Abstract
Objective
To analyze the deformity origins and distribution among valgus knees to individualize their morphological features.
Methods
Radiographic images of 105 valgus knees were analyzed. Long‐film radiographs and computed tomography were collected for every knee. A malalignment test was performed on standing long‐film radiographs. The hip‐knee‐ankle angle (HKA), the anatomical lateral distal femoral angle (aLDFA), and the anatomical medial proximal tibial angle (aMPTA) were measured on long‐film radiographs. The distal condylar angle and posterior condylar angle on distal femur were further measured on computed tomography scans. The tibial bone varus angle was measured on long‐film radiographs as well. All the valgus knees were sorted into different subtypes according to the origins of bony deformity, and the prevalence of each subtype was reported. Finally, to examine the inter‐observer reproducibility of this classification system, two observers measured the deformities and did the classification for all the 105 knees independently and then the intraclass correlation coefficient (ICC) was calculated.
Results
Among the 105 knees, 48 knees (45.7%) had apparent deformity from the tibial plateau, and 62 knees (59.0%) had apparent deformity from the supracondylar region of the femur. Eighteen knees (17.1%) had distal condylar angle >7°, among which 11 knees had posterior condylar angle >3° simultaneously. Valgus knees had five subtypes of bone deformity origins—the supracondylar part of the femur, the distal aspect of the lateral femoral condyle, both distal and posterior aspects of the lateral femoral condyle, the tibial plateau, or the metaphyseal segment of the tibia. A valgus knee could be labeled as only one subtype, or a combination of two or more subtypes. Labeling 105 knees with origin of the most severe deformity, the prevalence of each subtype was 40.0%, 5.7%, 9.5%, 28.6%, and 16.2%, respectively. The intra‐observer and inter‐observer ICC of this classification system was 0.992 and 0.976, respectively.
Conclusions
Valgus knees can be classified into different subtypes according to deformity origins. This radiological classification system has satisfactory reproducibility. It helps surgeons better individualize morphological features of valgus knees.
Keywords: Classification/Subtype, Deformity origin, Total knee arthroplasty, Valgus knee
Valgus deformities could be classified into five subtypes according to the deformity origin on radiological analysis—the supracondylar region of the femur (F2), the distal lateral femoral condyle (F1a), both distal and posterior lateral femoral condyle (F1b), the tibial plateau (T1), or the metaphyseal segment of the tibia (T2).
This classification helps personalize valgus knees in terms of deformity origins, and based on that, the status of the lateral collateral ligament (LCL) and lateral joint capsule can be sequentially predicted.
It helps determine the deformity correction and soft‐tissue balancing strategies and techniques in TKAs.
A new classification system (JST classification) for valgus knees and the prevalence of each subtype.
Introduction
Deformity correction and soft‐tissue balancing remain technically challenging in total knee arthroplasty (TKA) for knees with severe valgus deformity. Severe preoperative valgus deformity has been shown to be a predictor of inferior clinical outcome, higher incidence of residual deformity, and patellar maltracking after surgery 1 , 2 . Karachalios et al. reported 38.2% of the severe valgus knees had residual deformity after TKA, and they confirmed that worse clinical results were related to residual deformities 1 . Yang et al. reported a similar rate (35.9%) of residual deformity for valgus knees after TKA and they further revealed that different origins of valgus deformity had different risk on residual deformity 2 .
Morphological varieties in valgus knees consist of bone loss or hypoplasia from the lateral femoral condyle or the lateral tibial plateau, with or without valgus angulations at metaphyseal level, and concurrent soft‐tissue imbalance, including tight lateral structures, an attenuated medial collateral ligament, or both. Accordingly, different surgical techniques should be used for different sets of specific pathological changes 3 , 4 , 5 , 6 , 7 . Severe extra‐articular deformities could be corrected easily by wedged osteotomies but it is usually difficult to correct during TKAs. Even when corrected thoroughly by navigation‐guided cutting, an extra‐articular deformity could lead to severe soft tissue imbalance and thus constrained prosthesis might be necessary in TKAs. Different soft tissue balancing technique would be needed for different type of valgus knees. Medial and lateral collateral ligaments are the major stabilizers for soft tissue balance in coronal plane. Medial collateral ligament attenuation in some severe valgus knees usually necessitates constrained prosthesis or medial epicondylar advancement procedures. Lateral soft tissue contracture is more frequently seen in valgus knees than medial soft tissue attenuation. Different lateral releasing techniques had been recommended but lateral collateral ligament was seldom released. Lateral collateral ligament status plays an important role in lateral soft tissue contracture and determines the efficiency of lateral releasing. Categorizing the bony deformities of the femur and tibia will guide clinical decisions about deformity correction.
