Abstract
Objective
To better understand rheumatology patient and clinician pandemic-related experiences, medical relationships and behaviours in order to help identify the persisting impacts of the COVID-19 pandemic and inform efforts to ameliorate the negative impacts and build upon the positive ones.
Methods
Rheumatology patients and clinicians completed surveys (patients n = 1543, clinicians n = 111) and interviews (patients n = 41, clinicians n = 32) between April 2021 and August 2021. A cohort (n = 139) of systemic autoimmune rheumatic disease patients was also followed up from March 2020 to April 2021. Analyses used sequential mixed methods. Pre-specified outcome measures included the Warwick–Edinburgh Mental wellbeing score (WEMWBS), satisfaction with care and healthcare behaviours.
Results
We identified multiple ongoing pandemic-induced/increased barriers to receiving care. The percentage of patients agreeing they were medically supported reduced from 74.4% pre-pandemic to 39.7% during-pandemic. Ratings for medical support, medical security and trust were significantly (P <0.001) positively correlated with patient WEMWBS and healthcare behaviours, and decreased during the pandemic. Healthcare-seeking was reduced, potentially long-term, including from patients feeling ‘abandoned’ by clinicians, and a ‘burden’ from government messaging to protect the NHS. Blame and distrust were frequent, particularly between primary and secondary care, and towards the UK government, who <10% of clinicians felt had supported clinicians during the pandemic. Clinicians’ efforts were reported to be impeded by inefficient administration systems and chronic understaffing, suggestive of the pandemic having exposed and exacerbated existing healthcare system weaknesses.
Conclusion
Without concerted action—such as rebuilding trust, improved administrative systems and more support for clinicians—barriers to care and negative impacts of the pandemic on trust, medical relationships, medical security and patient help-seeking may persist in the longer term.
Trial registration
This study is part of a pre-registered longitudinal multi-stage trial, the LISTEN study (ISRCTN-14966097), with later COVID-related additions registered in March 2021, including a pre-registered statistical analysis plan.
Keywords: rheumatology, patient–clinician interactions, healthcare behaviours, COVID-19 pandemic, telemedicine, chronic diseases, mental health, medical security, NHS, healthcare systems, trust
Rheumatology key messages.
The pandemic exposed and exacerbated existing healthcare system weaknesses, increasing barriers to rheumatology patients accessing care.
Many clinicians reported that the UK government’s pandemic management left them feeling unsupported, undermined and/or endangered.
Enduring impacts are likely to include less trusting medical relationships and reduced patient healthcare-seeking and symptom-reporting.
Introduction
In addition to the devastatingly high global rates of mortality and morbidity directly attributable to COVID-19 infection, the pandemic has had a major impact on the delivery of healthcare for patients with chronic diseases [1]. This has included severe disruption to rheumatology care in the UK [2] and elsewhere [3], with appointments cancelled [4] or switched to telemedicine [5], problems accessing urgent care [6] and the fear of COVID-19 deterring hospital attendance [7]. In addition to the increased risk from COVID-19 in some rheumatology patient groups [8], pandemic-related disruptions to routine and emergency care were found to have had adverse impacts on the mental and physical health of rheumatology patients [6, 9] and left many feeling medically abandoned [6, 10]. These disruptions—including clinicians needing to provide COVID care while attempting to maintain normal care for their patients [11]—may also have contributed to the adverse impacts of the pandemic on clinicians’ mental health [12, 13]. These healthcare changes could have had significant impacts on rheumatology patient–clinician relationships [6]; and pre-pandemic studies [14] suggest that changes in patient–clinician relationships can influence rheumatology patient health-related behaviours [14, 15], the quality of healthcare and health outcomes [16]. While it is too soon to determine whether any such pandemic-related changes and impacts will be long-term, this study sought to achieve greater understanding of patient and clinician relationships, experiences and behaviours to help identify, and thus inform efforts to minimize, any persisting adverse impacts of the pandemic.
Methods
Participants and design
This mixed-methods study is part of a pre-registered longitudinal multi-stage trial (ISRCTN-14966097). Surveys were disseminated to three groups of participants via the online survey platform, Qualtrics:
A cohort of systemic autoimmune rheumatic disease (SARD) patients completed surveys in March 2020, June 2020 and March 2021.
A larger group of patients with a broader range of rheumatological diseases completed surveys in April 2021, through multiple rheumatology charities and online support groups.
Rheumatology clinicians completed a similar online survey in May/June 2021, through professional networks, including the British Society for Rheumatology (BSR).
Interviewees were purposely selected to ensure a range of demographic, disease and experience characteristics to inform, explore and further explain quantitative findings. Interviews were conducted by M.S., an experienced behavioural science researcher; lasted for ∼1 h; and were transcribed verbatim. Interviewing continued until thematic saturation (the point at which additional interviews did not provide significant new relevant insights or contradict the conclusions drawn from earlier interviews) was reached.
Inclusion criteria: patients: age ≥18 years and reporting a diagnosis of an autoimmune inflammatory rheumatological condition on their clinic letters. Clinicians: UK-based rheumatology clinicians and general practitioners (GPs). Ethical approval was obtained through the Cambridge Psychology Research Committee. Electronic informed consent was taken at the start of the survey and/or verbally recorded prior to interviews.
The surveys included the validated Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS) [17] and questions on: pre- and during-pandemic perceptions of trust, satisfaction with care and healthcare behaviours. The majority of questions used 5-point Likert-type scales. Medical security was measured on a scale of 0–100 with 0 signifying ‘completely medically abandoned’ (using patients’ terminology from earlier studies) and 100 signifying ‘completely medically secure’.
