In this commentary, we discuss the health equity implications of collecting and reporting data stratified by binary male/female categories in sexual health and STI/HIV research and surveillance without meaningful inclusion of transgender, non-binary and gender diverse identities. Numerous institutional bodies have recommended collecting and reporting data disaggregated by trans-inclusive categories, including the National Institutes of Health and the National Academy of Sciences.1,2 However, a review of articles published by Sexually Transmitted Diseases in 2020, for example, yielded 121 papers (of 166 that included human participants) that only reported data by male/female categories and conflated sex assigned at birth with gender (e.g. by referring to people assigned female at birth as women, and people assigned male at birth as men). In addition, core surveillance systems and large national data sources, such as the Centers for Disease Control and Prevention (CDC) 2018 STD Surveillance Report and Health People 2030, also continue to report data in this way.
Trans adults comprise 0.6% of the population, or at least 1.4 million adults living in the US, and a recent study estimated that approximately 1.2 million adults in the US identify as non-binary.3–5 In addition, an estimated 1.3% to 2.7% of adolescents in the US identify as trans or non-binary.6–8 Trans and non-binary people are disproportionally burdened by poor health outcomes, including STIs and HIV, due to socio-structural factors rooted in stigma and discrimination.9–11 In addition, trans and non-binary people report significant barriers to health care, including harassment, refusal of care by health care providers, and difficulty obtaining specific and trans-affirming health information.12,13 Notably, there are significant disparities within trans populations; for example, Black and Indigenous trans women are disproportionately living with HIV and experience syndemic conditions (such as unstable housing and reliance on sex work due to economic disenfranchisement) due to the intersectional impact of structural racism, colonialism, and misogyny, as well as transphobia.9,14 Lastly, while this commentary focuses on trans-inclusivity, it is essential to acknowledge the harms that are inflicted upon intersex individuals (who may or may not identify as transgender) through the use of the same prescriptive male/female sex categories in medicine and research, which are a product of Western colonial thought.15 Due to sociocultural and legal mandates in the US that categorize individuals as either male or female, intersex infants and children are often unnecessarily and involuntarily subjected to invasive surgeries, hormonal treatments, and social harms, while their identities and experiences are also frequently excluded from research.1,16
We recommend that Sexually Transmitted Diseases and other peer reviewed journals adopt policies that require authors to report disaggregated data for trans and non-binary identities and to use precise and inclusive language. In the absence of available and accurate data on gender identity, we recommend that journals require authors to explicitly acknowledge the limitations of their data. In the sections that follow, we explain how the practice of using binary male/female categories contributes to the erasure of trans and non-binary experiences, including health inequities, drawing on specific examples within the fields of sexual health and HIV/STIs. We conclude by providing five concrete recommendations for inclusive data collection and reporting.
We want to position ourselves in relation to this commentary and our call for researchers and public health practitioners to think critically about how cisnormative assumptions manifest in data collection and reporting. The authors include experts in epidemiology, nursing, infectious disease medicine, social work, and LGBTQ+ activism, all with significant experience working with and within queer and trans communities. Authors also have extensive experience conducting sexual health-related research and public health practice to reduce disparities in HIV/STIs. Authors identify as a gender non-binary queer person, a genderqueer drag queen, queer trans men, queer cis women, and heterosexual cis women. This commentary aims to reiterate and amplify existing pragmatic, actionable recommendations from trans communities, advocates, and scientists that improve the inclusion of trans and non-binary people in research and surveillance.
Erasure, Exclusion, and Misclassification
Erasure, exclusion, and misclassification are related processes that contribute to the informational and health inequities for trans and non-binary populations. As first described by Bauer et al.’s (2009) framework, erasure is one of the primary processes through which conscious and unconscious cisnormative bias produces systemic barriers to care for trans communities.17 In the context of data collection and reporting, erasure is a process that is often enacted through the misclassification and/or exclusion of trans and non-binary people and identities from surveillance, health systems, and research. It can occur—and be interrupted—at multiple stages of formative research, data collection and analysis and across institutional levels.
