material online.
Figure 1.
Main themes (outer circles) and sub-themes (inner circles). Circle size denotes theme strength.
Consequences of change
A state of emergency was declared in Victoria on 16 March 2020, followed by Government restrictions on 25 March temporarily closing non-essential services including hospital outpatient services, such as CR.23 This sudden impact was felt by CR clinicians and patients, and can be described across four subthemes.
Sudden change
Remote delivery presents many challenges in addition to sudden and unexpected changes. Services described rapidly needing new telehealth equipment and training. Another service was required to relocate sites and change their model of care. Many clinicians described moving to telehealth very quickly:
We had actually tentatively planned on a project around telehealth at the very start of the year, obviously taking our time [but instead]… it was all practically rolled out within a very short space of time [when COVID-19 restrictions began]. Participant (P) 5
Continuous improvement and learning
This sudden and significant change from usual practice required continuous learning and developing new ways of working, with both clinicians and patients learning together:
It was just fly as you go and work it out and say to patients, ‘I've never done this before. I'm going to try and share my screen.' P1
There was evidence of clinicians regularly observing and learning within their services thus operating with some consideration of continuous improvement methodology despite sudden change secondary to COVID-19:
… I think the six-week service seems to be about right. We're getting more sophisticated, particularly we're putting it on a Webex [video conferencing] now, a… multidisciplinary team Webex for clients across sites to link into for standardised education. P9
Funding ramifications
Funding was discussed in two ways: first, there was clinician concern that health service administrators would prioritize crude cost comparisons over comprehensive cost-effectiveness when deciding whether to reallocate funding to in-person CR delivery:
So I think we’ve got to work really hard. [to get] back to being able to offer face-to-face as best practice in this area [it] is really important because [lower costs of telehealth mean] it actually appeals to the bean counters just to keep us virtual. P3
Second, there were challenges with funding in the private health system as health insurance did not fund remote CR delivery.
… not many health funds [were] actually supporting the telehealth system. So we were really in a real bind about that. P7
Here, clinicians advocated strongly for funding to support patients who had already commenced CR, and worked with insurers to accept these new models of care:
At [private hospital] we were directed that private [health] funds prefer video mode of telehealth but would accept telephone if this was not possible. P7
Positive effects and unexpected benefits
Among such substantial and sudden changes came unexpected benefits, particularly the ability of clinicians to deliver more individualized care.
Our clients definitely appreciated the 1:1 telephone follow-up and the more individualised program. P9
In some programmes CR uptake was increased:
…because during COVID times, there was nothing else happening in their lives. P3
This individualized care enabled relationships to be formed with patients who appreciated frequent clinical contact.
Use of technology
The use of technology to deliver care was the strongest theme of the consultation. Broadly, three tools were used: videoconferencing, mobile, and web-based tools.
Inequitable access
Clinicians discussed several challenges with patients accessing remote CR using technology with technology skills mentioned often. However, descriptions of technology challenges were often followed with work-around solutions, demonstrating the resourcefulness of the clinician–patient relationship in overcoming technology barriers:
… not everyone's able to use this platform. What we've done to get around it is we orient a son or daughter who's often been around during COVID times…. P3
Other access issues, including equipment, internet, and data access, were also identified:
Half of my clientele do not have an email address and they do not have home internet or home Wi-Fi. P2
Group dynamics
Differences in group dynamics between telehealth and in-person CR were also commonly discussed. Difficulty managing large group discussions on videoconference led to restrictions on participant numbers. Many clinicians noted that remote delivery reduced the capability to gather incidental patient information, such as non-verbal cues, psychosocial status, and information about home life that can guide support and referrals:
…That's where [in-person CR] I got to find out all of that extra stuff that you don't get in a phone call, and I could then refer them on to services that they needed. P2
Clinicians also perceived telehealth delivery changed group dynamics and lacked peer support, which is a critical element of CR:
‘When we're having a [online] group session, I didn't think they were as comfortable supporting each other…’. P3
Reach
Clinicians perceived that telehealth CR enabled expanded reach of their service:
Certainly the forced remote delivery mode has opened up thought on how to access participants who may not have engaged in a face-to-face program - due to geography, return to work, [or] other long standing access limitations. P8
Continuing the above theme, this may have come at the cost of social interaction and peer support.