Analysis
Data collection was sequential, with quantitative and qualitative data then combined, analysed and presented together. SPSS v.26 was used to analyse the quantitative data. Correlations were calculated using Pearson’s or Spearman’s rank, depending on normality of distribution. T-tests were used to ascertain statistical significance of mean differences between and within groups. The qualitative data was analysed using thematic analysis [18] and NVivo12 for managing and coding data. A detailed description of methods, limitations and the criteria for reporting qualitative research (COREQ) [19] are included in Supplementary Data S1, available at Rheumatology online. Briefly, the stages of analysis involved in our qualitative research involves an inductive-deductive process, including: (i) immersion in the data where transcripts and subsequent coded sections are repeatedly read and discussed by multiple team members to improve reliability, and ensure multiple perspectives and possible interpretations are represented; (ii) a coding (classification) scheme is developed, trialled, discussed and refined, and each line of qualitative data is coded; and (iii) participant extracts for each code are combined. The key themes emerge directly from the data and team discussions, including with multiple patients and clinicians.
Consideration of deviant cases [20], member checking [21], triangulation of quantitative and qualitative results [22] and multiple perspectives were conducted to improve validity.
Ethical approval
Ethical approval was obtained through the Cambridge Psychology Research Committee: PRE.2019.099: approval for original trial; PRE.2020.089: approval for COVID-19-related additions and amendments.
Results
The results reported are from the rheumatology-patient survey (n = 1543) and interviews (n = 41), longitudinal cohort (n = 139), and clinician survey (n = 111) and interviews (n = 32). The majority of patients and clinicians were females residing in England (Table 1). Participant information for the longitudinal cohort is provided in Supplementary Data S1 (available at Rheumatology online). ‘During-pandemic’ refers to data collected from mid-March 2020 to August 2021.
Table 1.
Participant characteristics
| Characteristic | Patient survey (n = 1543) | Patient interviews (n = 41) | Clinician survey (n = 111) | Clinician interviews (n = 32) |
|---|---|---|---|---|
| Age | ||||
| <30 | 273 (18%) | 5 (12%) | 5 (5%) | 0 |
| 30–39 | 302 (20%) | 5 (12%) | 19 (17%) | 10 (31%) |
| 40–49 | 460 (30%) | 12 (29%) | 39 (35%) | 5 (16%) |
| 50–59 | 340 (22%) | 9 (22%) | 37 (33%) | 13 (41%) |
| 60+ | 168 (11%) | 10 (24%) | 11 (10%) | 4 (13%) |
| Gender | ||||
| Female | 1464 (95%) | 36 (88%) | 77 (69%) | 14 (44%) |
| Male | 71 (4%) | 5 (12%) | 34 (31%) | 18 (56%) |
| Other/undisclosed | 8 (1%) | 0 | 0 | 0 |
| Country/region | ||||
| England | 1196 (78%) | 25 (61%) | 87 (78%) | 25 (78%) |
| Scotland | 139 (9%) | 4 (10%) | 13 (11%) | 3 (9%) |
| Wales | 78 (5%) | 8 (20%) | 9 (8%) | 2 (6%) |
| N. Ireland | 48 (3%) | 2 (5%) | 2 (2%) | 2 (6%) |
| USA or Canada | 37 (2%) | 1 (2%) | 0 | 0 |
| Europe | 20 (1%) | 1 (2%) | 0 | 0 |
| Other | 25 (2%) | 0 | 0 | 0 |
| Disease | ||||
| Lupus | 497 (32%) | 12 (29%) | ||
| Inflammatory arthritis | 472 (31%) | 14 (34%) | ||
| Sjögren’s | 128 (8%) | 4 (10%) | ||
| Systemic sclerosis | 128 (8%) | 3 (7%) | ||
| PMR | 57 (4%) | 2 (5%) | ||
| Vasculitis | 53 (3%) | 1 (2%) | ||
| UCTD | 50 (3%) | 3 (7%) | ||
| MCTD or two or more inflammatory rheumatic diseases | 104 (7%) | 2 (5%) | ||
| Other inflammatory rheumatic disease | 53 (3%) | 0 | ||
| Time since diagnosis | ||||
| <1 year | 96 (6%) | 3 (7%) | ||
| 1–2 years | 187 (12%) | 6 (15%) | ||
| 3–5 years | 316 (21%) | 7 (17%) | ||
| 6–9 years | 293 (19%) | 11 (27%) | ||
| 10+ years | 645 (42%) | 13 (32%) | ||
| Unsure or missing | 6 (<1%) | 1 (2%) | ||
| Clinician role | ||||
| Rheumatology consultant | 72 (65%) | 15 (47%) | ||
| Rheumatologist registrar | 13 (12%) | 5 (16%) | ||
| Rheumatology nurse | 19 (17%) | 6 (19%) | ||
| GP | 0 (not surveyed) | 5 (16%) | ||
| Other speciality | 7 (6%) | 1 (3%) |
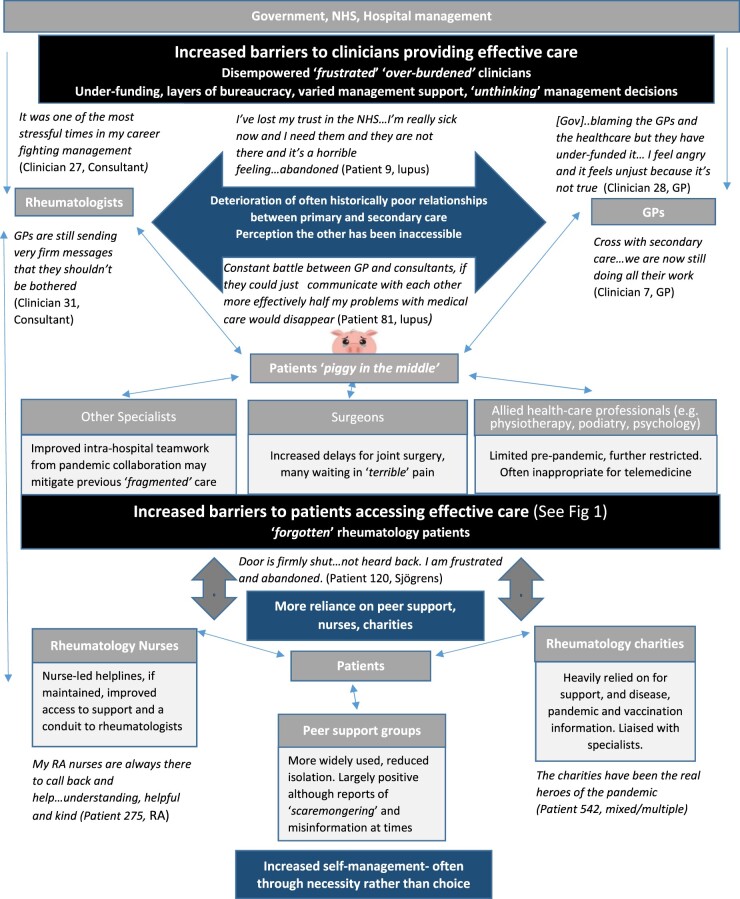
Pandemic-related barriers to and facilitators of effective care
Both patients and clinicians reported pandemic-related barriers and increased pre-existing barriers to rheumatology patients seeking and/or receiving effective care (Fig. 1). These included administrative barriers, such as non-responsive helplines, and patient-related barriers, including healthcare-avoidance. Administrative barriers were frequently encountered by patients, often without clinicians’ knowledge: ‘Counted and…tried 121 times to get through to GPs’ (Patient 1128, RA). In the large-scale survey (n = 1543), 74.4% of patients agreed that they were medically supported pre-pandemic, reducing to 39.7% during-pandemic, and only 47.9% felt they would be medically supported during the year following the survey (April 2021–April 2022). Facilitators to accessing care were much less commonly mentioned and were generally the opposite of the barriers (e.g. responsive helplines).