Some reports have revealed a difference in patterns of bony deformities and clinical results after TKA in valgus knees as compared with knees with neutral or varus alignment 8 , 9 , 10 . Eckstein et al. confirmed that the medial‐to‐lateral rate of femorotibial cartilage/bone loss depended on alignment, which contributed to the intra‐articular deformity 8 . Griffin et al. found posterior condylar deformity was associated with valgus alignment rather than varus or neutral alignment 10 . Some authors have reported various morphology of the distal femur in addition to different deformity origins in coronal plane 11 , 12 . Katz et al. reported various angulation deviations between the transepicondylar axis and the posterior condylar line in cadaver knees without evidence of degenerative arthritis 11 . Yoshioka et al. also reported large variations of the condylar twist angle in normal cadaver femur 12 . However, few studies have focused on radiological differences among subtypes of valgus knees. This information would be valuable to establish algorithms to aid choosing specific surgical procedures for valgus knees. So far, even though many classification systems of valgus knees are available, almost all of them are focused on the severity of valgus alignment and the status of medial collateral ligament 7 , 13 , 14 . There is still a lack of classification system to pinpoint bony deformity origins for valgus knees.
Radiological measurements and deformity analysis were performed on standing long‐film radiographs and computed tomography (CT). The purpose of study is to: (i) analyze bone deformity origins of valgus knees; (ii) propose a new radiological classification system for valgus knees; (iii) assess the reproducibility of this new classification system.
Methods
Patients
Approval for this study had been obtained from the institutional ethics committee.
One hundred and five consecutive valgus knees of 105 patients underwent TKAs performed by the senior surgeon's team from August 2007 to July 2013. During that period of time, CT scan was routinely taken for every TKA patients with valgus knees for preoperative deformity evaluation and three‐dimensional surgical planning, in addition to plain X‐rays and standard standing long‐film radiographs. The inclusion criteria for selecting the patients was set as knees operated between August 2007 and July 2013, with valgus deformity defined as a hip‐knee‐ankle angle (HKA, the angle between the mechanical axes of femur and tibia) >3° valgus on standing long‐film radiographs. The exclusion criteria were: knees without CT data available; or knees with flexion contracture >20°, which might significantly impede the measurement on long‐film radiographs.
Radiographic Evaluation
A standardized operating procedure was followed when taking long‐film radiographs with the patients in full standing position. The limb rotation was controlled by placing the patella pointing anteriorly and regularly re‐checked by a senior technician. Axial CT scans were performed with 0.5‐ to 0.8‐mm slice intervals.
Measurement and Classification
A malalignment test (MAT) was performed on long‐film radiographs using the method described by Paley and Tetsworth 15 . The HKA, the anatomical lateral distal femoral angle (aLDFA), and the anatomical medial proximal tibial angle (aMPTA) were measured on long‐film radiographs (Fig. 1) 15 . A deformity more than 3° was defined as an apparent deformity. The whole valgus deformity of the knee (recorded as S) was equal to the measured HKA minus 3°, which might come from the femoral side, the tibial side, or both sides.
Fig 1.

In the malalignment test (MAT), the hip‐knee‐ankle angle (HKA), the anatomical lateral distal femoral angle (aLDFA), and the anatomical medial proximal tibial angle (aMPTA) were measured.