COVID has really increased our ability to be flexible in the delivery of the CR program. We can cater better for all the individuals’ needs regarding focused education, individual exercises but it comes with a disadvantage of lack of social interaction. P14
Maintaining assessments
Another challenging aspect of remote CR delivery was undertaking physical assessments, such as physical assessments for exercise prescription and CR programme evaluation.
…the main issues there were about the exercise prescription… So prescribing exercise to a person that you haven't seen or assessed is probably the biggest challenge initially. P6
Clinicians were required to use proxy measures that they could implement via telehealth:
Well, the only outcome measure we couldn't do was the six-minute walk test, but I swapped that for a five-times sit and stand to show that there was improvement in fitness. P1
Technology as a threat
There was a brief but important discussion by a small group of participants about technology being a threat to the CR workforce. This was raised in two ways. The first was with regard to the use of pre-recorded materials:
…but I'm getting requests all the time, "Sorry, I'm going to miss tomorrow's session. Could you please record it so I can listen it later?" and… I wonder are we going to be redundant? P3
This may indicate that some patients are not as accountable or motivated to attend CR when they attend remotely. The other threat was through CR delivery platforms such as apps:
…my executive who've been approached by [a CR app] to take over our whole cardiac rehab… It's going to be cheaper for them than paying for [staff]… and then resetting up our gym again. P2
Capacity
Telehealth capacity
The issue of staff capacity and clinician–client ratios was highlighted many times during the consultation across different telehealth contexts. Increased documentation requirements and limited videoconference group capacity (due to challenges supervising patients and software user-caps) prompted members to ascertain safe working ratios with these new approaches:
Can I just ask everyone what your capacity is for the remote one-to-one groups? Based on my experience about 20 to 23 clients which we had consistently is probably enough. I can't manage any more I don't think the clinicians can either. P9
Participant 2 responded:
I have a limit of ten people in my groups, and I run two different sites … and what would normally take me three hours to do in a group session is actually taking me six and a half hours out of my day. So for me, trying to increase my capacity, which is what essentially we want to try and do, is just not physically possible.
In particular, many programmes that offered one-on-one telehealthcare acknowledged this inefficiency issue, which adversely affected waiting list time.
Staff time
The burden of remote CR delivery was exacerbated for some clinicians by pre-pandemic quality improvement projects:
But what's a challenge; we've just gone over to electronic medical record systems [EMR], and because these [telehealth] encounters create [government] funding, it takes longer to document the encounter [in the EMR system] than it does to perform the encounter with the patient. P3
Physical space
Physical space was the strongest capacity sub-theme. Due to physical-distancing measures, many gym spaces had been reallocated during the pandemic for other uses (clinical, clerical, and meal-break rooms), and members were uncertain whether CR space would be regained or replaced:
…Our gym's been taken over for chemotherapy… and our education meeting room is now a tea room. We physically don't have the space anymore to do it, and trying to reacquire that space again … is going to be difficult…. P2
The way forward
Finally, we asked clinicians about the way forward, specifically how their CR programmes would move to COVID-safe delivery.
Continuation of telehealth
The most prominent sub-theme was the desire to continue using telehealth to deliver CR. This was discussed in several ways; both to run in-person and telehealth concurrently as a hybrid model of CR and to continue telehealth to sustain increased reach:
…regardless of whether we get back face-to-face when COVID is a thing of the past, it'd be good to run … a virtual cardiac rehab program for the young return to work that have had a stent and run an accelerated virtual program from 5pm until 6pm. P3
Resuming in-person programmes
There was also a strong desire to resume in-person CR as participants felt this reflected best practice and restored elements missing from telehealth, such as peer support.
Capacity for multimodal delivery
While the desire to retain telehealth alongside existing in-person programmes in future was strong, the theme of capacity arose again. Clinicians flagged the difficulty of multimodal delivery with current staffing levels, as Participant 4 described:
…but I just don't see how I can do both [telehealth and in-person] from a staffing perspective with how much time remote and one-on-one telehealth takes. So it will be a big discussion with management for us as well as to how we'll move forward.
Several times, clinicians mentioned future discussions with management about the plan to move forward once COVID restrictions were lifted.