For example, institutions may “lack policies that accommodate trans identities or trans bodies, including the lack of knowledge that such policies are even necessary.”17 This includes medical forms/records, surveillance systems/surveys, and research studies that do not provide trans and non-binary response options. Institutional erasure also occurs when researchers intentionally or unintentionally exclude trans and non-binary people from research studies, or do not meaningfully engage trans communities, resulting in sample sizes that are too small for statistical inference or from which to draw conclusions. Exclusion constitutes more than the mere absence of trans representation in data; it also occurs when research fails to examine trans experience, and therefore cannot be generalized to trans and non-binary populations. In addition, when sample sizes are “too small,” data from trans and non-binary people are frequently evaluated in aggregate or even aggregated with cisgender populations.18
Erasure is also characterized by a lack of public health policies, guidelines and recommendations for trans and non-binary populations, and lack of trans-specific training for healthcare providers.19,20 For example, the CDC does not provide specific recommendations for STI screening, and the US Preventive Services Task Force does not provide specific recommendations for PrEP use among trans and non-binary people, despite this population having a high incidence of HIV/STIs.21,22 Both sets of recommendations point to a lack of available data on trans populations, for example, stating that: “trials of PrEP enrolled few transgender women and no trials have been conducted among transgender men… its use may be considered in all persons (cisgender and transgender) at high risk of sexual acquisition of HIV.”21
In this way, institutional erasure both produces and is reproduced by informational erasure, or a lack of “knowledge regarding trans people… and the assumption that such knowledge does not exist even when it may.”17 For example, few national surveys or surveillance systems use validated trans-inclusive measures for ascertaining gender.23,24 A review of 71 STI surveillance jurisdictions found that in 2015, 41 (58%) jurisdictions collected data using male/female categories only. In addition, although 11 (15%) jurisdictions collected disaggregated data on trans women and trans men, only 3 reported disaggregated data on trans populations in their STI surveillance reports, suggesting that these data are misclassified or that transgender data were excluded.25 Thus, even when data on trans and non-binary identities are collected, these data are frequently obfuscated when published/reported.26
In many cases, when data are reported by binary categories (male/female or man/woman), the direction and degree of misclassification is unclear. An assumption is frequently made that the male/female variable available in a data source refers to sex assigned at birth. However, trans and non-binary people may be misclassified into their sex assigned at birth (e.g. trans men may be categorized as female) or be aggregated with cisgender people of the same gender (e.g. data on transgender women are reported with cisgender women). The direction and degree of misclassification is dependent both on data collection methods and analytic choices made by the researcher. For example, prior studies have shown that when “sex” is ascertained based on the sound of a participant’s voice, such as in the telephone-base Behavioral Risk Factor Surveillance System, one-third of trans participants are categorized concordant with the gender (e.g. trans men as male and trans women as female) while the remaining two-thirds are categorized according to their presumed sex assigned at birth (e.g. trans men as female and trans women as male).27,28 In studies that conflate sex and gender in their survey questions (e.g. “Are you male or female?”), trans respondents may be more likely to provide a response that is concordant with their gender. In studies based on medical or insurance records, male/female categories most likely reflect the current gender marker on an individual’s identification documents, which could either reflect their current gender or their sex assigned at birth.
The aforementioned processes of erasure, exclusion and misclassification have led to a paucity of high-quality data on the sexual health and overall wellbeing of trans and non-binary people, since most data on trans health are from small, cross-sectional, and clinical samples.29,30 The conflation of sex assigned at birth and gender obscures health disparities among trans and non-binary populations and neglects important socio-structural factors that impact health outcomes.9,31s In addition, lack of meaningful data on trans experiences impacts how and in what ways funding streams are determined that are aimed at addressing trans health disparities. The absence of data on health outcomes, healthcare guidelines, and evidence-based treatment and interventions for trans and non-binary people has contributed to suboptimal or delayed sexual health care, such as lower rates of HIV/STI testing, pre-exposure prophylaxis (PrEP) uptake, antiretroviral therapy (ART) use, or cervical cancer screenings.32–35s
Recommendations
We recommend the following practices for trans-inclusive data collection and reporting in alignment with existing guidance.1,9,26,30,36–39s We believe that peer reviewed journals and editors can play an important role in promoting health equity and the availability of data on trans and non-binary populations by requiring authors to adopt the following recommendations.
