Abstract
The COVID-19 pandemic has forced federal, state, and local policymakers to respond by legislating, enacting, and enforcing social distancing policies. However, the impact of these policies on healthcare utilization in the United States has been largely unexplored. We examine the impact of county-level shelter in place ordinances on healthcare utilization using two unique datasets—employer-sponsored insurance for over 6 million people in the US and cell phone location data. We find that introduction of these policies was associated with reductions in the use of preventive care, elective care, and the number of weekly visits to physician offices, hospitals and other health care-related industries. However, controlling for county-level exposure to the COVID-19 pandemic as a way to account for the endogenous nature of policy implementation reduces the impact of these policies. Our results imply that while social distancing policies do lead to reductions in healthcare utilization, much of these reductions would have occurred even in the absence of these policies.
Keywords: COVID-19 pandemic, Health care utilization, Telehealth, Shelter-in-place policies
Introduction
The COVID-19 pandemic has impacted health systems and economies throughout the United States and the world. It is expected that the total economic cost of the pandemic may reach 16 trillion dollars (Cutler and Summers 2020). In the United States, policymakers have responded by enacting federal and state policies that seek to “flatten the curve” through shelter-in-place (SIP) policies that encourage social distancing. Previous research suggests that these policies had their intended effect and reduced spread of COVID-19 infection in the United States (Amuedo-Dorantes et al., 2020; Courtemanche et al., 2020; Matrajt and Leung 2020).
However, evidence on the impacts of social distancing and SIP policies on healthcare utilization remains limited (Ziedan et al., 2020). In previous work, we examined changes in use of preventive healthcare services, both in-person and telemedicine visits, after the declaration of nationwide emergency in March 2020 (Whaley et al., 2020). Consistent with other studies, we find that the use of preventive and elective services declined drastically, and that the share of visits replaced by telemedicine did not fully replace the gap (Mehrotra et al., 2020). However, it is unclear from this evidence whether the decline in utilization was in response to implementation of SIP policies or due to patients’ fears of COVID-19 infection while in a healthcare facility.
The effects of SIP policies on healthcare use are a-priori ambiguous. While the decline in COVID-19 cases associated with these policies might instill public confidence and encourage people to seek healthcare, SIP policies might encourage the public to stay at home and avoid doctors’ offices and hospitals. If these policies do reduce necessary medical care, then, while they may limit the spread of COVID-19, they may also impose costs. If delayed or forgone care worsens patient health outcomes, then the positive COVID-related health impacts of SIP policies must be balanced with the potentially adverse consequences of SIP policies on non-COVID care. Appropriately weighing these tradeoffs requires precise estimation of the impact of SIP policies on non-COVID care.
In this paper, we attempt to inform these tradeoffs by examining the effect of SIP polices on use of healthcare services. An important empirical challenge with evaluating the impacts of these policies is the endogenous nature of their implementation (Goodman-Bacon and Marcus 2020). While there is variation in the timing of implementation of SIP policies across counties, which can be used to identify the effects of these policies on health care utilization, counties might have implemented these policies in response to or concurrently with rising COVID cases. Therefore, it is important to disentangle the effects of SIP policies from the effects of changes in trajectory of the COVID-19 pandemic within a county. We address this potential endogeneity of SIP policies by non-parametrically controlling for the number of weeks since the first COVID-19 case and COVID-19 death in each county.
To assess the impacts of SIP policies on health services utilization, we used claims data from a nationwide sample of U.S. individuals with employer-sponsored health insurance. Our results indicate that county-level SIP policies appear to be endogenously implemented in response to COVID-19 exposure. We find large reductions in use of preventive care and elective services following the introduction of SIP policies. We find that fully controlling for variations in exposure to the COVID-19 pandemic significantly reduces the magnitude of SIP policies on healthcare utilization. For example, when not controlling for variations in COVID-19 exposure SIP policies are associated with 37% reduction in the use of mammograms. Adding COVID-19 controls for the number of weeks since the first COVID-19 case and death within a county reduces the impact of SIP policies on use of mammograms to 12%. We find similar reductions for other forms of preventive (e.g., colonoscopy screenings and infant immunizations) and elective care (e.g., MRIs, musculoskeletal surgery, and cataract surgery). In contrast, we find small changes in non-elective care (chemotherapy and angiograms) and no change in labor and delivery rates. Thus, while use of health services has declined during the COVID-19 pandemic, the decline is not due solely to SIP policies. Instead, variation in reductions in care are driven by both the implementation of SIP policies and variations in the intensity of the COVID-19 pandemic across counties. Our results imply that while SIP policies do lead to reductions in preventive and elective care, much of these reductions would have occurred even in the absence of these policies. We confirm our main findings by using cellphone geo-tracking data on in-person visits to physicians, hospitals, and other health care providers.
Additionally, we examine changes in telemedicine and in-person office visits because many providers have shifted towards telemedicine services during the pandemic, based on recommendations from Centers for Disease Control and Prevention (CDC) (Centers for Disease Control and Prevention 2020). For example, over 9 million Medicare beneficiaries have received a telemedicine service during the public health emergency, mid-March through mid-June (Verma 2020). Similarly, between March 2 and April 14, 2020, telemedicine visits increased from 102.4 daily to 801.6 daily at NYU Langone Health (Mann et al., 2020). Data from four national telehealth providers showed a 154 percent increase in telehealth visits during the last week of March 2020 compared to the same period in 2019 (Koonin et al., 2020). Consistent with the existing literature, we also find that even after controlling for variations in the intensity of the COVID-19 pandemic, the implementation of SIP policies led to a 10% reduction in the use of office-based clinician visits and a 53% increase in the use of telemedicine. However, the absolute change in telemedicine only offset 48% of the reduction in office-based clinician visits. Our results echo previous work which has also confirmed that telemedicine visits have not fully replaced office-based visits (Ziedan et al., 2020). Previous analysis of employer-based claims data indicates that patients living in zip codes with lower-income or majority racial/ethnic minority populations experienced smaller reductions in in-person visits but also had lower rates of adoption of telemedicine (Whaley et al., 2020).
We believe that these results have several important implications for public policy. First, our finding that necessary care has been delayed suggests that additional policies designed to restore avoided care may be required. This concern has been echoed by other studies (Jain and Santhosh 2020; Ziedan et al., 2020; Czeisler 2020). Second, for some patients, delaying necessary care could have potential adverse health impacts in the future. These non-COVID-19 health impacts are currently not fully accounted for in the health impacts of the COVD-19 pandemic nor the impact of SIP policies (Woolf et al., 2020). These impacts are also not a major focus in the current discussion on the impact of the pandemic on healthcare disparities despite the fact deferred care is happening disproportionately in some populations (Czeisler 2020). Third, the pandemic, SIP policies and their associated decline in utilization might also affect the supply side of the market. For example, the decline in utilization of care is expected to have severe impacts on healthcare provider finances (Farr 2020). This impact is in stark contrast to insurers where lower use of health care will improve their profitability putting them in a strong financial position to withstand COVID-19 (Lucia et al., 2020). The decline in health care utilization also seems to be impacting employment in the health care industry. Between March and April of 2020 alone, the ambulatory workforce fell by 1.19 million persons, a 14.9% drop, and the number of hospital employees decreased by 135, 000 (a 2.6% decline) (Himmelstein and Woolhandler 2020). Finally, we use real time cellphone mobility data on weekly visits to offices of physicians and hospitals to confirm the results of the detailed claims data. This is an important finding given that it suggests that regulators, healthcare providers, and health departments can use these types of data to make more rapid decisions on public health interventions.
The rest of the paper proceeds as follows. First, we outline the data sources and measures used in the present study. Second, we define the methods used for evaluating the impact county-level SIP policies on county-level healthcare utilization. Third, we report the results. Finally, we contextualize the results within the broader literature and present policy implications.
Data
Medical claims data
Our primary source of data on healthcare utilization comes from weekly aggregates of medical claims data collected by Castlight Health in 2019 and 2020. The panel covers all of calendar year 2019 through October 28, 2020. Castlight provides price transparency and health benefits to self-insured employers. As part of operating these services, Castlight receives medical claims data for all employees and beneficiaries of their employer customers. The customers vary in both size—ranging from 500 to 50,000 individuals—and in industry—including manufacturing, education, and financial services. The data covers all U.S. states and the District of Columbia. Throughout the analysis we focus on the under-age 65 population. The sample contains 6.4 million people in 2019 and 6.8 million people in 2020.
We obtained de-identified information on the number of patients, number of claims, and spending for common preventive care (colonoscopies for persons ages 46 to 64, mammograms for women ages 46 to 64, and vaccines and immunizations for children ages two and younger), elective (MRIs, musculoskeletal surgery, and cataract surgery), and non-elective (labor and delivery, chemotherapy, and angioplasty) services. We also obtained information on patient demographics (age, and gender), geographic market (state and county), and the number of eligible members within each cell. We used this information to calculate the weekly number of patients who received each procedure per 10,000 eligible persons. We similarly obtained the number of telemedicine interactions for this population.1
The demographics of the Castlight sample in both years are similar to the 2018 American Community Survey population that receives insurance coverage from an employer, as exhibited in Table 1 . We do not have access to individual-level race/ethnicity, income, or education information, and so are unable to directly test how the Castlight population compares to the broader population with employer-sponsored insurance along socioeconomic status dimensions. Because the Castlight population receives insurance coverage from an employer, our study population likely has higher income and education levels than the general population.