Applying the NASSS
Appling the NASSS framework to these data allows adoption of telehealth in CR to be assessed for barriers and enablers across multiple domains. We acknowledge the roll-out of remote CR was a very sudden response to changing requirements for outpatient care. However, by applying the NASSS to this initial and state-wide clinician experience, we can highlight domains that need to be focused on to enable sustainable large-scale adoption of the use of telehealth in CR. Our data indicate the greatest challenges are ‘the adopter system’, particularly for staff, and ‘the organization’, particularly for changes in team interactions and routines (Table 2).
Table 2.
NASSS domains, classifications, and rationales
| Domain/question | Classification and description | Theme(s)/example | ||
|---|---|---|---|---|
| Domain 1. The condition or illness | ||||
| 1A | What is the nature of the condition or illness? | Simple | Heart disease is well-characterized and well understood for the majority of conditions. | Not applicable |
| 1B | What are the relevant socio-cultural factors and comorbidities? | Complicated | Relevant sociocultural factors and comorbidities—must be factored into care plan and service model | Subthemes: Inequitable access, continuous improvement, and learning |
| Domain 2. The technology | ||||
| 2A | What are the key features of the technology? | Simple | Off the shelf and already in use. Freestanding, dependable. | Programmes used telephone calls and developed video conferencing software. One site used a developed, commercially available cardiac rehabilitation mobile application. |
| 2B | What kind of knowledge does the technology bring into play? | Not applicable | Not applicable in this instance as the aim of telehealth during COVID was to maintain CR and there was little or no remote monitoring that provided data for this subdomain. | Not applicable |
| 2C | What knowledge and/or support is required to use the technology? | Simple | A simple set of instructions were required. | Subtheme: Continuous improvement and learning |
| 2D | What is the technology supply model? | Simple | Technology used was generic, ‘plug and play’ | Pre-existing platforms and apps were used. |
| Domain 3. The value proposition | ||||
| 3A | What is the developer’s business case for the technology (supply-side value)? | Simple | Clear business case due to COVID-19 restrictions with strong chance of return on investment. | Subtheme: Reach |
| 3B | What is its desirability, efficacy, safety, and cost-effectiveness (demand-side value)? | Simple | Technology is desirable for patients, effective, safe, and cost-effective. | Subthemes: Reach, continuation of telehealth |
| Domain 4. The adopter system | ||||
| 4A | What changes in staff roles, practices, and identities are implied? | Complex | Existing staff must learn new skills and/or new staff be appointed and there is a threat to professional identity, values, or scope of practice; risk of job loss. | Theme: At capacity |
| Subthemes: continuous improvement and learning, tech as a threat | ||||
| 4B | What is expected of the patient (and/or immediate caregiver)—and is this achievable by, and acceptable to them? | Complicated | Routine tasks, e.g. log on, enter data, converse | Subthemes: continuous improvement and learning, inequitable access |
| 4C | What is assumed about the extended network of lay caregivers? | Complicated | Assumes caregiver will be available when needed | Subtheme: inequitable access (use of family) |
| Domain 5. The organization | ||||
| 5A | What is the organization’s capacity to innovate? | Complicated | Limited resources; suboptimal leadership and managerial relations, risk taking not encouraged | Subthemes: Continuous improvement and learning, telehealth capacity, staff time, capacity for multimodal delivery |
| 5B | How ready is the organization for this technology-supported change? | Complicated | Some work is needed to build shared vision, engage staff, enact new practices and monitor impact | Subthemes: Continuous improvement and learning, telehealth capacity, staff time, capacity for multimodal delivery, tech as a threat. |
| 5C | How easy will the adoption and funding decision be? | Complicated | Multiple organizations with partnership relationship; cost-benefit balance favourable or neutral; new infrastructure (e.g. staff roles, training, kit) can mostly be found from repurposing | Subthemes: funding ramifications, telehealth capacity, staff time, capacity for multimodal delivery |
| 5D | What changes will be needed in team interactions and routines? | Complex | New team routines or care pathways that conflict with established ones | Subthemes: Capacity for multimodal delivery, staff time, continuation of telehealth. |
| 5E | What work is involved in implementation and who will do it? | Complicated | Some significant work needed to build shared vision, engage staff, enact new practices, and monitor impact | Subthemes: Capacity for multimodal delivery, staff time, continuation of telehealth, tech as a threat. |
| Domain 6. The wider context | ||||
| 6A | What is the political, economic, regulatory, professional (e.g. medico legal), and sociocultural context for programme rollout? | Complicated | Financial and regulatory requirements being negotiated nationally; professional and lay stakeholders not yet committed | Subthemes: Funding ramifications, Tech as a threat |
| Domain 7. Embedding and adaption over time | ||||
| 7A | How much scope is there for adapting and coevolving the technology and the service over time? | Simple | Strong scope for adapting and embedding the technology as local need or context changes. | Subthemes: Continual improvement and learning, continuation of telehealth, capacity for multimodal delivery, funding ramifications. |
| 7B | How resilient is the organization to handling critical events and adapting to unforeseen eventualities? | Simple | Sense making, collective reflection, and adaptive action are ongoing and encouraged. | Subtheme: Continuous improvement and learning. |
| While there was some short-term adaption, this can only truly be assessed over time once changes have been embedded long term. | ||||
Adapted from Greenhalgh et al.14
Simple: straightforward, predictable, few components; Complicated: multiple interacting components or issues; Complex: dynamic, unpredictable, not easily disaggregated into constituent components.
