Abstract
Aims:
Most information on the relationship between medical cannabis laws (MCL) and the risk for opioid overdose fatality has been based on studies with ecological designs. To contribute additional information, we used a novel case-control design and individual-level data from national surveys to assess whether state medical cannabis laws were associated with reduced risk of fatal opioid overdose between 2000–2011.
Methods:
Data from participants surveyed in the National Health Interview Survey (NHIS) between 1986–2011 were included. For those sampled between 1986–2009, detailed mortality follow-up data were available from the National Death Index up to 12/31/2011. Opioid overdose decedents (n=791) were classified as cases. Between 2000–2011, all cases arising in a given year were matched to adult controls who were surveyed the same year and eligible for mortality follow-up (n=723,920). The distribution of exposure to state MCL was contrasted between cases and controls, providing an approximation of the rate ratio of fatal opioid overdose associated with MCLs. Due to a NHIS sample redesign, we stratified analysis using timeframes before and after 2005.
Results:
Overall, compared to controls, cases were more likely to be male, middle-aged, non-Hispanic White, separated/divorced; less educated, and have a family income below the poverty threshold. No overall association between state MCLs and the rate of opioid overdose was observed between 2000–2005 (aOR=1.22, 95% CI: 0.83–1.79) or between 2006–2011 (aOR=0.87, 95% CI: 0.60–1.25). No significant difference between sampling timeframes was observed (ratio of aOR’s = 0.71, 95% CI: 0.49–1.01).
Conclusions:
We found no overall protective relationship between state MCLs and opioid overdose. Future research with more recent mortality data and more refined cannabis policy classifications would be useful. The importance of the study is two-fold. First, the findings provide an additional source of information countering claims of a protective effect of MCLs on opioid overdoses, suggesting that other solutions to the opioid overdose crisis are needed. Second, the study offers a potentially useful design to answer important population-level public health questions.
INTRODUCTION:
While the proportion of ambulatory, office-based visits with a primary symptom or diagnosis of pain remained consistent from 2000 to 2010, the frequency of opioid prescribing among these visits nearly doubled from 11.3% to 19.6% (Daubresse et al., 2013). Concurrent with this rise in prescribing has been a tide of opioid overdose morbidity and mortality (Paulozzi & Ryan, 2006). Increased utilization of clinical alternatives to prescription opioids has been recognized as one option to curb this epidemic (Daubresse et al., 2013).
Currently, medical cannabis is available in states that have enacted medical cannabis laws (MCLs). Prior studies using ecological data between 1999–2010 found that MCLs were associated with reductions in state rates of opioid overdose mortality and treatment admissions (Bachhuber, Saloner, Cunningham, & Barry, 2014; D. Powell, Pacula, & Jacobson, 2018; Shover, Davis, Gordon, & Humphreys, 2019). In particular, a 2014 study that attracted widespread scientific and media attention was hailed by activists and the cannabis industry as suggesting that expanding access to medical cannabis would help reverse the opioid epidemic (Bachhuber et al., 2014). However, a recent review that included several additional ecological studies (Chihuri & Li, 2019) found no conclusive evidence overall that MCLs were associated with reduction in prescription opioid overdose mortality, although one study in the review (D. Powell et al., 2018; Smart, 2015) showed significant reductions among older age groups (Smart, 2015), and another study showed reductions in states with active dispensaries (D. Powell et al., 2018). A third study (Phillips & Gazmararian, 2017) found that MCLs without prescription drug monitoring programs (PDMPs) were associated with a significant increase in opioid mortality. Additional studies that extended the same data (CDC WONDER post-2010) and that used varying analytical methods (e.g., difference-in-difference vs. interrupted time series) also produced inconsistent findings (Chan, Burkhardt, & Flyr, 2020; Kaufman et al., 2021; Shover et al., 2019).
While ecological studies are not intended for individual-level inference, a partial explanation of the ecological findings that cannabis substitution in MCL states protects against opioid overdose comes from individual-level studies showing that state MCLs are associated with subsequent increases in adult cannabis use (Hasin et al., 2017; Martins et al., 2016; H. Wen, Hockenberry, & Cummings, 2015). However, the relationship of state MCLs to opioid use is arguably a more salient substance use outcome than cannabis use. These findings are more mixed. One individual-level study using a nationally representative database of the commercially insured found MCLs to be associated with lower odds of any opioid use, chronic opioid use, and high-risk opioid use (Shah, Hayes, Lakkad, & Martin, 2019), but another study using a nationally representative sample failed to find that MCLs were associated with non-medical prescription opioid use (Segura et al., 2019). Regarding state MCLs and opioid prescribing, several individual-level studies have shown reductions in opioid prescribing associated with MCLs across various populations (Bradford & Bradford, 2016, 2017; Kropp Lopez et al., 2020; Lopez, Boddapati, Jobin, & Hickernell, 2021; McMichael, Van Horn, & Viscusi, 2020; Neilson et al., 2021; Raji, Abara, Salameh, Westra, & Kuo, 2019; J. Wen, Wen, Butler, & Talbert, 2021).
