Abstract
Study Objectives
African Americans have faced disproportionate socioeconomic and health consequences associated with the COVID-19 pandemic. The current study examines employment and its association with sleep quality during the initial months of the pandemic in a low-income, predominantly African American adult sample.
Methods
In the early months of COVID-19 (March to May 2020), we administered a survey to an ongoing, longitudinal cohort of older adults to assess the impact of COVID-related changes in employment on self-reported sleep quality (N = 460; 93.9% African American). Participants had prior sleep quality assessed in 2018 and a subset also had sleep quality assessed in 2013 and 2016. Primary analyses focused on the prevalence of poor sleep quality and changes in sleep quality between 2018 and 2020, according to employment status. Financial strain and prior income were assessed as moderators of the association between employment status and sleep quality. We plotted trend lines showing sleep quality from 2013 to 2020 in a subset (n = 339) with all four waves of sleep data available.
Results
All participants experienced increases in poor sleep quality between 2018 and 2020, with no statistical differences between the employment groups. However, we found some evidence of moderation by financial strain and income. The trend analysis demonstrated increases in poor sleep quality primarily between 2018 and 2020.
Conclusions
Sleep quality worsened during the pandemic among low-income African American adults. Policies to support the financially vulnerable and marginalized populations could benefit sleep quality.
Keywords: COVID-19, employment, health disparities, sleep, socioeconomic status, job loss
Statement of Significance.
The coronavirus disease 2019 (COVID-19) pandemic has exacerbated existing disparities in health and employment. Prior research has documented high rates of sleep problems during COVID-19, but there has been limited focus on marginalized populations, including low-income African Americans. This study is the first to examine the association between employment and the level and change in sleep quality during COVID-19 in African American adults. Participants in all employment categories (still employed, not working pre-COVID-19, and lost job or reduced hours during COVID-19) demonstrated significant increases in poor sleep quality; however, there were no significant differences between the groups. Financial strain and prior income moderated associations between employment and sleep quality. Policy interventions are needed to address upstream determinants of racial inequities and downstream impacts on sleep.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has led to profound health and social consequences, with racial/ethnic minorities and other disadvantaged populations facing disproportionate burden both in terms of disease burden and mortality [1, 2], as well as socioeconomic impacts, such as job loss [3]. For example, in the early stages of the economic shutdown due to COVID-19 (between March and May 2020), the United States saw record-level increases in unemployment claims, with tens of millions of new claims filed [4]. African American workers consistently had higher unemployment rates than white workers throughout the pandemic, peaking in spring 2020 at 16.8% compared to 14.2% for white workers. Although legislation has been passed to assist workers in the United States, there are many people still suffering from severe economic distress caused by COVID-related disruptions to employment [5].
Involuntary job loss as well as stressful or precarious job conditions are significant psychosocial stressors and are linked with a wide range of health consequences, including poor sleep health [6–12]. For example, prior work has shown that unemployment and job loss are associated with increased rates of insomnia symptoms [13–15], as well as both short and long sleep durations [16].
Numerous recent studies have demonstrated rising rates of sleep problems associated with COVID-19 and related social policy [17]. Jahrami et al. conducted a systematic review of the literature, and found worsening sleep during the pandemic, with the most affected group being those who contracted COVID-19 [18]. They noted specifically the lack of research evaluating the role of changes in employment during the pandemic and sleep. Additionally, most of the literature has been cross-sectional and has not looked at potential moderators, such as pre-existing financial security or strain [18]. Cross-sectional studies suffer from several potential biases, such as from unobserved confounders and reverse causality, that longitudinal approaches can mitigate. With the ability to examine changes in sleep quality, these models offer stronger evidence of the impact of the pandemic, rather than pre-existing sleep problems or financial strain.
Furthermore, much of the extant literature on sleep disturbances during COVID-19 has been conducted outside of the United States and has therefore not focused on low-income African Americans, who have faced both disproportionate COVID-related disease burden and socioeconomic consequences, in part due to systemic racism in the United States [19, 20].
Understanding the impact of COVID-related changes in employment on sleep in African Americans is important for several reasons. First, prior to the pandemic, research demonstrated higher rates of sleep disturbances among African Americans, largely attributable to increased exposure to stressors operating at multiple levels, including discrimination and neighborhood disadvantage [21–23]. Moreover, the cumulative impact of centuries of systemic racism in the United States—including residential and labor market segregation and reduced educational opportunities—has rendered African Americans particularly vulnerable to both job loss as well as employment in potentially health-threatening environments [24]. Job loss and continued employment in health-threatening environments may both contribute to increased risk of sleep disturbances during COVID-19, albeit through different mechanisms [19]. For example, African Americans are more likely to face job insecurity [25–27], including during the pandemic [28–31], and are more likely to occupy low-wage jobs lacking benefits (e.g. paid sick leave) [32,33]. Loss of income due to job loss may contribute to increased risk for sleep disturbance, via increased stress due to financial strain. Such effects are likely to be exacerbated among those with lower incomes or already facing financial strain, as they lack the financial resources that could otherwise buffer the downstream consequences of loss of employment [34].
At the same time, African Americans are more likely to be front-line workers during COVID-19, thus facing heightened risk for potential exposure to the virus [24]. In turn, continued employment in this context may also heighten risk for sleep problems due to the increased stress and worry associated with health concerns [35]. African Americans have also been disproportionately impacted by COVID-19 in terms of incidence [36, 37], hospitalizations [38], and mortality [39]. Increased risk and incidence of these events may also negatively impact sleep quality [18, 40].
The current analysis is the first, to our knowledge, to examine how changes in employment, combined with financial strain or prior income, are associated with the prevalence of poor quality sleep or changes in sleep quality during the initial months of the COVID-19 lockdown among low-income African Americans. We also examined sleep quality trends over time between 2013 and 2020 among this cohort of residents from two predominantly African American neighborhoods in Pittsburgh, PA to provide a descriptive analysis of whether changes in sleep quality preceded the pandemic.