The total valgus deformity from the femoral side (recorded as Sf) was defined as 81° minus the aLDFA, which might come from the supracondylar area or the femoral condyle, or both. To further differentiate between intra‐articular and extra‐articular valgus deformity from the femoral side, the distal condylar angle (DCA) and posterior condylar angle (PCA) were measured (Fig. 2). Measurement was performed on CT with Mimics software (version 13.0; Materialize, Leuven, Belgium), and re‐slice process was used to relocate the images to a standard view. DCA was the angle between the surgical transepicondylar axis and the distal femoral joint line, while PCA was the angle between the surgical transepicondylar axis and the posterior femoral joint line. A normal DCA was defined as 4°, and a normal PCA as 3° 12 , 16 , 17 . Intra‐articular valgus deformity from femoral side (recorded as Sif) was defined as the measured DCA subtracting 4°, while extra‐articular valgus deformity from femoral side (recorded as Sef) was defined as the Sf minus the Sif. A deviated PCA indicated intra‐articular deformity in knee flexion (in axial plane) from the femoral side, and an increased PCA (PCA > 3°) hinted dysplasia or defect of posterior lateral femoral condyle.
Fig 2.

The tibial bone varus angle (TBVA) (A) was measured on long‐film radiographs. TBVA was the angle between the axis of the tibia and the axis of the epiphysis. The axis of the tibia was from the middle of the proximal tibial joint line to the middle of the ankle. The axis of the epiphysis in adults was a line passing the middle of the proximal tibial joint line and the middle of the fused growth plate. The distal condylar angle (DCA) (B) and the posterior condylar angle (PCA) (C) were measured on CT scans. DCA was the angle between the distal femoral joint line and the transepicondylar axis. PCA was the angle between the posterior femoral joint line and the transepicondylar axis.
In our measurement, if the surgical transepicondylar axis of the distal femur was not identifiable, the clinical transepicondylar axis was used instead; in this situation, the condylar twist angle (CTA) was converted into the PCA for uniform analysis. The difference between the PCA and CTA has been reported to be 3.2° to 3.4°, so the difference between the PCA and the CTA in this study was defined as 3.3° 17 , 18 .
The total valgus deformity from the tibial side (recorded as St) was defined as 87° minus the measured aMPTA. The tibial bone varus angle (TBVA) was measured to further differentiate between intra‐articular and extra‐articular deformitites (Fig. 2). On average, the TBVA in well‐aligned knees was previously reported to be 2.8° varus (SD, 2.7°) 19 . Extra‐articular valgus deformity of the tibia (recorded as Set) was defined as 2.8° minus the measured TBVA. Therefore, intra‐articular valgus deformity (recorded as Sit) of the proximal tibia was then equal to St minus Set.
After distinguishing intra‐ vs extra‐articular deformities for both the femur and the tibia, the prevalence and severity of valgus deformity was calculated for each part of the knee. In the frontal plane, deformity could originate from four distinct segments—extra‐articular femoral (Sef), intra‐articular femoral (Sif), intra‐articular tibial (Sit), and extra‐articular tibial segment (Set)—that could be isolated or combined. A deformity >3° was defined to be apparent deformity in this study, as a deformity <3° might be not clinically relevant. If apparent deformities originated from two or more segments, the contribution percentage of each one (dividing into S) was calculated, and the one contributing the most was taken as the most severe deformity (severest in S).
Assessment of the Reproducibility
To examine the inter‐observer reproducibility of this classification system, two observers measured the deformities and did the classification for all the 105 knees independently. The intraclass correlation coefficient (ICC) was calculated. For those cases with disagreement from the two observers, a senior doctor was assigned to bring an agreement on the classification. The final prevalence of each subtype we reported in this study was calculated after an agreement was achieved for every knee. To examine the intra‐observer reproducibility of the system, one of the two observers was assigned to re‐measure and re‐classify all the 105 knees after blinded processing of the basic information on radiographs and waiting for an interval time of more than 2 weeks for every case. The ICC was also calculated to evaluate the intra‐observer reproducibility. An ICC > 0.75 was considered to be with good consistency.