Discussion
This study has provided an in-depth qualitative exploration of clinicians’ experience of rapid change in CR delivery due to the COVID-19 pandemic, which to our knowledge, is the first study of this kind. The use of telehealth for CR in Australia has previously been reported as very low (2.4%),5 whereas services have now moved rapidly to remote delivery methods to ensure service continuity. Cardiac rehabilitation clinicians (along with their patients) also demonstrated flexibility, resourcefulness, and a willingness to use new models of care.
Rapid transition to telehealth
Due to pandemic stay-at-home directives, our findings echo other rehabilitation and allied health experiences during this time, with the rapid uptake of ‘off the shelf’ telehealth tools24–27 (e.g. Zoom, Webex, Health Direct) and increased individual phone consultations.28 Telehealth tools mandated by health services—and, as others report, were platforms that organizations already had access to26—were not appraised as being optimal for the purpose of rehabilitation. Staff had to navigate new technologies with little training or support and adapt them for group CR delivery.25 Additionally in the private sector, remotely delivered CR was not often reimbursed by private health insurers27 which necessitated staff to negotiate reimbursement arrangements directly with health funds. This problem extends beyond Australia with Ghisi et al.24 identifying that 79% of respondents in their recent international survey were not reimbursed for alternative CR models.
Capacity was a significant theme running throughout our data. While remote CR delivery can offer more choice and flexibility for patients, it has currently significantly reduced programme capacity. This was due to documentation requirements, time taken to use telehealth, and the capacity limits of the number of people online (driven both by the platforms used and the nature of online group dynamics). Staff familiarity with telehealth tools and workflows should improve this issue over time. However, these challenges have also been experienced internationally.24
Conversely, more individualized care was delivered, particularly via telephone, which was the predominant modality used by CR clinicians in the UK.28 While patients appreciated individualized care, clinicians also believe it had to be balanced with programme demand and staff capacity, which has been a longstanding problem for CR programmes.29 For several years there have been calls to increase patient choices for CR delivery modalities.6,30,31 While the clinicians in our sample were eager to refine and continue to offer telehealth, many were uncertain how this can be done alongside in-person programmes with current staffing levels, highlighting the need to urgently review staffing levels and CR funding models.
Challenges for patients accessing and using telehealth were also identified in our data with similar problems reported internationally.24 Patient access to telehealth is creating a paradox of reach. While reach is extended, some patients are excluded due to a digital divide (i.e. lack of skills, equipment, data caps, or internet access).32,33 While digital inequities may reduce over time as more people become ‘tech savvy’ and internet access and quality expands, consideration is needed in the short term as telehealth may not be suitable for some age groups, geographical areas, or low socioeconomic groups. This reinforces assertions that remotely delivered CR should complement, not replace, traditional in-person delivery.34
Using the NASSS to guide long-term adoption
The NASSS framework clearly articulated challenges of remote CR delivery, especially within the adopter system (staff, patients, and caregivers) and organization domains which were classified as complicated or complex. The framework highlights technology-supported health programmes characterized by complicatedness can be difficult (but not impossible) to implement, while those characterized by complexity rarely become mainstream.14 However, we believe learnings from these initial and rushed experiences can reduce or resolve many of the complicated and complex issues. We also propose the telehealth tools used during this time may not have been fit for purpose or used to their full extent. This was understandable during the rapid COVID-19 transition, but it would be beneficial for CR clinicians to now identify how they want remotely delivered CR to contribute to their CR service, what tools are best suited to those purposes, and what investment is required.