Methods
The primary analysis is based on a sample of 460 participants, enrolled in the ongoing the Pittsburgh Hill/Homewood Research on Neighborhood Change and Health (PHRESH) study, who had self-reported sleep quality measures in both the 2018 and 2020 data collection.
The initial PHRESH study enrolled a cohort of predominantly African American households randomly selected by address from two low-income neighborhoods in Pittsburgh, PA in 2011 [23, 41–44]. Based on the original PHRESH study aims, the primary food shopper for the household was enrolled into the study [41]. Thus, the sample is predominantly female. Our team has followed this original cohort over five assessment waves occurring in 2013, 2014, 2016, 2018, and 2020 (during the early months of COVID-19) [23, 41–44]. Participants were surveyed about their employment, income, and sleep quality in the 2013, 2016, 2018, and 2020 COVID-19 surveys [45, 46].
The primary analysis focused on the 2018 and 2020 survey waves. However, given age-related changes in sleep quality [47] and to examine whether observed differences in sleep quality between employment groups were evident prior to the pandemic, we also conducted a descriptive analysis to examine trends in sleep quality among a subsample of participants who had sleep quality data in all waves when sleep was collected (2013, 2016, 2018, and 2020). Study protocols were approved by the Human Subjects Protection Committee, RAND’s Institutional Review Board.
Predictors: employment/job loss
We created three employment categories based on survey items asked in the 2020 survey assessing the impact of COVID-19 on employment, as follows: (1) not employed before the pandemic (i.e. March 2020): “Not employed pre-COVID-19,” (2) employed before the pandemic but either experiencing job loss or a decrease in work hours during the pandemic: “Lost job or decreased hours during COVID-19,” and (3) employed before the pandemic and either staying at the same level of employment or increasing work hours during the pandemic: “Still employed with same or more work hours during COVID.” Supplement 1 describes in detail the questions upon which this classification is based. For employment category 1 (i.e. not employed before the pandemic), we did not have data on reasons for not working prior to the pandemic. Therefore, this may be a heterogeneous group consisting of some participants who were out of the labor force (e.g. retired) or in the labor force but unable to find work (unemployed).
Outcome: sleep quality
During the 2013, 2016, and 2018 data collection waves, participants completed a paper sleep diary each morning after waking up for a 7-day period in which they rated their sleep quality on a 5-point Likert scale from “very bad” to “very good.” We used these subjective ratings (averaged across the seven nights) to assess sleep quality, our primary outcome of interest. These measures have also been used in previous studies with our sample to assess sleep quality [23, 42, 45, 48]. To reduce participant burden during the rapidly deployed COVID-19 survey, participants did not complete sleep diaries in the 2020 survey, but rather were asked an item drawn from the PROMIS short-form sleep disturbance scale that most closely reflected our existing diary-assessed sleep quality rating: “In the past seven days, your sleep quality was…” [49], and given the same five response options, ranging from “very bad” to “very good.” Higher values indicate poorer sleep quality. The analyses focused on the prevalence of poor sleep quality in 2020, and changes in sleep quality using data collected in 2018 and 2020 (n = 460). For descriptive purposes, we additionally utilized all four waves of data to demonstrate trend lines in sleep across 2013 to 2020 in the subsample with sleep data available at all time points (n = 339).
Moderators: financial strain and prior income
We examined two potential moderators, financial strain, and 2018 per capita annual household income, of the relationship between employment status and sleep quality rating and change in sleep quality. Moderator was defined as a variable that could potentially alter the relationship between employment status and sleep quality rating (e.g. financial strain × employment status) [50]. Financial strain related to COVID-19 was measured in the survey using the following item: “Since the coronavirus outbreak, how much harder is it for you to pay for basics?” Response options were “Not harder at all,” “Somewhat harder,” or “Very much harder,” with the latter two response options combined as an indicator of financial strain. We also examined the individual’s per capita annual household income from the 2018 survey as a potential moderator.
Covariates
Sex (male, female), educational attainment (high school graduate or equivalent or less, some college but no bachelor’s degree, bachelor’s degree or higher), age (18–49, 50–65, 66, and older), marital status (married or living with partner, all else), presence of children in the home (yes, no), home-ownership status (yes, no), 2018 per capita household income (continuous), and neighborhood of residence (Hill, Homewood, other) were all included as covariates, given their association with employment and/or sleep [51–54].
Analytic strategy
The main analysis used the 2018 and 2020 PHRESH survey waves and restricted the sample to participants who responded to sleep quality in both surveys. The initial PHRESH study in 2011 included 1372 households; sleep questions were first asked in 2013 with 842 sleep responses. The 2020 survey was implemented by contacting all 2018 PHRESH survey respondents (2018; n = 855) by phone between March 23 and May 22, 2020; among those, 641 had sleep quality data available from 2018. Of the 641 participants, 16 were determined to be ineligible between 2018 and 2020 (death = 12, moving outside the study neighborhoods = 2, substantial physical or cognitive decline = 2). Of the remaining 625 eligible respondents in 2020, n = 5 responded to the survey but did not answer either the sleep or employment questions, n = 47 refused the 2020 survey, and n = 113 were unable to be contacted. Therefore, the analytic sample for the primary analyses is 460 participants, corresponding to a 74% response rate, and 460/842 = 55% from the parent sleep study in 2013 [46]. Supplementary Table S1 shows the demographics and 2018 sleep quality rating of those who were in the analytic sample (n = 460) compared to the eligible respondents who did not respond in 2020 (N = 165). Given a few observed differences between the analytic sample and the eligible sample at 2018, we calculated inverse probability weights using a logistic regression of 2020 survey response on 2018 demographics. These weights were used in regressions to adjust for potential biases associated with attrition.
The first set of analyses examined the sample characteristics overall and by employment category (i.e. not employed pre-COVID-19; lost job/reduced hours during COVID-19; still employed with same or more work hours during COVID).
The primary analyses examined the relationship between employment category and sleep quality rating and change in sleep quality rating between 2018 and 2020. We used ordinary least squares regressions of the outcome (sleep quality rating or change in sleep quality rating) on indicators for employment groups, with covariate adjustment. The reference group (still employed with the same or more work hours during COVID-19) were the omitted category.
