Abstract
Introduction:
Discrimination is associated with negative health outcomes among Latinos. Research on the link between discrimination and inflammation in adults has focused on pro-inflammatory markers rather than characterizing the more informative balance of pro- and anti-inflammatory markers. The purpose of this cross-sectional study was to examine the associations of everyday discrimination with inflammation ratio (defined as the ratio of pro- to anti-inflammatory cytokines) in a sample of middle-aged and older Latinas.
Methods:
Latinas were recruited from an existing study in New York City. Participants reported frequency and count of everyday discrimination. Peripheral blood was used to analyze pro- (IL-1B and IL-6) and anti-inflammatory (IL-4 and IL-10) cytokines. The inflammation ratio was calculated by dividing the sum of pro-inflammatory cytokines by the sum of anti-inflammatory cytokines. We used linear regression to assess the link between everyday discrimination and inflammation ratio.
Results:
The final sample included 40 Latinas (mean age = 63.2 years). Approximately 68% had household incomes less than $15,000. More than half (53%) reported experiencing some form of everyday discrimination. Regression models showed everyday discrimination was not associated with individual pro- and anti-inflammatory cytokines. In adjusted regression models, the frequency of everyday discrimination was not associated with inflammation ratios (B[SE] = 0.57[0.30], p = .07). However, a higher count of everyday discrimination was associated with inflammation ratios (B[SE] = 1.15[0.55], p = .04).
Conclusions:
The count of everyday discrimination was positively associated with inflammation in Latina women. Future studies should replicate these findings using longitudinal assessment of discrimination and inflammatory markers.
Keywords: discrimination, inflammation, Latino health, cardiovascular health
In 2019, approximately 60% of Latinos in the United States (U.S.) reported experiencing discrimination, such as being treated unfairly, due to their race or ethnicity (Pew Research Center, 2019). Previous work suggests Latino men report a higher prevalence of discrimination than Latina women. For instance, a cross-sectional study of young Latino men and women found that 60.2% of Latino men and 41.2% of Latina women reported experiencing everyday discrimination (chronic, but often minor experiences of unfair treatment that commonly occur in day-to-day interpersonal interactions; Otiniano Verissimo et al., 2013). In addition, in a sample of 150 pregnant Latina women (mean age = 27.6 years), investigators found approximately 44% of participants reported experiencing some form of everyday discrimination in their lifetimes (Santos et al., 2018). A recent systematic review of 33 studies found that perceived discrimination is consistently associated with a higher prevalence of depressive symptoms and substance use among Latinos across studies (Andrade et al., 2020). However, research investigating the associations of discrimination with physical health conditions, such as hypertension and diabetes, in Latinos is limited and mixed (Andrade et al., 2020).
Inflammation has been hypothesized as a potential physiologic pathway that links discrimination with negative physical health outcomes among racial and ethnic minority adults (Simons et al., 2018). In particular, nationally representative data indicate Latinas have a higher prevalence of pro-inflammatory conditions (such as diabetes and hyperlipidemia) than non-Latina White women (Carroll et al., 2017; Mendola et al., 2018). Latinas also have higher levels of C-reactive protein, a marker of chronic inflammation, relative to their non-Latina White peers (Beatty et al., 2014). These factors may place Latinas at greater risk for chronic conditions across the lifespan.
Health disparities among Latinas may be driven, at least in part, by exposure to discrimination. Analyses of population-based data, using different measures of discrimination, have found that report of discrimination is associated with higher levels of inflammatory markers, such as interleukin-6 (IL-6), among adults (Kershaw et al., 2016; Stepanikova et al., 2017). However, data are inconclusive and there has been limited examination of these associations among Latinas. In a multi-ethnic sample of adults, investigators found that everyday discrimination was associated with elevated IL-6 in women, especially non-Latina Black women (Kershaw et al., 2016). Analyses of data from the Health and Retirement Study found that greater report of lifetime discrimination (which includes major discriminatory events such as employment, healthcare, and education discrimination) was associated with elevated IL-6 in non-Latino White adults, but not non-Latino Black adults (Stepanikova et al., 2017). Neither of those studies reported findings for Latino adults.