Results
Measurement
The average age was 62.4 ± 8.6 years (range, from 41 to 84 years). Thirteen were male and 92 were female. The average HKA of 105 knees was 12.7 ± 6.2° (range, from 4.2° to 30.8°). Apparent deformities (>3°) and the most severe deformities (contributing the most in whole‐knee deformity) commonly originated from tibial plateau and the supracondylar portion of the femur (Table 1). Forty‐eight knees (45.7%) had apparent deformity from the tibial plateau, and 62 knees (59.0%) had apparent deformity from the supracondylar region of the femur. Intra‐articular deformity of the distal femur had different sub‐subgroups according to different combinations of DCA and PCA (Table 2). Ninety‐one knees (86.7%) had DCA >4°, of which 56 knees had PCA >3° simultaneously; and 18 knees (17.1%) had DCA > 7°, among which 11 knees had PCA >3° simultaneously.
TABLE 1.
Prevalence of deformity in the frontal plane from different segments around the knee
| Segment in the front plane | >0° | >3° | Severest in S |
|---|---|---|---|
| Sef | 86 (81.9%) † | 62 (59.0%) | 42 (40.0%) |
| Sif | 91 (86.7%) | 18 (17.1%) | 16 (15.2%) |
| Sit | 95 (90.5%) | 48 (45.7%) | 30 (28.6%) |
| Set | 54 (51.4%) | 18 (17.1%) | 17 (16.2%) |
S, the whole valgus deformity of the knee; Sef, valgus deformity from the extra‐articular portion of the femur; Sif, valgus deformity from the intra‐articular portion of the femur; Sit, valgus deformity from the intra‐articular part of the tibia; Set, valgus deformity from extra‐articular part of tibia.
Severest in S means the cases in which deformity of the correspondent segment contributes the most to the whole valgus deformity of the knee.
Number of knees (percentage in 105).
TABLE 2.
Sub‐subtypes of intra‐articular deformity of the distal femur
| Sub‐subtypes | >0° | >3° | Severest in S |
|---|---|---|---|
| Increased DCA + Normal PCA | 35 | 7 † | 6 |
| Increased DCA + Increased PCA | 56 | 11 (3) ‡ | 10 |
| Normal DCA + Increased PCA | 0 | 0 | 0 |
| Normal DCA + Normal PCA | 14 § | ‐ | ‐ |
DCA, distal condylar angle; PCA, posterior condylar angle.
S, the whole valgus deformity of the knee.
DCA >7° and PCA ≤3°.
DCA >7° and PCA >3° (DCA >7° and PCA >6°).
No intra‐articular deformity of the distal femur.
Classification
All the 105 knees were first sorted to four subgroups according to four distinct patterns of origin of their most severe deformity in frontal plane (Sef, Sif, Sit, and Set). Further, the subgroup with the intra‐articular femoral deformity could be divided into two sub‐subgroups according to the status of posterior aspect of the lateral femoral condyle: normal posterior femoral offset (increased DCA + normal PCA) vs decreased posterior femoral offset (increased DCA + increased PCA). No instances of an apparently increased PCA (increase of >3°) were found coexisting with a normal DCA.
Valgus deformities could be classified into five subtypes according to the deformity origin on radiological analysis—the supracondylar region of the femur (F2), the distal lateral femoral condyle (F1a), both distal and posterior lateral femoral condyle (F1b), the tibial plateau (T1), or the metaphyseal segment of the tibia (T2) (Table 3) (Fig. 3). Each valgus knee could be labeled with a single subtype or a combination of them.
TABLE 3.
Classification system and terminology for five subtypes of valgus knees
| Subtypes | Descriptions |
|---|---|
| Femoral deformity | |
| F1a |
Intra‐articular deformity (in the distal aspect of the lateral condyle) The LCL is relatively loose when the knee extends, with normal tension when the knee flexes. |
| F1b |
Intra‐articular deformity (in the distal and posterior aspects of the lateral condyle) LCL is tight through all the range of motion. |
| F2 |
Extra‐articular deformity (in the supracondylar portion) LCL remains at normal length and tension through the entire range of motion † . |
| Tibial deformity | |
| T1 |
Intra‐articular deformity (in lateral tibial plateau) LCL is tight through all the range of motion. |
| T2 |
Extra‐articular deformity (in metaphysic part) LCL remains at normal length and tension through the entire range of motion. |
LCL, lateral collateral ligament.