1. Collect data on trans and non-binary identities using validated and recommended methods.
All studies, health care systems, and surveillance systems should collect data on transgender, non-binary, and intersex identities using a two-step question that separately ascertains a respondent’s current gender identity and sex assigned at birth (Figure 1). The two-step question has been validated and used in both adult40–42s and adolescent populations43s and is currently recommended by numerous institutional bodies, including the National Academies of Science, the National Institute of Allergy and Infectious Diseases (NIAID) Division of AIDS, Institute of Medicine, Department of Health and Human Services, The Williams Institute, Fenway Health, and The Center of Excellence for Transgender Health at University of California San Francisco.39s,44s We strongly recommend including both non-binary categories and write-in gender options, since a large proportion of trans people identify with terms beyond the binary categories of man/woman (e.g. non-binary, genderqueer, gender non-conforming, gender fluid, agender, and more). In some settings, it may also be important to include indigenous and additional culturally specific response options, such as third-gender, two-spirit, hijra, fa’afafine, and mahu. Intersex identity may be best ascertained using a separate question since intersex individuals are often assigned a male or female sex at birth, underscoring the sociocultural construction of binary “sex” categories. In addition to addressing critical gaps in data available on trans and non-binary populations, the standardized collection of gender identity data using the two-step method facilitates direct comparison between studies and settings, including meta-analysis.30 Importantly, qualitative studies demonstrate that these data collection approaches reflect community preferences for how to ask about gender identity, although emerging literature suggests that some trans and non-binary people prefer data collection method that do not seek to ascertain sex assigned at birth.45–47s
Figure 1. Sample Two-Step Question.
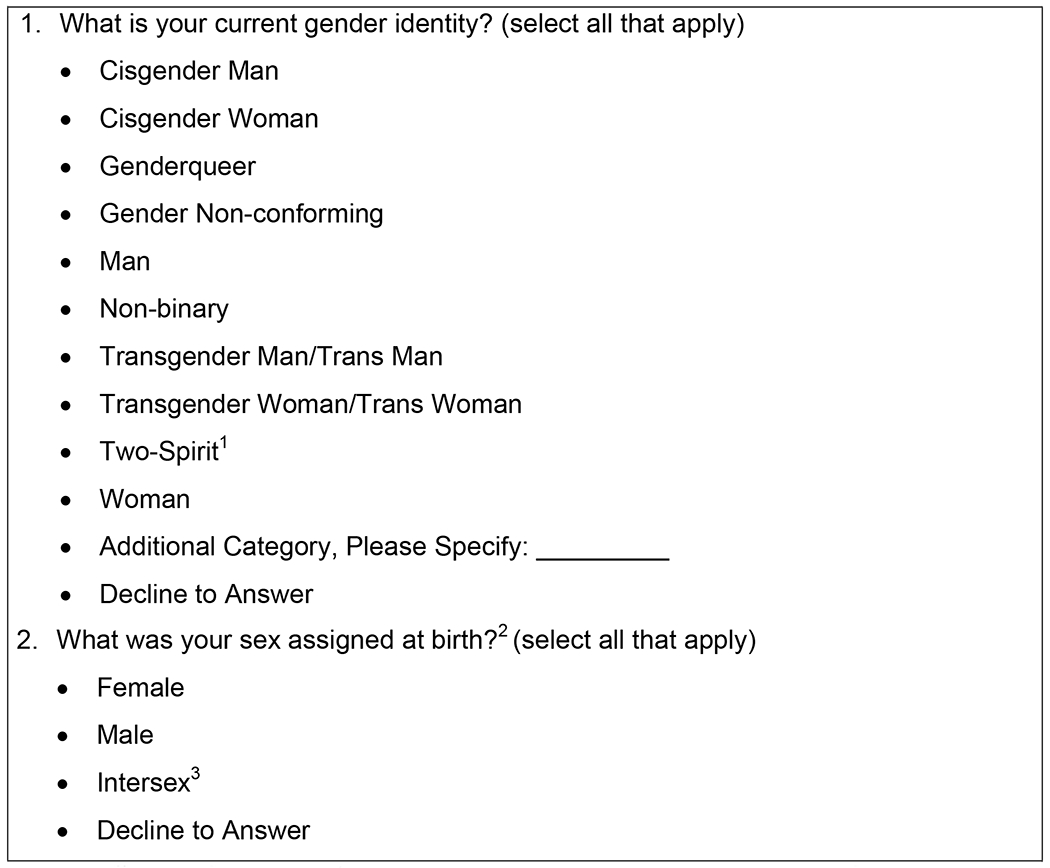
The wording for this sample two-step question is adapted from the NIAID’s Division of AIDS Cross-Network Transgender Working Group Recommendations.39s
1 In some settings, it may also be important to include additional indigenous and culturally specific response options, such as third-gender, hijra, fa’afafine, and mahu.