Cytokines, proteins released from monocytes and macrophages that include interleukins, play an important role in regulating the immune and inflammatory response (Dinarello, 2018). The immune-inflammatory response is notably complex and relies on coordinated feedback loops between both pro- and anti-inflammatory cytokines. Interestingly, exposure to stress differentially impacts release of pro- and anti-inflammatory cytokines depending on the nature of the stressor. Acute stress has been shown to activate pro-inflammatory cytokines, such as IL-1 beta (IL-1B) and IL-6 (Dhabhar, 2014). Anti-inflammatory cytokines, such as IL-4 and IL-10, may inhibit inflammatory response through decreased production of pro-inflammatory cytokines (Sundermann et al., 2019). There is growing evidence that a higher pro- to anti-inflammation ratio is associated with chronic health conditions, such as chronic lung disease and polycystic ovary syndrome (Silva et al., 2018; Tosatti et al., 2020). The ratio of pro- to anti-inflammatory cytokines provides a more informative measure of inflammation than a single cytokine (Morrisette-Thomas et al., 2014) and was, therefore, used in this study to provide a more holistic approach to the examination of inflammation in relation to discrimination.
To date, few studies have assessed if greater exposure to discrimination is associated with higher inflammation ratios in racial and ethnic minority adults. Longitudinal analyses of the Family and Community Health Study found that exposure to racial discrimination in adolescence predicted inflammation in adulthood and modulated the inflammatory effects of adult racial discrimination among non-Latino Black adults (Simons et al., 2018). Although Latinas have a higher risk for chronic diseases, such as cardiovascular disease, research on the link between discrimination and inflammation in Latinas is limited (Beatty et al., 2014; Carroll et al., 2017; Hales et al., 2020). Thus, the purpose of the present study was to investigate the associations of everyday discrimination with inflammation in a community sample of middle-aged and older Latinas. We hypothesized a higher frequency and count of everyday discrimination would be associated with a greater pro- to anti-inflammatory ratio.
Method
Sample
The present paper presents findings from a sub-analysis of an existing pilot study in New York City. The original objective of the pilot study was to examine social determinants (such as discrimination and interpersonal violence) of cardiovascular health in middle-aged and older Latina women. Participants for the pilot study were recruited from an existing study called the Washington Heights/Inwood Comparative Effectiveness Research Project (WICER; N > 6,000). The purpose of the WICER study was to improve the health of the primarily Latino immigrants that reside in the Washington Heights/Inwood neighborhoods of Northern Manhattan. Recruitment and data collection methods of the WICER study have been previously described (Lee et al., 2014).
We recruited female participants from the WICER study. We included all women who were (1) ≥ 40 years, (2) English and/or Spanish speaking, and (3) able to provide informed consent. A 6-item cognitive screener, used to determine capacity to provide informed consent, was completed by potential participants via telephone (Callahan et al., 2002). We excluded women with a history of cognitive impairment and those with a history of cardiovascular disease (including myocardial infarction, stroke, and coronary artery disease). The present paper reports on findings from our sub-analysis that investigated the associations of everyday discrimination with inflammation in a community sample of middle-aged and older Latinas.
Procedures
All procedures in the present study were approved by the Institutional Review Board at the Columbia University Irving Medical Center. Study procedures included a structured questionnaire, measurement of anthropometrics and blood pressure, and venipuncture. All procedures were completed in a private room at the Columbia University School of Nursing by trained research staff. Participants completed a structured questionnaire to assess demographic and clinical factors, health behaviors, and everyday discrimination. Upon completing the structured questionnaire research staff escorted participants to the Clinical Research Resource at CUIMC for venipuncture to obtain peripheral blood samples to measure pro- and anti-inflammatory cytokines.
Measures
Everyday discrimination
We used the Everyday Discrimination Scale to assess everyday discrimination (Williams et al., 1997). Everyday discrimination includes chronic but often minor experiences of unfair treatment that commonly occur in day-to-day interpersonal interactions. Participants were asked to rate the frequency at which they experienced 10 forms of unfair treatment due to being Latina using a 4-point scale (1 = never; 4 = often). Before listing the 10 items participants were asked: “In your day-to-day life, how often have any of the following things happened to you?” Example items include: “You are threatened or harassed,” “People act as if they are afraid of you,” “You are treated with less respect than other people,” and “You receive poorer service than other people at restaurants or stores.” Responses were summed with higher scores indicating greater frequency of everyday discrimination (possible range 10-40). Cronbach’s α was 0.84. We also created a count measure of everyday discrimination that assessed the count of different types of discrimination reported by participants (possible range 0-10).