For ease of use, the terminology of F1b and F2 had been modified from the primitive version firstly raised in 2010.
Speculation regarding LCL status in type F1b or T2 is made on the condition that little or minimal deformities of other patterns exist.
Fig 3.

Case examples: (A) a subtype F1a valgus knee has an increased aLDFA (76.1°), an increased DCA (7.5°), and a normal PCA (3.0°); (B) a subtype F1b valgus knee has an increased aLDFA (77.0°), an increased DCA (8.0°), and an increased PCA (6.5°); (C) a subtype F2 has an increased aLDFA (72.6°), a normal DCA (4.8°), and a normal PCA (3.6°); (D) a subtype T1 has an increased aMPTA (92.0°) and a normal TBVA (2.8°); (E) a subtype T2 has an increased aMPTA (96.9°) and a negtive/decreased TBVA (−3.3°).
According to the current classification system, F2 and T1 (40.0% and 28.6%, respectively) were the most common two subtypes of valgus deformities (Table 4). On the femoral side, extra‐articular deformity (F2) was more common than intra‐articular femoral deformity (F1a and F1b) (40.0% vs 15.2%). Intra‐articular tibial deformity (T1) was much more common than extra‐articular deformity (T2) (28.6% vs 16.2%). Of all the 105 valgus knees, 56.2% had extra‐articular deformities (F2, T2) as the severest deformity.
TABLE 4.
Prevalence of each subtype and descriptions of the distinguished manifestations of deformity (n = 105)
| Subtypes * | N (%) | DCA/° | PCA/° | Sef/° | Sit/° | Set/° |
|---|---|---|---|---|---|---|
| Femoral deformity | ||||||
| F1a | 6 (5.7) | 6.5 ± 0.6 | 2.6 ± 0.5 | 0.4 ± 1.0 | 0.8 ± 1.0 | 0.3 ± 0.8 |
| F1b | 10 (9.5) | 7.8 ± 1.3 | 6.1 ± 1.9 | 0.5 ± 2.1 | 1.3 ± 1.1 | 0.5 ± 0.8 |
| F2 | 42 (40.0) | 6.3 ± 2.5 | 3.9 ± 1.7 | 7.6 ± 4.8 | 2.1 ± 3.2 | 0.2 ± 2.2 |
| Tibial deformity | ||||||
| T1 | 30 (28.6) | 5.8 ± 1.3 | 4.6 ± 1.7 | 2.8 ± 2.6 | 6.4 ± 2.2 | −1.2 ± 1.6 |
| T2 | 17 (16.2) | 5.2 ± 1.1 | 3.4 ± 1.3 | 2.1 ± 2.3 | 1.3 ± 1.4 | 6.3 ± 2.7 |
| ANOVA test | ||||||
| P | 0.007 | 0.000 | 0.000 | 0.000 | 0.000 | |
DCA, distal condylar angle; PCA, posterior condylar angle.
Manifestation of deformity was shown as mean ± standard deviation. Positive value indicated valgus deformity and negative value is for varus deformity. Value with underline hinted the most significant manifestation of that subtype.
If two or more subtypes of deformity co‐existed in the same knee, the most severe one was counted in.
There were 49 knees (46.7%) with apparent deformities (>3°) originating from two or three parts around the knee. The most common combination was F2 + T1, which occurred in 24 knees.
Intra‐observer and Inter‐observer Reproducibility
The intra‐observer ICC of this classification system was 0.992 (95% CI, 0.989–0.995), and inter‐observer ICC was 0.976 (95% CI, 0.965–0.984).
Discussion
Among patients undergoing TKA, 10% to 17% have valgus knees 20 . Valgus knees could have worse clinical outcomes than well‐aligned knees or even varus knees 15 . Thorough knowledge of the pathological changes in bone and soft tissue is critical for surgeons to pursue good outcomes. Bone deformities originating from different segments usually need different correction strategies and different soft tissue balancing accordingly 1 , 3 , 7 , 21 , 22 . Pinpointing the origins of deformity and understanding morphological features of valgus knees helps to personalize a valgus knee, predict the soft tissue conditions, and thus, determines the deformity correction and soft tissue balancing strategies and techniques in TKAs.