One major critique of the initial ecologic studies is that because aggregated data were used, inference at the individual level is invalid (Caputi & Sabet, 2018; Hall et al., 2018; Harris, Humphreys, & Finney, 2015). This assumes that ecologic associations are only crude substitutes for individual-level associations, and that any discrepancy observed between associations found at different levels is evidence that the ecological study lacks utility (Finney, Humphreys, & Harris, 2015; Hall et al., 2018). This framework for assessing ecologic studies may limit our search for potential causes of disease and potential public health interventions to those found at the individual level (Schwartz, 1994). An alternative framework, based on an assessment of internal validity (e.g., is bias minimized?) as well as construct validity (e.g., is an aggregated variable measuring a different construct than the “same” individual-level variable?) might better explain potential discrepancies between individual and ecological associations, while also recognizing the potential for ecologic factors to influence disease etiology (Schwartz, 1994). For example, state MCLs represent a diverse social and environmental context (Pacula, Powell, Heaton, & Sevigny, 2015), not an aggregation of individual-level behaviors (e.g., percent past-month cannabis users). Due to the seriousness of the opioid epidemic, additional studies assessing the consequences of MCL are sorely needed, regardless of whether the study uses individual or aggregated data.
An ideal study using individual-level data would randomly assign MCL to a subset of a population, and include follow-up measurements of the exposure and outcome over time. Since such a design is not feasible, studies using existing observational data must be used. While state aggregated rates of overdoses can be compared over time using difference-in-difference methods to compare state rates before and after MCL, an alternative approach would utilize individual data and compares individuals with MCL to those without MCL. However, continuous follow-up of a time-varying exposure (e.g., MCL) can be cumbersome. A nested case-control design with incidence-based sampling offers a more efficient alternative, permitting the exposure to be measured simultaneously among both cases and controls. Therefore, in the present study, we used individual-level data and a nested case-control population study with incidence-density sampling. Cases arising within a particular year (e.g., 2000) were matched to controls that were interviewed that same year (e.g., 2000 National Health Interview Survey [NHIS] adult sample). The exposure (state MCL) distribution was contrasted among cases (overdose fatalities) versus calendar-matched controls to approximate the relative rate of opioid overdose associated with MCLs.
METHODS:
Source Population and data
Data for this study were derived from study participants surveyed in the National Health Interview Survey (NHIS) between the years 1986–2011. To our knowledge, no other study has assessed this question using NHIS data. The NHIS is a yearly household survey of the noninstitutionalized population (adults and children) residing in the US and is representative at the national and the Census Region level. In 2006, the NHIS underwent a sampling redesign that resulted in a reduced overall sample. Notably, this reduction was consistent across all states. For participants surveyed between 1986–2009, detailed mortality data through December 31, 2011 were available via linkage with death certificate records from the National Death Index (NDI) for approximately 94% of eligible respondents (Data Linkage Team, 2015). Death data include International Statistical Classification of Diseases, Injuries, and Causes of Death (ICD-9 and ICD-10) underlying and multiple cause of death codes. Table 1 provides unweighted sample size for each year, including the proportion eligible for mortality linkage. Eligibility was determined by the availability of sufficient identifying data including SSN, full name, and date of birth, and should be independent of living in any particular state. Eligible children were included as potential cases if they were over the age of 18 at time of death but never included as controls.
Table 1.
NHIS participants by linked mortality eligibility and status
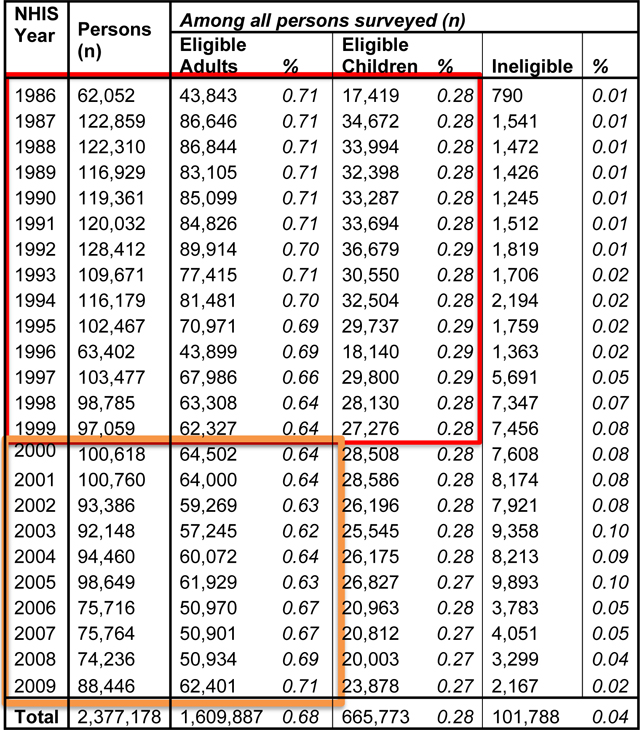
|
The red box indicates the initial source population for cases (including children if they died over age 18). Cases are individuals who were interviewed and then died of opioid overdose between 2000–2011. The orange box indicates the adult controls that are used, matched to cases by year of death, e.g, those interviewed in 2006 were controls for those who died in 2006. Adult controls later enter into the source population and are eligible to become cases (as are eligible children if they died over age 18). Adult controls in 2010 and 2011 (not shown) are not mortality-linked and are only used as controls.