Table 1.
Unadjusted Descriptive Statistics of Castlight Health population and American US Community Survey.
| Castlight Health (2019)+ | Castlight Health (2020)+ | ACS (2018) | |
|---|---|---|---|
| Number of enrolled persons | 6389,425 | 6828,031 | 162,136,077 |
| Gender, percent female (%) | 49.5% | 49.5% | 50.0% |
| Average age | 34.3 | 34.5 | 33.5 |
| Census region | |||
| South | 40.0% | 39.5% | 35.7% |
| Midwest | 23.2% | 24.4% | 22.8% |
| Northeast | 10.8% | 11.4% | 18.2% |
| West | 25.9% | 24.7% | 23.4% |
Castlight Health population limited to those ages 0 to 64.
Cellphone-based measures of healthcare utilization
In conjunction with medical claims data, we use data from SafeGraph as a second way to measure healthcare utilization. SafeGraph aggregates GPS pings from about 6 million points-of-interest (POI). The effect of this is measurements of traffic patterns, both to a large collection of POIs, and to/from residences of the users. We used the “Weekly Patterns” data from SafeGraph to quantify office-based healthcare utilization. In this dataset, for each weekly file, SafeGraph makes one row for each POI. For each POI, SafeGraph reports its geographic location, industry via the National American Industry Classification System (NAICS) code, and the total number of visitors in their mobile device panel that have visited each day. The weekly data measures begin on Monday and end the following Sunday. Since visits to each facility is a length 7 array, we are able to calculate this every day, then combine for each week for 2019 and 2020. We use the four-digit NAICS code to identify office of physicians (6211), general medical and surgical hospitals (6221) health and personal care stores (4461), offices of dentists (6212), medical and diagnostic laboratories (6215), nursing care facilities (6231), retirement communities and assisted living facilities (6233), and specialty hospitals (6223).2 These data have been commonly used to examine the effect of COVID-19 and COVID-19 related policies on social distancing (Cronin and Evans 2020; Goolsbee and Syverson 2020; Gupta et al., 2020; Cook et al., 2020; Moreland 2020; Gao et al., 2020). To our knowledge, there are only four studies that have used the SafeGraph data to measure utilization of healthcare services, proxied by either visits to hospitals (Jay et al., 2020), substance use disorder treatment facilities (Cantor et al., 2021), dental offices (Kranz et al., 2021), or abortion clinics (Andersen et al., 2020).
Data on social distancing policies
To measure county-level SIP policies, we use data collected by Cook et al. (2020). The data include SIP policies from the New York Times and local news and government websites. The authors collected the dates for statewide orders from the New York Times (The New York Times 2020). For states without a state-wide order the authors searched local news and government sites for SIP policy dates for individual counties. Counties that the authors failed to find a news report or website that contained a SIP policy were assumed to have followed the state's policy (Cook et al., 2020).
COVID-19 cases and deaths
We obtained the total number of COVID-19 cases and deaths for each county from USAFacts (USAFacts 2020). These data have been used in previous studies examining disparities in COVID-19 case rates (Adhikari et al., 2020; Brown and Ravallion 2020). The data are accumulated by the Centers for Disease Control and Prevention (CDC) using information from state public health websites. The data track the total number of COVID-19 cases and deaths in each county for each day. Based on these data we identified the week of the first COVID-19 case and COVID-19 death for each county.
Estimation approach
Effect of social distancing policies on healthcare utilization
To estimate the effect of SIP on healthcare utilization, we would ideally estimate two-way fixed effects difference-in-difference models that estimate the difference in utilization following the implementation of a SIP policy. However, a key challenge of the validity of this type of approach is the endogenous nature of SIP policies, which are likely implemented in response to growth in the COVID-19 pandemic. We attempt to address this limitation by controlling for county-level variations in exposure to the COVID-19 pandemic.
Our main approach uses non-parametric controls for the duration of exposure to the COVID-19 pandemic in each county. For each county and week , we calculate the number of weeks since the first COVID-19 case () and death () in that county. We avoid directly controlling for the number of COVID-19 cases or deaths because both cases and deaths could be impacted by the implementation of SIP policies. We estimate a regression that includes fixed effects for each measure of COVID-19 exposure duration:
| (1) |
In this model, represents the number of patients per 10,000 eligible members who receive each of the selected procedures. Using a dependent variable in level-terms allows for an absolute comparison in changes in utilization across procedures. To allow for a relative comparison, we also estimate models that use the log-transformed number of patients who receive each procedure. Patients () are grouped into cells at the age category, gender, and county level. We include controls for patient demographics—age and gender, in . We also include fixed effects for calendar week, year, and county. We also interact the year and week fixed effects to control for the nationwide trajectory of the COVID-19 pandemic. We weight each regression by the number of eligible members within each sample cell. We estimate these models using ordinary least squares and cluster standard errors at the county level. As an additional sensitivity test, we examine heterogeneous effects of SIP policies on utilization based on patient age, and the county's income and race composition.3
The coefficient measures the effect of SIP policies, indexed by , on utilization. For this coefficient to have a causal interpretation, there must not be an unobservable that changes both the implementation of policies () and utilization of care. Given the scope of the COVID-19 pandemic, the validity of this assumption may be challenging. In particular, changes in COVID-19 cases could lead to both implementation of policies and concerns of infection that lead to care avoidance that would have occurred even in the absence of formal policy declarations. Our controls for the duration of exposure and the nationwide trajectory of the COVID-19 pandemic attempt to address the potential endogeneity of SIP policies. We iteratively add these controls to assess the impacts of controlling for variations in exposure to COVID-19 on the impacts of SIP policies. To highlight the importance of the week since first COVID-19 case and death controls, Appendix Figs. 3 and 4 plot these fixed effects.
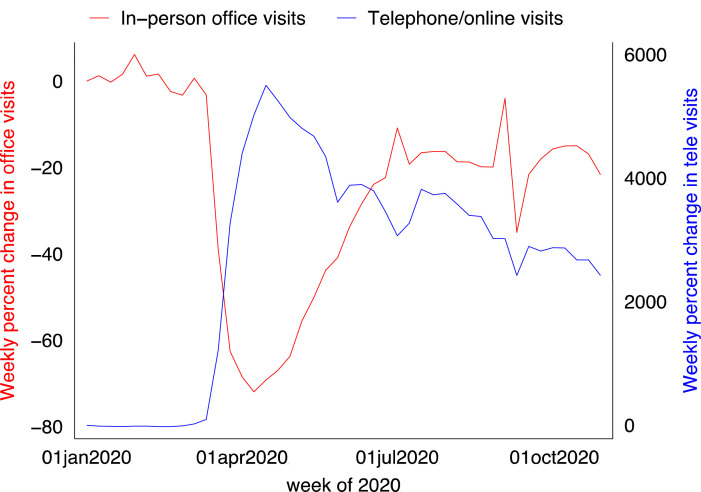
Fig. 3.
Unadjusted trends in in-person office visits and telemedicine use.
Caption: Figures show the unadjusted percent change in utilization of in-person office visits (red line, left axis) and telemedicine visits (blue line, right axis), relative to utilization rates per 10,000 for the same week in 2019.
