In South Korea, liver transplantation (LT) began in 1988 when the first deceased donor liver transplantation (DDLT) of a child with Wilson’s disease was successful. Then, in 1994, living donor liver transplantation (LDLT) was first attempted in the country. In 1999, the Korean Network for Organ Sharing (KONOS) was established as the national institution to carry out transplant-related tasks, such as organ allocation. Since 2002, the model for endstage liver disease (MELD) score has been used as a criterion for long-term distribution in many regions around the world, including the USA and Europe. In South Korea, the allocation system for emergency LT has been based on the MELD score since June 2016.
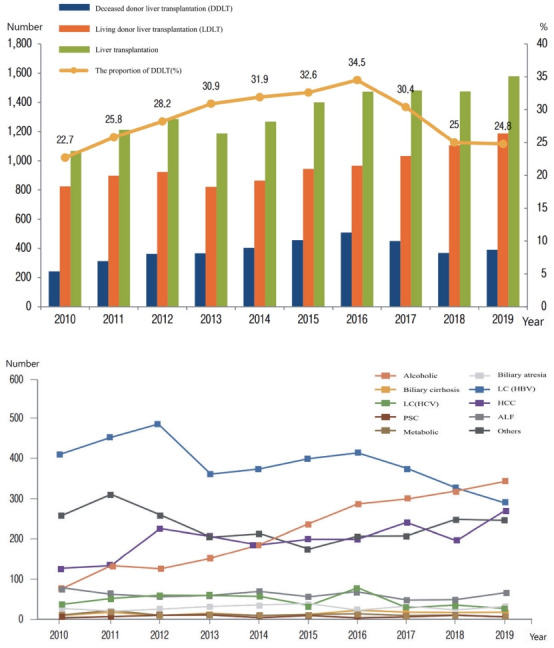
Since the 2010s, the DDLT rate has continuously increased, accounting for more than 20% of all liver transplants and 34.5% of all liver transplants in 2016. However, the amount of DDLT decreased again in 2017, with its proportion accounting for 25% of the total LT cases. In 2019, the number of brain-death organ donors in South Korea was 8.7 per million people. This was much lower than the 49.6 per million people in Spain and the 36.1 per million people in the USA, and also far less than the 20 or more per million people reported in France, UK, and Australia [1]. Due to the shortage of brain-death donors in South Korea, DDLT is being performed with an average MELD score as high as 36.5 points. Since DDLT is performed when the MELD score is too high, there is a concern that the number of cases with poor prognosis after DDLT may increase. Therefore, LT in South Korea, as in other East Asian countries, has been largely dependent on LDLT amid a shortage of brain-death donors.
A common indication for LT is an acute or chronic liver disease in which liver function is deteriorated severely to a point where it does not respond to any other treatments and can only be treated with a LT. Liver cirrhosis caused by viral hepatitis (hepatitis B or C) or alcohol, autoimmune hepatitis, primary sclerosing cholangitis, biliary atresia, Wilson’s disease, and hepatocellular carcinoma (HCC) are chronic liver diseases requiring LT. Due to the development of surgical technique, postoperative care, and expansion of LDLT, the indications for LT are gradually expanding. However, LT is still contraindicated in patients with severe heart and lung diseases, extrahepatic malignancy, and uncontrolled sepsis.
Hepatitis B and herbal medicine are the most common causes of acute liver failure requiring LT in South Korea [2]. Until 2000, the incidence of acute hepatitis A has declined; but after that, the number of hepatitis A-induced fulminant liver failure patients increased as the hepatitis A antibody-positive rate decreased in younger people under 30 years of age.
For chronic liver disease, in the past, more than 70% of adult LTs in South Korea were performed for cirrhosis and/or HCC caused by the hepatitis B virus. However, in recent years, this proportion has decreased due to the development of antiviral agents. The proportion of patients receiving LT for liver cirrhosis or HCC due to hepatitis C has been increasing; however, after treatment with direct acting antiviral agents (DAA) in 2014, the proportion has declined again. On the other hand, as viral hepatitis has decreased, the number of LT for alcoholic liver disease has been increasing. Also, similar to other countries, South Korea has been seeing a steady rise in the number of LT for nonalcoholic steatohepatitis or nonalcoholic fatty liver disease. Moreover, the number of patients receiving LT as a treatment for HCC has gradually increased as LDLT is being actively implemented in South Korea [3].