2 Emerging literature suggests that some trans and non-binary people oppose the sex assigned at birth question and propose alternatives such as explicitly asking “Do you identify as transgender?” and/or querying anatomy when necessary.45–47s
3 Intersex identity may be best ascertained using a separate question since intersex individuals are often assigned a male or female sex at birth, underscoring the sociocultural construction of binary “sex” categories.45s
2. Report disaggregated data.
Trans women, trans men and non-binary people are distinct and diverse populations. They differ with respect to their identities, burdens of disease, barriers and facilitators of health care, and other socio-structural factors that impact their health and wellness. Therefore, authors should not report data for trans and non-binary persons as a single group. Rather, we recommend reporting disaggregated data for trans women, trans men, and non-binary people, including descriptive statistics, measures of association, and incidence rates. In the case of small numbers, we recommend reporting the gender of all participants, regardless of cell size. When there are potential confidentiality concerns due to small sample sizes, we recommend reporting disaggregated health outcome data in accordance with local-, state- and institution-specific guidelines. To avoid issues related to small numbers, we recommend researchers to use trans-inclusive recruitment strategies and study designs that are powered to provide meaningful data for trans and non-binary people, even when not conducting trans-specific research.30,48–50s
3. Acknowledge limitations of the data.
We acknowledge that in many cases, researchers are analyzing historical data sources that only collect data on male/female categories; therefore, it is not possible to report data on trans and non-binary participants. We recommend that authors explicitly state the limitations of their data and their assumptions about the sex assigned at birth and genders of their study population. An implicit assumption is frequently made that a sex/gender variable refers to a participant’s sex assigned at birth. However, as described above, this variable likely misclassifies both sex assigned at birth and gender; and instead, may be a measure of an altogether different construct, such as a participant’s legal gender marker. Examples of how authors can address data limitations are provided in Table 1. In addition, authors should note other local, state, and institutional limitations related to confidentiality concerns or that influence data collection or reporting.
Table 1.
Examples of how to discuss limitations of existing data sources
| Scenario | Example |
|---|---|
| Medical and/or insurance records that collect a binary male/female variable. | “The binary male/female categories available in our data likely reflects the legal gender marker of each patient. This is neither an accurate measure of sex assigned at birth or of gender identity, since many transgender and non-binary individuals have a legal gender marker that does not reflect their gender identity, and few states allow for a gender-neutral gender marker. We are thus unable to identify transgender and non-binary patients, who are misclassified in our source data. The direction of this misclassification is also unknown.” |
| Survey or interview collects data using imprecise language that conflates sex assigned at birth and gender (e.g. “Are you male or female?”). | “The interview script does not distinguish between sex assigned at birth and gender identity, for example, by conflating individuals who are men with male sex assigned at birth. We assume that this measure may more likely reflect a participant’s reported gender identity rather than their sex assigned at birth. Notably, this measure does not allow us to identify transgender and non-binary participants, who are misclassified in our source data.” |
| Data source uses outdated or problematic language. | “We subsequently refer to individuals who selected transgender male to female or who reported female gender identity and male sex assigned at birth as transgender women.” |
4. Use trans-inclusive language that does not conflate sex assigned at birth and gender.
We recommend that authors use precise and inclusive language that does not conflate sex assigned at birth and gender. Specifically, authors should not generally refer to people assigned female at birth as women and people assigned male at birth as men. In addition, we recommend authors explicitly use the term cisgender when their study population includes cisgender men and cisgender women, rather than using the labels men and women to implicitly mean non-transgender (e.g. imprecisely using “men who have sex with men” when exclusively referring to cisgender men who have sex with other cisgender men). Language is always evolving, and there are a number of academic51–57s and community-based58s,59s resources about trans-inclusive language practices and specific terminology to use in place of harmful and/or outdated terms, including language guides developed by NIAID.39s,60s Some common terms that appear in sexual health research and their alternatives are presented in Table 2. Instead of reproducing terminology that appear in data collection instruments, researchers can acknowledge this limitation in the methodology section (Table 1).
Table 2.