Next, we tested two potential moderators of the relationship between employment category and sleep quality in 2020 and change in sleep quality between 2018 and 2020: financial strain during COVID-19 and 2018 per capita household income. In separate models, we included the interaction terms for the two employment categories with financial strain or prior income. All analyses were conducted using STATA 16.1 (College Station, TX).
Finally, we performed a descriptive analysis examining longitudinal, age-adjusted trends in sleep quality using all waves of data (i.e. 2013, 2016, 2018, and 2020). To do so, we regressed the sleep quality rating on the interaction of each survey wave year and employment category as well as indicators for the age groups. We graphed the age-adjusted means predicted by this regression.
To aid with interpretability of results, we additionally present standard-deviation scaled coefficients of interest by dividing by the standard deviation of the outcome. These standard deviation scaled coefficients are interpreted as how many standard deviations of the outcome arise from a unit change in the independent variable. This is measured on the same scale as Cohen’s d or Hedges’ g, and we can contrast the standard deviation scaled coefficients against the same common benchmarks from Cohen [55].
Results
Table 1 presents the summary statistics for the overall sample, and stratified by employment category. The sample was predominantly African American (93.9%) and female (84.6%), with approximately half of the sample with a high school degree or less. The average age of respondents was 62.3 years. Most individuals in the sample were unmarried and did not have children living at home; and 32.6% were homeowners. The average 2018 per capita annual household income was $15 300 and over half the sample (56.6%) reported experiencing financial strain since the start of the pandemic. In terms of employment categories, 62.6% were not employed before the start of the pandemic (employment category 1); 18.9% were employed before the start of the pandemic in March 2020 but had lost their jobs or had decreased hours by the time of the survey (employment category 2); 18.5% were still employed with the same or more work hours during COVID the time of the survey (employment category 3).
Table 1.
Sample statistics
| Variable | Total sample (n = 460) | Not employed pre-COVID (n = 288, 62.6%) | Lost job or decreased hours during COVID (n = 87, 18.9%) | Still employed with same or more work hours during COVID (n = 85, 18.5%) | P * |
|---|---|---|---|---|---|
| M(SD) or n(%) | M(SD) or n(%) | M(SD) or n(%) | M(SD) or n(%) | ||
| Demographics | |||||
| Male | 15.4% (71) | 16.3% (47) | 12.6% (11) | 15.3% (13) | .708 |
| Age | 62.30 (13.83) | 67.01 (12.39) | 54.61 (12.55) | 54.18 (12.45) | <.001 |
| High school or less | 49.3% (227) | 56.9% (164) | 41.4% (36) | 31.8% (27) | <.001 |
| Some college/tech | 36.3% (167) | 32.3% (93) | 39.1% (34) | 47.1% (40) | .038 |
| 4-year college or graduate degree | 14.3% (66) | 10.8% (31) | 19.5% (17) | 21.2% (18) | .017 |
| Married | 15.4% (71) | 12.5% (36) | 19.5% (17) | 21.2% (18) | .076 |
| Lived in Homewood | 26.3% (121) | 27.8% (80) | 20.7% (18) | 27.1% (23) | .416 |
| Lived outside of Hill and Homewood | 9.8% (45) | 10.1% (29) | 9.2% (8) | 9.4% (8) | .964 |
| No children at home | 81.1% (373) | 88.9% (256) | 70.1% (61) | 65.9% (56) | <.001 |
| Homeowner | 32.6% (150) | 29.2% (84) | 35.6% (31) | 41.2% (35) | .093 |
| Key predictors | |||||
| Has financial strain | 56.6% (260) | 54.0% (155) | 75.9% (66) | 45.9% (39) | <.001 |
| 2018 per capita household income, thousands of dollars | 15.37 (15.63) | 13.79 (13.93) | 15.41 (13.62) | 20.66 (21.11) | .002 |
| Outcomes | |||||
| Sleep quality rating 2018 | 2.27 (0.79) | 2.28 (0.81) | 2.26 (0.76) | 2.26 (0.77) | .948 |
| Sleep quality rating 2020 | 2.75 (1.05) | 2.77 (1.05) | 2.82 (1.04) | 2.65 (1.03) | .538 |
| Change in sleep quality rating | 0.48 (1.03) | 0.48 (1.02) | 0.56 (1.04) | 0.38 (1.04) | .521 |
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep.
*P-values are for an ANOVA test of difference in means across the three employment categories.
There were statistically significant differences between the three employment categories across several sociodemographic variables. Those participants who were not employed prior to COVID-19 (group 1) were older, had lower educational attainment, and were less likely to have children at home, compared to those who were employed prior to COVID-19 (groups 2 and 3). There were statistically significant differences in financial strain and 2018 income across the three employment categories, with those who had lost their jobs/decreased hours reporting the highest rates of financial strain (75.9%), and those not working before the pandemic having the lowest 2018 income ($13 800). Individuals who were still employed with the same or more work hours during COVID had both the lowest rate of financial strain (45.9%) and the highest average 2018 income ($20 700) of the three employment categories.
Employment status and sleep quality
Table 2 shows the primary coefficients of interest from the regression models predicting sleep quality rating at the time of the COVID-19 survey (2020) and changes in sleep quality between 2018 and 2020 according to employment category. As shown in Table 2, there were no statistically significant differences in sleep quality in 2020 or in the change in sleep quality between 2018 and 2020 according to employment categories. Supplementary Tables S2 and S3 present the full regression results including covariates.
Table 2.
Regression results for sleep quality during the pandemic according to employment category (n = 460).
| Sleep quality rating in 2020 |
Change in sleep quality rating (2018–2020) | |||||
|---|---|---|---|---|---|---|
| b | (95% CI) | P | b | (95% CI) | P | |
| Not employed pre-COVID | 0.228 | (−0.065 to 0.521) | .127 | 0.109 | (−0.186 to 0.405) | .467 |
| Lost job or decreased hours during COVID | 0.120 | (−0.199 to 0.439) | .459 | 0.137 | (−0.185 to 0.458) | .405 |
| Still employed with same or more work hours during COVID | Ref | Ref |
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep. b is the regression coefficient, CI is the confidence interval. Covariates included: 2018 per capita household income, some college, college graduate, gender, marital status, decade of age, home-ownership status, have children at home, and neighborhood lived in. Those employed during the pandemic without a reduction in work hours were the reference group. The regression uses attrition weights.