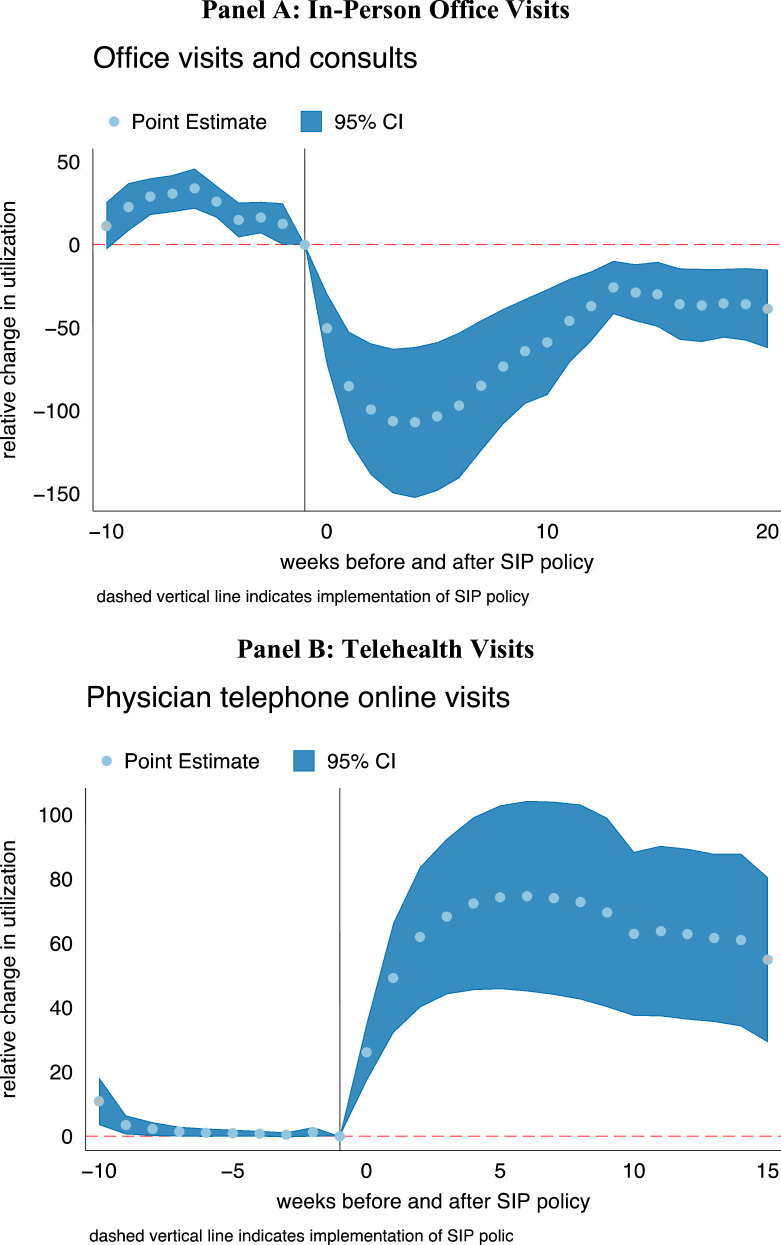
Fig. 4.
Event studies results of effect of social distancing policies on in-person office visit and telehealth utilization.
Caption: These event study figures show changes in regression-adjusted utilization of each service in the weeks before and after the county-level implementation of shelter-in-place policies. Regression models were estimated using ordinary least squares. Regression models include controls for the patient's age and gender, and fixed effects for week and county. The outcome measure is the number of patients, and all models are weighted for the total number of eligible enrollees. Standard errors are clustered at the county level.
We test for pre- and post-implementation trends using an event study approach. For the 10 weeks before and the 20 weeks following implementation of policy implementation, we estimate weekly differences in use of each procedure using a regression of the form
| (2) |
In this specification, the coefficients test the impacts of the policy in the weeks before and after implementation. As additional tests, we also estimate similar event studies that use each counties week of the first COVID-19 death and the first week with at least 10 COVID-19 deaths in the county as alternative policies.
Results
Effect of sip policies on use of preventive, elective, and non-elective care
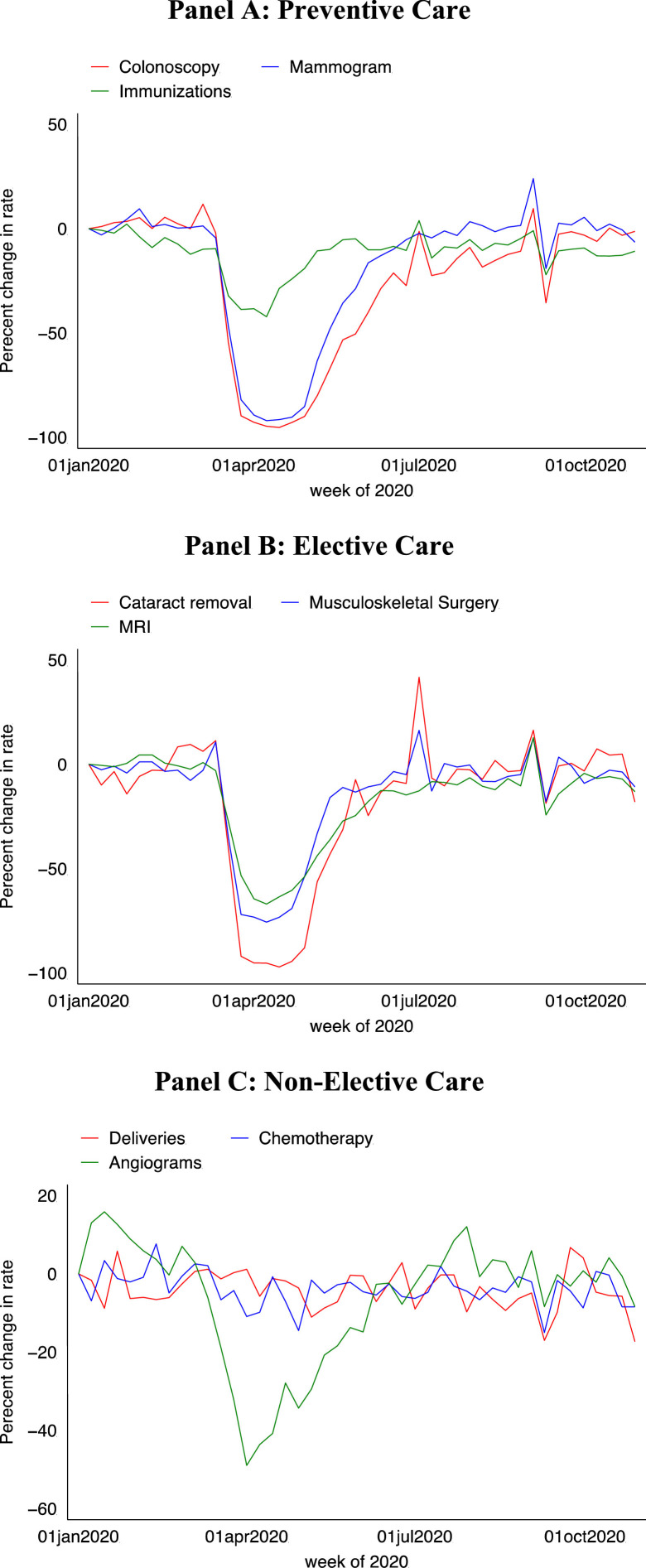
Fig. 1 presents unadjusted trends in the use of preventive (Panel A), elective (Panel B), and non-elective care (Panel C). For each outcome, 2020 use rates are relative to the use rates in the same week in 2019. For all three care categories, we observe stable trends in January and February. Beginning in March, after the declaration of the pandemic in the US, preventive and elective care use rates decline rapidly. The trends for non-elective care are more stable. Beginning in approximately June 2020, we observe large rebounds in care. By July 2020, utilization levels substantially rebounded, but not sufficiently to offset earlier reductions in care.
Fig. 1.
Unadjusted trends in healthcare service utilization.
Caption: Figures show the unadjusted percent change in utilization of each service, relative to utilization rates per 10,000 for the same week in 2019. Immunizations are restricted to those aged 2 or younger. Colonoscopies are restricted to those 46 or older. Mammograms were restricted to females aged 46 or older. Deliveries were restricted to women between the ages of 19 and 45.
While the unadjusted figures show reductions in care, they do not identify how policy responses to limit the spread of COVID-19 impacted non-COVID-19 healthcare services. Table 2 presents difference-in-difference estimates of changes in care utilization following county-level SIP policies. The unit of observation is at the week, county, gender, and age-group level.4 For colonoscopies, the first three columns, utilization rates decreased by 1.9 per 10,000 persons following SIP laws when not controlling for the county-level COVID-19 exposure, which translates to a 47% reduction when compared to the baseline mean utilization rate in the ninth week of 2019. Non-parametrically controlling for the weeks since the first COVID-19 case and death and interacting the week and year fixed effects substantially reduces the impact of SIP policies on colonoscopy use (columns 2–3). In the preferred specification in column 3 that includes the full set of controls, the introduction of SIP policies lead a 0.7-person decrease in the use of colonoscopies, a relative decrease of 16%. Thus, controlling for the trajectory of the COVID-19 pandemic reduces the impact of SIP policies on colonoscopy utilization by 65%.
Table 2.
Effect of social distancing policies on preventive, elective, and non-elective procedure utilization.