Fig. 1.
Pandemic-induced/increased barriers and facilitators to rheumatology patients receiving appropriate and timely care
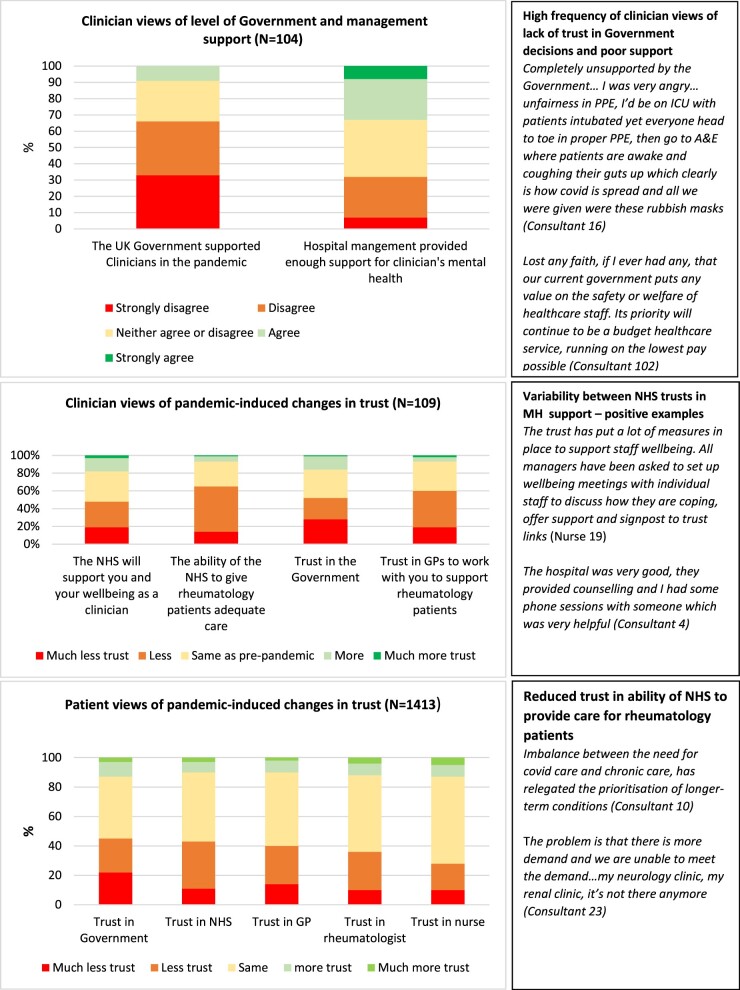
Altered healthcare relationships
Medical relationships at all levels altered during the pandemic (Fig. 2). Many participants expressed concern over the lack of face-to-face contact and the movement towards telemedicine. Several clinicians stated that telemedicine had greatly reduced their job satisfaction, was ‘soul-destroying’ (Clinician 7, GP) or like working in a ‘call centre’ (Clinician 23, Consultant) and/or had created additional barriers in relationship building.
Fig. 2.
Pandemic-induced/increased changes in support and relationships
Note: Words/phrases in italics are direct quotes from participants.
Patient–clinician relationships
Patients and clinicians greatly appreciated the other having shown concern for their respective pandemic experiences; and some felt that this had strengthened their relationship. A pre-existing secure medical relationship was often discussed as providing ongoing security, particularly when clinicians responded quickly in a crisis and/or spontaneously contacted patients. There was a moderately positive correlation of r = 0.43 (P =0.001) between feeling medically secure before and during the pandemic.
Clinician and patient mean ratings of patient security in their rheumatology team dropped to ∼50 (out of 100) during the pandemic. Clinicians’ estimate of patients’ pre-pandemic medical security (78.4) was significantly higher than patient ratings (69.5) (MD =−8.97, P <0.001, 95% CI =−13.66, −4.27). Experience of pandemic care was highly variable between participants. Worsening medical security levels were found in 67% of patients, although 18% of patients reported increased medical security during the pandemic. Many expressed gratitude towards the NHS and/or individual clinicians:
Grateful for the doctors who have cared for me throughout this scary pandemic. They truly are heroes (Patient 777, vasculitis)
Patients sharing their growing frustration at continuing reduced care was said by clinicians to be understandable given that many patients felt ‘abandoned’ or ‘forgotten’; but was also reported as ‘depressing’ or ‘demoralising’ for clinicians struggling to meet competing demands for COVID-19 and rheumatological care.