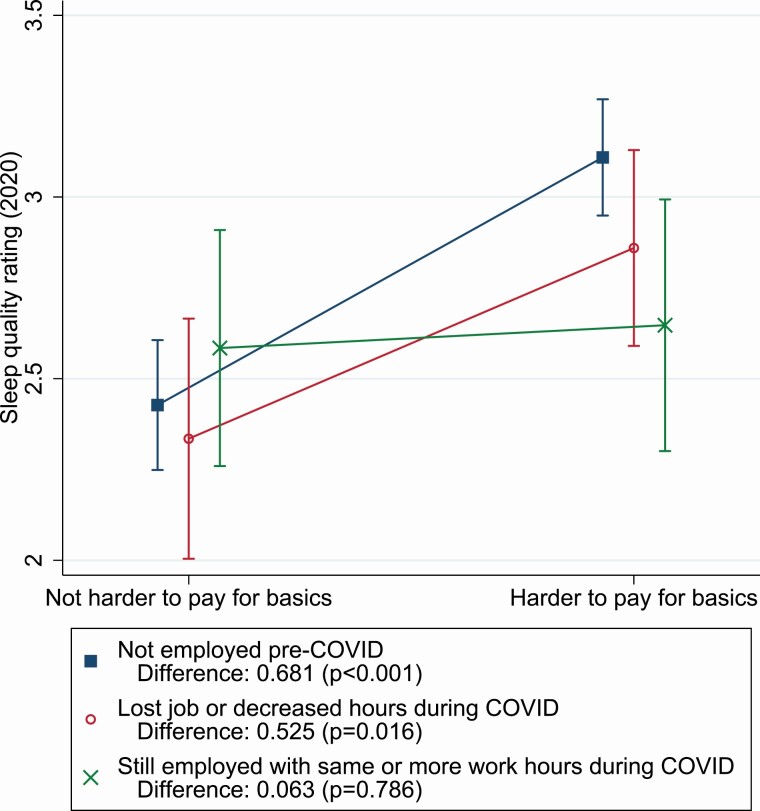
Financial strain as a moderator
There was a marginally significant joint interaction term for financial strain and employment category on sleep quality in 2020 (p = .059). However, as shown in Figure 1 there were statistically significant individual contrasts. Specifically, for both those not working before the pandemic and those who lost their jobs or decreased hours during the pandemic, reporting financial strain was associated with significantly worse sleep quality, with increases in the change in the Likert score for poor sleep quality of 0.681 (p = .002, b = 0.649) and 0.525 (p = .034, b = 0.520) compared to those not experiencing financial strain. Financial strain was not related to sleep quality for those who had were still employed with the same or more work hours during COVID-19. Supplementary Table S4 presents the full results for the underlying regression for Figure 1.
Figure 1.
Predicted sleep quality rating in 2020 by employment categories and financial strain.
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep. Predictions based on OLS regressions of sleep rating on interaction of employment status and financial strain, and covariates including 2018 per capita household income, some college, college graduate, gender, marital status, age, home-ownership status, have children at home, and neighborhood lived in. The regression uses attrition weights. Bars represent 95% confidence intervals.
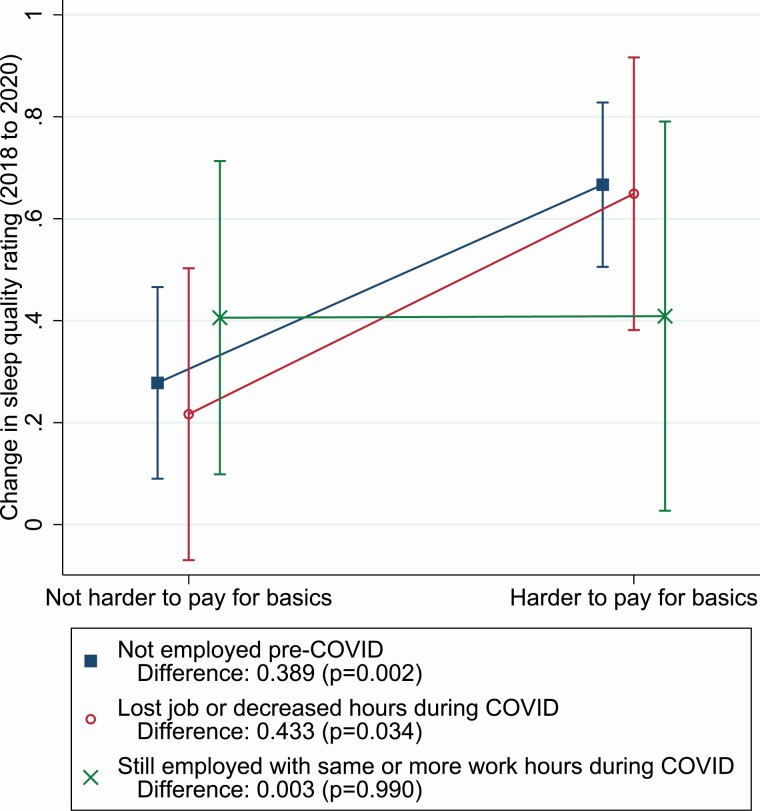
Overall, financial strain did not significantly moderate change in sleep quality (p-value of the joint significance of the interaction terms of financial strain and employment category on change in sleep quality is .329). Figure 2 presents the individual contrasts for change in sleep quality for the interaction between employment category and financial strain. Financial strain was associated with significantly worse changes in sleep quality for those not working before the pandemic (0.389, p = .002, b = 0.378) and for those who lost their jobs or decreased hours during the pandemic (0.433, p = .034, b = 0.420). Supplementary Table S5 reports the full regression results for the underlying regression for Figure 2.
Figure 2.