Main measures
Outcomes
The primary outcome is prescription opioid overdose mortality, defined as fatal drug overdoses (International Statistical Classification of Diseases, 10th revision [ICD-10], codes X40-X44, X60-X64, and Y10-Y14) where an opioid analgesic was also coded (T40.2-T40.4) (Supplementary Table S2).
Exposure
The primary exposure variable is current residence in a state with an operational MCL (Supplementary Table S1), defined previously as an effective law with allowances for home cultivation or the presence of active dispensaries (Bradford & Bradford, 2016, 2017; Kim et al., 2016). Current residence is measured at time of death for cases and time of survey for controls (i.e., measured at a single point in time).
Individual-level control covariates
For cases and controls, data on age, gender, race/ethnicity (white, black, other), marital status (married/cohabitate, widowed, separated/divorced, never married/single, unknown), educational attainment (less than HS, HS degree/GED, some college, BA/technical degree, post-college), poverty status (above or below federal poverty threshold) is coded (Supplementary Table S2). For cases, data on age, marital status and educational attainment is from time of death, as found in the mortality dataset. If unknown at time of death, data at time of survey is used for cases.
State-defined covariates
Due to potential regional differences in opioid overdose rates (Kim, 2019), region (Northeast, South, Midwest, West) was included as a covariate. Further, other state policies could confound any estimated association between state MCLs and opioid overdose, in particular, prescription drug monitoring programs (PDMP) (Phillips & Gazmararian, 2017). Therefore, we created a variable indicating whether a state was “permitted or required to identify suspicious or statistically outlying prescribing”, a more robust measure of PDMP effectiveness than PDMP enactment alone (Cerdá et al., 2020; Martins et al., 2019; David Powell, Pacula, & Jacobson, 2015). Data on proactive PDMP enactment were obtained via LawAtlas (LawAtlas, 2017) (Supplementary Table S3).
Analytical Plan
Prior to our study analytical years (2000–2011), our initial source population began with all adults and children surveyed in the NHIS years 1986–1999 who were eligible for mortality follow-up (Table 1). This population served as an initial source for potential cases, and was not used analytically as controls.
Then, starting in 2000, all fatal opioid overdoses (decedent ≥18 years old) that occurred within the source population were defined as cases for the year in which they died. Cases arising within a particular year (e.g., 2000) were matched to controls that were interviewed that same year (e.g., 2000 NHIS adult sample; orange box, Table 1). Due to sparse cell concerns, data were pooled prior to case vs. control comparisons. Because of the 2006 NHIS sample redesign, data were pooled from 2000–2005 and from 2006–2011.
With this study design, control selection was independent of exposure status (via the random probability sample of households), and the source population was clearly defined. Additionally, controls later entered into our source population and became eligible to be cases in later years, with one exception: controls interviewed in the 2010 and 2011 NHIS were not mortality-linked, and were only eligible to serve as controls. Importantly, the MCL exposure distribution (i.e., proportion arising in a state with a MCL) was contrasted among cases vs. controls to estimate the relative rate of opioid overdose associated with state MCLs. For descriptive purposes, this contrast was done biennially (see Figure 1).