Examples of trans-inclusive and gender affirming terminology
| Instead of… | Use… | References/Further Reading |
|---|---|---|
| sex, biological sex, or natal sex | sex assigned at birth | 39s,47s,55s,58s,60s,61s |
| male-to-female or MTF | transgender women or trans women | 39s,55s,58s,60s |
| female-to-male or FTM | transgender men or trans men | |
| biological female or female-bodied | assigned female at birth | 51–53s,58s |
| biological male or male-bodied | assigned male at birth | |
| female reproductive tract | name specific anatomy (e.g. vaginal, cervical), or people with vaginas | 51–53s,59s |
| male reproductive tract | name specific anatomy (e.g. penile, urethral), or people with penises | |
| women’s health | sexual and reproductive health | 57s |
| pregnant women | pregnant people | 57s,60s |
| cross-sex hormones | gender affirming hormone therapy | 55s |
| sex change or sex reassignment surgery | gender affirming surgery, or name specific procedures | 55s |
5. Engage with trans and non-binary communities.
We recommend that researchers elevate the work of trans scientists and healthcare providers and engage with local trans-led organizations and their respective communities at all stages of the research process using community-based participatory research or participatory action research approaches. Concepts, definitions, and language used to talk about sex, gender, and transgender bodies and experiences are cultural, historical, and have varied over place and time, and are likely to continue to change. Further, in order to develop and evaluate effective interventions for trans and non-binary populations, the lived experience of trans people must be reflected in the very design of research by asking questions that are meaningful and relevant to trans lives. Thus, we recommend ongoing practices for including trans and non-binary people in the process of creating knowledge. In addition, due to the power imbalances common in trans health research and the intersecting institutional harms experienced by these populations, community engagement is also important when conducting secondary analyses of existing data.
While many of the examples presented in this commentary are specific to HIV/STIs, these recommendations are relevant to all fields of behavioral health, public health, and medicine. Trans-inclusive data collection and reporting will facilitate a stronger understanding of the health and wellbeing of trans and non-binary communities, as well as disparities within trans populations. To optimize the health and policy influence of scientific inquiry, research must account for the impact of social determinants of health, structural racism, and stigma on all LGBTQ+ populations—especially trans and non-binary people. A fundamental goal of public health is to identify, describe, and explain disparities, with the ultimate aim of eliminating health inequity. However, we will never achieve health equity without changing our institutions and research practices to ensure that trans and non-binary people are meaningfully and intentionally represented.
Supplementary Material
Acknowledgements:
The authors thank Alic Shook for reviewing and providing feedback on this manuscript.
Conflicts of Interest and Sources of Funding:
DMT receives support from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (Award Number F31AI152542). LAB and CMK have received research support, unrelated to this work, from Hologic. All other authors have no conflicts of interest.
References
- 1.National Academies of Sciences Engineering and Medicine. Understanding the Well-Being of LGBTQI+ Populations. Published online 2020. doi: 10.17226/25877 [DOI]
- 2.National Institutes of Health Sexual and Gender Minority Research Office. Strategic Plan to Advance Research on the Health and Well-Being of Sexual & Gender Minorities.; 2020.
- 3.Meerwijk EL, Sevelius JM. Transgender Population Size in the United States: a Meta-Regression of Population-Based Probability Samples. Am J Public Heal. 2017;107(2):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flores AR, Herman JL, Gates GJ, Brown TNT. How Many Adults Identify as Transgender in the United States?; 2016. Accessed November 10, 2018. https://williamsinstitute.law.ucla.edu/wp-content/uploads/How-Many-Adults-Identify-as-Transgender-in-the-United-States.pdf
- 5.Wilson BD, Meyer IH. Nonbinary LGBTQ Adults in the United States.; 2021. doi: 10.1037/sgd0000384 [DOI]