Inflammation ratio
Peripheral blood samples were collected via venipuncture and stored in aliquots at −80°C. Serum levels of cytokines were analyzed using commercially available high sensitivity Enzyme-Linked Immunoassay (ELISA) kits (RD systems, Minneapolis, MN). Based on previously described methods, we assessed the balance of pro- to anti-inflammatory activity by dividing the sum of the pro-inflammatory cytokines (IL-1B + IL-6) by the sum of the anti-inflammatory cytokines (IL-4 + IL-10; Simons et al., 2018). A higher ratio indicates a greater pro-inflammatory state. Figure 1 shows the pro- and anti-inflammatory cytokines included in the present study.
Figure 1.
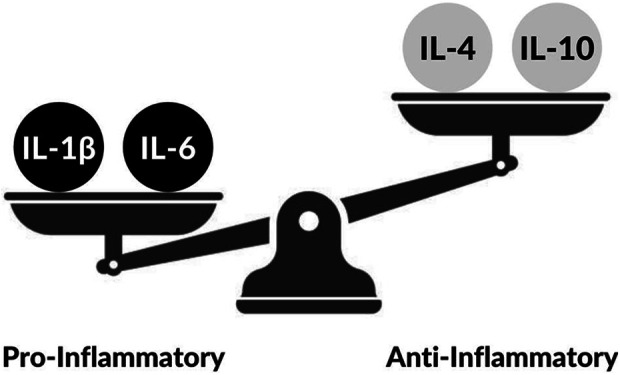
Pro-and anti-inflammatory cytokines.
Demographic and clinical factors
Demographic factors assessed were age (continuous) and annual household income. Clinical factors assessed were post-menopausal status (yes vs. no) and regular use of non-steroidal anti-inflammatory drugs (NSAID; such as aspirin, naproxen, ibuprofen, and motrin).
Cardiovascular health
We used the American Heart Association’s ideal cardiovascular health index, which includes three health-promoting behaviors and four health factors, to assess cardiovascular health (Lloyd-Jones et al., 2010). This measure has been associated with increased risk for inflammation among adults in analyses of population-based data (Mazidi et al., 2019). Self-report of usual moderate and vigorous recreational physical activities was assessed. Healthy diet scores included self-reported intake of fruits and vegetables, fish, fiber-rich whole grains, and sugar-sweetened beverages (Boylan & Robert, 2017). Tobacco use was assessed based on self-report of current or former cigarette smoking. Body mass index (kg/m2) was calculated using objectively measured height and weight. Total cholesterol and HbA1c were measured from serum obtained via venipuncture. We calculated the average of two blood pressure readings. For each component of the ideal cardiovascular health metric, participants were assigned a score of 2 for meeting ideal criteria, 1 for intermediate, and 0 for poor based on previously described methods (Lloyd-Jones et al., 2010). Scores were summed to create a measure of cardiovascular health with a range of 0–14. Higher scores indicate better cardiovascular health.
Statistical Analyses
Analyses were conducted in Stata version 16. We assessed frequencies, means, and distributions of study variables to characterize the sample. We used linear regression models to examine the associations of everyday discrimination with individual inflammatory markers and the inflammation ratio. Separate models were run with the frequency and count of everyday discrimination as the main exposure. Inflammation ratio was the outcome in both analyses. Model 1 was unadjusted. Model 2 was adjusted for the following covariates (selected a priori): age, annual household income, menopausal status, regular NSAID use, and cardiovascular health score. A p-value of less than .05 was used for all analyses.
Results
The sample included 40 Latinas. Sample characteristics are presented in Table 1. Approximately 85% of women were born in the Dominican Republic. The mean age was 63.2 ± 8.9 years (range 46–77). More than 65% of women had household incomes less than $15,000. The majority of women were post-menopausal (95%). The mean frequency of everyday discrimination score was 12.8 ± 4.2 (range = 10-31). The mean count of everyday discrimination was 2.0 ± 2.3 (range 0-7). Approximately 53% of women reported experiencing at least one type of everyday discrimination. The mean cardiovascular health score was 6.5 ± 1.6 (range of 4–11). Values for individual cytokines and the inflammation ratio are also shown in Table 1.