According to deformity origins and morphological features, valgus deformities were classified into five subtypes. This classification system has high level of reproducibility if preformed on the same radiographic images. It is a reliable tool for surgeons to label and sort valgus knees both in diagnosis and surgical planning. This classification helps personalize valgus knees in terms of deformity origins, and based on that, the status of the lateral collateral ligament (LCL) and lateral joint capsule can be sequentially predicted (Fig. 4). Several other classification systems could help to sort valgus knees based on the severity of angular deformity or medial collateral ligament status, but they cannot give detailed descriptions about the bone deformity location or anticipations of lateral soft‐tissue status 7 , 21 , 22 . Furthermore, medial collateral ligament deficiency only exists in about 17%–20% of all the valgus knees, which could strongly indicate utility of constrained prosthesis in TKA but only represent the minority in practice. Our classification system is able to further personalize about 80%–83% of the valgus knees, which would play a dominant role in guiding soft tissue balancing 2 , 7 .
Fig 4.
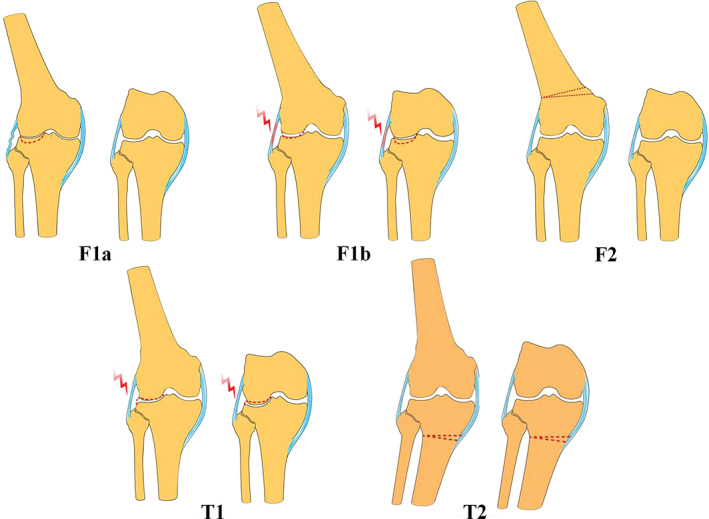
An overview of a new classification system for valgus knees defining five distinct subtypes of bone deformity origins (dotted line). F1a had bone defect in the distal aspect of the lateral condyle; F1b had bone defect in both the distal and posterior aspects of the lateral condyle; F2 had extra‐articular valgus deformity in the supracondylar portion; T1 had bone defect in lateral tibial plateau; T2 had extra‐articular valgus deformity in metaphysic part of the tibia. The status of the LCL can be reasonably predicted in each subtype both when the knee extends and flexes. The LCL contracts (lightning in red) in subtypes F1b and T1 but not in subtypes F1a, F2, and T2.
Supra‐condylar valgus deformity (F2) is the most common origin of valgus deformities. In TKA for a valgus knee with significant extra‐articular deformity, a simple bone cut perpendicular to mechanic axis would lead to severe soft tissue imbalance and unnecessary use of constrained prosthesis. The high incidence of extra‐articular deformity in valgus knees could probably be responsible for high incidence of residual valgus deformity and sub‐optimal clinical results after TKA 2 . One‐ or two‐stage corrective osteotomy is recommended for these subtypes of valgus knees. In some circumstances, surgeons could recruit an epicondylar sliding osteotomy to transform an extra‐articular deformity of the femur to a partially defected lateral femoral condyle with a balanced mediolateral gap.