Rheumatology nurses were the clinician group patients trusted the most, and received the least pandemic-induced reduction (<30%) in patient trust (Fig. 3), compared with ∼40% of patients having reduced trust in their rheumatologist, GP, their government and the NHS. Patients frequently expressed insecurity about future access to prompt care, especially during major flares. Widespread UK government and media messaging to ‘protect the NHS’ not only deterred help-seeking at the time, but reduced longer-term trust and potentially future help-seeking:
Fig. 3.
Clinicians’ and patients’ pandemic-induced changes to trust (quotes in italics)
I don’t trust my GP or surgery after being told I shouldn’t seek out help for my chronic disease during the pandemic (Patient 504, vasculitis)
The psychological impact of being unable to access care and feeling ‘abandoned’ were frequently discussed by both clinicians and patients as likely to adversely impact medical relationships in the longer term:
The feeling of abandonment will remain for longer than the memories of the chaos of Covid …we have a lot of work to do to re-build trust (Clinician 83, Consultant)
Primary–secondary care relationships
Clinician interviews indicated that relationships between primary and secondary care were historically poor and had deteriorated further during the pandemic. Over 40% of rheumatology clinicians had low levels of trust in GPs to work with them to support rheumatology patients, and almost 60% had less trust than before the pandemic (Fig. 3). GP interviewees discussed similar problems with secondary care:
Our local rheumatology has refused to accept referrals, deflected wherever possible and been very condescending (Clinician 6, GP)
Although empathy was sometimes expressed for the other party, both GPs and rheumatologists more commonly expressed resentment that they had taken on the other’s work during the pandemic and felt that the other was blocking access. Many clinicians stated that they had frequently dealt with symptoms outside their area of expertise due to sympathy for the patient’s difficulties in accessing the ‘correct’ channels of support. Clinicians being open with patients about their frustrations in taking on primary/secondary roles increased feelings of being a ‘burden’ and ‘rejection’ in some patients. Concerns were expressed by both patients and clinicians that patients were sometimes left with no medical support due to non-response and/or clinicians ‘passing the buck’:
Heartbroken by the abandonment and lack of empathy I was given by both the GP and rheumatology department…rheumatology department [said] that a UTI wasn’t their problem. Couldn’t get through to GP and was left with an infection and no antibiotics (Patient 1412, lupus)
Clinician—hospital management/government relationships
Clinician and patient trust in the UK government was low and declined further during the pandemic (Fig. 3); and <10% of clinicians agreed that the UK government had supported clinicians during the pandemic. Government decisions, particularly regarding delays to lockdown, and failure to provide appropriate personal protective equipment (PPE), impacted heavily on clinicians’ trust, and contributed to feelings of being unsupported, under-valued and put at unnecessary risk:
We need to retain doctors by giving them enough funding, not burning them out and not killing them by not giving them PPE (Clinician 28, GP)
Clinician mental health support was reported as being promoted by most hospital managements. However, some of the most senior clinicians reported additional stress as a result of disempowerment and having to ‘battle’ management:
We weren’t allowed to change anything locally…that really made me stressed, horribly stressed because I’ve got a position of responsibility but I can’t enable or enact change. (Clinician 13, Consultant)
Clinicians also discussed concerns about inappropriate ‘unthinking’ management target-setting for telemedicine:
… blanket decision…not based on clinical need or clinical reasoning on the number of patients that virtual appointments would disadvantage (Clinician 1, Registrar)
Intra-hospital/practice relationships
Teamwork, respect and a greater awareness of the importance of all hospital staff were apparent. Multiple narratives of support from peers and clinician managers, and increased camaraderie, were recounted:
It was an incredibly good team-working environment, really exemplary of what it should be…very supportive…some perfect MDTs…learnt a huge amount clinically…made some really close friends (Clinician 11, Registrar)
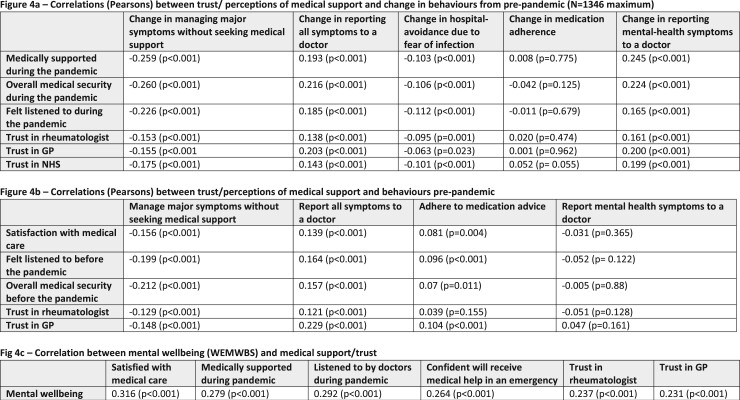
Change in behaviours
Patient measures of trust and satisfaction with care were significantly, albeit weakly, correlated with multiple patient behaviours (Fig. 4a and b). For example, ‘Feeling medically supported’ during the pandemic was significantly correlated with changes in reporting mental health symptoms (r = 0.245, P <0.001).
Fig. 4.
Correlations between medical support, behaviours and mental wellbeing
(a) Correlations (Pearsons) between trust/perceptions of medical support and change in behaviours from pre-pandemic (n = 1346 maximum). (b) Correlations (Pearsons) between trust/perceptions of medical support and behaviours pre-pandemic. (c) Correlation between mental wellbeing (WEMWBS) and medical support/trust. Note: WEMWBS scores are from 14 to 70, medical security used a scale of 0–100, and all other categories of trust and satisfaction used 5-point Likert-scales. Changes to behaviours (Fig. 4a) options were: 1 – much less than pre-pandemic; 2 – less; 3 –same as pre-pandemic; 4 – more; and 5 – much more than pre-pandemic. Pre-pandemic behaviour response options (Fig. 4b) were frequency-based: 1 – never; 2 – rarely; 3 – sometimes; 4 – usually; and 5 – always.