Figure 1.
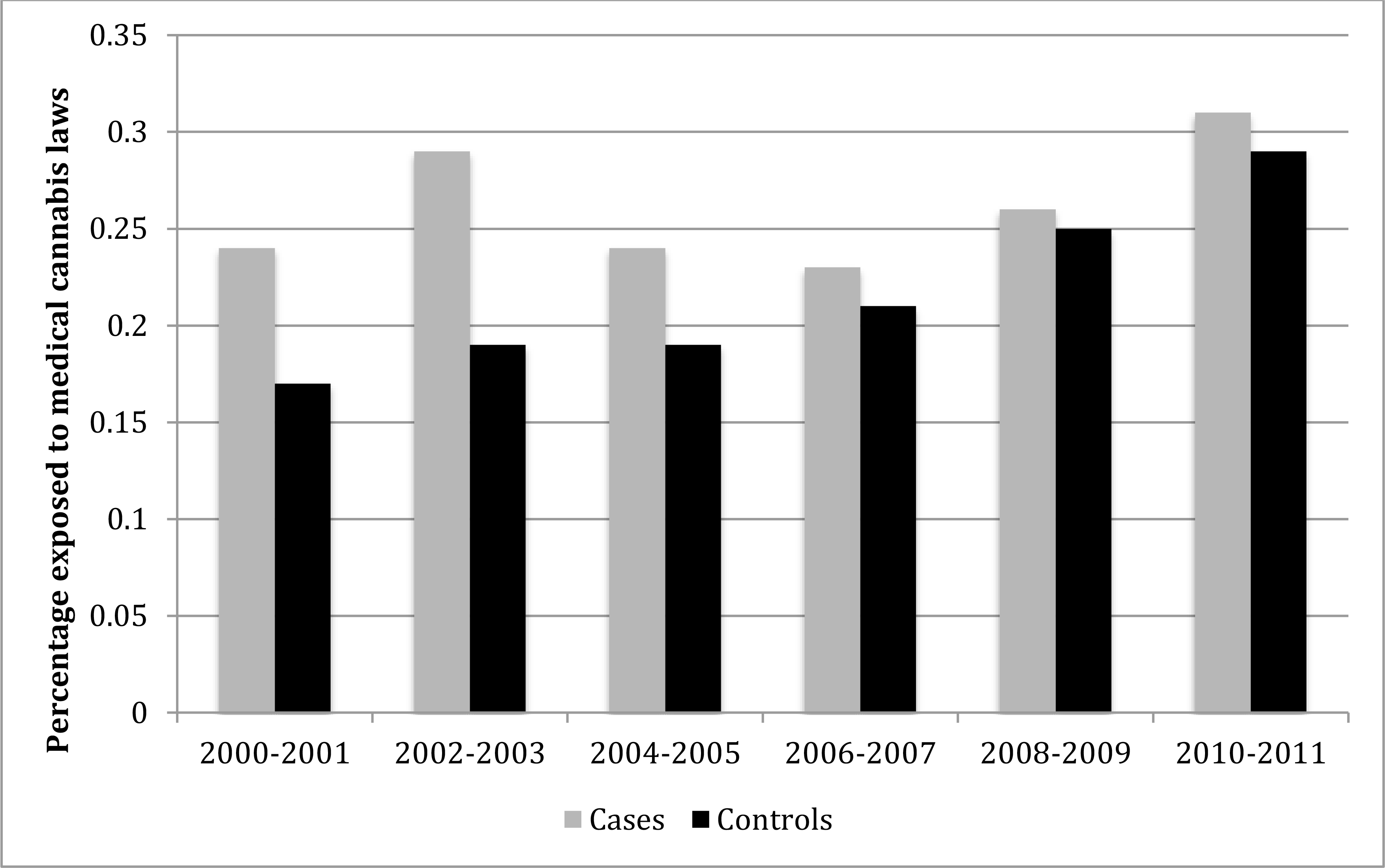
Proportion exposed to medical cannabis law, Cases vs. Controls from the National Health Interview Survey, 2000–2011
*Data (with n’s) is reproduced in Appendix Table 4
To test whether the proportion of cases and controls that were MCL-exposed differed significantly, we used a multivariable logistic regression to run four sets of models: (a) crude model adjusted for year only, (b) state-level model adjusted for year, census region, and PDMP, (c) individual-level model adjusted for year and all individual-level variables, and (d) combined model adjusted for year and all state-defined and individual-level variables. Analysis was stratified by sampling timeframe (2000–2005 vs. 2006–2011). To test whether the association varied by sampling timeframe, we ran the full set of models with an added interaction term between MCL status and sampling timeframe. All analysis was conducted using STATA 13 (StataCorp, 2013). Due to changes in sampling and analytical weight variables over time, survey weights were not incorporated.
RESULTS:
From our underlying cohort, 791 opioid decedent cases arose between the years 2000 and 2011 (Table 2). These cases were matched to 723,920 controls who were eligible for mortality follow-up, were 18 years or older at time of interview, and were surveyed in the same year as their matched cases (Table 2). Across all years, compared to controls, cases were more likely to be male, middle-aged, non-Hispanic White, never married, separated/divorced; less educated, and have a family income below the poverty threshold.
Table 2.
Characteristics of study sample: NHIS participants who died (cases) or were interviewed (controls) between the years 2000–2011.
| Cases (n=791) | Controls (n=723,920) | Chi-square p-value | |
|---|---|---|---|
| N (%) | N (%) | ||
| Sex | |||
| Male | 478 (0.60) | 342,005 (0.47) | <.001 |
| Female | 313 (0.40) | 381,915 (0.53) | |
| Age | |||
| 18–29 years | 143 (0.18) | 158,011 (0.22) | <.001 |
| 30–45 years | 296 (0.37) | 228,838 (0.32) | |
| 46–60 years | 289 (0.37) | 188,012 (0.26) | |
| 61+ years | 63 (0.08) | 149,059 (0.21) | |
| Race | |||
| White | 720 (0.91) | 565,568 (0.78) | <.001 |
| Black | 47 (0.06) | 103,423 (0.,4) | |
| Other | 24 (0.03) | 54,529 (0.08) | |
| Marital Status | |||
| Married/Cohabitant | 274 (0.35) | 455,833 (0.63) | <.001 |
| Widowed | 36 (0.05) | 44,071 (0.06) | |
| Separated/Divorced | 192 (0.24) | 76,733 (0.11) | |
| Never Married / Single | 274 (0.35) | 144,837 (0.20) | |
| Unknown | 15 (0.02) | 2,446 (0.003) | |
| Education | |||
| Never Attended | 16 (0.02) | 4,412 (0.01) | <.001 |
| Less than HS | 234 (0.30) | 133,614 (0.18) | |
| HS Degree / GED | 290 (0.37) | 208,056 (0.29) | |
| Some College | 158 (0.20) | 135,009 (0.19) | |
| BA/ Technical Degree | 63 (0.09) | 174,022 (0.24) | |
| Post College | 23 (0.03) | 56,067 (0.08) | |
| Unknown | 7 (0.01) | 12,740 (0.02) | |
| Federal Poverty Threshold | |||
| Above Threshold | 571 (0.72) | 497,214 (0.69) | <.001 |
| Below Threshold | 133 (0.17) | 77,041 (0.11) | |
| Unknown | 87 (0.11) | 149,665 (0.21) | |
| Region | |||
| Northeast | 86 (0.11) | 125,084 (0.17) | <.001 |
| Midwest | 151 (0.19) | 153,697 (0.21) | |
| South | 316 (0.40) | 265,393 (0.37) | |
| West | 237 (0.30) | 179,746 (0.25) |
Poverty threshold is based on family income and family size using the U.S. Census Bureau poverty thresholds. All counts and percentages are unweighted.