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | |
|---|---|---|---|---|---|---|---|---|---|
| Panel A: Preventive Care | Colonoscopy | Mammogram | Immunizations | ||||||
| post shelter in place | −1.909*** | −1.279*** | −0.663*** | −7.986*** | −4.181*** | −2.498*** | −3.891*** | −0.208 | −1.608*** |
| (0.428) | (0.274) | (0.212) | (1.613) | (1.061) | (0.964) | (0.849) | (1.400) | (0.560) | |
| Weeks since first case FE | X | X | X | X | X | X | |||
| Weeks since first death FE | X | X | X | X | X | X | |||
| Year X Week FE | X | X | X | ||||||
| Observations | 1064,825 | 1064,825 | 1064,825 | 529,256 | 529,256 | 529,256 | 418,103 | 418,103 | 418,103 |
| R-squared | 0.703 | 0.714 | 0.749 | 0.781 | 0.792 | 0.816 | 0.88 | 0.894 | 0.904 |
| baseline mean | 4.1 | 4.1 | 4.1 | 21.6 | 21.6 | 21.6 | 22.0 | 22.0 | 22.0 |
| Panel B: Elective Care | MRI | Musculoskeletal surgery | Cataract surgery | ||||||
| post shelter in place | −1.096*** | −0.687*** | −0.204** | −0.282*** | −0.155*** | −0.106** | −0.0629*** | −0.0560** | −0.0174 |
| (0.237) | (0.140) | (0.0866) | (0.0664) | (0.0403) | (0.0434) | (0.0185) | (0.0223) | (0.0123) | |
| Weeks since first case FE | X | X | X | X | X | X | |||
| Weeks since first death FE | X | X | X | X | X | X | |||
| Year X Week FE | X | X | X | ||||||
| Observations | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 |
| R-squared | 0.616 | 0.619 | 0.628 | 0.488 | 0.491 | 0.499 | 0.255 | 0.258 | 0.263 |
| baseline mean | 3.3 | 3.3 | 3.3 | 1.1 | 1.1 | 1.1 | 0.2 | 0.2 | 0.2 |
| Panel C: Non-Elective Care | Labor and delivery | Chemotherapy | Angiograms | ||||||
| post shelter in place | −0.111 | −0.0493 | 0.0675 | −0.128*** | −0.164*** | −0.0809** | −0.134*** | −0.0615* | −0.0188 |
| (0.0783) | (0.0942) | (0.0797) | (0.0402) | (0.0393) | (0.0348) | (0.0287) | (0.0352) | (0.0199) | |
| Weeks since first case FE | X | X | X | X | X | X | |||
| Weeks since first death FE | X | X | X | X | X | X | |||
| Year X Week FE | X | X | X | ||||||
| Observations | 1064,971 | 1064,971 | 1064,971 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 |
| R-squared | 0.555 | 0.556 | 0.556 | 0.542 | 0.543 | 0.544 | 0.439 | 0.441 | 0.442 |
| baseline mean | 1.8 | 1.8 | 1.8 | 1.5 | 1.5 | 1.5 | 0.5 | 0.5 | 0.5 |
Caption: Baseline means are calculated based on the ninth week of 2019. Regression models were estimated using ordinary least squares. Regression models also include controls for the patient's age and gender, and fixed effects for week and county. The outcome measure is the number of patients, and all models are weighted for the total number of eligible enrollees. Standard errors are clustered at the county level. Immunizations are restricted to those aged 2 or younger. Colonoscopy is restricted to those 46 to 64. Mammograms were restricted to females aged 46 to 64. Deliveries were restricted to women between the ages of 19 and 45. *** p<0.01, ** p<0.05, * p<0.1.
In the rest of Panel A, we observe similar results for the two other forms of preventive services—mammograms for women ages 46 to 64 (columns 4–6) and immunizations for children under the age of two (columns 7–9). SIP laws lead to an 8.0-person decline (37% relative reduction) in use of mammograms when not controlling for COVID-19 exposure. The effect falls by 69% to a 2.5-person reduction (12% relative reduction) when fully controlling for COVID-19 exposure. For immunizations, we find a 3.9-person reduction (18% relative reduction) when not controlling for COVID-19 exposure and a 1.6-person reduction (7% relative decline) when fully controlling for COVID-19 exposure.
SIP policies lead to similarly-sized reductions in the use of elective procedures, and the effect of SIP policies is again influenced by county exposure to the COVID-19 pandemic (Panel B). For MRIs, musculoskeletal surgery, and cataract surgery, we find absolute reductions of 1.1, 0.3, and 0.06 per 10,000 when not controlling for COVID-19 exposure, respectively. These absolute reductions translate to relative reductions of 33%, 26%, and 300% in the use of each service. However, adding the full set of COVID-19 controls reduces the impact of SIP policies on elective healthcare utilization by approximately 70%. In columns 3, 6, and 9, we find absolute reductions of 0.2, 0.1, and 0.02, which translate into relative reductions of 6%, 10%, and 8%.
For non-elective care (Panel C), we observe smaller changes following SIP policies. We do not observe changes in labor and delivery rates following SIP policies. We find a small reduction in use of chemotherapy (columns 4–6). When including the full set of COVID-19 controls, we find a 0.08-person reduction in chemotherapy rates, which translates to a 5% relative reduction. For cardiac angiograms, we find a 24% relative reduction when not controlling for COVID-19 exposure, but no effect when including the full set of COVID-19 controls.
As shown in Table 3 , we find similar results when using the log-transformed number of patients with each visit. For preventive care and when fully controlling for county-level exposure to the COVID-19 pandemic, we find a 9% reduction in the use of colonoscopies,5 a 8% reduction in mammogram use, and a 6% reduction in infant immunization rates. The effects of SIP policies are approximately 65% of the magnitude of the estimated effect when not controlling for exposure to the COVID-19 pandemic (columns 1, 4, and 7). We do not find that SIP policies led to large relative reductions in MRI, musculoskeletal surgery, and cataract surgery elective procedures when controlling for variations in exposure to COVID. The overall effects are similar. The magnitude of reduction in care following the implementation of SIP policies falls by approximately 80% when controlling for the county-level intensity of the COVID-19 pandemic. For non-elective care, we do not find changes in procedure rates in the specifications with the full set of controls.
Table 3.
Effect of social distancing policies on log-transformed preventive, elective, and non-elective procedure utilization.
| (1) | (4) | (5) | (6) | (9) | (10) | (11) | (14) | (15) | |
|---|---|---|---|---|---|---|---|---|---|
| Panel A: Preventive Care | Colonoscopy | Mammogram | Immunizations | ||||||
| post shelter in place | −0.341*** | −0.248*** | −0.0910*** | −0.384*** | −0.410*** | −0.0828*** | −0.122*** | −0.0832*** | −0.0583*** |
| (0.0341) | (0.0418) | (0.0285) | (0.0224) | (0.0527) | (0.0276) | (0.0134) | (0.0200) | (0.0199) | |
| Weeks since first case FE | X | X | X | X | X | X | |||
| Weeks since first death FE | X | X | X | X | X | X | |||
| Year X Week FE | X | X | X | ||||||
| Observations | 1064,825 | 1064,825 | 1064,825 | 529,256 | 529,256 | 529,256 | 418,103 | 418,103 | 418,103 |
| R-squared | 0.737 | 0.753 | 0.779 | 0.867 | 0.888 | 0.902 | 0.927 | 0.928 | 0.929 |
| baseline mean | 4.1 | 4.1 | 4.1 | 21.6 | 21.6 | 21.6 | 22.0 | 22.0 | 22.0 |
| Panel B: Elective Care | MRI | Musculoskeletal surgery | Cataract surgery | ||||||
| post shelter in place | −0.161*** | −0.119*** | −0.0209 | −0.0849*** | −0.0624*** | −0.0307*** | −0.0261*** | −0.0211*** | −0.00406 |
| (0.0159) | (0.0204) | (0.0132) | (0.0120) | (0.0121) | (0.0107) | (0.00570) | (0.00695) | (0.00588) | |
| Weeks since first case FE | X | X | X | X | X | X | |||
| Weeks since first death FE | X | X | X | X | X | X | |||
| Year X Week FE | X | X | X | ||||||
| Observations | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 |
| R-squared | 0.716 | 0.718 | 0.721 | 0.55 | 0.553 | 0.558 | 0.295 | 0.298 | 0.303 |
| baseline mean | 3.3 | 3.3 | 3.3 | 1.1 | 1.1 | 1.1 | 0.2 | 0.2 | 0.2 |
| Panel C: Non-Elective Care | Labor and delivery | Chemotherapy | Angiograms | ||||||
| post shelter in place | −0.0261*** | −0.0131 | −0.00882 | −0.0369*** | −0.0303*** | −0.0142 | −0.0531*** | −0.0350*** | −0.0109 |
| (0.00822) | (0.0120) | (0.00895) | (0.00599) | (0.00831) | (0.00902) | (0.00843) | (0.0102) | (0.00682) | |
| Weeks since first case FE | X | X | X | X | X | X | |||
| Weeks since first death FE | X | X | X | X | X | X | |||
| Year X Week FE | X | X | X | ||||||
| Observations | 1064,971 | 1064,971 | 1064,971 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 |
| R-squared | 0.646 | 0.646 | 0.646 | 0.626 | 0.626 | 0.626 | 0.477 | 0.479 | 0.479 |
| baseline mean | 1.8 | 1.8 | 1.8 | 1.5 | 1.5 | 1.5 | 0.5 | 0.5 | 0.5 |
Caption: Baseline means are calculated based on the ninth week of 2019. Regression models were estimated using ordinary least squares. Regression models also include controls for the patient's age and gender, and fixed effects for week and county. The outcome measure is the natural log for the number of patients, and all models are weighted for the total number of eligible enrollees. Standard errors are clustered at the county level. Immunizations are restricted to those aged 2 or younger. Colonoscopy is restricted to those 46 to 64. Mammograms were restricted to females aged 46 to 64. Deliveries were restricted to women between the ages of 19 and 45. *** p<0.01, ** p<0.05, * p<0.1.