There was no correlation between during-pandemic support and medication adherence, although a minority reported in interviews that they had adjusted their medication due to lack of clinician availability or fear of COVID-19. Hospital avoidance was influenced by fear of infection, but much more commonly by feeling like a ‘burden’ and/or ‘guilty’ about bothering busy clinicians:
Concerned for the doctors and nurses’well-being. Although I have full trust in my rheumatology team, I am very aware of their workloads and will try not to report problems to them (Patient 662, axial spondyloarthritis)
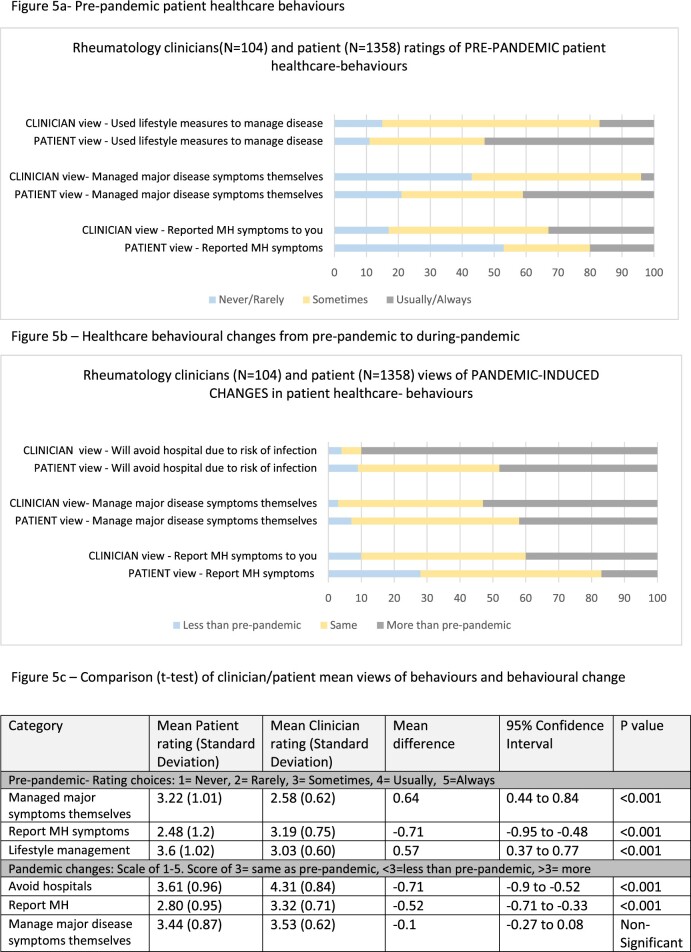
Mental health symptoms went unreported pre-pandemic significantly (P <0.001) more often than clinicians realized (Fig. 5). The percentage of patients never/rarely reporting mental health symptoms was assessed as <20% by clinicians, yet 50% of patients put themselves in this category. Time constraints, backlogs and increased telemedicine were felt to have further reduced both the eliciting and unprompted disclosure of mental-health symptoms:
Fig. 5.
Clinician and patient views of healthcare behaviours
(a) Pre-pandemic patient healthcare behaviours. (b) Healthcare behavioural changes from pre-pandemic to during-pandemic. (c) Comparison (t test) of clinician/patient mean views of behaviours and behavioural change. Note: Patients were asked to respond for their individual behaviours, clinicians were asked for their perceptions of rheumatology patient behaviour on average. MH = mental health.
I have been to some very dark places this last year and haven’t been able to admit it to myself let alone my doctors … no-one can pick that up on the telephone (Patient 132, lupus)
Several clinicians identified with regret that they had purposely shut down conversations about mental health difficulties on account of insufficient time/energy during the pandemic. A concerning patient response among those failing to obtain emergency support, including those who had tried to report suicidal feelings and severe flares, was that they were much less willing to report symptoms again:
I would never try and report it or ask them for help again…they just ignored me…you stop asking…it makes me feel worried for my life (Patient 136, mixed/multiple)
Charities and online peer-support groups were widely praised for having fulfilled multiple roles such as advice, moral support and reducing isolation. Improved self-management, including diet, pacing and exercise was reported as a positive by some. However, self-management of major symptoms—including ‘joint erosions’ and ‘kidney failure’—was in many instances felt to have been due to ‘abandonment’ rather than choice.
Some clinicians reported an increase in their understanding and empathy due to their pandemic experiences:
I’ve got empathy in ways I didn’t have before in that when you have actually thought about that for yourself in that I’ve got a disease and it might involve me dying (Clinician 4, Consultant)
Other clinicians reported increased time pressure and compassion fatigue. Many patients felt that clinician empathy and listening had decreased during the pandemic, often surmising that it was due to telemedicine and/or pandemic-induced stress:
My rheumy is clearly changed in the way he listens, empathises … maybe due to his Covid experiences … exhausted, overworked, burnt out … given up on me when I need him most … abandoned … feel hopeless (Patient 1132, mixed/multiple)
These were correlated with each row category; for example, increased trust in GP and rheumatologists was associated with more reporting of symptoms, less self-management of major symptoms, less avoidance of hospitals due to infection fears and not associated with any change in medication adherence.
Impact on patient and clinician health
The health impacts from pandemic-induced delays in seeking/receiving rheumatology care were reported to have ‘turned back the clock 20 years … ischaemic limbs, digital infarction’ (Clinician 2, Consultant) and appear on occasions to have contributed to potentially avoidable deaths:
Came in pretty darned ill… [in May 2020] we hadsixinpatients with very active lupus and two of them died very sadly and I don’t think they would have died if they’d come in earlier (Clinician 25, Consultant)
The vast majority of clinicians attributed the late presentations largely to patients avoiding seeking help due to fear of infection, and hospital avoidance was significantly (P < 0.001) over-estimated by clinicians. Almost 90% of clinicians thought patients were avoiding hospitals more than pre-pandemic due to fear of infection, compared with <50% of patients reporting that their own behaviour was more hospital-avoidant than pre-pandemic because of infection fears (Fig. 5). In addition, only 19% of patients reported that they had cancelled/not attended medical appointments (from March 2020 to March 2021) due to fear of COVID-19, yet 72% reported at least one appointment cancelled by hospital/surgery staff, and qualitative data revealed frequent difficulties accessing timely medical help in an emergency. Multiple patients detailed experiencing their ‘worst flare ever’, and some sustained irreversible damage:
I feel forgotten…Lack of care has caused bone deformity that I will have to live with for the rest of my life. Is it selfish to want care? I don’t know, all I know is I am suffering and I am scared and sad (Patient 686, RA)
Although many patients reported reduced mental health, and within the cohort antidepressants had been started (10%) or increased (8%), there were no statistically significant changes in mean mental wellbeing (WEMWBS) scores between surveys in March 2020, June 2020 and March 2021. Patient WEMWBS scores were significantly (P <0.001) correlated with multiple measures of medical support and trust (Fig. 4c), including feeling listened to by doctors during the pandemic (r = 0.292) and trust in rheumatologist (r = 0.237).