Figure 1 shows the proportion of cases vs. controls that were MCL-exposed (data available in Supplementary Table S4). For controls, this proportion ranged from 17% between 2000–2001 to 29% between 2010–2011, which reflects the growing adoption of MCL throughout our study period. For cases, the proportion exposed ranged between 23%−31%, albeit with much smaller sample sizes.
Between 2000 and 2005, 254 cases arose, of which 26% were MCL-exposed. In comparison, 367,519 controls were sampled in this period, of which 18% were MCL-exposed (Table 3). After adjusting for state and individual factors (Table 4), the rate of opioid overdose between 2000 and 2005 was not associated with MCL (aOR=1.22, 95% CI: 0.83–1.79). Between 2006–2010, 556 cases arose (27% MCL-exposed) and were compared to 356,401 controls (25% MCL-exposed). After adjusting for state and individual factors, the rate of opioid overdose between 2006 and 2011 was not associated with MCL exposure (aOR=0.87, 95% CI: 0.60–1.25). The tests of whether the association between MCLs and opioid overdose varied by sampling frame were not significant (ratio of aOR’s=0.71, 95% CI: 0.49–1.01).
Table 3.
Proportion of cases vs. controls residing in a state with a medical cannabis law (MCL), pooled by sample frame.
| 2000–2005 | Case (n) | (%) | Control (n) | (%) |
|
| ||||
| MCL | 65 | 0.26 | 66396 | 0.18 |
| No MCL | 189 | 0.74 | 301123 | 0.82 |
| Total* | 254 | 367519 | ||
|
| ||||
| 2006–2011 | Case (n) | (%) | Control (n) | (%) |
|
| ||||
| MCL | 149 | 0.27 | 90392 | 0.25 |
| No MCL | 407 | 0.73 | 266009 | 0.75 |
| Total* | 556 | 356401 | ||
Table 4.
Estimated odds ratios (OR) for Rx overdose associated with medical cannabis law (MCL) status stratified by sampling frame, and test of differences in association by sampling frame, NHIS participants 2000–2011. Region specific estimates at bottom.
| OR (p-value) 2000–2005 |
OR (p-value) 2006–2011 |
Ratio of OR’s 2006–2011 vs. 2000–2005 | |
|---|---|---|---|
| MCL vs. No MCL | |||
| crude model (year only)a | 1.43 (1.06–1.93) | 1.09 (0.90–1.32) | 0.76 (0.54–1.09) |
| state-level adjusted modelb | 1.21 (0.82–1.78) | 0.83 (0.58–1.20) | 0.70 (0.49–1.00) |
| individual-level adjusted modelc | 1.41 (1.04–1.92) | 1.03 (0.85–1.25) | 0.76 (0.53–1.08) |
| adjusted at both levelsd | 1.22 (0.83–1.79) | 0.87 (0.60–1.25) | 0.71 (0.49–1.01) |
crude model adjusts for analytical year only (the calendar match of cases and controls)
state-level model adjusts for census region and presence of “proactive” prescription monitoring programs.
individual-level model adjusted for age, race/ethnicity, sex, marital status, education, and poverty status.
adjusted at both levels includes all individual and state-level adjustments
DISCUSSION:
Using a novel nested case-control design with individual data from a yearly series of U.S. nationally representative surveys linked with death certificate records from the National Death Index, we did not find a significant association overall between MCL exposure and overdose. After adjusting for individual and state-level covariates, no association of MCL exposure and odds of opioid overdose fatality was found either between 2000–2005 or 2006–2010, and the association of MCL with odds of opioid overdose fatality did not differ significantly between these two time periods.