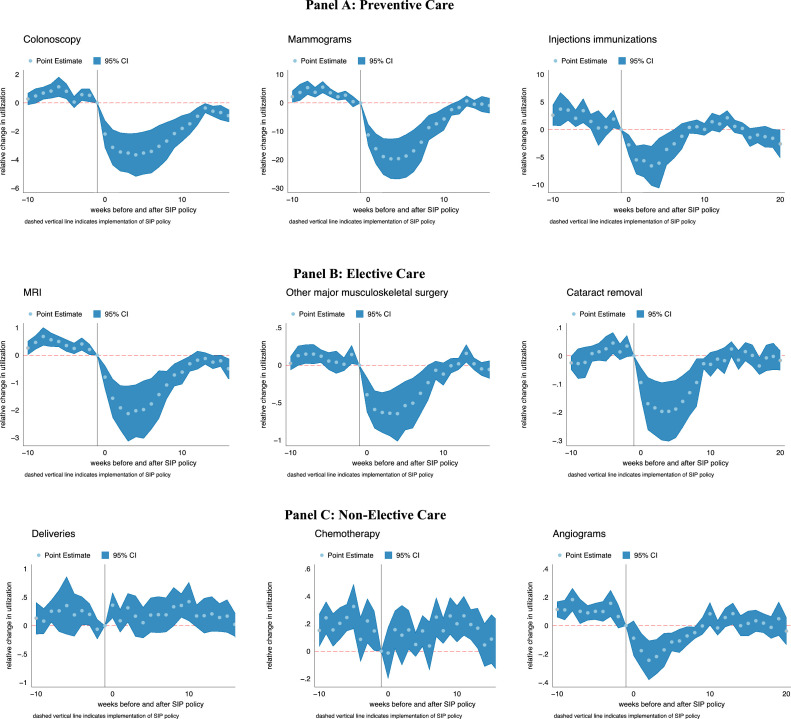
Event study results
We next estimate event studies that examine weekly trends in the use of each procedure for the year 2020. As shown in Fig. 2 , the event study results are similar to the previously discussed regression results. Following the implementation of SIP policies, we observe reductions in use rates for preventive and elective care, but smaller or no change in weekly trends for non-elective care. Importantly, we do also find some evidence that the reduction in utilization occurs in the one- or two-week period prior to the implementation of a SIP policies. This immediate pre-trend suggests that, consistent with the regression results, SIP policies are implemented in response to COVID-19 exposure, which concurrently contributes to reductions in use of preventive and elective services.
Fig. 2.
Event studies on effect of social distancing policies on preventive, elective, and non-elective procedure utilization.
Caption: These event study figures show changes in regression-adjusted utilization of each service in the weeks before and after the county-level implementation of shelter-in-place policies. Regression models were estimated using ordinary least squares. Regression models include controls for the patient's age and gender, and fixed effects for week and county. The outcome measure is the number of patients, and all models are weighted for the total number of eligible enrollees. Standard errors are clustered at the county level. Immunizations are restricted to those aged 2 or younger. Colonoscopy is restricted to those 46 to 64. Mammograms were restricted to females aged 46 to 64. Deliveries were restricted to women between the ages of 19 and 45.
In Appendix Figs. 1 and 2, we find similar patterns when using the week of the first COVID-19 death and the first week with 10 deaths. For both alternative policies, care utilization begins to decline in the weeks prior to the index week. At approximately 15 weeks following the index week, care utilization has rebounded to pre-pandemic levels.
Substitution of in-person office visits with telehealth visits
Similar to the procedure-level trends, Fig. 3 presents unadjusted weekly trends in the use of in-person office visits and telemedicine. Through February 2020, office visit trends were stable and averaged approximately 615 visits per week. During this period, telemedicine visits were minimal, and averaged 2.8 calls per 10,000 patients per week. Beginning in March 2020, there is a clear reduction in-person office visits and a corresponding spike in telemedicine use. By the end of April, in-person office visits decreased to 217 per 10,000 persons, relative to the year prior, an absolute reduction of 397 visits per 10,000 persons and a relative decrease of 64%. Use of telemedicine services increased from 3.7 to 206 per 10,000 persons, a relative increase of 5468%. However, the absolute increase in the use of telemedicine only offsets approximately 51% of the decline in-person office visits.
These descriptive findings are confirmed in the regression results presented in Table 4 . Panel A presents level changes and Panel B presents log changes. In column 1, following SIP laws, use of in-person office visits declined by 69.4 persons per 10,000. The inclusion of fixed effects for the number of weeks since the first COVID-19 case and death within the county reduces the magnitude of the SIP policy coefficient to 51.3 (column 2). Including the week-year fixed effect interactions, the preferred specification, further reduces the SIP coefficient to 17.0 (column 3). In Panel B, when using log-transformed in-person office visits, SIP policies lead to a 36% reduction in use of in-person office visits (column 1), which decreases to a 10% reduction when including the full set of controls (column 3).
Table 4.
Effect of social distancing policies and COVID-19 exposure on in-person office visit and telemedicine utilization.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| In-person office visits | Telemedicine | |||||
| Panel A: Level changes | ||||||
| post shelter in place | −69.40*** | −51.28*** | −16.99*** | 53.64*** | 35.77*** | 8.153** |
| (13.94) | (8.937) | (4.380) | (11.58) | (6.745) | (3.300) | |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 |
| R-squared | 0.725 | 0.729 | 0.751 | 0.387 | 0.425 | 0.595 |
| baseline mean | 161.8 | 161.8 | 161.8 | 1.4 | 1.4 | 1.4 |
| Panel B: Log changes | ||||||
| post shelter in place | −0.444*** | −0.391*** | −0.105*** | 1.935*** | 0.980*** | 0.426*** |
| (0.0195) | (0.0407) | (0.0212) | (0.0886) | (0.109) | (0.0660) | |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 | 3567,685 |
| R-squared | 0.937 | 0.941 | 0.945 | 0.794 | 0.810 | 0.856 |
Caption: Baseline means are calculated based on the ninth week of 2019. Regression models were estimated using ordinary least squares. Regression models include controls for the patient's age and gender, and fixed effects for week and county. The outcome measure is the number of patients, and all models are weighted for the total number of eligible enrollees. Standard errors are clustered at the county level. *** p<0.01, ** p<0.05, * p<0.1.
The same factors that cause a reduction in-person office visits also lead to an increase in telemedicine visits. SIP policies lead to a 53.6-person increase in the use of telemedicine when not controlling for variation in COVID-19 exposure, and an 8.2-person increase when adding the full set of COVID-19 controls. In relative terms (Panel B), the preferred specification in column 6 shows a 53% increase in the use of telemedicine, which is smaller than the estimated 592% in column 4 when not controlling for county-level COVID-19 exposure. However, the large relative shift towards telemedicine does not offset the even larger absolute reduction in-person office visits. The ratio between the absolute change coefficients in columns 3 and 6 (e.g., 8.15 / 16.99) shows that the increase in telemedicine offsets only approximately 48% of the decline in-person office visits.
These patterns are made clear in Fig. 4 , which plots event study results for both services. For in-person office visits (Panel A), we observe a decline in use that begins prior to the implementation of SIP policies. Following implementation, utilization continues to decline and stabilizes around week 15. For telehealth (Panel B), use immediately spikes following the implementation of SIP policies and then levels off at approximately five weeks post-SIP implementation.
Changes in healthcare utilization using mobile tracking data
As an additional test, we estimate changes in in-person visits to health care providers using mobile tracking data. An advantage of the mobile tracking data is that it does not come from insurance claims, which are limited to the population covered by the respective insurer. Instead, the mobile tracking data allow us to observe in-person visits to particular providers across all patient populations, including those without insurance. In Appendix Figures 5 and 6, we report the unadjusted number of weekly visits to healthcare providers and pharmacies in 2020. The number of weekly visits dropped drastically for each type of location after the national emergency declaration. For the regression models, we obtain similar results when using mobile tracking data that measures the weekly number of visits to healthcare providers (Tables 5 and 6 ). For physician office visits, columns in columns 1 and 2, we find that weekly visits to physicians decreased by 9.3 and 3.4 following the introduction of SIP policies, a relative decrease of 30% and 11% respectively. The dependent variable is weekly foot traffic to locations of individual offices of physicians. Panel B presents log-transformed visits, which can be interpreted as relative changes. Because the SafeGraph data derives from a sample approximately 10% of all cell phone users, the absolute reductions are an underestimate of the absolute changes in visits. The estimated impact of SIP laws falls considerably when controlling for the number of weeks since the first COVID-19 case and death and the additional inclusion of week by year fixed effects. In Panel A, we fail to find a statistically significant result after controlling for the week by year fixed effects. However, in Panel B, the log-transformed visits remain statistically significant.