Different subtypes of intra‐articular valgus deformities were also found from the femoral side. Dysplasia or defect of distal lateral femoral condyle leads to intra‐articular valgus deformity. However, the posterior offset of lateral femoral condyle may or may not be reduced according to the condition of posterior aspect of lateral femoral condyle (F1b or F1a). Differentiating the condition of posterior lateral condyle is clinically relevant. A well‐preserved posterior offset prevents LCL and postero‐lateral joint capsule from contraction. In contrast, a decreased posterior offset hints a potential tight LCL and contracted lateral joint capsule. Further, taking posterior condylar axis as the reference for femoral component rotation will be inaccurate and lead to malrotation (internal rotated) of the femoral component, which would compromise the patella tracking. These subtypes are also associated with different clinical signs of valgus knees. Provided the deformity comes only from femoral side, it presents no matter if the knee extends or flexes when posterior femoral condyle is compromised whereas it only presents when the knee extends if posterior femoral condyle is well‐maintained. A swing test has been developed to detect deformity in flexion clinically 23 . Prior to a CT scan, swing test would aid in revealing a decreased posterior offset of lateral femoral condyle.
In an F1a deformity, the LCL length would be well‐maintained, because the LCL could remain at normal tension and length in knee flexion due to a normal height of posterior aspect of lateral condyle. In an F1b deformity, the offset is consistently decreased no matter when the knee extends or flexes, indicating that contracture of the posterior lateral soft tissues (especially LCL) may bring difficulties in gap balancing. For the F2 subtype, the deformity is located superior to the collateral ligament frame, so the posterior lateral soft tissues would be well‐preserved. For the T1 subtype, there is bone defect on lateral plateau, and the posterior lateral soft tissues should be in contracture similar with the F1b type. And for a T2 deformity, posterior lateral soft tissues would be normal such as in F2. If apparent deformities originate from two or three segments simultaneously around the knee, it will increase the complexity of deformity correction and soft‐tissue balancing. For these knees, a combination or integration of surgical solutions would be needed to correct the bone deformity for such kind of valgus knee. This classification system based on deformity origin helps not only individualize bone defect location and soft tissue status, but also indicate different morphology of the cutting surface and aspect ratios of resected distal femurs 24 .
There are some limitations in this study and the new classification system. First, being a radiographic analysis based on X‐ray and CT, our study only revealed different patterns of bone deformities and allows only for speculation about soft tissue status. Thus, further intra‐operative gap and tense measurement is needed to confirm the soft tissue variations in different subtypes. Second, our study was based on CT scanning, which has limitations in detecting cartilage defects that can also contribute to intra‐articular deformities. Third, the bony landmarks such as epicondylar axis and the normal alignment we used in this study are not in agreement with a few other studies 25 , 26 , 27 . Those authors suggested other definitions of distal femoral rotation axis and normal alignment of the knee, which would affect our principles in knee reconstruction and prosthesis design, but no matter what measurement reference we used, the fact of different patterns of bone deformities and reasonable speculations on soft tissue status will still play an important role to label different valgus knees and guide our surgical techniques. And what is more, this is just a descriptive presentation of the morphological features of different valgus knees, but the effectiveness of this classification system in anticipation of clinical outcome still needs to be proved.
In conclusion, there are five subtypes of valgus deformities according to a new radiological classification system of valgus knees. This classification system has high reproducibility and helps to pinpoint deformity origins, display morphological features of the knee, and thus personalize a valgus knee and guide clinical treatments.
Authorship Declaration
We declare that all authors listed meet the authorship criteria, and all authors are in agreement with the manuscript.
Acknowledgments
This study was supported by the Beijing Talents Fund (No. 2017000021469G229) and Beijing Jishuitan Hospital Nova Program (No. XKXX201803).
Disclosure: We have no conflict of interest to declare.