Greenhalgh14 and others35 also recognize that for sustainable technology implementation, technology must be suited and adapted to individual environments. This is particularly relevant for CR in Australia where there is a lack of programme standardization. While there is now recommended standardized programme content,36 which was written to be delivery agnostic, this is not yet mandatory nor audited. However, it is recognized that CR programmes do need to be flexible to serve the many different patient populations across a large and diverse country such as Australia. Prior national surveys of Australian CR programmes revealed variability in programme settings, durations, exercise training, and staff professions, highlighting the need to match telehealth tools to specific organizational requirements and patient preferences.5,12
Strengths and limitations
Clinicians’ willingness to share experiences provided rich data and an in-depth picture of real-world experiences. We acknowledge that this was a large group consultation and was an opportunistic meeting of ACRA Victoria members which was time-efficient for clinicians during a pandemic and allowed them the chance to hear from many of their peers. We do not feel the large group hindered being able to hear from all participants as we heard directly from nearly all participants and they could contribute both by speaking and typing into the chat. However, we did not seek the experiences of patients directly. This should be considered in future research. We used robust methods of data analysis including analyst triangulation and member checking; but unfortunately, use of videoconference polling led to incomplete collection of demographic data. Finally, these results may not be generalizable to other states in Australia, or other countries. However, we did find many similarities with international reports.24,28
Implications for practice
Victorian CR clinicians indicated that they are eager to resume in-person CR delivery but would like to continue offering CR via telehealth. This desire for multimodal CR is in line with the opinion of Neubeck et al.37 that ‘telehealth has moved beyond an optional extra’. There is strong evidence that CR delivered via telehealth can provide equivalent outcomes as a traditional centre-based approach.6,38,39
Time now needs to be spent evaluating and refining telehealth technologies and the ways in which they are used in CR. Additionally protocols,37 and service provider guidelines and policies40 will need to be developed and be sensitive towards specific needs of programmes and patient cohorts. Funding also needs to be reviewed and secured.24,37 CR programmes have the ability to grow and significantly increase capacity with multimodal delivery; however, some additional funding investment is required in order to achieve this goal. While public funding of telehealth was made available through the pandemic via Medicare41 and has now been extended until the end of 202142 to support ongoing telehealth as the pandemic continues, funding also needs to be secured for long-term sustainability and private sector services.
Conclusion
Flexibility, resourcefulness, and dedication of CR clinicians achieved significant and rapid changes to CR delivery models amidst the unexpected COVID-19 pandemic. While there is appetite among clinicians to retain technology-enabled delivery within hybrid care models, there are many opportunities to refine rushed implementation approaches. Addressing these challenges could reduce friction, increase patient and clinician satisfaction, improve cost-efficiency, and economic viability. This could lead to increases in the number and diversity of people who receive high-quality CR and ultimately to improved patient outcomes.
Supplementary material
Supplementary material is available at European Journal of Cardiovascular Nursing online.
Supplementary Material
Acknowledgements
Thank you to the remaining members of the ACRA Victoria Committee who supported this study: Carmel Bourne, Cate Stevens, Katrien Janssen, Linda Macaulay, and Steve Foulkes. We also acknowledge and thank Robyn Sheppard for her assistance facilitating the ethics approval. Thank you to all participants who supported and took part in this research.
Funding
No funding was provided for this study. S.C. and J.C.R. are funded by National Heart Foundation of Australia Postdoctoral Fellowships (104860 and 102585). E.J.H. was supported by a National Heart Foundation of Australia Future Leader Fellowship (102536).
Conflict of interest: The authors declare that there is no conflict of interest and this study has been undertaken with approval from the membership of the Australian Cardiovascular Health & Rehabilitation Association (ACRA) Victoria and the ACRA National Committee. All authors are members of the ACRA Victoria Committee and S.C., E.J.H., and A.J. are members of the ACRA National Committee.