The pandemic also posed a major challenge to the mental health of our study clinician participants. Many expressed a similar fear of infection to patients, particularly in the early days with regard to putting their families at risk: ‘We didn’t know if it would kill our children’ (Clinician 7, GP). Mental wellbeing scores did not significantly differ between those who were re-deployed (∼50% of clinicians) to care for COVID patients and those who were not, although several of those re-deployed spoke emotively of the fear they experienced:
I was scared…everyone will tell you who went to the front line that they are going to stay with us…pictures in your head of the people in the ward dying…you have nightmares, horrible nightmares…PTSD, I was having flashbacks. (Clinician 4, Consultant)
Although a minority of clinicians had thrived on the pandemic challenges, many clinicians were extremely demoralized, several reported feeling ‘burntout’ and discussed how they may leave the profession. Deaths, long-COVID and suicides among clinician colleagues were discussed. Almost a quarter (23%) of clinicians felt that their mental health would be damaged in the long term from their pandemic experiences, although 28% strongly disagreed they would have any lasting mental health damage.
Discussion
Our findings indicate that the COVID-19 pandemic created multiple additional barriers to rheumatology patients receiving prompt and appropriate care, many of which remain. These barriers adversely impacted mental and physical health. They also had negative impacts on medical security and trust, reductions in which were associated with lower patient mental-wellbeing (WEMWBS) [17] and negative healthcare behaviours, including reduced symptom reporting. Clinicians frequently underestimated and/or misunderstood the severity and nature of the barriers that patients were continuing to experience when attempting to access care. This may have contributed to the identified discordances between patient and clinician perceptions of patient healthcare behaviours. In particular, clinicians appear to have over-attributed delayed presentations to hospital avoidance due to fear of COVID-19 infection. Patients, however, had often been more deterred by implicit and explicit messaging not to seek help during the pandemic, not wanting to be a ‘burden’, and/or repeated failed attempts to access help. Facilitators to accessing care during the pandemic included a pre-existing trusting medical relationship, responsive helplines and proactive individual clinicians.
The continuing disparity in the provision of routine and emergency care between hospitals, GP surgeries and individual clinicians, identified at earlier stages of the pandemic [6], has contributed to inequalities in care and a sense of abandonment in some patients. A particular concern was the reduction in access to the prompt care necessitated by the fluctuating and potentially life-threatening nature of some rheumatological conditions [23], and of key importance for medical security and trust [15]. The extensive self-management reported by some participants, including of major disease symptoms, was perceived to have arisen from pandemic-increased barriers to care rather than through choice, or education and clinical support as recommended by Williams et al. [24] Our study has further highlighted the importance of charities [25] and rheumatology nurses in providing support and empowerment, reducing isolation and disseminating information on disease, shielding and vaccinations.
Our findings are consistent with Ziadé et al.’s [26] conclusion that the pandemic-related barriers to healthcare could influence the longer-term prognosis of rheumatic diseases. Our data further suggests that the temporary reduction in care not only increased accrual of physical damage to an extent not seen for many years, but also generated psychological damage and medical insecurity in many patients. Although some of the early pandemic-related barriers (e.g. the closure of some departments) have lessened over time, this study highlights that more enduring psychological and behavioural barriers have been induced by failed attempts to navigate those earlier barriers to healthcare. For example, some patients who reported failing to obtain emergency support, including those with suicidal feelings or severe flares, discussed greater reticence to report future symptoms. This could exacerbate the divide between those patients who remain confident in their ability to initiate care, and those whose previous adverse medical experiences [27], including negative diagnostic [15] and/or pandemic experiences [6], have increased healthcare avoidance. This could delay assessment and treatment, with potentially life-threatening and life-shortening consequences.
Our clinician participants faced the same restrictions and fears as the general population, yet continued to work in high-risk stressful environments while attempting to balance the demands of acute and chronic care, and increasingly dissatisfied patients. Early US pandemic literature details sources of clinician anxiety, summarized into five requests to their organizations to ‘hear me, protect me, prepare me, support me, and care for me’ [28]. Our UK clinician participants reported similar anxieties and unmet needs, particularly regarding inadequate PPE, and feeling undervalued, unsupported and undermined by the UK government’s management of the pandemic. Although some clinicians reported little impact on their health, others—consistent with reports from the BMA [29]—mentioned stress, burn-out and compassion fatigue. These can adversely affect clinician quality of life and jeopardize medical relationships, clinical decision making [30] and longer-term staff recruitment and retention [31, 32], which have previously been identified as issues within primary care [33] and rheumatology [34]. Consultation time, listening and displaying empathy were also felt to be reduced due to pandemic constraints and the large-scale transition towards telemedicine. Telemedicine was felt to be inferior to face-to-face in most respects by rheumatology clinicians and patients in our previous study [35]. Some clinicians expressed concerns that the NHS and hospital management targets for telemedicine were over-ambitious, had been decided with insufficient consultation with clinicians, and were not necessarily clinically appropriate. Additional concerns were that ‘blanket targets’ would fail to differentiate between medical specialities and specific conditions (including some rheumatological diseases such as lupus or vasculitis) requiring a higher proportion of face-to face contact for safe care.