Table 1.
Sample Characteristics.
| Age in years (range 46–77; Mean[SD]) | 63.2 (8.9) |
|---|---|
| Annual household income (N[%]) | |
| Under $15,000 | 27 (67.5) |
| $15,000–$24,999 | 7 (17.5) |
| $25,000–$34,999 | 5 (12.5) |
| Over $35,000 | 1 (2.5) |
| Post-menopausal (N[%]) | 38 (95.0) |
| Regular NSAID use (N[%]) | 21 (52.5) |
| Frequency of everyday discrimination (range 10–31; Mean [SD]) | 12.8 (4.2) |
| Count of everyday discrimination (range 0–7; Mean [SD]) | 2.0 (2.3) |
| Cardiovascular health scores (range 4–11; Mean [SD]) | 6.5 (1.6) |
| IL-1B (range 0.01–0.41 pg/mL; Mean [SD]) | 0.13 (0.12) |
| IL-4 (range 0.02–0.80 pg/mL; Mean [SD]) | 0.14 (0.13) |
| IL-6 (range 0.54–7.89 pg/mL; Mean [SD]) | 2.82 (1.68) |
| IL-10 (range 0.03–1.99 pg/mL; Mean [SD]) | 0.35 (0.33) |
| Inflammation ratio (range 1.04–33.13 pg/mL; Mean [SD]) | 8.4 (7.5) |
Note. N = 40.
Table 2 presents results of multiple linear regression models examining the associations of everyday discrimination with inflammation ratio. Everyday discrimination was not associated with any of the individual cytokines assessed. Unadjusted analyses found frequency of everyday discrimination was positively associated with a higher inflammation ratio (B[SE] = 0.55[0.28], p = .05). This association was not significant after covariate adjustment (B[SE] = 0.57[0.30], p = .07). However, the count of everyday discrimination was significant in unadjusted (B[SE] = 1.01[0.50], p = .04) and adjusted (B[SE] = 1.15[0.55], p = .04) regression models.
Table 2.
Linear Regression Results Examining the Associations of Everyday Discrimination With Inflammation Ratio.
| Frequency of Everyday Discrimination | Count of Everyday Discrimination | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | Model 1 | p Value | Model 2 | p Value | Model 1 | p Value | Model 2 | p Value |
| B (95% CI) | B (95% CI) | B (95% CI) | B (95% CI) | |||||
| Frequency of everyday discrimination | 0.55 (−0.01, 1.12) | 0.55 | 0.57 (−0.06, 1.19) | 0.07 | – | – | – | – |
| Count of everyday discrimination | – | – | – | – | 1.01 (0.01, 2.03) | 0.05 | 1.15 (0.03, 2.27) | 0.04 |
| Age | – | – | −0.05 (−0.37, 0.25) | 0.70 | – | – | 0.05 (−0.36, 0.28) | 0.73 |
| Annual household income | – | – | 0.24 (−3.20, 3.68) | 0.89 | – | – | 0.26 (−3.13, 3.66) | 0.88 |
| Post-menopausal | – | – | −2.64 (−7.26, 1.97) | 0.25 | – | – | −3.28 (−7.92, 1.34) | 0.16 |
| Regular NSAID use | – | – | 1.31 (−3.74, 6.38) | 0.60 | – | – | 1.21 (03.74, 6.17) | 0.62 |
| Cardiovascular health score | – | – | 0.23 (−1.29, 1.76) | 0.76 | – | – | 0.19 (−1.31, 1.70) | 0.79 |
Note. N = 40. Model 1 was unadjusted; Model 2 was adjusted for age, annual household income, post-menopausal status, regular NSAID use, and cardiovascular health. p < .05
Discussion
This study is one of the first to examine inflammation ratio in relation to everyday discrimination in Latinas. In a low-income sample of middle-aged and older Latinas without a diagnosis of cardiovascular disease we found a higher count of everyday discrimination, but not a higher frequency of everyday discrimination, was associated with a higher inflammation ratio. Frequency and count of everyday discrimination were not associated with individual inflammatory cytokines. Our results are consistent with the work of Simons and colleagues (2018) who examined the longitudinal associations of discrimination and inflammation ratios in young non-Latino Black adults. However, their study included a greater number of cytokines and examined lifetime discrimination (as opposed to everyday discrimination).