Predicted change in sleep quality rating (2018 to 2020) by employment category and financial strain.
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep. Predictions based on OLS regressions of sleep rating on interaction of employment status and 2018 per capita household income, plus additional controls for 2018 per capita income, some college, college graduate, gender, marital status, age, home-ownership status, have children at home, and neighborhood lived in. The regression uses attrition weights. Bars indicate 95% confidence intervals.
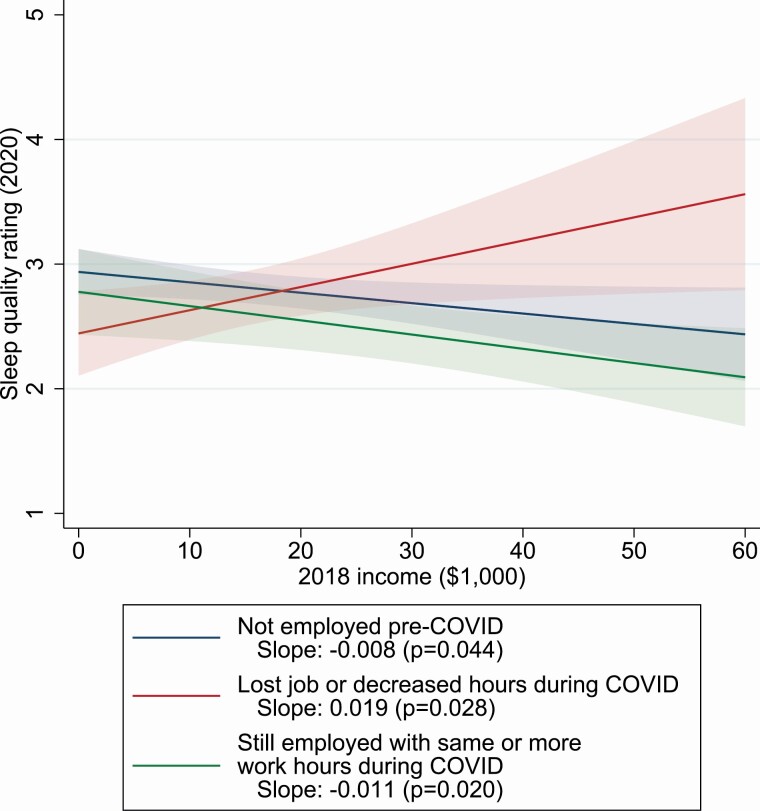
Prior income as a moderator
For the moderating association between 2018 income and employment category on sleep quality, the p-value of the joint significance of the interaction terms was .006. Figure 3 shows the results of the interaction between employment category and income at 2018 on sleep quality in 2020. For those who were not working pre-COVID-19 and for those still employed with the same or more work hours during COVID, higher 2018 income was associated with better sleep quality (−0.08 per $1000, p = .044, b = −0.0076 per $1000 and −0.011 per $1000, p = .020, b = −0.0105 per $1,000 respectively). However, among those who lost job or had decreased hours, higher 2018 income was associated with poorer sleep quality during COVID-19 (0.019 per $1000, p = .028, b = 0.0181 per $1000). Supplementary Table S6 reports the full results for the underlying regression for Figure 3.
Figure 3.
Predicted sleep quality rating in 2020 by employment categories and 2018 income.
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep. Predictions based on OLS regressions of change in sleep rating on interaction of employment status and financial strain, and covariates including 2018 per capita household income, some college, college graduate, gender, marital status, age, home-ownership status, have children at home, and neighborhood lived in. “2018 income ($1000)” refers to 2018 per capita household income as measured in thousands of dollars. The regression uses attrition weights. Shaded regions represent 95% confidence regions.
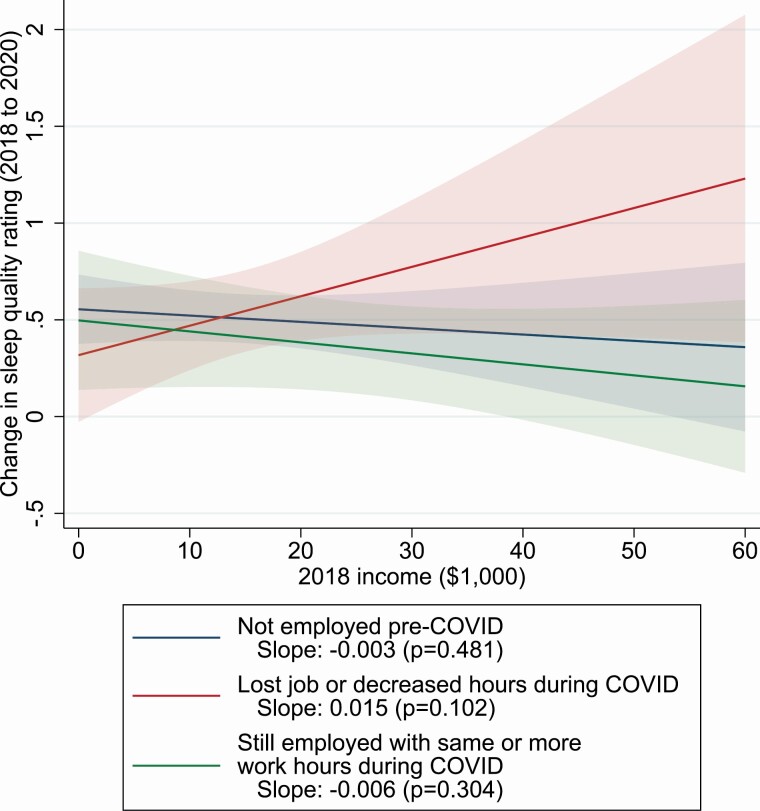
The p-value of the joint significance of the interaction terms for income and employment category on change in sleep quality was 0.116. Figure 4 presents the predicted sleep quality by income and employment category. While the overall trends are similar to Figure 3 (sleep quality in 2020), the slopes for individual contrasts are about half as large and are not statistically significant. Supplementary Table S7 presents the full results for the underlying regression for Figure 4.
Figure 4.