References
- 1. Karachalios T, Sarangi PP, Newman JH. Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg Br, 1994, 76: 938–942. [PubMed] [Google Scholar]
- 2. Yang DJ, Wang ZL, Bian T, Zhou BC, Zhou YX. Distribution and risk factors of residual deformities after total knee arthroplasty for valgus knee. Chin J Bone Joint Surg, 2020, 13: 579–584. [Google Scholar]
- 3. Aglietti P, Lup D, Cuomo P, Baldini A, De Luca L. Total knee arthroplasty using a pie‐crusting technique for valgus deformity. Clin Orthop Relat Res, 2007, 464: 73–77. [DOI] [PubMed] [Google Scholar]
- 4. Hadjicostas PT, Soucacos PN, Thielemann FW. Computer‐assisted osteotomy of the lateral femoral condyle with non‐constrained total knee replacement in severe valgus knees. J Bone Joint Surg Br, 2008, 90: 1441–1445. [DOI] [PubMed] [Google Scholar]
- 5. Healy WL, Iorio R, Lemos DW. Medial reconstruction during total knee arthroplasty for severe valgus deformity. Clin Orthop Relat Res, 1998, 356: 161–169. [DOI] [PubMed] [Google Scholar]
- 6. Puddu G, Cipolla M, Cerullo G, Franco V, Gianni E. Which osteotomy for a valgus knee? Int Orthop, 2010, 34: 239–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am, 2005, 87: 271–284. [DOI] [PubMed] [Google Scholar]
- 8. Eckstein F, Wirth W, Hudelmaier M, et al. Patterns of femorotibial cartilage loss in knees with neutral, varus, and valgus alignment. Arthritis Rheum, 2008, 59: 1563–1570. [DOI] [PubMed] [Google Scholar]
- 9. Faris PM, Herbst SA, Ritter MA, Keating EM. The effect of preoperative knee deformity on the initial results of cruciate‐retaining total knee arthroplasty. J Arthroplasty, 1992, 7: 527–530. [DOI] [PubMed] [Google Scholar]
- 10. Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees. J Arthroplasty, 1998, 13: 812–815. [DOI] [PubMed] [Google Scholar]
- 11. Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res, 1993, 286: 40–47. [PubMed] [Google Scholar]
- 12. Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am, 1987, 69: 873–880. [PubMed] [Google Scholar]
- 13. Krackow KA, Jones MM, Teeny SM, Hungerford DS. Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop Relat Res, 1991, 273: 9–18. [PubMed] [Google Scholar]
- 14. Williot A, Rosset P, Favard L, Brilhault J, Burdin P. Total knee arthroplasty in valgus knee. Orthop Traumatol Surg Res, 2010, 965: s37–s42. [DOI] [PubMed] [Google Scholar]
- 15. Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res, 1992, 280: 65–71. [PubMed] [Google Scholar]
- 16. Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res, 1993, 290: 259–268. [PubMed] [Google Scholar]
- 17. Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty, 2001, 16: 493–497. [DOI] [PubMed] [Google Scholar]
- 18. Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T. Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res, 2001, 388: 147–156. [DOI] [PubMed] [Google Scholar]
- 19. Bonnin M, Chambat P. Current status of valgus angle, tibial head closing wedge osteotomy in media gonarthrosis. Orthopade, 2004, 33: 135–142. [DOI] [PubMed] [Google Scholar]
- 20. Aglietti P, Baldini A, Buzzi R, Lup D, De Luca L. Comparison of mobile‐bearing and fixed‐bearing total knee arthroplasty: a prospective randomized study. J Arthroplasty, 2005, 20: 145–153. [DOI] [PubMed] [Google Scholar]
- 21. Politi J, Scott R. Balancing severe valgus deformity in total knee arthroplasty using a lateral cruciform retinacular release. J Arthroplasty, 2004, 19: 553–557. [DOI] [PubMed] [Google Scholar]
- 22. Whiteside LA. Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res, 1999, 367: 130–140. [PubMed] [Google Scholar]
- 23. Zhou YX, Yang DJ, Shao HY. A new physical examination technique for evaluating valgus knee deformity: swing test. Chin Med J (Engl), 2016, 129: 3004–3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yin XH, Yang DJ, Zhou YX, Shao HY, Huang Y, Huang XJ. Different femoral origins of valgus deformity affect aspect ratios of resected distal femurs in total knee arthroplasty. Knee, 2019, 26: 1073–1079. [DOI] [PubMed] [Google Scholar]
- 25. Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res, 2007, 461: 238–244. [DOI] [PubMed] [Google Scholar]
- 26. Eckhoff DG, Bach JM, Spitzer VM, et al. Three‐dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am, 2005, 87: 71–80. [DOI] [PubMed] [Google Scholar]
- 27. Howell SM, Howell SJ, Hull ML. Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Joint Surg Am, 2010, 92: 98–104. [DOI] [PubMed] [Google Scholar]