Data availability
The data, according to our analysis, is available as a Supplementary material online, File with this article. Extended consent was not sought from our participants to use data for future research.
References
- 1. Anderson L, Thompson DR, Oldridge N, Zwisler A-D, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016;1:CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chew DP, Scott IA, Cullen L, French JK, Briffa TG, Tideman PA, Woodruffe S, Kerr A, Branagan M, Aylward PEG; NHFA/CSANZ ACS Guideline 2016 Executive Working Group. National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Australian Clinical Guidelines for the Management of Acute Coronary Syndromes 2016. Heart Lung Circ 2016;25:895–951. [DOI] [PubMed] [Google Scholar]
- 3. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney M-T, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen M-L, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cowie A, Buckley J, Doherty P, Furze G, Hayward J, Hinton S, Jones J, Speck L, Dalal H, Mills J; British Association for Cardiovascular Prevention and Rehabilitation (BACPR). Standards and core components for cardiovascular disease prevention and rehabilitation. Heart 2019;105:510–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jackson AC, Higgins RO, Murphy BM, Rogerson M, Le Grande MR. Cardiac rehabilitation in Australia: a brief survey of program characteristics. Heart Lung Circ 2018;27:1415–1420. [DOI] [PubMed] [Google Scholar]
- 6. Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol 2015;22:35–74. [DOI] [PubMed] [Google Scholar]
- 7. Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart 2016;102:1183–1192. [DOI] [PubMed] [Google Scholar]
- 8. Jin K, Khonsari S, Gallagher R, Gallagher P, Clark AM, Freedman B, Briffa T, Bauman A, Redfern J, Neubeck L. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs 2019;18:260–271. [DOI] [PubMed] [Google Scholar]
- 9. Update on Coronavirus Measures. Prime Minister of Australia. https://www.pm.gov.au/media/update-coronavirus-measures-24-March-2020 (16 June 2021).
- 10. CR Directory – ACRA. https://www.acra.net.au/cr-services/cr-directory/ (12 April 2021).
- 11. National Heart Foundation of Australia. Interactive Heart Map Australia. The Heart Foundation. Interactive Heart Map Australia. https://www.heartfoundation.org.au/health-professional-tools/interactive-heart-map-australia (1 October 2021).
- 12. Abell B, Glasziou P, Briffa T, Hoffmann T. Exercise training characteristics in cardiac rehabilitation programmes: a cross-sectional survey of Australian practice. Open Heart 2016;3:e000374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–357. [DOI] [PubMed] [Google Scholar]
- 14. Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A'Court C, Hinder S, Fahy N, Procter R, Shaw S. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 2017;19:e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. ACRA – Australian Cardiovascular Health and Rehabilitation Association. https://www.acra.net.au/ (1 February 2021).
- 16. Rickham PP. Human experimentation. Code of ethics of the world medical association. Declaration of Helsinki. Br Med J 1964;2:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 18. Grbich C. Qualitative Research in Health. NSW: Allen & Unwin; 1999. [Google Scholar]
- 19. Hansen EC. Successful Qualitative Health Research: A Practical Introduction. NSW: Allen & Unwin; 2006. [Google Scholar]
- 20. Hertz R. Reflexivity & Voice. United States of America: SAGE Publications, Inc; 1997. [Google Scholar]
- 21. Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park, CA: SagePublications. [Google Scholar]
- 22. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 2017;16:160940691773384. [Google Scholar]
- 23. corporateName=Commonwealth Parliament; address=Parliament House C. COVID-19: A Chronology of State and Territory Government Announcements (up until 30 June 2020), https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Chronologies/COVID-19StateTerritoryGovernmentAnnouncements (2 August 2021).