This study contributes additional information questioning whether MCLs have any overall protective effects. Our null finding aligns with several prior studies that found no overall association between MCL and opioid mortality over the same study period (D. Powell et al., 2018; Smart, 2015). However, these studies did find that MCL was negatively associated with opioid mortality among either older groups or among MCLs with dispensaries. While our study did not find evidence for a protective effect for this time period, we assumed that the effect of MCLs was homogenous across states (i.e., with a single binary MCL variable). This was consistent with the original study (Bachhuber et al., 2014; Shover et al., 2019). However, had we looked among MCLs with dispensaries (Freisthler, Sumetsky, Kranich, Chadwick, & Mair, 2020; Hsu & Kovács, 2021; D. Powell et al., 2018; Smith, 2020), we may have observed a protective effect. In fact, adjusting for census region did have a sizable impact on our estimates in the negative direction. Regional heterogeneity in MCLs has been observed previously (Williams, Olfson, Kim, Martins, & Kleber, 2016), and this heterogeneity may be explained by the unbalanced presence of active dispensaries and program enrollees during this period (Hsu & Kovács, 2021; D. Powell et al., 2018; Smart, 2015). To address this heterogeneity in MCL across states, future studies with larger samples, expanded mortality data, and more defined MCL classifications are needed.
Study limitations warrant mention. First, our design does not account for unobserved sources of confounding. However, importantly, the design does address regional variations and includes individual-level controls. In addition, we included a measure of “whether a state PDMP is permitted or required to identify suspicious reporting” as a control variable. While this measure does not account for the all of the variability in PDMPs, it does represent a robust measure of PDMP effectiveness (Mars, Bourgois, Karandinos, Montero, & Ciccarone, 2014) and therefore contributes to the rigor of our analytic approach. However, other unaccounted sources of confounding may have introduced bias into our estimates if they occurred simultaneously with state MCLs and also influenced the rate of opioid overdose, such as other opioid prescribing laws and practices (Davis & Lieberman, 2020) or Medicaid expansion (Kaufman et al., 2021). While state-level studies must contend with the potential noncomparability of states with and without MCL, in our study, individuals living in states with and without MCL may be more comparable. Future studies wary of these threats to validity may incorporate specific designs (e.g., propensity score matching) to address specific concerns (e.g., noncomparability). Second, our study is limited in power from low number of cases. Our computed odds ratios had fairly broad confidence intervals, so their inclusion of 1.0 is not a highly precise estimate of no effect. Future approaches could include more mortality-linked individuals (e.g., 1999–2014 National Health and Nutrition Examination Survey) or extended years of individual-level mortality follow-up. Third, we assumed that any effect of MCLs on opioid overdose is homogenous across states. It is possible that MCLs with dispensaries (or MCLs in certain regions) have a differential impact on opioid use outcomes. A more refined categorization of cannabis policy is still needed, and future studies should continue to assess heterogeneity in MCL effects. Fourth, we assumed that any impact of MCL would be immediate and uniform over time, which is typically done in these studies. However, it is possible that any impact of MCL on opioid mortality is lagged or delayed over time. Potential lags include both time from MCL passage to full implementation as well as any lag between MCL implementation and opioid mortality. Future studies should determine if either lagged effect exists. Finally, we assumed that outcome misclassification, if any, was nondifferential by state MCL status. Some studies have indicated that states without MCL have worse overdose death determination reporting quality (Kaufman et al., 2021). If states with MCL were more likely to include potential cases versus states without, this apparent bias would likely be positive (and towards the null for a protective effect).
CONCLUSIONS:
Although an early paper on this topic indicated that MCLs might be protective against opioid mortality (Bachhuber et al., 2014), we found no overall protective association between state MCLs and opioid overdose. Nonetheless, future studies could extend this research with more recent mortality data and with more refined cannabis policy classifications. The importance of the present study, despite the restricted set of years included, is two-fold, First, importantly, the findings provide an additional source of information countering claims of a protective effect of MCLs on opioid overdoses, suggesting that other solutions to the opioid overdose crisis are needed. Second, the study offers a potentially useful design to answer important population-level public health questions.
Supplementary Material
Acknowledgments
Funding is acknowledged from NIH grants R01DA048860 and T32DA031099 (Hasin), R01DA037866 (Martins), R01DA045872 (Cerda & Martins) and the New York State Psychiatric Institute.
Disclosures
Dr. Hasin acknowledges funding from Syneos Health. Dr. Shmulewitz, Dr. Kim & Dr. Martins report no financial relationships with commercial interests.
DISCLAIMER
The findings and conclusions in this paper are those of the author(s) and do not necessarily represent the views of the Research Data Center, the National Center for Health Statistics, or the Centers for Disease Control and Prevention.