Given the growing evidence that chronic inflammation is associated with adverse health outcomes (Silva et al., 2018; Tosatti et al., 2020), our finding of an elevated pro- inflammatory milieu in Latinas with a higher count of everyday discrimination suggests this may contribute to elevated risk for chronic health conditions in this population. As such, these findings also support the need for future research that investigates the link between everyday discrimination and inflammation ratios in Latinas. Although there has been limited research on the association of discrimination and inflammation in Latino women and men, previous work suggests greater exposure to psychosocial stress is associated with inflammation in Latinos. For instance, analyses of the population-based data indicate that among Latinos greater exposure to chronic psychological stress (such as financial concerns and health problems) is associated with elevated CRP levels (McCurley et al., 2015). Overall, these data indicate future research that assesses the influence of everyday discrimination and other psychosocial stressors on inflammation in Latinos is needed.
Approximately 53% of women in our study reported experiencing discrimination, which is consistent with national estimates of discrimination among Latinos (Pew Research Center, 2019). The prevalence of discrimination among Latinos may be influenced by a number of characteristics like skin tone and accented speech. For instance, Latinos with darker skin are more likely to report discrimination than lighter skin counterparts (64% vs. 50%; Pew Research Center, 2019). Our sample was small and included a homogenous group of Latinas of primarily Dominican descent (approximately 85%). There is a need to examine if the associations of everyday discrimination with inflammation in Latinas differ by other characteristics such as skin tone. This may help identify which groups of Latinas may be at greater risk for negative health outcomes related to everyday discrimination.
This study has important implications for clinical practice and policy. Nurses and other clinicians should recognize inflammation is a potential physiological pathway linking everyday discrimination with poor health outcomes in Latinas. The elevated inflammation ratios we observed in relation to a higher count of everyday discrimination may place Latinas at higher risk for the development of chronic diseases. Further, our findings indicate clinicians and public health practitioners should advocate for policies to reduce the negative impact of discrimination on the health of Latinas.
Limitations
This study has several limitations. Given this study was cross-sectional we cannot infer causation from these findings. Next, we had a small sample size and only assessed 4 cytokines as part of our inflammation ratio. In addition, our sample was relatively homogenous consisting primarily of low-income Dominican middle-aged and older women. This is important to consider as recent studies have found that younger Latina women report a lower prevalence of everyday discrimination (approximately 41%–44%) than what was observed in the middle-aged and older women included in the present study (Otiniano Verissimo et al., 2013; Santos et al., 2018). Not surprisingly, the majority of women in this study were post-menopausal. This is a limitation as previous evidence suggests declines in estrogen levels in post-menopausal women are associated with elevations in pro-inflammatory cytokines (such as IL-1B and IL-8; Huang et al., 2017; Malutan et al., 2014). These limitations highlight the need for future studies to replicate our analyses in larger, more diverse, and younger samples of Latinas and include other measures of discrimination (such as lifetime discrimination and internalized racism). In particular, longitudinal studies that include more comprehensive assessment of pro- and anti-inflammatory cytokines in Latina women of various ages are needed to confirm if the association between a higher count of everyday discrimination and inflammation we found is consistent across other samples of Latinas. Last, we only assessed interpersonal forms of discrimination. Additional research that examines the role of structural discrimination, such as residential segregation, on inflammation and health in Latinas is needed.
Conclusion
This cross-sectional pilot study contributes to the limited body of research that has investigated the associations of discrimination and inflammation in Latinas. We found no relationship between everyday discrimination and individual cytokines. However, a higher count of everyday discrimination was associated with a higher inflammation ratio indicating a greater pro-inflammatory state. Our data have important implications for future research investigating the link between discrimination and inflammation in Latinas. In particular, longitudinal studies that include larger samples of Latinas and more comprehensive assessment of pro- and anti-inflammatory cytokines are needed.
Footnotes
Author Contributions: Billy A. Caceres has contributed to conception, design, and acquisition; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Veronica Barcelona contributed to analysis and interpretation; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Danny Vo contributed to acquisition, analysis, and interpretation; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Niurka Suero-Tejeda contributed to conception, acquisition, analysis, interpretation, and design; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Kasey Jackman contributed to analysis and interpretation; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Jacquelyn Taylor contributed to interpretation; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Elizabeth Corwin contributed to interpretation; drafted the manuscript; critically revised the manuscript; gave the final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Nursing Research (P30NR016587; K01NR017010); the National Heart, Lung, and Blood Institute (K01HL146965); and the National Center for Advancing Translational Science (UL1TR001873).