- 24. Ghisi G. L D M, Xu Z, Liu X, Mola A, Gallagher R, Babu AS, Yeung C, Marzolini S, Buckley J, Oh P, Contractor A, Grace SL. Impacts of the COVID-19 pandemic on cardiac rehabilitation delivery around the world. Glob Heart 2021;16:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Malliaras P, Merolli M, Williams CM, Caneiro JP, Haines T, Barton C. ‘It’s not hands-on therapy, so it’s very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract 2021;52:102340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Signal N, Martin T, Leys A, Maloney R, Bright F. Implementation of telerehabilitation in response to COVID-19: lessons learnt from neurorehabilitation clinical practice and education. NZ J Physiother 2020;48:117–126. [Google Scholar]
- 27. Bennell KL, Lawford BJ, Metcalf B, Mackenzie D, Russell T, van den Berg M, Finnin K, Crowther S, Aiken J, Fleming J, Hinman RS. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: a mixed-methods study. J Physiother 2021;67:201–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. O'Doherty AF, Humphreys H, Dawkes S, Cowie A, Hinton S, Brubaker PH, Butler T, Nichols S. How has technology been used to deliver cardiac rehabilitation during the COVID-19 pandemic? An international cross-sectional survey of healthcare professionals conducted by the BACPR. BMJ Open 2021;11:e046051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pack QR, Squires RW, Lopez-Jimenez F, Lichtman SW, Rodriguez-Escudero JP, Zysek VN, Thomas RJ. The current and potential capacity for cardiac rehabilitation utilization in the United States. J Cardiopulm Rehabil Prev 2014;34:318–326. [DOI] [PubMed] [Google Scholar]
- 30. Higgins RO, Murphy BM, Le Grande MR, Parkinson A, Worcester MUC, Goble AJ. Expressed preferences for health education of patients after percutaneous coronary intervention. Eur J Prev Cardiol 2005;12:572–579. [DOI] [PubMed] [Google Scholar]
- 31. Higgins RO, Rogerson M, Murphy BM, Navaratnam H, Butler MV, Barker L, Turner A, Lefkovits J, Jackson AC. Cardiac rehabilitation online pilot: extending reach of cardiac rehabilitation. J Cardiovasc Nurs 2017;32:7–13. [DOI] [PubMed] [Google Scholar]
- 32. Fang ML, Canham SL, Battersby L, Sixsmith J, Wada M, Sixsmith A. Exploring privilege in the digital divide: implications for theory, policy, and practice. Gerontologist 2019;59:e1–e15. [DOI] [PubMed] [Google Scholar]
- 33. Astley CM, Clarke RA, Cartledge S, Beleigoli A, Du H, Gallagher C, Millington S, Hendriks JM. Remote cardiac rehabilitation services and the digital divide: implications for elderly populations during the COVID19 pandemic. Eur J Cardiovasc Nurs 2021;20:521–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maddison R, Rawstorn JC, Stewart RAH, Benatar J, Whittaker R, Rolleston A, Jiang Y, Gao L, Moodie M, Warren I, Meads A, Gant N. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart 2019;105:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci 2013;8:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cartledge S, Thomas E, Hollier K, Maddison R. Development of standardised programme content for phase II cardiac rehabilitation programmes in Australia using a modified Delphi process. BMJ Open 2019;9:e032279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Neubeck L, Hansen T, Jaarsma T, Klompstra L, Gallagher R. Delivering healthcare remotely to cardiovascular patients during COVID-19: a rapid review of the evidence. Eur J Cardiovasc Nurs 2020;19:486–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Knudsen MV, Petersen AK, Angel S, Hjortdal VE, Maindal HT, Laustsen S. Tele-rehabilitation and hospital-based cardiac rehabilitation are comparable in increasing patient activation and health literacy: a pilot study. Eur J Cardiovasc Nurs 2020;19:376–385. [DOI] [PubMed] [Google Scholar]
- 39. Ramachandran HJ, Jiang Y, Tam WWS, Yeo TJ, Wang W. Effectiveness of home-based cardiac telerehabilitation as an alternative to Phase 2 cardiac rehabilitation of coronary heart disease: a systematic review and meta-analysis. Eur J Prev Cardiol 2021. doi: 10.1093/eurjpc/zwab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yeo TJ, Wang Y-TL, Low TT. Have a heart during the COVID-19 crisis: making the case for cardiac rehabilitation in the face of an ongoing pandemic. Eur J Prev Cardiol 2020;27:903–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tanne JH, Hayasaki E, Zastrow M et al. COVID-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ 2021. doi: 10.1136/bmj.m1090. [DOI] [PubMed] [Google Scholar]
- 42. Health AGD of Universal Telehealth extended through 2021. Australian Government Department of Health, 2021. https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/universal-telehealth-extended-through-2021 (2 August 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data, according to our analysis, is available as a Supplementary material online, File with this article. Extended consent was not sought from our participants to use data for future research.