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bachhuber MA, Saloner B, Cunningham CO, & Barry CL (2014). Medical cannabis laws and opioid analgesic overdose mortality in the united states, 1999–2010. JAMA Internal Medicine, 174(10), 1668–1673. doi: 10.1001/jamainternmed.2014.4005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford AC, & Bradford WD (2016). Medical Marijuana Laws Reduce Prescription Medication Use In Medicare Part D. Health Affairs (Millwood), 35(7), 1230–1236. doi: 10.1377/hlthaff.2015.1661 [DOI] [PubMed] [Google Scholar]
- Bradford AC, & Bradford WD (2017). Medical Marijuana Laws May Be Associated With A Decline In The Number Of Prescriptions For Medicaid Enrollees. Health Affairs (Millwood), 36(5), 945–951. doi: 10.1377/hlthaff.2016.1135 [DOI] [PubMed] [Google Scholar]
- Caputi TL, & Sabet KA (2018). Population-Level Analyses Cannot Tell Us Anything About Individual-Level Marijuana-Opioid Substitution. American Journal of Public Health, 108(3), e12. doi: 10.2105/ajph.2017.304253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Ponicki WR, Smith N, Rivera-Aguirre A, Davis CS, Marshall BDL, . . . Martins SS (2020). Measuring Relationships Between Proactive Reporting State-level Prescription Drug Monitoring Programs and County-level Fatal Prescription Opioid Overdoses. Epidemiology, 31(1), 32–42. doi: 10.1097/ede.0000000000001123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Nathan W., Burkhardt Jesse, & Flyr Matthew. (2020). THE EFFECTS OF RECREATIONAL MARIJUANA LEGALIZATION AND DISPENSING ON OPIOID MORTALITY. Economic Inquiry, 58(2), 589–606. doi: 10.1111/ecin.12819 [DOI] [Google Scholar]
- Chihuri S, & Li G (2019). State marijuana laws and opioid overdose mortality. Injury Epidemiology, 6, 38. doi: 10.1186/s40621-019-0213-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data Linkage Team. (2015). Comparative analysis of the NHIS public-use and restricted-use linked mortality files: 2015 public-use data release. In Center N & Statistics f. H. (Eds.). Hyattsville, Maryland. [Google Scholar]
- Daubresse M, Chang HY, Yu Y, Viswanathan S, Shah ND, Stafford RS, . . . Alexander GC (2013). Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010. Medical Care, 51(10), 870–878. doi: 10.1097/MLR.0b013e3182a95d86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CS, & Lieberman AJ (2020). Laws limiting prescribing and dispensing of opioids in the United States, 1989–2019. Addiction. doi: 10.1111/add.15359 [DOI] [PubMed] [Google Scholar]
- Finney John W., Humphreys Keith, & Harris Alex H. S. (2015). What Ecologic Analyses Cannot Tell Us About Medical Marijuana Legalization and Opioid Pain Medication Mortality. JAMA Internal Medicine, 175(4), 655–656. doi: 10.1001/jamainternmed.2014.8006 [DOI] [PubMed] [Google Scholar]
- Freisthler Bridget, Sumetsky Natalie, Kranich Christiana, Chadwick Caileigh, & Mair Christina. (2020). Opioid Misuse and the Availability of Medical Marijuana Through Dispensaries. Journal of studies on alcohol and drugs, 81(4), 489–496. doi: 10.15288/jsad.2020.81.489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, West R, Marsden J, Humphreys K, Neale J, & Petry N (2018). It is premature to expand access to medicinal cannabis in hopes of solving the US opioid crisis. Addiction. doi: 10.1111/add.14139 [DOI] [PubMed] [Google Scholar]
- Harris AH, Humphreys K, & Finney JW (2015). State-level relationships cannot tell us anything about individuals. American Journal of Public Health, 105(4), e8. doi: 10.2105/ajph.2015.302604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Cerdá M, Keyes KM, Stohl M, Galea S, & Wall MM (2017). US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry, 74(6), 579–588. doi: 10.1001/jamapsychiatry.2017.0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu Greta, & Kovács Balázs. (2021). Association between county level cannabis dispensary counts and opioid related mortality rates in the United States: panel data study. The BMJ, 372, m4957. doi: 10.1136/bmj.m4957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman DE, Nihal AM, Leppo JD, Staples KM, McCall KL, & Piper BJ (2021). Opioid Mortality Following Implementation of Medical Cannabis Programs in the United States. Pharmacopsychiatry, 54(2), 91–95. doi: 10.1055/a-1353-6509 [DOI] [PubMed] [Google Scholar]
- Kim JH (2019). State-level relationships cannot tell us anything about individuals, but what they tell us about states should still be of interest. Addiction, 114(4), 756–757. doi: 10.1111/add.14543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Santaella-Tenorio J, Mauro C, Wrobel J, Cerda M, Keyes KM, . . . Li G (2016). State Medical Marijuana Laws and the Prevalence of Opioids Detected Among Fatally Injured Drivers. American Journal of Public Health, e1–e6. doi: 10.2105/ajph.2016.303426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropp Lopez AK, Nichols SD, Chung DY, Kaufman DE, McCall KL, & Piper BJ (2020). Prescription Opioid Distribution after the Legalization of Recreational Marijuana in Colorado. International Journal of Environmental Research and Public Health, 17(9). doi: 10.3390/ijerph17093251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LawAtlas. (2017). State Laws and Other Regulatroy Policies Related to Pain Care. from https://lawatlas.org/datasets/state-laws-and-other-regulatory-policies-related-to-pain-care-final