Predicted change in sleep quality rating (2018 to 2020) by employment category and 2018 income.
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep. Predictions based on OLS regressions of change in sleep rating on interaction of employment status and 2018 per capita household income, plus additional controls for 2018 per capita income, some college, college graduate, gender, marital status, age, home-ownership status, have children at home, and neighborhood lived in. “2018 income ($1000)” refers to 2018 per capita household income as measured in thousands of dollars. The regression uses attrition weights. Shaded regions represent 95% confidence regions.
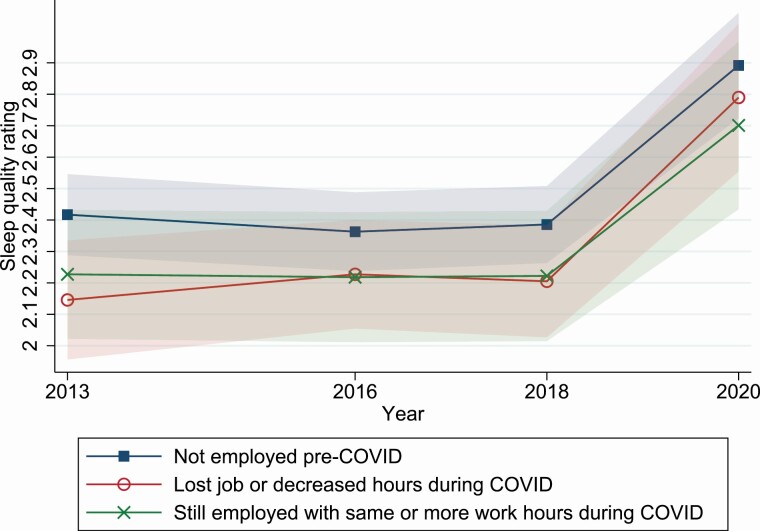
Trend analysis
For descriptive purposes, Figure 5 depicts the trends over time in sleep quality for each of the 2020 employment categories among the subsample of participants with sleep data available at all four waves (2013, 2016, 2018, and 2020). For all employment categories, sleep quality was relatively stable between 2013 and 2018, but worsened significantly between 2018 and 2020, with increases in poor sleep rating on the 1–5 Likert scale of 0.484, 0.582, and 0.467 for the for the three employment categories 1–3 respectively (p-value on the change < .001 for each difference). Standard deviation scaled coefficients were 0.541, 0.651, and 0.522 respectively, all qualifying as medium-sized effects by Cohen’s thresholds [55,56]. However, there were no statistically significant differences between participants in each of the employment categories in any year.
Figure 5.
Longitudinal trends in average sleep quality by 2020 employment status, adjusted for age.
Sleep quality rating is measured on a 1–5 Likert scale, with higher values representing poorer quality sleep. N = 339. Shaded regions represent 95% confidence regions.
Discussion
In response to the economic fall-out from the pandemic, including elevated unemployment, legislation has been passed to assist workers in the United States, including the CARES Act, Paycheck Protection Plan, the American Rescue Plan Act of 2021, and state-level loosening of unemployment claims requirements. Many who lost their job during the pandemic were eligible to receive benefits greater in size than their lost wages [57]. However, even with the actions of the government to support financially distressed individuals, there are many people still suffering from severe economic distress [5]. These enduring economic consequences have served to exacerbate pre-existing inequities in socioeconomic status and in health, particularly among racially marginalized populations, such as African Americans. One of the health consequences of this economic downturn includes disruptions in sleep quality [17–19]. This paper adds to the literature by exploring the extent to which changes in employment are related to the level and changes in sleep quality during the COVID-19 pandemic, within a sample of urban, primarily low-income, and African American community. Further, recognizing that the effects of COVID-19 may be exacerbated among those experiencing pre-existing financial hardship, we examined financial strain during the pandemic and income from 2018 as potential moderators of the association between employment category and sleep quality.
Across employment categories, we found significant declines in sleep quality between 2018 and 2020, with an average change of nearly 0.5 on a 1 to 5 Likert scale, or over half a standard deviation change, equivalent to a medium-sized effect in Cohen’s thresholds [55]. This decrease in sleep quality occurred similarly across those who were not working before the pandemic, those who lost their job or decreased their hours during the pandemic, and those who were still employed with the same or more work hours during COVID.
Although we did not find significant differences in prevalence of poor sleep quality or changes in sleep quality across the employment categories, we found that the association of employment on sleep quality depended to some extent on financial strain and prior income. Specifically, those who were not working pre-pandemic or who lost their job during the pandemic and who experienced financial strain reported significantly worse sleep quality and greater declines in sleep quality, compared to those in the same employment category who did not experience financial strain. However, among those who were still employed with the same or more work hours during COVID-19, there was no evidence of moderation by financial strain.
Further, for those who had lost their jobs during the pandemic, higher 2018 income was related to worse sleep. This somewhat unexpected finding could reflect stronger negative impacts of loss of employment among those working higher-wage jobs, as they experienced relatively greater decreases in earnings. In contrast, for those who were not working pre-COVID-19 or who were still working during the pandemic, higher 2018 income was associated with better sleep quality ratings, likely due to financial security from their prior higher income. Collectively, these findings highlight the importance of considering the impact of employment in conjunction with other key, socio-contextual factors to better identify the most at-risk group for sleep problems during the pandemic.