ORCID iDs: Billy A. Caceres  https://orcid.org/0000-0001-6865-5546
https://orcid.org/0000-0001-6865-5546
Veronica Barcelona  https://orcid.org/0000-0003-3070-1716
https://orcid.org/0000-0003-3070-1716
Danny Vo  https://orcid.org/0000-0001-8769-994X
https://orcid.org/0000-0001-8769-994X
Elizabeth Corwin  https://orcid.org/0000-0002-9348-415X
https://orcid.org/0000-0002-9348-415X
References
- Andrade N., Ford A. D., Alvarez C. (2020). Discrimination and Latino health: A systematic review of risk and resilience. Hispanic Health Care International. 10.1177/1540415320921489 [DOI] [PubMed]
- Beatty D. L., Matthews K. A., Bromberger J. T., Brown C. (2014). Everyday discrimination prospectively predicts inflammation across 7-years in racially diverse midlife women: Study of women’s health across the nation. The Journal of Social Issues, 70(2), 298–314. 10.1111/josi.12061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boylan J. M., Robert S. A. (2017). Neighborhood SES is particularly important to the cardiovascular health of low SES individuals. Social Science and Medicine, 188, 60–68. 10.1016/j.socscimed.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan C. M., Unverzagt F. W., Hui S. L., Perkins A. J., Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–781. https://10.1097/01.MLR.0000024610.33213.C8 [DOI] [PubMed] [Google Scholar]
- Carroll M. D., Fryar C. D., Nguyen D. T. (2017). Total and high-density lipoprotein cholesterol in Adults: United States, 2015-2016. NCHS Data Brief, 290, 1–8. [PubMed] [Google Scholar]
- Dhabhar F. S. (2014). Effects of stress on immune function: The good, the bad, and the beautiful. Immunologic Research, 58(2–3), 193–210. 10.1007/s12026-014-8517-0 [DOI] [PubMed] [Google Scholar]
- Dinarello C. A. (2018). Overview of the IL-1 family in innate inflammation and acquired immunity. Immunological Reviews, 281(1), 8–27. 10.1111/imr.12621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales C., Carroll M., Fryar C., Ogden C. (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, 360(360), 1–8. http://www.ncbi.nlm.nih.gov/pubmed/26633046 [PubMed] [Google Scholar]
- Huang W. Y., Hsin I. L., Chen D. R., Chang C. C., Kor C. T., Chen T. Y., Wu H. M. (2017). Circulating interleukin-8 and tumor necrosis factor-α are associated with hot flashes in healthy postmenopausal women. PLoS One, 12(8), 2–13. 10.1371/journal.pone.0184011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw K. N., Lewis T. T., Roux A. V. D., Jenny N. S., Liu K., Penedo F. J., Carnethon M. R. (2016). Self-reported experiences of discrimination and inflammation among men and women: The multi-ethnic study of atherosclerosis. Health Psychology, 35(4), 343–350. 10.1037/hea0000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. J., Boden-Albala B., Larson E., Wilcox A., Bakken S. (2014). Online health information seeking behaviors of Hispanics in New York City: A community-based cross-sectional study. Journal of Medical Internet Research, 16(7), e176. 10.2196/jmir.3499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Jones D. M., Hong Y., Labarthe D., Mozaffarian D., Appel L. J., Van Horn L., Greenlund K., Daniels S., Nichol G., Tomaselli G. F., Arnett D. K., Fonarow G. C., Ho P. M., Lauer M. S., Masoudi F. A., Robertson R. M., Roger V., Schwamm L. H., Sorlie P.,…American Heart Association Strategic Planning Task Force and Statistics Committee. (2010). Defining and setting national goals for cardiovascular health promotion and disease reduction: The American heart association’s strategic impact goal through 2020 and beyond. Circulation, 121(4), 586–613. 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- Malutan A. M., Dan M., Nicolae C., Carmen M. (2014). Proinflammatory and anti-inflammatory cytokine changes related to menopause. Przeglad Menopauzalny, 13(3), 162–168. 10.5114/pm.2014.43818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazidi M., Katsiki N., Mikhailidis D. P., Banach M. (2019). Association of ideal cardiovascular health metrics with serum uric acid, inflammation and atherogenic index of plasma: A population-based survey. Atherosclerosis, 284, 44–49. 10.1016/j.atherosclerosis.2018.09.016 [DOI] [PubMed] [Google Scholar]