Recently, the 1-year survival rate of DDLT has reached 77.9%, and the 1-year survival rate of LDLT has reached 89.9%. The 1-year survival rate of all LT is reported to be good enough to reach 86.9% due to improved surgical technique and patient management, as well as the appropriate use of various immunosuppressants. In addition, postoperative mortality is directly related to the severity of LT recipients; therefore, it is important to prepare for transplantation in a timely manner [4]. The 3-year and 5-year survival rates in South Korea have been excellent, reaching 83.7% and 80.9% for LDLT and 72.3% and 68.9% for DDLT, respectively (total, 80.8% and 77.9%, respectively). The long-term survival rate after LT in South Korea is also excellent, and the 10-year survival rate after transplantation has reached 70%, which is comparable to the 10-year survival rate of 63% in other countries [4,5].
The survival rate of LT in patients with HCC may vary depending on the size and number of tumors, as well as tumor biology. So far, LT has shown the best survival rate among the currently available treatment methods for HCC. However, LT for HCC patients still have problems that need to be addressed, including donor shortage and ethical issues. This is because LT in HCC is almost entirely dependent on LDLT. Liver resection for living donor is a procedure that requires high degree of surgical skills, with its mortality rate reported to be 0.2–0.5% in foreign countries [6]. In South Korea, one in 7,000 donors died after surgery. In addition, minimally invasive surgery, such as laparoscopic or robotic surgery, is being more actively performed for donor hepatectomy in South Korea than in any other country. This minimally invasive surgery helps donors to recover earlier.
Abbreviations
- DAA
direct acting antiviral agents
- DDLT
deceased donor liver transplantation
- HCC
hepatocellular carcinoma
- KONOS
Korean Network for Organ Sharing
- LDLT
living donor liver transplantation
- LT
liver transplantation
- MELD
model for end-stage liver disease
Footnotes
Conflicts of Interest
The author has no conflicts to disclose.
REFERENCES
- 1.Joo DJ. Current status of deceased donor liver transplantation for alcoholic liver disease in Korea in MELD era. Korean J Gastroenterol. 2021;77:4–11. doi: 10.4166/kjg.2020.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin YJ, Lim YS, Han S, Lee HC, Hwang S, Lee SG. Predicting survival after living and deceased donor liver transplantation in adult patients with acute liver failure. J Gastroenterol. 2012;47:1115–1124. doi: 10.1007/s00535-012-0570-7. [DOI] [PubMed] [Google Scholar]
- 3.Korean Network for Organ Sharing (KONOS) 2019 Annual report of organ and tissue donation and transplantation. KONOS web site, < https://www.konos.go.kr/konosis/common/bizlogic.jsp>. Accessed 1 Dec 2020.
- 4.Agopian VG, Petrowsky H, Kaldas FM, Zarrinpar A, Farmer DG, Yersiz H, et al. The evolution of liver transplantation during 3 decades: analysis of 5347 consecutive liver transplants at a single center. Ann Surg. 2013;258:409–421. doi: 10.1097/SLA.0b013e3182a15db4. [DOI] [PubMed] [Google Scholar]
- 5.Zarrinpar A, Busuttil RW. Liver transplantation: past, present and future. Nat Rev Gastroenterol Hepatol. 2013;10:434–440. doi: 10.1038/nrgastro.2013.88. [DOI] [PubMed] [Google Scholar]
- 6.Shiffman ML, Brown RS, Jr, Olthoff KM, Everson G, Miller C, Siegler M, et al. Living donor liver transplantation: summary of a conference at The National Institutes of Health. Liver Transpl. 2002;8:174–188. doi: 10.1053/jlts.2002.30981. [DOI] [PubMed] [Google Scholar]