Limitations
Findings from this study must be considered in light of several limitations, including the inability to rule-out reverse causality, potential survival bias, the inability to establish temporal ordering of moderating influences of financial strain and income, the potential that unmeasured confounding variables could have biased the estimates, and the potential for recall bias in reporting employment prior to the pandemic. However, we believe that recall bias should be limited given that the survey was fielded in March to May 2020, and participants were reporting on changes in employment related to COVID-19. Related to the sample size and sample characteristics, limited statistical power may have contributed to the lack of significance for joint interaction tests. In addition, while there are advantages to focusing on one geographic area and on an under-represented and high-risk population of predominantly female, African American adults, this also limits the potential generalizability of our findings. The sample is also older than the working population on average which may limit the generalizability of these findings to employment changes overall and to the US labor force in general. Further, there was sample attrition, with a 74% response rate for those eligible and included in the current analyses. To minimize the potential confounding by attrition bias, we used attrition weights in the analyses. However, there remains the potential of survival bias, which may bias the sample towards healthier individuals, though we note that there were relatively few COVID-related deaths in the city of Pittsburgh during our data collection. Therefore we are confident our results are not due to mostly sampling healthier individuals. Regarding measurement limitations, sleep quality was measured with a single item, and was measured differently in 2020 compared to earlier waves (survey vs. sleep diary, respectively), which may have introduced measurement error. Although findings would be strengthened by more in-depth sleep assessments, including objective measures, self-reported sleep quality is a critical component of overall sleep health. Additionally, in the analysis and using standard deviation scaled coefficients, we assume linearity. We tested a non-linear model and the results were very similar.
Conclusion
The current findings are the first to demonstrate significant increases in poor sleep quality during the early months of the COVID-19 pandemic according to different employment categories, and within a high-risk sample of urban, socioeconomically disadvantaged, African American adults. Although we found significant decreases in sleep quality across all groups, we did not find differences in the prevalence of poor sleep quality or change in sleep quality according to employment category. However, we found that among those were not employed pre-COVID-19 or who had lost their jobs during the pandemic or experienced a reduction in work hours, financial strain was associated with poorer sleep quality and greater increases in poor sleep quality, relative to those not experiencing financial strain. We further found that higher 2018 income was associated with better sleep quality for those not employed before the pandemic and for those who were still employed with the same or more work hours, but was associated with worse sleep quality for those who had lost their jobs or had reduced work hours, potentially due to a larger decrease in resources. These findings may reflect the very low-income nature of this sample, and may not apply to other sociodemographic groups. These findings provide further demonstration that COVID-19 has exacerbated existing inequities in socioeconomic status and health, including sleep health. Public policy interventions are needed that address upstream determinants of such inequities, including systemic racism, as well as downstream impacts, such as poverty and increased exposure to stress, which are in turn, associated with disparities in sleep as well as other health outcomes.
Supplementary Material
Acknowledgments
We sincerely thank our Field Coordinator, La’Vette Wagner, without whom this research could not have happened. Thank you to Robin Beckman, Rebecca Lawrence, Alexandra Mendoza-Graf, and Alvin Nugroho for their assistance in data collection and data cleaning. This research was also supported by the National Heart Lung Blood Institute/National Cancer Institute (R01HL131531 and R01CA149105). We thank and acknowledge our community partners, Homewood Children’s Village and Hill Community Development Corporation as well as participants in the PHRESH cohort. We also would like to thank Bonnie Ghosh-Dastidar, Andrea Richardson, and Becky Collins for valuable feedback on this research.
Disclosure Statement
Financial Disclosure: Wendy Troxel serves on the scientific advisory board for Feelmore Labs, National Sleep Foundation, and OneCare Media and Associate Editor for Sleep Health and Behavioral Sleep Medicine.
Nonfinancial Disclosure: none.
Institution of Research and Declaration of Clinical Trial Status
Research was performed at the RAND Corporation. This manuscript does not report on a clinical trial.
Author Approval
All authors have seen and approve of this manuscript.
Author Declarations
This research was also supported by the National Institutes of Health/National Cancer Institute (R01HL131531 and R01CA149105). The authors declare no conflicts of interest related to the research in this manuscript.
References
- 1. Smith AR. Emergency department visits for COVID-19 by race and ethnicity—13 States, October–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(15):566–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Figueroa JF, et al. Association of race, ethnicity, and community-level factors with COVID-19 cases and deaths across U.S. counties. Healthc (Amst). 2021;9(1):100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee SY(Tim), et al. Hit Harder, Recover Slower? Unequal Employment Effects of the Covid-19 Shock. Cambridge, MA: National Bureau of Economic Research; 2021. [Google Scholar]
- 4. DOL. News Release: Unemployment Insurance Weekly Claims. https://www.dol.gov/sites/dolgov/files/OPA/newsreleases/ui-claims/20201058.pdf. Accessed March 10, 2021
- 5. Béland LP, et al. Covid-19, Stay-at-Home Orders and Employment: Evidence from CPS Data. Social Science Research Network; 2020. https://papers.ssrn.com/abstract=3608531. Accessed March 10, 2021. [Google Scholar]
- 6. Gebel M, et al. The impact of employment transitions on health in Germany. A difference-in-differences propensity score matching approach. Soc Sci Med. 2014;108:128–136. [DOI] [PubMed] [Google Scholar]
- 7. Margerison-Zilko C, et al. Health impacts of the great recession: a critical review. Curr Epidemiol Rep. 2016;3(1):81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cooper B. Economic recession and mental health: an overview. Neuropsychiatrie. 2011;25(3):113–117. [PubMed] [Google Scholar]
- 9. Michaud PC, et al. The effect of job loss on health: evidence from biomarkers. Labour Econ. 2016;41:194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burgard SA, et al. Toward a better estimation of the effect of job loss on health. J Health Soc Behav. 2007;48(4):369–384. [DOI] [PubMed] [Google Scholar]
- 11. Julià M, et al. Precarious employment and quality of employment in relation to health and well-being in Europe. Int J Health Serv. 2017;47(3):389–409. [DOI] [PubMed] [Google Scholar]