- McCurley J. L., Mills P. J., Roesch S. C., Carnethon M., Giacinto R. E., Isasi C. R., Teng Y., Sotres-Alvarez D., Llabre M. M., Penedo F. J., Schneiderman N., Gallo L. C. (2015). Chronic stress, inflammation, and glucose regulation in U.S. Hispanics from the HCHS/SOL sociocultural ancillary study. Psychophysiology, 52(8), 1071–1079. 10.1111/psyp.12430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendola N. D., Chen T. C., Gu Q., Eberhardt M. S., Saydah S. (2018). Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016. NCHS Data Brief, 319, 1–8. [PubMed] [Google Scholar]
- Morrisette-Thomas V., Cohen A. A., Fülöp T., Riesco É., Legault V., Li Q., Milot E., Dusseault-Bélanger F., Ferrucci L. (2014). Inflamm-aging does not simply reflect increases in pro-inflammatory markers. Mechanisms of Ageing and Development, 139(1), 49–57. 10.1016/j.mad.2014.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otiniano Verissimo A. D., Gee G. C., Iguchi M. Y., Ford C. L., Friedman S. R. (2013). Discrimination, drugs, and alcohol among Latina/os in Brooklyn, New York: Differences by gender. International Journal of Drug Policy, 24(4), 367–373. 10.1016/j.drugpo.2013.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. (2019). Hispanics with darker skin are more likely to experience discrimination than those with lighter skin. https://www.pewresearch.org/fact-tank/2019/07/02/hispanics-with-darker-skin-are-more-likely-to-experience-discrimination-than-those-with-lighter-skin/
- Santos H. P., Nephew B. C., Bhattacharya A., Tan X., Smith L., Alyamani R. A. S., Martin E. M., Perreira K., Fry R. C., Murgatroyd C. (2018). Discrimination exposure and DNA methylation of stress-related genes in Latina mothers. Psychoneuroendocrinology, 98, 131–138. 10.1016/j.psyneuen.2018.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva B. S. A., Lira F. S., Ramos D., Uzeloto J. S., Rossi F. E., Freire A. P. C. F., Silva R. N., Trevisan I. B., Gobbo L. A., Ramos E. M. C. (2018). Severity of COPD and its relationship with IL-10. Cytokine, 106(November 2017), 95–100. 10.1016/j.cyto.2017.10.018 [DOI] [PubMed] [Google Scholar]
- Simons R. L., Lei M.-K., Beach S. R. H., Barr A. B., Simons L. G., Gibbons F. X., Philibert R. A. (2018). Discrimination, segregation, and chronic inflammation: Testing the weathering explanation for the poor health of black Americans. Developmental Psychology, 54(10), 1993–2006. 10.1037/dev0000511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepanikova I., Bateman L. B., Oates G. R. (2017). Systemic inflammation in midlife: Race, socioeconomic status, and perceived discrimination. American Journal of Preventive Medicine, 52(1), S63–S76. 10.1016/j.amepre.2016.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundermann E. E., Hussain M. A., Moore D. J., Horvath S., Lin D. T. S., Kobor M. S., Levine A. (2019). Inflammation-related genes are associated with epigenetic aging in HIV. Journal of NeuroVirology, 25(6), 853–865. 10.1007/s13365-019-00777-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosatti J. A. G., Sóter M. O., Ferreira C. N., Silva I. de F. O., Cândido A. L., Sousa M. O., Reis F. M., Gomes K. B. (2020). The hallmark of pro- and anti-inflammatory cytokine ratios in women with polycystic ovary syndrome. Cytokine, 134(June), 155187. 10.1016/j.cyto.2020.155187 [DOI] [PubMed] [Google Scholar]
- Williams D. R., Yu Y., Jackson J. S., Anderson N. B. (1997). Racial differences in physical and mental health. Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]