Although many patients felt personally abandoned by their clinicians, the vast majority of clinicians detailed the great efforts they had taken to provide continuing compassionate care for their patients, often at significant personal cost. Analysing the multiple perspectives suggests that the problems were more commonly systemic than individual failings, with clinicians’ efforts often thwarted by inefficient administration systems and technology, chronic understaffing [34] and under-funding [36]. In addition, there were difficulties navigating convoluted NHS management structures that were reported to offer limited clinical autonomy. A positive consequence of the pandemic was increased multi-disciplinary teamwork within hospitals. These enhanced professional relationships may facilitate long-term improvements in multi-disciplinary care, previously reported as ‘fragmented’ [37] for some rheumatology patients. Conversely, relationships between primary and secondary care had deteriorated, resulting in additional clinician stress and some patients being left without sufficient care from either. These relationships are important in the provision of effective integrated care [38–40] and a clearer division of responsibility might be required.
Limitations of this study include the self-selecting nature of online recruitment reducing the likelihood of a fully representative sample (including socio-demographically and in terms of disease severity), and the risk of left censorship bias as the study excludes those who had died or been too unwell to participate. Participants choosing to complete an online survey about their pandemic experiences may have stronger views than non-responders. However, we mitigated this by neutral phrasing of the invitation to participate and the use of pandemic data from our (coincidentally) pre-pandemic recruited cohort. Although males are in the minority in some rheumatological diseases, e.g. lupus, they are even further under-represented in online support groups and in choosing to complete online surveys. We attempted to ensure a more even overall balance of female–male opinions by purposeful sampling to include a higher proportion of males for interview than the proportion completing surveys. Strengths of this study were the triangulation [22] of multiple perspectives and data sources to enhance validity, and the active participation of patient representatives in every stage of the research as equally valued collaborators [41].
Some patients remain reluctant to report their needs, and those who attempt to do so are sometimes still facing insurmountable barriers to accessing care. Re-building trust and medical security is essential. Barriers could be reduced by increased investment in staff and administrative systems, and by reassuring patients that they are not perceived as a burden and how to access (more consistently responsive) urgent care. More support, teamwork and empowering clinicians may enable them to provide safer and more effective care for their patients. Although gratitude was often expressed towards both the NHS and individual clinicians, a common perception among clinicians and patients of the legacy of the COVID-19 pandemic is that the negative effects may endure well beyond the re-establishment of a ‘new normal’. This legacy can be summarized by re-iterating this rheumatologist’s quote, which although referring to patients may be equally applicable to some clinicians: ‘The feeling of abandonment will remain for longer than the memories of the chaos of Covid’.
Supplementary Material
Acknowledgements
Patient representatives are an invaluable part of the study team and are involved throughout every stage of the research process. With particular thanks to these expert team members: Lynn Holloway, Colette Barrere, Mike Bosley, Rupert Harwood and Mo Blane. Also to our wider clinician and psychology team members: Drs Chris Wincup, Peter Lanyon and Felix Naughton, and multiple rheumatology charity groups, who improve our research with their assistance and advice. With thanks also to the many patients and clinicians who gave up their time to complete surveys and interviews, often also then discussing key themes together with the researchers and reviewing the draft paper for agreement. This manuscript includes views expressed by the participants surveyed and interviewed. These do not necessarily represent the views of the authors or the organisations that they work for.
Funding: This study was an unfunded addition to the LISTEN study, funded by LUPUS UK.
Disclosure statement: The authors have declared no conflicts of interest.
Contributor Information
Melanie Sloan, Department of Public Health and Primary Care, School of Clinical Medicine.
Rupert Harwood, Patient and Public Involvement in Rheumatology Research Group, Institute of Public Health, University of Cambridge, Cambridge.
Caroline Gordon, Rheumatology Research Group, Institute of inflammation and ageing, College of Medical and Dental Science, University of Birmingham, Birmingham.
Michael Bosley, Patient and Public Involvement in Rheumatology Research Group, Institute of Public Health, University of Cambridge, Cambridge.
Elliott Lever, Rheumatology Department, West Middlesex Hospital.
Rakesh Modi, Department of Public Health and Primary Care, School of Clinical Medicine.
Moira Blane, Patient and Public Involvement in Rheumatology Research Group, Institute of Public Health, University of Cambridge, Cambridge.
James Brimicombe, Department of Public Health and Primary Care, School of Clinical Medicine.
Colette Barrere, Patient and Public Involvement in Rheumatology Research Group, Institute of Public Health, University of Cambridge, Cambridge.
Lynn Holloway, Patient and Public Involvement in Rheumatology Research Group, Institute of Public Health, University of Cambridge, Cambridge.
Stephen Sutton, Department of Public Health and Primary Care, School of Clinical Medicine.
David D’Cruz, The Louise Coote Lupus Unit, Guy’s and St Thomas’, NHS Foundation Trust, London, UK.
Data availability statement
Additional anonymised data may be made available on request.
Supplementary data
Supplementary data are available at Rheumatology online.
References
- 1. Kendzerska T, Zhu DT, Gershon AS. et al. The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Manag Healthc Policy 2021;14:575–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nune A, Iyengar K, Ahmed A, Sapkota H.. Challenges in delivering rheumatology care during COVID-19 pandemic. Clin Rheumatol 2020;39:2817–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Li J, Ringold S, Curtis JR. et al. Effects of the SARS-CoV-2 global pandemic on U.S. rheumatology outpatient care delivery and use of telemedicine: an analysis of data from the RISE registry. Rheumatol Int 2021;41:1755–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coronini-Cronberg S, Maile EJ, Majeed A.. Health inequalities: the hidden cost of COVID-19 in NHS hospital trusts? J R Soc Med 2020;113:179–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rutter-locher Z, Arumalla N, Bright Z, Garrood T.. P067 virtual care: the future, but to what extent? Rheumatology 2021;60 (Suppl 1):keab247.064. [Google Scholar]
- 6. Sloan M, Gordon C, Harwood R. et al. The impact of the COVID-19 pandemic on the medical care and health-care behaviour of patients with lupus and other systemic autoimmune diseases: a mixed methods longitudinal study. Rheumatol Adv Pract 2021;5:rkaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ciacchini B, Tonioli F, Marciano C. et al. Reluctance to seek pediatric care during the COVID-19 pandemic and the risks of delayed diagnosis. Ital J Pediatr 2020;46:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rutter M, Lanyon PC, Grainge MJ. et al. COVID-19 infection, admission and death amongst people with rare autoimmune rheumatic disease in England. Results from the RECORDER Project. Rheumatology 2022;61:3161--71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Maldonado D, Tu E, Mahmood SN. et al. Association of medication access difficulty and COVID-19–related distress with disease flares in rheumatology patients during the COVID-19 pandemic. Arthritis Care Res 2021;73:1162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. RAIRDA. Chronic crisis. The impact of COVID-19 on people with rare autoimmune rheumatic diseases. The Rare Autoimmune Rheumatic Disease Alliance. https://rairdaorg.files.wordpress.com/2020/08/chronic-crisis-report-june-2020-1.pdf (26 October 2021, date last accessed).