- 12. Catalano R. The health effects of economic insecurity. Am J Public Health. 1991;81(9):1148–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yoshioka E, et al. Effect of the interaction between employment level and psychosocial work environment on insomnia in male Japanese public service workers. Int J Behav Med. 2013;20(3):355–364. [DOI] [PubMed] [Google Scholar]
- 14. Grandner MA, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11(5):470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hyyppä MT, et al. Quality of sleep during economic recession in Finland: a longitudinal cohort study. Soc Sci Med. 1997;45(5):731–738. [DOI] [PubMed] [Google Scholar]
- 16. Ferrie JE, et al. The health effects of major organisational change and job insecurity. Soc Sci Med. 1998;46(2):243–254. [DOI] [PubMed] [Google Scholar]
- 17. Partinen M. Sleep research in 2020: COVID-19-related sleep disorders. Lancet Neurol. 2021;20(1):15–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jahrami H, et al. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jackson Chandra L., et al. Sleep disparities in the era of the COVID-19 pandemic highlight the urgent need to address social determinants of health like the virus of racism. J Clin Sleep Med. 16(8):1401–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johnson DA, et al. Are sleep patterns influenced by race/ethnicity – a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jackson CL, et al. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. 2015;36:417–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jackson CL, et al. Racial disparities in short sleep duration by occupation and industry. Am J Epidemiol. 2013;178(9):1442–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Troxel WM, et al. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep. 2018;41(10). doi: 10.1093/sleep/zsy140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bartel AP, et al. Racial and ethnic disparities in access to and use of paid family and medical leave: evidence from four nationally representative datasets. Mon Lab Rev. 2019;142:1. [Google Scholar]
- 25. Khubchandani J, et al. Association of job insecurity with health risk factors and poorer health in American workers. J Community Health. 2017;42(2):242–251. [DOI] [PubMed] [Google Scholar]
- 26. Manski CF, et al. Worker Perceptions of Job Insecurity in the Mid-1990s: Evidence from the Survey of Economic Expectations. Cambridge, MA: National Bureau of Economic Research; 1999. [Google Scholar]
- 27. Fullerton AS, et al. The role of job insecurity in explanations of racial health inequalities. In: Sociological Forum. Vol 28. Wiley Online Library; 2013:308–325. [Google Scholar]
- 28. Cowan BW. Short-Run Effects of COVID-19 on U.S. Worker Transitions. National Bureau of Economic Research; 2020. [Google Scholar]
- 29. Mongey S, et al. Which Workers Bear the Burden of Social Distancing Policies? Cambridge, MA: National Bureau of Economic Research; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wozniak A. Disparities and mitigation behavior during COVID-19. Minneapolis, MN: Federal Reserve Bank of Minneapolis; 2020. [Google Scholar]
- 31. Hall MH, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32(1):73–82. [PMC free article] [PubMed] [Google Scholar]
- 32. Jones J, et al. Trends in job quality for African-American workers, 1979–2011. Rev Black Polit Econ. 2016;43(1):1–19. [Google Scholar]
- 33. Storer A, et al. What explains racial/ethnic inequality in job quality in the service sector? Am Sociol Rev. 2020;85(4):537–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pew Research Center. About Half of Lower-Income Americans Report Household Job or Wage Loss Due to Covid-19; 2020. https://www.pewsocialtrends.org/wp-content/uploads/sites/3/2020/04/PSDT_04.21.20_covidfinance_FULL.REPORT.pdf. Accessed December 18, 2020. [Google Scholar]
- 35. Johnson DA, et al. The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep. 2016;39(7):1411–1419. doi: 10.5665/sleep.5974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ogedegbe G, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw Open. 2020;3(12):e2026881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Reitsma MB, et al. Racial/ethnic disparities in COVID-19 exposure risk, testing, and cases at the subcounty level in California. Health Aff (Millwood). 2021;40(6):870–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Azar KMJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253–1262. [DOI] [PubMed] [Google Scholar]
- 39. Lawton R, et al. A longitudinal study of convergence between Black and White COVID-19 mortality: a county fixed effects approach. Lancet Reg Health Am. 2021;1:100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. CDC. Cases, Data, and Surveillance. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed September 3, 2021. [Google Scholar]
- 41. Dubowitz T, et al. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Aff (Millwood). 2015;34(11):1858–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. DeSantis AS, et al. A preliminary study of a composite sleep health score: associations with psychological distress, body mass index, and physical functioning in a low-income African American community. Sleep Health. 2019;5(5):514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dubowitz T, et al. Results from a natural experiment: initial neighbourhood investments do not change objectively-assessed physical activity, psychological distress or perceptions of the neighbourhood. Int J Behav Nutr Phys Act. 2019;16(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Richardson AS, et al. Improvements in neighborhood socioeconomic conditions may improve resident diet. Am J Epidemiol. 2021;190(5):798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dubowitz T, et al. Does investing in low-income urban neighborhoods improve sleep? Sleep. 2021;44(6). doi: 10.1093/sleep/zsaa292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dubowitz T, et al. Food insecurity in a low-income, predominantly African American cohort following the COVID-19 pandemic. Am J Public Health. 2021;111(3):494–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hublin C, et al. Changes in sleep quality with age-a 36-year follow-up study of Finnish working-aged adults. J Sleep Res. 2018;27(4):e12623. [DOI] [PubMed] [Google Scholar]
- 48. Brooks Holliday S, et al. Do sleep and psychological distress mediate the association between neighborhood factors and pain? Pain Med. 2019;20(2):278–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yu L, et al. Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. 2011;10(1):6–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. VanderWeele TJ. On the distinction between interaction and effect modification. Epidemiology. 2009;20(6):863–871. [DOI] [PubMed] [Google Scholar]
- 51. Wilkins R, et al. Gender differences in involuntary job loss: why are men more likely to lose their jobs?. Ind Relat J Econ Soc. 2013;52(2):582–608. doi: 10.1111/irel.12024 [DOI] [Google Scholar]
- 52. Grandner MA, et al. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McLeod JD, et al. Socioeconomic status differences in vulnerability to undesirable life events. J Health Soc Behav. 1990;31(2):162–172. [PubMed] [Google Scholar]
- 54. Esping-Andersen G. Regulation and context: reconsidering the correlates of unemployment. In: Why Deregulate Labour Mark. Oxford: Oxford University Press, 2000:99–112. [Google Scholar]
- 55. Cohen J. Will global vaccine shortfalls end in 2022? Science. 2021;374(6575):1546. [DOI] [PubMed] [Google Scholar]
- 56. Sawilowsky SS. New effect size rules of thumb. J Mod Appl Stat Methods. 2009;8(2):26. [Google Scholar]
- 57. Ganong P, et al. US unemployment insurance replacement rates during the pandemic. J Public Econ. 2020;191:104273. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.