- Lopez CD, Boddapati V, Jobin CM, & Hickernell TR (2021). State Medical Cannabis Laws Associated With Reduction in Opioid Prescriptions by Orthopaedic Surgeons in Medicare Part D Cohort. Journal of the American Academy of Orthopaedic Surgeons, 29(4), e188–e197. doi: 10.5435/jaaos-d-19-00767 [DOI] [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, & Ciccarone D (2014). “Every ‘never’ I ever said came true”: transitions from opioid pills to heroin injecting. International Journal of Drug Policy, 25(2), 257–266. doi: 10.1016/j.drugpo.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, . . . Wall M (2016). State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug and Alcohol Dependence, 169, 26–32. doi: 10.1016/j.drugalcdep.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Ponicki W, Smith N, Rivera-Aguirre A, Davis CS, Fink DS, . . . Cerdá M (2019). Prescription drug monitoring programs operational characteristics and fatal heroin poisoning. International Journal of Drug Policy, 74, 174–180. doi: 10.1016/j.drugpo.2019.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael BJ, Van Horn RL, & Viscusi WK (2020). The impact of cannabis access laws on opioid prescribing. Journal of Health Economics, 69, 102273. doi: 10.1016/j.jhealeco.2019.102273 [DOI] [PubMed] [Google Scholar]
- Neilson LM, Swift C, Swart ECS, Huang Y, Parekh N, Munshi KD, . . . Good CB (2021). Impact of Marijuana Legalization on Opioid Utilization in Patients Diagnosed with Pain. Journal of General Internal Medicine. doi: 10.1007/s11606-020-06530-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Powell D, Heaton P, & Sevigny EL (2015). Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. Journal of Policy Analysis and Management, 34(1), 7–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi Leonard J., & Ryan George W. (2006). Opioid Analgesics and Rates of Fatal Drug Poisoning in the United States. American Journal of Preventive Medicine, 31(6), 506–511. doi: 10.1016/j.amepre.2006.08.017 [DOI] [PubMed] [Google Scholar]
- Phillips E, & Gazmararian J (2017). Implications of prescription drug monitoring and medical cannabis legislation on opioid overdose mortality. Journal of Opioid Management, 13(4), 229–239. doi: 10.5055/jom.2017.0391 [DOI] [PubMed] [Google Scholar]
- Powell D, Pacula RL, & Jacobson M (2018). Do medical marijuana laws reduce addictions and deaths related to pain killers? Journal of Health Economics, 58, 29–42. doi: 10.1016/j.jhealeco.2017.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell David, Pacula Rosalie Liccardo, & Jacobson Mireille. (2015). Do Medical Marijuana Laws Reduce Addictions and Deaths Related to Pain Killers? National Bureau of Economic Research Working Paper Series, No. 21345. doi: 10.3386/w21345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raji MA, Abara NO, Salameh H, Westra JR, & Kuo YF (2019). Association between cannabis laws and opioid prescriptions among privately insured adults in the US. Preventive Medicine, 125, 62–68. doi: 10.1016/j.ypmed.2019.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S (1994). The fallacy of the ecological fallacy: the potential misuse of a concept and the consequences. American Journal of Public Health, 84(5), 819–824. doi: 10.2105/ajph.84.5.819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura Luis E., Mauro Christine M., Levy Natalie S., Khauli Nicole, Philbin Morgan M., Mauro Pia M., & Martins Silvia S. (2019). Association of US Medical Marijuana Laws With Nonmedical Prescription Opioid Use and Prescription Opioid Use Disorder. JAMA Network Open, 2(7), e197216–e197216. doi: 10.1001/jamanetworkopen.2019.7216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah A, Hayes CJ, Lakkad M, & Martin BC (2019). Impact of Medical Marijuana Legalization on Opioid Use, Chronic Opioid Use, and High-risk Opioid Use. Journal of General Internal Medicine, 34(8), 1419–1426. doi: 10.1007/s11606-018-4782-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover CL, Davis CS, Gordon SC, & Humphreys K (2019). Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proceedings of the National Academy of Sciences of the United States of America, 116(26), 12624–12626. doi: 10.1073/pnas.1903434116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart Rosanna. (2015). The kids aren’t alright but older adults are just fine: Effects of medical marijuana market growth on substance use and abuse. Browser Download This Paper. [Google Scholar]
- Smith Rhet A. (2020). THE EFFECTS OF MEDICAL MARIJUANA DISPENSARIES ON ADVERSE OPIOID OUTCOMES. Economic Inquiry, 58(2), 569–588. doi: 10.1111/ecin.12825 [DOI] [Google Scholar]
- StataCorp. (2013). Stata Statistical Software. College Station, TX: StataCorp LP. [Google Scholar]
- Wen H, Hockenberry JM, & Cummings JR (2015). The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. Journal of Health Economics, 42, 64–80. doi: 10.1016/j.jhealeco.2015.03.007 [DOI] [PubMed] [Google Scholar]
- Wen Jiebing, Wen Hefei, Butler JS, & Talbert Jeffery C. (2021). The impact of medical and recreational marijuana laws on opioid prescribing in employer-sponsored health insurance. Health Economics, n/a(n/a). doi: 10.1002/hec.4237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams Arthur Robin, Olfson Mark, Kim June H., Martins Silvia S., & Kleber Herbert D. (2016). Older, Less Regulated Medical Marijuana Programs Have Much Greater Enrollment Rates Than Newer ‘Medicalized’ Programs. Health Affairs (Millwood), 35(3), 480–488. doi: 10.1377/hlthaff.2015.0528 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