Table 5.
Effect of social distancing policies on visits to physician office, general and medical service hospitals, health and personal care stores, and office of dentists.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Offices of Physicians | General and Medical Service Hospitals | |||||
| Panel A: Level changes | −9.270*** | −3.358*** | 0.672 | −78.35*** | −33.66** | −3.680 |
| post shelter in place | (0.298) | (0.655) | (0.490) | (12.36) | (13.09) | (15.07) |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 13,430,991 | 13,430,991 | 13,430,991 | 1045,379 | 1045,379 | 1045,379 |
| R-squared | 0.03 | 0.03 | 0.03 | 0.17 | 0.17 | 0.17 |
| baseline mean | 31.09 | 31.09 | 31.09 | 363.11 | 363.11 | 363.11 |
| Panel B: Log changes | ||||||
| post shelter in place | −0.251*** | −0.161*** | −0.0460*** | −0.116*** | −0.145*** | −0.0291 |
| (0.00591) | (0.0152) | (0.00692) | (0.0360) | (0.0388) | (0.0408) | |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 13,430,991 | 13,430,991 | 13,430,991 | 1045,379 | 1045,379 | 1045,379 |
| R-squared | 0.06 | 0.06 | 0.06 | 0.23 | 0.23 | 0.23 |
| Baseline mean | 2.60 | 2.60 | 2.60 | 4.44 | 4.44 | 4.44 |
| Health and Personal Care Stores | Office of Dentists | |||||
| Panel A: Level changes | −23.48*** | −13.83*** | −5.714*** | −4.545*** | −3.158*** | −0.780* |
| post shelter in place | (0.852) | (1.360) | (1.159) | (0.214) | (0.411) | (0.463) |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 3809,626 | 3809,626 | 3809,626 | 9332,246 | 9332,246 | 9332,246 |
| R-squared | 0.11 | 0.11 | 0.11 | 0.01 | 0.01 | 0.01 |
| baseline mean | 79.36 | 79.36 | 79.36 | 16.64 | 16.64 | 16.64 |
| Panel B: Log changes | ||||||
| post shelter in place | −0.324*** | −0.201*** | −0.0774*** | −0.212*** | −0.189*** | −0.0460*** |
| (0.0133) | (0.0171) | (0.0113) | (0.00546) | (0.0175) | (0.00640) | |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 3809,626 | 3809,626 | 3809,626 | 9332,246 | 9332,246 | 9332,246 |
| R-squared | 0.15 | 0.15 | 0.15 | 0.07 | 0.07 | 0.07 |
| Baseline mean | 3.85 | 3.85 | 3.85 | 2.27 | 2.27 | 2.27 |
Caption: Unit of analysis is the number of visits in a week to health care provider locations. Baseline means are calculated based on the ninth week of 2019. Regression models were estimated using ordinary least squares. The outcome measure is the number of visits and regressions include fixed effects for county and week. We use the four-digit NAICS code to identify office of physicians (6211), general medical and surgical hospitals (6221), health and personal care stores (4461), and offices of dentists (6212). Standard errors are clustered at the county level. *** p<0.01, ** p<0.05, * p<0.1.
Table 6.
Effect of social distancing policies on visits to medical and diagnostic laboratories, nursing care facilities, retirement communities and specialty hospitals.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Medical and Diagnostic Laboratories | Nursing Care Facilities | |||||
| Panel A: Level changes | −9.062*** | −4.619*** | −0.833 | −19.79*** | −8.468*** | −3.343*** |
| post shelter in place | (0.449) | (0.888) | (1.030) | (0.867) | (1.220) | (1.294) |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 1157,337 | 1157,337 | 1157,337 | 748,765 | 748,765 | 748,765 |
| R-squared | 0.07 | 0.07 | 0.07 | 0.21 | 0.21 | 0.22 |
| baseline mean | 28.09 | 28.09 | 28.09 | 61.54 | 61.54 | 61.54 |
| Panel B: Log changes | ||||||
| post shelter in place | −0.288*** | −0.201*** | −0.0843*** | −0.379*** | −0.207*** | −0.109*** |
| (0.00921) | (0.0213) | (0.0236) | (0.0134) | (0.0220) | (0.0235) | |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 1157,337 | 1157,337 | 1157,337 | 748,765 | 748,765 | 748,765 |
| R-squared | 0.10 | 0.10 | 0.10 | 0.23 | 0.24 | 0.24 |
| Baseline mean | 2.59 | 2.59 | 2.59 | 3.68 | 3.68 | 3.68 |
| Retirement Communities and Assisted Living Facilities | Specialty Hospitals | |||||
| Panel A: Level changes | −12.42*** | −4.019*** | 0.208 | −12.95*** | −2.926 | 4.368 |
| post shelter in place | (0.499) | (0.800) | (0.617) | (1.403) | (2.827) | (3.333) |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 1622,258 | 1622,258 | 1622,258 | 294,129 | 294,129 | 294,129 |
| R-squared | 0.13 | 0.13 | 0.13 | 0.16 | 0.16 | 0.16 |
| baseline mean | 39.80 | 39.80 | 39.80 | 39.71 | 39.71 | 39.71 |
| Panel B: Log changes | ||||||
| post shelter in place | −0.349*** | −0.150*** | −0.0321** | −0.299*** | −0.205*** | −0.0510 |
| (0.0110) | (0.0194) | (0.0139) | (0.0174) | (0.0362) | (0.0383) | |
| Weeks since first case FE | X | X | X | X | ||
| Weeks since first death FE | X | X | X | X | ||
| Year X Week FE | X | X | ||||
| Observations | 1622,258 | 1622,258 | 1622,258 | 294,129 | 294,129 | 294,129 |
| R-squared | 0.17 | 0.18 | 0.18 | 0.21 | 0.21 | 0.22 |
| Baseline mean | 3.19 | 3.19 | 3.19 | 2.77 | 2.77 | 2.77 |
Caption: Unit of analysis is the number of visits in a week to health care provider locations. Baseline means are calculated based on the ninth week of 2019. Regression models were estimated using ordinary least squares and regressions include fixed effects for county and week. The outcome measure is the number of visits. We use the four-digit NAICS code to identify medical and diagnostic laboratories (6215), nursing care facilities (6231), retirement communities and assisted living facilities (6233), and specialty hospitals (6223).Standard errors are clustered at the county level. *** p<0.01, ** p<0.05, * p<0.1.
Similar patterns exist for visits to general and medical service hospitals (Table 5, columns 4–6). Following the introduction of SIP policies, weekly visits to hospitals decreased by 78.4 visits per week, a relative decrease of 21%. Adding in the fixed effects that measure COVID-duration in each county reduces the magnitude of the SIP coefficient as does the inclusion of the week by year fixed effects. Following the first COVID-19 case, weekly visits to hospitals decrease by 33.7 visits per week, a relative decrease of 9%. In column 6, the impact of SIP laws on weekly visits to is no longer statistically significant for neither Panel A, nor Panel B. We find similar changes in both Tables 5 and 6 for health and personal care stores, office of dentists, medical and diagnostic laboratories, nursing care facilities, retirement communities and assisted living facilities, and specialty hospitals. Depending on the model the inclusion of the week by year fixed effects is statistically significant or not.
Sensitivity analyses
Potential confounding changes to sample population
A potential concern with this analysis is the mechanical relationship between employment status and employer-sponsored insurance coverage. Because our main data comes from employer-sponsored claims data, our population does not include individuals who lost employment because of the pandemic. If the remaining population has differential use of health services, our results could be biased. Existing work documents substantial heterogeneity in the labor market impacts of the COVID-19 pandemic (Forsythe et al., 2020). To assess the magnitude of this potential bias, we estimate changes in the number of covered individuals following the implementation of SIP policies.
As shown in Appendix Table 1, we find modest, and somewhat conflicting changes in the sample population size following the implementation of SIP policies. In columns 1–3, which use the raw sample population (at the age group, sex, county, and week level), we find a 3.7 person decrease in the number of people in each cell when not including fixed effects for COVID-19 exposure or the year-by-week fixed effects interactions. When adding these controls, we find a 5.9 person increase in the number of people in each cell. In columns 4–6, we use the log-transformed population and find a similar pattern, but with a relative interpretation. In column 4, we find a 2.2% reduction in the sample population, while in column 6, a 6% increase following the implementation of SIP policies.
Differences by county-level income and race
Our sensitivity tests that examine heterogeneous effects find small differences based on county-level income and race (Appendix Tables 2 and 3). However, these differences may be limited when compared to the broader population because our study population receives insurance through an employer. We observe a meaningful age gradient, with older adults more likely to reduce elective care. We also find increased magnitudes in care reductions for older patients and increased adoption of telehealth.