- 6.Eisenberg ME, Gower AL, McMorris BJ, et al. Risk and Protective Factors in the Lives of Transgender/Gender Nonconforming Adolescents. J Adolesc Heal. 2017;61(4):521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perez-Brumer A, Day JK, Russell ST, Hatzenbuehler ML. Prevalence and Correlates of Suicidal Ideation Among Transgender Youth in California: Findings From a Representative, Population-Based Sample of High School Students. J Am Acad Child Adolesc Psychiatry. 2017;56(9):739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johns MM, Lowry R, Andrzejewski J, et al. Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students — 19 States and Large Urban School Districts, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(3):67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wesp LM, Malcoe LH, Elliott A, Poteat T. Intersectionality Research for Transgender Health Justice: A Theory-Driven Conceptual Framework for Structural Analysis of Transgender Health Inequities. Transgender Heal. 2019;4(1):287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Gerwen OT, Jani A, Long DM, et al. Prevalence of Sexually Transmitted Infections and Human Immunodeficiency Virus in Transgender Persons: A Systematic Review. Transgender Heal. 2020;5(2):90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becasen JS, Denard CL, Mullins MM, et al. Estimating the Prevalence of HIV and Sexual Behaviors Among the US Transgender Population: A Systematic Review and Meta-Analysis, 2006–2017. Am J Public Health. 2019, 109(1): e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.James SE, Herman JL, Rankin S, et al. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality; 2016. http://www.transequality.org/sites/default/files/docs/usts/USTSFullReport-FINAL1.6.17.pdf [Google Scholar]
- 13.Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women—National HIV Behavioral Surveillance, 7 U.S. Cities, 2019–2020. HIV Surveillance Special Report 27.; 2021. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- 15.Feinberg L Transgender Warriors: Making History from Joan of Arc to Dennis Rodman. Beacon Press; 1996. https://books.google.com/books?id=xP-RngEACAAJ [Google Scholar]
- 16.Human Rights Watch & InterACT. “I Want to Be Like Nature Made Me”: Medically Unnecessary Surgeries on Intersex Children in the US.; 2017. Accessed April 29, 2021. https://www.hrw.org/sites/default/files/report_pdf/lgbtintersex0717_web_0.pdf
- 17.Bauer GR, Hammond R, Travers R, et al. “I Don’t Think This Is Theoretical; This Is Our Lives”: How Erasure Impacts Health Care for Transgender People. J Assoc Nurses AIDS Care. 2009;20(5):348–361. [DOI] [PubMed] [Google Scholar]
- 18.Poteat TC, van der Merwe LLA, Sevelius J, Keatley J. Inclusion as illusion : erasing transgender women in research with MSM. JIAS. 2021;24(1):10–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nowaskie DZ, Patel AU and Fang RC. A multicenter, multidisciplinary evaluation of 1701 healthcare professional students’ LGBT cultural competency: Comparisons between dental, medical, occupational therapy, pharmacy, physical therapy, physician assistant, and social work students. PLoS One. 2020;15(8):e0237670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hana T, Butler K, Young LT, et al. Transgender health in medical education. Bull World Health Organ. 2021;99(4):296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Owens DK, Davidson KW, Krist AH, et al. Preexposure Prophylaxis for the Prevention of HIV Infection: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;321(22):2203. [DOI] [PubMed] [Google Scholar]
- 22.Workowski KA, Bolan GA. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep. 2015;64(3):9–16. [PMC free article] [PubMed] [Google Scholar]
- 23.Patterson JG, Jabson JM, Bowen DJ. Measuring Sexual and Gender Minority Populations in Health Surveillance. LGBT Heal. 2017;4(2):82–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bauer GR, Braimoh J, Scheim AI, Dharma C. Transgender-inclusive measures of sex/gender for population surveys: Mixed-methods evaluation and recommendations. Dalby AR, ed. PLoS One. 2017;12(5):e0178043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen A, Katz KA, Leslie KS, Amerson EH. Inconsistent Collection and Reporting of Gender Minority Data in HIV and Sexually Transmitted Infection Surveillance Across the United States in 2015. Am J Public Health. 2018;108(S4):S274–S276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poteat T, German D, Flynn C. The conflation of gender and sex: Gaps and opportunities in HIV data among transgender women and MSM. Glob Public Health. 2016;11(7-8):835–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riley NC, Blosnich JR, Bear TM, Reisner SL. Vocal Timbre and the Classification of Respondent Sex in US Phone-Based Surveys. Am J Public Health. 2017;107(8):1290–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tordoff D, Andrasik M, Hajat A. Misclassification of Sex Assigned at Birth in the Behavioral Risk Factor Surveillance System and Transgender Reproductive Health. Epidemiology. 2019; 30(5): 669–678. [DOI] [PubMed] [Google Scholar]
- 29.MacCarthy S, Poteat T, Xia Z, et al. Current research gaps: a global systematic review of HIV and sexually transmissible infections among transgender populations. Sex Health. 2017;14(5):456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reisner SL, Deutsch MB, Bhasin S, et al. Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