- 11. Dacre J. Virtual rheumatology during COVID-19: a personal perspective. Rheumatol Ther 2020;7:429–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Greenberg N, Weston D, Hall C. et al. Mental health of staff working in intensive care during Covid-19. Occup Med 2021;71:62–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vanhaecht K, Seys D, Bruyneel L. et al. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int J Qual Health Care 2021;33:mzaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Georgopoulou S, Prothero L, D'Cruz DP.. Physician-patient communication in rheumatology: a systematic review. Rheumatol Int 2018;38:763–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sloan M, Naughton F, Harwood R. et al. Is it me? The impact of patient–physician interactions on lupus patients’ psychological well-being, cognition and health-care-seeking behaviour. Rheumatol Adv Pract 2020;4:rkaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H.. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2014;9:e94207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tennant R, Hiller L, Fishwick R. et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 19. Tong A, Sainsbury P, Craig J.. Consolidated criteria for reporting qualitative research (COREQ): a 32 item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. [DOI] [PubMed] [Google Scholar]
- 20. Seawright J. The case for selecting cases that are deviant or extreme on the independent variable. Sociol Methods Res 2016;45:493–525. [Google Scholar]
- 21. Birt L, Scott S, Cavers D. et al. Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qual Health Res 2016;26: 1802–11. [DOI] [PubMed] [Google Scholar]
- 22. Cresswell J, Clark V.. Designing and conducting mixed methods research. London, UK: Sage, 2017. [Google Scholar]
- 23. Mitratza M, Klijs B, Hak AE, Kardaun JWPF, Kunst AE.. Systemic autoimmune disease as a cause of death: mortality burden and comorbidities. Rheumatology 2021;60:1321–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Williams E, Egede L, Faith T, Oates J.. Effective self-management interventions for patients with lupus: potential impact of peer mentoring. Am J Med Sci 2017;353:580–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sloan M, Bosley M, Blane M. et al. ‘But you don’t look sick': a qualitative analysis of the LUPUS UK online forum. Rheumatol Int 2021;41:721–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ziadé N, Hmamouchi I, El Kibbi L. et al. The impact of COVID-19 pandemic on rheumatology practice: a cross-sectional multinational study. Clin Rheumatol 2020;39:3205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sloan M, Lever E, Gordon C. et al. Medication decision-making and adherence in lupus: patient–physician discordance and the impact of previous ‘adverse medical experiences’. Rheumatology 2022;61:1417--29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shanafelt T, Ripp J, Trockel M.. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020;323:2133–4. [DOI] [PubMed] [Google Scholar]
- 29.Personal Impact of the COVID 19 pandemic on doctors’ wellbeing revealed in major BMA survey. BMA Press Release, 1 June 2020.
- 30. Persson E, Barrafrem K, Meunier A, Tinghög G.. The effect of decision fatigue on surgeons’ clinical decision making. Health Econ 2019;28:1194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Figley C. Compassion fatigue; towards a new understanding of the costs of caring. In: Stamm BH, ed. Secondary traumatic stress; selfcare issues for clinicians, researchers, and educators. 2nd ed. Lutherville MB: Sidron Press, 1999. [Google Scholar]
- 32. Shanafelt TD. Enhancing meaning in work; a prescription for preventing physician burnout and promoting patient centred care. JAMA 2009;302:1338–40. [DOI] [PubMed] [Google Scholar]
- 33. Hall LH, Johnson J, Watt I, O'Connor DB.. Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Pract 2019;69:e507–e514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. British Society for Rheumatology. Rheumatology workforce: a crisis in numbers. Workforce policy report 2021.
- 35. Sloan M, Lever E, Harwood R. et al. Telemedicine in rheumatology: a mixed methods study exploring acceptability, preferences and experiences among patients and clinicians. Rheumatology 2022;61; 2262--74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Anandaciva S, Ewbank L, Thompson J, McKenna H.. NHS hospital bed numbers: past, present, future. London: Kings Fund, 2020. [Google Scholar]
- 37. Sumpton D, Hannan E, Kelly A. et al. Clinicians’ perspectives of shared care of psoriatic arthritis and psoriasis between rheumatology and dermatology: an interview study. Clin Rheumatol 2021;40:1369–80. [DOI] [PubMed] [Google Scholar]
- 38. Wallace DJ. Improving the prognosis of SLE without prescribing lupus drugs and the primary care paradox. Lupus 2008;17:91–2. [DOI] [PubMed] [Google Scholar]
- 39. Greenwood-Lee J, Jewett L, Woodhouse L, Marshall DA.. A categorisation of problems and solutions to improve patient referrals from primary to specialty care. BMC Health Serv Res 2018;18:986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Esteve-Matalí L, Vargas I, Sánchez E. et al. Do primary and secondary care doctors have a different experience and perception of cross-level clinical coordination? Results of a cross-sectional study in the Catalan National Health System (Spain). BMC Fam Pract 2020;21:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Van Emmenis M, Lloyd L. The strength of the wolf is the pack: how a study of lupus patient experiences involved patients. 2021.https://www.phpc.cam.ac.uk/pcu/lupus-patient-experiences (26 October 2021, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Additional anonymised data may be made available on request.