Alternative sip policy definition
To account for lags in behavior changes following the removal of SIP policies, we measure changes in non-COVID health care utilization following the implementation of SIP policies, regardless if the SIP policies are removed, using the approach outlined in previous studies (Cook et al., 2020). As an additional test, we measure changes in service utilization only when a SIP policy is actively in effect.
As shown in Appendix Tables 4 and 5, we find similar results with this alternative definition. Importantly, we observe the same pattern, where the reductions in preventive and elective care are driven by both SIP policies and exposure to the COVID-19 pandemic. For example, for preventive care (Panel A), fully controlling for exposure to the COVID-19 pandemic reduces the magnitude of the SIP coefficient by approximately 80%. In Appendix Tables 6 and 7, we conduct the same exercise, and examine changes in visits to health care providers in the SafeGraph data using the alternative SIP policy measure. We find similar results, with large reductions in visits to General and Medical Service Hospitals.
State elective procedure bans
A potentially co-occurring policy is the implementation of bans on elective procedures and non-essential business limitations. Ziedan et al. (2020) use electronic health record data and find that these policies lead to an approximately 15 percent reduction in outpatient utilization. As an additional test, we examine changes in utilization following the implementation of bans on elective procedures. To our knowledge, data on these policies is only available at the state level, and so we are unable to examine the effects of more granular policy variation. These policies are also highly correlated with county-level social distancing policies ().
As shown in Appendix Tables 8 to 11, we find similar patterns to county-level social distancing measures. The same pattern, where adding the controls for exposure to and the general trajectory of the COVID-19 pandemic, substantially reduces the magnitude of care reductions. For example, fully controlling for the COVID-19 pandemic reduces the magnitude of the SIP coefficient for elective care by approximately 65%. The fully-controlled specification also produces slightly larger reductions in care, across all care categories, than in the main results.
Alternative responses to COVID-19 pandemic exposure
Our event studies examine changes in use of services following the implementation of social distancing policies, but as we highlight, changes in use of non-COVID care could be driven by the pandemic. People in areas in which the pandemic is more intense may have increased concerns about infection, and thus may reduce use of non-COVID care regardless of whether a formal social distancing policy is in place. As a test of this mechanism, we estimate the event studies, but replace the SIP policy implementation date with the week of the first COVID-19 death in a county (Appendix Fig. 1) and the first week with at least 10 COVID-19 deaths in a county (Appendix Fig. 2).
We observe similar trends for each measure of exposure to the COVID-19 pandemic. We also observe similar patterns as our main results, which use SIP policy implementation. The similarity of the event studies that use SIP and COVID-19 exposure as the “event” highlights the importance of accounting for differential exposure to the COIVD-19 pandemic in our regressions, which we do through our fixed effects for the weeks since the first COVID-19 case and death in each county. Exposure to the COVID-19 pandemic both changes behavior among economic agents and endogenously leads to the implementation of SIP policies. As we demonstrate in this paper, not accounting for differences in underlying exposure to the pandemic will over-state the impact of both SIP and other COVID-19 risk mitigation policies.
Discussion
The COVID-19 pandemic has been an unprecedented shock to the U.S. healthcare delivery system. We found a drastic decline in preventive and elective services due to SIP policies related to the COVID-19 pandemic, but the impact of these policies is lessened when accounting for variations in exposure to the COVID-19 pandemic. These reductions in use of non-COVID care as a result of SIP policies should be weighed against potential benefits when evaluating the welfare implications of SIP policies.
Our results also suggest that the COVID-19 pandemic led to drastic reductions in use of health care. These effects were much larger than the decline in care due to SIP policies. Our estimates of decline in healthcare utilization during the early stages of the pandemic are in line with existing studies by Chatterji and Li (2020), Mehrotra et al. (2020) and Ziedan et al. (2020). It is important to note that our findings are during the initial stage of the pandemic, and that the length of the pandemic and mitigation strategies will define the aggregate cost on both consumers and providers (Cutler 2020). Some are concerned that the deferred care may cause some individuals with chronic conditions to become sicker and that it might increase aggregate costs (Lucia et al., 2020). This may also lead to constraints on care capacity post pandemic (Wosik et al., 2020). In addition, how the healthcare sector will be able to provide elective procedures once the pandemic has subsided is not known. Anecdotal evidence from some providers is that they will shift elective procedures to weekends (Lucia et al., 2020). Future researchers should explore this possibility and whether there are impacts on quality of care.
Our results provide a crucial first step on measuring the impact of COVID-19 on healthcare utilization based on various measures. The findings are important given that the Government Accountability Office has now pledged to track monthly changes in healthcare employment, change in volume of elective procedures across settings, median monthly changes in hospital operating margins, and changes in healthcare services as a proportion of personal consumption expenditures (Government Accountability Office 2020). The results using cellular phone geolocation data imply that these data should be considered when measuring healthcare utilization over the course of the pandemic while waiting for healthcare claims data to be released.
We also found that while there were drastic declines in in-person office visits that there was a rapid increase in telemedicine utilization. Telemedicine services have been used to maintain access and continuity of medical care (Wosik et al., 2020). However, in line with previous work, telemedicine utilization did not sufficiently replace the entire drop in in-person office visits (Mehrotra et al., 2020). Whether telemedicine use will be sustained during and following the COVID-19 pandemic remains uncertain. The uncertainty is driven in part by ambiguity if the existing policy landscape for telemedicine will be sustained as the pandemic proceeds and eventually ends (Lucia et al., 2020). For example, insurers are concerned that the increase in telemedicine may lead to increases in fraud and overutilization of services if it becomes additive over existing trends post pandemic (Lucia et al., 2020). Separately, many providers report that they do not have the technology system to make the shift to telemedicine or that in-person office visits are needed to achieve a positive health outcome (Lucia et al., 2020). These concerns should be addressed given that after the pandemic, telemedicine can serve as one way to proactively engage with patients who deferred care and to help the healthcare system manage the upcoming surge in demand for procedures unrelated to COVID-19 (Wosik et al., 2020).
This study is not without limitations. First, while we use medical claims data from a large and diverse study population that is employed, it represents a subset of individuals with private insurance and it does not include other important populations, such as patients with Medicaid, and those lacking insurance. Insurers have reported that Medicaid enrollment is increasing at a rapid rate when compared to marketplace enrollment, but surprisingly enough slower-than expected (Lucia et al., 2020). Job loss can reduce health care utilization use through both loss of insurance coverage and reductions in income. Due to the mechanical linkage between our study population and employment, our findings, while large, are potentially an underestimate for the declines in the number of visits. Second, the SafeGraph mobile tracking data, comprise of approximately 10 percent of all cellphone users and 6 million locations. Thus, our results using those data are limited to the population and those locations covered by the SafeGraph data. Our measures of number of visits are not necessarily tracking healthcare utilization, instead the number of individuals who visit locations under that particular NAICS code. The decline in the number of visits may be due to declines in employment in the healthcare sector as well. Third, we are not able to examine whether care that has been deferred during the early period of the COVID-19 pandemic will be deferred until the future or avoided completely. Our estimates do not capture potential innovative approaches by providers to ensure patient resumption of preventive care. This limitation is important, given that concerted efforts are being made to increase the use of preventive services such as vaccinations which has exhibited a sharp initial drop after the national emergency declaration. Future work must monitor each of the preventive measures that we track in the present study and disparities in the use of preventive services. Fourth, the present study does not include measures of healthcare capacity. That said, a recent report by the Government Accountability Office (2020) reports that intensive care unit bed availability data is not currently up to date given that only 60 percent of hospitals have reported their information as of early June 2020 and that 95 to 100 percent are needed for effective analysis (Government Accountability Office 2020). Fifth, we do not examine the use of telehealth broken down by the type of provider or cause for the interaction. Existing studies have shown that changes in telehealth utilization differ by the provider and the cause for the interaction (Lau et al., 2020; Patel et al., 2021). There is important heterogeneity in the use of telehealth during the pandemic that our study does not quantify. Finally, the claims data we use does not include detailed race and ethnicity characteristics of patients. The COVID-19 pandemic has had a disproportionate impact on communities of color and other marginalized groups (Khazanchi et al., 2020; Azar et al., 2020). Therefore, we are unable to examine differences in healthcare utilization by these key characteristics.
To our knowledge, our study is the most comprehensive to date on the effects of county-level SIP policies on healthcare utilization. We use multiple novel datasets and measures to evaluate the effect of these policies. Our results indicate that utilization has dropped drastically and that it varies by the type of care received and the severity of the COVID-19 pandemic within a county. Finally, our results indicate that while the use of telemedicine has increased, it has not fully replaced the use of office-based visits. Thus, it is critical that public policy and public health officials do more to ensure that individuals receive the care that they desperately need.
CRediT authorship contribution statement
Jonathan Cantor: Conceptualization, Data curation, Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. Neeraj Sood: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. Dena M. Bravata: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. Megan Pera: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. Christopher Whaley: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Footnotes
Funding provided by National Institute on Aging (K01AG061274, Whaley) and the Robert Wood Johnson Foundation. We thank Peter Hussey for helpful comments and David Kravitz for assistance with SafeGraph data. Bravata and Pera are employees of Castlight Health.
Telemedicine procedures were identified as claims with procedure codes in the following set: ('99441′,'99442′,'99443′,'99444′,'99421′,'99422′,'99423′,'98970′,'98971′,'98972′,'G2061′,'G2062′,'G2063′), claims with a procedure code modifier in ('95′,'GT','GQ'), or a place of service code equal to 2.
Note that our weeks which are Wednesday-Tuesday are different than SafeGraph weeks which are Monday-Sunday. This required breaking each row into seven different daily entries, then re-combining based upon our weeks. We used the Wednesday-Tuesday designation for computational reasons.
County income and race composition are measured using data from the 2018 American Community Survey 5 year estimates and categorized as quartiles of the share of households with incomes below the federal poverty line and the share of residents who are non-white race.
The population for colonoscopy procedures is limited to those ages 46 to 64. Mammograms are limited to women ages 46 to 64.
Because the dependent variable is log-transformed, the coefficients can be interpreted in percentage terms by applying .
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jhealeco.2022.102581.
Appendix. Supplementary materials
References
- Adhikari S., Pantaleo NP., Feldman JM., Ogedegbe O., Thorpe L., Troxel AB. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US Metropolitan Areas. JAMA Netw. Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.16938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amuedo-Dorantes C., Kaushal N., Muchow A.N. National Bureau of Economic Research; 2020. Is the Cure Worse than the Disease? County-Level Evidence from the COVID-19 Pandemic in the United States. Working Paper 27759. Working Paper Series. [DOI] [Google Scholar]
- Andersen M., Bryan S., Slusky D. National Bureau of Economic Research; 2020. COVID-19 Surgical Abortion Restriction Did Not Reduce Visits to Abortion Clinics.https://www.nber.org/papers/w28058#fromrss Working Paper 28058. [Google Scholar]
- Azar KM.J., Shen Z., Romanelli RJ., Lockhart SH., Smits K., Robinson S., Brown S., Pressman AR. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598. https://doi.org/10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- Brown C.S., Ravallion M. Inequality and the Coronavirus: Socioeconomic Covariates of Behavioral Responses and Viral Outcomes Across US Counties. National Bureau of Economic Research; 2020. Working Paper 27549. Working Paper Series. [DOI] [Google Scholar]
- Cantor J., Kravitz D., Sorbero M., Andraka-Christou B., Whaley C., Bouskill K., Stein BD. Trends in Visits to Substance Use Disorder Treatment Facilities in 2020. J. Subst. Abuse Treat. 2021;127(August) doi: 10.1016/j.jsat.2021.108462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; 2020. Healthcare Facilities: Managing Operations During the COVID-19 Pandemic.https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html 2020. [Google Scholar]
- Cook J., Newberger N., Smalling S. The spread of social distancing. Econ. Lett. 2020;196 doi: 10.1016/j.econlet.2020.109511. November. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff. 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608. https://doi.org/10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- Cronin CJ., Evans WN. Private Precaution and Public Restrictions: What Drives Social Distancing and Industry Foot Traffic in the COVID-19 Era? 2020. https://www.nber.org/papers/w27531.ack National Bureau of Economic Research Working Paper SeriesJuly. [Google Scholar]
- Cutler D. How will COVID-19 affect the health care economy? JAMA Health Forum. 2020;1(4) doi: 10.1001/jamahealthforum.2020.0419. [DOI] [PubMed] [Google Scholar]
- Cutler DM., Summers LH. The COVID-19 pandemic and the $16 trillion virus. JAMA. 2020 doi: 10.1001/jama.2020.19759. October. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler MÉ. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69 doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farr C. CNBC; 2020. Hospitals Losing Millions of Dollars per Day in Covid-19 Pandemic- and Recovery May Take Years.https://www.cnbc.com/2020/05/05/hospitals-losing-millions-of-dollars-per-day-in-covid-19-pandemic.html 2020. [Google Scholar]
- Forsythe E., Kahn LB., Lange F., Wiczer D. Labor demand in the time of COVID-19: evidence from vacancy postings and UI claims. J. Public Econ. 2020;189(September) doi: 10.1016/j.jpubeco.2020.104238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao S., Rao J., Kang Y., Liang Y., Kruse J., Dopfer D., Sethi AK., Reyes J.F.M., Yandell BS., Patz JA. Association of mobile phone location data indications of travel and stay-at-home mandates with COVID-19 infection rates in the US. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.20485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman-Bacon A., Marcus J. Discussion Papers of DIW Berlin 1870. German Institute for Economic Research; DIW Berlin: 2020. Difference-in-differences to identify causal effects of COVID-19 policies. n.d. [Google Scholar]
- Goolsbee A., Syverson C. Fear, Lockdown, and Diversion: Comparing Drivers of Pandemic Economic Decline 2020. National Bureau of Economic Research; 2020. Working Paper 27432. Working Paper Series. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government Accountability Office . 2020. Covid-19: Opportunities to Improve Federal Response and Recovery Efforts.https://www.gao.gov/products/gao-20-625 [Google Scholar]
- Gupta S., Montenovo L., Nguyen T.D., Rojas F.L., Schmutte I.M., Simon K.I., Weinberg B.A., Wing C. Effects of Social Distancing Policy on Labor Market Outcomes. National Bureau of Economic Research; 2020. Working Paper 27280. Working Paper Series. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein DU., Woolhandler S. The U.S. Health Care System on the eve of the Covid-19 epidemic: a summary of recent evidence on its impaired performance. Int. J. Health Serv. 2020:1–7. doi: 10.1177/0020731420937631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain S., Santhosh L. On treatments and tests deferred: preparing for collateral damage from COVID-19. Ann. Am. Thorac. Soc. 2020 doi: 10.1513/AnnalsATS.202004-387VP. July. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jay J., Bor J., Nsoesie EO., Lipson SK., Jones DK., Galea S., Raifman J. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat. Hum. Behav. 2020:1–9. doi: 10.1038/s41562-020-00998-2. November. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazanchi R., Evans CT., Marcelin JR. Racism, not race, drives inequity across the COVID-19 continuum. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19933. [DOI] [PubMed] [Google Scholar]
- Koonin LM., Hoots B., Tsang CA., Leroy Z., Farris K., Jolly B., Antall P., et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic — United States, January–March 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(43):1595–1599. doi: 10.15585/mmwr.mm6943a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranz AM., Chen A., Gahlon G., Stein BD. 2020 trends in dental office visits during the COVID-19 pandemic. J. Am. Dent. Assoc. 2021 doi: 10.1016/j.adaj.2021.02.016. March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J., Knudsen J., Jackson H., Wallach AB., Bouton M., Natsui S., Philippou C., et al. Staying connected in the COVID-19 pandemic: telehealth at the largest safety-net system in the United States. Health Aff. 2020 doi: 10.1377/hlthaff.2020.00903. Junehttps://doi.org/10.1377/hlthaff.2020.00903. [DOI] [PubMed] [Google Scholar]
- Lucia K., Blumberg LJ., Curran E., Holahan J., Wengle E., Hoppe O., Corlette S. Urban Institute; 2020. The COVID-19 Pandemic – Insurer Insights Into Challenges, Implications, and Lessons Learned.https://www.urban.org/research/publication/covid-19-pandemic-insurer-insights-challenges-implications-and-lessons-learned June 29, 2020. [Google Scholar]
- Mann DM., Chen Ji, Chunara R., Testa PA., Oded COVID-19 transforms health care through telemedicine: evidence from the field. J. Am. Med. Inform. Assoc. 2020;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matrajt L., Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg. Infect. Dis. 2020;26(8):1740–1748. doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra A., Chernew M., Linetsky D., Hatch H., Cutler D. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerge. 2020. s. 2020. [DOI] [Google Scholar]
- Moreland A. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement — United States, March 1–May 31, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69 doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SY., Mehrotra A., Huskamp HA., Uscher-Pines L., Ganguli I., Barnett M.L. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff. (Millwood) 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The New York Times . 2020. See How All 50 States Are Reopening (and Closing Again)https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html 2020. [Google Scholar]
- USAFacts . 2020. Coronavirus Outbreak Stats & Data.https://usafacts.org/issues/coronavirus/ 2020. [Google Scholar]
- Verma S. 2020. Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19.https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/ 2020. [Google Scholar]
- Whaley C., Pera M., Cantor J., Chang J., Velasco J., Hagg H., Bravata D. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH., Chapman DA., Sabo RT., Weinberger DM., Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wosik J., Fudim M., Cameron B., Gellad ZF., Cho A., Phinney D., Curtis S., et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Inform. Health Biomed. 2020;27(6):957–962. doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziedan E., Simon K.I., Wing C. Effects of State COVID-19 Closure Policy on NON-COVID-19 Health Care Utilization. National Bureau of Economic Research; 2020. Working Paper 27621. Working Paper Series. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.